Abstract
Objectives
Since the safety of coronary CT angiography (CTA) is of great importance, especially with regard to widening indications and increasing morbidity, the aim of this study was to assess influencing factors.
Methods
Patients undergoing coronary CTA in a third-generation dual-source CT in a radiological centre were included in a clinical registry. Up to 20 mg metoprolol was administered intravenously to attain a heart rate ≤65/min. Glyceryl trinitrate (GTN) was administered in doses of 0.8 mg and 0.4 mg. Blood pressure was measured before the administration and after the CTA.
Results
Out of 5500 consecutive patients (3194 men, 62.3 (54.9–70.0) years), adverse events occurred in 68 patients (1.2%) with mild anaphylactoid reactions (0.4%), vasovagal symptoms (0.3%) and extravasation (0.3%) being most frequent. Anti-allergic drugs were given in 17 patients, atropine in 3 patients and volume in 1 patient. Drug administration resulted in a significant mean arterial pressure decline (96.0 (88.3–106.0) vs 108.7 (99.7–117.3) mmHg; p<0.001). Patients who suffered systolic blood pressure drops >20 mmHg or >40 mmHg were older (66.5 (58.6–73.3) vs 60.5 (53.6–68.3) years; 70.2 (63.3–76.5) vs 62.1 (54.7–69.6) years), more often male (65.1% vs 54.4%; 68.9% vs 57.3%) and had higher Agatston score equivalents (83.0 (2.0–432.0) vs 15.0 (0.0–172.0); 163.0 (16.3–830.8) vs 25.0 (0.0–220.0); all p<0.001). GTN dose reduction lowered the fraction of patients suffering from blood pressure drops >20 mmHg or >40 mmHg from 34.5% to 27.4% and from 6.1% to 3.5% (both p<0.001), respectively. The proportion of coronary segments with impaired image quality did not differ significantly.
Conclusions
Coronary CTA with intravenous beta-blocker administration is a safe procedure in an outpatient setting as adverse events are rare and mostly mild. Reduced GTN doses can further improve safety by lowering the rate of significant blood pressure drops, which occurred especially in elderly men with increased plaque burden.
Trial registration number
Keywords: Coronary heart disease, Cardiovascular imaging, Computed tomography, Cardiology, Adverse events, CLINICAL PHARMACOLOGY
Strengths and limitations of this study.
The study includes a large population of real-world patients and, thus, its results may be applicable to clinical routine.
Adverse events, heart rate and blood pressure characteristics were systematically recorded.
Analyses were performed to identify patients at increased risk of adverse events.
To our knowledge, this is the first study assessing the influence of the glyceryl trinitrate dose on blood pressure and image quality in coronary CT angiography.
Follow-up data on the delayed effects of contrast agent administration, for example, on renal function, were not available.
Introduction
Over the recent years, cardiac CT has emerged as an essential diagnostic modality for the detection and assessment of coronary artery disease (CAD). Calcium scoring measures the calcified plaque burden without the need for contrast agent application, adding incremental prognostic value to standard cardiovascular risk factors.1 2 Coronary CT angiography (CTA) offers a detailed visualisation of the entire coronary tree. In contrast to invasive coronary angiography, coronary CTA not only allows for the quantification of coronary artery stenosis but also the evaluation of plaque morphology including the detection of high-risk plaque features indicating vulnerable lesions.3–5 In addition, cardiac CT renders the evaluation of the cardiac morphology and adjacent anatomical structures like the aorta and the lungs possible.6 Its high sensitivity and negative predictive value allow for the reliable exclusion of obstructive CAD. Thus, cardiac CT and especially coronary CTA have been implemented in current guidelines for the diagnosis and management of CAD even being the first-line imaging modality in the current National Institute for Health and Care Excellence guidelines.7–10 As cardiac CT is increasingly used and modern CT scanners enable the assessment of significantly calcified vessels or even coronary artery stents, the fragility and morbidity of the patients undergoing coronary CTA increase.11–13 Thus, the safety of cardiac CT examinations is of paramount importance, especially in an outpatient setting. Although CTA is generally regarded to be safe, real-world data on coronary CTA assessing the impact of glyceryl trinitrate (GTN) and intravenous beta-blocker administration are scarce.
