Abstract
Public health is defined as the science of protecting the safety and improving the health of communities through education, policy-making and research for the prevention of disease (Gatseva and Argirova in J Public Health 19(3):205–6, 2011, 10.1007/s10389-011-0412-8; Winslow in Mod Med 2(1306):183–91, 1920. 10.1126/science.51.1306.23; What is public health. Centers for Disease Control Foundation. Centers for Disease Control, Atlanta, https://www.cdcfoundation.org/what-public-health; What is the WHO definition of health? from the Preamble to the Constitution of WHO as adopted by the International Health Conference, New York, On 7 April 1948. The definition has not been amended since. 22 July 1946; signed by the representatives of 61 States (Official Records of WHO, no. 2, p. 100) and entered into force, 19 June;1948. https://web.archive.org/web/20190307113324/https:/www.who.int/about/who-we-are/frequently-asked-questions). Translational research in healthcare is not only useful and satisfying for the researchers to bring their work to market but it would also support public health by bringing affordable, attainable and scalable solutions to the community at large. This is of high significance because instead of increasing the GDP spent in public health, we should focus on the increasing the translational research spending, as this would lead to improved solutions. Hence, the public health offering would reach a larger community at an improved cost. The COVID-19 pandemic and the huge number of lives it claimed exposes challenges in the public health. The pandemic has caused economic and social disruption to millions of people around the world, with many falling into extreme poverty. In early 2021, it was estimated nearly 690 million people are undernourished and by end of 2021 to increase further by 132 million (Joint statement by ILO, FAO, IFAD and WHO. Impact of COVID-19 on people's livelihoods, their health and our food systems https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people's-livelihoods-their-health-and-our-food-systems). The spending for public health has increased many folds during the pandemic and this is where translational research in healthcare can play a transformative role to reduce the burden on government healthcare budget (Covid-19 and its impact on Indian society. https://timesofindia.indiatimes.com/readersblog/covid-19-and-its-impact-on-india/covid-19-and-its-impact-on-indian-society-27565/). Over the past decade, public health research has started playing a major role in Indian academic settings. COVID-19 pandemic has further highlighted the role of public health. However, the potential of using technological advancement has not been fully utilised. This is where translational research and public health can play a role to tap the full potential of technology. This review paper explores the public health practices to understand the different practices to examine how both public health and translational research can cross-fertilise. It concludes with a short discussion on implications on policymakers.
Introduction
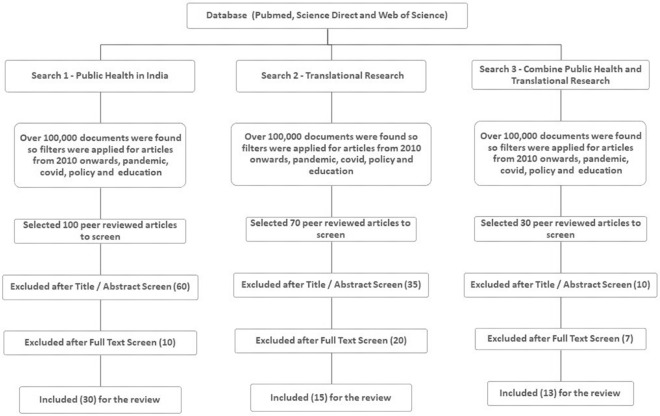
This review paper is based on the literature available in the field of translational research7 and public health. This review explores the role of both public health and translational research and also highlights how the cross-fertilisation of these two principles can be of immensely beneficial to the community. This review scrutinises the ‘gaps’ in the work carried out since 2010 in these two principles. Using relevant keywords, a literature search was performed within three databases—Web of Science, Scopus and PubMed—identifying 250 articles. PRISMA (Preferred Reporting Items for Systematics Reviews and Meta-Analyses) guidelines were adopted to direct further analysis. This review is based on 58 articles.
Scary statistics on the state of health in India based on Oxfam website8. Only 1.4% GDP is spent on health which is less than most of its neighbours. Households spent over 70% of their expense in medicine and a third of the population does not have regular access to medicine. Primary health centre two out of three lack operation theatres, one out of three lack labour room and four out of five lack specialists. Inpatient for two out of three people happens in private care. Studies shows out of pocket expense is pushing large numbers of people below the poverty line. Heart disease happens one in four people. One in four people cannot afford healthcare, and this pushes more people to below poverty lines and many due to medicine only.
The cross-fertilisation of public health and translational research can benefit from the various government scheme9. Prime Minister Modi in his address10 for health day 2022 said “The Government of India is working tirelessly to augment India’s health infrastructure.” He also noted he is happy that many have benefited from PM Jan Aushadhi program11 as it is the focus of the government to provide affordable healthcare leading to major savings for the poor and middle class and strengthening the Ayush network to further enhance healthcare.
An example of cross-fertilisation of these two disciplines is the COVID-19 vaccine development. Without involving the public health, the translational research of this would have not happened so quickly to get large number of the population vaccinated. And without the translation research for the development of the vaccine, public health would have not been able to bring COVID-19 pandemic to the current levels under control; The important three ‘Ps’ in model is the patients, providers (professionals) and policymakers. Patients is the key to the success of this model. Effective planning and allocating more funds for this cross-fertilisation model can overcome many shortcomings in the health system. This review looks at the influence of both principles and how both can work together for a better reach. Having established method and looking at these literatures at the benefits, and limitations which can be extremely advantageous for future research, this review intends to identify gaps in the methodological approaches and propose future research best practices to address this gap. More specifically, in this review, we are looking at a framework, model and stakeholder benefits for both these principles.
Method
A systematic method to the literature search and information extraction was adopted. The following sections describe how the literature search was conducted, how the study selection was done from the literature search, and how information was extracted from the selected literature.
Literature Search Approach
A systematic literature search was conducted in with the public health single search, then translational research single search, and then a combined search of public health and translational research. The search was limited to journal articles published in English within three databases—Web of Science, Scopus, and PubMed—since 2010 and identified 250 articles. PRISMA (Preferred Reporting Items for Systematics Reviews and Meta-Analyses) guidelines were adopted (Fig. 1).
Figure 1:
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).
Review Selection
Inclusion and exclusion criteria based on Table 1 were applied to select the articles. A two-stage process was conducted on all three searches. In the first stage, the title and abstract were reviewed to verify that they are relevant to both the principles. After screening the title and abstract, a total of 95 articles were Accessed. In the second stage, full-text screening was carried out to assess the eligibility for this review that resulted in 58 studies (Fig. 1).
Table 1:
Inclusion and exclusion criteria for review.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Original peer-to-peer reviewed articles after 2010 | Original peer-to-peer reviewed articles before 2010 |
| The focus of the articles in public health or translational study in Covid, pandemic, policy and education | The focus of the articles not in public health or translational study in Covid, pandemic, policy and education |
| Articles focused on stakeholders, models and framework | Full text not available, commentaries and editorials |
Public Health
Public health is different from public healthcare. Public healthcare is publicly funded healthcare, and public health is defined as the science of protecting the safety and improving the health of communities through education, policy-making and research for the prevention of disease1–4.
The actual traits of a coronavirus criticism 2019 (COVID-19) outbreak that spark public health interventions are inadequately defined12. The intention of this study is to evaluate the vital timing and quantity of public health interventions to comprise COVID-19 outbreaks in Australia. The joint efforts by public health interventions and the vital range of instances for intervention to prevent transmission helped to control the spread of the Delta variant, public health interventions alone are not enough unless the vaccination content material became ≥ 70%. Vaccination is highly imperative to control new variants.
A cross-sectional study13 was used to investigate how COVID-19 affects health and healthcare costs in China. Proactively gathered information from the US Centres for Disease Control and Prevention and designated hospitals was obtained to determine public health and hospitalisation costs under COVID-19 and estimated public health-related resource consumption and direct medical costs. As of May 20, 2020, COVID-19-related public healthcare costs ($ 6.83 billion) were 18.31 times higher than hospitalisations.
In Switzerland14, the population seems to have missed a healthcare dispatch for malignant tumours, and organ donation is in a positive position. Based on qualitative research on organ donation, this paper aims to provide a working solution to support the unwanted benefits of public health communication. This study provides an oral analysis on organ donation produced by the Swiss health authorities. Such a system provides an understanding of who is communicating what, who, how and for what, and provides ethical data on the usefulness of communication in public health. Beyond criteria related to organ donation (consent, altruism, etc.), analysis of public health communication shows that ethical issues are predicted primarily at three relationship boundaries (intersubjectivity, cooperation, impartiality). Procedures for assessing the ethics of public health communication in relation to social personality and the consequences of relationships can identify and help with unwanted communication-related problems.
During the COVID-19 epidemic, public health authorities and policymakers15 have used social media to disseminate information and encourage community support and funding. Their message helps to educate the general public about the pitfalls and the benefits of public health activities to flatten the epidemic. This study analyses COVID-19 tweets from Canada’s public health tweet account during the first six months of the epidemic, looks for differences in tweets based on region, and attempts to communicate by attempting to enter the threat of COVID-19. Studies show that Canadian public health tweet accounts, especially geographic accounts, do not always adhere to health communication practices. In addition, to reflect the increasing number of intervening complaints, public health account tweets that promote change and community fabrication should be deployed whenever health pitfalls are high. Their research emphasises the need for public health professionals to deliver messages appropriate to the level of threat they encounter in a particular geographic environment. The use of medical services after COVID-19 outbreak is a major challenge for as medical care was largely politically dependent.
