Abstract
Purpose
Transoral laser microsurgery (TOLMS) with carbon dioxide is a safe approach for laryngeal carcinoma. In literature there are three main methods for evaluating speech outcomes: acoustic and aerodynamics analysis, perceptual evaluation and patient-reported outcomes (PROs). The aim of this study was to systematically review the literature about the voice quality outcomes of TOLMS according to type of cordectomy.
Methods
A systematic literature review was performed and all the results until December 2021 were extrapolated. We evaluated the acoustic and aerodynamics parameters (fundamental frequency, harmonics to noise ratio, jitter, shimmer and maximum phonation time), perceptual data (GRBAS scale) and patient-related outcomes (VHI scale).
Results
24 studies met the inclusion criteria for a total number of 1207 patients enrolled. The number for each type of cordectomy are: 287 type I (23.78%), 311 type II (25.78%), 328 type III (27.14%), 129 type 4 (10.69%) and 152 type V (12.60%). Patients are grouped according to the type of cordectomy in: limited cordectomy (type I and II) and extended cordectomy (types III–IV–V). The difference between two groups is statistically significative in terms of acoustic analysis, perceptual data and patient-related outcomes (p < 0.05).
Conclusions
Patients who underwent type I or II cordectomy have significantly better quality of voice in terms of VHI, perceptual voice quality evaluations and acoustic parameters compared to type III, IV and V cordectomies. The effect of TOLMS on the voice should depend from the extent of the resection and in particular from the scar of the vocal muscle.
Keywords: Laser microsurgery, Laryngeal cancer, Voice outcomes, Systematic review
Introduction
Transoral laser microsurgery (TOLMS) with carbon dioxide (CO2) is a safe approach for laryngeal squamous cell carcinoma (LSCC) [1, 2] and is considered, such as the radiotherapy treatment, the standard of care for primary early stage (T1 and T2) LSCC. Several types of TOLMS are described and are classified according to the European Laryngological Society (ELS) Classification [3]. The laser CO2 cordectomy are: Type I subepithelial, Type II subligamental, Type III transmuscolar, Type IV total and Type V extended.
In literature the oncological outcomes of TOLMS have been extensively investigated by systematic reviews and meta-analysis. In fact, is clear that TOLMS and radiotherapy for early stage of LSCC are similar for overall survival [4], but TOLMS is favored due to lower costs and fewer post-treatment adverse events [5].
About the functional and vocal outcomes after TOLMS, in literature are present a lot of case series papers about single center experience, but at the best of our knowledge, is not present a systematic review on this topic. In literature there are three main methods for evaluating speech outcomes: acoustic analysis, perceptual evaluation [8] and patient-reported outcomes (PROs) [9]. The goal of the study is to review the literature regarding laser cordectomy to outline the voice profile in the various degrees of this type of intervention.
Materials and methods
Literature search strategy
Following the Preferred Reporting Items for Systematic and Meta-Analyses (PRISMA) guidelines, a systematic literature review was performed using MEDLINE, EMBASE, PubMed and Scopus databases. The search strategy was conducted using combinations of the following terms: “cordectomy and acoustic analysis” OR “cordectomy GRBAS” OR “cordectomy VHI” OR “cordectomy voice outcome” OR “vocal laser surgery GRBAS” OR “vocal laser surgery VHI”.
Study selection
For this review we considered and extrapolated all the results until December 2021. The papers considered for this review reported: abstract available in English language, type of cordectomy according to ELS and the results of voice outcomes after 6 months to 1 year from TOLMS (acoustic analysis, perceptual evaluation and PROs). We enrolled studies also with some of these analyses, because in literature, in general, there are present papers that analyzed just a few of speech outcomes.
We excluded articles with lacking information regarding the type of cordectomy, time of voice evaluation, previous RT treatment on the larynx and article in other languages or abstract unavailable.
Title and abstract were watchfully examined by two authors (A.C and C.D.E) independently, and disagreements were resolved by a discussion with a third author (M.R).
Data extraction
The full text of the included studies was reviewed and data extraction was performed using a standard registry database. The data registered in each case were: number of patients, type of cordectomy, acoustic and aerodynamics analysis (fundamental frequency, harmonics to noise ratio, jitter, shimmer and maximum phonation time), perceptual data (GRBAS scale) and PROs (VHI scale).
Voice outcomes
In this review we considered some outcomes widely used in literature. In the following section we introduce them and in Table 1 are resumed these parameters.
Table 1.