The aims of this study were to assess the safety of coronary CTA in a real-world outpatient population, identify influencing factors and evaluate the benefit of an optimised CTA examination protocol with a reduced GTN dose.
Methods
Patients underwent coronary CTA at a radiological centre using a dual-source CT (DSCT) scanner of the third generation (SOMATOM Force, Siemens Healthineers Erlangen, Germany). Patients were referred to the CT examination by their attending physicians considering their symptoms, cardiovascular risk profiles and previous examination results. The indication was counter-checked by a radiologist. Subjects were enrolled in the Heidelberg Cardiac CT Registry and examinations, which were performed between May 2017 and April 2020, were included in this study. The workflow of the optimised coronary CTA examination protocol is given in figure 1. Usually, an 18 G venous cannula was placed in the antecubital vein, but also 20 G cannulas were inserted into veins of the forearm or even the dorsum of the hand in individual cases. Patients were trained in breathing manoeuvres as image acquisition was performed in inspiration breath-hold. Patients received up to 20 mg metoprolol tartrate (Lopressor, Recordati Pharma, Ulm, Germany) intravenously to achieve a heart rate of ≤65/min. GTN (Nitrolingual, Pohl-Boskamp, Hohenlockstedt, Germany) was administered sublingually to improve the coronary artery visualisation in standard doses of 0.8 mg (until April 2019) or 0.4 mg (from May 2019).
Figure 1.
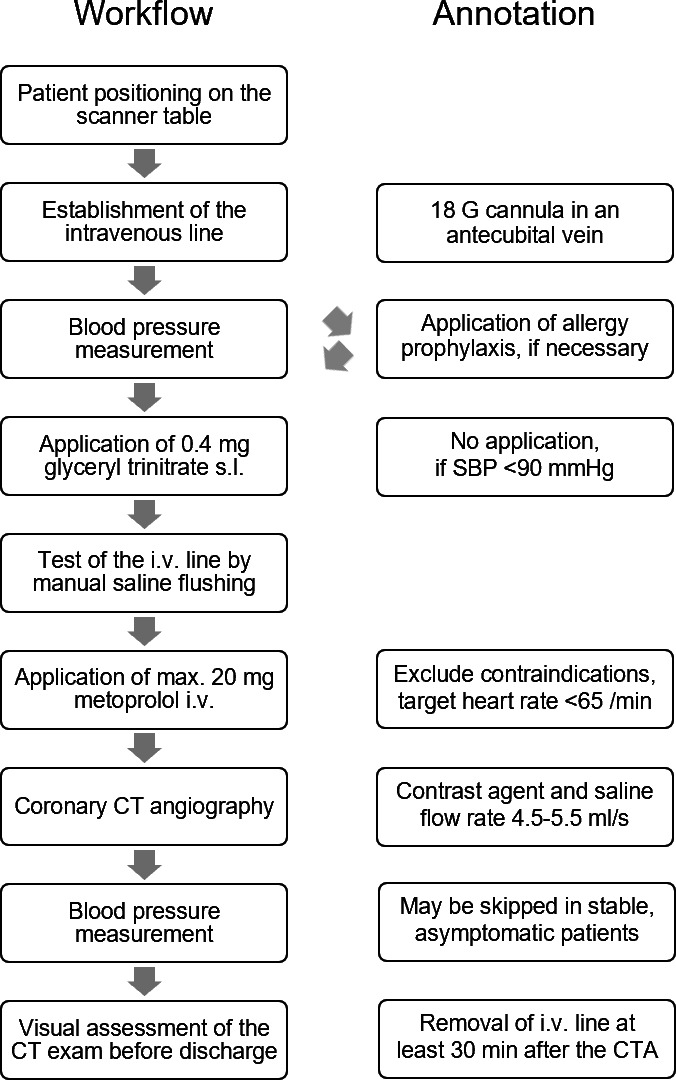
Optimised coronary CTA examination protocol. Common contraindications to metoprolol administration: haemodynamic instability, SBP <90 mmHg, heart rate <50/min, sick sinus syndrome, atrioventricular blockage II°/III°, severe asthma, intake of non-dihydropyridine calcium channel blockers, allergy to beta-blockers. CTA, CT angiography; G, gauge; i.v.: intravenously; SBP, systolic blood pressure; s.l., sublingually.