This study16 was aims to investigate the impact of public perception on COVID-19-related public health interventions on the experience of older people with unmet health needs in South Korea. Three different logistic regression models were used to assess the impact of public perception. Understanding, trust and satisfaction with COVID-19 public health interventions for unmet health needs.
This study examined17 how to develop system leadership among UK healthcare professionals. First, a quick literature review identified three key documents in three relevant areas: system governance theory and practice, changing conditions in the UK public health system and education and training of UK public health professionals. Second, it consulted with 29 stakeholders to understand the background and needs of the development of system leadership in public health. Four major themes were identified, namely the nature and purpose of system governance, development needs and opportunities for public health professionals, giving the environment for a broader contextual factor that affects public health.
The COVID-19 epidemic has spawned companies investing in public health18. Among the OECD countries, public health accounts for a significant share of Canada’s total healthcare costs. Therefore, reinforcement learning (RL) is the perfect model for the various complex decision problems encountered in health, such as epidemics, resource allocation during monitoring or testing and adaptive slices for retirees. RL has been successfully used in a variety of areas, including precision medicines, but has not been widely endorsed in public health. This study presents key ideas for RL and for identifying challenges and openings related to the application of R. RL’s findings helped to have a trans-constructive effect on many issues in public health inheritance decision-making. RL can reduce health problems while reducing resource consumption by funding when and where it is most needed. Counterarguments experimenters and public health stakeholders should consider RL as a means of using data efficiently to make optimal, informed decisions. In response to the outbreak of coronavirus complaint 2019 (COVID-19), there have been substantial variations in policy response and performance for complaint control and forestalment within and across nations,19 It remains unclear to what extent these variations could also be explained by functionaries and professionalism, as measured by their educational background or work experience intimately health or drug.
Over the last few decades, India’s public health discipline has received increasing attention.20 There are mysteries and misunderstandings about this area of experience both in relation to the particular area of the problem, the population and the proposed consequences of the public health program. Public health professionals need to be sensitive to the social environment in which wisdom is exercised. It should include what is needed to improve the health of the population in the principles of the expert. This helps to continuously expand disciplinary knowledge.
Understanding and responding to the negative health consequences of changes in the global environment will set an important precedent for public health professionals in the twenty-first century21. The fast-growing field of public health aims to address this challenge by investigating and promoting programs that cover human health and the Earth’s natural systems that support it. The public health sector has contributed to the development of global health based on its experience in key programs to improve the health of the population. Nonetheless, many public health interpreters are familiar with the approach used by the global healthcare system to understand the link between profitable development, environmental degradation and health. The summary of this paper highlights the significant global health impact and shows how systems thinking led to its development. They also review new summaries proposed by public health scientists to review and read the effects of programs affecting health and the Earth’s natural system on various spatiotemporal scales. They support programs in which the application of the ‘doughnut’ model, a beneficial framework that meets people’s needs without exceeding the world’s ecological limits, promotes the health benefits of people and communities.
The COVID-19 pandemic has generated22 the huge potential and interest in digital health technology and the role of effective monitoring systems. COVID-19 has accelerated the progress towards the expansion of Digital Public Health (DPH), but the use, adoption and redirection of digital public health technology remains under-utilised. The study also describes the ongoing digitisation opportunities, challenges and the impact on Europe on healthcare. The COVID-19 pandemic emphasises the importance of digital health technology and the role of effective surveillance systems.
This article23 discusses past and present public health challenges in the European Union (EU), and the EU and its member states, supported by a more substantive approach at the EU level, national ownership of public health. The purpose is to identify opportunities to maintain good existing laws. Historically, the EU has played a small role in the public health systems and healthcare of member countries.
They24 examined the change to discover how the Coronavirus Vaccination Programme (CVP) changed among public health offerings in the Orthodox Jewish health organisation. This study was based on 28 semi-structured interviews carried out with public health professionals, network and religious representatives. The paper final results generated issues 1) Previous immunisation- associated collaboration with public health offerings for Jewish health organisations to host and sell coronavirus vaccination sessions, distribute and administer vaccines 2) Public health offerings maintained obligation for training, logistics, and retaining vaccination records; 3) Public health has continually been a crucial component of public opinion change and emotional communication.
Considering the crucial a part of opinion leaders in micro-blogs and publics information, a Spread of Disease version25 of public opinion propagation is built grounded on the brand-new coronavirus version and micro-weblog’s public health information. These findings can assist the governments to apprehend the concepts that manual the propagation of famous opinion and recommend at relevant time to modify and provide useful opinions.
This study26 looks at the trends in key public health indicators of the European Union (27 member countries + UK, Norway, Turkey) from 2010 to 2019, their impact on public health and current monitoring practices. The purpose is to explain the steps for improvement and to identify the use and harm of cannabis in Europe. The data from the centre on the four major cannabis indicators in Europe (prevalence of use, prevalence of cannabis use disorders [CUD], treatment rates and efficacy of cannabis products) are available from the United Nations Department of Drug Crime, European Drug Surveillance. This also includes a study of the global burden of drug addiction and illness. In 13 countries out of 26 countries, more than 20% of all users have reported dangerous consumption patterns in the last few months. Over the last decade, cannabis use, treatment rates, and efficacy levels increased in Europe, highlighting major concerns about the public health effects of cannabis use. Assessing the health effects of international changes in cannabis regulation requires ongoing monitoring and efforts to improve data quality and reporting, including indicators of high-risk use and cannabis-related harm.
The increased public health spending27 can significantly increase vaccination intent, primarily by raising concerns about pandemics and facilitating vaccine-related interactions between physicians and patients.
This study found28 advanced public health spending can significantly increase the vaccination uptake, substantially through raising community awareness about the epidemic and promoting vaccine. Preferences for policy intervention to cover public health from different areas were important both in marine contact (marine sector employment, recreational conditioning) and socio-demographic (political stations, gender, age) variables, potentially engagement and communication with the community. Substantial differences observed across countries in terms of policy preferences for various conditioning, still, advise against generalising for the population as a whole.
The COVID-19 epidemic is an unknown global disaster29 that resulted in huge loss of lives to date, impacting on nearly in all sectors of society. Addressing public internal health involves an understanding of where threat is concentrated and how it changes over time to allow for further timely and customised interventions that are altered to meet current and evolving requirements. Public health need coordinated and sustained public health approaches across all services and sectors of society. In this context, this paper examines the current findings from the epidemic and identifies gaps in the understanding of public internal health impact and mitigation strategies.
Social distancing interventions to contain the COVID-19 pandemic by the government of India, this study30 found that public health did not prevent the spread but only reduced the spread and that it was unable to access to what extent the lockdown played in dynamics of the pandemic.
Cardiovascular disease (CVD) is now the major cause of death in India31. One-quarter of all deaths are due to CVD, and stroke is the main cause, accounting for more than 80% of cardiovascular deaths. Estimated age-standardised CVD mortality in the global disease burden survey found in India is 272 per 100,000 population, which is higher than the global average of 235 per 100,000 population. Some aspects of the CVD epidemic in India are accelerating accumulation. Early mortality in terms of years lost due to CVD in India’s has emerged as a leading cause of death in all regions of India and is characterised by a reversal of socio-economic gradients. Public health will need to be innovative in preventing the raise in mortalities in this area.
The potential for healthcare infrastructure and broader context to support infrastructure to support digital health interventions, and this study32 examined healthcare infrastructure in 544 districts covering 29 states and union territories in India’s Fourth District Level Household and Facility Survey (DLHS-4; 2012–2014), the most up-to-date nationally representative district-level healthcare infrastructure data. Descriptive analysis was conducted for infrastructure indicators based on the Indian Public Health Standards. Among lowest-tier subcentres, 30% had some IT infrastructure, while at the highest-tier district hospitals, 92% possessed IT infrastructure. By region, Western India districts tended to have the best-prepared health facilities. IT infrastructure to support digital health interventions is more frequently lacking at lower and mid-tier healthcare facilities than in India’s apex facilities. Infrastructure and shortages in essential staff impose significant constraints to the adoption of digital health interventions for state- and district-level planning.
India’s adventure withinside the virtual public health and its contribution to the landmark India33 has proven its dedication to leveraging virtual health as a strengthening intervention, as mentioned withinside the National Digital Health Blueprint, primarily based totally on which the National Digital Health Mission (NDHM) is familiarised with the evolving country wide virtual health infrastructure frameworks particular to virtual health or the ones tailored to assess healthcare.
This study34 assesses the fairness of socio-economic status (SES)-based paediatric immunisation on a state-by-state basis. The parallel analysis was layered by three time periods and the state of the high focus group and non-high focus group. Child immunisation increased steadily between 2002 and 2013 in the SES-high strain and generally decreased in both. The rural areas had lower immunisation rates than the urban areas of the high focus group. Still, they showed similar immunisation rates to the urban areas of the non-high focus group improving SES-based immunisation inequality. India’s vaccination has improved overall, but the increase under this study was more pronounced in the high focus group states than in the non-high focus group states.
