Abstract
Spontaneous intracranial hypotension (SIH) is a rare condition where the CSF pressure is lower than expected. In this report, we introduce a case of SIH in a 32-year-old pregnant woman who came to our emergency department at 32 weeks’ gestation with a postural and bilateral headache. After MRI confirmation, conservative treatment was started for her, and a cesarean section was scheduled. After the operation, CT-myelography and CT-cisternography were performed for the patient to find the source of the CSF leak, which was located in the C3-C5 level. Still, due to the dangerous nature of the operation, the patient continued supportive treatment and had a significant improvement in his next MRI without any invasive procedure.
Keywords: Intracranial hypotension, Orthostatic headache, Pregnant women, Pregnancy
Case report
Spontaneous intracranial hypotension (SIH) is a rare condition where the CSF pressure is lower than expected. The disease is more likely to present with orthostatic headaches, neck stiffness, nausea, vomiting, photophobia, and phonophobia [1]. SIH was first named aliquorrhea by Schaltenbrand et al. [2]. He also explained that low CSF pressure could be rooted in decreased production, increased absorption, and CSF leakage [3], which recent studies have suggested that CSF leakage from the thoracic spinal cord is the most common cause of intracranial hypotension [4].There are various theories about the cause of orthostatic headache in SIH. the strongest theory states that a normal brain (weighing 1500 grams) weighs only 48 grams when surrounded by an appropriate amount of CSF [5]. A decrease in CSF pressure increases traction in pain-sensitive tissues, which is at its maximum in the standing position [6].
From an epidemiological point of view, the incidence of SIH is reported to be 5 in 100,000 per year, and the highest prevalence is reported at the age of 40. Also, in terms of gender distribution, women are twice as likely as men to be affected by the disease [7]. Despite the higher prevalence of SIH in women, the role of pregnancy in this disease has not been thoroughly studied. This case report describes a 32-year-old pregnant woman diagnosed with SIH who improved after childbirth without any aggressive treatment.
A 32-year-old pregnant woman, gravid two para one ab zero, presented to our emergency department at 34 weeks’ gestation with a chief complaint of Severe bilateral parietal headache. The patient stated that the first episode of the headache started mildly at 25 weeks of gestation, which was controlled with analgesics. In the recent episode, the onset of headache was 2 days before admission, which had a progressive pattern. The location of the pain was bilateral in the parietal area of the head, which had a pulsating character and radiated to the patient's neck. In addition, the headache was worse in the standing position than in the supine position and did not respond to analgesia. The patient also complained of photophobia, insomnia, nausea, and vomiting.
She mentioned migraine in her medical history, but her migraine headaches mainly affected the left side of the patient's head and, according to the patient, had different characteristics from her recent headaches. Her pre-admission medications included Famotidine 40 mg orally once a day, Citalopram 20 mg orally once a day, Acetaminophen PRN.
On initial physical examination, she had a blood pressure of 110/60 mmHg with a pulse rate of 88 beats per minute (bpm). She was fully conscious and oriented to time and place. In addition, all the cranial nerves, cerebellum, and speech center functions were unremarkable. The fundoscopic examination was also normal, and Laboratory data were in the standard range.
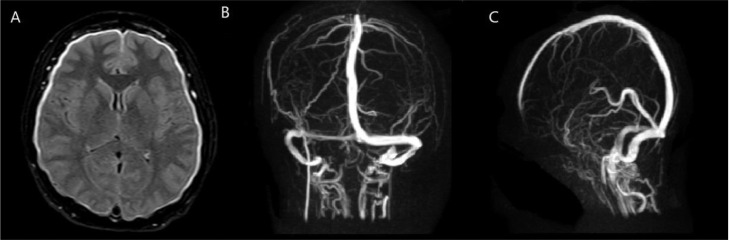
At the beginning of the admission, intravenous heparin was started with suspicion of Cerebral Venous Thrombosis (CVT), and an emergency MRI and MRV was requested. MRV ruled out the diagnosis of CVT and MRI confirmed the diagnosis of SIH (Fig. 1). Lumbar puncture (LP) could not be performed to measure the CSF pressure, which is usually performed to confirm SIH due to high-risk pregnancy. Subsequently, during consultations with neurologists and obstetricians, the decision was made to terminate the pregnancy by cesarean section because it was harmful for the patient to tolerate labor pain. She finally gave birth to a healthy girl. After the cesarean section, Caffeine 200 mg orally Q8hr and complete bed rest were prescribed for her, and she remained asymptomatic in the hospital for several days. She was discharged with outpatient follow-up of a neurologist for further investigation of the cause of intracranial hypotension.
