Abstract
Climate change is one of the greatest threats to human health in the 21st century. The human health impacts of climate change contribute to approximately 1 in 4 deaths worldwide. Health care itself is responsible for approximately 5% of annual global greenhouse gas (GHG) emissions. Canada is a recent signatory of the 26th United Nations Climate Change Conference (COP26) health agreement that is committed to developing low carbon and climate resilient health systems. Kidney care services have a substantial environmental impact and there is opportunity for the kidney care community to climate align clinical care. We introduce a framework of redesigned kidney care and describe examples of low carbon kidney disease management strategies to expand our duty of care to the environment which completes the triple bottom line of optimal patient outcomes and cost effectiveness in the Anthropocene.
Keywords: planetary health, sustainable healthcare, sustainable nephrology, green nephrology, triple bottom line
Introduction
Climate change is one of the greatest threats to human health in the 21st century, with an extraordinary 12.6 million deaths, approximately 1 in 4 worldwide, attributable to environmental factors. 1 Kidney disease and climate change each worsen the other. Excessive heat, through recurrent or severe volume depletion insults, increases the risk of both acute and chronic kidney diseases. Particle pollution, of which fossil fuel combustion is a major source, is potentially responsible for a significant attributable burden of prevalent chronic kidney disease (CKD) as well as CKD-associated morbidity. 2 Health care itself is responsible for 5% of annual global greenhouse gas (GHG) emissions, equivalent to airplane travel. 3
Worldwide, Canada has the ninth highest absolute and the third highest per capita health care sector carbon emissions. 4 Greenhouse gas emissions from Canadian health care have been linked to more than 20 000 disability-adjusted life years per annum from direct exposure or environmental changes caused by pollution. 5 While few studies have evaluated the carbon footprint of nephrology practice, our services are among the most resource intensive within clinical care.6-9 More than 20 000 patients require maintenance dialysis care in Canada, the prevalence of which has doubled over the last 20 years. 10 Kidney failure is an outcome universally undesirable by patients, providers, programs, and payers alike. It is also environmentally costly, owing to the resource intensiveness of end-stage disease management, with dialysis services requiring significant expenditures of energy, water, and single-use disposable materials, as well as the powering, heating, or cooling, and transportation of patients and ourselves to our many and often sizable health care facilities. One year per patient hemodialysis-related emissions range between 4 and 10 tonnes CO2-eq (carbon dioxide equivalents).11,12 Methodologic issues of carbon accounting in published emissions data from peritoneal dialysis (PD) limit direct modality comparison, though these data suggest that PD emissions are comparably high.
The Paris Accord is an international agreement aiming to keep global warming below 2°C; Canada is a signatory hence we are legally bound to our Paris obligations. Canada seeks to reduce emissions by 40% to 45% below 2005 levels by 2030 and achieve net zero emissions by 2050. It is widely accepted that to succeed in reaching this goal, all sectors of the Canadian economy must comply with these reductions. 13 Furthermore, Canada is a recent signatory of the 26th United Nations Climate Change Conference (COP26) health agreement; hence, there is a new national ambition and necessity to build climate resilient health systems. Sustainability is identified as a goal of provincial medical services plans as well as regional nephrology programs across our country. Our need to align processes to avert climate change’s most alarming, forecasted effects are motivating transformation throughout society - health and kidney care included. The COVID-19 pandemic quickly taught us that system redesign is achievable in the face of necessity. By analogy, in tackling the climate crisis all aspects of our status quo must be “on the table” in considering how to redesign patient centered, quality kidney care in this new era.
Planetary health is a value-based approach to care that views health in the context of human caused disruptions to Earth’s natural systems. Planetary health seeks to maximize outcomes while being cost efficient and environmentally responsible. A Planetary Health Care Redesign Model (Figure 1) was created in anticipation of the Lancet Commission on health and climate change, with objectives to identify and develop a standardized transdisciplinary approach to sustainable clinical care. In an accompanying commentary to this article, Dr Stigant has detailed the urgent need for kidney care to align with planetary health principles. Here, the Sustainable Nephrology Action Planning (SNAP) committee of the Canadian Society of Nephrology (CSN) outlines our vision of sustainable nephrology practice based on the 3 principles of the Planetary Health Care Redesign Model (Figure 1): (1) reducing demand for health care services, (2) matching supply of health services to demand, and (3) reducing emissions from the supply of health services. 14
Figure 1.
