Abstract
Objective
To describe a new alignment technique of adjusted restricted kinematic alignment (arKA) for the treatment of severe varus deformity in total knee arthroplasty.
Methods
Three female patients (three severe varus knees) who underwent navigation‐assisted total knee arthroplasty (TKA) using arKA from April 2020 to September 2020 were included in this study, with an average age of 71.33 years (range, 61 to 80 years). General anesthesia was given to all patients. Intraoperative observations including tibia resection angle, frontal femoral angle, axial femoral angle, medial and lateral gap in the extension and flexion positions and joint line translation were recorded. Also, operation duration and drainage volume were recorded. Radiographic parameters including the mechanical axis (α), coronal femoral component angle (β), coronal tibial component angle (γ), sagittal femoral component angle (δ), tibial posterior slope angle (ε), femoral‐patella angle (θ), and femoral notching were assessed. Clinical evaluation was performed using the Hospital for Special Surgery (HSS) Score and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Score. Both individual and mean measurement data were displayed.
Results
The mean tibial resection was 4.00° varus (range, 3° to 5°), and the mean frontal femoral angle was 3.67° varus (range, 3° to 4°) in extension. The flexion lateral gap was wider than the medial gap with a mean laxity of 1.34 mm. Moreover, the mean axial femoral angle was 2.67° external (range, 0° to 6°) in flexion, and the mean joint line translation was 1.00 mm proximal (range, 0 to 3 mm). In addition, the mean preoperative mechanical axis was 156.22° (range, 153.65° to 158.90°) and the mean postoperative mechanical axis was 174.04° (range, 173.83° to 174.17°) with a mean correction of 17.82°. The mean femoral angle was 92.60° (range, 91.29° to 93.30°) and the mean tibial angle was 86.95° (range, 86.83° to 87.04°) in coronal plane. The HSS score improved from an average of 46.67 points (range, 42 to 51) preoperatively to 83.67 points (range, 81 to 86) at 3 months postoperatively. The mean WOMAC score was 16.33 points at 3 months postoperatively.
Conclusions
The new alignment technique of arKA aims to balance the flexion and extension gap without extensive releases of soft tissue and restore the native pre‐arthritic alignment, may be a promising alignment strategy for treating severe varus deformity. However, further study and comparison with other alignment techniques is needed.
Keywords: alignment, severe, total knee arthroplasty, varus
The new alignment technique of arKA, aims to balance the flexion and extension gap without unnecessary releases of soft tissue and restore the native pre‐arthritic alignment, may be a promising alignment strategy for treating severe varus deformity.
INTRODUCTION
Varus deformity is the most frequently seen angular malformation of the knee in total knee arthroplasty (TKA), characterized by a lower extremity load‐bearing alignment transferred to the medial side of the knee center with both bony deformity and soft tissue imbalance. 1 Several intra‐ or extra‐articular factors have been considered as contributing to the varus deformity, including loss of articular cartilage, remodeling of bone, tibia vara, femoral bowing, stress fractures, prior osteotomy, etc. 2 In addition, severe varus deformity of the knee is presented in approximately 10% of cases with varus arthritis, commonly associated with contracture of flexion and medial soft tissue and elongation of lateral soft tissue, making reconstruction more difficult. 3
Restoration of normal neutral mechanical alignment in varus knees has been identified as the gold standard for TKA by most surgeons for decades. 4 The resection of femur and tibia was perpendicular to neutral axis of each bone in mechanically aligned TKA. As a result, an extremely imbalanced trapezoidal flexion and extension gap frequently remained, especially in severe varus knees. Extensive release of medial soft tissue may be required to pursue the balance of flexion‐extension gap. 5 However, repeat multiple soft tissue and ligament releases may lead to over‐release and create more instability. 6 For example, massive subperiosteal releasing of the tibial attachment of the superficial medial collateral ligament would enhance the risk of extension mediolateral instability. 7 The over‐release and significant imbalance of flexion and extension gap may necessitate the use of constrained implant. 8 Therefore, neutral mechanical alignment (MA) with conventional surgical techniques in TKA has difficulty correcting the severe varus deformity of the knee (deformity>20°). 9
Constitutional varus (physiologic mechanical alignment more than 3° varus) was found in 32% of males and 17% of females in the European population. 10 Even with restoration of alignment to neutral in these cases, the clinical outcomes may not be satisfied due to biomechanical changes. 11 Therefore, alternative TKA alignment philosophies have been proposed, including: (i) anatomic alignment (AA), aiming to resume the natural 2°–3° oblique of proximal tibial plateau; 12 (ii) kinematic alignment (KA), aiming to maintain pre‐arthritis limb alignment and knee laxity using pure bony resection technique; 13 (iii) restricted kinematic alignment (rKA), aiming to compromise the kinematic alignment in a safe zone (≤3°) by tuning the position of tibial component; 14 (iv) adjusted mechanical alignment (aMA), aiming to preserve a slight constitutional deformity (≤3°) based on the MA technique by adjusting the femoral component positioning. 15 These alignment techniques succeed in obtaining good clinical outcomes in varus knees, however, the application of hybrid alignment techniques, such as aMA and rKA, are most appropriate to correct mild or moderate coronal deformity. 16 For severe varus deformity, adequate medial soft tissue releases are also needed in TKA using aMA or rKA technique. 16 , 17 In addition, although KA technique would resume native pre‐arthritic alignment, a significant residual varus was commonly produced and safe zones for postoperative residual deformity are still unclear. 14 , 18
Here, we first described a new alignment technique of “adjusted restricted kinematic alignment” (arKA), characterized by preserved moderate constitutional coronal deformity by adjusting the position of both femoral and tibial components. This technique aims to produce a biomimetic wider lateral flexion‐extension gap and minimize or even avoid releases of soft tissue in severe varus deformity. Briefly, the arKA technique is defined as the hybrid of aMA and rKA. The tibial side osteotomy is the same as rKA, and the femoral side osteotomy is the same as aMA. The purpose of this study was: (i) to present a new aligned technique, which aims to balance the flexion and extension gap by adjusting the resection of both femur and tibia with the assistance of computer navigation system; (ii) to evaluate the effectiveness and clinical outcomes of this new technique for the treatment of patients who underwent TKA with severe knee varus deformity.