Fig. 1.
Diffuse dura-arachnoid enhancement suggestive of SIH (A). CVT ruled out with Magnetic Resonance Venography (MRV) (B, C).
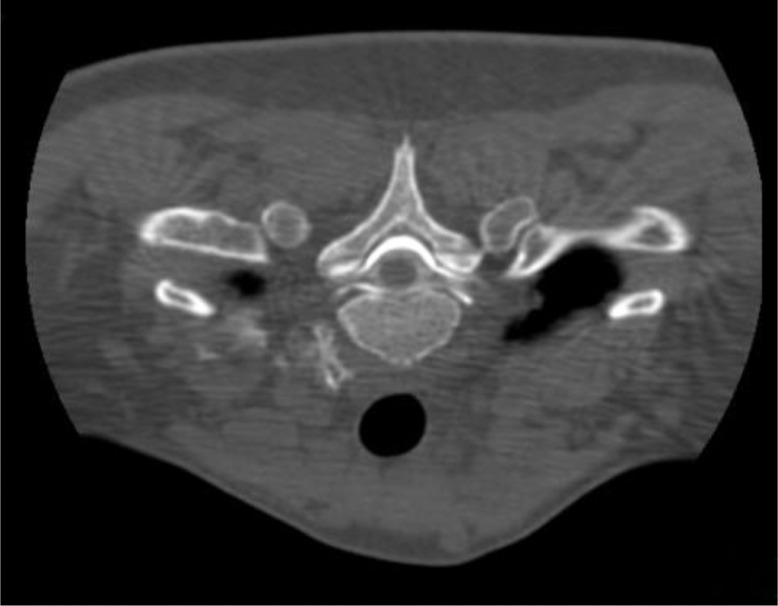
In a 10-day follow-up, she continued to complain of headaches. Therefore, CT-cisternography and CT-myelography were requested to find the underlying cause of the disease and the exact location of the CSF leak. CT-myelography showed extravasation of contrast at the level of C5-T5 into the anterior segment of the epidural space (Fig. 2). On the other hand, CT-cisternography showed similar results. There was contrast leakage at the level of C1-T7 into the epidural space, and the most significant bulk of extravasation of contrast was seen at the level of C3-C5 (Fig. 3).
Fig. 2.
CT-myelography shows extravasation of contrast into the epidural space.
Fig. 3.
Coronal cut of CT-cisternography shows extravasation of contrast into the epidural space in cervical region.
Epidural blood patch was not recommended for the patient due to the sensitive area of CSF leakage which was located in the cervical region. The surgical option for Dural reconstruction was provided to the patient. Still, due to the high risk of the operation and the possibility of further complications, she requested to continue conservative treatment and refused to operate. Therefore, a high-salt diet, high-liquid intake, bed rest, acetaminophen, caffeine, and a follow-up for 3 months later were prescribed for her. At the next visit, the patient stated that the frequency and severity of headaches were significantly reduced, and to confirm this claim; a brain MRI was performed for the patient, which had notable improvement compared to the patient's previous MRIs and showed almost no abnormal findings (Fig. 4).
Fig. 4.
Normal brain MRI of the patient with and without contrast.
