Abstract
We present a case of vertebral osteomyelitis following multiple vertebral augmentations in a patient with an insidious presentation. Vertebral augmentation (kyphoplasty and/or vertebroplasty) is a minimally invasive procedure that has become a fairly common and highly effective method in treating compression fractures. A large majority of patients that undergo this procedure suffer from osteoporosis. Numerous studies have shown that patients who undergo the procedure obtain substantial pain relief and improve functional status, often times to a greater extent than other surgical and nonsurgical management. Although its prevalence is low, infection after vertebral augmentation can be a serious consequence of the procedure. Blood cultures in this case were positive for Clostridium septicum. C septicum is a gram-positive, spore forming bacteria that is part of the normal gut flora in humans and is commonly associated with GI malignancy, necrosis, and inflammation. The patient did not respond to long-term intravenous antibiotics and required vertebral corpectomy and debridement with instrumentation. Vertebral body cultures obtained intraoperatively were positive for C septicum. It was noted historically that the patient had a hemorrhoidectomy 4 weeks prior to her initial fracture presentation. Although the risk of infection after vertebral augmentation is low, it is imperative that careful pre- and postoperative evaluation as well as follow-up is completed in order to prevent catastrophic consequences for patients. In patients with recent gastrointestinal tract manipulation/surgery, appropriate antibiotic prophylaxis should be considered prior to vertebral augmentation procedures.
Keywords: Case report, Clostridium septicum, Vertebroplasty, Vertebral augmentation, Osteomyelitis
Introduction
In the United States, a growing elderly population has resulted in an increasing demand for the care of osteoporotic injuries, specifically vertebral compression factures [1]. Many current pharmaceutical, medical, and surgical methods of treatment have been shown to provide only minimal and transient pain relief. They have also proven to be slow and costly, and they come with significant health risks for the elderly patient. Vertebral augmentation (kyphoplasty and/or vertebroplasty) is a minimally invasive procedure that has become a fairly common and highly effective method in treating compression fractures. Numerous studies have shown that patients who undergo the procedure obtain substantial pain relief and improve functional status, often times to a greater extent than other surgical and nonsurgical management [2,3]. Furthermore, it has been reported that vertebral augmentation procedures are more cost-effective than traditional conservative therapy for those with osteoporotic vertebral fractures at 1 week, 3 months, and 12 months [4]. Postvertebral augmentation complications are rare and mostly due to leakage of PMMA cement or allergic reactions to cement [5].
Infection after vertebral augmentation can be a serious consequence of the procedure, however the prevalence is low. Nevertheless, the incidence of infection may rise as the procedure becomes increasingly integrated into healthcare. We report here of a patient who presented insidiously with no signs of infection prior to her initial procedure and 27 days after. She only had positive blood cultures (Day 27) for Clostridium septicum after her third vertebral augmentation (vertebroplasty on Day 16).
Patient case presentation
An 81-year-old Caucasian female with a past medical history of chronic rheumatoid arthritis, coronary artery disease, essential hypertension, atrial fibrillation and chronic obstructive pulmonary disease presented to the hospital through the ER (Day 1) with acute onset of sharp lower back pain one day following being transferred from her nursing home bed. The patient had taken tramadol with no relief in her pain. She denied any fevers, chills, nausea, vomiting, weight loss, malaise, bowel, or bladder problems. The patient denied any recent falls, radiculopathy, or previous back injuries. The patient did not have any family history or personal history of osteoporosis. In addition, she never had a DEXA scan or any evidence of osteopenia on her initial plain films. It is notable that a month prior to her presentation, she had hemorrhoidectomy with no postoperative complications and remained in stable health up to her presentation in the ER.