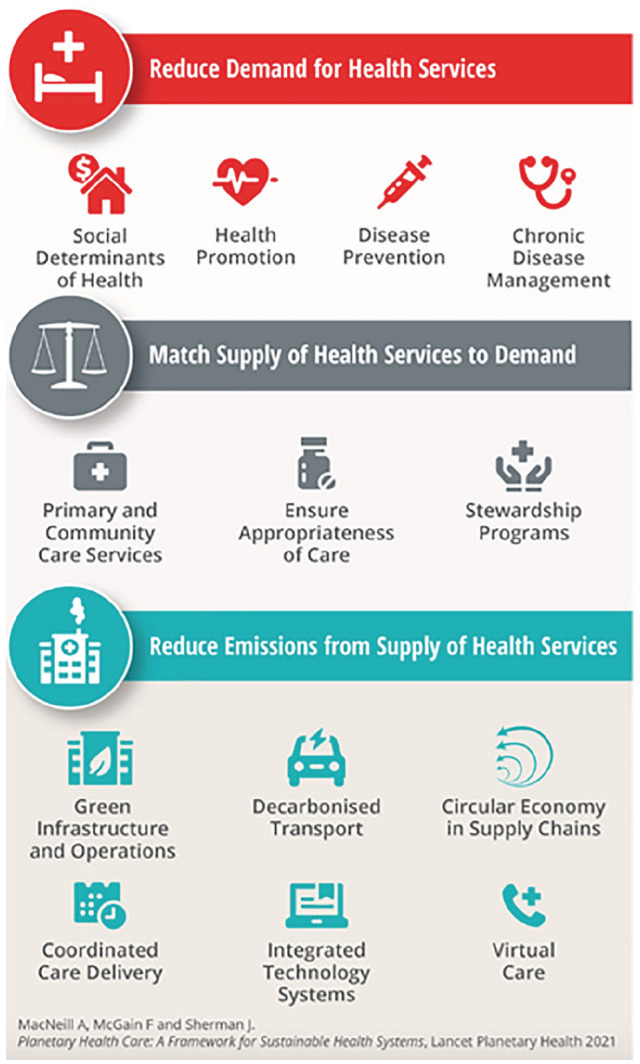
Framework for sustainable health systems generated by MacNeill et al. 14
Reducing Demand for Health Services
Pediatric and adult nephrologists alike must engage effectively in general population health promotion, given that considerable disease typically accrues before any contact is made with a kidney care provider. Opportunities to engage individuals directly through newer media such as podcasts, online events including World Kidney Day, or even engagement of social media champions can be leveraged. We call for renewed enthusiasm toward robust, evidence-based management of non-communicable diseases, in particular hypertension and diabetes. Promotion of healthy lifestyles includes exercise and diet prescribing, as well as recently proposed prescription of time in nature, demonstrated to improve numerous health outcomes. 15 For patients with CKD, kidney care professionals could advocate for subsidized patient exercise programs to improve cardiovascular health, and routinely and strongly inform that smoking is harmful to overall health, including kidney health, as well as having competency in smoking cessation strategies. 16 In addition, in our era of climate crisis, providers must learn, lead by example, and inform about the health benefits of a low carbon lifestyle. One accessible example is the “Jump” program that focuses on clear, constructive, impactful, and achievable personal change. 17
Engagement with an informed network of primary care partners is essential; this will involve medical education outreach to ensure our colleagues have skills to recognize and effectively treat earlier stages of disease. There is ample opportunity to collaborate with other medical specialties in increasing awareness of CKD, and through this collaboration to broaden health promotion, given the ubiquity of lifestyle diseases across the spectrum of care. Updating the Canadian Task Force on Preventive Health Care, 18 or through this resource providing an overarching framework for cardiovascular disease prevention and management, could simplify messaging, prescribing, and effectiveness of care.