Parameters of voice outcomes analysed in this study
| Acoustic Analysis | Fundamental Frequency (F0): result of the rate of vibration of the (neo) glottis which oscillate in the airflow when appropriately tensed |
| Harmonics to Noise Ratio (HNR): ratio between the total energy of the periodic voice signal and the energy of noise components | |
| Jitter: relative variability in the F0 between contiguous (neo) glottal cycles | |
| Shimmer: relative variability in the amplitude of sound waves | |
| Aerodynamics Parameter | Maximum Phonation Time (MPT): the longest period during which a patient can sustain phonation of a vowel sound, typically /a/ |
| Perceptual Evaluation | GRBAS: Grade, Roughness, Breathiness, Asthenia, Strain scale assessment |
| Patient-Reported Outcomes (PROs) | VHI: Voice Handicap Index |
Acoustic and aerodynamics analysis
Quantitative acoustic measurements are more regularly studied and are obtained from tools that digitize and analyze the voice and quantify the characteristics [6, 7].
The parameters considered in this review are: fundamental frequency (F0), Noise Harmonics to Ratio (NHR), Jitter% (Jitt), Shimmer% (Shim).
The aerodynamics parameter is the maximum phonation time (MPT) measured (in seconds) with the pronunciation of/aa/as the primary value.
These outcomes are indicated in literature to obtain information about the pitch, the stability and the amount of noise components [8, 9].
Perceptual analysis
Another of the factors to take into account is the auditive perception generated in the listener and is evaluated by ways of perceived voice quality.
For the perceptual outcomes we have considered a well-established assessment tool, such as the GRBAS [10] scale in which are estimates the grade of hoarseness (G), roughness (R), breathiness (B), asthenia (A) and strain in the voice (S) on a scale from 0 to 3 (0, normal; 1, mild; 2, moderate; 3, severe).
Patient-reported outcomes (PROs)
The patient’s perceived voice quality in literature is evaluated questionnaires that give an idea of the subjective impact that a vocal problem produces in the subject. The patient-reported outcomes (PROs) mostly used in literature is the VHI scale [11].
The VHI consists in a questionnaire of 30 items: 10 items on emotional issues, 10 items on physical issues, and 10 items on functional issues. Scoring is from 0 to 120, with 120 representing the maximum perceived disability. Each item is scored on a four point scale: 0 = never, 1 = almost never, 2 = sometimes, 3 = almost always, and 4 = always. A VHI score of 0–40 points indicate a handicap of slight impact, a score of 41–60 indicates moderate impact, and a score of 61 indicates severe impact.
Statistical methods
All statistical analyses were performed using SPSS Version 25.0 (IBM Corp, Armonk, NY, USA). Descriptive analyses were mainly applied. Data are indicated as mean, range and percentage. Student t test was used for outcome comparisons between groups of patients. A level of significance of p < 0.05 was used.
Results
Search results, data synthesis and analysis
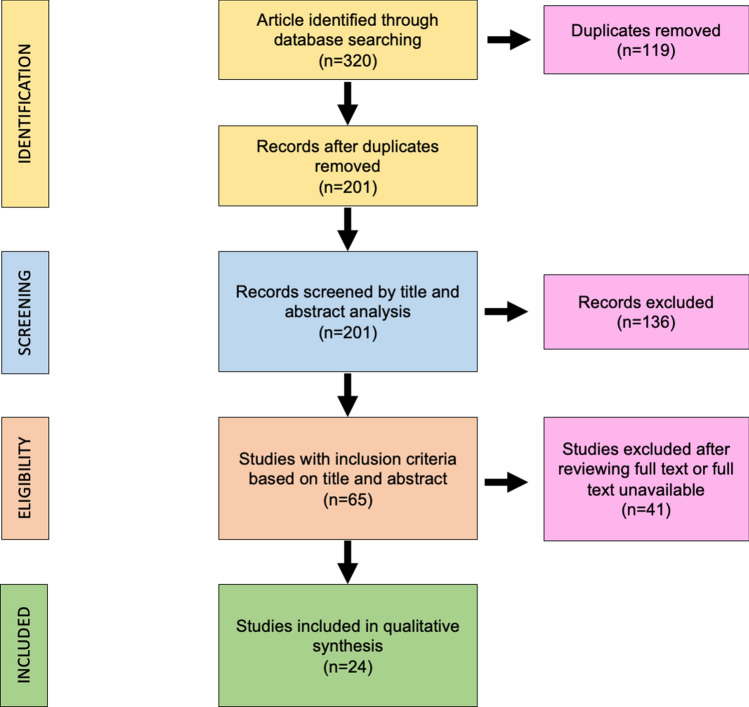
The search algorithm and review results are outlined in Fig. 1.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram followed in this review. The diagram shows the information flow through the different phases of the review and illustrates the number of records that were identified and included