MATERIALS AND METHODS
Inclusion and Exclusion Criteria
Inclusion criteria were: (i) patients suffered from end‐stage osteoarthritis with severe varus deformity (>20° varus); (ii) patients underwent computer‐assisted navigation TKAs using arKA technique; (iii) all TKAs were performed by a single experienced knee surgeon (Y.‐Z. Xu). Exclusion criteria were: (i) any tumors or secondary neoplasia diseases; (ii) associated with knee joint infection; and (iii) severe cardiopulmonary dysfunction.
This was a retrospective cohort study. From April 2020 to September 2020, consecutive patients who met the inclusion criteria were included. The study was approved by the medical ethics committee of the First Affiliated Hospital of Soochow University (Ethics Approval Number: 2022057) and informed consent was obtained from patients.
Preoperative Planning
Radiographic evaluation was performed preoperatively to identify the osseous landmarks, osteophytes, and loose bodies in the knee joint. EOS® standing full‐lower limb radiograph was performed to measure the degree of varus deformity. The range of knee motion (ROM) was measured by a goniometer. In addition, the Kellgren–Lawrence (K‐L) grade, Western Ontario, and McMaster Universities Osteoarthritis Index (WOMAC) score and Hospital for Special Surgery (HSS) score were evaluated preoperatively.
Alignment Technique
Definition
Briefly, the arKA technique is a hybrid of adjusted mechanical alignment (aMA) and restricted kinematic alignment (rKA). The elements of gap balancing and measured resection techniques were both involved. This technique allowed us to preserve moderate constitutional frontal deformity in a relatively safe zone (medial proximal tibial angle [MPTA] >85° varus; hip‐knee‐ankle [HKA] angle>174°) due to the protection of soft tissue. 19 , 20 In addition, the adjustment of prosthesis positioning was fine‐tuned on both femoral and tibial sides according to the real‐time feedback of navigation (Figures 1, 2, 3).
Fig. 1.

Radiographs of an 80‐year‐old female patient who underwent navigation‐assisted TKA. The arKA technique was performed on the right knee and aMA was used on the left knee. (A) Preoperative standing full‐lower limb X ray (EOS) showed an osteoarthritis right knee with 153.65° severe varus deformity. (B) Preoperative X‐ray of the right severe varus knee. (C) Postoperative EOS showed a restored right knee with an angle of 5.87° varus and a coronal femoral component angle (β) of 91.29° with a coronal tibial component angle (γ) of 86.98°. (D) Postoperative X‐ray showed a sagittal femoral component angle (δ) of 0.71°, tibial posterior slope angle (ε) of 89.47°, and femoral‐patella angle (θ) of 30.57°
Fig. 2.

Radiographs of a 61‐year‐old female patient using arKA on the left knee and rKA on the right knee in TKA. (A) Preoperative standing full‐lower limb X ray (EOS) showed a severe varus deformity of 158.90° on the left knee. (B) Preoperative X‐ray of the left knee showed malunion of the tibia and fibula. (C) Postoperative EOS showed a restored left knee with an angle of 5.83° varus and a coronal femoral component angle (β) of 93.21° with a coronal tibial component angle (γ) of 87.04°. (D) Postoperative X‐ray showed a sagittal femoral component angle (δ) of 0.56°, tibial posterior slope angle (ε) of 88.10°, and femoral‐patella angle (θ) of 30.50°
Fig. 3.

Radiographs of a 73‐year‐old female patient who underwent TKA using arKA on the left knee and rKA on the right knee. (A) Preoperative standing full‐lower limb X ray (EOS) showed a severe varus deformity of 156.10° on the left knee. (B) Preoperative X‐ray of the left severe varus knee. (C) Postoperative EOS showed a restored left knee with an angle of 6.17° varus and a coronal femoral component angle (β) of 93.30° with a coronal tibial component angle (γ) of 86.83°. (D) Postoperative X‐ray showed a sagittal femoral component angle (δ) of 1.00°, tibial posterior slope angle (ε) of 88.76°, and femoral‐patella angle (θ) of 30.86°
Tibial Resection
The tibial cutting guide was positioned at 3° varus to the vertical line of the mechanical axis of the tibia in coronal plane. The aim was to cut the amounts of medial and lateral bone on the tibial plateau as equal as possible, which restored the pre‐arthritis MPTA in a safe zone and minimized the release of soft tissue. The tibial component slope was set at 0°–3° posterior tilt.