Contraindications to the administration of beta-blockers, GTN or iodine-based contrast agents were assessed by checking the patients’ medical history and records as well as the measurement of the renal and thyroid function. Patients with a known allergy to iodinated contrast agents were pretreated according to the current guidelines of the European Society of Urogenital Radiology.14 15 Calcium scoring was performed before the contrast agent administration for the quantification of the coronary calcium burden and further optimisation of the coronary CTA protocol. Between 40 mL and 80 mL prewarmed iomeprol with a concentration of 400 mg I/mL (Imeron 400, Bracco Imaging, Konstanz, Germany) was administered at a flow rate between 4.5 and 5.5 mL/s depending on the respective protocol followed by a chaser of 30 mL isotonic saline at the same flow rate. Axial or helical scan modes with automated attenuation-based tube potential and tube current selection were applied. The collimation was 96×0.6 mm and a slice acquisition of 192×0.6 mm using a z-flying focal spot was used. Advanced Modeled Iterative Reconstruction level 3 with dedicated cardiac kernels (usually Bv36 and Bv40) was applied for image reconstruction. The heart rate was recorded during the coronary CTA scan and blood pressure was measured before the drug administration. In a subgroup, an additional blood pressure measurement was performed immediately after the coronary CTA examination. The intravenous access was left for 30 min after contrast agent administration as anaphylactoid reactions might occur delayed.
Image analysis was performed on a dedicated workstation (syngo.via, Siemens Healthineers, Erlangen, Germany) by an experienced cardiologist and radiologist (>4000 cardiac CT examinations). The CT examinations were reviewed visually before the patient was discharged to account for critical findings, which might have an immediate therapeutic consequence, whereas the detailed analysis was conducted afterwards. The results of the examination, as well as clinical data and periprocedural events, were documented in a dedicated database. Periprocedural events were defined as any incident impairing the patient’s well-being including not only potentially dangerous adverse events, for example, anaphylactoid reactions, but also unpleasant symptoms, for example, transient nausea.
Anaphylactoid reactions were graded according to severity as described before.16 17 Briefly, four classes with increasing severity were employed: I: pruritus or dermal symptoms; II: abdominal, respiratory or circulatory symptoms; III: more severe abdominal, respiratory or circulatory symptoms including cyanosis and shock; IV: respiratory or cardiac arrest.
The cardiac CT examinations were clinically indicated by the referring physicians. The Heidelberg Cardiac CT Registry aims to assess the real-world diagnostic and prognostic performance of cardiac CT examinations by including all patients undergoing cardiac CT examinations in an outpatient centre.
The effect of the GTN dose on the proportion of coronary artery segments with impaired or non-diagnostic image quality was assessed by two experienced readers in 100 randomly selected patients with half of them receiving the reduced GTN dose.
Patient and public involvement
Patients, who were prospectively enrolled in the clinical registry, were informed about the general aims and research questions. Since the cardiac CT examinations were clinically indicated, patients could not be involved in the recruitment of the study population or the conduct of the examinations. The results of this study will be implemented in clinical routine and, thus, may be beneficial to future patients.
Statistics
Continuous data are uniformly given as a median and interquartile range (IQR) as part of the data showed a non-parametric distribution. Normal distribution was assessed using the D’Agostino-Pearson test. Categorial data are given as numbers and proportions. The Mann-Whitney test was used for the comparison of two groups, the Wilcoxon test for paired samples and the Kruskal-Wallis test with a post hoc analysis (Conover) for the analysis of several groups as appropriate. The Fisher’s exact test was employed for the comparison of categorical data. Multivariate logistic regression analysis was used to model the effect of independent variables on a dichotomous characteristic of interest. In the case of missing values, the number of subjects included in the respective analysis is given at first mention. A p value of <0.05 was regarded as statistically significant. Analyses were conducted using dedicated statistical software (MedCalc Statistical Software V.19 and V.20, MedCalc Software, Ostend, Belgium).
