Abstract
Little is known about the temporal patterns of infection and transmission of Lassa virus (LASV) within its natural reservoir (Mastomys natalensis). Here, we characterize infection dynamics and transmissibility of a LASV isolate (Soromba-R) in adult lab-reared M. natalensis originating from Mali. The lab-reared M. natalenesis proved to be highly susceptible to LASV isolates from geographically distinct regions of West Africa via multiple routes of exposure, with 50% infectious doses of < 1 TCID50. Postinoculation, LASV Soromba-R established a systemic infection with no signs of clinical disease. Viral RNA was detected in all nine tissues examined with peak concentrations detected between days 7 and 14 postinfection within most organs. There was an overall trend toward clearance of virus within 40 days of infection in most organs. The exception is lung specimens, which retained positivity throughout the course of the 85-day study. Direct (contact) and indirect (fomite) transmission experiments demonstrated 40% of experimentally infected M. natalensis were capable of transmitting LASV to naïve animals, with peak transmissibility occurring between 28 and 42 days post-inoculation. No differences in patterns of infection or transmission were noted between male and female experimentally infected rodents. Adult lab-reared M. natalensis are highly susceptible to genetically distinct LASV strains developing a temporary asymptomatic infection associated with virus shedding resulting in contact and fomite transmission within a cohort.
Significance Statement.
Lassa virus (LASV) is a zoonotic pathogen and a prominent etiological agent of viral hemorrhagic fever in humans. In nature, it is maintained in, and primarily transmitted to humans, by rodent reservoirs. The association of LASV with Mastomys natalensis was quickly made following the initial description of Lassa fever in 1969; however, to date, very little is known about the temporal patterns of infection of LASV in these rodents. Here, we model infection kinetics and transmissibility of LASV in a natural rodent reservoir, M. natalensis.
Introduction
The Arenaviridae is large group of zoonotic viruses that have been documented world-wide (1). The majority of these viruses utilize rodents as their natural reservoirs, though recently reptilian- and fish-borne arenaviruses have been recognized (2). The prototype Mammarenavirus, Lymphocytic choriomeningitis virus (LCMV), was originally isolated from clinical specimens in 1933 and its association with a rodent host (the common house mouse, Mus musculus) was suggested shortly thereafter (3, 4). Since then, at least 50 distinct members of the Arenaviridae, including over 40 Mammarenaviruses have been documented. Although most are thought to be nonpathogenic to humans, no less than seven Mammarenaviruses, including New World species from South America (Chapare, Guanarito, Junin, Machupo, and Sabia viruses) and Old World species from Africa (Lassa and Lujo viruses), are associated with hemorrhagic fever diseases in humans (2, 5).
Among the Mammarenaviruses, Lassa virus (LASV) has the highest incidence of human infection/disease with an estimated 300,000 cases occurring per annum (6, 7). In humans, LASV infection demonstrates a wide variety of symptoms from clinically asymptomatic to hemorrhagic manifestations associated with multiorgan failure, which is referred to as Lassa fever (8, 9). In general, case fatality rates for Lassa fever vary up to approximately 30%, though it increases in pregnant women (10–13). In endemic regions of West Africa, LASV infections represent a significant burden on health care systems with an estimated 15% of hospitalizations due to LASV infection (14–16). Although human-to-human transmission is known to occur, particularly in nosocomial settings, LASV outbreaks and the majority of cases are believed to result from direct transmission from infected rodents to humans (17).
Despite the significant disease manifestations in humans associated with several Mammarenaviral infections, little is known about the virus–host interactions in the natural reservoirs. The lone exception is LCMV, which is widely used as a model for the study of viral persistence versus clearance in mice (18). LASV was initially described in 1969 during an outbreak of human disease in the Jos plateau region of Nigeria and its association with its natural rodent reservoir, Mastomys natalensis, documented within a few years (19, 20). Despite this, outside of the geographic distribution of naturally infected rodents, very little is known about the infection dynamics and transmissibility of LASV in the rodent host. In 1975, Walker et al. described experimental infections of field-collected Mastomys rodents with LASV and demonstrated their susceptibility to viral infection (21). However, methodological details in the report are minimal and the number of animals were relatively small (eight adults, 12 neonatal rodents). Further, this work was conducted prior to the subspeciation of Mastomys into M. natalensis and the often sympatric and physiologically similar relative species of M. huberti, and M. erythroleucus, as well as other commensal rodents including M. coucha, so the exact identity of Mastomys rodents utilized cannot be certain.
Recently, we established a genetically confirmed colony of M. natalensis from founder stock captured in Southern Mali and confirmed their susceptibility to LASV infection (22). Additional studies have provided normal reference ranges for M. natalensis as well as patterns of infection with LASV Josiah (23–25). Here, we characterize an experimental infection model using the geographically matched LASV isolate (Soromba-R) in captive-breed M. natalensis originating from Mali and use the model to assess direct (contact) and indirect (fomite) transmission.
Methods
Ethics statement
Animal studies were approved by the Institutional Animal Care and Use Committee of the Rocky Mountain Laboratories (RML). Animal work was conducted adhering to the institution's guidelines for animal use and followed the guidelines and basic principles in the United States Public Health Service Policy on Humane Care and Use of Laboratory Animals as well as the Guide for the Care and Use of Laboratory Animals by certified staff in an Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International accredited facility.
Biosafety
All work with infectious LASV and potentially infectious materials derived from animals was conducted in a Biosafety Level 4 (BSL 4) laboratory in the Integrated Research Facility of the RML, National Institute of Allergy and Infectious Diseases (NIAID), and National Institutes of Health (NIH). Sample inactivation and removal was performed according to standard operating protocols approved by the RML Institutional Biosafety Committee (26, 27).
