Abstract
Objective
Growing rods surgery is the mainstay of treatment for early‐onset scoliosis (EOS) while proximal junctional kyphosis (PJK) is one of the most commonly reported postoperative complications. We sought to investigate the impact of the location of upper instrumented vertebra (UIV) in relation to the sagittal apex on proximal junctional kyphosis in EOS after traditional growing rods (GRs) treatment.
Methods
A total of 102 EOS patients who received traditional growing rods treatment with a follow‐up of at least 2 years between 2009 and 2020 were retrospectively reviewed. Radiographic measurements were performed before and after the index surgery and at the latest follow‐up. We investigated the coronal Cobb angle and spinopelvic parameters of the whole spine. The location of the UIV, apex, lower instrumented vertebra (LIV), inflection vertebra (IV), the number and distance of UIV‐apex, LIV‐apex and IV‐apex were also recorded. Risk factors for PJK were analyzed by logistic regression analysis.
Results
PJK was observed in 21 patients (20.6%) during the follow‐up period. The PJK group showed a younger age at the index surgery (5.9 vs. 7.1 years, P = 0.042), more lengthening procedure times (5.0 vs. 4.0, P = 0.032), larger preoperative coronal Cobb angle (82.0 vs. 75.6°, P = 0.038), higher correction rate (51.2% vs. 44.4%, P = 0.047) and larger postoperative proximal junctional angle (PJA) (13.9 vs. 5.5°, P < 0.001) than the non‐PJK group. The ratio of the number and distance from UIV‐apex to IV‐apex also differed significantly between the two groups. The logistic regression revealed that age at the index surgery ≤ 7 years, the ratio of the number from UIV‐ apex to IV‐ apex ≤ 0.6 and the ratio of the distance from UIV‐ apex to IV‐ apex ≤ 0.6 were independent risk factors for postoperative PJK.
Conclusion
Besides younger age, a closer location of UIV relative to the sagittal apex is identified to be an independent risk factor of postoperative PJK. Selection of UIV at a relatively farther location away from the sagittal apex might help prevent occurrence of PJK.
Keywords: Complications, Early‐onset scoliosis, Growing rods treatment, Proximal junctional kyphosis, Upper instrumented vertebra

The current study firstly involved the concept of symmetric or non‐symmetric instrumentations in growing rods (GRs) treatment and compared the effects of these two surgical strategies on the occurrence of postoperative proximal junctional kyphosis (PJK).
Introduction
Early‐onset scoliosis (EOS), a rapidly progressive spinal deformity, refers to scoliosis that occurred before the age of 10 years. 1 , 2 In past decades, traditional growing rods (GRs) treatment has been widely applied in EOS patients because of its effectiveness in controlling the progression of spinal deformity while allowing the growth of the spine. 3 , 4 , 5 However, the complication rate of GRs treatment is reported as high as 50%, including implant‐related complications, alignment‐related complications, and general complication. 6 , 7 , 8 , 9
Proximal junctional kyphosis (PJK) is the most common alignment‐related complication in EOS patients after GRs treatment. Although the current definition of PJK is mainly the imaging manifestations, severe PJK may cause vertebra collapse, acute subluxation or implant failure around the upper instrumented vertebra (UIV), also known as proximal junctional failure. 10 The incidence of PJK varied from 12% to 56% due to the differences in study samples, patient etiologies, surgical strategies, and follow‐up times. Different risk factors have been reported to be associated with PJK, including preoperative hyperkyphosis, low pelvic incidence (PI) and the location of UIV or lower instrumented vertebra (LIV). 4 , 11 , 12 , 13 Pan et al. found that patients with UIV at T2 and above were more likely to avoid postoperative PJK. 12 Watanabe et al. reported that an LIV at or cranial to L3 increased the occurrence of PJK. However, previous studies only focused on the independent selection of UIV and LIV while the influence of the relative position of UIV and LIV on PJK received little attention. Each patient with EOS has a different pattern on the coronal or sagittal plane. If we follow the rule that in any case that UIV is selected at T2 or above and LIV at L3 or below, GRs surgery may interfere with the growth and activity function of non‐deformity area. Therefore, a more specific protocol for the selection of UIV and LIV is needed.
Although previous studies have reported the effect of the location of UIV or LIV on postoperative PJK in EOS patients, to our knowledge, no studies have evaluated the distance between UIV and the sagittal apex vertebra in EOS patients who had undergone GRs treatment. Thus, the aim of this study was: (i) to determine the risk factors of postoperative PJK during growing rods treatment; and (ii) to investigate the influence of the location of UIV in relation to the sagittal apex on the occurrence of PJK.
Materials and Methods
Study Sample
Following institutional ethical approval (IRB No.2017–119–08), a retrospective review was performed on our spinal deformity database. Between January 2009 and December 2020, a total of 102 EOS patients underwent GRs treatment at a single center. The inclusion criteria were: (i) lengthening procedures≥2 times; (ii) follow‐up more than 2 years; and (iii) availability of complete radiographs. The exclusion criteria were: (i) previous history of spinal surgery or spinal tumors; and (ii) vertical expandable prosthetic titanium rib technique (VEPTR). Based on the medical records, the basic information data, such as age, gender and etiology were collected. Subsequently, surgical information, including the locations of UIV, LIV and inflection vertebra (IV), were also gathered. According to whether PJK occurred, patients were divided into PJK group and non‐PJK group.
