Abstract
Objective
To perform conventional, morphological, and T2 mapping compositional MRI imaging to assess the cartilage degeneration and osteoarthritic progression in patients with medial meniscus posterior root tears (MMPRTs) who underwent trans-posterior cruciate ligament (PCL) all-inside repair or partial meniscectomy.
Design
Patients with MMPRTs after trans-PCL all-inside repair (group AR) or partial meniscectomy (group PM) between 2015 and 2018 were retrospectively identified. Preoperative and postoperative conventional MRI were collected to assess medial meniscus extrusion (MME) and the whole-organ magnetic resonance imaging score (WORMS). Postoperative morphological MRI and T2 mapping compositional MRI were collected to evaluate the quantitative cartilage thickness/volume and cartilage composition.
Results
The final cohort consisted of 21 patients in group AR and 22 patients in group PM, with no differences in demographic data and baseline patient characteristics between the 2 groups. Group AR demonstrated less progression of articular cartilage wear (P < 0.05) and decreased meniscal extrusion (P = 0.008) than group PM at the final follow-up. In addition, group AR demonstrated less extracellular matrix degeneration in the cartilage subregion of the medial compartment (P < 0.05) than group PM with lower T2 relaxation times in the superficial layer of the articular cartilage.
Conclusion
Trans-PCL all-inside repair of MMPRTs could delay the initial cartilage deterioration and morphological cartilage degeneration compared with partial meniscectomy. However, the amount of residual meniscal extrusion is clinically important, and an improved root repair fixation method should be investigated.
Keywords: meniscus root tear, medial meniscus, all-inside repair, MRI evaluation
Introduction
Medial meniscus posterior root tears (MMPRTs) are an important subset of medial meniscus tears within 1 cm of posterior horn attachment to the tibial plateau.1-3 MMPRTs disrupt the circumferential fibers of the meniscus, leading to increases in peak contact pressure in the medial compartment to a functionally total meniscectomized condition,4,5 resulting in accelerated knee osteoarthritis.6-11 Previous studies have demonstrated that conservative treatment and partial meniscectomy provide no benefit for MMPRTs with total knee arthroplasty (TKA) conversion rates of 31% 12 and 54%, 13 respectively. On account of unsatisfactory outcomes of conservative treatment and meniscectomy,12,13 arthroscopic meniscal repair methods, including transtibial pull-out repair, anchor suture, and all-inside repair, have been developed to restore the integrity and hoop tension of the meniscus to prevent further joint degeneration.11,14,15 For all-inside repair via suture fixation to the posterior cruciate ligament (PCL), restoration of tibiofemoral contact mechanics has been demonstrated in current biomechanical studies. 16 While current studies on meniscal repair have demonstrated significant improvements in clinical scores and high survival rates,17-21 the early change in cartilage and progression of knee osteoarthritis (KOA) over time have not been sufficiently investigated.22,23
Considered as a disease of the whole joint, KOA is characterized by cartilage degradation, subchondral bone changes, meniscus degeneration, and synovial inflammation. 24 However, these arthritic changes in the joint tissue were not visible by radiographs. Thus, MRI was introduced to provide a comprehensive and accurate evaluation of osteoarthritis (OA), which is more sensitive for detecting cartilage defects, subchondral bone changes, bone morrow lesions (BMLs), synovitis, and extracellular cartilage matrix (ECM) degeneration.25-27 Recently, MRI assessment in OA research has been classified into semiquantitative and quantitative methods. 25 The Whole-Organ Magnetic Resonance Imaging Score (WORMS) is the first and most common MRI-based semiquantitative scoring system for whole-joint assessment of KOA with high inter-reader agreement, 28 which enables grading of osteoarthritic features.25,28 Quantitative MRI evaluation of KOA includes morphological measurement and compositional imaging.29-32 Considering that cartilage damage is one of the central elements in KOA progression, quantitative measurement of the thickness/volume of cartilage is needed to aid in the diagnosis of early OA.30,33 Compositional MRI analysis has been performed in MMPRTs, and localized compositional changes in cartilage were observed in the weightbearing regions 6 months after partial meniscectomy, suggesting that the loading environment has been altered enough to result in early cartilage degeneration in a very brief period of time. 34
To date, there are limited clinical studies on cartilage degradation and OA progression based on semiquantitative and quantitative MRI evidence in patients with MMPRTs after meniscal root repairs via fixation to the PCL. Therefore, our purpose was to investigate medial meniscus extrusion (MME), the local cartilage changes and BMLs in MMPRTs after meniscal root repair, and partial meniscectomy according to MRI-based WORMS system; to compare the postoperative quantitative measurement of cartilage thickness/volume between different treatments in MMPRTs; and to determine the effects of different treatments on cartilage composition using T2 relaxation time mapping. It is hypothesized that trans-PCL all-inside repair could decrease articular cartilage degeneration and prevent OA progression with less cartilage damage and BMLs, increased cartilage thickness volume, and improved compositional outcomes compared with partial meniscectomy.
Methods
Study Design
The study was approved by the Institutional Review Board of Peking University People’s Hospital. A retrospective review was performed on patients with isolated MMPRTs who underwent trans-PCL all-inside repair and partial meniscectomy at our institutions from 2015 to 2018. An MMPRT was defined as avulsion injuries or radial tears located within 10 mm of the meniscal attachment or a bony root avulsion. 35 The inclusion criteria for the study were as follows: (1) isolated complete medial meniscal posterior root tears confirmed by arthroscopy, (2) Kellegren-Lawrence (K-L) grade ≤2, and (3) Outerbridge grade ≤3 based on arthroscopy. The exclusion criteria were as follows: (1) concomitant multiple ligament injuries or lateral meniscus tears, (2) imaging evidence of arthritis or local full-thickness cartilage injury, and (3) additional operative procedures such as microfracture and osteochondral autograft transplantation.
Trans-PCL all-inside repair was performed in patients (1) who had meniscal posterior roots suitable for performing refixation and (2) who are willing to follow a rehabilitation distinctly required after repair surgery. Patients received partial meniscectomy if they did not meet any of the above criteria. 36 All arthroscopic surgeries were performed by the senior orthopedic surgeon (T.S.). Patient demographics (sex, age, and body mass index [BMI]) and surgical details (history of knee surgery, side of knee injury, root tear location, mechanism of injury, K-L grade, knee alignment, and follow-up time) were recorded and compared between the 2 groups.
Surgical Technique
Standard anteromedial and anterolateral arthroscopic portals were established. Routine arthroscopic examinations were performed, and the diagnosis of isolated MMPRTs was reconfirmed with a probe. All-inside repair was performed with a suture device (FasT-FixTM 360 Meniscal Repair System; Smith & Nephew, Endoscopic Division) by suturing the medial meniscal posterior root to the adjacent PCL fibers ( Fig. 1 ). Partial meniscectomy was performed with biters and a 4.5-mm shaver, and the torn meniscus were debrided back to a stable and smooth base. The resection range was determined according to the tear type, tear location, and quality of meniscal tissue.
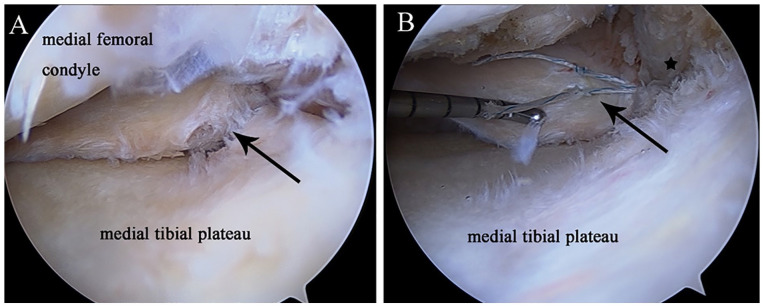
Figure 1.
Arthroscopic pictures with a 30° arthroscope through the anterolateral portal showing medial meniscus posterior root tear refixation to the adjacent posterior cruciate ligament by the all-inside repair technique. (A) Black arrow: complete radial tear of medial meniscus posterior root; (B) black star: posterior cruciate ligament; black arrow: the torn meniscus root was refixed to the adjacent posterior cruciate ligament fibers. Confirmation of improved meniscal tension and stability after refixation by probing.