We suggest consideration of expanded CKD screening, as modeled on criteria outlined in the KDIGO Improving Global Outcomes Conference on early CKD identification and intervention, that includes screening for conditions that nephrologists readily recognize as kidney disease risks, including HIV infection, systemic lupus, environmental exposures, and, sadly, low socioeconomic status. Canadian examples of broader medical community engagement in CKD screening include the FINISHED program in Manitoba, which provided community-based screening for Indigenous people on several reserves to identify and manage early hypertension, proteinuria, and diabetes from ages 10 to 80. The Can-SOLVE CKD Network allows recognition of higher risk subgroups, as well as targeted management strategies.
Policymakers must also be engaged, adapting the WHO “Health in All Policies” framework and leveraging UN Sustainable Development Goals to effect structural factors that affect risk and outcome of kidney disease. The nephrology community can advocate for greater access to preventive pharmacotherapies, including renin-angiotensin-aldosterone system (RAAS) and sodium-glucose-cotransporter-2 (SGLT2) inhibitors, through improved and ideally universal coverage for these agents in CKD patients with therapeutic indication.
As we emerge from the COVID-19 pandemic, increased access to preventive care, as well as social determinants of health, must be highlighted. Kidney health promotion starts with maternal health. Our pediatric population also warrants particular attention, with reduced access to community supports including schools, sports, and social interaction, having occurred during a key developmental life stage.
A secondary focus to reduce demand for individual, financial, and environmental kidney failure treatment costs is optimizing the uptake of transplantation, in particular live donation, our treatment of choice for eligible patients with kidney failure. Efficiencies in care provision should be optimized, such as single-day transplant donor evaluation. 19 Expanded up-front funding for donor expenses, including lost wages, childcare, and elder care, should be explored. Resources and staffing should be optimized to ensure timely completion of donor and recipient workup.
It is well known that the need for donors far outweighs supply. The climate crisis provides a unique focus for reconsideration of national policies to optimize the number of deceased donor organs available, including public awareness campaigns, establishment of a national organ donor registry, and review of policies previously demonstrated to modestly impact organ donation, including the universal presumed consent (opt out) deceased organ donor national policy. 20 More studies are needed to explore other avenues such as xenotransplantation and organoids, noting recent progress toward human trials as well as short-term success. 21
Although there have been significant advances in transplantation, there needs to be renewed investment in exploring strategies for increasing graft survival. Recently, Health Canada has invested significant funding to study artificial intelligence and its role in matching donor organs to recipients to maximize graft survival. Messenger RNA (mRNA) technology, employed for the coronavirus pandemic in vaccine production, could be applied to organ-destroying viruses like cytomegalovirus (CMV) and BK. Finally, optimizing medication adherence is a key to the longevity of transplanted organs. Engaging with patients to improve health literacy, advocating for combination pills to reduce overall pill burden, pharmacy consultation, and reminder tools are all areas worthy of renewed attention. Digital technology such as mobile innovations (mHealth), text messaging, electronic medication monitoring devices, and telehealth could be adopted. Notably, these tools have successfully supported people living with HIV to maintain engagement in care and medication adherence in lower- and middle-income countries. 22
Matching Supply to Demand
Matching supply to demand involves appropriateness of care and the avoidance of both underuse and overuse, as both result in suboptimal patient outcomes and ultimately higher health care costs. Appropriate care encompasses the investigations ordered, treatments prescribed, as well as the setting in which the care is provided.
Patients with CKD undergo routine laboratory tests and investigations that likely do not consistently improve outcome, and studies determining the optimal frequency of routine lab testing are needed. In addition, kidney patients are prescribed numerous medications, many of which are poorly tolerated, not taken, or interact with other drugs. System-wide strategies to better steward drug prescribing in kidney disease are needed, including deprescribing, medication reconciliation, and frank conversations regarding goals of care.
