Abstract
Background
Cardiovascular disease (CVD) is the leading cause of disease burden in the world by non-communicable diseases. Nutritional interventions promoting high-quality dietary patterns with low caloric intake value and high nutrient density (ND) could be linked to a better control of CVD risk and recurrence of coronary disease. This study aims to assess the effects of a dietary intervention based on MedDiet or Low-Fat dietary intervention over changes in ND and food intake after 1 and 7 years of follow-up of the CORDIOPREV study.
Methods
We prospectively analyzed the results of the 802 coronary patients randomized to two healthy dietary patterns (MedDiet = 425, Low-Fat Diet = 377) who completed the 7 years of follow-up and had all the dietary data need. Dietary intake information obtained from a validated 137-item Food Frequency Questionnaire was used to calculate 1- and 7-year changes in dietary intake and ND (measured as nutrient intake per 1000 kcal). T test was used to ascertain differences in food intake and ND between groups across follow-up time. Within-subject (dietary allocation group) differences were analyzed with ANOVA repeated measures.
Results
From baseline to 7 years of follow-up, significant increases of vegetables, fruits, and whole cereals within groups (p < 0.001) was found. We found a higher increase in dietary intake of certain food groups with MedDiet in comparison with Low-Fat Diet for vegetables (46.1 g/day vs. 18.1 g/day, p < 00.1), fruits (121.3 g/day vs. 72.9 g/day), legumes (4.3 g/day vs. 0.16 g/day) and nuts (7.3 g/day vs. − 3.7 g/day). There was a decrease in energy intake over time in both groups, slightly higher in Low-Fat Diet compared to MedDiet group (− 427.6 kcal/day vs. − 279.8 kcal/day at 1st year, and − 544.6 kcal/day vs. − 215.3 kcal/day after 7 years of follow-up). ND of all the nutrients increased within group across follow-up time, except for Saturated Fatty Acids (SFA), cholesterol and sodium (p < 0.001).
Conclusions
A comprehensive dietary intervention improved quality of diet, reducing total energy intake and increasing the intake of healthy food groups and overall ND after 1 year and maintaining this trend after 7 years of follow-up. Our results reinforce the idea of the participation in trials, enhance nutrition literacy and produces better nutritional outcomes in adult patients with established CVD.
Clinical trial registry
The trial was registered in 2009 at ClinicalTrials.gov (number NCT00924937).
Keywords: Mediterranean diet, Low-fat diet, Dietary intervention, Nutrient density, Dietary intake, Cardiovascular disease
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the world, accounting for a combined 18 million deaths in 2020 [1]. Despite of this rate, the number of patients with established CVD is growing in developed countries as a result of improved survival after acute vascular events and ageing population [2], which implies very high healthcare expenditures derived directly or indirectly from their care [3].
The risk of future cardiovascular events is higher in subjects with established CVD compared with those without this previous condition [4]. Recurrence of CVD is associated to unhealthy lifestyle habits, such as physical inactivity and poor dietary habits [5]. Regarding diet, potential favourable effects of healthy dietary patterns on CVD prevention have been ascribed to the intake of low energy-dense food groups as vegetables and fruits, legumes, whole-grains and nuts, instead of processed products and sugar-sweetened beverages providing the necessary amount of nutrients but with a low energy content [6, 7]. That is, not only the total energy is important, but also the nutritional value of the overall dietary pattern prescribed. The nutrient density (ND) is used as a measure of the quality of the diet, and it indicates the ratio of the nutrients present in a diet according to its caloric value [8].
Nutritional education interventions are comprehensive programmes based on healthy dietary behaviour deliver to patients aimed at improving patients’ clinical outcomes through the increase and maintenance of health behaviour [9]. Although some epidemiological studies as the INTERSTROKE case–control study [10] or Lyon study [11] showed that adherence to a healthy dietary pattern plays a preventive role in secondary CVD, to our knowledge, no large clinical trial on established CVD has assessed whether dietary intervention increases the quality of the food intake and ND after a long period of intervention.
The CORonary Diet Intervention with Olive oil and cardiovascular PREVention study (the CORDIOPREV study) is a large trial which randomized established CVD patients to follow a MedDiet (rich in olive oil) or a Low-Fat Diet for secondary prevention. The aim of the CORDIOPREV study is to compare the appearance of a composite of cardiovascular major events recurrence after an average follow-up of 7 years, supporting a causal association between adherence to both dietary patterns and diet quality over recurrence of coronary events [12].
The purpose of the present study was to assess the effects of a dietary intervention based on MedDiet or Low-Fat dietary intervention over changes in nutrient density (ND) and food intake after 1 and 7 years of follow-up of the CORDIOPREV study.
Methods
Design of the study
A detailed description of the design and methods of the CORonary Diet Intervention with Olive Oil and Cardiovascular PREVention (CORDIOPREV) study can be found elsewhere [12]. Briefly, the CORDIOPREV study was a 7-year unicentric, randomized, parallel-group, secondary prevention trial conducted in Spain, to compare 2 controlled dietary interventions: (a) Mediterranean-type diet, vs. (b) low-fat diet, on the risk of suffering new CVD.
Ethics approval
The protocol was written in accordance with the principles of the Declaration of Helsinki. The respective Institutional Review Board (IRB) by the Human Investigation Review Committee of the Reina Sofia University Hospital (Córdoba, Spain) approved the study protocol. The trial was registered in 2009 at ClinicalTrials.gov (number NCT00924937). Recruitment took place from July 2009 to February 2012. All subjects provided written informed consent.
Participants and data collection procedures.
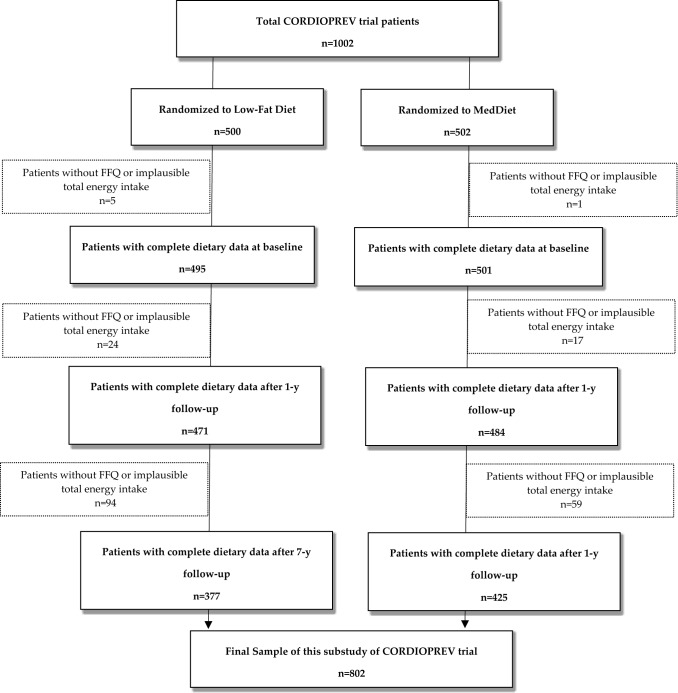
Eligible participants were men and women (aged over 20, but under 76 years) who had established CVD and without any clinical events in the previous 6 months, no severe illnesses or an expected life expectancy lower than the length of the study. From the 1002 participants recruited to the CORDIOPREV Study, we selected for the present longitudinal analysis those participants who completed at baseline and at 7 years of follow-up a Food Frequency Questionnaire (FFQ) and a Low-fat and Mediterranean Diet baseline adherence questionnaire. Those who failed to complete the FFQ were excluded from this sub-study. Among the available participants, we also excluded those individuals with extreme values for total energy intake in FFQ (< 800 kcal/day or > 4000 kcal/day for men; < 500 kcal/day or > 3500 kcal/day for women) according to the established criteria proposed by Willet et al. [13]. Finally, data from 802 participants were included in our analyses (Fig. 1). According to Fig. 1, 200 participants (around 20% of overall sample), did not complete the assessment of dietary intake after 7 years of follow-up. Considering that this attrition could introduce bias in our study, we performed an ancillary analyses comparing the characteristics of the participants without data at 7 years with those who completed the follow-up period.
Fig. 1.
Flow chart of Participants from the CORDIOPREV trial included in this substudy
Dietary Intervention and adherence appraisal
Participants randomized to the MedDiet group were instructed to follow a Mediterranean Diet, with a minimum of 35% of calories as fat (22% Monounsaturated fat (MUFA), 6% Polyunsaturated fat (PUFA) and < 10% Saturated fat (SFA)), 15% proteins and a maximum of 50% carbohydrates. On the other hand, participants allocated in Low-Fat Diet followed a diet with less than 30% of total fat (< 10% SFA, 12–14% MUFA AND 6–8% PUFA), 15% protein and a minimum 55% carbohydrates. Trained dietitians conducted group sessions and individual motivational interview at inclusion and every 6 months. These sessions consisted of dietary counselling and informative talks reinforcing the dietary habits. No energy restriction and physical activity was promoted in any group. Prior the randomization and also yearly, adherence to each diet was appraised. The MedDiet was evaluated by a 14 item score previously validated tool [14] named MEDAS (MedDiet Adherence Score). Compliance with each of the 14 items relating to characteristic food habits was scored with 1 point if the goal was met or 0 points otherwise. Therefore, the total MEDAS range was 0–14, with 0 meaning no adherence and 14 meaning maximum adherence to Mediterranean Diet [15]. This tool was administered in both groups. To assess the adherence into low-fat diet, a 9-item dietary score was only administered to the participants allocated in this group. This screener was used in the PREDIMED (PREvención con DIeta MEDiterránea) study [16]. The total score ranged from 0 to 9.
More details on dietary intervention during the follow-up time are described and have been published in detail previously [12].