Animal husbandry and manipulations
Mastomys natalensis were provided from an in-house breeding colony maintained at RML (22). Animals were housed in a hepa-filtered rat caging system with additional locking wire tops (Innovive). Animals were maintained on a 12/12 hour light cycle and environmental conditions were set at 22°C with 50% humidity. Water and feed were given ad lib and enrichment, including nestlets, crinkle paper, huts, wood cubes, and Nylabones, was provided.
Experiments were conducted on animals of mixed sex (generally 1:1 male to female ratio) aged 6 to 12 weeks at the time of inoculation. All experimental manipulations were conducted on anesthetized animals. To prevent potential escape, rodents were initially sedated directly in their cages with isoflurane after which they were transferred to induction chambers and maintained with vaporized isoflurane to effect. Postinoculation, animals were observed a minimum of once daily by trained veterinary staff for signs of illness or disease including but not limited to reduced food and water intake, unkempt fur, hunched posture, and preference for segregation; however, for safety concerns animals were not weighed daily. At indicated time points animals were euthanized via exsanguination while under deep sedation.
Virus
Unless otherwise stated, animals were inoculated with LASV strain Soromba-R (accession numbers KF478765 and KF478762), which was originally isolated from a naturally infected M. natalensis captured in the village of Soromba in southern Mali (28). The virus was passaged three times on Vero cells and titered using standard 50% tissue culture infectivity assays (TCID50). In the heterologous challenge study, groups of M. natalensis were also inoculated with LASV strains Z-132 (Liberia) (29) and Josiah (Sierra Leone) (30), which were propagated and titered as outlined for Soromba-R.
Route of infection
In order to assess the susceptibility of the lab-reared M. natalensis, five groups of eight animals were infected with 5 × 103 TCID50s of LASV Soromba-R via intraperitoneal (i.p., 100 µl each into the right and left quadrant of the abdomen), intramuscular (i.m., 50 µl of inoculum delivered each into the right and left hind leg musculature), or subcutaneous (s.c., 200 µl delivered to one site in the intrascapular region) injections as well as intranasal (i.n., 50 µl per nare) and oral gavage (200 µl delivered with a 20-gauge feeding tube) administration. At 10 and 21 dpi, four animals per group were euthanized and blood and tissue samples were collected to assess extent of LASV infection.
Heterologous LASV challenge
To assess the susceptibility of the lab-reared M. natalensis of Malian origin to geographically distinct (heterologous) LASV isolates, groups of 12 animals were inoculated with 1 × 103 TCID50’s of strains Z-132 or Josiah via the i.m. route (as outlined above). At 10 and 21 dpi, six animals per group were euthanized and tissue samples (blood, lung, heart, liver, and kidney) collected for virological analysis by conventional RT-PCR.
50% infectious dose study
To determine the lowest dose of virus capable of infecting 50% of M. natalensis (ID50), four groups of six animals were inoculated with 10-fold serial dilutions of LASV Soromba-R (range 1 to 1,000 TCID50’s) via i.m. injection as above. At 12 dpi, animals were euthanized and blood and liver samples were collected to determine if a productive LASV infection was established. In a second experiment, the ID50 for s.c. injection was determined according to the same experimental outline.
Temporal analysis of LASV infection
Groups of eight rodents (four males and four females per group) were infected with 1 × 103 TCID50’s LASV Soromba-R via i.m. injection. At 3, 7, 14, 21, 35, 42, 62, and 85 dpi, a single group of infected animals as well as two sham inoculated control animals (one male and one female) were euthanized for specimen collection and analysis. Animals were exsanguinated with blood aliquots prepared for serology (plasma) and RT-PCR analysis. Solid organ specimens, including heart, lung, liver, spleen, kidney, mesenteric lymph nodes, gastrointestinal tract, reproductive organs (testes or uterus), and brain, were collected for RT-PCR analysis.
Indirect transmission
Indirect, fomite transmission was evaluated using the first 56 infected animals from the temporal study outlined above. Transmission via fomites was assessed for 0 to 7, 7 to 14, 14 to 21, 28 to 35, 35 to 42, 55 to 62, and 78 to 85 dpi. To accomplish this, experimentally infected animals were individually housed in fresh cages 7 days prior to allotted euthanasia and sampling point (defined as the transmission period postinoculation). For example, to assess transmission between 7 and 14 dpi, individual animals were placed in clean cages at 7 dpi and maintained in the cage until day 14. The exception to this was the animals used to assess transmission within 0 and 7 dpi, which were immediately placed in individual clean ages after inoculation. At the end of the specified time period, the infected animals were removed (for analysis in the temporal study) and a single naïve M. natalensis was placed in each potentially LASV contaminated cage. Naïve animals were housed in the “dirty” cage for 7 days after which they were removed and maintained individually in clean cages. The sentinel rodents were maintained for 45 days postintroduction to the “dirty” cage at which point they were exsanguinated and tested for evidence of seroconversion to the LASV NP antigen.
Direct transmission
A total of 10 cages of four animals (litter and sex matched to avoid overt aggression) were cohoused for the duration of the experiment. A single animal per cage was randomly selected, ear-tagged, and inoculated with 1 × 103 TCID50’s LASV Soromba-R via i.m. injection as outlined above. Postinoculation animals remained sedated for 1 to 2 minutes during which time the fur around the injection site was cleaned with 70% ethanol to avoid potential cross-contamination via immediate physical interactions. Animals were maintained together for 45 dpi at which point the experimentally infected rodent as well as its three cage mates were exsanguinated and tested for evidence of seroconversion to the LASV NP antigen.