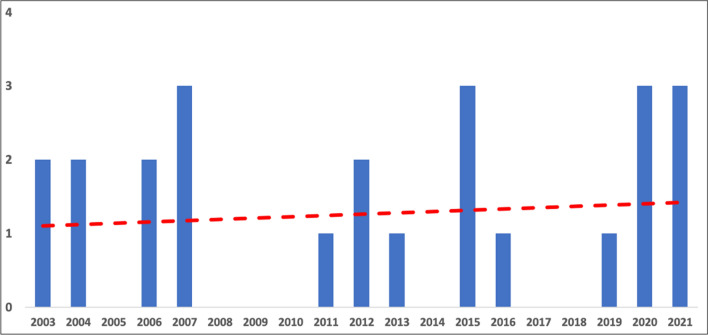
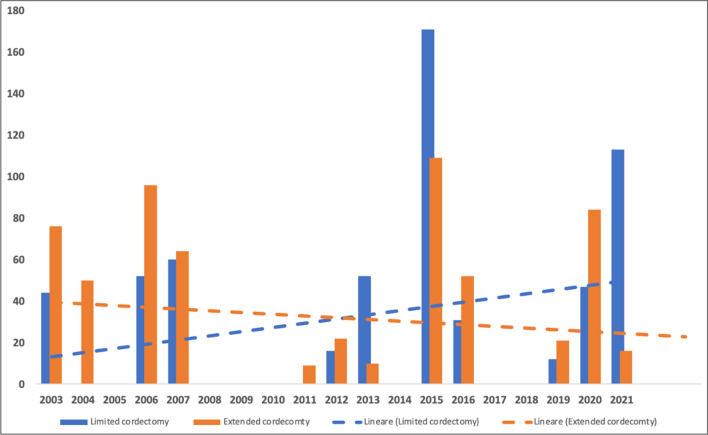
The initial search found 320 studies on the MEDLINE database, EMBASE, Scopus and the Cochrane Library databases. The removal of duplicates identified 201 publications. All the 201 papers were screened in title and abstract, and 65 manuscripts were reviewed in full text. Of these, 24 studies met the inclusion criteria, while the remaining 41 studies were excluded. The included studies were published in peer-reviewed journals. The data collected from each study were transcribed in a tabular form. In Fig. 2 is report the histogram with the number of studies considered for years of publication, and in Fig. 3, the type of cordectomy performed along the time.
Fig. 2.
Histogram with the number of papers for every year. In red is the trend line of published articles considered in this review
Fig. 3.
Histogram of type of cordectomy (limited or extended) for every year. The trend lines show an increment of limited cordectomy and a progressive reduction of extended cordectomy
Studies considered in this review, the total number of patients for each study and the number of patients according to the type of cordectomy are reported in Table 2.
Table 2.
Papers considered in this review and patients subdivided according to ELS cordectomy classification
| Author | Year | Total patients of the study | Type of cordectomy according to ELS classification | Number of patients |
|---|---|---|---|---|
| Peretti et al. [12] | 2003 | 69 | Type I | 7 |
| Type II | 11 | |||
| Type III | 21 | |||
| Type IV | 14 | |||
| Type V | 16 | |||
| Peretti et al. [13] | 2003 | 51 | Types I–II | 26 |
| Types III–IV–V | 25 | |||
| Krengli et al. [14] | 2004 | 30 | Types III–IV | 30 |
| Policarpo et al. [15] | 2004 | 20 | Type III | 7 |
| Type IV | 13 | |||
| Haddad et al. [16] | 2006 | 15 | Type I | 3 |
| Type II | 5 | |||
| Type III | 4 | |||
| Type IV | 3 | |||
| Ledda et al. [17] | 2006 | 133 | Type I | 16 |
| Type II | 28 | |||
| Type III | 31 | |||
| Type IV | 13 | |||
| Type V | 45 | |||
| Roh et al. [18] | 2007 | 75 | Types I–II | 45 |
| Types III–IV | 17 | |||
| Type V | 13 | |||
| Xu et al. [19] | 2007 | 30 | Types III–IV | 30 |
| Vilaseca et al. [20] | 2007 | 19 | Types I–II | 15 |
| Type V | 4 | |||
| Chu et al. [21] | 2011 | 9 | Type III | 9 |
| Chu et al. [22] | 2012 | 25 | Types I–II | 13 |
| Types III–IV–V | 12 | |||
| Galletti et al. [23] | 2012 | 13 | Type II | 3 |
| Type III | 6 | |||
| Type IV | 4 | |||
| Bahannan et al. [24] | 2013 | 62 | Types I–II | 52 |
| Types III–IV–V | 10 | |||
| Bertino et al. [25] | 2015 | 101 | Types I–II | 66 |
| Types III–IV | 35 | |||
| Greulich et al. [26] | 2015 | 179 | Types I–II | 105 |
| Type III | 74 | |||
| Lee et al. [27] | 2016 | 57 | Types I–II | 21 |
| Types III–IV–V | 36 | |||
| Fink et al. [28] | 2016 | 26 | Type I | 7 |
| Type II | 3 | |||
| Type III | 12 | |||
| Type V | 4 | |||
| Del Mundo et al. [29] | 2019 | 33 | Type I | 8 |
| Type II | 4 | |||
| Type III | 21 | |||
| Hamzany et al. [30] | 2020 | 55 | Types I–II | 34 |
| Types III–IV–V | 21 | |||
| Kosztyła-Hojna et al. [31] | 2020 | 30 | Type III | 13 |
| Type IV | 6 | |||
| Type V | 11 | |||