Femoral Resection
On the femoral side, distal resection of the femur was appropriate varus to the line perpendicular to the mechanical axis of the femur in extension. The aim was to restore the medial joint height and obtain an approximate rectangular extension gap without ligament releases. In addition, the distal femur over‐resection was not allowed to prevent proximal translation of the joint line over a distance of 3 mm and to maintain flexion stability. Subsequently, a slight asymmetric flexion gap was achieved using the gap balancing technique by externally rotating the femoral component.
The Flexion and Extension Gap
The balance of flexion and extension gap in arKA technique was simulated with a physiological medial pivoting human knee. The lateral gap laxity was wider than the medial gap in extension and flexion with 1–2 mm more laxity. In addition, a wider flexion gap laxity of 1 mm was produced by the posterior condyle design of the femoral prosthesis (Figure 4).
Fig. 4.
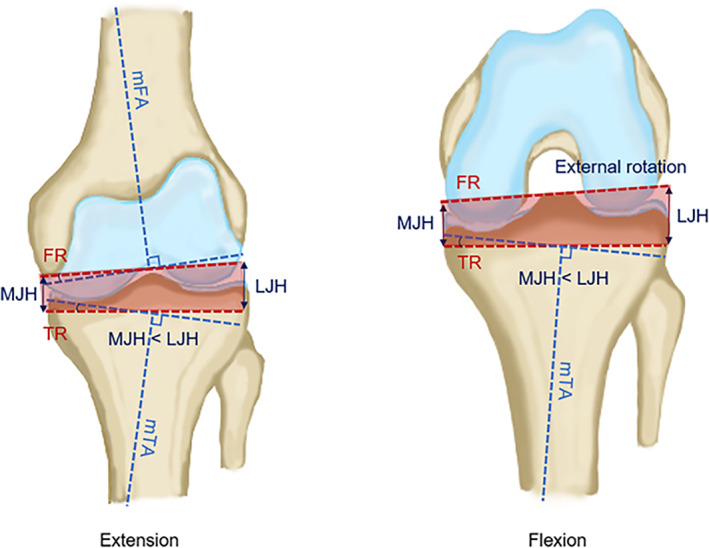
Illustration of the arKA technique. The tibial cutting guide was positioned at 3° varus to the vertical line of the mechanical axis of the tibia in coronal plane. On the femoral side, the resection of the femur was appropriate varus to the line perpendicular to the mechanical axis of the femur, aiming to restore the medial joint height and obtain an approximate rectangular gap in the extension position without ligament release. For flexion gap, external rotation of the femoral component was regulated by soft tissue tension. In addition, a wider flexion lateral gap was produced. Abbreviations: mFA mechanical femoral axis; mTA mechanical tibial axis; FR femoral resection; TR tibial resection; MJH medial joint height; LJH lateral joint height
Surgical Technique
Anesthesia
All operations were performed using general anesthesia.
Position
The patient was placed in the supine position with the operative knee flexed at 90°. The position of the navigation device (OrthoPilot®; B. Braun Aesculap, Tuttlingen, Germany) was leveled with the contralateral shoulder of the patient at a 45° angle to the longitudinal axis of the patient.
Approach and Exposure
The medial parapatellar capsular approach through an approximately 15‐cm midline skin incision was performed in all operations. The skin, subcutaneous tissue, and joint capsule were sequentially cut to expose the knee joint. Then, the anteromedial portion of medial meniscus and anterior and posterior cruciate ligaments were removed. Soft tissues were stripped off 3 cm below the joint line of the tibial medial condyle. Subsequently, the tibial plateau was dislodged, and the lateral meniscus was resected to expose the lateral tibial plateau. Then, femoral and tibial transmitters were positioned 8 cm above and 10 cm below the knee joint line to capture the infrared for the registration step. After the approval of bony anatomical landmarks, osteophytes were then removed which allowed the surgeon to correct the coronal deformity by a manually applied valgus force. Regular releases of soft tissue were not performed at this step. Typically, most varus deformities can be corrected by exposure and removal of osteophytes. Then, the residual varus angle was measured by navigation system again. If residual varus deformity exceeds 6°, appropriate medial soft tissue release or tibial plateau reduction may be needed before using the arKA technique; if residual varus deformity is within 3°–6°, then arKA could be chosen directly; if residual varus deformity is less than 3°, then the aMA or rKA technique could be used.
Intraoperative Observation
The parameters of bony resection and soft tissue balance, including tibia resection angle, frontal femoral angle, axial femoral angle, medial and lateral gap in extension, and flexion position and joint line translation were assessed and recorded intraoperatively (Figure 5). Additionally, the size of the femoral implant and the total height of tibial component (metal plate with PE inlay) were assessed to reach maximum feasible coverage to avoid notching or overhanging. Intraoperative validation was performed immediately after tibial and femoral resection by the attached navigation transmitters (OrthoPilot®; B. Braun Aesculap, Tuttlingen, Germany) according to prior planning.
Fig. 5.