LASV detection
LASV RNA was detected and quantified using previously established methods (28, 31). Tissue and blood samples were inactivated and RNA extracted using Qiagen blood and tissue kits according to the manufacturer’s specifications and approved RML BSL-4 standard operating procedures.
Serology
Serum samples were tested for anti-LASV nucleocapsid IgG antibodies using a standard enzyme-linked immunosorbent serological assay (ELISA) methodologies as previously described using a recombinant, purified LASV nucleocapsid protein as the bait antigen (32, 33).
Role of funding source
The funders had no role in the design of the study, analysis of the data, or decisions to publish.
Results
Susceptibility to homologous LASV infection
Previously, we have demonstrated the susceptibility of the lab-reared M. natalensis to infection with LASV Soromba-R via i.p. injection (22). Here, we further assessed the susceptibility of these animals to infection with LASV via different routes of inoculation. Groups of eight rodents were inoculated with 5 × 103 TCID50’s of LASV Soromba-R via i.p., i.m., or s.c. injection, i.n. installation or oral gavage. On days 10 and 21 postinoculation, four animals per group were euthanized and samples were collected for virological analysis. Of the 40 inoculated animals, LASV RNA was readily detectable in at least one tissue sample from all but three rodents (all of which were sampled 21 days postoral inoculation). The majority (75%) of animals demonstrated evidence of a systemic infection, with LASV RNA detected in ≥ 4 tissues analyzed, with no overt signs of disease (Table 1). Horizontal transmission of LASV between M. natalensis in the natural setting is unclear though it is likely to occur by ingestion of contaminated food, inhalation of viral particles, or via wounding or other direct contact. Experimentally, the oral route was least effective in establishing infection. I.p. injections and i.n. administration were uniformly successful for infecting M. natalensis. While both these routes are convenient methods for inoculation in laboratory settings, i.p. inoculation and i.n. administration without the use of an aerosol generator, may not adequately mimic natural routes of exposure. For these reasons, the 50% infectious dose (ID50) was determined for s.c. and i.m. injections.
Table 1.
Real-time PCR analysis of tissues collected from laboratory-reared M. natalensis experimentally infected with LASV strain Soromba-R.
| Route of inoculation | Day* of sample collection | Blood | Lung | Liver | Spleen | Lymph node | Brain |
|---|---|---|---|---|---|---|---|
| I.p. | 10 | 4/4 | 4/4 | 4/4 | 4/4 | n.d. | 4/4 |
| 21 | 4/4 | 4/4 | 4/4 | 4/4 | 2/4 | 4/4 | |
| I.m. | 10 | 3/4 | 4/4 | 4/4 | 3/4 | 3/4 | 2/4 |
| 21 | 0/4 | 3/4 | 2/4 | 2/4 | 4/4 | 2/4 | |
| S.c. | 10 | 4/4 | 4/4 | 4/4 | 4/4 | 4/4 | 4/4 |
| 21 | 1/4 | 4/4 | 4/4 | 3/4 | 3/4 | 1/4 | |
| I.n. | 10 | 4/4 | 4/4 | 4/4 | 4/4 | 4/4 | 3/4 |
| 21 | 0/4 | 4/4 | 3/4 | 3/4 | 4/4 | 0/4 | |
| Oral | 10 | 2/4 | 1/4 | 1/4 | 2/4 | 2/4 | 3/4 |
| 21 | 0/4 | 1/4 | 0/4 | 1/4 | 1/4 | 0/4 |
*With respect to challenge; n.d. = not done. Numbers represent positive samples/samples tested.
Determination of the 50% infectious dose
As the natural reservoir, it is expected that naïve M. natalenesis would be highly susceptible to low-doses of LASV. To assess this, four groups of six rodents were inoculated via the s.c. or i.m. routes with 10-fold serial dilutions, representing challenge doses of 1 to 1,000 TCID50’s LASV Soromba-R. Tissue samples (liver and blood) were collected at 12 dpi and tested for the presence of LASV. The results of these two independent studies demonstrated productive infections in all animals resulting in an ID50 of < 1 TCID50 of LASV Soromba-R for either route of infection. Based on these results and with the intent of mimicking wounding as a route of exposure, subsequent experiments were conducted using the i.m. injection route.
Susceptibility to geographically divergent LASV isolates
In order to assess the susceptibility of M. natalenesis originating from Mali to infection with geographically distinct LASV isolates, groups of 12 animals (six males and six females) were inoculated with 1 × 103 TCID50’s LASV strains Z-132, (Liberia, lineage IV) or Josiah (Sierra Leone, lineage IV) as well as Soromba-R (Mali, lineage V) for comparison purposes, via the i.m. route (34). On days 10 and 21 postinfection, six animals per group were euthanized and samples collected for virological analysis. Due to the genetic heterogeneity of the LASV isolates used in this experiment, tissue samples were analyzed via conventional RT-PCR for the presence or absence LASV genome. Tissue (blood, lung, liver, kidney, and heart) samples collected at days 10 and 21 postinfection were uniformly positive for the presence of a LASV RNA (Table 2). A subset of RT-PCR products were sequences via Sanger sequencing and confirmed the authenticity of the expectant LASV sequence. As in previous experiments, infected rodents did not display signs of infection throughout the course of the study.
Table 2.