| Şencan et al. [32] | 2020 | 46 | Types I–II | 13 |
| Type III | 16 | |||
| Types IV–V | 17 | |||
| Lechien et al. [5] | 2021 | 60 | Type I | 30 |
| Type II | 30 | |||
| Song et al. [33] | 2021 | 51 | Type I | 24 |
| Type II | 18 | |||
| Type III | 9 | |||
| Staníková et al. (34) | 2021 | 18 | Types I–II | 11 |
| Types III–IV–V | 7 |
Study cohort
A total of 1207 patients were enrolled in this review. The number of patients for each type of cordectomy are: 287 type I (23.78%), 311 type II (25.78%), 328 type III (27.14%), 129 type 4 (10.69%) and 152 type V (12.60%).
In almost all studies considered for the vocal analysis the patients are grouped according to the type of cordectomy in: limited cordectomy (type I and II) and extended cordectomy (types III–IV–V). For this reason, in this we review we follow the same division to create a population of patients as homogeneous as possible. Among the limited cordectomy we found 598 (49.5%) patients and for extended cordectomy 609 (50.5%). The study cohort characteristics are resumed in Table 3.
Table 3.
Study cohort characteristics
| Total patients | 1207 |
|---|---|
| Type of cordectomy | |
| • Type 1 | 287 (23.78%) |
| • Type 2 | 311 (25.78%) |
| • Type 3 | 328 (27.14%) |
| • Type 4 | 129 (10.69%) |
| • Type 5 | 152 (12.6%) |
| Limited cordectomy | |
| • Type I + II | 598 (49,5%) |
| Extended cordectomy | |
| ● Type III + IV + V | 609 (50,5%) |
Voice outcomes
Subjective and objective voice quality outcomes after limited or extended cordectomy are resumed in Table 4. The difference of every parameter is statistically significative between two groups; the only parameter that is not statistically significative is the Harmonics to Noise Ratio (HNR). About the acoustic outcomes the mean F0 for limited cordectomy is 153.57 ± 18.01 Hz and for extended cordectomy is 171.13 ± 22.3 Hz. The difference was statistically significative (p < 0.05). The difference for jitter, shimmer and MPT is statistically significative between the two groups of cordectomy.
Table 4.
Vocal outcomes in the sub-group of cordectomy
| Limited cordectomy | Extended cordectomy | p (95% CI) | |
|---|---|---|---|
| Acoustic parameters | |||
| • F0 (Hz) | 153.57 ± 18.01 | 171.13 ± 22.32 | p = 0.02* |
|
• HNR • Jitter (%) |
0.22 ± 0.20 1.61 ± 0.72 |
0.36 ± 0.31 3.43 ± 2.33 |
p = 0.193** p = 0.0013* |
| • Shimmer (%) | 6.66 ± 4.13 | 10.77 ± 4.88 | p = 0.0046* |
| Aerodynamics parameter | |||
| • MPT (seconds) | 13.87 ± 2.73 | 9.68 ± 3.22 | p = 0.002* |
| GRBAS scale | |||
| • Grade of hoarseness (G) | 1.16 ± 0.34 | 1.65 ± 0.37 | p = 0.0008* |
| • Roughness (R) | 1.08 ± 0.23 | 1.64 ± 0.76 | p = 0.037* |
| • Breathiness (B) | 0.78 ± 0.41 | 1.33 ± 0.61 | p = 0.0051* |
| • Asthenia (A) | 0.35 ± 0.39 | 0.88 ± 0.63 | p = 0.0233* |
| • Strain in the voice (S) | 0.70 ± 0.43 | 1.34 ± 0.92 | p = 0.0277* |
| • Total | 4.09 ± 0.79 | 6.25 ± 2 | p = 0.0009* |
| VHI scale | 15.09 ± 6.77 | 28.67 ± 12.46 | p = 0.0012* |
*p statistically significative
**p no statistically significative
The GRBAS scale total is statistically different (p = 0.0009) and similarly each parameter is statistically different. The mean value of VHI evaluation for limited cordectomy is 15.09 ± 6.77 and for extended cordectomy is 28.67 ± 12.46 and the difference is statistically significative (p = 0.0012).