Results
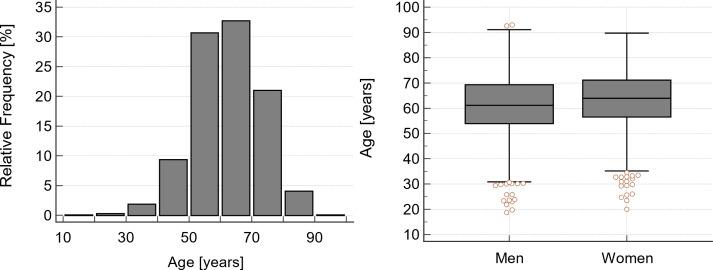
Coronary CTA examinations of 5500 consecutive patients were included in the final study population. Of note, safe venous access could not be established in seven additional patients and another two patients aborted the examination after the calcium scoring scan due to panic attacks and severe claustrophobia. Male subjects were significantly younger than female subjects (61.2 (53.9–69.3) years vs 63.9 (56.5–71.1) years; p<0.001). While in most patients an obstructive CAD was not known, 175 patients (3.2%) had previously undergone percutaneous coronary intervention with coronary stent implantation and 48 patients (0.9%) coronary artery bypass surgery or both. Further patient characteristics are given in table 1 and displayed in figure 2.
Table 1.
Patient characteristics
| Age [years] | 62.3 (54.9–70.0) |
| Sex | 3194 men (58.1%) |
| BMI [kg/m²; n=5285] | 27.0 (24.4–30.4) |
| Systolic arterial pressure* [mmHg; n=5185] | 150.0 (136.0–165.0) |
| Mean arterial pressure* [mmHg; n=5185] | 108.7 (99.7–117.3) |
| Agatston score equivalent [n=5499] | 28.0 (0.0–242.0) |
*Before the administration of beta-blocker and glyceryl trinitrate.
BMI, body mass index.
Figure 2.
Age distribution. The majority of patients were between 50 and 70 years old and men were slightly but significantly younger than women (61.2 (53.9–69.3) years vs 63.9 (56.5–71.1) years; p<0.001).
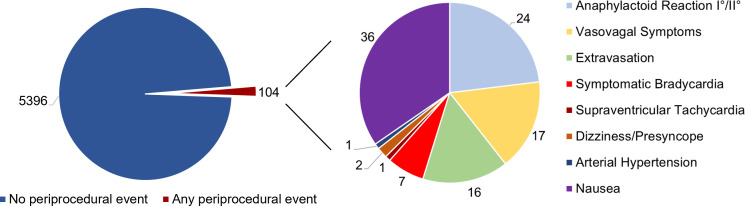
Adverse events occurred in 68 patients (1.2%) with mild anaphylactoid reactions, vasovagal symptoms and extravasations being the most frequent. Of note, only mild forms of anaphylactoid reactions occurred in our study population. Another 36 patients (0.7%) suffered from severe nausea, which abated spontaneously within a few minutes in all subjects. An overview of all adverse events is given in table 2 and figure 3. Out of 24 patients (0.4%) with anaphylactoid reactions, 17 received a medication. Atropine was administered in three patients with symptomatic bradycardia and isotonic saline was administered in one patient with vasovagal symptoms. One patient was referred to the chest pain unit due to critical coronary artery stenoses in combination with bradycardia after beta-blocker administration. Two patients were hospitalised due to unstable CAD and another one due to unexpected pulmonary embolism. In 5 of 16 cases of extravasation, only saline was injected extravascularly. Of note, all patients suffering from extravasation could be treated conservatively. Patients with adverse events were significantly younger (57.3 (50.8–61.6) years vs 62.4 (55.0–70.1) years; p<0.001), which was mainly driven by the lower age of the subjects suffering from mild anaphylactoid reactions and vasovagal symptoms (p<0.05). The rate of adverse events did not differ significantly between the male and female patients (p=n .s.).
Table 2.