For patients with a Risser grade ≥ 2 or those with limited growth remaining, some received definitive fusion surgery while the others retained their previous implants with no additional surgery and followed up for 2 years or more. These patients were called “graduates.” 14 , 15 , 16
Radiographic Evaluation
Relying on the Picture Archiving and Communications Systems workstation, the radiographic measurement of the whole spine anterior and lateral radiographs was accomplished. Radiographic measurements include following parameters: coronal Cobb angle, thoracic kyphosis (TK), lumbar lordosis (LL), PI and proximal junctional angle (PJA). The T1‐S1 height was measured from the superior endplate of T1 to the superior endplate of S1. And the T1‐T12 height was the vertical distance between the mid‐points of the superior endplate of T1 and the inferior endplate of T12. Apex was considered as the apex of the thoracic kyphosis. IV was defined as the vertebra where the lumbar lordosis transitioned into the thoracic kyphosis. As an important parameter to classify the normal sagittal shapes of spinopelvic organization, IV represents the actual location where the kyphotic curve turns in the lordotic curve. The number and relative distance of vertebra from UIV to apex and IV to apex were recorded while the span number ratio (span NR) and the span relative distance ratio (span DR) of vertebra were calculated by UIV‐apex/IV‐apex. In order to evaluate the effectiveness, the implant‐related complications (rod breakage and dislodged), alignment related complications (PJK), and surgical site infection were all recorded.
PJA was defined as the Cobb angle between the lower endplate of the UIV and the upper endplate of the second supradjacent vertebra above the UIV. PJK was defined as a PJA ≥ 10° and an increase of more than 10° from the preoperative value. Yagi's classification 17 was employed for PJK types: (i) Type 1, ligamentous failure; (ii) Type 2, bone failure, such as fracture at or above the UIV; and (iii) Type 3, implant/bone interface failure (Fig. 1).
Fig. 1.
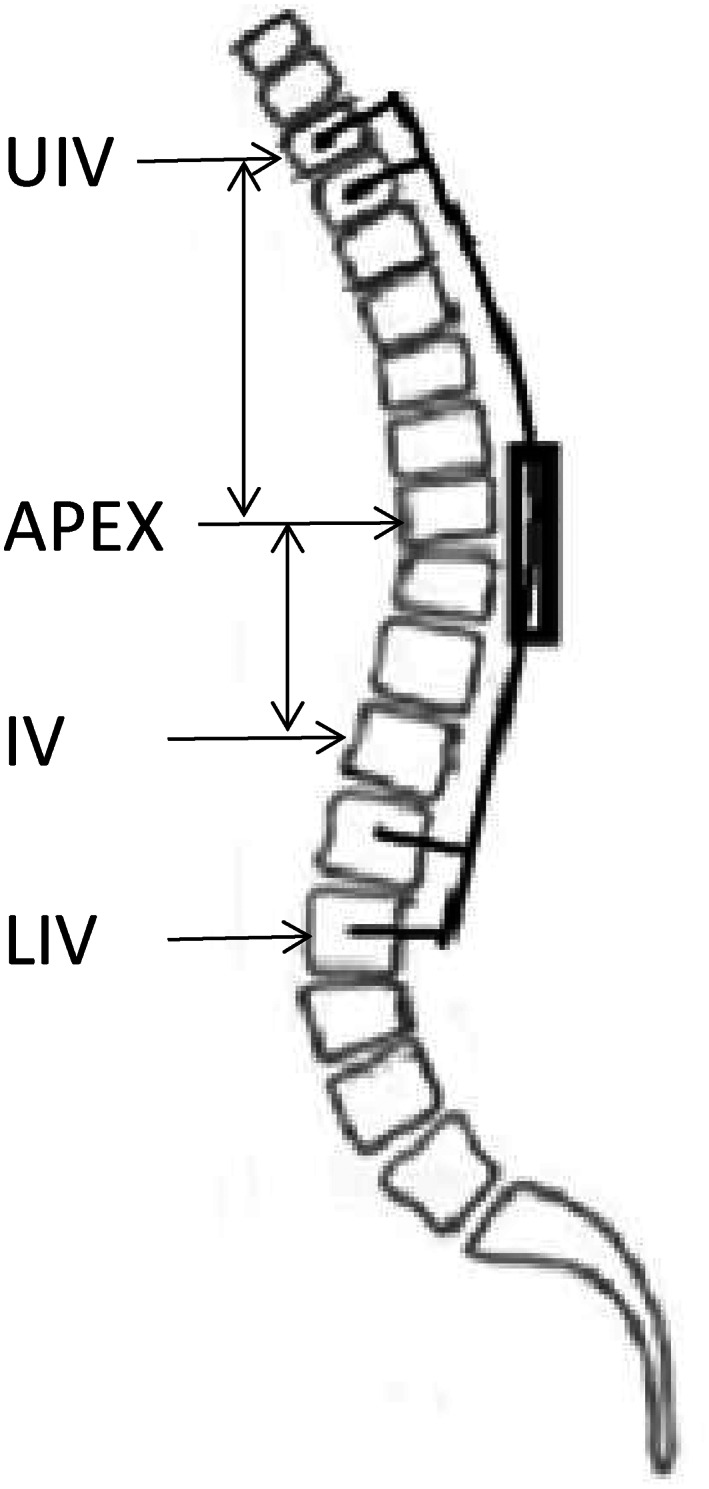
The measurement of apex, infection vertebra, UIV‐apex, and IV‐apex
Statistical Analyses
All analyses were performed by SPSS version 22.0 software (SPSS Inc., Chicago, IL, USA). The data were represented as mean ± standard deviation. The independent‐sample t test was used to assess the differences between the PJK and non‐PJK groups. The chi‐squared tests was used to assess the impact of categorical variables on the development of PJK. Subsequently, logistic regression analysis was performed on predictors with a univariate P value of <0.10 to analyze the covariate effects of the possible indicators for the development of PJK. Receiver operating characteristic (ROC) curve analysis was used to determine the cutoff value for an independent variable. P < 0.05 was considered statistically significant.