Operation using the arKA technique assisted by the navigation system. (A) Tibial resection was performed at 4° varus to the vertical line of the mechanical axis of the tibia and 2° posterior slope. (B) A moderate varus deformity was preserved on the femoral side with a biomimetic wider lateral flexion gap. (C) Record after resection of tibia and femur. (D) Final coronal alignment after cementation of the definitive prosthesis. (E) Illustration of arKA in a severe varus knee. Tibial and femoral resection (red) was more varus using arKA than MA (orange). Abbreviations: mFA mechanical femoral axis; mTA mechanical tibial axis; FR femoral resection; TR tibial resection
Placement of Prosthesis and Reconstruction
Moreover, a final set of checks, including stability, ROM and patellar trajectory were performed before cementation of the full cemented type UC fixed‐bearing design prosthesis (Columbus UC, B. Braun Aesculap, Tuttlingen, Germany) in situ. The incision was closed and bandaged under pressure.
Outcome Assessment
Radiographic Evaluation
The anteroposterior and lateral views of X‐ray and standing EOS imaging were made pre‐ and postoperatively. 21 The radiographic parameters included the mechanical axis (α), coronal femoral component angle (β), coronal tibial component angle (γ), sagittal femoral component angle (δ), tibial posterior slope angle (ε), femoral‐patella angle (θ), and femoral notching were assessed (Figure 6).
Fig. 6.
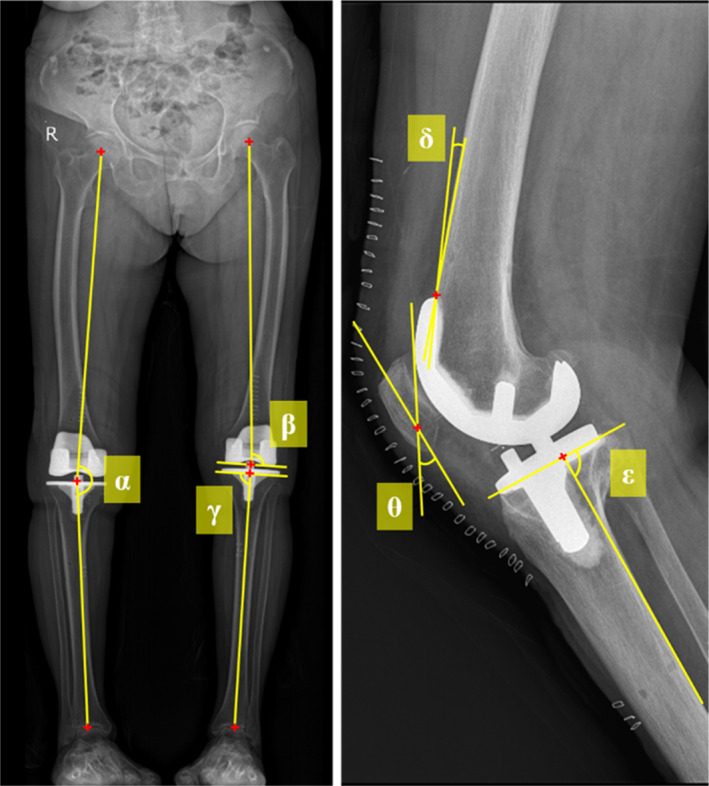
Postoperative radiographic evaluation. The mechanical axis (α) is the line connected among the center of the femoral head, knee, and ankle; the coronal femoral component angle (β) is measured by the angle between the line from the femoral head center to the center of the distal femur and a line tangent to the femoral condyles; the coronal tibial component angle (γ) is measured by the angle between the line from the center of ankle to the center of the proximal tibia and a line tangent to the plateau of tibial component; the sagittal femoral component angle (δ) is measured by the angle between the frontal femoral cortex and the inner frontal part of the femoral component; the tibial posterior slope angle (ε) is measured by the angle between the posterior tibial cortex and the plateau of the tibial component; the femoral‐patella angle (θ) is measured by the angle between the tangent of anterior femoral component and the anatomical axis of patella
Hospital for Special Surgery (HSS) Score
The HSS score was used to evaluate the function of knee pre‐ and postoperatively, which consisted of six parts: pain, function, range of motion, muscle strength, flexion deformity, and knee stability. The maximum of the HSS was 100 points and graded as follows: 85–100 excellent; 70–84 good; 60–69 fair; and 0–59 poor.
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score
The WOMAC score was used to evaluate the severity of knee arthritis and clinical outcome across three aspects: pain, stiffness, and activity. The maximum WOMAC score was 96 points and graded as follows: 49–96 severe; 21–48 moderate; and 1–20 mild.
RESULTS
General Results
All three patients were female, and the average age of patients was 71.33 ± 9.61 years with an average body mass index of 25.67 ± 4.60 kg/m2. All patients met K‐L grade IV. The average preoperative varus deformity was 23.78° ± 2.63°. The range of motion was 88.33° ± 2.89°. The average operation duration was 77.33 ± 5.57 min, and the drainage volume was 83.33 ± 15.28 mL. In addition, the average preoperative HSS score was 46.67 ± 4.51 points and the WOMAC score was 66.00 ± 5.57 points.
Bone Resection Results
During surgery, the mean tibial resection was 4.00° varus (range, 3° to 5° varus, Table 1). The mean medial cutting height of the tibia was 4.67 mm (range, 1 to 8 mm) and the mean lateral cutting height was 9.33 mm (range, 7 to 11 mm). In the extension position, the mean frontal femoral angle was 3.67° varus (range, 3° to 4° varus). The mean distal medial cut of the femur was 8.67 mm (range, 8 to 9 mm) and the mean distal lateral cut was 10.33 mm (range, 9 to 13 mm). In the flexion position, the mean axial femoral angle was 2.67° external (range, 0° to 6° external). The mean posterior medial and lateral cuts of the femur were 8.67 mm (range, 8 to 9 mm) and 7.00 mm (range, 5 to 9 mm), respectively. Additionally, the mean anterior cut of the femur was 1.00 mm (range, 0 to 2 mm). In addition, the mean joint line was 1.00 mm proximal translation (range, 0 to 3 mm).