Kidney care providers are skilled at building relationships with our patients and engaging in goals of care discussions. Selection of appropriate candidates for dialysis is a particular strength. Most programs have robust conservative care pathways for comprehensive and compassionate support of patients who either choose not to pursue, or would be felt not to benefit from, dialysis. Provision of patient centered timely care with optimal control of symptom burden throughout this pathway must be universally optimized in terms of education, staffing, and clinical and pharmacologic resources to improve quality of life. Once dialysis therapy is initiated, allowing continued consideration of dialysis adequacy measures, both peritoneal and hemodialysis prescriptions can be individualized using incremental or decremental regimens when appropriate.
Patients with kidney disease must often travel from distant or isolated communities to access kidney care, which is most often provided in tertiary or quaternary health care facilities. This is a universally challenging aspect of pediatric kidney care, often requiring families to travel frequently or even permanently relocate to major centers, factors that introduce tremendous emotional and often financial stress on patients and their families. Care that maximizes home supports related to home dialysis and transplantation ranging from virtual care appointments to home dialysis must be optimized. 23
Reducing Emissions From the Supply of Health Services
Strategies to improve operational efficiencies of dialysis care must be successively introduced while transformative end-stage disease treatments are envisioned, studied, and then implemented. Kidney services in the United Kingdom (UK) have introduced numerous water savings, waste reduction and diversion, and energy reduction strategies to their daily operations that could be swiftly adapted to most Canadian care settings. 24 Other health regions, notably Australia, have implemented renewable energy sourcing for hemodialysis facilities. 25 Use of RO reject water for “gray” purposes, or capture then recirculation of this water through the RO system, can greatly reduce water consumption and cost. 26 Industry partners can and must do more to curtail their emissions at all product stages, including design, production, and transport. Novel bioplastics should be explored and acknowledging per treatment plastic hemodialysis waste currently exceeding 1 kg, there is pressing need to evaluate optimal plastic handling, including development of a circular plastic economy. 27 There is ample opportunity for innovation in production of durable dialysis equipment, and most importantly novel dialysis systems, such as sorbent-based systems or portable options. Sorbent hemodialysis systems had early safety and efficacy issues that have been largely overcome with modern cartridges. 28 This technology deserves renewed attention in view of its marked reduction in water consumption compared to existing single pass hemodialysis system infrastructure. 28 New dialysis builds should be data informed by capture of progressive kidney disease prevalence data and constructed with deliberate incorporation of sustainable infrastructure.
Importantly, all kidney care service centers must evaluate their waste management. There is opportunity for a nationally coordinated infrastructure for recycling non-biohazard plastic waste, reprocessing spent machinery, and provision of high-efficiency incineration when reuse options do not apply. In both product use and waste disposal, appropriateness of cleanliness versus sterility should be considered. Patients and colleagues alike, receiving care and working in dialysis programs, are increasingly voicing moral distress regarding the vast amounts of waste generated by these necessary life-sustaining therapies. Their enthusiasm can be harnessed to effect system change, toward better stewardship of waste reduction and management strategies. We ought to steward therapeutic resources optimally to ensure that patients do not suffer additional burden caused by the environmental impact of clinical care.
Despite demonstrating enormous environmental impact of dialysis therapies, previous studies have lacked standardization of carbon footprint analysis inputs and included different energy sources and consumption, as well as different waste disposal mechanisms. As a result, it is difficult to generalize results to one’s center or region and to compare the environmental effect of different dialysis modalities. Carbon footprint analyses have not been performed for nephrology services in Canada. Life cycle assessment (LCA) has emerged as the gold standard environmental impact methodology, with quantification of a comprehensive suite of environmental impacts of products, processes, and services. To our knowledge, there are no published LCA data performed for kidney care. This essential information would identify areas of high environmental impact, thereby allowing targeted emission reductions.
We acknowledge that stakeholder engagement is required throughout medical systems to enact this proposed planetary health lens and call on each member of our community to change their clinical practice by thinking and functioning in a planetary health framework.