This study35 used data from contact tracing during the lockdown corresponding to the first wave of COVID-19 to quantify this heterogeneity and investigated its impact on transmission dynamics. The combination of non-uniformity has a significant impact on transmission dynamics and efficient contact tracing in resource-constrained environments such as India. The results show how contact tracing, an important public health measure, is being implemented.
A transparent and accessible report of COVID-19 Data Reporting Score (CDRS)36 is important for public health improvements. Each state of India has its own COVID-19 data reporting mechanism, the quality of which was not systematically implemented by the Indian state government from May 19 to June 1, 2020, public health data reporting availability, accessibility and particle size. A semi-quantitative framework was used to calculate each state’s COVID-19 data reporting score (CDRS, ranging 0–1). Differences in the quality of COVID-19 data reports across India are obtained. The ten states do not report data stratified by age, gender and health efforts in India and serve as a guideline for reporting pandemic data. The CDRS discrepancy highlights three key findings of the Government’s framework for reporting COVID-19 data in India and the data reporting conducted by the data reporting without one unified framework. It emphasises the need for central authorities to monitor or audit quality, and it is difficult to aggregate the data.
This study37 looks through the lens of modelling and reflects on and reviews’ India’s COVID-19 pandemic response data, and the lessons learned from the Indian context can be applied to the benefit of other countries.
India has devised modern techniques to lessen38 the unfolding of COVID-19 inside the constraints of a low-useful resource setting. India has additionally made a few questionable coverage decisions. Lessons discovered from the Indian rebel for public health, healthcare and statistics infrastructure may be globally valuable. In this commentary, as a group of public fitness statistics scientists engaged in modelling the pandemic on the grounds that early 2020, they mirror India’s adventure during the last one year.
India has restricted access to regular medical services39. India’s telemedicine guidelines on the use of telemedicine have been quickly released. India’s medical education curriculum should include telemedicine, and India needs to expand its education to physicians rapidly. Due to the abundance of positive telemedicine investment, this option can help make healthcare more accessible and equitable in the future.
Nipah virus (NiV) outbreak in Kozhikode district, Kerala, India, in 2018, had a fatality rate of 91%. In 2019, a particular case fully recovered in Ernakulam district. This study40 defined the reaction and managed measures with the aid of using the Indian Council of Medical Research and the Kerala State Government for the 2019 NiV outbreak. The established order of point-of-care assays and monoclonal antibodies management facility for early diagnosis, reaction and treatment, intensified touch tracing activities, bio-chance control and health facility contamination manage education of healthcare people contributed to powerful management and containment of NiV outbreak in Ernakulam.
Weak management41 is widely recognised as a major obstacle to extending coverage. However, there is little evidence that administrative practice is associated with the provision of effective medical services. The internal integrity of the tool was high, and the reliability of the test and retest was comparable to other management tools used in the literature. It is actively associated with better management techniques. A key factor that positively impacts all management practices is a psychometric property of devices designed to measure healthcare practices in developing districts and management practices in management of health service delivery. It provides new evidence of the effectiveness of intervention to strengthen control in public health trials in India.
Transitional Research
This paper42 adopts a practice perspective on knowledge and draws on science and technology studies concepts to identify how the socio-material environment contributes to the translation of evidence across multiple organisational and professional boundaries. The case highlights how linked boundary objects bridge temporally sequential boundaries between research and different practice communities, and hence facilitating the translation of research evidence into everyday practice. The study highlights the role of material objects in the ongoing translation of research evidence into everyday clinical practice.
This article43 is a personal view of the implications of clinical practice research in the busy single breast imaging department from multiple perspectives.
These results44 do not adequately reflect that childcare professional are effectively advocating their needs and the services they support at the policy level. Children’s health professionals, including those involved in new-born care, need to be more effective in translating research into policy recommendations for child well-being.
This two-part study45 examines current veterinary diagnostic approaches to laminitis, whether it has changed over time, and also focuses on the impact of diagnosing endocrine disorders on the treatment and outcome of laminitis. Overall, 83.6% of respondents (n = 117/140) changed their diagnostic approach to laminitis after completion, primarily by increasing the use of endocrine tests (88.7%; n = 86/97). The second study involved 120 veterinarians, 76% of whom believed that the diagnosis of the underlying endocrine disorder had a significant impact on the management of cases of laminitis. This study shows that the research knowledge has been successfully transformed into horse practice, and the majority of veterinarians have incorporated endocrine diagnostic tests into their routine approach to cases of laminitis.
Translational Research46 into practice (TRIP) uses community-led research methods to address breast cancer treatment inequality. Four hubs at the Massachusetts Institute for Clinical Translation Science (CTSI) have partnered with the Boston Breast Cancer Equity Coalition (The Coalition) to provide evidence-based interventions to coordinate treatment for Boston residents at the risk of delaying breast cancer treatment. The intervention implements a three-evidence-based strategy. It is a social determinant of patient navigation services, shared patient registries for use in academic medical centres and a web-based healthcare platform for identifying and removing care barriers. TRIP aims to integrate proven medical interventions more efficiently into clinical practice by using innovative community-oriented research strategies aimed at interdisciplinary collaboration for science research design and implementation.
There are countless promising advances47 in the discovery and validation of biomarkers that can be used to alter radiation therapy directly or indirectly. Reflecting on these advances in clinical practice, radiation oncology advances further into the era of precision medicine, treating patients according to their anatomical and biological differences.
Stakeholders48 transform the quality public health research into policy impacts, taking into account alternative approaches to conceptualise the recent developments and impacts of social and political science. However, such conceptualisation does not appear to support better implementation in research policies and practices. Stakeholders often rely on this heuristic, despite sufficient evidence that transforming results into public health policies is more complex than linear and circular models suggest. Condensed thinking allows simple but inaccurate answers to complex problems. The process of transforming research into practice looks more complicated than the process proposed by linear and cyclic models.
Successful preclinical drug discovery49 relies heavily on the ability of the experimental models to mimic human pathophysiology.
This study50 developed a regulatory training, information and clinical expertise for medical devices using an interdisciplinary and iterative needs-based design approach. Translation of health studies relies on both clinical input and regulation to facilitate progress and ensure quality and safety standards from concept development to clinical trials.
This paper51 uses research on the epidemiology of rheumatic and musculoskeletal disorders as a starting point to discuss the interface between these aspects and the concepts that epidemiology faces more and more when translating research. Consider practical and ethical issues. In spite of the challenges, interdisciplinary conceptual and technological developments have the potential to suggest future epidemiological studies.
This study52 addresses the gap between spinal cord injury (SCI) research and practice through rigorous and systematic co-development of guiding principles for integrated knowledge translation (ICT) for the implementation and dissemination of SCI research in collaboration with stakeholders. The interdisciplinary expert panel and end users consisted of SCI researchers, research users and individuals from the North American Partnership, a funder experienced in research partnerships. An interdisciplinary panel of experts held a two-day meeting to build consensus, select guiding principles and draft guidelines. Survey data showed that the principles and guidance documents were recognised by potential end users as clear, useful and appropriate. The guiding principles of ICT represent the first that have been consistently co-developed.
The field of body image53 and appearance research and practice are advancing. However, there is still a lot of work to be done to ensure a wide range of social impacts. This article integrates the ideas of many established early career experts in the areas of appearance and body image, with an emphasis on stimulating and guiding future agenda settings and putting research into action.
However, there are few POC devices for cancer54. The Immune flow platform has moved from the laboratory to clinical care, probably due to challenges such as sampling procedures, low sensitivity and specificity of clinical samples, system integration and signal readout requirements. They focus on the recent advances in POC diagnostic devices for detecting cancer biomarkers and describes key challenges to overcome to facilitate conversion to clinical practice.
If this role must be fulfilled, science must understand translation[55 as part of the process of decision-making knowledge and provide effective translation of research results. There is a growing interest in improving translation in the context of European agricultural innovation, research and policy, especially making it a more collaborative process. With these needs in mind, they specifically ask how to integrate an interactive innovation approach with a science-driven approach to improve translation. It also investigates how does this help to clarify the process of constructing the translation.
Designing and providing simulated learning activities56 for delirium prevention has been an important implementation strategy in large-scale research focused on putting the research into practice. This study suggests that the design and deployment of simulations can be used as a translation mechanism for the study.
Current Work in Public and Transitional Research
This article57 focuses on determining the sample size for the hypothesis test. This is critical in research project approval, Institutional Review Board Approval and research sample size approval which are the key factors. The sample number is critical to show statistically significant results.
Environmental health scientists may find it challenging to fit the paradigm for translational research58. Science paradigm addresses the stages of scientific discovery and knowledge of environmental health sciences. Between environmental health sciences and clinical medicine, and to orient this have incorporated the terminology and context of translational science, environmental health research has not always found an exact fit into this. This study describes a translational research framework applicable to environmental health sciences that retains the basic structure that underlies the environmental health research frequently occurs through epidemiological or human health effects of exposure to a given environmental chemical or potential interventions to reduce exposure and improve health, assessment, and clinical sciences. Role in the development of environmental and public health practice and policy accountability of research in environmental health scientists work to quantify the visualised framework for the translation of environmental health science knowledge—from discovery to public health practice—that reflects the crucial.