Dietary intake assessment
Trained dieticians collected data on dietary intake at baseline and yearly basis during follow-up in a face-to-face interview. Dietary intake was assessed using a 137-item semi-quantitative FFQ previously and repeatedly validated in Spain [17]. The FFQ provides a list of foods and beverages commonly used by the Spanish population and asks about the consumption of these foods during the previous year. It includes 9 response options (never or almost never, 1–3 times a month, once a week, 2–4 times a week, 5–6 times a week, once a day, 2–3 times a week day, 4–6 times a day and more than 6 times a day). The indicated frequencies of consumption were converted to intakes per day and multiplied by the weight of the standard serving size to estimate the intake in grams per day. Nutrient information was derived from Spanish food composition tables [18, 19]. Thus, the dietary intake of a selection of nutrients including carbohydrates (CHO), total fat, monounsaturated (MUFAs), polyunsaturated (PUFAs) and saturated fatty acids (SFAs), cholesterol, protein, dietary fiber, vitamin A, all the B-vitamins, C, D, E and K, calcium, iron, phosphorus, magnesium, potassium, selenium, iodine, and zinc was assessed. The food intake of a selection of food groups including vegetables, fruits, dairy products, red/white meat, fish/seafood, nuts, legumes, bakery/sweets, olive oil and cereals/whole cereals was also assessed adjusting food groups intake by total energy intake [20].
To evaluate the ND of the diet, density intake of all nutrients aforementioned was calculated by dividing absolute nutrient intake by total energy intake. The nutrient density was expressed as nutrient intake per 1000 kcal [8]. Mean change was estimated for each nutrient as follows: (baseline nutrient density at 1 year—nutrient density at baseline) and similarly for 7-year follow-up. The procedure was equal for food groups. For the present analysis, we have included the changes in ND and food intake after 1 and 7 years of follow-up as dependent variables to ascertain the effect of dietary intervention on these changes.
Covariate assessment
At baseline and once yearly, trained CORDIOPREV study staff collected information on lifestyle variables and sociodemographic data. The variables included were sex, age, smoking habit (non-smoker, current smoker or never smoker), and physical activity [21, 22]. Anthropometric variables (weight, height and waist circumference) were determined in accordance with the CORDIOPREV trial operations protocol. Weight and height were measured with calibrated scales and a wall-mounted stadiometer, respectively. Body Mass Index (BMI) was calculated as the weight in kilograms divided by the height in meters squared. Waist circumference (WC) was measured midway between the lowest rib and the iliac crest using an anthropometric tape.
Statistical analysis
Qualitative variables were described as frequencies and percentages, n (%), whereas the quantitative variables were expressed as means and standard deviations (SD). T test was used to ascertain differences in food intake and ND between groups. To compare changes in dietary habits, analysis of variance (ANOVA) repeated measures within-subject variable (dietary group) was performed for each of the outcome measures. The significance level was set at 5%. All analyses were performed using Stata software (15.0, StataCorp LP, Tx. USA).
Results
Characteristics of study patients at baseline according to dietary intervention group
The baseline characteristics of participants according to dietary intervention group are presented in Table 1. The current study included a total of 802 participants (673 men) with an average age of 59.2 years at baseline. Both groups showed similar socio-demographic and clinical characteristics except for diabetes condition (being slightly higher in low-fat diet group). The ancillary analysis comparing the baseline characteristics of the participants without data at 7 years with those who completed the follow-up assessment is shown in Table 4 Appendix. There were no differences between groups for any sociodemographic or lifestyle variables, (p > 0.05) except for educational level.
Table 1.
Baseline characteristics of the CORDIOPREV study participants according to dietary intervention of the population with all data available included in this article (n = 802)
| Mediterranean diet | Low-fat diet | p value | |||
|---|---|---|---|---|---|
| n | 425 | 377 | |||
| n | (%) | n | (%) | ||
| Sex | 0.945 | ||||
| Men | 357 | (84.0) | 316 | (83.8) | |
| Women | 68 | (16.0) | 61 | (16.2) | |
| Family history of premature CHD | 0.472 | ||||
| No | 364 | (85.7) | 316 | (83.8) | |
| Yes | 61 | (14.4) | 61 | (16.2) | |
| Smoking habit | 0.578 | ||||
| Never smoker | 124 | (29.2) | 100 | (26.5) | |
| Former smoker | 265 | (62.4) | 239 | (63.4) | |
| Current smoker | 36 | (8.5) | 38 | (10.1) | |
| Hypertension | 0.955 | ||||
| No | 139 | (32.7) | 124 | (32.9) | |
| Yes | 286 | (67.3) | 253 | (67.1) | |
| Dyslipidaemia | 0.463 | ||||
| LdL < 100 mg/dL | 301 | (70.8) | 258 | (68.4) | |
| LdL > = 100 mg/dL | 124 | (29.2) | 119 | (31.6) | |
| Diabetes | |||||
| No | 217 | (51.1) | 163 | (43.2) | 0.027 |
| Yes | 208 | (48.9) | 214 | (56.8) | |
| Marital status | 0.563 | ||||
| Married | 363 | (85.4) | 329 | (87.3) | |
| Othersa | 53 | (12.5) | 46 | (12.2) | |
| Missing value | 9 | (2.1) | 2 | (0.5) | |
| Educational level | 0.246 | ||||
| Primary education | 281 | (66.1) | 263 | (69.8) | |
| Secondary education | 86 | (20.2) | 78 | (20.7) | |
| University education | 43 | (10.1) | 26 | (6.9) | |
| Missing Value | 15 | (3.6) | 10 | (2.6) | |
| Mediterranean diet | Low-fat diet | p value | |||
|---|---|---|---|---|---|
| n | 425 | 377 | |||
| Mean | (SD) | Mean | (SD) | ||
| Age (years) | 59.2 | (9.2) | 59.2 | (8.2) | 0.929 |
| BMI (kg/m2) | 31.0 | (4.4) | 31.2 | (4.5) | 0.557 |
| Adherence to MedDiet (points) | 8.9 | (2.0) | 8.7 | (1.8) | 0.923 |
| Adherence to low-fat diet (points) | 3.9 | (1.5) | 3.9 | (1.6) | 0.912 |
| Physical activity (METs-min/day) | 193.3 | (235.7) | 186.1 | (212.0) | 0.699 |
Values are presented as means ± SD for continuous variables and n (%) for categorical variables. Pearson’s χ2 test was performed for categorical variables and T student test for continuous variables.
BMI: Body Mass Index
Othersa: Includes single, widowed and divorced.
Table 4.
Characteristics of the participants without data at 7 years, compared to those who completed the follow-up period at the CORDIOPREV study (n = 802 vs. n = 200)
| Study sample | Lost of follow-up | p value | |||
|---|---|---|---|---|---|
| n | 802 | 200 | |||
| n | (%) | n | (%) | ||
| Sex | 0.514 | ||||
| Men | 673 | (83.9) | 164 | (82.0) | |
| Women | 129 | (16.1) | 36 | (18.0) | |
| Family history of premature CHD | 0.543 | ||||
| No | 680 | (84.8) | 173 | (86.5) | |
| Yes | 122 | (15.2) | 27 | (13.5) | |
| Smoking habit | 0.051 | ||||
| Never smoker | 224 | (27.9) | 41 | (20.5) | |
| Former smoker | 504 | (62.8) | 133 | (66.5) | |
| Current smoker | 74 | (9.2) | 26 | (13.0) | |
| Hypertension | 0.073 | ||||
| No | 263 | (32.8) | 51 | (26.2) | |
| Yes | 539 | (67.2) | 144 | (73.9) | |
| Dyslipidaemia | 0.182 | ||||
| LdL < 100 mg/dL | 559 | (69.7) | 149 | (74.5) | |
| LdL > = 100 mg/dL | 243 | (30.3) | 51 | (25.5) | |
| Diabetes | 0.105 | ||||
| No | 380 | (47.4) | 82 | (41.0) | |
| Yes | 422 | (52.6) | 118 | (59.0) | |
| Marital status | 0.811 | ||||
| Married | 692 | (87.4) | 176 | (88.0) | |
| Othersa | 99 | (12.5) | 24 | (12.0) | |
| Missing value | 1 | (0.1) | |||
| Educational level | < 0.005 | ||||
| Primary education | 544 | (70.0) | 169 | (84.5) | |
| Secondary education | 164 | (21.1) | 25 | (12.5) | |
| University education | 69 | (8.9) | 6 | (3.0) | |
| n | 802 | 200 | p value | ||
|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | ||
| Age (years) | 59.2 | (8.7) | 61.2 | (8.8) | 0.664 |
| BMI (kg/m2) | 31.1 | (4.5) | 31.3 | (4.7) | 0.368 |
| Adherence to MedDiet (points) | 8.8 | (1.9) | 8.6 | (2.0) | 0.158 |
| Adherence to low-fat diet (points) | 3.9 | (1.6) | 3.7 | (1.6) | 0.470 |
| Physical activity (METs-min/day) | 190.0 | (225.4) | 151.6 | (207.8) | 0.167 |
Values are presented as means ± SD for continuous variables and n (%) for categorical variables. Pearson’s χ2 test was performed for categorical variables and T student test for continuous variables
BMI: Body Mass Index
Othersa: Includes single, widowed and divorced
Changes in dietary sources according to dietary intervention group after 1 and 7 years of follow-up
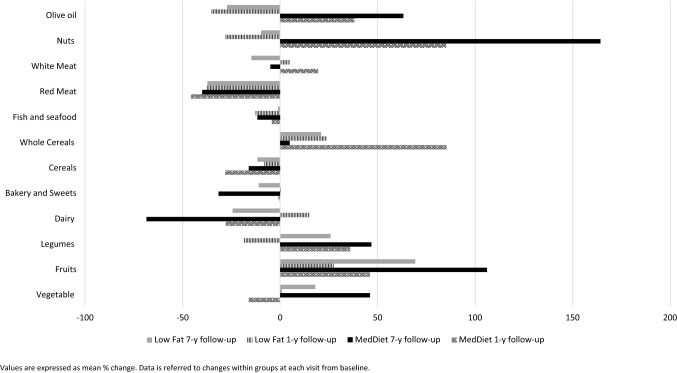
Table 2 shows changes in food sources according to randomization group. The dietary intake of vegetables, fruits, and whole cereals significantly increased within groups across follow-up period (< 0.001). Meanwhile, the mean intake of dairy products, bakery/sweets, cereals and red meat decreased in both groups compared to baseline intake (< 0.001). Differences between groups were notorious after 7-year follow-up. Some of the greatest increases in dietary intake were observed in MedDiet in comparison with Low-Fat Diet for vegetables (46.1 g/day vs. 18.1 g/day, p < 00.1), fruits (121.3 g/day vs. 72.9 g/day), legumes (4.3 g/ day vs. 0.16 g/day) and nuts (7.3 g/day vs. − 3.7 g/day). The relatives mean % changes after follow-up are represented in Fig. 1. The largest changes (more than 20%) were observed for the intakes of fruits and legumes, being the increased intake upper at 7 years of follow-up compared to 1st year in both groups.