Periprocedural events—frequency and patient characteristics
| n | Fraction | Male | Female | Age [years] | |
| Anaphylactoid reaction I°/II° | 24 | 0.4% | 12 | 12 | 52.5 (48.0–59.5) |
| Anaphylactoid reaction III°/IV° | 0 | 0.0% | 0 | 0 | |
| Vasovagal symptoms | 17 | 0.3% | 11 | 6 | 56.0 (48.7–61.6) |
| Extravasation | 16 | 0.3% | 8 | 8 | 60.5 (53.4–67.1) |
| Symptomatic bradycardia | 7 | 0.1% | 7 | 0 | 59.1 (56.7–67.0) |
| Supraventricular tachycardia | 1 | 0.02% | 1 | 0 | 58.1 |
| Dizziness/presyncope | 2 | 0.04% | 0 | 2 | 53.6 (51.5–55.6) |
| Arterial hypertension | 1 | 0.02% | 0 | 1 | 78.9 |
| Nausea | 36 | 0.7% | 20 | 16 | 59.8 (52.9–65.7) |
Figure 3.
Number of periprocedural events. The rate of all periprocedural events inclusive of transient nausea was low with 104 of 5500 patients (1.9%). Adverse events aside from nausea occurred in only 68 patients (1.2%) and were mostly mild.
The administration of beta-blocker and GTN resulted in a significant decline of the systolic and mean arterial pressure (134.0 (122.0–150.0) mmHg vs 150.0 (136.0–165.0) mmHg and 96.0 (88.3–106.0) mmHg vs 108.7 (99.7–117.3) mmHg; both p<0.001, n=5185). Median heart rate was 62.0 (56.0–68.0)/min (n=5324) with men showing a little but significant lower frequency (61.0 (56.0–67.0)/min vs 63.0 (68.0–69.0)/min; p<0.001) during the image acquisition. Patients suffering from systolic blood pressure drops of more than 20 mmHg and more than 40 mmHg were significantly older (66.5 (58.6–73.3) years vs 60.5 (53.6–68.3) years and 70.2 (63.3–76.5) years vs 62.1 (54.7–69.6) years; both p<0.001), were more often male (65.1% vs 54.4%; p<0.001 and 68.9% vs 57.3%; both p<0.001) and had higher Agatston score equivalents (83.0 (2.0–432.0) vs 15.0 (0.0–172.0) and 163.0 (16.3–830.8) vs 25.0 (0.0–220.0), both p<0.001, n=5184). Age, sex and the Agatston score equivalent were significant predictors for systolic blood pressure drops of more than 40 mmHg in the multivariate regression analysis, whereas age and sex but not the Agatston score equivalent reached statistical significance for systolic blood pressure drops of more than 20 mmHg (n=5184).
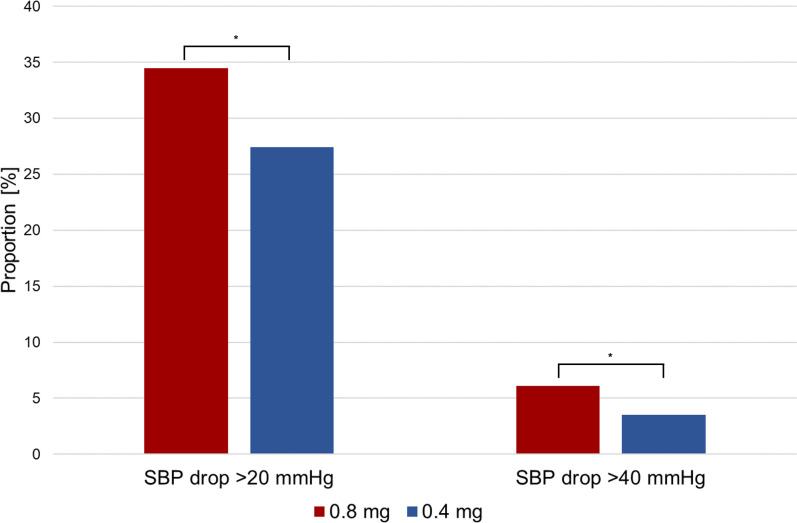
The reduction of the standard GTN dose from 0.8 mg to 0.4 mg (n=3688; n=1812) resulted in small but significant decreases of the systolic blood pressure drop (15.0 (6.0–25.0) mmHg vs 12.0 (3.0–21.5) mmHg) as well as the mean arterial pressure drop (12.3 (5.7–18.7) mmHg vs 9.7 (3.7–16.3) mmHg; n=5185; both p<0.001). Of note, the proportions of patients suffering a drop of the systolic blood pressure of more than 20 mmHg (34.5% vs 27.4%; p<0.001) as well as more than 40 mmHg (6.1% vs 3.5%; p<0.001) declined significantly with the reduction of the GTN dose (figure 4). Age (62.6 (55.1–70.4) years vs 62.2 (54.9–69.6 years), n=5185), sex (57.3% men vs 59.1% men, n=5185) and the Agatston score equivalent (30.0 (0.0–261.0) vs 25.0 (0.0–219.0); n=5184) did not differ significantly between the GTN groups included in the blood pressure analysis (all p=n .s.).