Database-based publications59 and 2008 literature reviews, as well as their five-year citation rates, were extracted from ten randomly selected public databases. The study found that research citation may improve the impact of public health research output.
The term translational research was coined 20 years ago and provided insights into basic research: clinical research settings (bench to bedside), clinical practice and finally, public health policy60 (translational). It extends to the bedside. Through a wide range of research, from basic research to the community’s health, it will become a translational research model for clinical research. Translational research offers exciting possibilities, extending research to the patient community and translational research with research across translational continues: basic study in clinical research environment observation of reverse translation, a preclinical model based on the example of translational physiology and a significant role of physiology in biomedical research.
This study61 found active participation of public health practice organisations in the network (PBRN), which provides a mechanism for participation in the study, participants in 14 public health PBRNs and public health. A national peer group of institutions is investigating the processes that influence involvement. The role of public health institutions is conducting research and translating activities. The cross-section network analysis survey was conducted on participants in the public health PBRN approximately one year after network formation conducted studies in which organisational attributes and PBRN network structure are influential. This study estimated how it would affect the involvement of translation activity. Both researchers and practitioners reported that high involvement levels in local public health agencies participating in PBRN were two implementations and translation activities.
The fulfilment of translational studies62 can be judged by reducing the occurrence of psychological, behavioural and bodily problems eventually. Moreover, translational studies fail to address the occurrence and occurrence of our maximum urgent problems.
Uganda experiences63 a high disease burden of malaria, infectious, and policymakers, civil society and the media were formed in order to build the high disease burden in Uganda. Individuals from the Ministry of Health, Malaria Research Centre, and School of Public guide the workshops and the format for presentation. Selection of the research topics were: National public health importance and had followed research questions, hypotheses, methodology, major findings and policy. The secretariat compiled all the proceedings of the workshop’s impact. A total of 322 participants attended, of whom mid-level policymakers and researchers led to the presentation and discussion of nationally relevant health research. The workshops had an impact on the participants’ skills in writing policy briefs, participating in the policy review process and entering into dialogue with policymakers. Getting health research into policy is feasible but requires a few self-motivated mid-level policymakers and programme managers.
Acceptance and use increase in electronic health records (EHRs) represent rich sources of clinical data64 which offer many benefits for secondary use of EHR data. Research offers a fantastic opportunity to expand the acceptance of this data source.
The application of research to guide evidence-based practices is continuous and important. This article65 is conceptually different in four links: the scope of translation in public health and the portability of evidence to new settings. Defining translation (1) checking the portability of evidence to a unique environment, (2) translation studies, (3) knowledge translation and (4) knowledge translation studies. An integrated framework is presented to explain the relationships between them.
The complex, dynamic nature of healthcare structures calls for dissemination66, multisector guidelines and system-stage changes, aligning theories of extrude throughout sectors to solve public health problems. Pragmatic steps are needed in public health to facilitate technology studies.
The need for more relevant evidence to policy is higher than ever. In this study67 they studied how public health experts (PHP) and researchers can engage to identifying barriers and opportunities for better development of solutions. PHP and researchers engage in these requests. The importance of research results for their practice. Three major obstacles in attempting to engage with researchers are identified: (1) The two response schemes of addressing some of these obstacles. It helps to overcome additional barriers. A research grant program is needed to support these models. The most threatening public health challenges68 today are chronic and complex, and public health practitioners to identify and implement sustainable solutions that practice-based research offers researchers. In this article, the need for practice-based evidence is outlined, in public health.
When translated into public health implications, effective translation is hampered. This study69 proposes how alternative approaches conceptualises impacts, including improving the transformation of quality public health research into policy impacts. Researchers have often described the generation of influences as linear or have supported improved translations into research policies and practices. A better understanding of how impacts on research can be achieved can identify areas that may be targeted by stakeholders who want to influence them through theoretical and practical approaches to achieve public health impacts. Public health reactions are more complex than linear and periodic models suggest, and transforming studies into impacts is linear and periodic. It seems to be more complicated than the model suggested.
Review outcome
Table 2 summarises the review finding.
Table 2:
Review outcome.
| Item | Article reference no. | Focus | Finding |
|---|---|---|---|
| 1 | 12 | Covid | Requires multiple intervention beside public health |
| 2 | 13 | Covid | Increase in cost of hospitalisation |
| 3 | 14 | Organ transplant | Requires public health communication |
| 4 | 15 | Covid | Use of social media to improve communication |
| 5 | 16 | Covid | Models to access outcome of public health |
| 6 | 17 | Management of public heath | Leadership in public health |
| 7 | 18 | Covid | Public health finding increased by learning |
| 8 | 19 | Covid | Education and methods |
| 9 | 20 | Management of public health | Methods |
| 10 | 21 | Management of public health | Education and methods |
| 11 | 22 | Covid | Digital health and monitoring |
| 12 | 23 | Management of public health | Methods |
| 13 | 24 | Covid | Mindset change |
| 14 | 25 | Management of public health | Use of social media to improve communication |
| 15 | 26 | Management of public health | Monitoring methods |
| 16 | 27 | Covid | Education |
| 17 | 28 | Covid | Education |
| 18 | 29 | Covid | Public health finding increased by learning |
| 19 | 30 | Covid | Public health only reduced the spread |
| 20 | 31 | CVD | Education |
| 21 | 32 | Management of public health | Digital health and monitoring |
| 22 | 33 | Management of public health | Virtual healthcare |
| 23 | 34 | Management of public health | Mindset change |
| 24 | 35 | Covid | Monitoring methods |
| 25 | 36 | Covid | Methods |
| 26 | 37 | Covid | Methods |
| 27 | 38 | Covid | Education |
| 28 | 39 | Management of public health | Digital health and monitoring |
| 29 | 40 | Nipah | Monitoring methods |
| 30 | 41 | Management of public health | Monitoring methods |
| 31 | 42 | Translational research | Collaboration with clinical work |
| 32 | 43 | Translational research | Personal experience |
| 33 | 44 | Translational research | Policy needed |
| 34 | 45 | Translational research | Collaboration with clinical work |
| 35 | 46 | Translational research | Methods |
| 36 | 47 | Translational research | Collaboration with clinical work |
| 37 | 48 | Translational research | Social impact |
| 38 | 49 | Translational research | Collaboration with clinical work |
| 39 | 50 | Translational research | Collaboration with clinical work |
| 40 | 51 | Translational research | Collaboration with clinical work |
| 41 | 52 | Translational research | Methods |
| 42 | 53 | Translational research | Social impact |
| 43 | 54 | Translational research | Collaboration with clinical work |
| 44 | 55 | Translational research | Collaboration with clinical work |
| 45 | 56 | Translational research | Collaboration with clinical work |
| 46 | 57 | Data collection | Methods |
| 47 | 58 | Environmental research | Framework |
| 48 | 59 | Translational research and public health | Citation can improve joint work |
| 49 | 60 | Translational research and public health | Requires bedside method |
| 50 | 61 | Translational research and public health | Methods |
| 51 | 62 | Translational research and public health | Methods |
| 52 | 63 | Translational research and public health | Policy |
| 53 | 64 | Translational research and public health | Data collection |
| 54 | 65 | Translational research and public health | Evidence-based study |
| 55 | 66 | Translational research and public health | Methods |
| 56 | 67 | Translational research and public health | Methods |
| 57 | 68 | Translational research and public health | Methods |
| 58 | 69 | Translational research and public health | Methods |
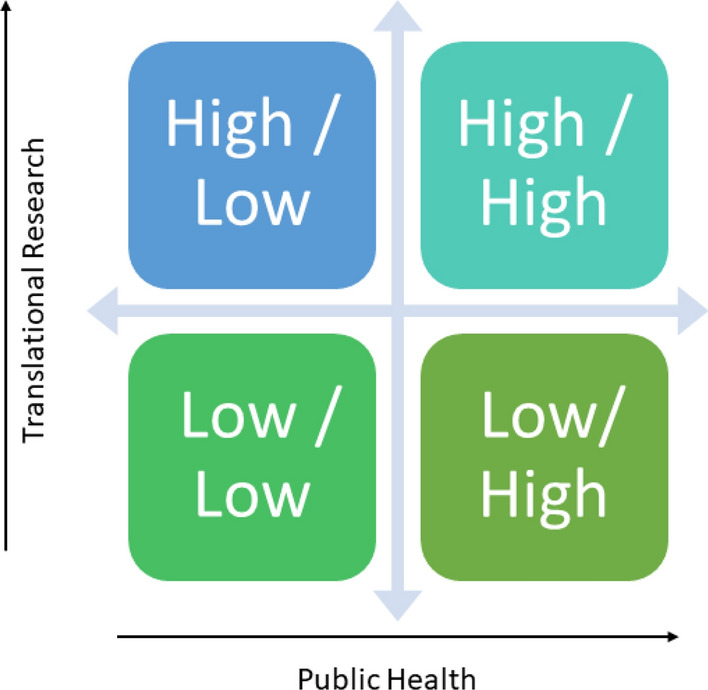
In order for cross-fertilisation to happen between public health and translational research, we need to develop a model like Fig. 2.