Table 2.
Mean values and mean changes in dietary sources according to dietary pattern at baseline and after 1 and 7 years of follow-up in the CORDIOPREV study (n = 802)
| MedDiet | Low-fat diet | p value between group | |
|---|---|---|---|
| Vegetable, Mean (SD), (g/day) | |||
| Baseline | 261.8 (94.5) | 254.3 (99.4) | 0.276 |
| 1-year change, (95%, CI) | − 16.0 (− 27.1, − 5.0) | 0.9 (− 11.4, 13.3) | 0.044 |
| 7-year change, (95%, CI) | 46.1 (35.4, 56.7) | 18.1 (6.0, 30.2) | 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Fruits, Mean (SD), (g/day) | |||
| Baseline | 346.3 (181.3) | 343.2 (191.2) | 0.815 |
| 1-year change, (95%, CI) | 39.3 (17.4, 61.3) | 27.7 (6.8, 48.7) | 0.456 |
| 7-year change, (95%, CI) | 121.3 (99.7, 142.8) | 72.9 (50.3, 95.5) | 0.002 |
| p value within group | < 0.001 | < 0.001 | |
| Legumes, Mean (SD), (g/day) | |||
| Baseline | 22.6 (11.8) | 23.9 (17.3) | 0.206 |
| 1-year change, (95%, CI) | 3.4 (1.7, 5.1) | − 1.5 (− 3.7, 0.7) | 0.001 |
| 7-year change, (95%, CI) | 4.3 (2.9, 5.8) | 0.16 (− 1.9, 2.2) | 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Dairy, Mean (SD), (g/day) | |||
| Baseline | 387.0 (191.5) | 351.3 (186.8) | 0.008 |
| 1-year change, (95%, CI) | − 27.9 (− 47.2, − 8.6) | 15.2 − 3.6, 34.1) | 0.002 |
| 7-year change, (95%, CI) | − 68.6 (− 88.8, − 48.3) | − 24.3 (− 46.1, − 2.5) | 0.004 |
| p value within group | < 0.001 | < 0.001 | |
| Bakery and Sweets, Mean (SD), (g/day) | |||
| Baseline | 26.9 (24.7) | 27.4 (26.0) | 0.793 |
| 1-year change, (95%, CI) | − 9.8 (− 12.2, − 7.4) | 0.2 (− 3.0, 3.3) | < 0.001 |
| 7-year change, (95%, CI) | − 15.8 (− 18.1, − 13.6) | − 13.2 (− 15.9, − 10.4) | 0.134 |
| p value within group | < 0.001 | < 0.001 | |
| Cereals, Mean (SD), (g/day) | |||
| Baseline | 176.8 (80.5) | 182.8 (86.1) | 0.310 |
| 1-year change, (95%, CI) | − 23.3 (− 32.2, − 14.4) | − 35.1 (− 45.2, − 25.0) | 0.085 |
| 7-year change, (95%, CI) | − 36.9 (− 45.7, − 28.0) | − 41.3 (− 51.7, − 31.0) | 0.515 |
| p value within group | < 0.001 | < 0.001 | |
| Whole Cereals, Mean (SD), (g/day) | |||
| Baseline | 40.1 (72.3) | 43.9 | 0.481 |
| 1-year change, (95%, CI) | 23.2 (14.5, 31.8) | 19.4 (9.9, 29.0) | 0.567 |
| 7-year change, (95%, CI) | 6.9 (− 1.5, 15.4) | 2.6 (− 7.3, 12.4) | 0.507 |
| p value within group | < 0.001 | < 0.001 | |
| Fish and seafood, Mean (SD), (g/day) | |||
| Baseline | 106.0 (47.2) | 102.9 (46.3) | 0.361 |
| 1-year change, (95%, CI) | − 19.3 (− 24.5, − 14.1) | − 26.3 (− 31.2, − 21.4) | 0.056 |
| 7-year change, (95%, CI) | − 7.8 (− 12.6, − 3.0) | − 22.6 (− 27.7, − 17.6) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Red Meat, Mean (SD), (g/day) | |||
| Baseline | 40.7 (31.1) | 46.8 (35.5) | 0.102 |
| 1-year change, (95%, CI) | − 23.0 (− 25.9, − 20.1) | − 23.8 (− 27.3, − 20.3) | 0.737 |
| 7-year change, (95%, CI) | − 24.0 (− 27.1, − 21.0) | − 25.9 (− 29.5, − 22.3) | 0.439 |
| p value within group | < 0.001 | < 0.001 | |
| White Meat, Mean (SD), (g/day) | |||
| Baseline | 69.7 (34.4) | 72.3 (37.5) | 0.304 |
| 1-year change, (95%, CI) | 19.6 (10.0, 29.3) | 5.0 (− 3.1, 13.1) | 0.025 |
| 7-year change, (95%, CI) | − 60.2 (− 65.0, − 55.4) | − 60.3 (− 65.7, − 54.9) | 0.980 |
| p value within group | < 0.001 | < 0.001 | |
| Nuts, Mean (SD), (g/day) | |||
| Baseline | 9.3 (10.7) | 8.5 (10.5) | 0.289 |
| 1-year change, (95%, CI) | 2.1 (0.8, 3.3) | − 3.8 (− 4.8, − 2.7) | < 0.001 |
| 7-year change, (95%, CI) | 7.3 (5.9, 8.7) | − 3.7 (− 4.9, − 2.5) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Olive oil, Mean (SD), (g/day) | |||
| Baseline | 34.9 (12.8) | 33.4 (12.3) | 0.099 |
| 1-year change, (95%, CI) | 5.2 (3.6, 6.8) | − 14.0 (− 15.5, − 12.4) | < 0.001 |
| 7-year change, (95%, CI) | 12.9 (11.5, 14.4) | − 11.7 (− 13.3, − 10.1) | < 0.001 |
| p value within group | < 0.001 | < 0.001 |
Values are presented as means and standard deviations (SD) at baseline point and changes (95% CI) at 1 and 7 years of follow-up. p value for differences between groups at 1- and 7-year follow-up using t test. p value for differences within group using ANOVA for repeated measure. Values in bold showed significant association
CI Confidence Intervals, MedDiet Mediterranean Diet
Changes in ND according to dietary intervention group after 1 and 7 years of follow-up
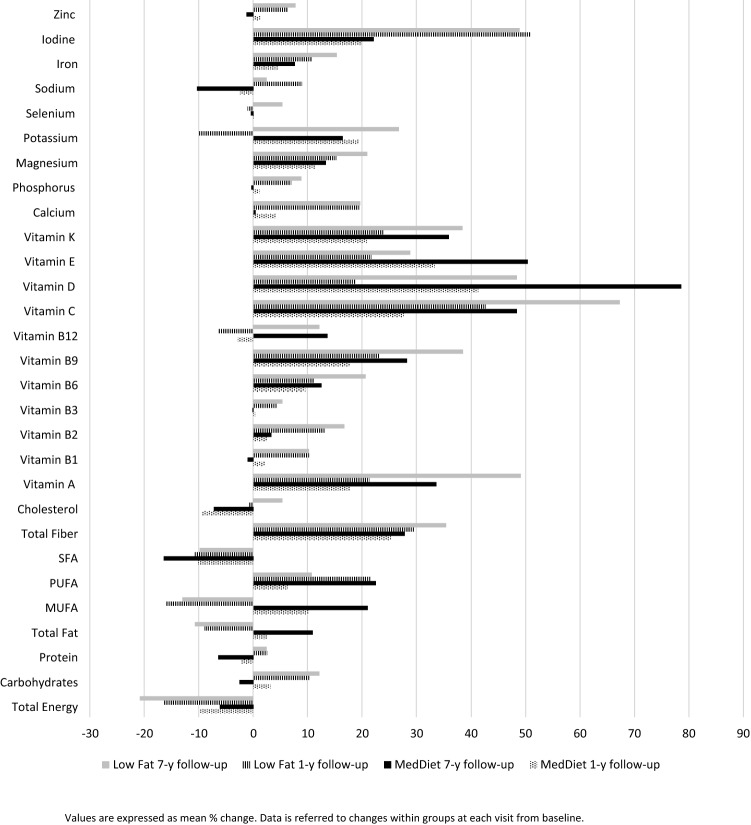
There was a decrease in energy intake over time in both groups, slightly higher in Low-Fat Diet compared to MedDiet group (− 427.6 kcal/day vs. − 279.8 kcal/day at 1st year, and − 544.6 kcal/day vs. − 215.3 kcal/day after 7 years of follow-up) (Table 3). ND of all the nutrients increased within group across follow-up time, except for SFA, cholesterol, vitamin B12 and sodium (p < 0.001). Taking into account the differences between participants, those allocated in MedDiet compared with the respective counterparts, exhibited higher ND of total fat and quality subtypes of dietary fat (MUFA and PUFA), vitamin D and E through the follow-up study (p < 0.001). By contrary, Low-Fat Diet participants displayed higher ND for vitamin B9, calcium, phosphorus, magnesium, potassium, selenium, iodine, iron and zinc (p < 0.05). The relatives mean % changes of food intake, ND and total energy are represented in Figs. 2 and 3, respectively. ND increases after 1 year as compared to baseline, although the increase was larger after 7 years. The largest changes were found for iodine, potassium, vitamin K, E, D, C, A, total fiber and PUFA. According to food groups, red meat intake decreases in both groups; meanwhile, the intake of fruits, vegetables and legumes increases in both groups after the dietary intervention, maintaining this trend over time. Significantly, the largest changes were found for nuts and olive oil in the MedDiet group.
Table 3.