ResultsBaseline Data
Of these 102 EOS patients (50 boys and 52 girls; mean age at surgery, 6.8 ± 2.4 years), they can be divided into: congenital in 65 patients, neuromuscular in 11, idiopathic in 13, and syndromic in 13 according to the etiology. The average follow‐up time was 52.8 ± 22.8 months (range, 24–111 months), and the mean lengthening procedures were 4.4 ± 1.7 times, respectively. (Table 1) Dual rods were performed in 84 cases and single rod in 18 cases. The proximal instrumentation type included pedicle screws in 83 patients, hooks in eight and hybrid constructs in 11 while the distal instrumentation was exclusively with pedicle screws. The locations of UIV, IV and LIV are shown in Table 2. Till the last follow‐up, 25 patients graduated from GRs treatment, including 16 who had undergone definitive spinal fusion surgery and 9 who had retained their previous implants with no additional surgery.
TABLE 1.
Demographic and baseline information of EOS patients
| Sample size | 102 |
| Sex (M/F) | 50/52 |
| Age at index surgery (y) | 6.8 ± 2.4 (2–10) |
| Follow up (y) | 4.4 ± 1.9 |
| Lengthening procedures | 4.4 ± 1.7 |
| Diagnosis | |
| Congenital | 65 |
| Neuromuscular | 11 |
| Idiopathic | 13 |
| Syndromic | 13 |
TABLE 2.
Comparison in demographic and surgical data
| Total | PJK group | non‐PJK group | P | |
|---|---|---|---|---|
| Sex (Male/female) | 50/52 | 9/12 | 41/40 | 0.526 |
| BMI (kg/m2) | 16.0 ± 4.2 | 15.5 ± 3.2 | 16.2 ± 4.5 | 0.641 |
| Age at index surgery (y) | 6.8 ± 2.4 | 5.9 ± 2.3 | 7.1 ± 2.4 | 0.042 |
| Follow up (y) | 4.4 ± 1.9 | 4.8 ± 2.6 | 4.3 ± 1.7 | 0.051 |
| Single/Dual rod (s) | 18/84 | 4/17 | 14/67 | 0.849 |
| Proximal anchors (screws/hooks/hybrid) | 83/8/11 | 18/1/2 | 65/7/9 | 0.810 |
| Lengthening procedures | 4.4 ± 1.7 | 5.0 ± 2.2 | 4.2 ± 1.6 | 0.032 |
| Location of UIV | ||||
| T1 | 9 | 0 | 9 | |
| T2 | 28 | 2 | 26 | |
| T3 | 30 | 5 | 25 | |
| T4 | 24 | 8 | 16 | |
| T5 | 11 | 6 | 5 | |
| Location of LIV | ||||
| L1 | 8 | 1 | 7 | |
| L2 | 13 | 1 | 12 | |
| L3 | 42 | 5 | 37 | |
| L4 | 36 | 13 | 23 | |
| L5 | 3 | 1 | 2 | |
| Location of IV | ||||
| T11 | 1 | 0 | 1 | |
| T12 | 21 | 2 | 19 | |
| L1 | 33 | 13 | 20 | |
| L2 | 14 | 4 | 10 | |
| L3 | 4 | 2 | 2 | |
General Results after GR Treatment
As shown in Table 3, the major Cobb angle (76.6 ± 18.1 vs. 41.0 ± 12.9°, P < 0.001) and the TK (43.5 ± 13.8 vs. 30.1 ± 8.8°, P < 0.001) were significantly improved after the index surgery. Both the major curve and the TK remained steady during follow up. The postoperative T1‐T12 height increased from 15.0 ± 2.6 cm to 17.1 ± 2.7 cm and increased to 19.9 ± 3.4 cm at the last follow up. The mean T1‐S1 height preoperatively was 24.9 ± 4.6 cm. After the index surgery, the mean T1‐S1 height increased to 27.5 ± 3.8cm. As of last follow‐up, the mean TI‐S1 height was 33.7 ± 3.7 cm.
TABLE 3.