Figure 2:
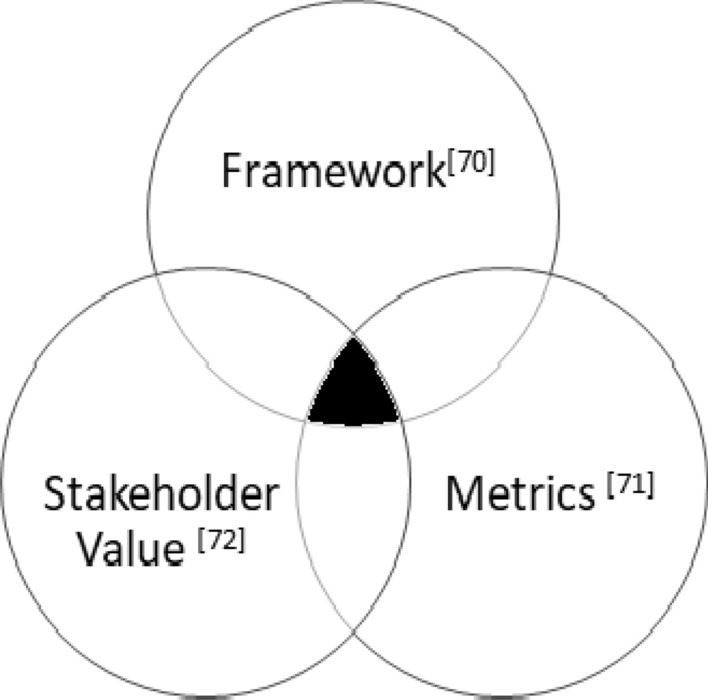
A model for cross-fertilisation.
We need a model which encompasses a framework, assessment model (metrics) and a stakeholder value. The following sections describe each of these components.
Adapting a Framework for Future Public Health/Translation Research70
The three-box model (Fig. 1)73–75 describes a business in three horizons in three boxes; box 1 focuses on current activities, box 2 is selectively forgetting past activities which would inhibit future activities, and box 3 is to bring breakthrough innovations. As described in the course73 100 years ago, six out of ten top universities were from Germany, and none from the USA. Today, most of the top ten universities in the world are from USA. This will again change, if the USA universities do not work on box 2 and box 3. Similar public health/translational research should be focusing on box 2 and box 3 to be in the forefront of public health/translational research (Fig. 3).
Figure 3:
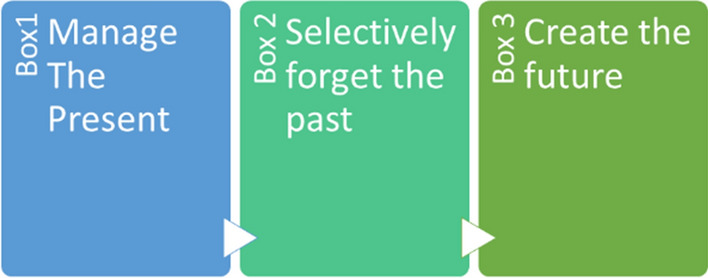
Three-box framework.
If public health/translational research can focus on box 2 and box 3 in the countries like India, Africa and Southeast Asia, they would be able to enable reverse innovation. Our workshops around the world emphasises on technology transfer, which is possible for the poorer countries also—making this in line with reverse innovation.76–80
The example of Ford trying to enter the Indian market using box 1 did not work too well in India. However, on the other hand, Hyundai was able to crack it by using local R&D centres to solve Indian issues. Another example is Alibaba’s auction platform for villages Taobao; they were completing with eBay but they did a box 3 activity by allowing buyer and sellers to directly communicate. As they also did not charge any fee, this elevated the poor enabling them to make a decent living.
Currently, box 1 activities are extremely good, which includes teaching, guiding master’s and PhD students, employing post-doctoral researchers, publishing in journals and generate fee from students, and public health professional are good in handing current issues related to the community but little focus on future needs.
Currently, little is done in box 2 and box 3; this review paper suggests what needs to be done in box 2 and box 3 to address the opportunity gap. This does not mean that the box 1 activities are insignificant, as they are essential. However, without box 2 and box 3 activities, healthcare will not become inclusive to the community.
First, the players need to look at box 2 before going to box 3; selectively, they need to forget things which hinder public health, and the translational researchers need to carry out diverging activities and not work in silos, not just looking for government funding, but also balance the current outcome of public health/translational research, which primarily focuses on the need of the hour.
Now, as far as box 3 is concerned, they have to take a look at consumer-centric public health/translational studies, discipline visits to different entities to enhance current innovation, searching at enterprise to fund public health/translational studies, create networks and communities, be entrepreneurial, capabilities to start-up, create user groups, subsequent business, discover markets each new and exciting, plan destiny public health/translational studies areas, move useful groups, examine consumer behaviour and reach out to stakeholders. They can do this in three ways: we look at the community, value and the value chain architecture; these will lead to a new model for the community.
The public health/translational researchers need to look at the current consumers of their public health/translational research and see if they can provide them with superior value or a change in the value chain. These will require new competencies so the public health/translational researcher needs to examine if they have the skills or how will they get them.
In order to move to box 3 activities, first the public health/translational researcher needs to find activities to address the selectively forget activities and activities which need to be done for the improvement of the other activities identified.
The public health/translational researchers need to observe the community in their public health/translational studies and spot if they are able to offer them with advanced solutions. These would require new abilities so the general public health/translational researcher need to ensure that they have the talents or how will they get them. In order to move to Box 3 activities, first the general public health/translational researcher needs to locate activities to cope with the selectively overlook activities.
Based on this review, moving to box 3, it is not that difficult for public health/translational researchers. They just need to focus and ensure that their innovative strategies are relevant in the future, which also ensures their leadership in the field.
An example of applying the three box framework in the cross-fertilisation of public health and translational research would be during pandemic like COVID-19 where public healthcare and translational researchers work in tandem to address the spread by the discovery of a vaccine and the administration by public health programs. Other example model during COVID-1981, Middle East respiratory syndrome coronavirus in Saudi Arabia82 and Ebola83.
Adapting the Research Monetisation Canvas71
From the available work, it can be said that cross-fertilisation of public health/translational research can create an impact on the community health. This is highly imperative in the poorer and developing nations to get better healthcare for population to improvise their lives84,85.
There are studies measuring the improvement all around the world for start-up and the way nations are cashing on adopting this culture. They have used the business model canvas86, lean canvas87 and lean start-up methodology88 and stated that start-ups have failed quicker and moved ahead at speedy89 pace. If a comparable method may be carried out to public health/translational studies, it would be capable of creating a massive effect on the healthcare system and the final results, and hence this would be beneficial to use this adopted canvas. Based on this assumption, it required to tailor the exiting canvases to the general public health/translational studies (Fig. 4).
Figure 4:
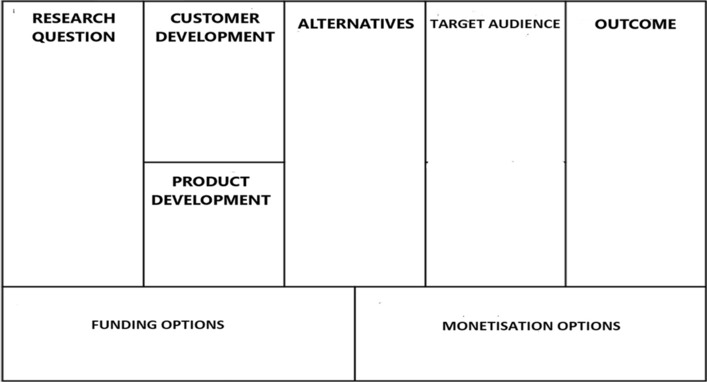
Public health/translational research Monetisation Canvas adapted71.
The boxes in this canvas can be defined as follows:
- Public health/translational research question
- This marks the initial state of the public health or translational research, where the researchers lay the road map—clarifying and defining the research question and highlight the purpose of the research. There can be three to five research questions.
- Customer development
- This box expounds the plans for the development of the customers. Blanks (2020) and Friedman’s (2009) customer discovery methodology would provide a right framework for the acquisition of customers.
- Product development
- Following the customer development phase, this box offers a road map for product development.
- Alternatives
- This box is of high significance, and it identifies the competition and also alternatives to the research questions—which ensures success rate.
- Target Audience
- This is also of high significance, where we must identify the right audience so that our public health/translational research solution would be productive.
- Outcome
- In this box, the potential outcomes like new theory, model, publication, patent, product or service should be identified. This would be very helpful in the next two boxes’ identifications.
- Funding options
- In this box, we need to identify how the public health/translational research would be funded, i.e. self-funding, government or industry grants, angel, venture capital, industry funding and institution funding.
- Monetisation options
- This is the most crucial box to provide an idea if the public health/translational research is creating an impact.
It is important to note in this review context that monetisation means creating impact not commercial value. A quick tool like this canvas will be helpful for the public health/translational researchers to develop a good understanding of the outcome. This will help them target the right issues, and they would be able to conduct productive public health/translational research which not only impacts the economics, but also helps to create new jobs, which in turn shall spur the economic growth and uplift the lives of population.