TABLE 1.
Resection and soft tissue balance data
| Parameters | No.1 | No.2 | No.3 | Mean |
|---|---|---|---|---|
| Tibial resection (°) | 3° varus | 5° varus | 4° varus | 4.00° varus |
| Medial cutting height (mm) | 5.00 | 8.00 | 1.00 | 4.67 |
| Lateral cutting height (mm) | 7.00 | 10.00 | 11.00 | 9.33 |
| Extension | ||||
| Frontal femoral angle (°) | 4° varus | 3° varus | 4° varus | 3.67° varus |
| Distal medial cut (mm) | 8.00 | 9.00 | 9.00 | 8.67 |
| Distal lateral cut (mm) | 9.00 | 9.00 | 13.00 | 10.33 |
| Medial gap (mm) | 0.00 | −1.00 b | 1.00 a | 0.00 |
| Lateral gap (mm) | 1.00 | 1.00 | 2.00 | 1.33 |
| Difference of M‐L extension laxity (mm) | 1.00 | 2.00 | 1.00 | 1.33 |
| Flexion | ||||
| Axial femoral angle (°) | 6° external | 0° external | 2° external | 2.67° external |
| Posterior medial cut (mm) | 9.00 | 8.00 | 9.00 | 8.67 |
| Posterior lateral cut (mm) | 9.00 | 7.00 | 5.00 | 7.00 |
| Anterior cut (mm) | 1.00 | 0.00 | 2.00 | 1.00 |
| Medial gap (mm) | 0.00 | 1.00 | 0.00 | 0.33 |
| Lateral gap (mm) | 2.00 | 1.00 | 2.00 | 1.67 |
| Difference of M‐L flexion laxity (mm) | 2.00 | 0.00 | 2.00 | 1.34 |
| Joint line translation (mm) | 3.00 b | 0.00 | 0.00 | 1.00 |
Abbreviations: difference of M‐L laxity, lateral gap‐medial gap; M‐L, medial‐lateral.
Positive signifies laxity of the soft tissue
Negative signifies distension of the soft tissue
Positive signifies proximal translation.
Soft Tissue Balance Results
The mean medial extension gap was 0.00 mm (range, −1 to 1 mm, Table 1) and the mean lateral extension gap was 1.33 mm (range, 1 to 2 mm) with a mean difference of 1.33 mm laxity between the medial and lateral gaps in extension. In addition, the mean medial flexion gap was 0.33 mm (range, 0 to 1 mm) and the mean lateral flexion gap was 1.67 mm (range, 1 to 2 mm). The lateral flexion gap was wider than the medial gap with a mean laxity of 1.34 mm.
Radiographic Results
Radiographic evaluation revealed that the mean preoperative mechanical axis was 156.22° (range, 153.65° to 158.90°) and the mean postoperative mechanical axis was 174.04° (range, 173.83 to 174.17°) with a mean difference of 17.82° (Table 2). The mean femoral angle was 92.60° (range, 91.29° to 93.30°) in the coronal plane and 0.76° (range, 0.56° to 1.00°) in the sagittal plane. In addition, the mean tibial angle was 86.95° (range, 86.83° to 87.04°) in the coronal plane and 88.78° (range, 88.10° to 89.47°) in the sagittal plane. No femoral notching was observed in three cases.
TABLE 2.
Radiographic data
| Parameters | No.1 | No.2 | No.3 | Mean |
|---|---|---|---|---|
| Mechanical axis | ||||
| Preop. (°) | 153.65 | 158.90 | 156.10 | 156.22 |
| Postop. (°) | 174.13 | 174.17 | 173.83 | 174.04 |
| Femoral angle | ||||
| Coronal plane (°) | 91.29 | 93.21 | 93.30 | 92.60 |
| Sagittal plane (°) | 0.71 | 0.56 | 1.00 | 0.76 |
| Tibial angle | ||||
| Coronal plane (°) | 86.98 | 87.04 | 86.83 | 86.95 |
| Sagittal plane (°) | 89.47 | 88.10 | 88.76 | 88.78 |
| Femoral‐patella angle (°) | 30.57 | 30.50 | 30.86 | 30.64 |
| Femoral Notching | no | no | no | no |
Hospital for Special Surgery (HSS) Score
Clinical evaluation showed that the HSS score improved significantly from an average of 46.67 points (range, 42 to 51) preoperatively to 83.67 points (range, 81 to 86) at 3 months postoperatively with a mean HSS improvement of 37 points (Table 3).
TABLE 3.