Discussion
Headaches, nausea, vomiting, and sensitivity to light are symptoms that can easily be attributed to the nature of pregnancy or even be confused with conditions such as migraine and sinus thrombosis, so taking a mindful history can help the diagnosis of SIH [8]. Another difficulty in accurately diagnosing SIH is that most patients have unremarkable neurological exams, desirable laboratory tests, and sometimes even normal cerebrospinal fluid pressure [9,10].
Lumbar puncture (LP) with opening pressure can aid us in diagnosing SIH. Usually, CSF pressure is reported below 6 cm H2O in these patients [11]. However, it is unnecessary to perform LP in centers with access to MRI. The most common diagnostic finding of MRI is a diffuse meningeal enhancement, which was also observed in supra-tentorial and infra-tentorial regions of our patient's brain [12]. In addition, there were signs of bilateral subpleural effusion or hygroma (one of the characteristic radiographic findings in spontaneous intracranial hypotension), in her neuroimaging [13].
Conservative treatments such as avoidance of upright position and consuming more fluids are generally recommended for the treatment of these patients. Also, analgesic and glucocorticoid therapies have been performed on these patients and have responded well to treatment, but more studies are still needed to establish their use [14], [15], [16].
Epidural blood patch (EBP) is another treatment available for SIH that has shown a significant impact on the recovery of patients which declared in several studies [17,18]. EBP was not performed for our patient due to the sensitive location of the Dural defect. However, in a survey conducted by Kapoor et al. [19] in the field of cervical epidural blood patch, no major neurological complications were observed in any patient while injecting EBP or later.
The interesting point about our patient was that she had improved with delivery and supportive therapies without any invasive treatment, which could indicate the role of pregnancy in exacerbating SIH symptoms. In a similar case reported by McGrath et al. [20], their patient had headaches in her first pregnancy and was completely cured. After that, she did not show any symptoms for five years until she came back with postural headaches in her second pregnancy. Therefore, pregnancy may be considered as a possible aggravating factor for spontaneous intracranial hypotension, and further studies are needed to test this hypothesis.
In conclusion, spontaneous intracranial hypotension (SIH) is still a rare disease in pregnancy, but with severe consequences, if not diagnosed correctly and on time. Clinical complaints of the disease, along with brain MRI and other imaging modalities, can help diagnose SIH and the exact location of the CSF leak. Furthermore, treatments such as analgesics, a high-salt diet, generous caffeine intake, epidural blood patch, and surgery can be used to treat various scenarios of this disease.
Patient Consent
The authors have obtained a written informed consent from the patient to publish his case (including publication of images).
Footnotes
Competing Interests: All authors declare no conflict of interest.
References
- 1.Rahman M, Bidari SS, Quisling RG, Friedman WA. Spontaneous intracranial hypotension: dilemmas in diagnosis. Neurosurgery. 2011;69(1):4–14. doi: 10.1227/NEU.0b013e3182134399. discussion. [DOI] [PubMed] [Google Scholar]
- 2.Schaltenbrand G. Neuere Anschauungen zur Pathophysiologie der Liquorzirkulation. Zentralbl Neurochir. 1938;3:290–300. [Google Scholar]
- 3.Schaltenbrand G. Normal and pathological physiology of the cerebrospinal fluid circulation. Lancet. 1953;1(6765):805–808. doi: 10.1016/s0140-6736(53)91948-5. [DOI] [PubMed] [Google Scholar]