Mean values and changes in nutrient density according to dietary pattern at baseline and after 1 and 7 years of follow-up in the CORDIOPREV study (n = 802)
| MedDiet | Low-fat diet | p value between group | |
|---|---|---|---|
| Energy, Mean (SD), (kcal/day) | |||
| Baseline | 2247.8 (498.7) | 2266.1 (523.9) | 0.613 |
| 1-year change, (95%, CI) | − 279.8 (− 327.5, − 232.0) | − 427.6 (− 479.2, − 375,9) | < 0.001 |
| 7-year change, (95%, CI) | − 215.3 (− 262.2, − 168.3) | − 544.6 (− 599.4, − 489.9) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Carbohydrates, Mean (SD), (g/1000 kcal) | |||
| Baseline | 103.5 (16.1) | 103.8 (16.7) | 0.802 |
| 1-year change, (95%, CI) | 1.0 (− 0.9, 2.9) | 8.6 (6.5, 10.7) | < 0.001 |
| 7-year change, (95%, CI) | − 4.9 (− 6.8, − 3.0) | 9.9 (7.8, 11.9) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Protein, Mean (SD), (g/1000 kcal) | |||
| Baseline | 46.3 (6.7) | 46.4 (7.3) | 0.814 |
| 1-year change, (95%, CI) | − 1.7 (− 2.4, − 0.9) | 0.6 (− 0.2, 1.4) | < 0.001 |
| 7-year change, (95%, CI) | − 3.7 (− 4.4, − 3.0) | 0.3 (− 0.5, 1.2) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Total Fat, Mean (SD), (g/1000 kcal) | |||
| Baseline | 41.4 | 40.9 | 0.241 |
| 1-year change, (95%, CI) | 0.2 (− 0.6, 1.0) | − 4.3 (− 5.2, − 3.5) | < 0.001 |
| 7-year change, (95%, CI) | 3.6 (2.7, 4.4) | − 5.2 (− 6.0, − 4.3) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| MUFA, Mean (SD), (g/1000 kcal) | |||
| Baseline | 20.4 (3.9) | 19.9 (3.7) | 0.080 |
| 1-year change, (95%, CI) | 1.4 (0.9, 1.9) | − 3.6 (− 4.1, − 3.1) | < 0.001 |
| 7-year change, (95%, CI) | 3.5 (2.9, 4.0) | − 3.1 (− 3.6, − 2.6) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| PUFA, Mean (SD), (g/1000 kcal) | |||
| Baseline | 7.1 (1.9) | 7.0 (1.9) | 0.327 |
| 1-year change, (95%, CI) | 0.1 (− 0.1, 0.4) | 1.1 (0.8, 1.5) | < 0.001 |
| 7-year change, (95%, CI) | 1.1 (0.9, 1.4) | 0.3 (0.1, 0.6) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| SFA, Mean (SD), (g/1000 kcal) | |||
| Baseline | 9.9 (2.0) | 9.9 (2.1) | 0.961 |
| 1-year change, (95%, CI) | − 1.2 (− 1.4, − 1.0) | − 1.3 (− 1.6,− 1.1) | 0.586 |
| 7-year change, (95%, CI) | − 1.8 (− 2.1, − 1.6) | − 1.3 (− 1.6, − 0.9) | 0.009 |
| p value within group | < 0.001 | < 0.001 | |
| Total Fiber, Mean (SD), (g/1000 kcal) | |||
| Baseline | 11.3 (3.3) | 11.4 (3.4) | 0.751 |
| 1-year change, (95%, CI) | 2.1 (1.7, 2.4) | 2.6 (2.1, 3.0) | 0.079 |
| 7-year change, (95%, CI) | 2.2 (1.9, 2.6) | 3.1 (2.6, 3.5) | 0.005 |
| p value within group | < 0.001 | < 0.001 | |
| Cholesterol, Mean (SD), (g/1000 kcal) | |||
| Baseline | 147.9 (35.9) | 147.9 (36.4) | 0.981 |
| 1-year change, (95%, CI) | − 18.5 (− 22.4, − 14.6) | − 7.1 (− 11.8, − 2.4) | 0.001 |
| 7-year change, (95%, CI) | − 17.0 (− 20.8, − 13.3) | 0.2 (− 4.2, 4.6) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin A, Mean (SD), (µg/1000 kcal) | |||
| Baseline | 341.5 (196.7) | 333.7 (214.0) | 0.593 |
| 1-year change, (95%, CI) | − 18.7 (− 56.6, 19.2) | 4.2 (− 21.1, 29.6) | 0.335 |
| 7-year change, (95%, CI) | 35.7 (9.8, 61.7) | 61.8 (31.9, 91.8) | 0.194 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin B1, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 0.7 (0.1) | 0.7 (0.1) | 0.794 |
| 1-year change, (95%, CI) | 0.1 (− 0.01, 0.10) | 0.1 (0.04, 0.70) | < 0.001 |
| 7-year change, (95%, CI) | − 0.1 (− 0.04, − 0.10) | 0.1 (0.04, 0.70) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin B2, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 0.9 (0.2) | 0.9 (0.2) | 0.321 |
| 1-year change, (95%, CI) | 0 (− 0.03, 0.02) | 0.1 (0.07, 0.11) | < 0.001 |
| 7-year change, (95%, CI) | 0 (0.04, 0.07) | 0.1 (0.01, 0.14) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin B3, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 18.6 (3.4) | 18.8 (3.7) | 0.528 |
| 1-year change, (95%, CI) | − 0.3 (− 0.72, 0.03) | 0.4 (− 0.03, 0.75) | 0.010 |
| 7-year change, (95%, CI) | − 0.5 (− 0.89, − 0.15) | 0.6 (0.18, 1.05) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin B6, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 1.0 (0.2) | 1.0 (0.2) | 0.293 |
| 1-year change, (95%, CI) | 0.1 (0.04, 0.09) | 0.1 (0.06, 0.11) | 0.299 |
| 7-year change, (95%, CI) | 0.1 (0.06, 0.11) | 0.2 (0.14, 0.20) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin B9, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 144.5 (40.0) | 142.6 (40.1) | 0.507 |
| 1-year change, (95%, CI) | 17.0 (12.61, 21.33) | 25.3 (20.62, 30.00) | 0.011 |
| 7-year change, (95%, CI) | 29.3 (24.79, 33.74) | 41.6 (36.23, 46.96) | 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin B12, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 3.8 (1.2) | 3.8 (1.3) | 0.980 |
| 1-year change, (95%, CI) | − 0.1 (− 0.27, 0.06) | − 0.2 (− 0.39, − 0.09) | 0.232 |
| 7-year change, (95%, CI) | 0.2 (0.07, 0.35) | 0.1 (− 0.08, 0.25) | 0.279 |
| p value within group | < 0.001 | < 0.001 | |
| Iron, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 6.9 (1.0) | 6.9 (1.0) | 0.621 |
| 1-year change, (95%, CI) | 0.2 (0.09, 0.32) | 0.7 (0.55, 0.77) | < 0.001 |
| 7-year change, (95%, CI) | 0.4 (0.27, 0.51) | 0.9 (0.82, 1.07) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin C, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 83.6 (34.8) | 82.6 (34.1) | 0.672 |
| 1-year change, (95%, CI) | 8.8 (4.6, 13.0) | 17.3 (12.6, 21.9) | 0.008 |
| 7-year change, (95%, CI) | 22.7 (18.9, 26.5) | 31.1 (26.6, 35.6) | 0.005 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin D, Mean (SD), (µg/1000 kcal) | |||
| Baseline | 3.5 (1.8) | 3.4 (2.0) | 0.380 |
| 1-year change, (95%, CI) | 0.1 (− 0.1, 0.3) | − 0.7 (− 0.9, − 0.5) | < 0.001 |
| 7-year change, (95%, CI) | 0.9 (0.6, 1.1) | − 0.1 (− 0.4, 0.1) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin E, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 8.4 (2.39 | 7.9 (2.3) | 0.004 |
| 1-year change, (95%, CI) | 1.8 (1.5, 2.1) | 1.0 (0.6, 1.3) | 0.001 |
| 7-year change, (95%, CI) | 3.2 (2.9, 3.4) | 1.3 (1.0, 1.6) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Vitamin K, Mean (SD), (µg/1000 kcal) | |||
| Baseline | 136.0 (60.7) | 129.6 (63.4) | 0.142 |
| 1-year change, (95%, CI) | 5.3 (− 1.8, 12.3) | 11.5 (3.7, 19.3) | 0.243 |
| 7-year change, (95%, CI) | 15.9 (8.6, 23.1) | 19.3 (10.9, 27.6) | 0.542 |
| p value within group | < 0.001 | < 0.001 | |
| Calcium, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 451.5 (126.4) | 433.1 (125.7) | 0.040 |
| 1-year change, (95%, CI) | 0.7 (− 12.4, 13.8) | 65.1 (50.0, 80.2) | < 0.001 |
| 7-year change, (95%, CI) | − 21.1 (− 34.6, − 7.7) | 58.4 (42.3, 74.5) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Phosphorus, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 746.9 (127.6) | 745.7 (129.0) | 0.890 |
| 1-year change, (95%, CI) | − 3.8 (− 17.5, 9.9) | 42.7 (28.4, 56.9) | < 0.001 |
| 7-year change, (95%, CI) | − 18.1 (− 31.4, − 4.8) | 50.7 (35.3, 66.0) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Magnesium, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 165.3 (32.8) | 165.1 (32.6) | 0.909 |
| 1-year change, (95%, CI) | 13.9 (10.2, 17.7) | 21.0 (17.1, 24.9) | 0.011 |
| 7-year change, (95%, CI) | 16.1 (12.3, 20.0) | 28.7 (24.4, 33.0) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Potassium, Mean (SD), (µg/1000 kcal) | |||
| Baseline | 1674.6 (333.8) | 1653.7 (322.2) | 0.369 |
| 1-year change, (95%, CI) | 107.7 | 274.1 | < 0.001 |
| 7-year change, (95%, CI) | 217.2 | 380.2 | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Selenium, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 56.8 (10.9) | 57.0 (10.8) | 0.841 |
| 1-year change, (95%, CI) | − 1.4 (− 2.7, − 0.1) | − 1.5 (− 2.8, − 0.2) | 0.920 |
| 7-year change, (95%, CI) | − 2.0 (− 3.3, − 0.8) | 1.3 (− 0.1, 2.7) | 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Sodium, Mean (SD), (µg/1000 kcal) | |||
| Baseline | 1191.7 (225.6) | 1201.3 (235.5) | 0.558 |
| 1-year change, (95%, CI) | − 54.0 (− 82.4, − 25.6) | 72.3 (41.8, 102.7) | < 0.001 |
| 7-year change, (95%, CI) | − 154.8 (− 180.1, − 129.5) | − 9.7 (− 39.8, 20.4) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Iodine, Mean (SD), (mg/1000 kcal) | |||
| Baseline | 143.4 (75.0) | 135.7 (72.5) | 0.140 |
| 1-year change, (95%, CI) | 1.7 (− 6.8, 10.3) | 33.6 (24.9, 42.4) | < 0.001 |
| 7-year change, (95%, CI) | − 2.9 (− 11.1, 5.3) | 29.4 19.4, 39.3) | < 0.001 |
| p value within group | < 0.001 | < 0.001 | |
| Zinc, Mean (SD), (µg/1000 kcal) | |||
| Baseline | 5.7 (1.0) | 5.8 (1.0) | 0.242 |
| 1-year change, (95%, CI) | − 0.1 (− 0.2, 0.1) | 0.2 (0.1, 0.4) | 0.001 |
| 7-year change, (95%, CI) | − 0.2 (− 0.3, − 0.1) | 0.3 (0.2, 0.4) | < 0.001 |
| p value within group | < 0.001 | < 0.001 |
Values are presented as means and standard deviations (SD) at baseline point and changes (95% CI) at 1 and 7 years of follow-up. p value for differences between groups at 1- and 7-year follow-up using t test. p value for differences within group using ANOVA for repeated measure. Values in bold showed significant association
CI Confidence Intervals, MedDiet Mediterranean Diet
Fig. 2.