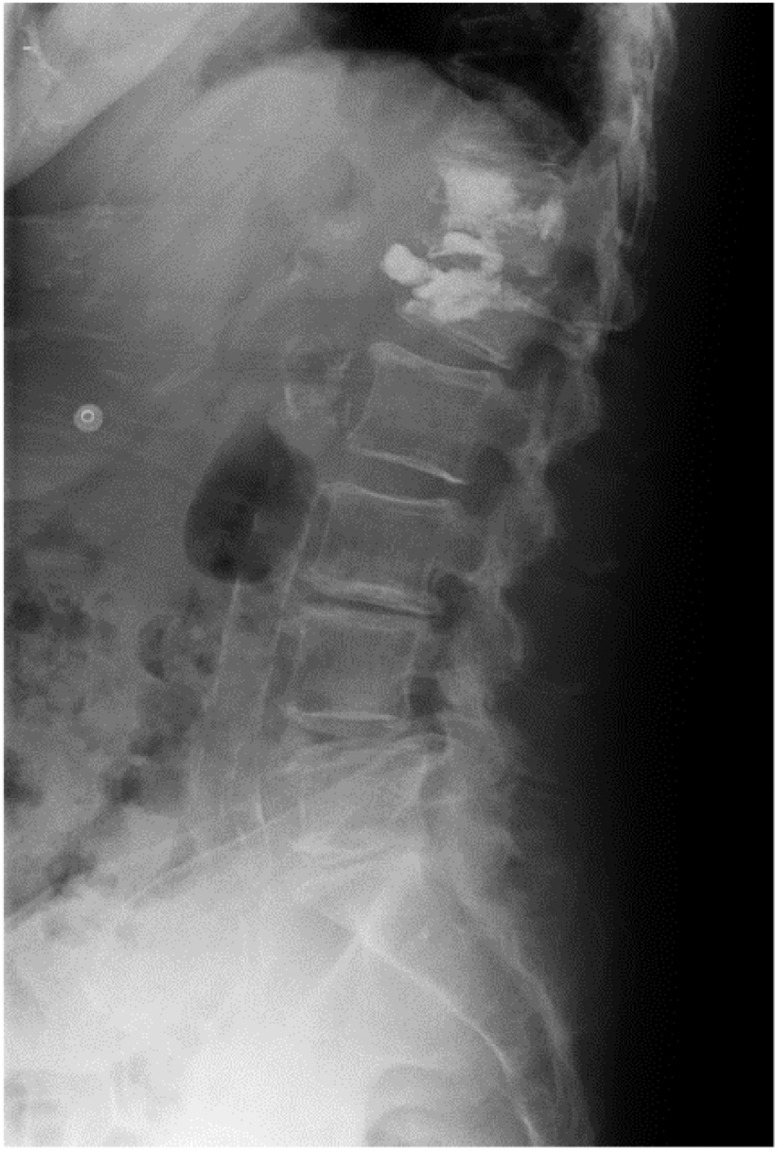
Plain films of the spine were obtained initially (Day 1) and revealed no evidence of osteolysis or endplate destruction, but mild thoracic and lumbar spondylosis was noted. MRI on the following day (Day 2) showed an acute compression fracture of L1 vertebral body with approximately 20% height loss at the superior endplate and an acute injury to the T12 vertebral body without evidence for height loss (Fig. 1). Interventional radiology was consulted for vertebral augmentation. Physical examination during this initial presentation revealed a BMI of 28.4, blood pressure of 138/76, pulse of 111, and temperature of 98.1°F. Neurological exam did not reveal any focal deficits. Laboratory evaluation showed a sodium level of 125, potassium level of 5.5, hemoglobin of 9.3, and white blood cell count (WBC) of 11.8.
Fig. 1.

T2-weighted sagittal image of the lumbar spine (Day 2) prior to vertebroplasty demonstrates a vertebral body compression fracture of superior endplate of L1 with mild height loss. There is hyperintense signal below the superior endplate within the vertebral body likely indicating a fluid-filled cleft.