Clinical data
| Parameters | No.1 | No.2 | No.3 | Mean |
|---|---|---|---|---|
| Preop. | ||||
| Range of motion (°) | 90.00 | 85.00 | 90.00 | 88.33 |
| HSS score (points) | 47.00 | 42.00 | 51.00 | 46.67 |
| WOMAC score (points) | 65.00 | 61.00 | 72.00 | 66.00 |
| Postop. | ||||
| Range of motion (°) | 130.00 | 121.00 | 126.00 | 125.67 |
| 1 month postop. | ||||
| HSS score (points) | 78.00 | 71.00 | 74.00 | 74.33 |
| WOMAC score (points) | 20.00 | 25.00 | 22.00 | 22.33 |
| 3 months postop. | ||||
| HSS score (points) | 86.00 | 81.00 | 84.00 | 83.67 |
| WOMAC score (points) | 15.00 | 18.00 | 16.00 | 16.33 |
Abbreviations: HSS, Hospital for Special Surgery; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score
Consistently, the WOMAC score in these three cases decreased from a mean preoperative 66.00 points (range, 61 to 72) to 16.33 points (range, 15 to 18) at 3 months postoperatively, with a mean WOMAC score decrease of 49.67 points, which met the classification of mild (Table 3).
Case Reports
Case 1: An 80‐year‐old female patient complained that both knees felt pain 10 years earlier and the pain dramatically increased in the last 3 months, even though the motion of the knees was limited. Physical examination revealed slightly swelling of the bilateral knee and medial joint space tenderness with negative floating patellar test. The range of motion (ROM) of left knee was 0° to 100° in extension‐flexion (E‐F). ROM of right knee was 0° to 90° in E‐F. X‐ray showed obvious medial joint space narrowing and the formation of marginal spurs on both knees (Figure 1). Standing EOS revealed a 6.49° varus deformity in the left knee and 26.35° varus in the right knee, which met the standard of severe varus deformity. The Kellgren–Lawrence (K‐L) grade of right knee was grade IV and HSS (hospital for special surgery) knee score was 47 preoperatively. The arKA technique was performed on the right knee and aMA was used on the left knee.
Case 2: A 61‐year‐old female patient complained of pain in both knees for more than 40 years and knee activity was restricted in the last half year. Past medical history: previous tibial osteotomy 30 years ago. Physical examination revealed slight swelling of both knees and tenderness in the medial joint space. ROM of left knee was 0° to 85° in E‐F. ROM of right knee was 0° to 90°. Radiographs indicated a 21.10° varus deformity in the left knee and a 17.95° varus in the right knee, with malunion of left tibia and fibula (Figure 2). The varus deformity of left knee was severe and achieved K‐L grade IV. HSS score was 42 before surgery. The arKA technique was performed on the left knee and rKA was used on the right knee.
Case 3: A 73‐year‐old female patient presented to the hospital with severe osteoarthritis in both knees. Similar clinical symptoms and physical signs were observed as described before. ROM of left knee was 10° to 100° in E‐F. ROM of right knee was 30° to 95°. A 23.90° severe varus deformity on the left knee and 14.85° varus on the right knee were found by standing EOS (Figure 3). The K‐L grade of left knee was grade IV and the HSS score was 51 preoperatively. The arKA technique was performed on the left knee and rKA was used on the right knee.
DISCUSSION
Main Findings of Study
Various alignment techniques have been used in TKA for the treatment of varus deformity, including the MA, aMA, KA, rKA, and AA techniques. Most of these alignment techniques, such as MA, aMA, rKA, and AA, are not adequate to treat severe varus knee without extensive medial soft tissue releases. The residual constitutional coronal deformity was overly significant in TKA using the KA technique. Therefore, our study has described a new alignment technique of arKA for the first time, characterized by preserved moderate constitutional coronal deformity by adjusting the position of both femoral and tibial components. In our study, the average tibial resection was 4.00° varus, and the frontal femoral angle was 3.67° varus in extension. Moreover, the mean axial femoral angle was 2.67° external in flexion. In addition, the flexion lateral gap was wider than the medial gap with a mean laxity of 1.34 mm. Also, the mean joint line translation was 1.00 mm proximal. Overall, this technique aims to produce a biomimetic wider lateral flexion‐extension gap and minimize or avoid releases of soft tissue for treatment of severe varus deformity.
Safe Zones
The first disputable point of the arKA technique might be the safe zones of residual constitutional frontal deformity. Hirschmann et al. found that the distribution of HKA angle phenotypes was within a zone of 6° varus to 3° valgus represented in 96% of young non‐osteoarthritic Caucasian knees. 19 Moreover, patients with slight under correction (3°–6° varus) following TKA even resulted in superior functional outcomes in preoperative varus knees with a mean of 7.2 years of follow‐up. 22 For MPTA, 93.8% of non‐osteoarthritic knees had MPTA within a zone of 82.5° (varus) to 91.5° (valgus) in young Caucasian population. 20 Nakajima et al. showed that patients with an angle of postoperative joint line obliquity ≥2° led to higher satisfaction and better clinical outcomes. 23 All these data provide a better understanding of physiological knee alignment variability. Moreover, several studies showed no significant difference in 15‐year prosthesis survivorship between postoperative mechanical axes beyond and within the range of 0° ± 3°. 24 , 25 Therefore, in contrast to the traditional safe zones (0° ± 3° varus/valgus), the safe zones of preserved constitutional deformity using the arKA technique we defined were HKA angle ≥174° (varus) and MPTA ≥85° (varus) due to the protection of soft tissue and restoration of native pre‐arthritic alignment as much as possible in severe varus knees. This alignment technique matches the stated concept of the kinematic alignment technique. 26 In addition, the safe zones are mainly targeted for the previous prosthesis, taking into account the prosthetic wear factors. As a result, surgeons tried to establish a systematically “biomechanically friendly” prosthesis knee with a neutrally aligned lower limb. However, great strides are being made in modern knee joints regardless of prosthetic design and materials, allowing deviations in prosthesis position. Therefore, the safe zones also increase, which could be regarded as the basis for various new alignments.