Comparison in radiographic measurements
| Total | PJK group | non‐PJK group | P | |
|---|---|---|---|---|
| Major Cobb | ||||
| Preoperative | 76.6 ± 18.1 | 82.0 ± 21.2 | 75.6 ± 17.2 | 0.038 |
| Postoperative | 41.0 ± 12.9 | 39.4 ± 12.9 | 41.7 ± 13.0 | 0.842 |
| Correction rate (%) | 45.9 ± 12.9 | 51.2 ± 12.8 | 44.4 ± 12.7 | 0.047 |
| Latest follow‐up | 46.1 ± 13.1 | 46.7 ± 12.8 | 45.7 ± 12.8 | 0.739 |
| PJA | ||||
| Preoperative | 5.6 ± 3.0 | 6.7 ± 4.0 | 5.3 ± 2.6 | 0.056 |
| Postoperative | 7.2 ± 5.7 | 13.9 ± 9.0 | 5.5 ± 2.5 | 0.000 |
| Latest follow‐up | 9.1 ± 6.8 | 20.2 ± 6.3 | 6.4 ± 3.2 | 0.000 |
| TK | ||||
| Preoperative | 43.5 ± 13.8 | 47.2 ± 15.2 | 42.6 ± 13.5 | 0.179 |
| Postoperative | 30.1 ± 8.8 | 30.1 ± 7.6 | 30.2 ± 9.1 | 0.994 |
| Latest follow‐up | 34.1 ± 10.2 | 35.9 ± 10.7 | 33.7 ± 10.6 | 0.391 |
| PI | ||||
| Preoperative | 37.6 ± 9.4 | 34.8 ± 9.3 | 38.8 ± 9.1 | 0.407 |
| Postoperative | 39.8 ± 8.2 | 38.5 ± 7.7 | 40.5 ± 8.3 | 0.653 |
| Latest follow‐up | 40.3 ± 9.6 | 40.4 ± 12.1 | 40.2 ± 9.0 | 0.883 |
| Number | ||||
| UIV‐APEX | 4.3 ± 1.7 | 3.2 ± 1.3 | 4.6 ± 1.6 | 0.001 |
| IV‐APEX | 5.6 ± 1.7 | 6.1 ± 1.1 | 5.4 ± 1.6 | 0.111 |
| LIV‐APEX | 7.5 ± 1.8 | 7.8 ± 1.4 | 7.5 ± 1.6 | 0.595 |
| Span NR (UIV‐IV) | 0.8 ± 0.6 | 0.6 ± 0.3 | 0.9 ± 0.7 | 0.028 |
| Span NR (UIV‐LIV) | 0.6 ± 0.5 | 0.5 ± 0.3 | 0.6 ± 0.2 | 0.435 |
| Distance | ||||
| UIV‐APEX | 53.0 ± 18.5 | 46.0 ± 17.2 | 57.5 ± 21.2 | 0.036 |
| IV‐APEX | 87.0 ± 29.3 | 106.2 ± 30.5 | 85.9 ± 32.4 | 0.020 |
| LIV‐APEX | 119.1 ± 38.1 | 121.0 ± 39.9 | 115.4 ± 29.1 | 0.472 |
| Span NR (UIV‐IV) | 0.7 ± 0.4 | 0.5 ± 0.2 | 0.7 ± 0.4 | 0.047 |
| Span NR (UIV‐LIV) | 0.6 ± 0.5 | 0.5 ± 0.5 | 0.6 ± 0.6 | 0.511 |
In total, there were 61 complications in 32 patients, including four wound infections (in 4 patients), 21 rod breakages (in 13), one screw breakage (in one), eight screw pullout (in eight), six coronal imbalance (in six) and 21 PJK (in 21), respectively. It was worth noting that five of 21 (23.8%) PJK patients developed rod breakage, whereas only nine of 81 (11.1%) non‐PJK patients developed rod breakage or screw breakage. Among them, wound infection was cured by dressing changes daily and antibiotic treatment while implant‐related complications were treated in the next lengthening procedure. During the series of surgeries, no neurological deficits occurred.
Incidence, Classification, and Timing of PJK
Generally, PJK occurred in 21 patients (20.6%) during the follow up, including 18 patients of type 1, three patients of type 3 and no patients had PJK of type 2. Among them, six cases developed PJK immediately after the index surgery, 10 cases developed PJK after the first lengthening procedure while the remaining five cases developed PJK after the subsequent lengthening procedures. In addition, 15 cases of PJK remained stable while the other six continued to progress. Brace treatment would be recommended for those progressive PJK patients while those with stable PJK required close observation.
Comparisons between thePJKand theNon‐PJKGroups
Patients who developed PJK were significantly younger than the non‐PJK group (5.9 ± 2.3 vs. 7.1 ± 2.4 years, P = 0.042). The mean number of lengthening procedures was 5.0 ± 2.2 and 4.2 ± 1.6 (P = 0.033) in the PJK and non‐PJK groups, and the mean follow‐up was 4.8 ± 2.6 and 4.3 ± 1.7 years (P = 0.051), respectively. There was no difference in gender (9/12 vs. 41/40, p = 0.526), BMI (15.5 ± 3.2 vs. 16.2 ± 4.5 kg/m2, P = 0.641) and implant type (4/17 vs. 14/67, P = 0.849) between these two groups.
As shown in Table 3, the PJK group differed from the non‐PJK group with larger preoperative major Cobb angle (82.0 ± 21.2 vs. 75.6 ± 17.2°, P = 0.038) and greater correction rate (51.2 ± 12.8% vs. 44.4 ± 12.7%, P = 0.047). The average preoperative TK was 47.2 ± 15.2° in the PJK group and 42.6 ± 13.5° in the non‐PJK group (P = 0.179), but there was no difference observed postoperatively and at the final follow‐up visit. The LL and PI did not impact the occurrence of PJK.
The preoperative PJA was slightly higher in the PJK group than in the non‐PJK group although the differences were not statistically significant (6.7 ± 4.0 vs. 5.3 ± 2.6°, P = 0.056). However, the postoperative PJA (13.9 ± 9.0 vs. 5.5 ± 2.5°, P < 0.001) and the final PJA (20.2 ± 6.3 vs. 6.4 ± 3.2°, P < 0.001) were significantly higher in the PJK group. Patients with PJK also had a smaller number of UIV‐apex (3.2 ± 1.3 vs. 4.6 ± 1.6, P = 0.001) and smaller mean span NR from UIV‐apex to IV‐apex (0.6 ± 0.3 vs. 0.9 ± 0.7, P = 0.028) when compared with the non‐PJK group. Besides, the relative distance of UIV‐apex (PJK group, 46.0 ± 17.2 vs. non‐PJK group, 57.5 ± 21.2 mm, P = 0.036), the relative distance of IV‐apex (106.2 ± 30.5 vs. 85.9 ± 32.4 mm, P = 0.020) and span DR from UIV‐apex to IV‐apex (0.5 ± 0.2 vs. 0.7 ± 0.4, P = 0.047) were all significant different. No statistical difference in either the number of LIV‐apex or the distance of LIV‐apex was observed between the PJK group and the non‐PJK group. The mean span NR from UIV‐apex to LIV‐apex and the mean span DR from UIV‐apex to LIV‐apex were also similar in the two groups, respectively (Figs. 2, 3).