Analysis of tissues collected from laboratory-reared M. natalensis experimentally infected with LASV strains Josiah, Z-132 or Soromba-R.
| LASV strain | Day* of sample collection | Blood | Lung | Liver | Kidney | Heart |
|---|---|---|---|---|---|---|
| Josiah | 10 | 6/6 | 6/6 | 6/6 | 6/6 | 6/6 |
| 21 | 6/6 | 6/6 | 6/6 | 6/6 | 6/6 | |
| Z-132 | 10 | 6/6 | 6/6 | 6/6 | 6/6 | 6/6 |
| 21 | 6/6 | 6/6 | 6/6 | 6/6 | 6/6 | |
| Soromba-R | 10 | 6/6 | 6/6 | 6/6 | 6/6 | 6/6 |
| 21 | 6/6 | 6/6 | 6/6 | 6/6 | 6/6 |
*With respect to challenge. Mastomys were infected via i.m. injection with 1 × 103 TCID50’s LASV. Each sample point consisted of three experimentally infected males and females. Numbers represent positive samples/samples tested.
Temporal LASV infection study
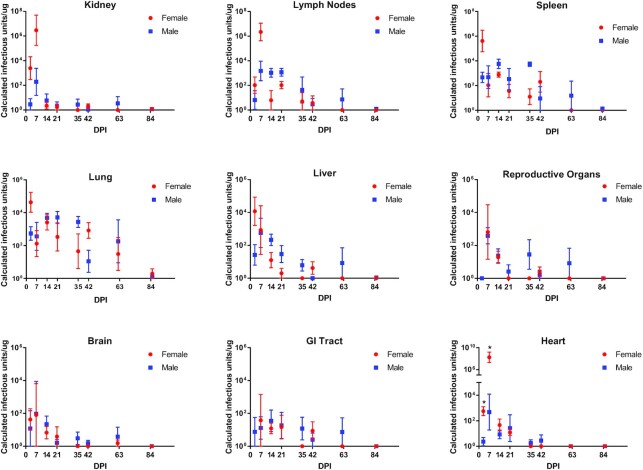
To chronologically characterize LASV infection in adult M. natalensis, groups of eight rodents (four males and four females) were infected with 1 × 103 TCID50’s LASV Soromba-R via i.m. injection, and samples were collected on nine different time points postinfection over the course of 85 days (Fig. 1). Throughout the course of the experiment, LASV infected Mastomys did not display any signs of infection and no gross pathological abnormalities were noted in the infected rodents during necropsy. By day 3 postinfection, viral RNA was detectable in most tissues analyzed. The patterns of positivity suggest a systemic infection peaking within 1 to 2 weeks postinfection and resolving within approximately 40 days in most tissues. The exception noted in this study is lung specimens, which maintained viral RNA for at least 85 dpi. Overall, no discernable differences in infection were observed in most organs between male and female rodents suggesting both are equally susceptible to LASV infection. However, RNA persisted in the testis when compared to ovaries (Fig. 1) suggesting that sexual transmission of virus and in utero infection of pups may be driven by infected males. Further study on this topic is required to elucidate these patterns.
Fig. 1.
Temporal analysis of tissue specimens from LASV-infected M. natalensis. Groups of eight (four males and four females) M. natalensis was experimentally infected with 1 × 103 TCID50’s LASV strain Soromba-R via i.m. injection and euthanized from specimen collection at indicated time points. Total RNA was extracted, standardized, and analyzed in duplicate by real-time RT-qPCR methodologies. Data shown represent the average calculated infectious units/µg of tissue from four animals. Error bars represent the standard error of the mean. * show statistical significance between samples from male and female heart samples at days 3 (P = 0.0023) and 7 (P = 0.0168). Reproductive organs and GI tract specimens from female rodents at the 3 dpi time point were inadvertently not collected.
Transmission studies
To account for variations in infection kinetics due differing inoculum doses and routes of exposure, sentinel-testing methodologies, relying on seroconversion, were employed in the two independent transmission studies. In an initial assessment of transmissibility, a direct contact transmission study was conducted. Briefly, one animal was infected with 1 × 103 TCID50’s LASV Soromba-R via i.m. injection and cohoused with three naïve littermates for 45 days (Fig. 2). Infection in naïve and inoculated animals was confirmed via seroconversion to the LASV NP antigen. All 10 animals directly infected with LASV Soromba-R seroconverted with titers of ≥ 400 (Fig. 2). Within the 10 cages, six had no evidence of direct transmission (0 for 18 naive animals), one cage had a single animal that was serologically reactive to the LASV NP, and three cages had two rodents each with serological reactivity (Fig. 2). Overall, serological evidence of intracage transmission occurred in seven of 30 naïve rodents, or 23.3%; however, in the four (40%) of cages where transmission did occur 58.3% of naïve rodents (7 of 12) seroconverted (Fig. 2).
Fig. 2.
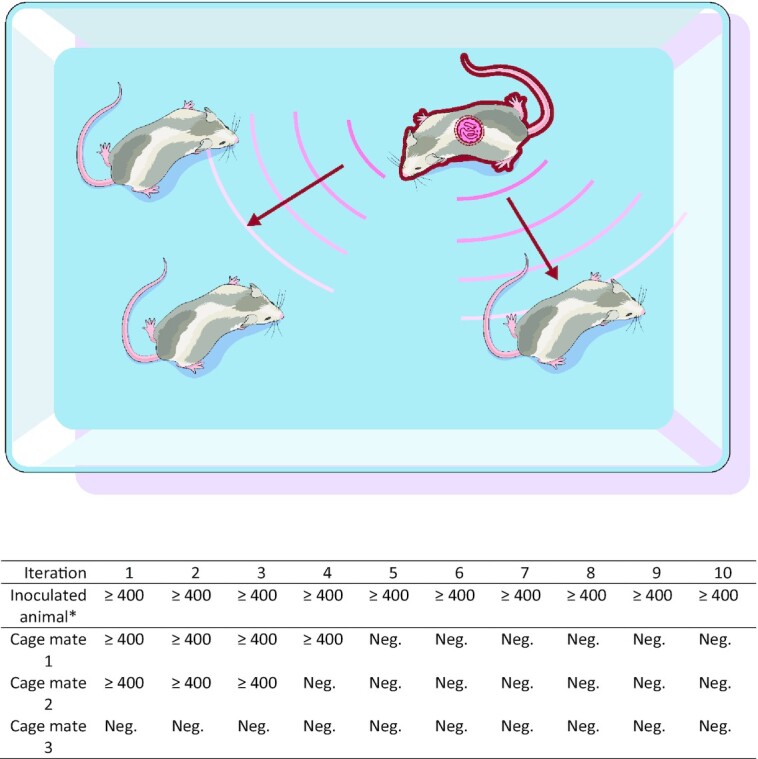
Direct tranmission of LASV. A single lab-reared M. natalensis was experimentally infected with 1 × 103 TCID50’s LASV strain Soromba-R via i.m. injection and immediately housed with three naïve cage mates. The rodents were cohoused for 45 days postinfection after which terminal serum samples were collected to assess seroconversion to the LASV nucleocapsid antigen. A total of 10 iterations of the experiment were conducted. Arrows represent the potential for direct contact between the infected rodent and its naïve cage mates, while waves represent hypothetical transmission of virus. * Original animal experimentally infected with LASV Soromba-R. Data shown are reciprocal titers based on ELISA serological analysis using a recombinant LASV nucleocapsid antigen.