Postoperative Rehabilitation
All patients were required to avoid deep squats. For the patients with all-inside repair, a 3-month walking assistant and protection of the knee by braces were necessary after surgery. In the initial 4 weeks, the knee joint was immobilized with the knee brace locked in full extension. The range of motion of the knee joint started at 30° at least 4 weeks after surgery and increased by 30° per week. Full weightbearing and progressive closed kinetic chain strengthening exercises were allowed at 3 months after surgery. For the patients with partial meniscectomy, partial weightbearing and range of motion were allowed immediately postoperatively within a tolerable range, and full weightbearing and progressive closed kinetic chain strengthening exercises were allowed at 1 month after surgery. For all patients, returning to sports was allowed at 6 months.
Clinical Evaluation
Patient-reported outcomes were collected at baseline and final follow-up, and included the Lysholm scores and International Knee Documentation Committee (IKDC) Subjective Knee Form criteria.
MRI Evaluation
MRI evaluation was performed in all patients at baseline and final follow-up. MRI was performed using a 1.5-T imager (Magnetom Tim Trio; Siemens Medical Solutions, Erlangen, Germany) with a transmit-receive quadrature knee coil. The imaging protocol included sagittal T1-weighted spin echo sequence (TR/TE, 400/9.4 ms; field of view[FOV],180 mm; matrix size, 320 × 224; slice thickness, 4.0 mm); sagittal, coronal, axial proton-density-weighted fat-saturated sequence (TR/TE 2,500/40 ms; FOV, 180 mm; matrix size, 320 × 224; slice thickness, 4.0 mm); and 3-dimensional (3D) double-echo steady state (DESS) (TR/TE 19.44/7.02 ms; FOV, 160 mm; matrix size, 320 × 224; slice thickness, 1.0 mm) which was used to create cartilage 3D models and sagittal 2-dimensional dual-echo fast spin echo (FSE) sequence (TR/TE, 1,000/13.8, 27.6, 41.4, 55.2, 69.0 ms; FOV, 160 mm; matrix size, 320 × 214; slice thickness, 3 mm) which was used for measuring T2 relaxation times.
The WORMS28,37 was used as a semiquantitative tool to evaluate osteoarthritic degeneration (including cartilage defects, BMLs, and synovitis) of the joint at baseline and follow-up. In addition, the medial femur (MF) was divided into 2 articular subregions (central, MFc; posterior, MFp), and the medial tibia (MT) was divided into 3 subregions (anterior, MTa; central, MTc; posterior, MTp) for further accurate assessment of cartilage damage and BMLs. Region of interest (ROI) segmentation and specific semiquantitative evaluation for cartilage degeneration of KOA have been described in previous studies.28,37 MME was defined as the distance from the medial edge of the MT plateau to the peripheral edge of the medial meniscus at the level of the medial collateral ligament in coronal imaging 36 ( Fig. 2 ). The correlation between the progression of WORMS-cartilage scores and the severity of MME (patients with MME <3 mm or MME ≥3 mm) in all patients postoperatively was evaluated.
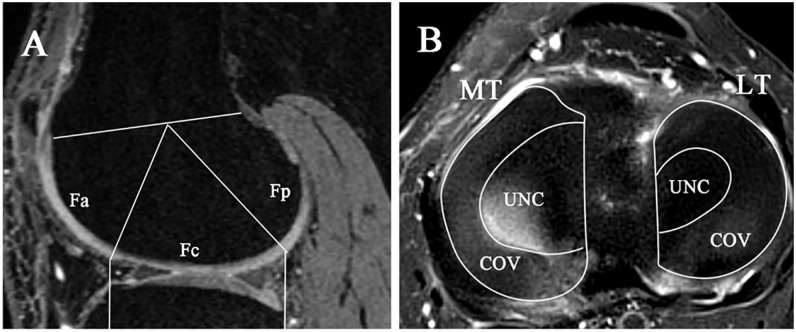
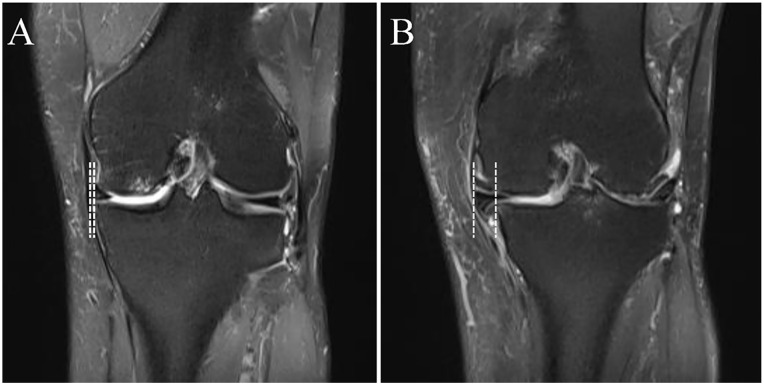
Figure 2.
Measurement of medial meniscus extrusion. Medial meniscus extrusion was measured from the tangent perpendicular to the medial tibial edge and the lateral edge of the medial meniscus on coronal MRI at the level of the medial collateral ligament.
Healing after meniscal repair was classified as complete, partial, and failed healing. Complete healing was defined as confirmed continuity in all 3 (sagittal, coronal, and axial) MRI views, whereas partial healing was defined as a loss of continuity in any 1 view, and failed healing was defined as no continuity in any view. 38 The correlation between the progression of the WORMS-cartilage scores and the healing status of meniscus in group AR was evaluated.
The results were evaluated by an orthopedic surgeon (J.S.) and a radiologist (H.W.) separately with the picture archiving and communication system (MME: intraclass correlation coefficient [ICC] >0.80; WORMS-cartilage scores: κ >0.80).
Morphological MRI Evaluation
Cartilage volume and thickness assessed by MRI have been regarded as important quantitative markers of knee osteoarthritic status.29,30,33,39 The DESS DICOM data were analyzed in Mimics (Materialize Interactive Medical Image Control System; 26.0) software. Slice by slice, the profiles of the patellar, femoral and tibial cartilage were outlined manually. The cartilage profiles were automatically rendered to create polygon-based 3D surface models by Mimics. The model was then divided into subregions for further volume and thickness analysis based on previous studies.40,41 The articular cartilage of the knee was segmented into patellar, trochlear, medial femoral, lateral femoral, medial tibial, and lateral tibial subregions. The medial and lateral femoral condyles were further segmented into anterior, central, and posterior subregions. The central region, regarded as the weightbearing region during the stance phase of gait, was defined relative to the anterior and posterior aspects of the proximal tibia (at the margin of the tibial plateau). The medial and lateral tibial subregions were further segmented into the regions uncovered and covered by the meniscus ( Fig. 3 ). The volume and thickness of each subregion were then automatically calculated by the software.
Figure 3.
Definition of the regions for analysis of cartilage volume in the femoral condyles and tibial plateau. (A) The medial and lateral femoral condyles were further segmented into anterior (Fa), central (Fc), and posterior (Fp) subregions. The central region was defined relative to the anterior and posterior aspect of the proximal tibia (at the margin of the tibial plateau). (B) The medial and lateral tibial subregions were further segmented into the regions uncovered (UNC) and covered by the meniscus (COV). MT = medial tibia; LT = lateral tibia.
The volume and thickness were normalized based on the distance of the medial and lateral femoral condyles. The normalized volume V = Vn × (Davg/Dn) 3 ; the normalized thickness T = Tn × (Davg/Dn). All subjects were segmented again over a 2-week period to evaluate intrarater reliability of this technique, which was found to be excellent (ICC >0.85).