The patient then underwent percutaneous kyphoplasty of L1 vertebral body (Day 3) with cavity creation using the Parallax Contour Vertebral Augmentation Device (Arthrocare, Austin, TX) under fluoroscopic guidance. Cortoss (Orthovita, Malvern, PA) cement (2 cc) was then inserted into the cavity and into the vertebral body. The patient continued to have back pain following the procedure. A second MRI performed 5 days after kyphoplasty (Day 7) revealed persistent compressive deformity of L1, now status postvertebroplasty and worsened medullary edema at T12, representing a worsening of the known fracture of T12. Subsequently, the patient underwent T12 vertebroplasty 2 days after the second MRI (Day 9), and a total of 4 cc of polymethylmethacrylate (PMMA) (Carefusion, San Diego, CA) was infused into the T12 vertebral body. The patient was then discharged 2 days later (Day 11). Of note, the patient received 1g of Ancef intravenously 30 minutes prior to both vertebral augmentation procedures.
She was readmitted 4 days later (Day 15) with intractable lower back pain, which had been getting progressively worse. A repeat MRI revealed interval worsening of edema of L1 vertebral body and increased retropulsion at T12-L1. There was severe disc edema with severe left posterior paracentral disc protrusion. There was no evidence of extra-axial collection and the protrusion was believed to be due to postvertebral augmentation related change given her normal WBC count and being afebrile. She underwent a redo L1 vertebroplasty the next day (Day 16) with successful injection of 4 cc of Cortoss cement to the inferior portion of the L1 vertebral body. The next day (Day 17) following the vertebroplasty, her pain was improved and she was able to ambulate with less pain. Her white blood cell count remained normal and in fact was decreasing throughout the hospitalization (WBC declined from 10.2 to 5.3). She was discharged the next day (Day 18). The patient received 1g of Ancef intravenously 30 minutes prior to the 3rd vertebral augmentation procedure as per our protocol.
The patient went to her primary care physician for follow-up 4 days later (Day 22) and complained of persistent pain. She was then placed on a Fentanyl patch. The patient was readmitted 2 days later (Day 24) with hallucinations that were initially attributed to her new Fentanyl patch versus digoxin toxicity. The patient was complaining of chest pain with palpitations, shortness of breath, lightheadedness, abdominal discomfort with an episode of vomiting, and continued severe back pain. Vitals revealed a temperature of 97.5°F, BP and pulse were normal and her WBC was normal at 7.1. ESR was elevated to 70 mm/hr (nl 0-29 mm/hr).
As part of the workup for her change of mental status 2 sets of blood cultures were drawn 2 days later (Day 26). The blood cultures returned positive the next day (Day 27) for gram-positive rods in 2 of 2 cultures and she was empirically treated with IV Vancomycin and Ampicillin/Sulbactam. Antibiotic sensitivity was not performed since this was the routine for anaerobic cultures. Neurosurgery and Infectious Disease consultations were obtained as she continued to have back pain. Incidentally, the patient denied having fevers but did report having chills to the infectious disease consultant. MRI and plain film radiograph images on Day 27 revealed frank osteomyelitis of T12 and L1 (Figs. 2-5). Her temperature maximum reached 99.1 F by Day 28. Her sodium decreased to 123 and required treatment to correct it.
Fig. 3.
Postvertebroplasty lateral plain film radiograph of the lumbar spine (Day 26). Note the loss of disc space at T12-L1.
Fig. 4.

Postvertebroplasty sagittal T1-weighted fat-saturated MRI with gadolinium contrast of the lumbar spine (Day 27). Note is made of the extensive enhancement of T12 and L1 vertebral bodies. There is also enhancing epidural extension anteriorally and posteriorally at that level. The posterior epidural extension is demarcated by the blue arrow.
Fig. 2.