In a second study, and concurrent to the temporal analysis study above, fomite transmission from infected to naïve M. natalensis was evaluated (Fig. 3). Briefly, rodents were infected with 1 × 103 TCID50’s LASV Soromba-R via i.m. injection at specific dpi were individually housed in clean cages for 3 or 7 days prior to euthanasia for sample collection. At the time of necropsy of the infected animal (as determined by the temporal study above), a naïve animal was placed into the potentially LASV contaminated cage and housed for a minimum of 2 weeks. A total of 45 days postexposure, the “naïve” animals were euthanized and serum assessed for seroconversion to the LASV NP antigen. Within the first 21 days postinfection, only 3 of the 24 experimentally infected animals contaminated their cages resulting in seroconversion of the naïve animals (3/24, 12.5%; Fig. 3). Peak contamination of cages (suggesting active transmission of virus) was observed in animals of between 28 and 42 days infection duration, with 10 of 24 (41.7%) naïve animals serorconverting for the LASV NP antigen (Fig. 3). Between 42 and 85 dpi, only a single naïve animal seroconverted (1/8, 12.5%; Fig. 3). Overall, indirect transmission was observed in 14 of 56 (25%) of potentially contaminated cages.
Fig. 3.
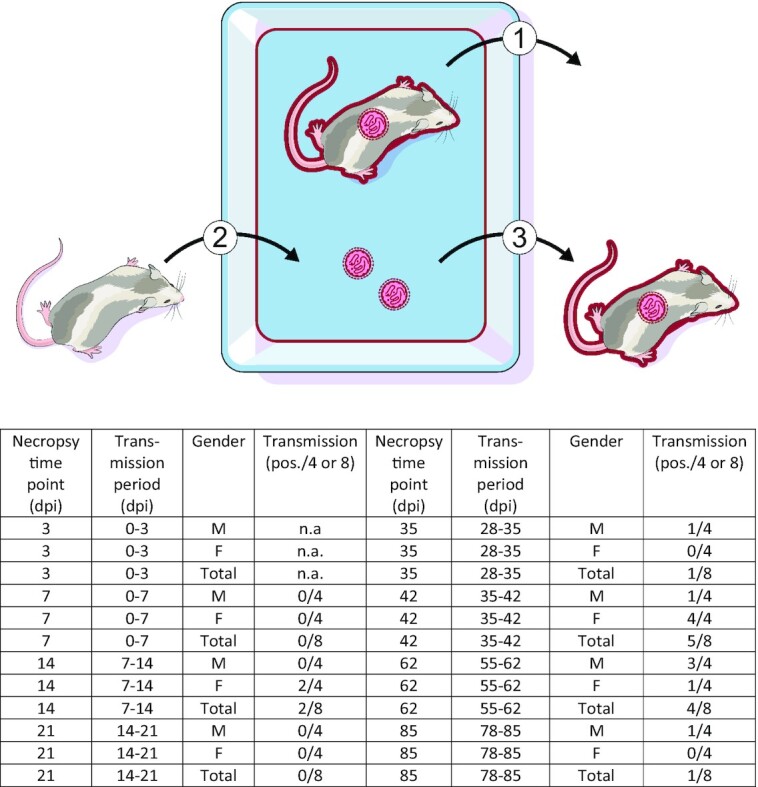
Indirect transmission of LASV. (1) Male (M) and female (F) lab-reared M. natalensis were experimentally infected with 1 × 103 TCID50’s LASV strain Soromba-R via i.m. injection. A total of 7 days prior to schedule necropsy, infected rodents were individually housed. (2) After 7 days in clean cages, infected animals were removed for necropsy. Immediately following, a naive sentinel M. natalensis was placed in the potentially contaminated cage and maintained for another 7 days. (3) A total of 45 days later, the sentinel rodent was euthanized and assessed for exposure to LASV via seroconversion. Necropsy time point refers to the day postinfection for the experimentally infected rodent from the temporal kinetics study. Gender refers to the sex of the experimentally infected rodent. n.a. = not assessed.
Discussion
In West Africa, LF is one of the most prominent human viral hemorrhagic diseases known resulting in thousands of deaths each year. The association of LASV with Mastomys species rodents was first described during early outbreaks in the late 1960s to early 1970s, and yet, despite this critical link to human disease, to date little effort has been placed on understanding the dynamics of infection in the rodent reservoirs outside of ecological or prevalence studies. This gap in knowledge may impede our full understanding of the pathophysiological mechanisms of disease versus no disease. For example, the study of Seoul and Sin Nombre orthohantaviruses in rats and deer mice, their respective rodent reservoirs, coupled with analysis of clinical patient samples has established the role of regulatory T cell (T-reg) responses in rodents (no disease, high T-reg response) and humans (disease, low T-reg response) (35, 36).