Discussion
The best objective to achieve during microsurgery on larynx is a compromise between oncological radicality, vocal fold function and impact on the quality of life of the patients [35]. In general, in the field of oncological surgery, quality of voice is secondary to the radical oncological excision of the neoplasm. However, is important to analyze the impact on the vocal outcome and quality of life.
Almost all papers on this topic present in literature, comparing the voice outcomes after TOLMS and RT in LSCC treatment. The results are contradictory; some works show a better voice outcome after TOLMS [36, 37], some better voice after RT [38, 39] and other found no statistically significant difference between RT and TOLMS [40].
To date in literature is not present a systematic review analyzing vocal outcomes according to each type of cordectomy. In this review we analyze only the most frequent parameters reported in literature, but one of the most important and useful tools in the assessment of the voice function is laryngophotography. This includes: High definition laryngophotography, Ultra high speed laryngophotography to study the various parameters of the glottic wave which relates well to the quality of voice, as well as Laryngostroboscopy [41].
When comparing the voice parameters of limited cordectomy (subepithelial and subligamental) and extended cordectomy (transmuscolar, total and extended), the results are better for limited: F0, Jitter and Shimmer are statistically different from extended cordectomy. The only acoustic parameter that is not better is the HNR. The Aerodynamics parameter (MPT) is statistically different between the two group of cordectomies too.
Voice one of the most important relational tools and the auditive perception generated in the listener is an outcome analyzed in literature. For this reason, some scales are proposed and approved, such as GRBAS [10] and IINFV0 [42, 43]. The most diffuse in literature is GRBAS and in this review we found a statistically significative difference between limited and extended cordectomy for each parameter (G, R, B, A, S) and for the total score.
The last parameters are the patient-reported outcomes (PROs) and represent the patient’s perceived voice quality. In this review we considered the Voice Handicap Index, the scale largely diffuses in literature. Despite the spread of rapid and economic self-evaluation methods, such as VHI, is important to underline that the questionnaires collecting data about the patient's own evaluation of voice is very subjective, and liable to uncertainties and fallacies.
The VHI scale analysis shown, such as GRBAS and acoustic parameters, a statistically significative difference from limited to extended cordectomy.
These results in each field (acoustic parameters, perceptual analysis and PRO’s) between the extension of cordectomy should be explained by the alteration and subsequent regeneration of laryngeal structures, such as vocal ligament and vocal muscle (thyro-arytenoid muscle).
The cordectomies I and II reach the tissues superficial to the vocal ligament. Any deeper excision shall traumatize the vocal ligament leading to healing by fibrosis which will affect the free mobility of the vocal fold mucosa on the deeper structures, leading to various degrees of derangement of the vocal function. Limited cordectomies shall derange the voice function due to interference with the layered structure of the vocal fold, creating scars of various extends and depths. These scars most probably disturb the regular glottic wave, thus affecting the voice quality. On the other hand, extended cordectomies, shall add an important organic factor to the derangement in addition to the disturbed vocal fold layered structure and scarring. This added factor is the reduction of the bulk of the vocal fold due to the excision of parts of the thyro-arytenoid muscle, leaving the glottis with one vibrator, the healthy non-operated vocal fold.
The vocal muscle does not participate in the vibratory mechanism of voice production, but it helps in the approximation of the vocal folds leading to good closure of the glottis allowing the aerodynamic processes to produce good vibrations at the vocal folds' mucosal edges. The scarring of the vocal muscle may not be the mechanism worsening of the voice results with the extended cordectomy group.
The future prospects are approaches of regenerative medicine to improve the vocal fold vibration and muscle contraction.
Conclusions
This review underlines that patients who underwent type I or II cordectomy have significantly better quality of voice in terms of VHI, perceptual voice quality evaluations and acoustic parameters compared to type III, IV and V cordectomies. The effect of TOLMS on the voice should depend from the extent of the resection and in particular from the scar of the vocal muscle. At the best of our knowledge this is the first review comparing the vocal outcomes after cordectomies according to the type of resection.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. The authors received no financial support for the research, authorship, and/or publication of this article.
Declarations
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics statement
All the investigations detailed in the manuscript have been conducted in accordance with the Declaration of Helsinki and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
9/2/2022
Missing Open Access funding information has been added in the Funding Note.