- 4.D'Antona L, Jaime Merchan MA, Vassiliou A, Watkins LD, Davagnanam I, Toma AK, et al. Clinical presentation, investigation findings, and treatment outcomes of spontaneous intracranial hypotension syndrome: a systematic review and meta-analysis. JAMA Neurol. 2021;78(3):329–337. doi: 10.1001/jamaneurol.2020.4799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horton JC, Fishman RA. Neurovisual findings in the syndrome of spontaneous intracranial hypotension from dural cerebrospinal fluid leak. Ophthalmology. 1994;101(2):244–251. doi: 10.1016/s0161-6420(94)31340-6. [DOI] [PubMed] [Google Scholar]
- 6.D'Amico D, Usai S, Chiapparini L, Erbetta A, Gioppo A, Messina G, et al. Headache in spontaneous intracranial hypotension: an overview with indications for differential diagnosis in the clinical practice. Neurol Sci. 2020;41(Suppl 2):423–427. doi: 10.1007/s10072-020-04642-9. [DOI] [PubMed] [Google Scholar]
- 7.Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. Jama. 2006;295(19):2286–2296. doi: 10.1001/jama.295.19.2286. [DOI] [PubMed] [Google Scholar]
- 8.Chisholm ME, Campbell DC. Postpartum postural headache due to superior sagittal sinus thrombosis mistaken for spontaneous intracranial hypotension. Can J Anaesth. 2001;48(3):302–304. doi: 10.1007/BF03019763. [DOI] [PubMed] [Google Scholar]
- 9.Kranz PG, Tanpitukpongse TP, Choudhury KR, Amrhein TJ, Gray L. How common is normal cerebrospinal fluid pressure in spontaneous intracranial hypotension? Cephalalgia. 2016;36(13):1209–1217. doi: 10.1177/0333102415623071. [DOI] [PubMed] [Google Scholar]
- 10.Robblee J, Secora KA, Alhilali LM. Spontaneous intracranial hypotension. Pract Neurol. 2020;20:41–52. [Google Scholar]
- 11.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 12.Mokri B, Piepgras DG, Miller GM. Syndrome of orthostatic headaches and diffuse pachymeningeal gadolinium enhancement. Mayo Clin Proc. 1997;72(5):400–413. doi: 10.4065/72.5.400. [DOI] [PubMed] [Google Scholar]
- 13.Inamasu J, Moriya S, Shibata J, Kumai T, Hirose Y. Spontaneous intracranial hypotension manifesting as a unilateral subdural hematoma with a marked midline shift. Case Rep Neurol. 2015;7(1):71–77. doi: 10.1159/000381667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hashmi M. Low-pressure headache presenting in early pregnancy with dramatic response to glucocorticoids: a case report. J Med Case Rep. 2014;8:115. doi: 10.1186/1752-1947-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmann J, Goadsby PJ. Update on intracranial hypertension and hypotension. Curr Opin Neurol. 2013;26(3):240–247. doi: 10.1097/WCO.0b013e328360eccc. [DOI] [PubMed] [Google Scholar]
- 16.Bel I, Moreno LA, Gomar C. Epidural dextran-40 and paramethasone injection for treatment of spontaneous intracranial hypotension. Can J Anaesth. 2006;53(6):591–594. doi: 10.1007/BF03021850. [DOI] [PubMed] [Google Scholar]
- 17.Ferrante E, Trimboli M, Petrecca G, Allegrini F, Ferrante MM, Rubino F. Management of spontaneous intracranial hypotension during pregnancy: a case series. Headache. 2020;60(8):1777–1787. doi: 10.1111/head.13942. [DOI] [PubMed] [Google Scholar]
- 18.Grange J, Lorre G, Ducarme G. Iterative epidural blood patch for recurrent spontaneous intracranial hypotension during pregnancy. J Clin Anesth. 2016;34:239–243. doi: 10.1016/j.jclinane.2016.04.040. [DOI] [PubMed] [Google Scholar]
- 19.Kapoor SG, Ahmed S. Cervical epidural blood patch—a literature review. Pain Medicine. 2015;16(10):1897–1904. doi: 10.1111/pme.12793. [DOI] [PubMed] [Google Scholar]
- 20.McGrath E, Monaghan TS, Alexander M, Hennessy MJ. Recurrent spontaneous intracranial hypotension in early pregnancy. BMJ Case Rep. 2010;2010 doi: 10.1136/bcr.05.2010.3040. [DOI] [PMC free article] [PubMed] [Google Scholar]