Soft Tissue Balance
Another different point of the arKA technique was the goal of soft tissue balance. The classical symmetrical rectangular extension and flexion gap was considered the gold standard for TKA, due to the imbalanced soft tissue possibly being attributed to the failure of TKA. 27 Generally, an extreme trapezoidal gap remained after resection of the tibia and femur using conventional alignment technique in severe varus knees. Multiple additional soft tissue releases may necessitate compensation for the imbalanced gap in flexion and extension. However, repeat extensive releases of soft tissue and ligaments may easily over‐release and create more instability. A distinctive feature of the native human knee is medial‐pivot motion with less activity of the medial compartment. 28 During the passive flexion from 90° to 162°, the backwards movement was 6.5 mm on the medial femoral condyle and 28 mm on the lateral femoral condyle, which indicated a more relaxed lateral compartment. 29 Studies on cadaveric knees have revealed that lateral flexion laxity is typically wider than medial flexion laxity and that the flexion gap tends to be larger than the extension gap when both anterior and posterior ligaments are intact. 30 In our study, we achieved a biomimetic medial pivoting balance of flexion and extension gap by adjusting the tibial and femoral components positioning to avoid unnecessary releases of soft tissue. A wider lateral and flexion gap laxity was produced with the arKA technique, which is consistent with the results of McEwen et al. who even advocated a greater degree laxity (>2 mm) of the lateral flexion gap to obtain superior clinical outcomes. 31 Therefore, we believe that a slight asymmetry with a wider lateral flexion‐extension gap laxity of 1–2 mm achieves better soft tissue balance than a conventional symmetric gap.
High Accuracy of Bone Resection
The third feature of the arKA technique was the challenge of precise bone resection. The lower surgical accuracy of traditional instruments might increase the risk of having a deleterious excessive varus or valgus alignment. However, with the assistance of a computer navigation system, surgeons were able to finely adjust the prosthesis position consciously. The bone cut was accurate to 1 mm and lower limb alignment was controlled to 1° under navigation system. Therefore, the use of precision tools for implant positioning, such as the computer navigation system in this study, can compensate for the lack of surgical accuracy and obtain the effects of the arKA technique.
Clinical Evaluation
In these three cases, the clinical and functional outcomes of the arKA technique were satisfactory. No surgical complications, including neurovascular injury, infection of the knee, patellofemoral problems and dislocation were observed during the follow‐up, which indicated the short‐term feasibility and effectiveness of the arKA technique for the treatment of severe varus deformity.
Limitations of the Study
The current study has several limitations. First, the sample size was small with inadequate follow‐up to systematically evaluate the new alignment technique. Second, the arKA technique was performed with the assistance of computer navigation system or robotic technology, which may not be applied to patients who underwent TKA using traditional instruments. In addition, the subarticular bone was used as a surrogate for the joint line because wear cartilage was not compensated by MR reconstruction. Finally, prospective investigation and further comparison with other existing alignment techniques are needed to determine the value of this new alignment technique.
Conclusions
The clinical relevance of our findings is that the new alignment technique of arKA, which aims to balance the flexion and extension gap without unnecessary releases of soft tissue and restore native pre‐arthritic alignment, may be a promising alignment strategy for treating severe varus deformity.
DECLARATIONS
ETHICS APPROVAL
This study was approved by the local Ethics Committee of the First Affiliated Hospital of Soochow University.
INFORMED CONSENT
Written informed consent was obtained from the patients for publication of related clinical data and images.
DISCLOSURE
The authors have no conflicts of interest to declare that are relevant to the content of this article.
AUTHORSHIP CONTRIBUTION STATEMENT
Kai Zheng: conceptualization, data collection, manuscript writing. Feng Zhu: data collection, manuscript editing. Weicheng Zhang: statistical analysis, manuscript editing. Houyi Sun: data analysis. Jun Zhou: manuscript revision. Rongqun Li: supervision, manuscript revision. Yaozeng Xu: patients' treatments, supervision, and final approvement of submission. All authors read and approved the manuscript.
ACKNOWLEDGMENTS
This work is supported by grants from the National Natural Science Foundation of China (Nos. 82072498, 81672238 and 81873990).
Kai Zheng, Feng Zhu, and Weicheng Zhang authors contributed equally to this work.