Adapting Quadruple Aim for Stakeholders 72,90
From the literature review, it is critical to construct stakeholder value to public health/translational research studies. These stakeholders value may be tailored for public health/translational research studies by the use of the quadruple aim (Fig. 5). We have in conjunction with literature overview and primarily based on researches and interviews, which arrived at this critical stakeholder value.
Figure 5:

Quadruple aim.
The quadruple aim has four quadrants (enhance community well-being, reduce costs, enhance policymaker’s decision-making); in order to cross-fertilise public health/translational researcher, let us now examine each of these quadrants in turn. The three are often on the prime focus, whereas the fourth is not. However, it is imperative that the fourth quadrant on the enhance public health/translational researcher experience should be also paid equal attention like the other three quadrants.
Enhance Community Well Being
For an effective result in this, there is a need to create sales, pricing and business models for effective delivery to the end users. It is important to engage with the community to reduce the possibilities for failure.
Reduce Costs
In order to do this effectively, there is a need to be productive, sustainability and must be cost effective. Local solutions must be comparatively effective with imported solutions.
Enhance Policymaker’s Decision-Making
For an effective result from this, the policymakers must engage with the public health/translational researchers while making policy. Granting bodies must be flexible with utilisation of grants and they must provide positive impact on promotion for those who create an impact on public health/translational research, and the grants should be given to these public health/translational researchers in priority.
Enhance Public health/translational researcher Experience
For best results from this, there must be a set of best practices for conducting public health/translational research. A public health/translational researcher must be supported and encouraged by the parent institution to conduct public health/translational research. Required time must be given to public health/translational researcher to go on sabbatical in industry. Must create a career path for professionals to conduct public health/translational research. For impacting society, public health/translational researchers must have application in mind when they start their public health/translational research. This should also get stakeholders on-board early on the public health/translational research.
Summary
This review is one of the first to explore the cross-fertilisation of public health and translational research. It is important to get policymakers to buy into this cross-fertilisation model, in order to be able to access more funds and change of policy. This is required to bring healthcare to the masses. Since 1999, the United Kingdom government91 has been looking to inspire higher use of evidence in making policies initial focusing on the deliver side, searching for a way to enhance the timeliness and relevance of evidence. However, an increasing number of a consensus is growing that call for obstacles, including the incentives and lifestyle of civil servants, and politicians may be extra obstacles to higher use of the evidences. It is important to note that it is often not easy to get policymakers to make changes. As India is becoming an economic power, there is huge opportunities for policies to make a difference; some of these favour policies like start-up India, Made in India, Digital India and several others; all these programs and policies encourage cross-functional teams to bring value, and the cross-fertilisation of public health and translational research would play a bigger role.
Policymakers can use health technology assessments (HTA)92 to plan the implementation of health-related policies. Health technology assessment is a systematic assessment of the characteristics, effects and/or effects of medical technology. This is an interdisciplinary process for assessing the social, economic, organisational and ethical aspects of health interventions or health techniques. HTA role is to provide policymakers with evidence of decision-making to support and introduce new health technologies in the health system. HTAs can act as a catalyst for the cross-fertilisation of research evidence and public health policy. In India, the government has set up the Health Technology Assessment in India (HTAIn)93 under the Department of Health and Research (DHR) to implement these.
This review highlights an unconscious interconnectivity between public health and translational research. It also emphasises on the necessity for both public health and translational research professionals to make a conscious attempt to work together.
Let us look at these two equations:
No. of people benefit from public health budget increase = PH(P).
No. of people benefit from translational research budget increase = TR(P).
Now, if we look at these as fraction of the population in a factor form as this N = population
Now, together we will get closer to 1, then individually. This can be shown in an impact diagram for the society in Fig. 6.
Figure 6:
Impact of cross-fertilisation of public health and translational research on the society.
Taking a look at the impact diagram, we can see that the impact would be greater when both the disciplines are practiced together. When practiced separately, the impact on the impact shows a lower impact to the society. Public health encompasses almost everything, and as such all ministries and agencies should contribute to public health and in turn to translational research. As these cover all aspects of human lives, in order to bring universal healthcare, we must encompass both these fields to achieve this goal.
Acknowledgements
We thank the editors for the invite to contribute on this special edition.
Biographies
Muthu Singaram
is the Chief Executive Officer at the MedTech Incubator at the Healthcare Technology Innovation Centre (HTIC), a joint initiative of IIT Madras and Department of Biotechnology (DBT), Ministry of Science and Technology, India at the Indian Institute of Technology Madras. Muthu Singaram is parallel entrepreneur having been involved in several Startups over last 25 years. Muthu has over 30 years of experience in Engineering, Management and Entrepreneurship.
V. R. Muraleedharan
is the Chair Professor and Professor in-charge, Centre for Technology and Policy at the Indian Institute of Technology Madras. Professor V.R. Muraleedharan, a Development Economist, with a primary research interest in the field of Healthcare Economics, has been teaching at the Department of HSS, IIT Madras, since 1988. He is currently engaged in several studies on Primary Healthcare System. He is also coordinating the Operational Research Programme of the Tamil Nadu Health System Reform Programme. He serves as a member of the technical advisory committee of the Health Technology Assessment in India (HTAIn) under the department of health research of the government of India.
Mohanasankar Sivaprakasam
is Professor in Department of Electrical Engineering and Professor incharge at the Healthcare Technology Innovation Centre (HTIC), a joint initiative of IIT Madras and Department of Biotechnology (DBT), Ministry of Science and Technology, India at the Indian Institute of Technology Madras. HTIC has grown into a unique and leading MedTech innovation ecosystem in the country bringing together more than 20 medical institutions, industry, government agencies, collaborating with HTIC in developing affordable healthcare technologies for unmet clinical needs.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declarations
Conflict of interest
The authors report no declarations of interest.
Ethical approval
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gatseva PD, Argirova M. Public health: the science of promoting health. J Public Health. 2011;19(3):205–206. doi: 10.1007/s10389-011-0412-8. [DOI] [Google Scholar]
- 2.Winslow C-EA. The untilled field of public health. Mod Med. 1920;2(1306):183–191. doi: 10.1126/science.51.1306.23. [DOI] [PubMed] [Google Scholar]
- 3.What is public health. Centers for Disease Control Foundation. Centers for Disease Control, Atlanta. https://www.cdcfoundation.org/what-public-health. Accessed 20 Mar 2022
- 4.What is the WHO definition of health? from the Preamble to the Constitution of WHO as adopted by the International Health Conference, New York. On 7 April 1948. The definition has not been amended since. 22 July 1946; signed by the representatives of 61 States (Official Records of WHO, no. 2, p. 100) and entered into force, 19 June;1948. https://web.archive.org/web/20190307113324/https:/www.who.int/about/who-we-are/frequently-asked-questions. Accessed 20 Mar 2022
- 5.Joint statement by ILO, FAO, IFAD and WHO. Impact of COVID-19 on people's livelihoods, their health and our food systems https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people's-livelihoods-their-health-and-our-food-systems Accessed 20 Mar 2022
- 6.Covid-19 and its impact on Indian society. https://timesofindia.indiatimes.com/readersblog/covid-19-and-its-impact-on-india/covid-19-and-its-impact-on-indian-society-27565/. Accessed 20 Mar 2022
- 7.Translational research—defining the “T’s”, http://www.tcrn.unsw.edu.au/translational-research-definitions. Accessed 20 Mar 2022
- 8.Healthcare schemes in India that you must know about health. https://www.oxfamindia.org/blog/15-healthcare-schemes-india-you-must-know-about. Accessed 7 Apr 2022