Conclusions
Canada is one of 51 countries that have committed to low carbon and sustainable health care systems. Herein, the SNAP committee of the Canadian Society of Nephrology has adapted an overview of kidney care through a planetary health care framework. Stakeholder engagement at health facility, regional renal program, and national levels is required to enact planetary health aligned kidney care. Sustainable Nephrology Action Planning members are presently working to describe both idealized kidney care pathways, as well as details of specific low carbon kidney disease management strategies. In the Anthropocene, our duty of care is expanded to the environment, making sustainable medical practice an essential component of care that must be considered alongside existing quality metrics of patient outcome and cost reduction.
Acknowledgments
The CSN Sustainable Nephrology Action Planning Committee thanks Dr. Andrea MacNeill, Filomena Picciano, Diane Perazzo, and Frank Lindo Verission for their invaluable assistance.
Footnotes
Ethics Approval and Consent to Participate: As this is an opinion piece Ethical approval and consent to participate needs to be deleted. All authors consent for publication of the manuscript in its current form. No additional data and material are available.
Consent for Publication: All authors consent for publication of the manuscript in itscurrent form.
Availability of Data and Materials: No additional data and material are available.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: R.S. is on the Advisory Board for GSK-Benlysta and Novartis-Ipatocopan. She has also received honoraria with GSK. All the authors have no conflicts of interest relevant to this opinion piece. All the authors approved the final version of the submitted manuscript. We certify that this manuscript is not being considered for publication elsewhere.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Tasleem Rajan  https://orcid.org/0000-0003-4343-2041
https://orcid.org/0000-0003-4343-2041
Ratna Samanta  https://orcid.org/0000-0002-3014-7316
https://orcid.org/0000-0002-3014-7316
Ahmad Tarakji  https://orcid.org/0000-0001-8806-4911
https://orcid.org/0000-0001-8806-4911
Caroline Stigant  https://orcid.org/0000-0003-2578-0966
https://orcid.org/0000-0003-2578-0966
References
- 1. IPCC 2021. Summary for policymakers. In: Masson-Delmotte V, Zhai P, Pirani A, et al. eds. Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, England: Cambridge University Press; in press. [Google Scholar]
- 2. Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. Particulate matter air pollution and the risk of incident CKD and progression to ESRD. J Am Soc Nephrol. 2018;29(1):218-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lenzen M, Malik A, Li M, Fry J, Weisz H, Pichler PP, Chaves LS, Capon A, Pencheon D. The environmental footprint of health care: a global assessment. Lancet Planet Health. 2020. Jul 1;4(7):e271-9. [DOI] [PubMed] [Google Scholar]
- 4. Watts N, Amann M, Arnell N, et al. The 2019 report of the lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394(10211):1836-1878. [DOI] [PubMed] [Google Scholar]
- 5. Eckelman MJ, Sherman JD, MacNeill AJ. Life cycle environmental emissions and health damages from the Canadian healthcare system: an economic-environmental-epidemiological analysis. PLoS Med. 2018;15(7):e1002623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Connor A, Lillywhite R, Cooke MW. The carbon footprint of a renal service in the United Kingdom. QJM. 2010;103(12):965-975. [DOI] [PubMed] [Google Scholar]
- 7. Lim AE, Perkins A, Agar JW. The carbon footprint of an Australian satellite haemodialysis unit. Aust Health Rev. 2013;37(3):369-374. [DOI] [PubMed] [Google Scholar]
- 8. Mtioui N, Zamd M, Ait Taleb A, et al. Carbon footprint of a hemodialysis unit in Morocco. Ther Apheresis and Dial. 2021;25:613-620. [DOI] [PubMed] [Google Scholar]
- 9. Chen M, Zhou R, Du C, et al. The carbon footprints of home and in-center peritoneal dialysis in China. Int Urol Nephrol. 2017;49(2):337-343. [DOI] [PubMed] [Google Scholar]
- 10. IPCC, 2021: Summary for Policymakers. In: Climate Change 2021: The Physical Science Basis. Contribution of Working Group 1 to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Masson-Delmotte V, Zhai P, Pirani A, Connors SL, Pean C, Berger S, Caud N, Chen Y, Goldfarb L, Gomes MI, Huang M, Leitzell K, Lonny E, Matthews JBR, Maycock TK, Waterfield T, Yelekci R, Yu R, Zhou B (Ed’s.)]. Cambridge University Press, Cambridge, United Kingdom and New York, NY, USA, pp.332, doi:10.1017/9781009157896.001. [Google Scholar]
- 11. Blankestijn PJ. Towards sustainable environmental development in nephrology care, research and education. Nat Rev Nephrol. 2021;17(1):7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barraclough KA, Agar JW. Green nephrology. Nat Rev Nephrol. 2020;16:257-268. [DOI] [PubMed] [Google Scholar]
- 13. Government of Canada. Environment and climate change Canada. 2030 emissions reduction plan: clean air, strong economy. https://www.canada.ca/en/services/environment/weather/climatechange/climate-plan/climate-plan-overview/emissions-reduction-2030.html?utm_campaign=not-applicable&utm_medium=vanity-url&utm_source=canada-ca_emissions-reduction-plan. Published 2022. Accessed May 8, 2022.