REFERENCES
- 1. Verdonk PC, Pernin J, Pinaroli A, Ait Si Selmi T, Neyret P. Soft tissue balancing in varus total knee arthroplasty: an algorithmic approach. Knee Surg Sports Traumatol Arthrosc. 2009;17:660–6. [DOI] [PubMed] [Google Scholar]
- 2. Mullaji A, Marawar S, Sharma A. Correcting varus deformity. J Arthroplasty. 2007;22:15–9. [DOI] [PubMed] [Google Scholar]
- 3. Rossi R, Cottino U, Bruzzone M, Dettoni F, Bonasia DE, Rosso F. Total knee arthroplasty in the varus knee: tips and tricks. Int Orthop. 2019;43:151–8. [DOI] [PubMed] [Google Scholar]
- 4. Riviere C, Iranpour F, Auvinet E, et al. Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res. 2017;103:1047–56. [DOI] [PubMed] [Google Scholar]
- 5. Engh GA. The difficult knee: severe varus and valgus. Clin Orthop Relat Res. 2003;416:58–63. [DOI] [PubMed] [Google Scholar]
- 6. Kim MS, Koh IJ, Choi YJ, Kim YD, In Y. Correcting severe Varus deformity using trial components during total knee arthroplasty. J Arthroplasty. 2017;32:1488–95. [DOI] [PubMed] [Google Scholar]
- 7. D'Lima DD, Patil S, Steklov N, Colwell CW Jr. An ABJS best paper: dynamic intraoperative ligament balancing for total knee arthroplasty. Clin Orthop Relat Res. 2007;463:208–12. [PubMed] [Google Scholar]
- 8. Sim JA, Lee YS, Kwak JH, Yang SH, Kim KH, Lee BK. Comparison of complete distal release of the medial collateral ligament and medial epicondylar osteotomy during ligament balancing in varus knee total knee arthroplasty. Clin Orthop Surg. 2013;5:287–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mullaji AB, Shetty GM. Correction of varus deformity during TKA with reduction osteotomy. Clin Orthop Relat Res. 2014;472:126–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vandekerckhove PTK, Matlovich N, Teeter MG, MacDonald SJ, Howard JL, Lanting BA. The relationship between constitutional alignment and varus osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2017;25:2873–9. [DOI] [PubMed] [Google Scholar]
- 12. Hungerford DS, Kenna RV, Krackow KA. The porous‐coated anatomic total knee. Orthop Clin North Am. 1982;13:103–22. [PubMed] [Google Scholar]
- 13. Lee YS, Howell SM, Won YY, Lee OS, Lee SH, Vahedi H, et al. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25:3467–79. [DOI] [PubMed] [Google Scholar]
- 14. Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli PA. The impact of mechanical and restricted kinematic alignment on knee anatomy in Total knee arthroplasty. J Arthroplasty. 2017;32:2133–40. [DOI] [PubMed] [Google Scholar]
- 15. Winnock de Grave P, Luyckx T, Claeys K, Tampere T, Kellens J, Müller J, et al. Higher satisfaction after total knee arthroplasty using restricted inverse kinematic alignment compared to adjusted mechanical alignment. Knee Surg Sports Traumatol Arthrosc. 2020;30:488–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Oussedik S, Abdel MP, Victor J, Pagnano MW, Haddad FS. Alignment in total knee arthroplasty. Bone Joint J. 2020;102‐B:276–9. [DOI] [PubMed] [Google Scholar]
- 17. Chang JS, Kayani B, Wallace C, Haddad FS. Functional alignment achieves soft‐tissue balance in total knee arthroplasty as measured with quantitative sensor‐guided technology. Bone Joint J. 2021;103‐B:507–14. [DOI] [PubMed] [Google Scholar]
- 18. Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S. Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non‐osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc. 2019;27:1394–402. [DOI] [PubMed] [Google Scholar]
- 19. Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB. Phenotyping of hip‐knee‐ankle angle in young non‐osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc. 2019;27:1378–84. [DOI] [PubMed] [Google Scholar]
- 20. Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S. Phenotyping the knee in young non‐osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc. 2019;27:1385–93. [DOI] [PubMed] [Google Scholar]
- 21. Melhem E, Assi A, El Rachkidi R, Ghanem I. EOS((R)) biplanar X‐ray imaging: concept, developments, benefits, and limitations. J Child Orthop. 2016;10:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:2325–30. [DOI] [PubMed] [Google Scholar]
- 23. Nakajima A, Sonobe M, Akatsu Y, Aoki Y, Takahashi H, Suguro T, et al. Association between limb alignment and patient‐reported outcomes after total knee arthroplasty using an implant that reproduces anatomical geometry. J Orthop Surg Res. 2018;13:320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Morgan SS, Bonshahi A, Pradhan N, Gregory A, Gambhir A, Porter ML. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop. 2008;32:639–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen‐year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–9. [DOI] [PubMed] [Google Scholar]
- 26. Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471:1000–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Romero J, Stahelin T, Binkert C, Pfirrmann C, Hodler J, Kessler O. The clinical consequences of flexion gap asymmetry in total knee arthroplasty. J Arthroplasty. 2007;22:235–40. [DOI] [PubMed] [Google Scholar]
- 28. Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br. 2000;82:1189–95. [DOI] [PubMed] [Google Scholar]
- 29. Nakagawa S, Kadoya Y, Todo S, Kobayashi A, Sakamoto H, Freeman MAR, et al. Tibiofemoral movement 3: full flexion in the living knee studied by MRI. J Bone Joint Surg Br. 2000;82:1199–200. [DOI] [PubMed] [Google Scholar]
- 30. Nowakowski AM, Majewski M, Muller‐Gerbl M, Valderrabano V. Measurement of knee joint gaps without bone resection: "physiologic" extension and flexion gaps in total knee arthroplasty are asymmetric and unequal and anterior and posterior cruciate ligament resections produce different gap changes. J Orthop Res. 2012;30:522–7. [DOI] [PubMed] [Google Scholar]
- 31. McEwen P, Balendra G, Doma K. Medial and lateral gap laxity differential in computer‐assisted kinematic total knee arthroplasty. Bone Joint J. 2019;101‐B:331–9. [DOI] [PubMed] [Google Scholar]