The lab-reared M. natalensis were highly susceptible to infection with LASV via multiple routes of inoculation (i.m., s.c., i.p., i.n., and oral) with ID50 values of < 1 TCID50 for i.m. and s.c. injections. Given the low infectious dose and sensitivity via multiple routes, it is plausible that in natural settings LASV is maintained in rodent populations via several mechanisms including aggressive encounters between rodents, infestation of contaminated food sources or, similar to humans, inhalation of viral particles. Although not assessed in the current study and discussed further below, based on positive reproductive tracts, sexual transmission is also probable. Additionally, despite considerable genetic variability within LASV isolates that correlate with their geographic distribution, the M. natalensis originating from southern Mali were not only susceptible to infection with LASV from southern Mali (Soromba-R), but also those from genetically distinct LASV strains originated from nearby countries including Sierra Leone (Josiah) and Liberia (Z-132). Given the hypothesized movement of LASV across West Africa, most likely in both infected rodents and humans, this may not be surprising. However, further studies focused on characterization of Mastomys rodents in these areas should be considered to determine if reservoir host genetics have a role in LASV prevalence rates and/or outbreaks.
Postinoculation, LASV establishes a systemic infection in adult M. natalensis reservoirs without signs of illness or disease. Viral RNA was detected in most tissue types analyzed by 3 dpi. Peak RNA titers were observed between 7 and 14 dpi and in most tissues (brain, kidney, liver, heart, female reproductive tract, and GI tract) was cleared within 30 to 40 dpi. Detection of LASV RNA in lungs and spleens was relatively consistent for at least 60 days. These data advance those of Walker et al. who found that postinfection Mastomys rodents do not demonstrate any adverse signs of infection and adult rodents seem to be capable of clearing the LASV infection, at least in the organs analyzed (21). Recent studies using LASV Josiah (a genetically distinct isolate from Sierra Leone) in descendants from Malian M. natalensis colony similarly showed a systemic LASV infection that trended toward clearance in the same period as that observed herein (25). Furthermore, similar patterns of infection have been hypothesized based patterns of molecular and serological positivity in samples collected from naturally infected rodents collected during ecological studies in southern Mali (33).
Unlike Ebola virus, which spills over infrequently from zoonotic reservoirs with outbreaks resulting from, and maintained by, human-to-human transmission, LASV infection in humans are most commonly associated with direct rodent exposure. Annual and seasonally influenced epidemics overlap with the dry season in West Africa when food sources in fields are inadequate and rodents move into areas in close proximity to humans (37). Given the prolonged and often explosive nature of outbreaks, this suggests that spillover events occur frequently meaning infected rodents remain infectious and are capable of efficiently shedding the virus for sustained periods. Recent studies have demonstrated the presence of viral RNA and infectious virus in oral and rectal swabs as well as urine samples from experimentally infected M. natalensis suggesting the virus is readily able to actively transmit (22, 25). To address this further, both direct (contact) and indirect (fomite) methods were utilized. In the first iteration, intracage transmission, as determined by seroconversion in naïve cage mates, was documented in a total of seven of 30 rodents (23.3%). A total of 4 of 10 cages (40%), each with a single experimentally inoculated Mastomys, had evidence of transmission and within these cages 7 of the 12 naïve rodents (58.3%) seroconverted. Transmission within cages was not uniform with no instance documented in which all three naïve cage mates contracted infection. In the second assessment and in parallel with the temporal infection kinetics study above, a chronological assessment of indirect or fomite transmission was conducted and demonstrated similar results. Unlike LASV infection dynamics in individual rodents, which peaked between 7 and 14 dpi, transmission appeared to be delayed with most events resulting from rodents of 28 to 42 days postinfection (41.7%) as opposed to rodents infected for a duration of 21 days or less (12.5%) or greater than 42 dpi (12.5%). Similar observations of delayed transmission (albeit intracage transmission) postinfection were also noted with SNV in Peromyscus rodents, though in that study transmission events were rare (38). Overall, the percentage of experimentally inoculated Mastomys actively transmitting LASV, as determined by seroconversion in surrogate naïve animals, was similar across both the direct and peak indirect transmission experiments (40% and 41.7%, respectively). Future studies are required to elucidate shedding routes (oropharyngeal fluids, urine, and feces) and more precisely define the nature of these transmission events (i.e. droplet or aerosol transmissibility).
Although neither neonatal nor in utero (vertical transmission) infections were conducted in the current studies, future work will focus this aspect of the LASV/rodent–host relationship. Importantly, infection of neonatal rodents with LASV appeared to result in prolonged and potentially lifelong persistent infections as characterized by viremia up to at least 74 dpi (21). Similar persistent infections with Mammarenaviruses have been described for LCMV in mice as well as Morogoro virus, a close genetic relative to LASV, also in M. natalensis (18, 39). Further experimental studies are required in colonized M. natalensis to not only assess vertical transmission, but also persistent LASV infection and/or transmission within these rodents. If confirmed for LASV in lab-reared M. natalensis, this would suggest that viral persistence in nature may rely on vertical transmission and chronically infected offspring, while epizootics and outbreaks in humans result from overall increases in recently infected rodents. These patterns are anecdotally supported by the seasonality of LF outbreaks coinciding with rodents inhabiting human dwellings in large numbers (dry season) versus low numbers (wet season) (37).