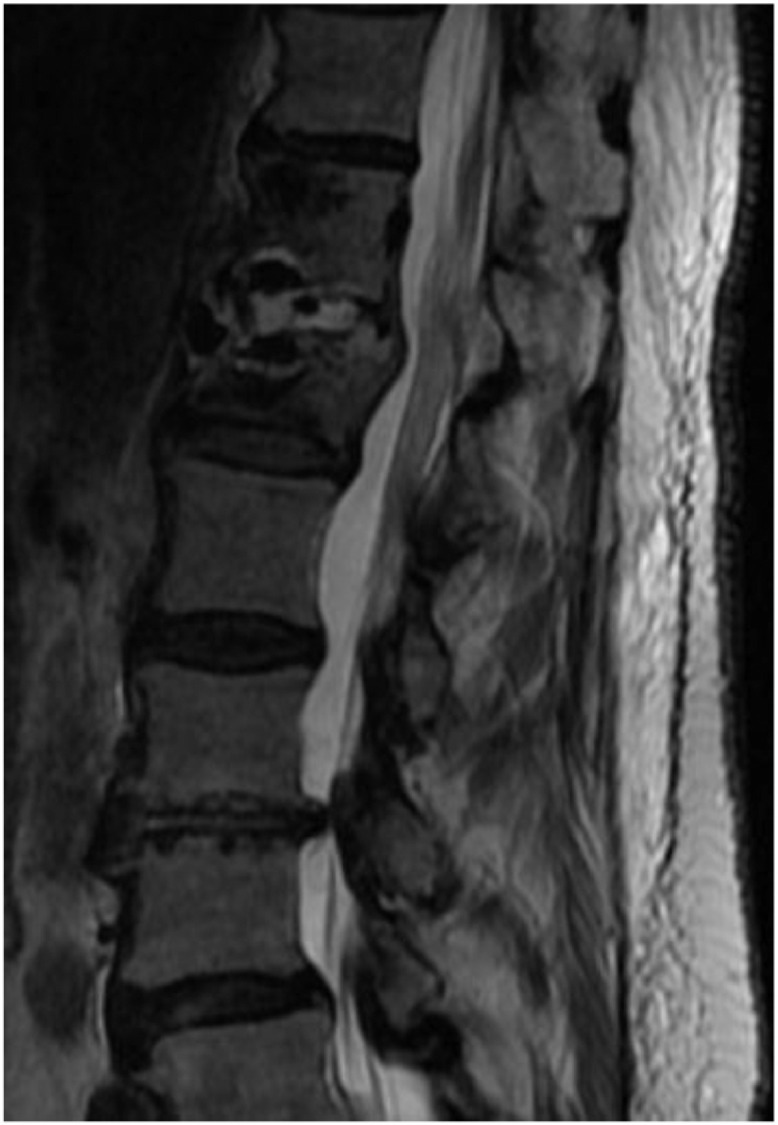
T2-weighted sagittal image of the lumbar spine (Day 27) postvertebroplasty of T12 (Day 9) and L1 (Day 3 & 16) demonstrates irregularity of the endplates of T12 and L1 with further height loss of L1 and obvious fluid within the T12-L1 disk space. STIR and T1-weighted images also demonstrate intense edema within these vertebral bodies.
Fig. 5.
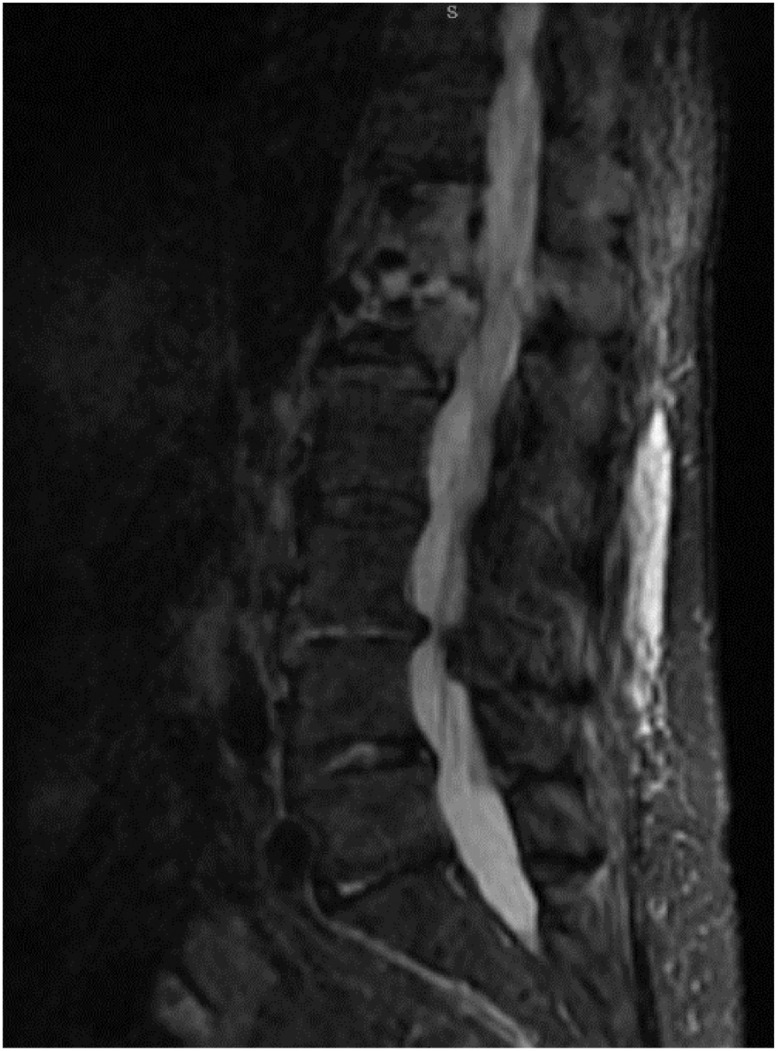
Postvertebroplasty sagittal STIR MRI (Day 27). Note is made of the extensive marrow edema within T12 and L1, as well as disc fluid with irregular endplates of T12 and L1.
The organism on blood culture was identified as C septicum. A diagnosis of osteomyelitis and spinal discitis with C septicum bacteremia was therefore made. The patient was continued on intravenous Ampicillin/Sulbactam at the recommendation of infectious disease consult. The patient then underwent mini-open decompression laminectomy of T12-L1, debridement, interbody stabilization, and reconstruction of T12-L1 vertebrae with removal of spinal discitis and osteomyelitis on Day 40. Surgical pathology revealed necrotic tissue with acute and chronic inflammation, acute osteomyelitis, and granulation tissue formation. Intraoperative culture of osteomyelitic bone was positive for C septicum.
Discussion
C septicum is a gram-positive, spore forming bacteria that is part of the normal gut flora in humans and is commonly associated with gastrointestinal malignancy, necrosis, and inflammation [6]. Its motility and anaerobic nature allow it to live off a variety of substances and be very adaptable to different environmental conditions. These qualities also increase the risk of infection in regions of decreased blood flow.
However, C septicum infections are rare, and mostly found in people with a history of trauma, surgery, skin infections, burns, peripheral vascular disease, diabetes, and colon cancer [7]. One if its unique properties is its ability to infect fresh or recent operative sites. In particular, its isolated alpha toxin has been shown to cause intravascular hemolysis as well as tissue necrosis, and has been identified to be its primary virulent factor [8].