Compositional MRI Evaluation
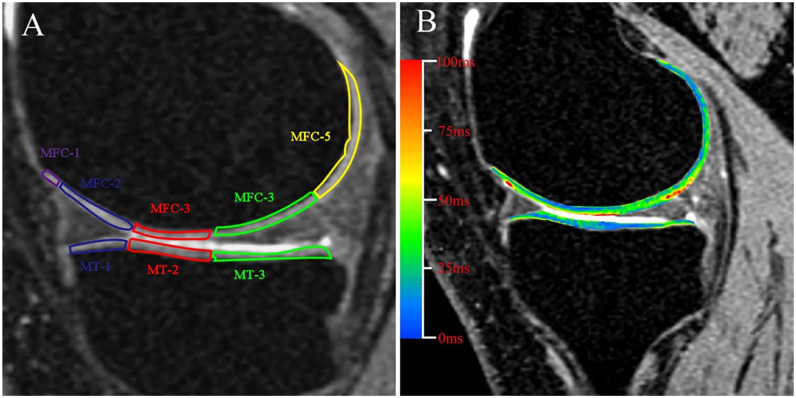
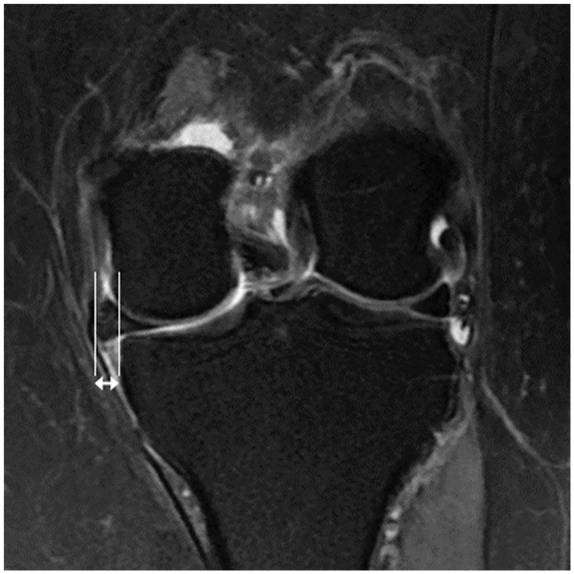
Cartilage degeneration is commonly defined as the central hallmark of OA. Alterations in the ECM, such as destruction of the collagen network and proteoglycans, characterize the early stages of cartilage degeneration, so T2 mapping shows an increase in the T2 relaxation times of cartilage.25,31,42-45 The medial femoral condyle (MFC) and MT were segmented manually into 5 and 3 subregions, respectively, according to the meniscus. Next, each subregion was assessed by further segmenting full-thickness cartilage into 2 approximately equal sections: a deep zone extending from the subchondral bone to the center of the tissue to encompass the bottom half of the tissue thickness, and a superficial zone extending from the center to the articular surface. MRI slice selection and ROI segmentation were manually performed by one experienced person (J.S.) according to the published methods43,46 ( Fig. 4 ). Mean T2 mapping values for each cartilage ROI were recorded for analysis. To reduce artifacts caused by partial volume effects with synovial fluid, pixels with relaxation times greater than 160 ms T2 maps were removed from the data used for quantification.
Figure 4.
(A) Regions of interest (ROI) segmentation of the medial tibiofemoral compartment. The MFC and MT were segmented manually into 5 and 3 subregions, respectively, according to the meniscus. Each subregion was assessed by further segmenting full-thickness cartilage into 2 approximately equal sections. MFC-3 and MT-2 are contacting regions of femoral and tibial cartilage during standing. MFC-2, MFC-4 and MT-1, MT-3 are regions above and below the meniscal horn, respectively. MFC-1 and MFC-5 are non-weightbearing portions of the femoral condyle during standing. T2 mappings of the MMPRTs after surgery. (B) Mean T2 values from superficial and deep layers in each defined subregions, as shown in (A), were recorded. MFC = medial femoral condyle; MT = medial tibia; MMPRTs = medial meniscus posterior root tears.
The compositional MRI outcomes were all evaluated by 2 orthopedic surgeons (J.S. and Y.P.), and the interobserver reliability of this method was found to be excellent (ICC >0.80).
Statistical Analysis
All data analyses were conducted in IBM SPSS Statistics (SPSS Inc., version 25.0) with significance determined to be P = 0.05. Distribution of continuous variables was assessed by the Shapiro-Wilk test. For normally distributed continuous variables, the independent t test was performed. For skewed distributed variables, the Mann-Whitney test was performed. Person’s χ2 test was used to compare unordered categorical variables, and if more than 20% of the expected frequencies were less than 5, a Fisher exact test was used. For ordered categorical variables, the Mann-Whitney test was used. The Pearson correlation coefficient was performed to determine the correlation between the severity of MME and cartilage damage, as well as the meniscus healing score and cartilage damage.
Results
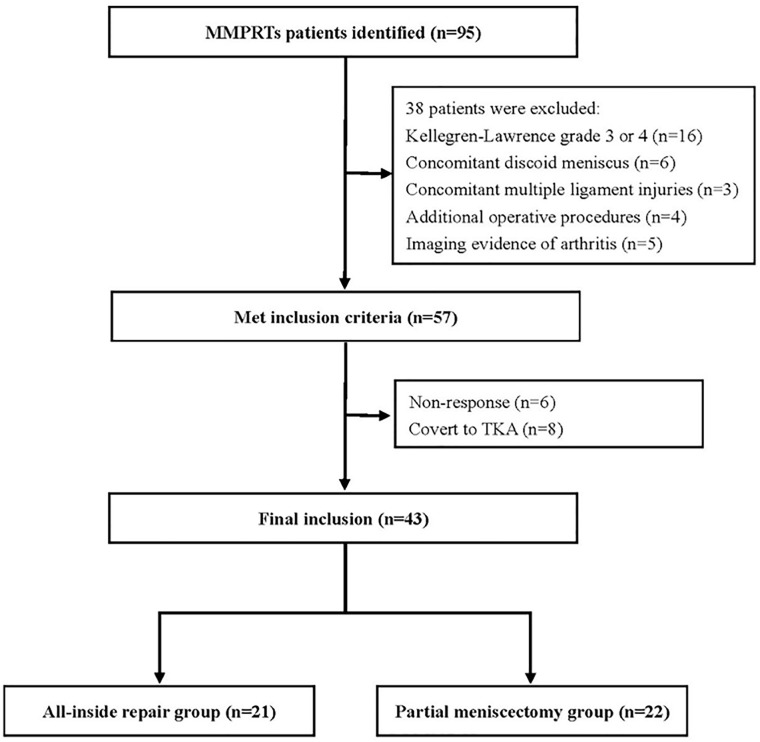
A total of 95 patients with MMPRTs who underwent trans-PCL all-inside repair or partial meniscectomy were screened from 2015 to 2018; of them, 57 patients were included in the study according to the inclusion and exclusion criteria. Six patients did not respond at final follow-up and 8 patients converted to TKA; thus, 21 patients in group AR and 22 patients in group PM were available for follow-up at an average of 3.70 ± 1.21 years ( Fig. 5 ). Neither the preoperative demographic data nor the patient characteristics differed significantly between the groups ( Table 1 ).
Figure 5.
Flowchart of included participants. MMPRTs = medial meniscus posterior root tears; TKA = total knee arthroplasty.
Table 1.