- 14. MacNeill AJ, McGain F, Sherman JD. Planetary health care: a framework for sustainable health systems. Lancet Planet Health. 2021;5(2):e66-e68. [DOI] [PubMed] [Google Scholar]
- 15. Müller-Riemenschneider F, Petrunoff N, Yao J, et al. Effectiveness of prescribing physical activity in parks to improve health and wellbeing-the park prescription randomized controlled trial. Int J Behav Nutr Phys Act. 2020;17:1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee S, Kang S, Joo YS, et al. Smoking, smoking cessation, and progression of chronic kidney disease: results from KNOW-CKD study. Nicotine Tob Res. 2021;23(1):92-98. [DOI] [PubMed] [Google Scholar]
- 17. The Jump. Take the jump. Date unknown. https://takethejump.org/. Accessed 29 May, 2022.
- 18. Canadian Task Force on Preventative Health Care. https://canadiantaskforce.ca/. Published 2019. Accessed May 20, 2022.
- 19. Graham JM, Courtney AE. The adoption of a one-day donor assessment model in a living kidney donor transplant program: a quality improvement project. Am J Kidney Dis. 2018;71(2):209-215. [DOI] [PubMed] [Google Scholar]
- 20. Saab S, Saggi SS, Akbar M, Choi G. Presumed consent: a potential tool for countries experiencing an organ donation crisis. Dig Dis Sci. 2019;64(5):1346-1355. [DOI] [PubMed] [Google Scholar]
- 21. Montgomery RA, Stern JM, Lonze BE, et al. Results of two cases of pig-to-human kidney xenotransplantation. N Engl J Med. 2022;386(20):1889-1898. [DOI] [PubMed] [Google Scholar]
- 22. Jongbloed K, Parmar S, van der Kop M, Spittal PM, Lester RT. Recent evidence for emerging digital technologies to support global HIV engagement in care. Curr HIV/AIDS Rep. 2015;12(4):451-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Holmner A, Ebi KL, Lazuardi L, Nilsson M. Carbon footprint of telemedicine solutions-unexplored opportunity for reducing carbon emissions in the health sector. PLoS One. 2014;9(9):e105040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Connor A, Mortimer F, Tomson C. Clinical transformation: the key to green nephrology. Nephron Clin Pract. 2010;116(3):c200-c206. [DOI] [PubMed] [Google Scholar]
- 25. Agar JW. Conserving water in and applying solar power to haemodialysis: ‘green dialysis’ through wiser resource utilization. Nephrology. 2010;15(4):448-453. [DOI] [PubMed] [Google Scholar]
- 26. Agar JW. Reusing and recycling dialysis reverse osmosis system reject water. Kidney Int. 2015;88(4):653-657. [DOI] [PubMed] [Google Scholar]
- 27. Bendine G, Autin F, Fabre B, et al. Haemodialysis therapy and sustainable growth: a corporate experience in France. Nephrol Dial Transplant. 2020;35(12):2154-2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Agar JW. Understanding sorbent dialysis systems. Nephrology. 2010;15(4):406-411. [DOI] [PubMed] [Google Scholar]