Vertebral osteomyelitis is a rare complication of vertebral augmentation that is associated with significant morbidity and mortality. Recent surgery or infection serves as 2 of the main predisposing factors. Immunocompromised states such as prolonged steroid use or diabetes mellitus may also increase the risk of osteomyelitis. Although Staphylococcus Aureus has been noted to be by far the most common source of osteomyelitis, many organisms are capable of causing the condition [9,10]. Osteomyelitis/discitis following kyphoplasty has been described in multiple reports [5], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20]. Although infections involving vertebral augmentations are rare, preoperative antibiotics should be the gold standard. Typical agents to cover Staphylococcus Aureus and C septicum simultaneously include: ampicillin-sulbactam, cefazolin, cefoxitin, clindamycin, gentamicin, metronidazole, or piperacillin-tazobactam [21].
In this instance, this patient may have been predisposed to an infection with C septicum due to her recent hemorrhoidectomy. Even though this patient presented 4 weeks after her surgical procedure, it is possible that her mucosal integrity was compromised and she was intermittently seeding her blood stream. In addition, the initial imaging could have indicated osteomyelitis with pathological collapse and vertebral discitis due to there being no traumatic injury, no history of osteoporosis, and the presence of fluid within the T12-L1 disk space most likely associated with bone marrow edema within the T12 vertebral body. The presence of edema seen with postvertebroplasty MRI could also suggest that there was potential for bacterial seeding due to postvertebral augmentation.