References
- 1.De Seta D, Campo F, D'Aguanno V, Ralli M, Greco A, Russo FY, de Vincentiis M. Transoral laser microsurgery for Tis, T1, and T2 glottic carcinoma: 5-year follow-up. Lasers Med Sci. 2021;36(3):507–512. doi: 10.1007/s10103-020-03049-4. [DOI] [PubMed] [Google Scholar]
- 2.Gallo A, de Vincentiis M, Manciocco V, Simonelli M, Fiorella ML, Shah JP. CO2 laser cordectomy for early-stage glottic carcinoma: a long-term follow-up of 156 cases. Laryngoscope. 2002;112(2):370–374. doi: 10.1097/00005537-200202000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Remacle M, Eckel HE, Antonelli A, Brasnu D, Chevalier D, Friedrich G, Olofsson J, Rudert HH, Thumfart W, de Vincentiis M, Wustrow TP. Endoscopic cordectomy. A proposal for a classification by the working committee, European laryngological society. Eur Arch Otorhinolaryngol. 2000;257(4):227–231. doi: 10.1007/s004050050228. [DOI] [PubMed] [Google Scholar]
- 4.Campo F, Zocchi J, Ralli M, De Seta D, Russo FY, Angeletti D, Minni A, Greco A, Pellini R, de Vincentiis M. Laser microsurgery versus radiotherapy versus open partial laryngectomy for T2 laryngeal carcinoma: a systematic review of oncological outcomes. Ear Nose Throat J. 2021;100(1_suppl):51S–58S. doi: 10.1177/0145561320928198. [DOI] [PubMed] [Google Scholar]
- 5.Lechien JR, Crevier-Buchman L, Circiu MP, Lisan Q, Hans S. Evolution of voice quality in type 1–2 transoral CO2 laser cordectomy: a prospective comparative study. Laryngoscope. 2021 doi: 10.1002/lary.29924. [DOI] [PubMed] [Google Scholar]
- 6.Li G, Hou Q, Zhang C, Jiang Z, Gong S. Acoustic parameters for the evaluation of voice quality in patients with voice disorders. Ann Palliat Med. 2021;10(1):130–136. doi: 10.21037/apm-20-2102. [DOI] [PubMed] [Google Scholar]
- 7.Maslan J, Leng X, Rees C, Blalock D, Butler SG. Maximum phonation time in healthy older adults. J Voice. 2011;25(6):709–713. doi: 10.1016/j.jvoice.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van As-Brooks CJ, Koopmans-van Beinum FJ, Pols LC, Hilgers FJ. Acoustic signal typing for evaluation of voice quality in tracheoesophageal speech. J Voice. 2006;20(3):355–368. doi: 10.1016/j.jvoice.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Dejonckere PH, Moerman MB, Martens JP, Schoentgen J, Manfredi C. Voicing quantification is more relevant than period perturbation in substitution voices: an advanced acoustical study. Eur Arch Otorhinolaryngol. 2012;269(4):1205–1212. doi: 10.1007/s00405-011-1900-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hirano M. Psycho-acoustic evaluation of voice. In: Arnold GE, Winckel F, Wyke BD, editors. Clinical examination of voice. New York: Springer-Verlag; 1981. pp. 81–84. [Google Scholar]
- 11.Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS, Newman CW. The voice handicap index (VHI) development and validation. Am J Speech Lang Pathol. 1997;6(3):66–70. doi: 10.1044/1058-0360.0603.66. [DOI] [Google Scholar]
- 12.Peretti G, Piazza C, Balzanelli C, Cantarella G, Nicolai P. Vocal outcome after endoscopic cordectomies for Tis and T1 glottic carcinomas. Ann Otol Rhinol Laryngol. 2003;112(2):174–179. doi: 10.1177/000348940311200212. [DOI] [PubMed] [Google Scholar]
- 13.Peretti G, Piazza C, Balzanelli C, Mensi MC, Rossini M, Antonelli AR. Preoperative and postoperative voice in Tis-T1 glottic cancer treated by endoscopic cordectomy: an additional issue for patient counseling. Ann Otol Rhinol Laryngol. 2003;112(9 Pt 1):759–763. doi: 10.1177/000348940311200903. [DOI] [PubMed] [Google Scholar]
- 14.Krengli M, Policarpo M, Manfredda I, Aluffi P, Gambaro G, Panella M, Pia F. Voice quality after treatment for T1a glottic carcinoma–radiotherapy versus laser cordectomy. Acta Oncol. 2004;43(3):284–289. doi: 10.1080/02841860410026233. [DOI] [PubMed] [Google Scholar]
- 15.Policarpo M, Aluffi P, Brovelli F, Borello G, Pia F. Oncological and functional results of CO2 laser cordectomy. Acta Otorhinolaryngol Ital. 2004;24(5):267–274. [PubMed] [Google Scholar]