Relatives changes in food intake after 1- and 7-year follow-up according to randomization group in the CORDIOPREV study
Fig. 3.
Relatives changes in total energy and nutrient density after 1- and 7-year follow-up according to randomization group in the CORDIOPREV study
Discussion
In the present study, we evaluated the association between dietary intervention promoting two healthy dietary patterns on changes in food and ND intake in a population of persons in cardiovascular secondary prevention. The main findings are twofold: first, dietary intervention improves quality of diet, increasing the intake of healthy foods and the ND and reducing the energy intake in both groups. Second, the aforementioned enhancement persists through long-term follow-up, with the improvements lasting for 7 years, independently of randomization group.
As far as we know, this is the first study to present data on intra and inter-individual changes in diet quality over a large sample of population with established CVD after a long follow-up period time. The CORDIOPREV participants stayed in contact with the research staff receiving individualized nutritional counselling and reinforcing food choices. These interventions have been related to dietary intake changes, with a markedly increased of healthy food as vegetables, fruits and whole cereals and a decrease of undesirable ones as bakery/sweets and red meat in both groups. These findings are consistent with the previously reported preliminary findings of this trial [23] and similar to a recent interim analysis of the ongoing PREDIMED-Plus trial [24].
Although some studies question the feasibility of having a large number of dietary changes during the follow-up dietary intervention [25], our findings support the idea that the overall mentioned changes in food intakes were at least maintained through follow-up. Probably, this significant maintenance of behavioural changes were only possible by the perseverance in the level of dietary intervention, and focusing on individual’s health knowledge and nutrition literacy [26]. Other factors may also contribute to explain the high retention rates and long-term dietary adherence in our study. One of them could be attributable to the health characteristic of participants included in the study. It is possible that CORDIOPREV trial participants were aware of their coronary problems and its relationship with poor food habits, and thus firmly motivated to comply with dietary advices. Contrary to our results, other studies have reported that improvements in diet quality appears in the short term, declining after a long follow-up period [27–29]. All of these studies are pointing out a trend toward worsening diet quality across follow-up. Nevertheless, these studies evaluated the changes after short follow-up time, usually 6, 12 or 24 months after intervention with different settings and populations. In fact, dietary interventions with a so long follow-up are really scarce, and one of the added values of this article is that it shows that, with an adequate intervention, chronic maintenance of dietary adherence and long-term change of dietary habits is possible (which had not been well established until now).
Even though the CORDIOPREV dietary intervention did not promoted energy restriction, the energy intake decreased significantly in both groups, being the energy reduction slight higher in Low-Fat Diet group, probably attributable to its low fat content [30]. In this line of thought, dietary quality has been broadly defined by the ratio energy/nutrient intake, being inversely linked between them [31]. Based on our findings, at the same time that the energy intake decreased, the ND of the majority of the vitamins and minerals increased in both groups with reference to baseline point. Between the different healthy dietary patterns assessed, the MedDiet group showed relatively better ND compared to the other group, specifically for MUFA, PUFA, Vitamins D and E. This result could be explained by the higher intake of some specified food groups as nuts and olive oil, foods richest in these nutrients, and the hallmark of MedDiet [32]. A recent study including high risk CVD adults [33] that evaluated the effect of improving MedDiet adherence on ND after 1 year of follow-up reported similar findings. However, their results should be carefully interpreted, because although they examined the same cohort over time, the follow-up time was shorter and they not compared to another dietary group as we do. Regarding secondary prevention, it is well documented that requires a multidisciplinary approach, highlighting the role of dietary intervention. Dietary patterns with low caloric value and high ND are key in the prevention of its recurrence [34]. These findings highlight that the changes in dietary quality are present and can be maintained after a long dietary intervention. The following step is to assess if these dietary changes could be part of several effect in health, as a decreased risk of CVD recurrence and development of other chronic diseases. Although the energy reduction and ND for some minerals is higher in Low-Fat Diet allocation group, is important to note that anyone enrolled in the CORDIOPREV study, have obtained a nutritional benefit. This idea reinforces not only the fact that nutritional counselling improves quality of diet, but also that the participation in this trial, independently of allocation group, enhanced nutrition literacy and produced better nutritional outcomes.
The current study has some limitations that need to be addressed. First, the study sample is not representative of the general population, since only adults with established CVD were included, being the results not extrapolated to the overall population. Nevertheless, our population represents an important proportion of current adult Western societies. Second, other possible determinants of ND might have not been evaluated in this study; however, the most prominent sociodemographic and lifestyle factors in the literature have been collected. Third, although we used a FFQ to measure dietary intakes validated in adult Spanish individuals with good reproducibility and validity [35], it might not be the ideal tool to measure micronutrient intake [36]. Fourth, the use of FFQ could include a memory bias and, we could not rule out the possibility that intake of some nutrients have been misclassified. However, because we are using the same tool and in the same way, the potential measurement errors should be constant in magnitude and direction, so we think that our estimates of differences are still valid. Furthermore, there may be concern that FFQ responses may change simply as a result of the advice given, rather than reflecting real change. One way to check this would have involved using some objective laboratory measures of nutritional components, something that we did not have in our study, for correlation with FFQ scores. However, the FFQ employed in our study is a validated tool with a high reproducibility [17]. Reproducibility reflects reliability and refers to the similarity of the same method at different timepoints [37], so FFQ is a tool that is established to be responsive to change and the observed differences are reliable. Fifth, there may be an impact of learning bias arising from repeated FFQ measurements. Participation in clinical trials may improve outcomes due to the simple fact of being monitored within the study [38]. The possibility of learning bias may arise due to repetition of FFQs during the follow-up period. This could result in improvements in the dietary changes reported by control participants due to their increased knowledge of healthy living. This bias may lead to a negative study, like ours. In our defence, FFQ validation would have ensured responsiveness to change [37]. Critics may argue that this validation may not map well onto out repetition and follow-up time frame. However, in other studies that have address the same question as ours [33, 39] with similar FFQ repetition and follow-up with emphasis on healthy living, have shown positive findings. This means that in these studies the control group responses were not influenced by repeated FFQ measurements. While learning bias is possible, it is unlikely that it materially impacted on control group responses compared to intervention.
Sixth, after 7 years of follow-up, we had a decrease of around 20% of our overall sample, a feature that may introduce bias depending on the numbers and the manner of the loss. Therefore, we performed an ancillary analysis (Table 4 Appendix), where we demonstrated that, except for one of 13 variables, there weren´t any differences between groups. Give this lack of systematic difference, it is reasonable to assume that results of the complete data set are trustworthy.
Seventh, increasing average age of the participants during the 7-year course of the trial may impact on changes in diet independent of the intervention. However, these changes would be expected to influence both control and intervention groups equally within a randomised study. One of the most important changes in dietary intake of population is the decrease in total energy influenced by ageing process [40]. An observational study (SUN, Seguimiento Universidad de Navarra study) [41] carried out in Spanish population reported an average decreased energy consumption in both sexes nearly to 2.7% after 10 years of follow-up. Another study which assessed the diet quality and ND in subjects with metabolic syndrome also showed a similar energy decrease trend [42]. For this reason, we estimated the ND of the diet, which is the ratio of nutrients to the food's energy content for the amount that is commonly consumed. Our results showed that changes in energy intake are much larger than in those reported in the aforementioned observational studies, thus the dietary intervention had an effect on this issue rather than a simple fact derived from ageing process.
Finally, we are conscious about the effect of non-dietary characteristics as health status on the influence of food intake. However, at baseline both groups were comparable in all the sociodemographic and health variables analysed. For this reason, the effect observed should be attributable to the nutritional intervention performed instead of a possible modifier effect exerted by the variables mentioned previously.
Notwithstanding the above limitations, our study includes several strengths that reinforce the results obtained. Standing out the large sample size of coronary patients (n = 802), the use of a standardized protocol which reduces the possibility of information bias about food intake and the vast amount of sociodemographic/lifestyles variables collected in both groups. Finally, in the CORDIOPREV study, the same participants were evaluated over a period of time (7 years of follow-up). Therefore, the observed changes are less likely to be the result of differences in the sample characteristics.
Conclusion
In conclusion, Dietary counselling after 7 years of follow-up with two healthy diets in persons at cardiovascular secondary prevention improved quality of diet, reducing total energy intake at the same time that there is a mean increasing on the intake of healthy food groups and overall ND compared to baseline. Our results reinforce the idea of the participation in trials, enhance nutrition literacy and produces better nutritional outcomes in adult patients with established CVD.
Acknowledgements
The authors especially thank the CORDIOPREV participants for their collaboration and the CORDIOPREV staff for their support and effort. CIBEROBN and CIBERESP are an initiative of ISCIII, Spain. We would like to thank the EASP (Escuela Andaluza de Salud Pública), Granada (Spain), for carrying out the randomization process in this study.