Fig. 2.
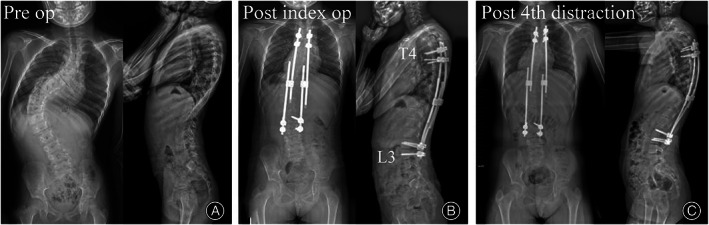
A 6‐year‐old girl with congenital scoliosis. (A) The preoperative PJA between T2 and T4 was 6°. (B) The apex located at T6 and IV at L1, respectively. The PJA increased to 11° while the span NR of UIV‐apex to IV‐apex was 0.3 and the span DR was 0.3. (C) The PJA increased to 20° after the 4th distraction, leading to PJK
Fig. 3.
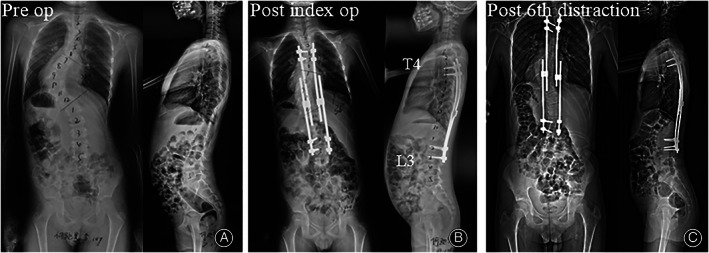
A 10‐year‐old boy with syndromic scoliosis (neurofibromatosis Type 1). (A) The preoperative PJA was 1°. (B) The apex located at T8 and IV at L1, respectively. PJA was 3° while the span NR of UIV‐apex to IV‐apex was 0.8 and the span DR was 0.8. (C) the PJA was stabilized at 4° after the 6th lengthening procedures, no PJK
Risk Factors forPJK
The possible candidates related to PJK were recruited from the univariate analysis, including age at the index surgery ≤ 7 years, the Cobb angle≥80°, the correction rate of Cobb Angle>50%, postoperative PJA > 10°, span NR from UIV‐apex to IV‐apex ≤ 0.6 and span DR from UIV‐apex to IV‐apex ≤ 0.6 (Table 4). After logistic regression analysis, age at the index surgery ≤ 7years, span NR from UIV‐apex to IV‐apex ≤ 0.6 and span DR from UIV‐apex to IV‐apex ≤ 0.6 were identified as independent risk factors in predicting the occurrence of PJK. (Table 4) Upon ROC curve analysis, a threshold for span NR from UIV‐apex to IV‐apex was identified between the groups with and without PJK. The results showed that span NR from UIV‐apex to IV‐apex was 0.6, the area under the curve was 0.668, the sensitivity was 0.36, and 1‐specificity was 0.09. Therefore, span NR from UIV‐apex to IV‐apex ≤ 0.6 can be regarded as a relatively good predictor (Fig. 4).
TABLE 4.
Multivariate analysis of PJK risk factors
| Parameters | B | SE | Wald | df | P | Exp (B) | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Age at index surgery ≤ 7 years | 0.037 | 0.016 | 5.486 | 1 | 0.019 | 1.038 | 1.019 | 1.17 |
| Cobb > 80° | 0.016 | 0.026 | 0.373 | 1 | 0.403 | 0.497 | 0.641 | 4.031 |
| TK > 40° | 0.003 | 0.034 | 0.008 | 1 | 0.930 | 1.003 | 0.519 | 2.956 |
| The span NR ≤ 0.6 | 3.952 | 1.801 | 4.816 | 1 | 0.028 | 52.05 | 1.668 | 16.625 |
| The span DR ≤ 0.6 | 1.557 | 0.760 | 4.200 | 1 | 0.040 | 4.211 | 1.239 | 18.309 |
Fig. 4.
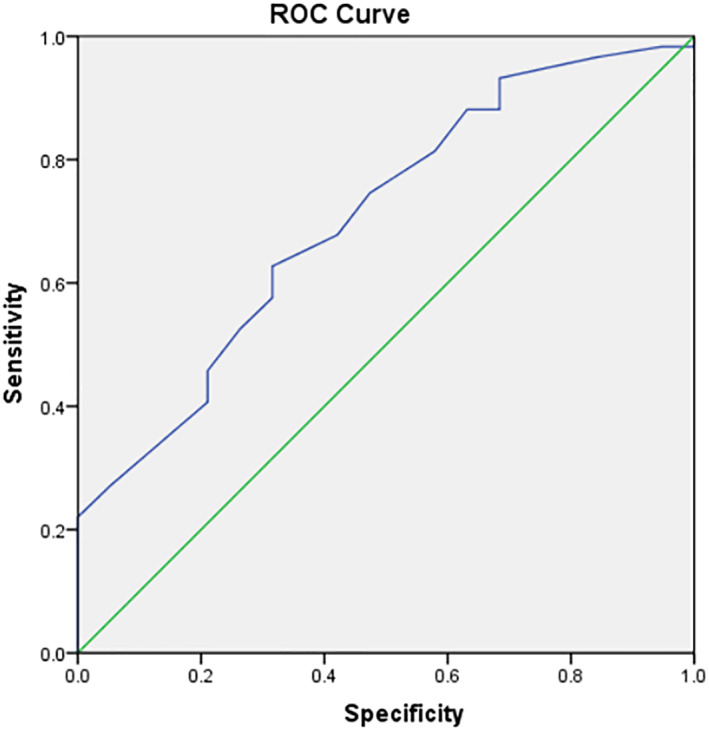
ROC curve analysis of the ratio of number of UIV‐apex to apex‐IV
Discussion
The current study retrospectively reviewed 102 patients with EOS who had undergone GRs treatment with a minimum 2‐year follow‐up. Our results showed that the incidence of PJK was 20.6%. In addition, patients undergoing GRs surgery with younger age and a closer location of UIV relative to the sagittal apex have a higher risk of PJK.