Figure 4.
Rate of significant blood pressure drops depending on glyceryl trinitrate (GTN) dose. The reduction of the standard GTN dose from 0.8 mg to 0.4 mg resulted in significantly lower proportions of patients suffering a drop of the systolic blood pressure (SBP) >20 mmHg as well as >40 mmHg. *P<0.001.
The proportion of coronary artery segments with impaired or non-diagnostic image quality did not differ significantly between the GTN dose groups (both p=n .s.). Of note, neither the Agatston score equivalent nor the heart rate differed significantly between groups (both p=n .s.).
Discussion
Coronary CTA is increasingly used as the first-line diagnostic modality for CAD replacing more and more diagnostic invasive coronary angiography for the primary assessment of coronary anatomy. Consequently, the fragility and morbidity of the patients referred to coronary CTA increase. Periprocedural safety is of great importance in clinical routine and especially in outpatient settings. Prior data indicate that adverse reactions may occur more frequently in outpatient than inpatient settings18 and, additionally, the ability to address emergencies may be limited in some outpatient facilities. Thus, we assessed the safety of coronary CTA in a large real-world population and evaluated an optimised coronary CTA examination protocol. The key findings of our study were as follows: (1) adverse events such as anaphylactoid reactions and extravasations are rare and mostly mild; (2) the intravenous administration of beta-blockers in combination with GTN can be regarded as safe when the dose is thoroughly adapted to the individual patient; (3) the fraction of patients suffering from significant blood pressure drops is increased especially in elderly men with increased plaque burden; (4) the reduction of the GTN dose reduces the rate of significant blood pressure drops without impairing the diagnostic image quality.
In the study population, anaphylactoid reactions were the most common adverse event with 0.4% of cases of whom about two-thirds received medical treatment. Of note, only mild reactions occurred in our study population and none of the patients required hospitalisation. About 0.7% of the patients reported transient nausea with none of them needing any medication, which is in line with previously published studies.19–21 Adverse reactions occurred more often in younger patients, which is in agreement with a study by Gomi et al, showing a higher incidence of adverse reactions in patients aged 59 years or less compared with older ones.20
While the high level of safety of the intravenous administration of current contrast agents was shown in several studies,22 23 the use of GTN and beta-blockers in cardiac patients requires an individual clinical assessment, especially in outpatient settings. Current guidelines approve the oral, intravenous or both routes of beta-blocker administration, while an oral premedication followed by supplemental intravenous application, when necessary, is given as the most common approach.24 The intravenous administration results in an immediate reduction of the heart rate and, thus, allows for a precise titration. In a retrospective study of 560 consecutive patients, the intravenous administration of atenolol resulted in a better heart rate reduction as well as a faster preparation than the oral intake of metoprolol.25 Although patients with atrial fibrillations were not excluded from our study, the median heart rate after beta-blocker administration was 62.0 (56.0–68.0)/min and, thus, suitable for coronary CTA using a third-generation DSCT scanner, which is able to provide diagnostic image quality independent of heart rate and heart rhythm.13 Yet, safety data on the sole use of intravenous beta-blockers for rapid heart rate control are limited.25 26 In our study population, the fraction of patients with symptomatic bradycardia was approximately 0.1% and medical intervention was needed in less than half of the cases. Thus, we consider the intravenous administration of metoprolol immediately before CT image acquisition to be safe, when individually adapted to the patient.