In conclusion, in this study we defined infection dynamics and transmissibility of LASV in adult lab-reared M. natalensis, the natural reservoir. Malian originated M. natalenesis were not just highly susceptible to the geographically matched LASV Soromba-R isolate, but similarly to isolates from geographically distinct West Africa regions. Postinoculation, very low infectious doses of LASV Soromba-R (< 1 TCID50) established a systemic asymptomatic infection via multiple routes of exposure. Peak viral RNA loads were detected in multiple tissues within 1 to 2 weeks postinfection following by virus clearance within about 6 weeks postinfection. Mastomys natalensis were capable of transmitting LASV to naïve animals through direct (contact) and indirect (fomite) exposure, with peak transmissibility at around 4 to 7 weeks postinfection. No differences in patterns of infection or transmission were noted between male and female rodents. Our results define M. natalensis as a highly potent reservoir species for LASV warranting rodent control efforts and proper education in LASV endemic area as key public health measures.
ACKNOWLEDGEMENTS
We thank Rose Perry-Gottschalk (NIH and NIAID) for assistance in preparing the illustrations used in the figures. The maintenance of the Mastomys natalensis colony would not have been possible without the Rocky Mountain Veterinary Branch (NIH and NIAID) whose care and dedication to these animals was vital, and Kathy Cordova, Sandy Skorupa, Jayne Faris, Amanda Weidow, and Richard Cole for animal husbandry and assistance with experimental manipulations in the BSL-4 environment.
Notes
Competing Interest: The authors declare no competing interest.
Contributor Information
David Safronetz, Special Pathogens, National Microbiology Laboratory Branch, Public Health Agency of Canada, Winnipeg, Manitoba, Canada.
Kyle Rosenke, Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, national Institutes of Health, Rocky Mountain Laboratories, Hamilton, MT, USA.
Kimberley Meade-White, Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, national Institutes of Health, Rocky Mountain Laboratories, Hamilton, MT, USA.
Angela Sloan, Special Pathogens, National Microbiology Laboratory Branch, Public Health Agency of Canada, Winnipeg, Manitoba, Canada.
Ousmane Maiga, University of Sciences Techniques and Technologies of Bamako, Bamako, Mali.
Sidy Bane, University of Sciences Techniques and Technologies of Bamako, Bamako, Mali.
Cynthia Martellaro, Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, national Institutes of Health, Rocky Mountain Laboratories, Hamilton, MT, USA.
Dana P Scott, Rocky Mountain Veterinary Branch, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rocky Mountain Laboratories, Hamilton, MT, USA.
Nafomon Sogoba, University of Sciences Techniques and Technologies of Bamako, Bamako, Mali.
Heinz Feldmann, Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, national Institutes of Health, Rocky Mountain Laboratories, Hamilton, MT, USA.
Funding
This research was financially supported by the Division of Intramural Research (DIR), the National Institute of Allergy and Infectious Diseases (NIAID), and the NIH.
Authors’ Contributions
D.S., K.R., D.P.S., and H.F. designed the study. D.S., K.R., K.M.W., C.M., and D.P.S. conducted the study and collected the data. D.S., K.R., K.M.W., A.S., O.M., S.B., D.P.S., N.S., and H.F. analyzed the data. D.S., K.R., and H.F. wrote the paper.
Data Availability
All data is included in the manuscript
References
- 1. Safronetz D, Feldmann H, Falzarano D.. 2012. Arenaviruses and filoviruses: viral haemorrhagic fevers. In: Medical microbiology. 18th edn. Galveston (TX): University of Texas Medical Branch. DOI: 10.1016/B978-0-7020-4089-4.00068-8. [Google Scholar]
- 2. Maes P, et al. 2018. Taxonomy of the family Arenaviridae and the order Bunyavirales: update 2018. Arch Virol. 163:2295–2310. [DOI] [PubMed] [Google Scholar]
- 3. Muckenfuss RS, Armstrong C, Webster LT.. 1934. Etiology of the 1933 epidemic of encephalitis. JAMA. 103:731–733. [Google Scholar]
- 4. Traub E. 1936. An epidemic in a mouse colony due to the virus of acute lymphocytic choriomeningitis. J Exp Med. 63:533–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hallam SJ, Koma T, Maruyama J, Paessler S. 2018. Review of mammarenavirus biology and replication. Front Microbiol. 9:1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCormick JB, Webb PA, Krebs JW, Johnson KM, Smith ES. 1987. A prospective study of the epidemiology and ecology of Lassa fever. J Infect Dis. 155:437–444. [DOI] [PubMed] [Google Scholar]
- 7. Mylne AQN, et al. 2015. Editor's choice: mapping the zoonotic niche of Lassa fever in Africa. Trans R Soc Trop Med Hyg. 109:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ogbu O, Ajuluchukwu E, Uneke CJ.. 2007. Lassa fever in West African sub-region: an overview. J Vector Borne Dis. 44:1–11. [PubMed] [Google Scholar]
- 9. Merson L, et al. 2021. Clinical characterization of Lassa fever: a systematic review of clinical reports and research to inform clinical trial design. PLoS NeglTrop Dis. 15:e0009788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Okokhere P, et al. 2018. Clinical and laboratory predictors of Lassa fever outcome in a dedicated treatment facility in Nigeria: a retrospective, observational cohort study. Lancet Infect Dis. 18:684–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Akpede GO, et al. 2019. Corrigendum: caseload and case fatality of Lassa fever in Nigeria, 2001–2018: a specialist center's experience and its implications. Front Publ Heal. 7:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kayem ND, et al. 2020. Lassa fever in pregnancy: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 114:385–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Duvignaud A, et al. 2021. Lassa fever outcomes and prognostic factors in Nigeria (LASCOPE): a prospective cohort study. Lancet Glob Heal. 9:e469–e478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Africa CDC . Lassa fever. [accessed 2022 Mar 2]. https://africacdc.org/disease/lassa-fever/. [Google Scholar]