Incidence of PJK after GR Treatment
PJK is a common alignment‐related complication which should not be neglected. The incidence of PJK in EOS patients treated with GRs treatment ranges from 12% to 56%. Our study revealed the incidence of PJK was 20.6% with average 4.5 ± 2.6 years of follow‐up. The discrepancy in the incidence of PJK may be due to the different inclusion criteria, surgical strategies, and follow‐up time. Malick et al. reported that the incidence of PJK was only 4% in idiopathic scoliosis patients who were treated with a traditional growing rod after a mean follow‐up of 5 years. 18 Sun et al. showed that the incidence of PJK was 30.7% in congenital scoliosis patients. 19 Whereas, Jain et al. found the incidence of PJK to be as high as 37.5% in EOS patients with NF1 who were treated with GRs surgery. 20 In addition, this study demonstrated that PJK following GRs treatment in EOS patients mainly occurred during the first year after surgery (between the index surgery and the first distraction) and progressed in the subsequent lengthening procedures. A trend of gradual increase in PJA after repeated lengthening procedures was also reported by Shah's study on growing rod treatment. 21 Similarly, Li et al. analyzed 68 EOS patients treated with VEPTR and found four patients developed PJK, all of which occurred within the first year after VEPTR insertion and gradually progressed. 22 This is possibly due to the excessive forces in proximal junctional spine during the surgical correction to reduce localized kyphosis. As a type of local distraction surgery, the subsequent lengthening surgery tends to aggravate the kyphosis of the proximal junctional area, ultimately leading to the occurrence of PJK.
Severe PJK may cause vertebra collapse, acute subluxation or implant failure around the upper instrumented vertebra, leading to post‐operative deformity, pain, and dissatisfaction. Yagi et al. reported 32 AIS patients undergoing long instrumented spinal fusion developed PJK, of which six patients were symptomatic and four patients underwent revision surgery due to local pain. 17 Results of our study revealed that the proportion of rod or screw breakage in the PJK group was higher than that in the non‐PJK group, indicating that PJK potentially increased the incidence of implant‐related complications. Thus, it is important to pay attention to the risk factors and preventative strategies for postoperative PJK.
Risk Factors of PJK after GR Treatment
In previous studies, some authors investigated the location of UIV or LIV to assess the effect on postoperative PJK. 12 , 23 But none of these studies focused on the relative position of the anchor point and the apex in the sagittal plane. Therefore, we tried to investigated the sagittal spinal profile by the ratio between UIV‐apex and LIV‐apex. However, no significant differences were detected in the ratio of distance from UIV‐apex to LIV‐apex between the PJK group and the non‐PJK group. According to our clinical experience, the LIV is often determined at the coronal stable vertebra while PJK manifests as a sagittal plane complication. At the same time, IV acts as an important parameter to classify the normal sagittal shapes of spinopelvic organization, since it represents the actual location where the kyphotic curve turns in the lordotic curve. 24 In previous studies, some authors investigated the apices of the sagittal curvature to assess the sagittal morphological shape of the spine. 25 , 26 , 27 , 28 Jakinapally et al. 25 reported that the IV is significantly cranial and posterior in the PJK group in adult spinal deformity. Investigation of the location of UIV, apex and IV is a simple method of evaluating the spinal curvature. Considering the sagittal geometrical shape of the spine to decrease junctional stress and PJK is important. Thus, we use IV instead of LIV to analyze the sagittal plane. Our results demonstrated that the ratio of number and distance from UIV‐apex to IV‐apex in PJK group were significantly lower when compared to the non‐PJK group. This find can be easily explained by biomechanics. When the location of the UIV is very close to the apex, the proximal junctional stress is significantly greater than that at the distal junctional, leading to the occurrence of PJK subsequently. There are also some studies on the relationship between the PJK and the location of UIV and LIV.
Through ROC curve analysis and univariate regression analysis, we further found that the span NR from UIV‐apex to IV‐apex ≤ 0.6 and the span DR from UIV‐apex to IV‐apex ≤ 0.6 are significant independent risk factors for PJK. In clinical application, it is more convenient and intuitive to choose span NR from UIV‐apex to IV‐apex as the evaluation parameter. This finding suggests that the selection of UIV should be made with reference to the position of apex and IV. Besides, surgeons are suggested to pay attention to the protection of paraspinal musculature and facet joints, avoiding destroying the integrity and stability of the posterior structures of the spine.