Demographic Data and Basic Characteristics at Baseline.
| Group AR (n = 21) | Group PM (n = 22) | P Value | |
|---|---|---|---|
| Age (y) | 62.05 ± 9.12 | 57.77 ± 9.5 | 0.140 |
| Sex (male/female, n) | 4/17 | 2/20 | 0.616 |
| Side (left/right, n) | 12/9 | 12/10 | 0.846 |
| BMI (kg/m2) | 26.25 ± 2.56 | 25.59 ± 2.51 | 0.400 |
| Duration from injury to surgery (mo) | 3.17 ± 2.56 | 3.05 ± 2.20 | 0.893 |
| Duration from baseline MRI to surgery (mo) | 1.46 ± 1.00 | 1.31 ± 1.27 | 0.274 |
| Follow-up time (y) | 3.54 ± 1.11 | 3.86 ± 1.31 | 0.398 |
| MF-Outerbridge grade | 2 (1;2) | 2 (1;3) | 0.153 |
| MT-Outerbridge grade | 1 (1;2) | 1 (1;2) | 0.254 |
| Lysholm | 38.76 ± 14.51 | 39.41 ± 15.63 | 0.990 |
| IKDC | 24.13 ± 9.95 | 26.66 ± 10.65 | 0.355 |
| K-L grade | 1 (1;1.5) | 1 (1;2) | 0.141 |
| MME (mm) | 3.28 ± 1.06 | 3.44 ± 1.22 | 0.981 |
| WORMS-cartilage morphological score | |||
| MFc | 1 (0;2) | 2 (0.75;2) | 0.119 |
| MFp | 0 (0;1) | 0 (0;1) | 1.000 |
| MTa | 0 (0;1) | 0 (0;0) | 0.313 |
| MTc | 0 (0;1) | 0 (0;1) | 0.377 |
| MTp | 0 (0;1) | 0 (0;0) | 0.065 |
| WORMS-BML score | |||
| MFc | 0 (0;1) | 0 (0;0) | 0.261 |
| MFp | 0 (0;0) | 0 (0;0) | 1.000 |
| MTa | 0 (0;0) | 0 (0;0) | 0.527 |
| MTc | 0 (0;0) | 0 (0;0) | 0.527 |
| MTp | 0 (0;0) | 0 (0;0) | 1.000 |
| WORMS-synovitis | 0 (0;2) | 1 (0;1.5) | 0.832 |
Continuous variables are expressed as mean ± SD and categorical variables as median (interquartile range) or n (%)
AR = all-inside repair; PM = partial meniscectomy; BMI = body mass index; MF = medial femoral condyle; MT = medial tibia; IKDC = International Knee Documentation Committee; K-L grade = Kellgren-Lawrence grade; MME = medial meniscus extrusion; WORMS = Whole-Organ Magnetic Resonance Imaging Score; c = central; p = posterior; a = anterior; BML = bone marrow lesion.
Patient-Reported Outcomes
Baseline patient-reported outcomes showed no significant differences between the AR and PM groups with respect to the Lysholm and IKDC ( Table 1 ). The patient-reported outcomes in both groups were significantly improved from baseline to the final follow-up (P < 0.001) ( Table 2 ). Regarding the results at the final follow-up, no significant differences were seen between the groups ( Table 3 ).
Table 2.
Within-Group Changes in WORMS From Baseline to Follow-Up.
| Group AR (n = 21) | P Value | Group PM (n = 22) | P Value | |||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | |||
| Lysholm | 38.76 ± 14.51 | 86.67 ± 7.88 | <0.001 a | 39.41 ± 15.63 | 82.55 ± 15.98 | <0.001 a |
| IKDC | 24.13 ± 9.95 | 73.7 ± 7.63 | <0.001 a | 26.66 ± 10.65 | 71.37 ± 16.33 | <0.001 a |
| MME (mm) | 3.28 ± 1.06 | 3.62 ± 1.52 | 0.144 | 3.44 ± 1.22 | 5.03 ± 1.48 | 0.001 a |
| WORMS-cartilage morphological score | ||||||
| MFc | 1 (0;2) | 1 (0;2.25) | 0.016 a | 2 (0.75;2) | 4 (1.5;5) | 0.001 a |
| MFp | 0 (0;1) | 1 (0;1) | 0.197 | 0 (0;1) | 1 (0;1.25) | 0.010 a |
| MTa | 0 (0;1) | 0 (0;1) | 0.046 a | 0 (0;0) | 0.5 (0;2) | 0.010 a |
| MTc | 0 (0;1) | 0 (0;1) | 0.041 a | 0 (0;1) | 1.5 (0;4) | 0.002 a |
| MTp | 0 (0;1) | 0 (0;1) | 1.000 | 0 (0;0) | 1 (0;2.25) | 0.003 a |
| WORMS-BML score | ||||||
| MFc | 0 (0;1) | 0 (0;1) | 0.206 | 0 (0;0) | 1 (0;2) | 0.004 a |
| MFp | 0 (0;0) | 0 (0;0) | 0.157 | 0 (0;0) | 0 (0;0) | 0.059 |
| MTa | 0 (0;0) | 0 (0;0) | 0.414 | 0 (0;0) | 0 (0;1.25) | 0.017 a |
| MTc | 0 (0;0) | 0 (0;0.5) | 0.157 | 0 (0;0) | 0 (0;2) | 0.019 a |
| MTp | 0 (0;0) | 0 (0;0) | 0.157 | 0 (0;0) | 0 (0;0) | 0.102 |
| WORMS-synovitis | 0 (0;2) | 1 (0;1) | 0.227 | 1 (0;1.5) | 0 (0;1) | 1.000 |
Categorical variables are expressed as median (interquartile range) or n (%).
WORMS = Whole-Organ Magnetic Resonance Imaging Score; AR = all-inside repair; PM = partial meniscectomy; IKDC = International Knee Documentation Committee; MME = medial meniscus extrusion; MF = medial femoral condyle; c = central; p = posterior; MT = medial tibia; a = anterior; BML, bone marrow lesion.
Significant at the level of P < .05.
Table 3.
Comparison of Postoperative MRI Outcomes Between Groups at the Final Follow-Up.
| Repair (n = 21) | Menisectomy (n = 22) | P Value | |
|---|---|---|---|
| Lysholm | 86.67 ± 7.88 | 82.55 ± 15.98 | 0.855 |
| IKDC | 73.70 ± 7.63 | 71.37 ± 16.33 | 0.865 |
| MME (mm) | 3.62 ± 1.52 | 5.03 ± 1.48 | 0.008 a |
| MME ≥3 mm, n (%) | 12 (57.14) | 21 (95.45) | |
| WORMS-cartilage morphological score | |||
| MFc | 1 (0;2.25) | 4 (1.5;5) | 0.003 a |
| MFp | 1 (0;1) | 1 (0;1.25) | 0.193 |
| MTa | 0 (0;1) | 0.5 (0;2) | 0.226 |
| MTc | 0 (0;1) | 1.5 (0;4) | 0.009 a |
| MTp | 0 (0;1) | 1 (0;2.25) | 0.038 a |
| WORMS-BML score | |||
| MFc | 0 (0;1) | 1 (0;2) | 0.222 |
| MFp | 0 (0;0) | 0 (0;0) | 0.396 |
| MTa | 0 (0;0) | 0 (0;1.25) | 0.078 |
| MTc | 0 (0;0.5) | 0 (0;2) | 0.372 |
| MTp | 0 (0;0) | 0 (0;0) | 0.646 |
| WORMS-synovitis score | 1 (0;1) | 0 (0;1) | 0.230 |
| Changes in cartilage (progression/no change, n) | |||
| MFc | 8/13 | 15/7 | 0.048 a |
| MFp | 3/18 | 8/14 | 0.097 |
| MTa | 4/17 | 9/13 | 0.119 |
| MTc | 5/16 | 13/9 | 0.019 a |
| MTp | 2/19 | 11/11 | 0.004 a |
| Changes in BML (progression/no change, n) | |||
| MFc | 5/16 | 10/12 | 0.137 |
| MFp | 2/19 | 4/18 | 0.705 |
| MTa | 2/19 | 7/15 | 0.155 |
| MTc | 4/17 | 7/15 | 0.337 |
| MTp | 2/19 | 3/19 | 1.000 |
Continuous variables are expressed as mean ± SD and categorical variables as median (interquartile range) or n (%).
IKDC = International Knee Documentation Committee; MME = medial meniscus extrusion; WORMS = Whole-Organ Magnetic Resonance Imaging Score; MF = medial femoral condyle; c = central; p = posterior; MT = medial tibia; a = anterior; BML = bone marrow lesion.
Significant at the level of P < .05.