Once C septicum has established itself in a site of infection, the course may be insidious. This would be especially true in a vertebral body with potentially limited pain sensation due to structural alteration with PMMA. Additionally, it is possible that this patient's atypical presentation with regards to a lack of an immune response (lack of elevated WBC's or fever) was due to her advanced age and underlying medical comorbidities. A high clinical suspicion for infection must therefore be given for early or borderline MRI findings in this setting such as disc edema and epidural/paravertebral inflammatory change. Although disc fluid can be seen normally postprocedure, the threshold for fluoroscopically guided culture and bone biopsy should be low.
PMMA is a bioactive silicated ceramic material used in a large portion of vertebroplasties for stable bone augmentation. Unfortunately, the presence of PMMA as a foreign body may possibly prevent the clearance of infection even with prolonged appropriate intravenous antibiotic treatment. In this situation, the only curative treatment remains surgical corpectomy and debridement.
Although the risk of infection after vertebral augmentation is low, it is imperative that careful pre- and postoperative evaluation as well as follow up are completed in order to prevent catastrophic consequences for the patient. It has been found that penicillin, tetracycline, and clindamycin are suitable antibiotics in the treatment of C. septicum [22]. Thus, we propose that patients with recent gastrointestinal tract manipulation should have antibiotic prophylaxis to cover C septicum prior to vertebral augmentation procedures.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Mubin I. Syed, Matthew Kurian, Omar Khan, Allen Guehl, Nicholas Pavlatos, Feras Deek, and Azim Shaikh. The first draft of the manuscript was written by Mubin I. Syed, Matthew Kurian, Omar Khan, Allen Guehl, Nicholas Pavlatos, Feras Deek, and Azim Shaikh and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Availability of data and material/code availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. Any additional materials can be requested by contacting the corresponding author.
Ethics approval
No ethical approval was required for this manuscript, as it does not meet the requirements of human subjects research as defined in 45 CFR Part 46.
Patient consent
All patients included in this reported gave written consent for the publication of their cases.
Author consent for publication
All authors consent to the publication of this manuscript and to the release of identifiable information associated with the submission.
Footnotes
Competing Interests: The authors have no relevant competing interests or conflicts of interest to disclose.
Funding: The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
References
- 1.Riggs B.L., Melton L.J., 3rd The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone. 1995;17(5 Suppl) doi: 10.1016/8756-3282(95)00258-4. 505s–511s. [DOI] [PubMed] [Google Scholar]
- 2.Papanastassiou I.D., et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J. 2012;21(9):1826–1843. doi: 10.1007/s00586-012-2314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans A.J., et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty retrospective report of 245 cases. Radiology. 2003;226(2):366–372. doi: 10.1148/radiol.2262010906. [DOI] [PubMed] [Google Scholar]
- 4.Masala S., et al. Cost-effectiveness of percutaneous vertebroplasty in osteoporotic vertebral fractures. Eur Spine J. 2008;17(9):1242–1250. doi: 10.1007/s00586-008-0708-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nussbaum D.A., Gailloud P., Murphy K. A review of complications associated with vertebroplasty and kyphoplasty as reported to the Food and Drug Administration medical device related web site. J Vasc Interv Radiol. 2004;15(11):1185–1192. doi: 10.1097/01.RVI.0000144757.14780.E0. [DOI] [PubMed] [Google Scholar]