The present study also identified that age at the index surgery ≤ 7 years is an independent risk factor of PJK. In literature, much controversy remains regarding the relationship between age and PJK. A multicenter study conducted by Upasani et al. revealed that earlier age at implantation increased the probability of PJK. 29 Bess et al. identified younger age as a risk factor for PJK. 30 In contrast, Akbarnia et al. and El‐Hawary et al found no such association. 31 , 32 Several theories may explain our finding. Generally, very younger children have poorer soft tissue and lower bone quality than older children. It is also possible that children receiving an index surgery at a younger age will likely accept more lengthening procedures than those older patients.
Clinical Relevance
The clinical significance of this study is to emphasize the importance of the location of UIV relative to the sagittal apex in preventing the occurrence of postoperative PJK. When choosing the location of UIV, we need to consider not only the need of correction of coronal deformity, but also the location relationship between UIV and apex. Sagittal plane also has important reference significance for the selection of UIV. 25 , 33 Admittedly, it is not possible for every EOS patient to have an UIV as high as T2 or above because minimizing the interference of GR surgery to the non‐deformity area is essential. Therefore, this study provides a relatively individualized UIV selection scheme.
Limitations The selection of the appropriate location of UIV based on apex and IV will help to reduce the risk for the development of PJK in EOS patients treated with GR. However, there were some limitations in this study. First, it is a retrospective cohort analysis, and the etiology of the case is complex. Second, a much larger study population is required while most of the cases had not yet “graduated” for GRs treatment at the last follow up. Third, most of the patients were too young to fill out questionnaires independently; therefore, we cannot accurately assess the clinical outcomes.
Conclusions
In conclusion, among EOS patients who received growing rod treatment, the prevalence of PJK was 20.6%. Besides younger age, a closer location of UIV relative to the sagittal apex is identified to be an independent risk factor of postoperative PJK. Selection of UIV at a relatively farther location away from the sagittal apex might help prevent occurrence of PJK. Future prospective research is needed to verify findings of the current study.
Authors’ Contributions
Bo Yang and Liang Xu reviewed radiographs. Bo Yang performed statistical analysis and drafted the manuscript. Zhuang Qian, Bin Wang and Zezhang Zhu gave administrative and intellectual support. Xu Sun and Yong Qiu conceived the study, finalized the manuscript and is responsible. All authors read and approved the final manuscript.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant No. 81772422) and the Natural Science Foundation of Jiangsu Province (BE2017606). We would like to thank all participating patients.
References
- 1. Hardesty C, Huang R, El‐Hawary R, Samdani A, Hermida P, Bas T, et al. Early‐onset scoliosis: updated treatment techniques and results. Spine Deform. 2018;6(4):467–72. [DOI] [PubMed] [Google Scholar]
- 2. Karol LJ. The natural history of early‐onset scoliosis. JBJS. 2019;39:S38–43. [DOI] [PubMed] [Google Scholar]
- 3. Yang S, Andras LM, Redding GJ, Skaggs DL. Early‐onset scoliosis: a review of history, current treatment, and future directions. Pediatrics. 2016;137. [DOI] [PubMed] [Google Scholar]
- 4. Bouthors C, Dukan R, Glorion C, Miladi LJ, Jon S. Outcomes of growing rods in a series of early‐onset scoliosis patients with neurofibromatosis type. J Neurosurg: Spine. 2020;1:1–8. [DOI] [PubMed] [Google Scholar]
- 5. Bekmez S, Dede O, Yazici MJ. Advances in growing rods treatment for early onset scoliosis. Curr Opin Pediatr. 2017;29(1):87–93. [DOI] [PubMed] [Google Scholar]
- 6. Zhang YB, Zhang JGJ. Treatment of early‐onset scoliosis: techniques, indications, and complications. Chin Med J. 2020;133(03):351–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Latalski M, Fatyga M, Sowa I, Wojciak M, Starobrat G, Danielewicz A. Complications in growth‐friendly spinal surgeries for early‐onset scoliosis: literature review. World J Orthop. 2021;12(8):584–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Matsumoto H, Fields M, Roye B, Roye D, Skaggs D, Akbarnia B, et al. Complications in the treatment of EOS: is there a difference between rib vs spine‐based proximal anchors? Spine Deform. 2021;9(1):247–53. [DOI] [PubMed] [Google Scholar]
- 9. Zarei M, Tavakoli M, Ghadimi E, Moharrami A, Nili A, Vafaei A, et al. Complications of dual growing rod with all‐pedicle screw instrumentation in the treatment of early‐onset scoliosis. J Orthop Surg Res. 2021;16(1):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yagi M, Rahm M, Gaines R, Maziad A, Ross T, Kim HJ, et al. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine. 2014;39(10):E607–14. [DOI] [PubMed] [Google Scholar]
- 11. Carender CN, Morris WZ, Poe‐Kochert C, Thompson GH, Liu RW. Low pelvic incidence is associated with proximal junctional kyphosis in patients treated with growing rods. Spine. 2015;41(9):1–797. [DOI] [PubMed] [Google Scholar]