Conventional MRI Evaluation
Conventional MRI was performed in all patients. For group PM, significant increases of WORMS-cartilage morphological scores were observed in all subregions (P < 0.05) and BML progression was found in MFc (P = 0.004), MTa (P = 0.017), and MTc (P = 0.019) ( Table 2 ). For group AR, significant increases in WORMS-cartilage morphological scores only in MFc (P = 0.016), MTa (P = 0.046), and MTc (P = 0.041) were noted from baseline to follow-up; however, no significant differences were seen in WORMS-BML scores. Between-group analysis at final follow-up indicated that cartilage morphology scores in group AR were better than group PM in MFc (P = 0.003), MTc (P = 0.009), and MTp (P = 0.038). There were no significant differences in BML scores and synovitis scores between the groups ( Table 3 ).
The average MME significantly increased from baseline (3.44 ± 1.22 mm) to final follow-up (5.03 ± 1.48 mm) (P = 0.001) in group PM, and no significant differences were seen in group AR ( Table 2 ; Fig. 6 ). A total of 57.14% of patients in group AR and 95.45% of patients in group PM showed severe MME postoperatively. In addition, group AR (3.62 ± 1.52 mm) showed less MME compared with group PM (5.03 ± 1.48 mm) (P = 0.008) ( Table 3 ). Moreover, the correlation between the severity of MME and the progression of cartilage damage was examined in all patients postoperatively. The severity of MME and cartilage damage were weakly correlated in MTc (r = 0.356; P < 0.05) ( Table 4 )
Figure 6.
Coronal MRI at the final follow-up. (A) MRI of patient with trans-posterior cruciate ligament all-inside repair demonstrating medial meniscus extrusion (1.29 mm). (B) MRI of patient with partial meniscectomy demonstrating medial meniscus extrusion (8.70 mm).
Table 4.
Correlation of MME, Meniscal Healing Status, and Progression of WORMS-Cartilage Morphological Scores.
| Changes in Cartilage | MME | Meniscus Healing Status | ||
|---|---|---|---|---|
| r | P Value | P Value | ||
| MFc | 0.259 | 0.093 | −0.503 | 0.020 a |
| MFp | 0.197 | 0.206 | −0.203 | 0.378 |
| MTa | 0.243 | 0.117 | −0.522 | 0.015 a |
| MTc | 0.356 | 0.019 a | −0.213 | 0.354 |
| MTp | 0.123 | 0.433 | 0.215 | 0.350 |
MME = medial meniscus extrusion; WORMS = Whole-Organ Magnetic Resonance Imaging Score; MF = medial femoral condyle; c = central; p = posterior; MT = medial tibia; a = anterior.
Significant at the level of P < .05.
Meniscal healing status was assessed in group AR, 15 patients showed complete healing, 5 patients showed partial healing, and 1 patient showed failed healing. In addition, a negative correlation between the meniscus healing status and progression of cartilage damage in MFc and MFa was found (r = −0.503 and r = −0.522, respectively; P < 0.05) ( Table 4 ).
Morphological MRI Evaluation
Postoperative morphological MRI evaluation was performed in all patients. Intergroup analysis was performed, and no significant difference was seen in cartilage volume or thickness of each subregion of articular cartilage between AR and PM groups ( Table 5 ).
Table 5.
Comparison of Postoperative Morphological MRI Outcomes Between Groups at the Final Follow-Up.
| Cartilage Volume | Cartilage Thickness | |||||
|---|---|---|---|---|---|---|
| Group AR (n = 21) | Group PM (n = 22) | P Value | Group AR (n = 21) | Group PM (n = 22) | P Value | |
| Pa | 2,040.25 ± 922.18 | 1,829.79 ± 676.13 | 0.397 | 1.83 ± 0.41 | 1.76 ± 0.36 | 0.588 |
| TR | 1,423.71 ± 533.41 | 1,304.05 ± 659.64 | 0.518 | 1.67 ± 0.26 | 1.75 ± 0.43 | 0.482 |
| MFa | 905.93 ± 373.57 | 891.68 ± 431.36 | 0.680 | 1.65 ± 0.32 | 1.65 ± 0.33 | 0.697 |
| MFc | 1,625.55 ± 601.84 | 1,490.83 ± 494.7 | 0.594 | 1.31 ± 0.24 | 1.34 ± 0.14 | 0.426 |
| MFp | 1,665.17 ± 528.19 | 1,589.34 ± 433.71 | 0.609 | 2.02 ± 0.31 | 2.09 ± 0.36 | 0.491 |
| LFa | 1,403.65 ± 619.62 | 1,318.00 ± 475.39 | 0.613 | 1.81 ± 0.36 | 1.8 ± 0.37 | 0.920 |
| LFc | 1,859.66 ± 493.99 | 1,924.48 ± 592.64 | 0.304 | 1.32 ± 0.24 | 1.29 ± 0.24 | 0.700 |
| LFp | 1,206.42 ± 300.42 | 1,111.94 ± 314.13 | 0.320 | 1.44 ± 0.2 | 1.52 ± 0.28 | 0.734 |
| MTco | 640.92 ± 310.53 | 699.51 ± 312.8 | 0.541 | 1.02 ± 0.25 | 1.14 ± 0.31 | 0.152 |
| MTunco | 1,108.59 ± 328.78 | 1,194.5 ± 520.47 | 0.771 | 1.54 ± 0.27 | 1.6 ± 0.36 | 0.555 |
| LTco | 961.81 ± 323.18 | 969.96 ± 355.08 | 0.593 | 1.42 ± 0.33 | 1.5 ± 0.38 | 0.644 |
| LTunco | 871.72 ± 383.24 | 703.57 ± 393.42 | 0.080 | 1.67 ± 0.32 | 1.55 ± 0.38 | 0.285 |
Values are expressed as mean ± SD.
AR = all-inside repair; PM = partial meniscectomy; Pa = patella; TR = trochlea; MF = medial femoral condyle; a = anterior; c = central; p = posterior; LF = lateral femoral condyle; MT = medial tibia; co = covered by the meniscus; unco = uncovered by the meniscus; LT: lateral tibia.
Compositional MRI Evaluation
Postoperative compositional MRI (T2 mapping) was performed in 28 patients (17 patients in group AR and 11 patients in group PM), and patients with severe morphological cartilage damage (4 patient in group AR and 11 in group PM with WORMS-Cartilage Morphological grades 4-6) were excluded from further compositional MRI evaluation. For the superficial layer of the cartilage, group AR showed lower T2 relaxation times in MFC-3 (P = 0.033) and MT-2 (P = 0.010) than group PM. In terms of the deep layer, there was no significant difference between the 2 groups ( Table 6 ).
Table 6.
Comparison of T2 Mapping Compositional MRI Outcomes Between the AR and PM Groups at Final Follow-Up.
| Superficial Layer | Deep Layer | |||||
|---|---|---|---|---|---|---|
| Group AR (n = 17) | Group PM (n = 11) | P Value | Group AR (n = 17) | Group PM(n = 11) | P Value | |
| MFC-1 | 38.71 ± 13.73 | 41.57 ± 16.94 | 0.628 | 23.78 ± 9.83 | 25.81 ± 11.82 | 0.627 |
| MFC-2 | 44.01 ± 9.98 | 44.15 ± 18.71 | 0.980 | 21.74 ± 7.48 | 22.30 ± 6.30 | 0.838 |
| MFC-3 | 44.10 ± 8.47 | 56.93 ± 16.51 | 0.033 a | 13.66 ± 3.02 | 15.48 ± 6.22 | 0.308 |
| MFC-4 | 45.10 ± 10.00 | 51.05 ± 15.36 | 0.224 | 15.19 ± 3.82 | 17.15 ± 5.04 | 0.253 |
| MFC-5 | 48.21 ± 9.57 | 52.75 ± 9.23 | 0.225 | 18.92 ± 5.81 | 21.26 ± 5.28 | 0.291 |
| MT-1 | 29.68 ± 10.12 | 36.49 ± 15.49 | 0.170 | 16.85 ± 6.83 | 14.81 ± 3.38 | 0.305 |
| MT-2 | 32.87 ± 6.99 | 44.71 ± 11.91 | 0.010 a | 12.00 ± 2.70 | 11.65 ± 1.79 | 0.708 |
| MT-3 | 40.67 ± 5.77 | 51.26 ± 17.29 | 0.074 | 16.59 ± 6.06 | 14.78 ± 3.26 | 0.373 |
Values are expressed as mean ± SD.