- 16.Haddad L, Abrahão M, Cervantes O, Ceccon FP, Gielow I, Carvalho JR, Leonhardt FD. Vocal assessment in patients submited to CO2 laser cordectomy. Braz J Otorhinolaryngol. 2006;72(3):295–301. doi: 10.1016/s1808-8694(15)30960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ledda GP, Grover N, Pundir V, Masala E, Puxeddu R. Functional outcomes after CO2 laser treatment of early glottic carcinoma. Laryngoscope. 2006;116(6):1007–1011. doi: 10.1097/01.MLG.0000217557.45491.BD. [DOI] [PubMed] [Google Scholar]
- 18.Roh JL, Kim DH, Kim SY, Park CI. Quality of life and voice in patients after laser cordectomy for Tis and T1 glottic carcinomas. Head Neck. 2007;29(11):1010–1016. doi: 10.1002/hed.20625. [DOI] [PubMed] [Google Scholar]
- 19.Xu W, Han D, Hou L, Zhang L, Yu Z, Huang Z. Voice function following CO2 laser microsurgery for precancerous and early-stage glottic carcinoma. Acta Otolaryngol. 2007;127(6):637–641. doi: 10.1080/00016480600987776. [DOI] [PubMed] [Google Scholar]
- 20.Vilaseca I, Huerta P, Blanch JL, Fernández-Planas AM, Jiménez C, Bernal-Sprekelsen M. Voice quality after CO2 laser cordectomy–what can we really expect? Head Neck. 2008;30(1):43–49. doi: 10.1002/hed.20659. [DOI] [PubMed] [Google Scholar]
- 21.Chu PY, Hsu YB, Lee TL, Fu S, Wang LM, Kao YC. Modified type III cordectomy to improve voice outcomes after transoral laser microsurgery for early glottic canser. Head Neck. 2012;34(10):1422–1427. doi: 10.1002/hed.21936. [DOI] [PubMed] [Google Scholar]
- 22.Chu PY, Hsu YB, Lee TL, Fu S, Wang LM, Kao YC. Longitudinal analysis of voice quality in patients with early glottic cancer after transoral laser microsurgery. Head Neck. 2012;34(9):1294–1298. doi: 10.1002/hed.21914. [DOI] [PubMed] [Google Scholar]
- 23.Galletti B, Freni F, Cammaroto G, Catalano N, Gangemi G, Galletti F. Vocal outcome after CO2 laser cordectomy performed on patients affected by early glottic carcinoma. J Voice. 2012;26(6):801–805. doi: 10.1016/j.jvoice.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Bahannan AA, Slavíček A, Černý L, Vokřal J, Valenta Z, Lohynska R, Chovanec M, Betka J. Effectiveness of transoral laser microsurgery for precancerous lesions and early glottic cancer guided by analysis of voice quality. Head Neck. 2014;36(6):763–767. doi: 10.1002/hed.23368. [DOI] [PubMed] [Google Scholar]
- 25.Bertino G, Degiorgi G, Tinelli C, Cacciola S, Occhini A, Benazzo M. CO2 laser cordectomy for T1–T2 glottic cancer: oncological and functional long-term results. Eur Arch Otorhinolaryngol. 2015;272(9):2389–2395. doi: 10.1007/s00405-015-3629-2. [DOI] [PubMed] [Google Scholar]
- 26.Greulich MT, Parker NP, Lee P, Merati AL, Misono S. Voice outcomes following radiation versus laser microsurgery for T1 glottic carcinoma: systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2015;152(5):811–819. doi: 10.1177/0194599815577103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee HS, Kim JS, Kim SW, Noh WJ, Kim YJ, Oh D, Hong JC, Lee KD. Voice outcome according to surgical extent of transoral laser microsurgery for T1 glottic carcinoma. Laryngoscope. 2016;126(9):2051–2056. doi: 10.1002/lary.25789. [DOI] [PubMed] [Google Scholar]
- 28.Fink DS, Sibley H, Kunduk M, Schexnaildre M, Kakade A, Sutton C, McWhorter AJ. Subjective and objective voice outcomes after transoral laser microsurgery for early glottic cancer. Laryngoscope. 2016;126(2):405–407. doi: 10.1002/lary.25442. [DOI] [PubMed] [Google Scholar]
- 29.Del Mundo DAA, Morimoto K, Masuda K, Iwaki S, Furukawa T, Teshima M, Shinomiya H, Miyawaki D, Otsuki N, Sasaki R, Nibu KI. Oncologic and functional outcomes of transoral CO2 laser cordectomy for early glottic cancer. Auris Nasus Larynx. 2020;47(2):276–281. doi: 10.1016/j.anl.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Hamzany Y, Crevier-Buchman L, Lechien JR, Bachar G, Brasnu D, Hans S. Multidimensional voice quality evaluation after transoral CO2 laser cordectomy: a prospective study. Ear Nose Throat J. 2021;100(1_suppl):27S–32S. doi: 10.1177/0145561320906328. [DOI] [PubMed] [Google Scholar]