- 15. McCormick JB. 1986. Clinical, epidemiologic, and therapeutic aspects of Lassa fever. Med Microbiol Immunol. 175:153–155. [DOI] [PubMed] [Google Scholar]
- 16. Fisher-Hoch SP, et al. 1995. Review of cases of nosocomial Lassa fever in Nigeria: the high price of poor medical practice. BMJ. 311:857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bell-Kareem AR, Smither AR.. 2021. Epidemiology of Lassa fever. Curr Top Microbiol Immunol. 33861373. last accessed: 2021 Apr 17, DOI:10.1007/82_2021_234. PMID:33861373. [DOI] [PubMed] [Google Scholar]
- 18. Zhou X, Ramachandran S, Mann M, Popkin DL.. 2012. Role of Lymphocytic Choriomeningitis Virus (LCMV) in understanding viral immunology: past, present and future. Viruses. 4:2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Frame JD, Baldwin JM, Gocke DJ, Troup JM.. 1970. Lassa fever, a new virus disease of man from West Africa. I. Clinical description and pathological findings. Am J Trop Med Hyg. 19:670–676. [DOI] [PubMed] [Google Scholar]
- 20. Monath TP, Newhouse VF, Kemp GE, Setzer HW, Cacciapuoti A.. 1974. Lassa virus isolation from Mastomys natalensis rodents during an epidemic in Sierra Leone. Science. 185:263–265. [DOI] [PubMed] [Google Scholar]
- 21. Walker DH, Wulff H, Lange JV, Murphy FA.. 1975. Comparative pathology of Lassa virus infection in monkeys, guinea-pigs, and Mastomys natalensis. Bull World Health Organ. 52:523–534.. last accessed 16 March 2022. https://pubmed.ncbi.nlm.nih.gov/821625/. [PMC free article] [PubMed] [Google Scholar]
- 22. Safronetz D, et al. 2021. Establishment of a genetically confirmed breeding colony of Mastomys natalensis from wild-caught founders from West Africa. Viruses. 13:590590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wozniak DM, et al. 2021. Hematology and clinical chemistry reference ranges for laboratory-bred natal multimammate mice (Mastomys natalensis). Viruses. 13:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith BJ, et al. 2021. Hematologic and serum biochemistry reference intervals using defined ASCVP methodology for laboratory natal multimammate mice (Mastomys natalensis). Lab Anim. 55:417–427. [DOI] [PubMed] [Google Scholar]
- 25. Wozniak DM, et al. 2021. Inoculation route-dependent Lassa virus dissemination and shedding dynamics in the natural reservoir - Mastomys natalensis. Emerg Microbes Infect. 10:2313–2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Feldmann F, Shupert WL, Haddock E, Twardoski B, Feldmann H.. 2019. Gamma irradiation as an effective method for inactivation of emerging viral pathogens. Am J Trop Med Hyg. 100:1275–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Haddock E, Feldmann F, Feldmann H.. 2016. Effective chemical inactivation of Ebola virus. Emerg Infect Dis. 22:1292–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Safronetz D, et al. 2010. Detection of Lassa virus, Mali. Emerg Infect Dis. 16:1123–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jahrling PB, Frame JD, Smith SB, Monson MH.. 1985. Endemic Lassa fever in Liberia. III. Characterization of Lassa virus isolates. Trans R Soc Trop Med Hyg. 79:374–379. [DOI] [PubMed] [Google Scholar]
- 30. Wulff H, Johnson KM.. 1979. Immunoglobulin M and G responses measured by immunofluorescence in patients with Lassa or Marburg virus infections. Bull World Health Organ. 57:631. last accessed 16 March 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2395825/. [PMC free article] [PubMed] [Google Scholar]
- 31. Vieth S, et al. 2007. RT-PCR assay for detection of Lassa virus and related Old World arenaviruses targeting the L gene. Trans R Soc Trop Med Hyg. 101:1253–1264. [DOI] [PubMed] [Google Scholar]
- 32. Branco LM, et al. 2008. Bacterial-based systems for expression and purification of recombinant Lassa virus proteins of immunological relevance. Virol J. 5:74. DOI: 10.1186/1743-422X-5-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Safronetz D, et al. 2013. Geographic distribution and genetic characterization of Lassa virus in Sub-Saharan Mali. PLoS NeglTrop Dis. 7:e2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Manning JT, Forrester N, Paessler S.. 2015. Lassa virus isolates from Mali and the Ivory Coast represent an emerging fifth lineage. Front Microbiol. 6:1037. DOI: 10.3389/FMICB.2015.01037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schountz T, et al. 2007. Regulatory T cell-like responses in deer mice persistently infected with Sin Nombre virus. Proc Natl Acad Sci USA. 104:15496–15501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Easterbrook JD, Zink MC, Klein SL.. 2007. Regulatory T cells enhance persistence of the zoonotic pathogen Seoul virus in its reservoir host. Proc Natl Acad Sci USA. 104:15502–15507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yaro CA, et al. 2021. Infection pattern, case fatality rate and spread of Lassa virus in Nigeria. BMC Infect Dis. 21:149. DOI: 10.1186/S12879-021-05837-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Botten J, et al. 2002. Shedding and intracage transmission of Sin Nombre hantavirus in the deer mouse (Peromyscus maniculatus) model. J Virol. 76:7587–7594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hoffmann C, et al. 2021. Experimental morogoro virus infection in its natural host, Mastomys natalensis. Viruses. 13:851. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data is included in the manuscript