AR = all-inside repair; PM = partial meniscectomy; MFC = medial femur condyle; MT = medial tibia.
Significant at the level of P < 0.05.
Discussion
The most important finding of the current study was that medial meniscus posterior root repair via fixation to the PCL (group AR) demonstrated better WORMS-cartilage morphology scores in the weightbearing subregions of medial compartment than partial meniscectomy (group PM). For patients with non-osteoarthritic cartilage, group AR showed lower T2 relaxation times in the cartilage-to-cartilage subregions (MFC-3, MT-2) than group PM, which suggests that trans-PCL all-inside repair could protect the cartilage against localized degeneration compared with partial meniscectomy.
Arthroscopic transtibial pullout suture technique and anchor refixation are the common techniques to repair MMPRTs. Biomechanical and clinical studies have shown that these repairs could restore the integrity and biomechanical function of the meniscus, preventing cartilage degeneration and the progression of OA in short and mid-term.11,14,17 However, these repair techniques require accurate anatomical placement of the meniscal root, as even a 5-mm error in placement has been associated with increased joint contact loads. 47 In addition, it can be technically difficult to determine the anatomic position of the posterior horn of the medial meniscus, particularly if the meniscal root tear has scarred against the capsule, retracted, or extruded posteromedially.48,49 Given the proximity of the medial meniscal posterior to the most proximal PCL tibial attachment (which was directly 8.2 mm from the medial posterior root attachment center 50 ), all-inside repair via suture fixation to the PCL could provide an analog to the Wrisberg ligament with the potential for decreased technical difficulty, increased speed, and fewer surgical incisions as compared with other treatment options. Saltzman et al. 16 reported that the all-inside repair of MMPRTs via suture fixation to the PCL was able to restore the contact area, contact pressures, and peak contact pressures to that of the intact knee in human cadaver.
The medial meniscus posterior root has been shown to be a biomechanically integral structure that prevents the development of OA.6,8 MMPRTs have been associated with the development of OA of the far posterior femoral condyle. 6 Previous clinical studies have demonstrated that nonoperative management and partial meniscectomy for complete MMPRTs provide no benefit in halting arthritis with poor clinical and radiographic outcomes, as well as a high arthroplasty rate at 5-year follow-up.12,13 To restore the anchoring structure of the meniscal horn and prevent post-traumatic OA, arthroscopic repair was proven to be an effective technique in MMPRT patients with satisfactory clinical outcomes and a lower rate of TKA.17-21 However, just demonstrating the clinical and radiographic results without MRI evaluation, these studies could not provide an accurate and comprehensive assessment of osteoarthritic progression in MMPRT after surgery. Thus, our study fills this gap in MMPRT research with semiquantitative and quantitative MRI assessments to provide a visualization of OA changes in the whole-joint organ.
The protective effect of meniscal root repair on cartilage in patients with MMPRTs is dependent on MME and meniscus healing status. 51 With the re-establishment of integrity and hoop tension of the medial meniscus root, trans-PCL all-inside repair (group AR) could prevent cartilage damage and degeneration to some degree compared with partial meniscectomy (group PM). Group AR showed less MME than group PM. There was a weak correlation between the severity of MME and cartilage degeneration in MTc. The postoperative MME in 57% patients with trans-PCL all-inside repair is still greater than 3 mm. The amount of residual meniscal extrusion is clinically important, which is associated with a loss of medial compartment cartilage volume and progression of OA. 52 Thus, the MMPRTs with less MME should be repaired as soon as possible once the diagnosis was made, and an improved root repair fixation method should be investigated. The healing status of the torn meniscus is also a crucial factor in cartilage protection in meniscal repair. Kodama et al. 22 demonstrated that there was a negative correlation between high meniscus healing scores and International Cartilage Repair Society (ICRS) grades in the medial compartment loading area. In our study, 65.21% of patients in group AR showed compete meniscal healing, and a negative correlation between the meniscus healing status and progression of cartilage damage in MFc and MFa was found. Therefore, cartilage degeneration in some patients with meniscal repair might be due to the poor healing status of medial meniscus roots and progression of MME.
Considered as the essential part of OA, cartilage is the most-commonly assessed structure in quantitative MRI of OA research.29,30,33,39 Previous studies have reported that cartilage thickness decreased in the medial load-bearing regions primarily between K-L grade 2 and K-L grade 3 radiographic stages, 29 while it increased in the posterior aspect of femoral condyles throughout the disease due to anabolic processes initiated in reaction to OA. 30 However, Reichenbach et al. 33 reported that quantitative measurement of cartilage volume and thickness did not distinguish focal cartilage loss in mild OA from non-OA, which could be detected by experienced readers applying semiquantitative methods. 33 Similarly, no significant differences were seen in quantitative cartilage volume/thickness measurement evaluation between the AR and PM groups in our study, as distinguished changes between the groups in the semiquantitative MRI assessment of cartilage damage have been found. There were two reasons that could explain the findings. First, the entire full-layer cartilage damage did not occur in the majority of patients with mild OA after surgery, and small areas of focal damage in cartilage may not be picked up manually by quantitative measures that describe the entire cartilage plates. Cartilage swelling has been shown in animal models to be a feature of early stages of experimental OA. 53 Swelling of cartilage surrounding cartilage defects could negate the effect of focal losses on quantitative measurements that sum cartilage morphometry over a large region. Therefore, quantitative measures are not very sensitive to the degeneration of cartilage, and semiquantitative MRI tools, such as WORMS and MOAKS (MRI Osteoarthritis Knee Score), are more suitable for the evaluation of cartilage lesions in early OA.
In the compositional MRI analysis, group AR showed lower T2 relaxation times in the cartilage subregions (MFC-3, MT-2) than group PM. Previous studies have proven that premorphological cartilage degeneration could be evaluated earlier by compositional MRI (T1rho or T2 mapping) in the absence of radiographic or conventional MRI evidence, indicating that T1rho or T2 mapping may serve as a premorphological marker of cartilage degeneration and early OA. 45 Kumar et al. 54 reported that individuals with MMPRTs are associated with increased T2 relaxation times in the deep cartilage layer of all compartments. Russell et al. 55 found that MMPRTs with non-osteoarthritic cartilage showed increased T1rho and T2 relaxation times when compared with patients with intact meniscus. They perceived cartilage degeneration with disruption of the collagen network in direct response to reduced load-sharing by the torn meniscus.54,55 Premorphological cartilage degeneration in the cartilage-on-cartilage region with elevated T2 relaxation times has been found in MMPRTs with meniscectomy. 34 An incremental decrease in contact area and a concomitant increase in peak contact stress that was proportional to the amount of meniscus resected put the articular cartilage into an “overloaded condition,” 56 and the ECM deterioration of overloaded cartilage has occurred.34,57,58 Moreover, an early laboratory study proved that histologic degeneration in articular cartilage was proportional to the amount of meniscus resected. 59 For trans-PCL all-inside repair, restoration of tibiofemoral contact mechanics has been demonstrated in current biomechanical studies. 16 Thus, we highlight that meniscectomy could not prevent degeneration of cartilage ECM with the debrided meniscus, while trans-PCL all-inside repair would be beneficial to the loading condition of articular cartilage and could protect articular ECM from early degeneration with reconstruction of the meniscal integrity.