- 6.Chew S.S.B., Lubowski D.Z. Clostridium septicum and malignancy. ANZ Journal of Surgery. 2001;71(11):647–649. doi: 10.1046/j.1445-1433.2001.02231.x. [DOI] [PubMed] [Google Scholar]
- 7.Smith-Slatas C.L., Bourque M., Salazar J.C. Clostridium septicum infections in children: a case report and review of the literature. Pediatrics. 2006;117(4):e796–e805. doi: 10.1542/peds.2005-1074. [DOI] [PubMed] [Google Scholar]
- 8.Hickey M.J., et al. Molecular and cellular basis of microvascular perfusion deficits induced by Clostridium perfringens and Clostridium septicum. PLoS Pathog. 2008;4(4) doi: 10.1371/journal.ppat.1000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sapico F.L., Montgomerie J.Z. Vertebral osteomyelitis. Infect Dis Clin North Am. 1990;4(3):539–550. [PubMed] [Google Scholar]
- 10.Kumar A., Sandoe J., Kumar N. Three cases of vertebral osteomyelitis caused by Streptococcus dysgalactiae subsp. equisimilis. J Med Microbiol. 2005;54(Pt 11):1103–1105. doi: 10.1099/jmm.0.46061-0. [DOI] [PubMed] [Google Scholar]
- 11.Syed M.I., et al. Vertebral osteomyelitis following vertebroplasty: is acne a potential contraindication and are prophylactic antibiotics mandatory prior to vertebroplasty? Pain Physician. 2009;12(4):E285–E290. [PubMed] [Google Scholar]
- 12.Buttermann G.R., Mullin W.J. Percutaneous vertebral body cement augmentation for back pain related to occult osteomyelitis/diskitis. Orthopedics. 2011;34(11):e788–e792. doi: 10.3928/01477447-20110922-31. [DOI] [PubMed] [Google Scholar]
- 13.Söyüncü Y., et al. Posterior spinal epidural abscess: an unusual complication of vertebroplasty. Joint Bone Spine. 2006;73(6):753–755. doi: 10.1016/j.jbspin.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Mummaneni P.V., et al. Infected vertebroplasty requiring 360 degrees spinal reconstruction: long-term follow-up review. Report of two cases. J Neurosurg Spine. 2006;5(1):86–89. doi: 10.3171/spi.2006.5.1.86. [DOI] [PubMed] [Google Scholar]
- 15.Alfonso Olmos M., et al. Infected vertebroplasty due to uncommon bacteria solved surgically: a rare and threatening life complication of a common procedure: report of a case and a review of the literature. Spine (Phila Pa 1976) 2006;31(20):E770–E773. doi: 10.1097/01.brs.0000240202.91336.99. [DOI] [PubMed] [Google Scholar]
- 16.Yu S.W., et al. Serious pyogenic spondylitis following vertebroplasty–a case report. Spine (Phila Pa 1976) 2004;29(10):E209–E211. doi: 10.1097/00007632-200405150-00023. [DOI] [PubMed] [Google Scholar]
- 17.Lin W.C., et al. Unusual presentation of infected vertebroplasty with delayed cement dislodgment in an immunocompromised patient: case report and review of literature. Cardiovasc Intervent Radiol. 2008;31(Suppl 2):S231–S235. doi: 10.1007/s00270-007-9234-z. [DOI] [PubMed] [Google Scholar]
- 18.Vats H.S., McKiernan F.E. Infected vertebroplasty: case report and review of literature. Spine (Phila Pa 1976) 2006;31(22):E859–E862. doi: 10.1097/01.brs.0000240665.56414.88. [DOI] [PubMed] [Google Scholar]
- 19.Walker D.H., Mummaneni P., Rodts G.E., Jr. Infected vertebroplasty. Report of two cases and review of the literature. Neurosurg Focus. 2004;17(6):E6. doi: 10.3171/foc.2004.17.6.6. [DOI] [PubMed] [Google Scholar]
- 20.Schmid K.E., et al. Spondylitis following vertebroplasty: a case report. Eur Spine J. 2005;14(9):895–899. doi: 10.1007/s00586-005-0905-7. [DOI] [PubMed] [Google Scholar]
- 21.Bratzler D.W., et al. Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery. Surgical Infections. 2013;14(1):73–156. doi: 10.1089/sur.2013.9999. [DOI] [PubMed] [Google Scholar]
- 22.Aldape M.J., et al. Comparative efficacy of antibiotics in treating experimental Clostridium septicum infection. Int J Antimicrob Agents. 2018;52(4):469–473. doi: 10.1016/j.ijantimicag.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]