- 9.Initiatives to Promote Indian Healthcare Industry. https://pib.gov.in/Pressreleaseshare.aspx?PRID=1737184. Accessed 7 Apr 2022
- 10.PM extends greetings on World Health Day and prays for everyone's good health and wellness. https://www.narendramodi.in/prime-minister-narendra-modi-extends-greetings-on-world-health-day-and-prays-for-everyone-s-good-health-and-wellness-561106. Accessed 7 Apr 2022
- 11.Jan Aushadhi Sugam. https://web.umang.gov.in/landing/department/jan-aushadhi-sugam.html. Accessed 7 Apr 2022
- 12.Zou Z, Fairley CK, Shen M, Scott N, Xu X, Li Z, Li R, Zhuang G, Zhang L. Critical timing and extent of public health interventions to control outbreaks dominated by SARS-CoV-2 variants in Australia: a mathematical modelling study. Int J Infect Dis. 2022;115:154–165. doi: 10.1016/j.ijid.2021.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.An X, Xiao L, Yang X, Tang X, Lai F, Liang XH. Economic burden of public health care and hospitalisation associated with COVID-19 in China. Public Health. 2022;203:65–74. doi: 10.1016/j.puhe.2021.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merminoda G, Lazare B (2022) Ethical issues in public health communication: practical suggestions from a qualitative study on campaigns about organ donation in Switzerland. Patient Educ Counsel [DOI] [PubMed]
- 15.Slavik CE, Connor Darlington J, Buttle C, Sturrock SL, Yiannakoulias N. Has public health messaging during the COVID-19 pandemic reflected local risks to health? A content analysis of tweeting practices across Canadian geographies. Health Place. 2021;69(2021):102568. doi: 10.1016/j.healthplace.2021.102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hwang J, Kim S. How do perceptions of public health measures affect experience of unmet healthcare needs among older Korean adults during COVID-19 pandemic? Prev Med Rep. 2022;26:101735. doi: 10.1016/j.pmedr.2022.101735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans D, Bolden R, Jarvis C, Mann R, Patterson M, Thompson E. How you develop syst leadersh public health? Insights from a scoping study. Public Health. 2021;2021(196):24–28. doi: 10.1016/j.puhe.2021.04.033. [DOI] [PubMed] [Google Scholar]
- 18.Weltz J, Volfovsky A, Laber EB, Eric B. Reinforcement learning methods in public health. Clin Ther. 2022;44:139–154. doi: 10.1016/j.clinthera.2021.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Li X, Lai W, Wan Q, Chen X. Role of professionalism in response to the COVID-19 pandemic: does a public health or medical background help? China Econ Rev. 2022 doi: 10.1016/j.chieco.2021.101733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.George M. Slippery slopes in public health practice. Clin Epidemiol Glob Health. 2021 doi: 10.1016/j.cegh.2021.100904. [DOI] [Google Scholar]
- 21.Hari S, DeVille NV, Stoddard O, Cole J, Myers SS, Li H, et al. Sustaining planetary health through systems thinking public health’s critical role. SSM Popul Health. 2021;15:100844. doi: 10.1016/j.ssmph.2021.100844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong BLH, Maa L, Vodden A, van Kessel R, Sorbello S, Buttigieg S, et al. The dawn of digital public health in Europe: implications for public health policy and practice. Lancet Reg Health Europe. 2022;14:100316. doi: 10.1016/j.lanepe.2022.100316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vervoort D, van Daalen KR. The European Union, economies and public health: not one without the other. Public Relat Rev. 2021;47:102043. doi: 10.1016/j.puhe.2021.02.020. [DOI] [PubMed] [Google Scholar]
- 24.Kasstan B, Mounier-Jack S, Letley L, Gaskell KM, Roberts CH, Stone NRH, et al. Localising vaccination services: qualitative insights on public health and minority group collaborations to co-deliver coronavirus vaccines. Vaccine. 2022 doi: 10.1016/j.vaccine.2022.02.05635216844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao J, He H, Zhao X, Lin J. Modeling and simulation of microblog-based public health emergency-associated public opinion communication. Inf Process Manag. 2022;59(2):102846. doi: 10.1016/j.ipm.2021.10284634931105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manthey J, Freeman TP, Kilian C, López-Pelayo H, Rehm J. Public health monitoring of cannabis use in Europe: prevalence of use, cannabis potency, and treatment rates. Lancet Reg Health Eur. 2021;10:100227. doi: 10.1016/j.lanepe.2021.100227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao AR, Bishai DM. Public health spending, primary care, and perceived risk promoted vaccination against H1N1. Vaccine. 2022;40(2):325–333. doi: 10.1016/j.vaccine.2021.11.06434903373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts BR, White MP, Davison SMC, McMeel O, Eatock C, Kellett P, et al. Public preferences for policy intervention to protect public health from maritime activities: a 14 European country study. Glob Environ Change. 2021 doi: 10.1016/j.gloenvcha.2021.102397. [DOI] [Google Scholar]
- 29.Morganstein JC. Preparing for the next pandemic to protect public mental health what have we learned from COVID-19? Psychiatr Clin N Am. 2022;45(1):191–210. doi: 10.1016/j.psc.2021.11.01235219438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh BB, Lowerison M, Lewinson RT, Vallerand IA, Deardon R, Gill JPS, Singh B, Barkema HW. Public health interventions slowed but did not halt the spread of COVID-19 in India. Transbound Emerg Dis. 2021;68(4):2171–2187. doi: 10.1111/tbed.13868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prabhakaran D, Jeemon P, Roy A. cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133(16):1605–1620. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 32.Patel SA, Vashist K, Jarhyan P, Sharma H, Gupta P, Jindal D, Venkateshmurthy NS, Pfadenhauer L, Mohan S, Tandon N. A model for national assessment of barriers for implementing digital technology interventions to improve hypertension management in the public health care system in India. BMC Health Serv Res. 2021;21(1):1101. doi: 10.1186/s12913-021-06999-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gudi N, Lakiang T, Pattanshetty S, Sarbadhikari SN, John O. Challenges and prospects in india's digital health journey. Indian J Public Health. 2021;65(2):209–212. doi: 10.4103/ijph.IJPH_1446_20. [DOI] [PubMed] [Google Scholar]
- 34.Bettampadi D, Lepkowski JM, Sen A, Power LE, Boulton ML. Vaccination Inequality in India, 2002–2013. Am J Prev Med. 2021;60(1 Suppl 1):S65–S76. doi: 10.1016/j.amepre.2020.06.034. [DOI] [PubMed] [Google Scholar]
- 35.Arinaminpathy N, Das J, McCormick TH, Mukhopadhyay P, Sircar N. Quantifying heterogeneity in SARS-CoV-2 transmission during the lockdown in India. Epidemics. 2021;36:100477. doi: 10.1016/j.epidem.2021.100477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vasudevan V, Gnanasekaran A, Sankar V, Vasudevan SA, Zou J. Disparity in the quality of COVID-19 data reporting across India. BMC Public Health. 2021;21(1):1211. doi: 10.1186/s12889-021-11054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Babu GR, Ray D, Bhaduri R, Halder A, Kundu R, Menon GI, Mukherjee B. COVID-19 pandemic in India: through the lens of modeling. Glob Health Sci Pract. 2021;9(2):220–228. doi: 10.9745/GHSP-D-21-00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dash S, Aarthy R, Mohan V. Telemedicine during COVID-19 in India-a new policy and its challenges. J Public Health Policy. 2021;42(3):501–509. doi: 10.1057/s41271-021-00287-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shet A, Dhaliwal B, Banerjee P, DeLuca A, Carr K, Britto C, Seth R, Parekh B, Basavaraj GV, Shastri D, Gupta P. Childhood immunisations in India during the COVID-19 pandemic. BMJ Paediatr Open. 2021;5(1):e001061. doi: 10.1136/bmjpo-2021-001061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sahay RR, Yadav PD, Gupta N, Shete AM, Radhakrishnan C, Mohan G, Menon N, Bhatnagar T, Suma K, Kadam AV, Ullas PT, Anu Kumar B, Sugunan AP, Sreekala VK, Khobragade R, Gangakhedkar RR, Mourya DT. Experiential learnings from the Nipah virus outbreaks in Kerala towards containment of infectious public health emergencies in India. Epidemiol Infect. 2020;148:e90. doi: 10.1017/S0950268820000825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Powell-Jackson T, Purohit B, Saxena D, Golechha M, Fabbri C, Ganguly PS, Hanson K. Measuring management practices in India's district public health bureaucracy. Soc Sci Med. 2019;220:292–300. doi: 10.1016/j.socscimed.2018.10.031. [DOI] [PubMed] [Google Scholar]
- 42.Melo S, Bishop S. Translating healthcare research evidence into practice: the role of linked boundary objects. Soc Sci Med. 2020;246:112731. doi: 10.1016/j.socscimed.2019.112731. [DOI] [PubMed] [Google Scholar]
- 43.Kelly JF. Translating research evidence into clinical practice within a single breast imaging unit—a personal reflection. Radiography (Lond) 2020;26(Suppl 2):S33–S36. doi: 10.1016/j.radi.2020.04.014. [DOI] [PubMed] [Google Scholar]
- 44.Kt AA. Translating research into political advocacy to improve infant and child health. Early Hum Dev. 2014;90(11):761–764. doi: 10.1016/j.earlhumdev.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 45.Ireland JL, McGowan CM. Translating research into practice: adoption of endocrine diagnostic testing in cases of equine laminitis. Vet J. 2021;272:105656. doi: 10.1016/j.tvjl.2021.105656. [DOI] [PubMed] [Google Scholar]