Limitations
There are several limitations in this study. First, it is a nonrandomized, retrospective comparative study with a small sample size and short-term follow-up period. There may be selection bias during participant enrollment without a randomized procedure in which patients with irreparable meniscus who were excluded for repair would have more cartilage degeneration. Although most demographic and preoperative data were similar between the groups, it was difficult for us to match the cohorts perfectly with the small sample size. Second, the actual meniscal healing and restoration of hoop tension after surgery were not assessed because second-look arthroscopy was not performed. Third, the amount of postoperative MME in patients with trans-PCL all-inside repair is still greater than 3 mm, so the nonanatomic refixation technique could not rectify the meniscal extrusion completely and an improved root repair fixation method should be investigated in future studies. Fourth, preoperative quantitative morphological MRI and compositional MRI assessments were not performed, and longitudinal changes in both groups were not evaluated. Additional prospective randomized controlled studies with long-term follow-up, large sample sizes, and multiple assessment methods, allowing for a better understanding of longitudinal osteoarthritic progression, will be needed in the future to determine the mechanism of OA after medial meniscus posterior horn tears and guide future preventive treatments.
Conclusion
Trans-PCL all-inside repair of MMPRTs could delay the initial cartilage deterioration and morphological cartilage degeneration compared with partial meniscectomy. However, the amount of residual meniscal extrusion is clinically important, and an improved root repair fixation method should be investigated in future studies.
Footnotes
Acknowledgments and Funding: This study was funded by the Peking University People’s Hospital Research and Development Funds, Grant/Award Number: RDL2020-05.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: The study was approved by the Institutional Review Board of Peking University, People’s Hospital.
ORCID iD: Jiarong Su  https://orcid.org/0000-0003-2689-5810
https://orcid.org/0000-0003-2689-5810
References
- 1. Moatshe G, Chahla J, Slette E, Engebretsen L, Laprade RF. Posterior meniscal root injuries. Acta Orthop. 2016. Oct;87(5):452-8. doi: 10.1080/17453674.2016.1202945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Papalia R, Vasta S, Franceschi F, D’Adamio S, Maffulli N, Denaro V. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull. 2013;106:91-115. doi: 10.1093/bmb/ldt002. [DOI] [PubMed] [Google Scholar]
- 3. Smigielski R, Becker R, Zdanowicz U, Ciszek B. Medial meniscus anatomy-from basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015. Jan;23(1):8-14. doi: 10.1007/s00167-014-3476-5. [DOI] [PubMed] [Google Scholar]
- 4. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008. Sep;90(9):1922-31. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 5. Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Surgical technique. J Bone Joint Surg Am. 2009. Oct 1;91 Suppl 2:257-70. doi: 10.2106/JBJS.I.00500. [DOI] [PubMed] [Google Scholar]
- 6. Sebro R, Ashok SS, Uriell M. Association between tears of the posterior root of the medial meniscus and far posterior femoral condyle osteoarthritis. Diagn Interv Radiol. 2020. Jul;26(4):349-54. doi: 10.5152/dir.2019.19358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim JY, Bin SI, Kim JM, Lee BS, Oh SM, Park MH. Tear gap and severity of osteoarthritis are associated with meniscal extrusion in degenerative medial meniscus posterior root tears. Orthop Traumatol Surg Res. 2019. Nov;105(7):1395-9. doi: 10.1016/j.otsr.2019.09.015. [DOI] [PubMed] [Google Scholar]
- 8. Choi ES, Park SJ. Clinical evaluation of the root tear of the posterior horn of the medial meniscus in total knee arthroplasty for osteoarthritis. Knee Surg Relat Res. 2015. Jun;27(2):90-4. doi: 10.5792/ksrr.2015.27.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Han SB, Shetty GM, Lee DH, Chae DJ, Seo SS, Wang KH, et al. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010. Oct;26(10):1326-32. doi: 10.1016/j.arthro.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 10. Kim C, Bin SI, Kim JM, Lee BS, Kim TH. Progression of radiographic osteoarthritis after partial meniscectomy in degenerative medial meniscal posterior root tears was greater in varus- than in neutral-aligned knees: a minimum 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2020. Nov;28(11):3443-9. doi: 10.1007/s00167-020-05905-w. [DOI] [PubMed] [Google Scholar]
- 11. Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014. Mar;42(3):699-707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 12. Krych AJ, Reardon PJ, Johnson NR, Mohan R, Peter L, Levy BA, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017. Feb;25(2):383-9. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 13. Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2018. Apr;26(4):1117-22. doi: 10.1007/s00167-017-4454-5. [DOI] [PubMed] [Google Scholar]
- 14. Okimura S, Mae T, Tachibana Y, Iuchi R, Nakata K, Yamashita T, et al. Biomechanical comparison of meniscus-suture constructs for pullout repair of medial meniscus posterior root tears. J Exp Orthop. 2019. Apr 15;6(1):17. doi: 10.1186/s40634-019-0186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Faucett SC, Geisler BP, Chahla J, Krych AJ, Kurzweil PR, Garner AM, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019. Mar;47(3):762-9. doi: 10.1177/0363546518755754. [DOI] [PubMed] [Google Scholar]
- 16. Saltzman BM, Habet NA, Rao AJ, Trofa DP, Corpus KT, Yeatts NC, et al. Biomechanical evaluation of an all-inside posterior medial meniscal root repair technique via suture fixation to the posterior cruciate ligament. Arthroscopy. 2020. Sep;36(9):2488-97.e6. doi: 10.1016/j.arthro.2020.04.042. [DOI] [PubMed] [Google Scholar]
- 17. Chung KS, Noh JM, Ha JK, Ra HJ, Park SB, Kim HK, et al. Survivorship analysis and clinical outcomes of transtibial pullout repair for medial meniscus posterior root tears: a 5- to 10-year follow-up study. Arthroscopy. 2018. Feb;34(2):530-5. doi: 10.1016/j.arthro.2017.08.266. [DOI] [PubMed] [Google Scholar]
- 18. Dragoo JL, Konopka JA, Guzman RA, Segovia N, Kandil A, Pappas GP. Outcomes of arthroscopic all-inside repair versus observation in older patients with meniscus root tears. Am J Sports Med. 2020. Apr;48(5):1127-33. doi: 10.1177/0363546520909828. [DOI] [PubMed] [Google Scholar]
- 19. Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011. Dec;27(12):1644-53. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 20. Chung KS, Ha JK, Ra HJ, Yu WJ, Kim JG. Root repair versus partial meniscectomy for medial meniscus posterior root tears: comparison of long-term survivorship and clinical outcomes at minimum 10-year follow-up. Am J Sports Med. 2020. Jul;48(8):1937-44. doi: 10.1177/0363546520920561. [DOI] [PubMed] [Google Scholar]
- 21. LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017. Mar;45(4):884-91. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 22. Kodama Y, Furumatsu T, Okazaki Y, Takihira S, Hiranaka T, Miyazawa S, et al. Transtibial pullout repair of medial meniscus posterior root tears: effects on the meniscus healing score and ICRS grade among patients with mild osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2021. Oct 28;29:3001-9. doi: 10.1007/s00167-020-06332-7. [DOI] [PubMed] [Google Scholar]
- 23. Chung KS, Ha JK, Ra HJ, Lee HS, Lee DW, Park JH, et al. Pullout fixation for medial meniscus posterior root tears: clinical results were not age-dependent, but osteoarthritis progressed. Knee Surg Sports Traumatol Arthrosc. 2019. Jan;27(1):189-96. doi: 10.1007/s00167-018-5024-1. [DOI] [PubMed] [Google Scholar]