- 31.Kosztyła-Hojna B, Łuczaj J, Berger G, Duchnowska E, Zdrojkowski M, Łobaczuk-Sitnik A, Biszewska J. Perceptual and acoustic voice analysis in patients with glottis cancer after endoscopic laser cordectomy. Otolaryngol Pol. 2020;74(3):23–28. doi: 10.5604/01.3001.0013.7850. [DOI] [PubMed] [Google Scholar]
- 32.Şencan Z, Cömert E, Tunçel Ü, Kılıç C. Voice and quality-of-life outcomes of diode laser for Tis-T1a glottic cancer. Ear Nose Throat J. 2020;99(4):229–234. doi: 10.1177/0145561319839868. [DOI] [PubMed] [Google Scholar]
- 33.Song W, Caffier F, Nawka T, Ermakova T, Martin A, Mürbe D, Caffier PP. T1a Glottic cancer: advances in vocal outcome assessment after transoral CO2-laser microsurgery using the VEM. J Clin Med. 2021;10(6):1250. doi: 10.3390/jcm10061250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Staníková L, Zeleník K, Formánek M, Seko J, Walderová R, Kántor P, Komínek P. Evolution of voice after transoral laser cordectomy for precancerous lesions and early glottic cancer. Eur Arch Otorhinolaryngol. 2021;278(8):2899–2906. doi: 10.1007/s00405-021-06751-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zeitels SM. Premalignant epithelium and microinvasive cancer of the vocal fold: the evolution of phonomicrosurgical management. Laryngoscope. 1995;105(suppl 3):1–4. doi: 10.1288/00005537-199503001-00001. [DOI] [PubMed] [Google Scholar]
- 36.Gandhi S, Gupta S, Rajopadhye G. A comparison of phonatory outcome between trans-oral CO2 Laser cordectomy and radiotherapy in T1 glottic cancer. Eur Arch Otorhinolaryngol. 2018;275(11):2783–2786. doi: 10.1007/s00405-018-5152-8. [DOI] [PubMed] [Google Scholar]
- 37.Loughran S, Calder N, MacGregor FB, Carding F, Mackenzie K. Quality of life and voice following endoscopic resection or radiotherapy for early glottic cancer. Clin Otolaryngol. 2005;30:42–47. doi: 10.1111/j.1365-2273.2004.00919.x. [DOI] [PubMed] [Google Scholar]
- 38.Aaltonen L-M, et al. Voice quality after treatment of early vocal cord cancer: a randomized trial comparing laser surgery with radiation therapy. Int J Radiat Oncol. 2014;90(2):255–260. doi: 10.1016/j.ijrobp.2014.06.032. [DOI] [PubMed] [Google Scholar]
- 39.Taylor SM, Kerr P, et al. Treatment of T1b glottic SCC: laser vs. radiation- a Canadian multicenter study. J Otolaryngol Head Neck Surg. 2013;42:22–25. doi: 10.1186/1916-0216-42-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Demir B, Binnetoglu A, Gurol E, Oysu C. Comparison of voice quality of life in early stage glottic carcinoma treated with endoscopic cordectomy using radiofrequency microdissection electrodes, laser cordectomy, and radiotherapy. J Voice. 2021;35(3):477–482. doi: 10.1016/j.jvoice.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Yang Y, Fang J, Zhong Q, Xu W, Ma H, Feng L, Shi Q, Lian M, Wang R, Hou L. The value of narrow band imaging combined with stroboscopy for the detection of applanate indiscernible early-stage vocal cord cancer. Acta Otolaryngol. 2018;138(4):400–406. doi: 10.1080/00016489.2017.1388542. [DOI] [PubMed] [Google Scholar]
- 42.Moerman MB, Martens JP, Van der Borgt MJ, Peleman M, Gillis M, Dejonckere PH. Perceptual evaluation of substitution voices: development and evaluation of the (I)INFVo rating scale. Eur Arch Otorhinolaryngol. 2006;263(2):183–187. doi: 10.1007/s00405-005-0960-z. [DOI] [PubMed] [Google Scholar]
- 43.Moerman M, Martens JP, Crevier-Buchman L, de Haan E, Grand S, Tessier C, Woisard V, Dejonckere P. The INFVo perceptual rating scale for substitution voicing: development and reliability. Eur Arch Otorhinolaryngol. 2006;263(5):435–439. doi: 10.1007/s00405-005-1033-z. [DOI] [PubMed] [Google Scholar]