- 12. Pan A, Hai Y, Yang J, Zhang Y, Zhang Y. Upper instrumented vertebrae distal to T2 leads to a higher incidence of proximal junctional kyphosis during growing‐rod treatment for early onset scoliosis. Clin Spine Surg. 2018;31:E337–41. [DOI] [PubMed] [Google Scholar]
- 13. Chen Z, Qiu Y, Zhu Z, Li S, Sun X. How does Hyperkyphotic early‐onset scoliosis respond to growing rod treatment?. J Pediatr Orthop. 2017;37(8):e593–98. [DOI] [PubMed] [Google Scholar]
- 14. Pizones J, Martín‐Buitrago MP, Sánchez Márquez JM, Fernández‐Baíllo N, Baldan‐Martin M, Sánchez Pérez‐Grueso FJ. Decision making of graduation in patients with early‐onset scoliosis atthe end of distraction‐based programs: risks and benefits of definitive fusion. Spine Deform. 2018;6(3):308–13. [DOI] [PubMed] [Google Scholar]
- 15. Murphy RF, Barfield WR, Emans JB, Akbarnia B, Thompson G, Sponseller P, et al. Minimum 5‐year follow‐up on graduates of growing spine surgery for early onset scoliosis. J Pediatr Orthop. 2020;40:e942–6. [DOI] [PubMed] [Google Scholar]
- 16. Xu L, Sun X, Du C, Zhou Q, Shi B, Zhu Z, et al. Is growth‐friendly surgical treatment superior to one‐stage posterior spinal fusion in 9‐ to 11‐year‐old children with congenital scoliosis? Clin Orthop Relat Res. 2020;478(10):2375–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yagi M. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine. 2011;36:E60–8. [DOI] [PubMed] [Google Scholar]
- 18. Malick B, Anna MC, Pawelek JB, Ron EH, Thompson GH, Smith JT, et al. Idiopathic early‐onset scoliosis: growing rods versus vertically expandable prosthetic titanium ribs at 5‐year follow‐up. J Pediatr Orthop. 2020;40(3):142–8. [DOI] [PubMed] [Google Scholar]
- 19. Sun X, Xu L, Chen Z, Chen X, Liu Z, Yu Y, et al. Comparison of hybrid and traditional growing rod techniques in the treatment of early‐onset congenital scoliosis. Chin J Surg. 2019;57(5):342–7. [DOI] [PubMed] [Google Scholar]
- 20. Jain V, Berry C, Crawford A, Emans J, Sponseller P. Growing rods are an effective Fusionless method of controlling early‐onset scoliosis associated with Neurofibromatosis type 1 (NF1): a multicenter retrospective case series. J Pediatr Orthop. 2017;37(8):e612–8. [DOI] [PubMed] [Google Scholar]
- 21. Shah SA, Karatas AF, Dhawale AA, Dede O, Mundis GM, Holmes L, et al. The effect of serial growing rod lengthening on the sagittal profile and pelvic parameters in early‐onset scoliosis. Spine. 2014;39(22):E1311–7. [DOI] [PubMed] [Google Scholar]
- 22. Li Y, Gold M, Karlin L. Proximal junctional kyphosis after vertical expandable prosthetic titanium rib insertion. Spine Deform. 2013;1(6):425–33. [DOI] [PubMed] [Google Scholar]
- 23. Watanabe K, Uno K, Suzuki T, Kawakami N, Tsuji T, Yanagida H, et al. Risk factors for proximal junctional kyphosis associated with dual‐rod growing‐rod surgery for early‐onset scoliosis. Clin Spine Surg. 2016;29:E428–33. [DOI] [PubMed] [Google Scholar]
- 24. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):1558–353. [DOI] [PubMed] [Google Scholar]
- 25. Jakinapally S, Yamato Y, Hasegawa T, Togawa D, Yoshida G, Banno T, et al. Effect of sagittal shape on proximal junctional kyphosis following thoracopelvic corrective fusion for adult spinal deformity: postoperative inflection vertebra cranial to T12 is a significant risk factor. Spine Deform. 2020;8(6):1313–23. [DOI] [PubMed] [Google Scholar]
- 26. Bernhardt M, Bridwell KJS. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14(7):717–21. [DOI] [PubMed] [Google Scholar]
- 27. Lowe TG, Spine MKJ. An analysis of sagittal curves and balance after Cotrel‐Dubousset instrumentation for kyphosis secondary to Scheuermann's disease: a review of 32 patients. Spine. 1994;19(15):1680–5. [DOI] [PubMed] [Google Scholar]
- 28. Kobayashi T, Atsuta Y, Matsuno T, Takeda NJS. A longitudinal study of congruent sagittal spinal alignment in an adult cohort. Spine. 2004;29(6):671–6. [DOI] [PubMed] [Google Scholar]
- 29. Upasani VV, Parvaresh KC, Pawelek JB, Miller PE, Thompson GH, Skaggs DL, et al. Age at initiation and deformity magnitude influence complication rates of surgical treatment with traditional growing rods in early‐onset scoliosis. Spine Deform. 2016;4(5):344–50. [DOI] [PubMed] [Google Scholar]
- 30. Bess S, Akbarnia BA, Thompson GH, Sponseller PD, Shah SA, Sebaie HE, et al. Complications of growing‐rod treatment for early‐onset scoliosis: analysis of one hundred and forty patients. JBJS. 2010;92(15):2533–43. [DOI] [PubMed] [Google Scholar]
- 31. Akbarnia BA, Emans JB. Complications of growth‐sparing surgery in early onset scoliosis. Spine. 2010;35(25):2193–204. [DOI] [PubMed] [Google Scholar]
- 32. El‐Hawary R, Sturm P, Cahill P, Samdani A, Smith JT. What is the risk of developing proximal junctional kyphosis during growth friendly treatments for early‐onset scoliosis? J Pediatr Orthop. 2015;37(2):86–91. [DOI] [PubMed] [Google Scholar]
- 33. Gomez J, Kubat O, Tovar Castro M, Hanstein R, Flynn T, Lafage V, et al. The effect of spinopelvic parameters on the development of proximal junctional kyphosis in early onset: mean 45‐year follow‐up. J Pediatr Orthop. 2020;40(6):261–6. [DOI] [PubMed] [Google Scholar]