- 24. Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697-707. doi: 10.1002/art.34453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hayashi D, Roemer FW, Guermazi A. Imaging of osteoarthritis-recent research developments and future perspective. Br J Radiol. 2018. May;91(1085):20170349. doi: 10.1259/bjr.20170349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Culvenor AG, Øiestad BE, Hart HF, Stefanik JJ, Guermazi A, Crossley KM. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med. 2019. Oct;53(20):1268-78. doi: 10.1136/bjsports-2018-099257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Juras V, Chang G, Regatte RR. Current status of functional MRI of osteoarthritis for diagnosis and prognosis. Curr Opin Rheumatol. 2020;32(1):102-9. doi: 10.1097/BOR.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, et al. Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004. Mar;12(3):177-90. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 29. Edd SN, Omoumi P, Jolles BM, Favre J. Longitudinal femoral cartilage T2 relaxation time and thickness changes with fast sequential radiographic progression of medial knee osteoarthritis-data from the osteoarthritis initiative (OAI). J Clin Med. 2021. Mar 21;10(6):1294. doi: 10.3390/jcm10061294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Omoumi P, Babel H, Jolles BM, Favre J. Cartilage can be thicker in advanced osteoarthritic knees: a tridimensional quantitative analysis of cartilage thickness at posterior aspect of femoral condyles. Br J Radiol. 2018. Jul;91(1087):20170729. doi: 10.1259/bjr.20170729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Stahl R, Blumenkrantz G, Carballido-Gamio J, Zhao S, Munoz T, Hellio Le Graverand-Gastineau MP, et al. MRI-derived T2 relaxation times and cartilage morphometry of the tibio-femoral joint in subjects with and without osteoarthritis during a 1-year follow-up. Osteoarthritis Cartilage. 2007. Nov;15(11):1225-34. doi: 10.1016/j.joca.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 32. Wang L, Chang G, Xu J, Vieira RL, Krasnokutsky S, Abramson S, et al. T1rho MRI of menisci and cartilage in patients with osteoarthritis at 3T. Eur J Radiol. 2012. Sep;81(9):2329-36. doi: 10.1016/j.ejrad.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Reichenbach S, Yang M, Eckstein F, Niu J, Hunter DJ, McLennan CE, et al. Does cartilage volume or thickness distinguish knees with and without mild radiographic osteoarthritis? the Framingham Study. Ann Rheum Dis. 2010;69(1):143-9. doi: 10.1136/ard.2008.099200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Souza RB, Wu SJ, Morse LJ, Subburaj K, Allen CR, Feeley BT. Cartilage MRI relaxation times after arthroscopic partial medial meniscectomy reveal localized degeneration. Knee Surg Sports Traumatol Arthrosc. 2015. Jan;23(1):188-97. doi: 10.1007/s00167-014-2997-2. [DOI] [PubMed] [Google Scholar]
- 35. Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Meniscal root tears: current concepts review. Arch Bone Jt Surg-Ab. 2018. Jul;6(4):250-9. [PMC free article] [PubMed] [Google Scholar]
- 36. Kim CW, Lee CR, Gwak HC, Kim JH, Park DH, Kwon YU, et al. Clinical and radiologic outcomes of patients with lax healing after medial meniscal root repair: comparison with subtotal meniscectomy. Arthroscopy. 2019. Nov;35(11):3079-86. doi: 10.1016/j.arthro.2019.05.051. [DOI] [PubMed] [Google Scholar]
- 37. Wang XZ, Zheng YX, Cao YL, Gu XF, Wei SP, Gao NY, et al. [Study on the diagnostic value of whole-organ magnetic resonance imaging score (WORMS) in knee osteoarthritis]. Zhongguo Gu Shang. 2012. May;25(5):364-8. [PubMed] [Google Scholar]
- 38. Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011. Mar;27(3):346-54. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 39. Omoumi P, Michoux N, Roemer FW, Thienpont E, Vande Berg BC. Cartilage thickness at the posterior medial femoral condyle is increased in femorotibial knee osteoarthritis: a cross-sectional CT arthrography study (part 2). Osteoarthritis Cartilage. 2015. Feb;23(2):224-31. doi: 10.1016/j.joca.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 40. Arno S, Walker PS, Bell CP, Krasnokutsky S, Samuels J, Abramson SB, et al. Relation between cartilage volume and meniscal contact in medial osteoarthritis of the knee. Knee. 2012;19(6):896-901. doi: 10.1016/j.knee.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM, et al. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis Cartilage. 2011. Aug;19(8):990-1002. doi: 10.1016/j.joca.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ashraf S, Zahoor A. Magnetic resonance imaging of articular cartilage. JBJS Rev. 2016. Aug 16;4(8):e1. doi: 10.2106/JBJS.RVW.15.00093. [DOI] [PubMed] [Google Scholar]
- 43. Li X, Kuo D, Theologis A, Carballido-Gamio J, Stehling C, Link TM, et al. Cartilage in anterior cruciate ligament-reconstructed knees: MR imaging T1{rho} and T2–initial experience with 1-year follow-up. Radiology. 2011. Feb;258(2):505-14. doi: 10.1148/radiol.10101006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Goldring MB, Goldring SR. Articular cartilage and subchondral bone in the pathogenesis of osteoarthritis. Ann N Y Acad Sci. 2010. Mar;1192:230-7. doi: 10.1111/j.1749-6632.2009.05240.x. [DOI] [PubMed] [Google Scholar]
- 45. Prasad AP, Nardo L, Schooler J, Joseph GB, Link TM. T(1)rho and T(2) relaxation times predict progression of knee osteoarthritis. Osteoarthritis Cartilage. 2013. Jan;21(1):69-76. doi: 10.1016/j.joca.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Titchenal MR, Williams AA, Chehab EF, Asay JL, Dragoo JL, Gold GE, et al. Cartilage subsurface changes to magnetic resonance imaging UTE-T2* 2 years after anterior cruciate ligament reconstruction correlate with walking mechanics associated with knee osteoarthritis. Am J Sports Med. 2018. Mar;46(3):565-72. doi: 10.1177/0363546517743969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015. Apr;43(4):912-20. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 48. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014. Dec;42(12):3016-30. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 49. Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004. Oct;33(10):569-74. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 50. Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012. Oct;40(10):2342-7. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 51. Daney BT, Aman ZS, Krob JJ, Storaci HW, Brady AW, Nakama G, et al. Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019. Jun;47(7):1591-600. doi: 10.1177/0363546519844250. [DOI] [PubMed] [Google Scholar]
- 52. Furumatsu T, Kamatsuki Y, Fujii M, Kodama Y, Okazaki Y, Masuda S, et al. Medial meniscus extrusion correlates with disease duration of the sudden symptomatic medial meniscus posterior root tear. Orthop Traumatol Surg Res. 2017. Dec;103(8):1179-82. doi: 10.1016/j.otsr.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 53. Calvo E, Palacios I, Delgado E, Ruiz-Cabello J, Hernandez P, Sanchez-Pernaute O, et al. High-resolution MRI detects cartilage swelling at the early stages of experimental osteoarthritis. Osteoarthr Cartilage. 2001. Jul;9(5):463-72. doi: 10.1053/joca.2001.0413. [DOI] [PubMed] [Google Scholar]
- 54. Kumar D, Schooler J, Zuo J, McCulloch CE, Nardo L, Link TM, et al. Trabecular bone structure and spatial differences in articular cartilage MR relaxation times in individuals with posterior horn medial meniscal tears. Osteoarthritis Cartilage. 2013. Jan;21(1):86-93. doi: 10.1016/j.joca.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Russell C, Pedoia V, Souza RB, Majumdar S. Cross-sectional and longitudinal study of the impact of posterior meniscus horn lesions on adjacent cartilage composition, patient-reported outcomes and gait biomechanics in subjects without radiographic osteoarthritis. Osteoarthritis Cartilage. 2017. May;25(5):708-17. doi: 10.1016/j.joca.2016.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lee SJ, Aadalen KJ, Malaviya P, Lorenz EP, Hayden JK, Farr J, et al. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006. Aug;34(8):1334-44. doi: 10.1177/0363546506286786. [DOI] [PubMed] [Google Scholar]
- 57. Lanzer WL, Komenda G. Changes in articular cartilage after meniscectomy. Clin Orthop Relat Res. 1990. Mar;252:41-8. [PubMed] [Google Scholar]
- 58. Takahashi K, Hashimoto S, Nakamura H, Mori A, Sato A, Majima T, et al. Medial meniscal posterior root/horn radial tears correlate with cartilage degeneration detected by T1rho relaxation mapping. Eur J Radiol. 2015. Jun;84(6):1098-104. doi: 10.1016/j.ejrad.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 59. Cox JS, Cordell LD. The degenerative effects of medial meniscus tears in dogs’ knees. Clin Orthop Relat Res. 1977. Jun;125:236-42. [PubMed] [Google Scholar]