Abbreviations
- ANOVA
Analysis of variance
- BMI
Body Mass Index
- CORDIOPREV
CORonary Diet Intervention with Olive oil and cardiovascular PREVention study
- CVD
Cardiovascular disease
- FFQ
Food frequency questionnaire
- IRB
Institutional review board
- MEDAS
Mediterranean diet adherence score
- MedDiet
Mediterranean diet
- MUFA
Monounsaturated fatty acids
- ND
Nutrient density
- PUFA
Polyunsaturated fatty acids
- SD
Standard deviation
- WC
Waist circumference
Appendix
See Appendix Table 4.
Author contributions
NC-I, JD-L, JL-M, and GMQ-N: conceived and designed the study. NC-I and GMQ-N: analyzed data. The first draft of this paper was written by NC-I, JD-L, and JL-M: all authors discussed, made contributions to the article, and approved the final version of the article.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. N.C.-I. is a recipient of the Juan de la Cierva Formación Programme. E.M.Y-S is a recipient of the Nicolás Monardes Programme (C1-0005–2019, Servicio Andaluz de Salud, Junta de Andalucía, Spain). A.P.A-L is supported by a Río-Hortega Programme (Instituto de Salud Carlos III). The CORDIOPREV study is supported by the Fundacion Patrimonio Comunal Olivarero. The sponsor was not involved in the design or carrying out the study, and its participation was limited to funding and providing the olive oil used in the study. CORDIOPREV trial also received additional funding from CITOLIVA, CEAS, Junta de Andalucia (Consejeria de Salud, Consejeria de Agricultura y Pesca, Consejeria de Innovacion, Ciencia y Empresa), Diputaciones de Jaen y Cordoba, Centro de Excelencia en Investigacion sobre Aceite de Oliva y Salud and Ministerio de Medio Ambiente, Medio Rural y Marino and the Spanish Government. It was also partly supported by research grants from the Ministerio de Ciencia e Innovacion (AGL2009-122270 to J L-M, FIS PI10/01041 to P. P.-M, FIS PI13/00023 to J. D.-L); Ministerio de Economia y Competitividad (AGL2012/39615 to J L-M); Consejeria de Salud, Junta de Andalucia (PI0193/09 to J. L.-M, PI-0252/09 to J. D.-L, and PI-0058/10 to P. P.-M, PI-0206–2013 to A. G.-R); Proyecto de Excelencia, Consejería de Economía, Innovación, Ciencia y Empleo (CVI-7450 to J. L.-M).
Availability of data and materials/code availability
Data described in the manuscript, code book, and analytic code will not be made available because of study`s embargo.
Declarations
Conflict of interest
The authors declare that they have no current or potential conflicts of interest.
Ethics approval
The protocol was written in accordance with the principles of the Declaration of Helsinki. The respective Institutional Review Board (IRB) by the Human Investigation Review Committee of the Reina Sofia University Hospital (Córdoba, Spain) approved the study protocol. The trial was registered in 2009 at ClinicalTrials.gov (number NCT00924937). Recruitment took place from July 2009 to February 2012. All subjects provided written informed consent.
Footnotes
Naomi Cano-Ibáñez and Gracia M. Quintana-Navarro have contributed equally to this work.
Javier Delgado-Lista and Jose Lopez-Miranda have share joint seniorship.
Change history
10/3/2022
A Correction to this paper has been published: 10.1007/s00394-022-03006-7
Contributor Information
Javier Delgado-Lista, Email: delgadolista@gmail.com.
Jose Lopez-Miranda, Email: jlopezmir@uco.es.
References
- 1.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V, Beaton A, Carapetis JR, Chugh S, Criqui MH, DeCleene NK, Fernández-Sola J, Fowkes FGR, Kassebaum NJ, Koroshetz WJ, Misganaw AT, Mokdad AH, Oliveira GMM, Otto CM, Owolabi MO, Reitsma MB, Rigotti NA, Sable CA, Shakil SS, Sliwa K, Stark BA, Tleyjeh II, Zuhlke LJ, Abbasi-Kangevari M, Abdi A, Abedi A, Aboyans V, Abrha WA, Abu-Gharbieh E, Abushouk AI, Acharya D, Adair T, Adebayo OM, Ademi Z, Advani SM, Afshari K, Afshin A, Agarwal G, Agasthi P, Ahmad S, Ahmadi S, Ahmed MB, Aji B, Akalu Y, Akande-Sholabi W, Aklilu A, Akunna CJ, Alahdab F, Al-Eyadhy A, Alhabib KF, Alif SM, Alipour V, Aljunid SM, Alla F, Almasi-Hashiani A, Almustanyir S, Al-Raddadi RM, Amegah AK, Amini S, Aminorroaya A, Amu H, Amugsi DA, Ancuceanu R, Anderlini D, Andrei T, Andrei CL, Ansari-Moghaddam A, Anteneh ZA, Antonazzo IC, Antony B, Anwer R, Appiah LT, Arabloo J, Ärnlöv J, Artanti KD, Ataro Z, Ausloos M, Avila-Burgos L, Awan AT, Awoke MA, Ayele HT, Ayza MA, Azari S, B DB, Baheiraei N, Baig AA, Bakhtiari A, Banach M, Banik PC, Baptista EA, Barboza MA, Barua L, Basu S, Bedi N, Béjot Y, Bennett DA, Bensenor IM, Berman AE, Bezabih YM, Bhagavathula AS, Bhaskar S, Bhattacharyya K, Bijani A, Bikbov B, Birhanu MM, Boloor A, Brant LC, Brenner H, Briko NI, Butt ZA, Caetano dos Santos FL, Cahill LE, Cahuana-Hurtado L, Cámera LA, Campos-Nonato IR, Cantu-Brito C, Car J, Carrero JJ, Carvalho F, Castañeda-Orjuela CA, Catalá-López F, Cerin E, Charan J, Chattu VK, Chen S, Chin KL, Choi JYJ, Chu DT, Chung SC, Cirillo M, Coffey S, Conti S, Costa VM, Cundiff DK, Dadras O, Dagnew B, Dai X, Damasceno AAM, Dandona L, Dandona R, Davletov K, De la Cruz-Góngora V, De la Hoz FP, De Neve JW, Denova-Gutiérrez E, Derbew Molla M, Derseh BT, Desai R, Deuschl G, Dharmaratne SD, Dhimal M, Dhungana RR, Dianatinasab M, Diaz D, Djalalinia S, Dokova K, Douiri A, Duncan BB, Duraes AR, Eagan AW, Ebtehaj S, Eftekhari A, Eftekharzadeh S, Ekholuenetale M, El Nahas N, Elgendy IY, Elhadi M, El-Jaafary SI, Esteghamati S, Etisso AE, Eyawo O, Fadhil I, Faraon EJA, Faris PS, Farwati M, Farzadfar F, Fernandes E, Fernandez Prendes C, Ferrara P, Filip I, Fischer F, Flood D, Fukumoto T, Gad MM, Gaidhane S, Ganji M, Garg J, Gebre AK, Gebregiorgis BG, Gebregzabiher KZ, Gebremeskel GG, Getacher L, Obsa AG, Ghajar A, Ghashghaee A, Ghith N, Giampaoli S, Gilani SA, Gill PS, Gillum RF, Glushkova EV, Gnedovskaya EV, Golechha M, Gonfa KB, Goudarzian AH, Goulart AC, Guadamuz JS, Guha A, Guo Y, Gupta R, Hachinski V, Hafezi-Nejad N, Haile TG, Hamadeh RR, Hamidi S, Hankey GJ, Hargono A, Hartono RK, Hashemian M, Hashi A, Hassan S, Hassen HY, Havmoeller RJ, Hay SI, Hayat K, Heidari G, Herteliu C, Holla R, Hosseini M, Hosseinzadeh M, Hostiuc M, Hostiuc S, Househ M, Huang J, Humayun A, Iavicoli I, Ibeneme CU, Ibitoye SE, Ilesanmi OS, Ilic IM, Ilic MD, Iqbal U, Irvani SSN, Islam SMS, Islam RM, Iso H, Iwagami M, Jain V, Javaheri T, Jayapal SK, Jayaram S, Jayawardena R, Jeemon P, Jha RP, Jonas JB, Jonnagaddala J, Joukar F, Jozwiak JJ, Jürisson M, Kabir A, Kahlon T, Kalani R, Kalhor R, Kamath A, Kamel I, Kandel H, Kandel A, Karch A, Kasa AS, Katoto PDMC, Kayode GA, Khader YS, Khammarnia M, Khan MS, Khan MN, Khan M, Khan EA, Khatab K, Kibria GMA, Kim YJ, Kim GR, Kimokoti RW, Kisa S, Kisa A, Kivimäki M, Kolte D, Koolivand A, Korshunov VA, Koulmane Laxminarayana SL, Koyanagi A, Krishan K, Krishnamoorthy V, Kuate Defo B, Kucuk Bicer B, Kulkarni V, Kumar GA, Kumar N, Kurmi OP, Kusuma D, Kwan GF, La Vecchia C, Lacey B, Lallukka T, Lan Q, Lasrado S, Lassi ZS, Lauriola P, Lawrence WR, Laxmaiah A, LeGrand KE, Li MC, Li B, Li S, Lim SS, Lim LL, Lin H, Lin Z, Lin RT, Liu X, Lopez AD, Lorkowski S, Lotufo PA, Lugo A, M NK, Madotto F, Mahmoudi M, Majeed A, Malekzadeh R, Malik AA, Mamun AA, Manafi N, Mansournia MA, Mantovani LG, Martini S, Mathur MR, Mazzaglia G, Mehata S, Mehndiratta MM, Meier T, Menezes RG, Meretoja A, Mestrovic T, Miazgowski B, Miazgowski T, Michalek IM, Miller TR, Mirrakhimov EM, Mirzaei H, Moazen B, Moghadaszadeh M, Mohammad Y, Mohammad DK, Mohammed S, Mohammed MA, Mokhayeri Y, Molokhia M, Montasir AA, Moradi G, Moradzadeh R, Moraga P, Morawska L, Moreno Velásquez I, Morze J, Mubarik S, Muruet W, Musa KI, Nagarajan AJ, Nalini M, Nangia V, Naqvi AA, Narasimha Swamy S, Nascimento BR, Nayak VC, Nazari J, Nazarzadeh M, Negoi RI, Neupane Kandel S, Nguyen HLT, Nixon MR, Norrving B, Noubiap JJ, Nouthe BE, Nowak C, Odukoya OO, Ogbo FA, Olagunju AT, Orru H, Ortiz A, Ostroff SM, Padubidri JR, Palladino R, Pana A, Panda-Jonas S, Parekh U, Park EC, Parvizi M, Pashazadeh Kan F, Patel UK, Pathak M, Paudel R, Pepito VCF, Perianayagam A, Perico N, Pham HQ, Pilgrim T, Piradov MA, Pishgar F, Podder V, Polibin RV, Pourshams A, Pribadi DRA, Rabiee