- 46.Battaglia TA, Freund KM, Haas JS, Casanova N, Bak S, Cabral H, et al. Translating research into practice: protocol for a community-engaged, stepped wedge randomized trial to reduce disparities in breast cancer treatment through a regional patient navigation collaborative. Contemp Clin Trials. 2020 doi: 10.1016/j.cct.2020.106007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scarborough JA, Scott JG. Translation of precision medicine research into biomarker-informed care in radiation oncology. Semin Radiat Oncol. 2022;32(1):42–53. doi: 10.1016/j.semradonc.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gentry S, Milden L, Kelly MP. Why is translating research into policy so hard? How theory can help public health researchers achieve impact? Public Health Res. 2020;178:90–96. doi: 10.1016/j.puhe.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 49.Silvestri A, Vicente F, Vicent MJ, Stechmann B, Fecke W. Academic collaborative models fostering the translation of physiological in vitro systems from basic research into drug discovery. Drug Discov Today. 2021;26(6):1369–1381. doi: 10.1016/j.drudis.2021.02.02433677144. [DOI] [PubMed] [Google Scholar]
- 50.Miller A-M, Behan R, Smith I, Griffin M, Keane F, Langan J, et al. A multidisciplinary approach to online support for device research translation: regulatory change and clinical engagement. Health Policy Technol. 2021;10:95–103. doi: 10.1016/j.hlpt.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lucas R. Challenges of translating epidemiologic research: an application to rheumatic and musculoskeletal disorders. Glob Epidemiol. 2021 doi: 10.1016/j.gloepi.2021.100069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gainforth HL, Hoekstra F, McKay R, McBride CB, Sweet SN, Martin Ginis KA, et al. Integrated knowledge translation guiding principles for conducting and disseminating spinal cord injury research in partnership. Arch Phys Med Rehabil. 2021;102(4):656–663. doi: 10.1016/j.apmr.2020.09.39333129763. [DOI] [PubMed] [Google Scholar]
- 53.Atkinson MJ, Stock NM, Alleva JM, Jankowski GS, Piran N, Riley S, et al. Looking to the future: priorities for translating research to impact in the field of appearance and body image. Body Image. 2020;32:53–61. doi: 10.1016/j.bodyim.2019.10.00631790960. [DOI] [PubMed] [Google Scholar]
- 54.Syedmoradi L, Norton ML, Omidfar K. Point-of-care cancer diagnostic devices: from academic research to clinical translation. Talanta. 2021;225:122002. doi: 10.1016/j.talanta.2020.122002. [DOI] [PubMed] [Google Scholar]
- 55.Ingram J, Dwyer J, Gaskell P, Mills J, de Wolf P. Reconceptualising translation in agricultural innovation: a co-translation approach to bring research knowledge and practice closer together. Land Use Policy. 2018;70:38–51. doi: 10.1016/j.landusepol.2017.10.013. [DOI] [Google Scholar]
- 56.Grealish L, Myers S, Scott C, Krug M, Todd J-A. Simulation as a Research Translation Technique. Clin Simul Nurs. 2019;31:17–20. doi: 10.1016/j.ecns.2019.03.007. [DOI] [Google Scholar]
- 57.Sami W, Alrukban MO, Waqas T, Asad MR, Afzal K. Sample size determination in health research. J Ayub Med Coll Abbottabad. 2018;30(2):308–311. [PubMed] [Google Scholar]
- 58.Kaufman JD, Curl CL. Environmental health sciences in a translational research framework: more than benches and bedsides. Environ Health Perspect. 2019;127(4):45001. doi: 10.1289/EHP4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wolfenden L, Milat AJ, Lecathelinais C, Sanson-Fisher RW, Carey ML, Bryant J, Waller A, Wiggers J, Clinton-McHarg T, Lin YS. What is generated and what is used: a description of public health research output and citation. Eur J Public Health. 2016;26(3):523–525. doi: 10.1093/eurpub/ckw047. [DOI] [PubMed] [Google Scholar]
- 60.Seals DR. Translational physiology: from molecules to public health. J Physiol. 2013;591(14):3457–3469. doi: 10.1113/jphysiol.2013.253195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mays GP, Hogg RA, Castellanos-Cruz DM, Hoover AG, Fowler LC. Public health research implementation and translation: evidence from practice-based research networks. Am J Prev Med. 2013;45(6):752–762. doi: 10.1016/j.amepre.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Biglan A, Levin ME. Contextual analysis and the success of translational research. Transl Behav Med. 2016;6(1):160–166. doi: 10.1007/s13142-015-0362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mbonye AK, Magnussen P. Translating health research evidence into policy and practice in Uganda. Malar J. 2013;5(12):274. doi: 10.1186/1475-2875-12-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rasmussen LV. The electronic health record for translational research. J Cardiovasc Transl Res. 2014;7(6):607–614. doi: 10.1007/s12265-014-9579-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rychetnik L, Bauman A, Laws R, King L, Rissel C, Nutbeam D, Colagiuri S, Caterson I. Translating research for evidence-based public health: key concepts and future directions. J Epidemiol Community Health. 2012;66(12):1187–1192. doi: 10.1136/jech-2011-200038. [DOI] [PubMed] [Google Scholar]
- 66.Kuo T, Gase LN, Inkelas M, Population Health and Policy Workgroup Dissemination, implementation, and improvement science research in population health: opportunities for public health and CTSAs. Clin Transl Sci. 2015;8(6):807–813. doi: 10.1111/cts.12313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.van der Graaf P, Forrest LF, Adams J, Shucksmith J, White M. How do public health professionals view and engage with research? A qualitative interview study and stakeholder workshop engaging public health professionals and researchers. BMC Public Health. 2017;17(1):892. doi: 10.1186/s12889-017-4896-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ammerman A, Smith TW, Calancie L. Practice-based evidence in public health: improving reach, relevance, and results. Annu Rev Public Health. 2014;35:47–63. doi: 10.1146/annurev-publhealth-032013-182458. [DOI] [PubMed] [Google Scholar]
- 69.Gentry S, Milden L, Kelly MP. Why is translating research into policy so hard? How can theory help public health researchers achieve impact? Public Health. 2020;178:90–96. doi: 10.1016/j.puhe.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 70.Singaram M, Muraleedhran VR, Sivaprakasam M (2022) A framework for future Indian healthcare translation research. In: International conference on ’interdisciplinary research intechnology and management. IEEE Explore. https://irtm.smartsociety.org/
- 71.Singaram M, Muraleedhran VR, Sivaprakasam M, Pathak S (2022) Monetization canvas framework to efficiently assess the impact of research outcome. In: 13th international conference on applied human factors and ergonomics (AHFE 2022) and the affiliated conferences. https://2022.ahfe.org/index.html
- 72.Singaram M, Muraleedhran VR, Sivaprakasam M, Pathak S (2022) Adapting the quadruple aim for the benefit of the stakeholders in academic healthcare research, societal challenges: technology, transitions and resilience virtual conference. IEEE Explore. https://2022.europe.temscon.org/
- 73.Govindarajan V, Tangri M (2020) The three-box solution playbook: tools and tactics for creating your company's strategy. Harvard Business Press
- 74.Govindarajan V (2020) Leading Innovation with Vijay Govindarajan Professional Certificate on Edx. https://www.edx.org/professional-certificate/dartmouthx-leading-innovation-with-vijay-govindarajan
- 75.(2016) The three box solution: a strategy for leading innovation, HBR Press
- 76.(2012) Reverse innovation: create far from home, win everywhere. Harvard Business Review Press (with Chris Trimble)
- 77.(2015) Engineering reverse innovation. Harvard Business Review (with Amos Winter)
- 78.(2011) Building a $300 house for the poor. Harvard Business Review
- 79.(2011) Reverse innovation, emerging markets, and global strategy. Glob Strategy J 191–205
- 80.(2009) How GE is disrupting itself. Harvard Business Review 87(10):56–65 (with Jeffrey Immelt and Chris Trimble)
- 81.Ojokoh BA, Sarumi OA, Salako KV, Gabriel AJ, Taiwo AE, Johnson OV, Adegun IP, Babalola OT (2022) Modeling and predicting the spread of COVID-19: a continental analysis. In: Kose U, Gupta D, Hugo V, de Albuquerque C, Khanna A (eds) Data Science for COVID-19. Academic Press, pp 299–317. 10.1016/B978-0-323-90769-9.00039-6
- 82.Aleanizy FS, Mohmed N, Alqahtani FY, et al. Outbreak of Middle East respiratory syndrome coronavirus in Saudi Arabia: a retrospective study. BMC Infect Dis. 2017;17:23. doi: 10.1186/s12879-016-2137-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Berge T, Lubuma JM, Moremedi GM, Morris N, Kondera-Shava R. A simple mathematical model for Ebola in Africa. J Biol Dyn. 2017;11(1):42–74. doi: 10.1080/17513758.2016.1229817. [DOI] [PubMed] [Google Scholar]
- 84.Singaram M, Muraleedhran VR, Sivaprakasam M (2022) Translational research in healthcare: a paradigm shift from traditional research. MAMC J Med Sci (in production)
- 85.Singaram M, Muraleedhran VR, Sivaprakasam M (2022) Translational research in health care: a qualitative analysis of 24 case studies in India. J Health Manag (peer review)
- 86.Osterwalder (2010) Business model generation, 1st edn. Wiley
- 87.Maurya (2020) Leanstack. https://leanstack.com/lean-canvas
- 88.Blank (2020) The four steps to the Epiphany: Successful strategies for products that win, 1st edn. Wiley
- 89.Ries (2011) The lean startup. Penguin
- 90.Timmermans O. The continued social transformation of the medical profession. J Health Soc Behav. 2010;51(Suppl 1):S94–106. doi: 10.1177/0022146510383500. [DOI] [PubMed] [Google Scholar]
- 91.Policy makers. https://www.publicengagement.ac.uk/do-engagement/understanding-audiences/policy-makers. Accessed 27 Mar 2022
- 92.O'Rourke B, Oortwijn W, Schuller T, Group, the International Joint Task The new definition of health technology assessment: A milestone in international collaboration. Int J Technol Assess Health Care. 2020;36(3):187–190. doi: 10.1017/S0266462320000215. [DOI] [PubMed] [Google Scholar]
- 93.Welcome to the health technology assessment In India, https://htain.icmr.org.in/. Accessed 2 Apr 2020