N, Rabiee M, Radfar A, Rafiei A, Rahim F, Rahimi-Movaghar V, Ur Rahman MH, Rahman MA, Rahmani AM, Rakovac I, Ram P, Ramalingam S, Rana J, Ranasinghe P, Rao SJ, Rathi P, Rawal L, Rawasia WF, Rawassizadeh R, Remuzzi G, Renzaho AMN, Rezapour A, Riahi SM, Roberts-Thomson RL, Roever L, Rohloff P, Romoli M, Roshandel G, Rwegerera GM, Saadatagah S, Saber-Ayad MM, Sabour S, Sacco S, Sadeghi M, Saeedi Moghaddam S, Safari S, Sahebkar A, Salehi S, Salimzadeh H, Samaei M, Samy AM, Santos IS, Santric-Milicevic MM, Sarrafzadegan N, Sarveazad A, Sathish T, Sawhney M, Saylan M, Schmidt MI, Schutte AE, Senthilkumaran S, Sepanlou SG, Sha F, Shahabi S, Shahid I, Shaikh MA, Shamali M, Shamsizadeh M, Shawon MSR, Sheikh A, Shigematsu M, Shin MJ, Shin JI, Shiri R, Shiue I, Shuval K, Siabani S, Siddiqi TJ, Silva DAS, Singh JA, Mtech AS, Skryabin VY, Skryabina AA, Soheili A, Spurlock EE, Stockfelt L, Stortecky S, Stranges S, Suliankatchi Abdulkader R, Tadbiri H, Tadesse EG, Tadesse DB, Tajdini M, Tariqujjaman M, Teklehaimanot BF, Temsah MH, Tesema AK, Thakur B, Thankappan KR, Thapar R, Thrift AG, Timalsina B, Tonelli M, Touvier M, Tovani-Palone MR, Tripathi A, Tripathy JP, Truelsen TC, Tsegay GM, Tsegaye GW, Tsilimparis N, Tusa BS, Tyrovolas S, Umapathi KK, Unim B, Unnikrishnan B, Usman MS, Vaduganathan M, Valdez PR, Vasankari TJ, Velazquez DZ, Venketasubramanian N, Vu GT, Vujcic IS, Waheed Y, Wang Y, Wang F, Wei J, Weintraub RG, Weldemariam AH, Westerman R, Winkler AS, Wiysonge CS, Wolfe CDA, Wubishet BL, Xu G, Yadollahpour A, Yamagishi K, Yan LL, Yandrapalli S, Yano Y, Yatsuya H, Yeheyis TY, Yeshaw Y, Yilgwan CS, Yonemoto N, Yu C, Yusefzadeh H, Zachariah G, Zaman SB, Zaman MS, Zamanian M, Zand R, Zandifar A, Zarghi A, Zastrozhin MS, Zastrozhina A, Zhang ZJ, Zhang Y, Zhang W, Zhong C, Zou Z, Zuniga YMH, Murray CJL (2020) Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 76 (25):2982–3021. 10.1016/j.jacc.2020.11.010
- 2.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528. doi: 10.1161/cir.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 3.Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37(42):3232–3245. doi: 10.1093/eurheartj/ehw334. [DOI] [PubMed] [Google Scholar]
- 4.Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, Goldstein LB, Gorelick P, Halperin J, Harbaugh R, Johnston SC, Katzan I, Kelly-Hayes M, Kenton EJ, Marks M, Schwamm LH, Tomsick T. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: A statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke - Co-sponsored by the Council on Cardiovascular Radiology and Intervention. The American Academy of Neurology affirms the value of this guideline. Circulation. 2006;113(10):e409–e449. doi: 10.1161/01.STR.0000199147.30016.74. [DOI] [PubMed] [Google Scholar]
- 5.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, Van Wagner LB, Tsao CW, Wong SS, Heard DG (2020) Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation E139–E596. 10.1161/CIR.0000000000000757 [DOI] [PubMed]
- 6.Martínez-González MA, Salas-Salvadó J, Estruch R, Corella D, Fitó M, Ros E. Benefits of the Mediterranean diet: insights from the PREDIMED study. Prog Cardiovasc Dis. 2015;58(1):50–60. doi: 10.1016/j.pcad.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA (2018) Retraction and republication: primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–90. N Engl J Med 378 (25):2441–2442. 10.1056/NEJMc1806491 [DOI] [PubMed]
- 8.Nicklas TA, Drewnowski A, O'Neil CE. The nutrient density approach to healthy eating: challenges and opportunities. Public Health Nutr. 2013;17(12):2626–2636. doi: 10.1017/S136898001400158X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carbone ET, Zoellner JM. Nutrition and health literacy: a systematic review to inform nutrition research and practice. J Acad Nutr Diet. 2012;112(2):254–265. doi: 10.1016/j.jada.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 10.O'Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, Rao-Melacini P, Zhang X, Pais P, Agapay S, Lopez-Jaramillo P, Damasceno A, Langhorne P, McQueen MJ, Rosengren A, Dehghan M, Hankey GJ, Dans AL, Elsayed A, Avezum A, Mondo C, Diener HC, Ryglewicz D, Czlonkowska A, Pogosova N, Weimar C, Iqbal R, Diaz R, Yusoff K, Yusufali A, Oguz A, Wang X, Penaherrera E, Lanas F, Ogah OS, Ogunniyi A, Iversen HK, Malaga G, Rumboldt Z, Oveisgharan S, Al Hussain F, Magazi D, Nilanont Y, Ferguson J, Pare G, Yusuf S. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 11.De Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–785. doi: 10.1161/01.CIR.99.6.779. [DOI] [PubMed] [Google Scholar]
- 12.Delgado-Lista J, Perez-Martinez P, Garcia-Rios A, Alcala-Diaz JF, Perez-Caballero AI, Gomez-Delgado F, Fuentes F, Quintana-Navarro G, Lopez-Segura F, Ortiz-Morales AM, Delgado-Casado N, Yubero-Serrano EM, Camargo A, Marin C, Rodriguez-Cantalejo F, Gomez-Luna P, Ordovas JM, Lopez-Miranda J, Perez-Jimenez F. CORonary Diet Intervention with Olive oil and cardiovascular PREVention study (the CORDIOPREV study): Rationale, methods, and baseline characteristics: a clinical trial comparing the efficacy of a Mediterranean diet rich in olive oil versus a low-fat diet on cardiovascular disease in coronary patients. Am Heart J. 2016;177:42–50. doi: 10.1016/j.ahj.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Willet W. Nutritional epidemiology. 3. New York: Oxford University Press; 2013. [Google Scholar]
- 14.Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Lamuela-Raventós R, Ros E, Salaverría I, Fiol M, Lapetra J, Vinyoles E, Gómez-Gracia E, Lahoz C, Serra-Majem L, Pintó X, Ruiz-Gutierrez V, Covas MI. A Short screener is valid for assessing mediterranean diet adherence among older spanish men and women. J Nutr. 2011;141(6):1140–1145. doi: 10.3945/jn.110.135566. [DOI] [PubMed] [Google Scholar]
- 15.Martinez-Gonzalez MA, Garcia-Arellano A, Toledo E, Salas-Salvado J, Buil-Cosiales P, Corella D, Covas MI, Schroder H, Aros F, Gomez-Gracia E, Fiol M, Ruiz-Gutierrez V, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pinto X, Munoz MA, Warnberg J, Ros E, Estruch R. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS ONE. 2012;7(8):e43134. doi: 10.1371/journal.pone.0043134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martinez-Gonzalez MA, Corella D, Salas-Salvado J, Ros E, Covas MI, Fiol M, Warnberg J, Aros F, Ruiz-Gutierrez V, Lamuela-Raventos RM, Lapetra J, Munoz MA, Martinez JA, Saez G, Serra-Majem L, Pinto X, Mitjavila MT, Tur JA, Portillo MP, Estruch R. Cohort profile: design and methods of the PREDIMED study. Int J Epidemiol. 2012;41(2):377–385. doi: 10.1093/ije/dyq250. [DOI] [PubMed] [Google Scholar]
- 17.Martin-moreno JM, Boyle P, Gorgojo L, Maisonneuve P, Fernandez-rodriguez JC, Salvini S, Willett WC. Development and validation of a food frequency questionnaire in Spain. Int J Epidemiol. 1993;22(3):512–519. doi: 10.1093/ije/22.3.512. [DOI] [PubMed] [Google Scholar]
- 18.Moreiras OCA, Cabrera L, Cuadrado C (2003) Tablas de Composición de alimentos. (Spanish food composition tables), vol 7. Pirámide, Madrid
- 19.J MV (2003) Tabla de composición de alimentos españoles. (Spanish food composition tables), vol 4. Universidad de Granada, Granada
- 20.Willett W, Stampfer M. Implications of total energy intake for epidemiologic analyses. Nutr Epidemiol. 2009 doi: 10.1093/acprof:oso/9780195122978.003.11. [DOI] [PubMed] [Google Scholar]
- 21.Elosua R, Garcia M, Aguilar A, Molina L, Covas MI, Marrugat J. Validation of the Minnesota leisure time physical activity questionnaire in Spanish women. Med Sci Sports Exerc. 2000;32(8):1431–1437. doi: 10.1097/00005768-200008000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Elosua R, Marrugat J, Molina L, Pons S, Pujol E. Validation of the minnesota leisure time physical activity questionnaire in Spanish men. Am J Epidemiol. 1994;139(12):1197–1209. doi: 10.1093/oxfordjournals.aje.a116966. [DOI] [PubMed] [Google Scholar]
- 23.Quintana-Navarro GM, Alcala-Diaz JF, Lopez-Moreno J, Perez-Corral I, Leon-Acuña A, Torres-Peña JD, Rangel-Zuñiga OA, Arenas de Larriva AP, Corina A, Camargo A, Yubero-Serrano EM, Rodriguez-Cantalejo F, Garcia-Rios A, Luque RM, Ordovas JM, Perez-Martinez P, Lopez-Miranda J, Delgado-Lista J. Long-term dietary adherence and changes in dietary intake in coronary patients after intervention with a Mediterranean diet or a low-fat diet: the CORDIOPREV randomized trial. Eur J Nutr. 2020;59(5):2099–2110. doi: 10.1007/s00394-019-02059-5. [DOI] [PubMed] [Google Scholar]
- 24.Sayón-Orea C, Razquin C, Bulló M, Corella D, Fitó M, Romaguera D, Vioque J, Alonso-Gómez ÁM, Wärnberg J, Martínez JA, Serra-Majem L, Estruch R, Tinahones FJ, Lapetra J, Pintó X, Tur JA, López-Miranda J, Bueno-Cavanillas A, Delgado-Rodríguez M, Matía-Martín P, Daimiel L, Sánchez VM, Vidal J, Vázquez C, Ros E, Ruiz-Canela M, Sorlí JV, Castañer O, Fiol M, Navarrete-Muñoz EM, Arós F, Gómez-Gracia E, Zulet MA, Sánchez-Villegas A, Casas R, Bernal-López R, Santos-Lozano JM, Corbella E, Bouzas C, García-Arellano A, Basora J, Asensio EM, Schröder H, Moñino M, García De La Hera M, Tojal-Sierra L, Toledo E, Díaz-López A, Goday A, Salas-Salvadó J, Martínez-González MA. Effect of a nutritional and behavioral intervention on energy-reduced Mediterranean diet adherence among patients with metabolic syndrome: interim analysis of the PREDIMED-plus randomized clinical trial. JAMA. 2019;322(15):1486–1499. doi: 10.1001/jama.2019.14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Middleton KR, Anton SD, Perri MG. Long-term adherence to health behavior change. Am J Lifestyle Med. 2013;7(6):395–404. doi: 10.1177/1559827613488867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zazpe I, Sanchez-Tainta A, Estruch R, Lamuela-Raventos RM, Schröder H, Salas-Salvado J, Corella D, Fiol M, Gomez-Gracia E, Aros F, Ros E, Ruíz-Gutierrez V, Iglesias P, Conde-Herrera M, Martinez-Gonzalez MA. A large randomized individual and group intervention conducted by registered dietitians increased adherence to mediterranean-type diets: the PREDIMED study. J Am Diet Assoc. 2008;108(7):1134–1144. doi: 10.1016/j.jada.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Lapointe A, Weisnagel SJ, Provencher V, Bégin C, Dufour-Bouchard AA, Trudeau C, Lemieux S. Comparison of a dietary intervention promoting high intakes of fruits and vegetables with a low-fat approach: long-term effects on dietary intakes, eating behaviours and body weight in postmenopausal women. Br J Nutr. 2010;104(7):1080–1090. doi: 10.1017/S0007114510001716. [DOI] [PubMed] [Google Scholar]
- 28.Ylimäki EL, Kanste O, Heikkinen H, Bloigu R, Kyngäs H. The effects of a counselling intervention on lifestyle change in people at risk of cardiovascular disease. Eur J Cardiovasc Nurs. 2015;14(2):153–161. doi: 10.1177/1474515114521725. [DOI] [PubMed] [Google Scholar]
- 29.Zenk SN, Tarlov E, Wing C, Matthews SA, Tong H, Jones KK, Powell LM. Long-term weight loss effects of a behavioral weight management program: Does the community food environment matter? Int J Environ Res Public Health. 2018 doi: 10.3390/ijerph15020211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bray GA, Popkin BM. Dietary fat intake does affect obesity. Am J Clin Nutr. 1998;68(6):1157–1173. doi: 10.1093/ajcn/68.6.1157. [DOI] [PubMed] [Google Scholar]
- 31.Drewnowski A. Nutrient density: addressing the challenge of obesity. Br J Nutr. 2018;120(s1):S8–S14. doi: 10.1017/S0007114517002240. [DOI] [PubMed] [Google Scholar]
- 32.Trichopoulou A, Martínez-González MA, Tong TYN, Forouhi NG, Khandelwal S, Prabhakaran D, Mozaffarian D, de Lorgeril M. Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Med. 2014 doi: 10.1186/1741-7015-12-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cano-Ibáñez N, Bueno-Cavanillas A, Martínez-González MÁ, Salas-Salvadó J, Corella D, Freixer GL, Romaguera D, Vioque J, Alonso-Gómez ÁM, Wärnberg J, Martínez JA, Serra-Majem L, Estruch R, Tinahones FJ, Lapetra J, Pintó X, Tur JA, García-Ríos A, García-Molina L, Delgado-Rodríguez M, Matía-Martín P, Daimiel L, Martín-Sánchez V, Vidal J, Vázquez C, Ros E, Bartolomé-Resano J, Palau-Galindo A, Portoles O, Torres L, Miquel F, Sánchez MTC, Sorto-Sánchez C, Moreno-Morales N, Abete I, Álvarez-Pérez J, Sacanella E, Bernal-López MR, Santos-Lozano JM, Fanlo-Maresma M, Bouzas C, Razquin C, Becerra-Tomás N, Ortega-Azorin C, Llimona R, Morey M, Román-Maciá J, Goicolea-Güemez L, Vázquez-Ruiz Z, Barrubés L, Fitó M, Gea A. Effect of changes in adherence to Mediterranean diet on nutrient density after 1-year of follow-up: results from the PREDIMED-Plus Study. Eur J Nutr. 2019 doi: 10.1007/s00394-019-02087-1. [DOI] [PubMed] [Google Scholar]
- 34.Panagiotakos DB, Notara V, Kouvari M, Pitsavos C. The mediterranean and other dietary patterns in secondary cardiovascular disease prevention: a review. Curr Vasc Pharmacol. 2016;14(5):442–451. doi: 10.2174/1570161114999160719104731. [DOI] [PubMed] [Google Scholar]
- 35.Fernández-Ballart JD, Piñol JL, Zazpe I, Corella D, Carrasco P, Toledo E, Perez-Bauer M, Martínez-González MA, Salas-Salvadó J, Martn-Moreno JM. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr. 2010;103(12):1808–1816. doi: 10.1017/S0007114509993837. [DOI] [PubMed] [Google Scholar]
- 36.Ortiz-Andrellucchi A, Sánchez-Villegas A, Doreste-Alonso J, de Vries J, de Groot L, Serra-Majem L. Dietary assessment methods for micronutrient intake in elderly people: a systematic review. Br J Nutr. 2009;102(Suppl 1):S118–149. doi: 10.1017/S0007114509993175. [DOI] [PubMed] [Google Scholar]
- 37.Turconi G, Bazzano R, Roggi C, Cena H. Reliability and relative validity of a quantitative food-frequency questionnaire for use among adults in Italian population. Int J Food Sci Nutr. 2010;61(8):846–862. doi: 10.3109/09637486.2010.495329. [DOI] [PubMed] [Google Scholar]
- 38.Braunholtz DA, Edwards SJ, Lilford RJ. Are randomized clinical trials good for us (in the short term)? Evidence for a "trial effect". J Clin Epidemiol. 2001;54(3):217–224. doi: 10.1016/s0895-4356(00)00305-x. [DOI] [PubMed] [Google Scholar]
- 39.Martínez-González MA, Fernandez-Lazaro CI, Toledo E, Díaz-López A, Corella D, Goday A, Romaguera D, Vioque J, Alonso-Gómez ÁM, Wärnberg J, Martínez JA, Serra-Majem L, Estruch R, Tinahones FJ, Lapetra J, Pintó X, Tur JA, López-Miranda J, Cano-Ibáñez N, Delgado-Rodríguez M, Matía-Martín P, Daimiel L, Sánchez VM, Vidal J, Vázquez C, Ros E, Buil-Cosiales P, Portoles O, Soria-Florido M, Konieczna J, Navarrete-Muñoz EM, Tojal-Sierra L, Fernández-García JC, Abete I, Henríquez-Sánchez P, Muñoz-Garach A, Santos-Lozano JM, Corbella E, Bibiloni MDM, Becerra-Tomás N, Barragán R, Castañer O, Fiol M, García de la Hera M, Belló-Mora MC, Gea A, Babio N, Fitó M, Ruiz-Canela M, Zazpe I, Salas-Salvadó J. Carbohydrate quality changes and concurrent changes in cardiovascular risk factors: a longitudinal analysis in the PREDIMED-Plus randomized trial. Am J Clin Nutr. 2020;111(2):291–306. doi: 10.1093/ajcn/nqz298. [DOI] [PubMed] [Google Scholar]
- 40.Ter Borg S, Verlaan S, Mijnarends DM, Schols JMGA, De Groot LCPGM, Luiking YC. Macronutrient intake and inadequacies of community-dwelling older adults, a systematic review. Ann Nutr Metab. 2015;66(4):242–255. doi: 10.1159/000435862. [DOI] [PubMed] [Google Scholar]
- 41.De La Fuente-Arrillaga C, Zazpe I, Santiago S, Bes-Rastrollo M, Ruiz-Canela M, Gea A, Martinez-Gonzalez MA. Beneficial changes in food consumption and nutrient intake after 10 years of follow-up in a Mediterranean cohort: The SUN project. BMC Public Health. 2016 doi: 10.1186/s12889-016-2739-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cano-Ibáñez N, Gea A, Ruiz-Canela M, Corella D, Salas-Salvadó J, Schroder H, Ma Navarrete-Muñoz E, Romaguera D, Alfredo M, Javier Barón-López F, Lopez-Miranda J, Estruch R, Riquelme-Gallego B, Alonso-Gómez Á, Tur JA, Tinahones F, Serra-Majem L, Martín V, Lapetra J, Bueno-Cavanillas A. Diet quality and nutrient density in subjects with metabolic syndrome: influence of socioeconomic status and lifestyle factors. A cross-sectional assessment in the PREDIMED-Plus study. Clin Nutr. 2019 doi: 10.1016/j.clnu.2019.04.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data described in the manuscript, code book, and analytic code will not be made available because of study`s embargo.