GTN causes vasodilation, which can result in a drop in blood pressure and a reactive increase in heart rate. While some protocols recommend the application of GTN immediately before the coronary CTA due to its short half-life of 2.5–4.4 min,27 we recommend its administration before the beta-blocker application for two reasons. First, the potential reactive heart rate increase can be counteracted by metoprolol administration adequately. Second, some patients may show an excessive blood pressure drop and may need the reactive heart rate increase to sustain a sufficient mean arterial pressure, which would be impeded by prior administered beta-blockers. This compensatory mechanism may be of importance, especially in multimorbid patients, who often already suffer from a reduced heart rate adaptation. Of note, in our study, systolic blood pressure drops of more than 20 mmHg or even more than 40 mmHg occurred prevalently in elderly men with a high plaque burden indicated by the Agatston score equivalent.
In order to further improve the safety of coronary CTA examinations, especially in fragile patients, we assessed the reduction of the standard GTN dose from 0.8 mg to 0.4 mg. This led to a reduction of the systolic as well as the mean arterial pressure drops of approximately 3 mmHg, respectively. Although being statistically highly significant, the clinical relevance of this reduction may seem to be low. However, the fraction of patients showing systolic blood pressure drops of more than 20 mmHg as well as more than 40 mmHg decreased significantly from 34.5% to 27.4% and 6.1% to 3.5%, respectively. Of note, the image quality of the coronary CTA was not impaired, being possibly due to the fact that the time of the maximal drug level of sublingually administered GTN ranges between 2 and 10 min and the half-life of its vasoactive metabolites is even longer covering the time of the coronary CTA.28 Thus, the reduction of the GTN dose may improve patient safety without impairing diagnostic accuracy.
Limitations
As the data analysis was conducted retrospectively, prospective trials are needed to confirm the improvement in patient safety by the optimised coronary CTA examination protocol. The number of adverse events was low hampering further statistical analyses, especially of subgroups. Since all patients were examined in an outpatient setting, follow-up data on late reactions after contrast agent administration as well as on renal function were not available. Late reactions, occurring up to 1 week after contrast agent administration, are commonly mild to moderate skin manifestations, for example, maculopapular exanthema, which are self-limiting.29 Since thyroid function was assessed in all patients and contrast agent was not given in those with contraindications such as manifest hyperthyroidism, the risk of very late reaction occurring after 1 week, that is, thyrotoxicosis, was negligible.14 30 The risk of a contrast-induced acute kidney injury was very low as patients with an estimated GFR <45 mL/min/1.73 m² were not examined routinely in this study.31 32
Coronary CTA has a lower frequency of major procedure-related complications than invasive coronary angiography, with a similar risk of major adverse cardiovascular events, as shown in a recent multicentre trial comparing both modalities as initial diagnostic imaging strategies for guiding the treatment of patients with stable chest pain.33 Since its general safety could be confirmed by our study, which analysed an even larger population of real-world patients, coronary CTA can be considered an optimal diagnostic modality for CAD assessment in the outpatient setting.
Conclusions
Coronary CTA with GTN and intravenous beta-blocker administration allows for a safe assessment of CAD in an outpatient setting showing a low frequency of mostly mild adverse events. The use of an optimised coronary CTA examination protocol with a reduced GTN dose results in a lower fraction of patients with significant blood pressure drops and, thus, may further improve safety, especially in fragile patients.
Supplementary Material
Acknowledgments
We thank Katrin Buechler and the other technicians for the excellent image acquisition. For the publication fee we acknowledge financial support by Deutsche Forschungsgemeinschaft within the funding programme "Open Access Publikationskosten" as well as by Heidelberg University.
Footnotes
Contributors: FA and SJB designed the study and performed the data analysis. PF, SJB, JG, MB, FG, RS and AS contributed to the data acquisition and ME and SS collected and administered the data. JG, AS and NF gave administrative support. All authors contributed to the writing and editing of the manuscript and approved the final version. FA acted as guarantor.
Funding: This work was supported by a research grant from Siemens Healthineers (grant number N/A).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The data set analysed in this study is not publicly available due to data protection regulations. It is available on reasonable request from the corresponding author.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Approval for the scientific data analysis was obtained from the ethics committee of the University of Heidelberg (S-226/2016 and S-758/2018).
References
- 1.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336–45. 10.1056/NEJMoa072100 [DOI] [PubMed] [Google Scholar]
- 2.Yeboah J, McClelland RL, Polonsky TS, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012;308:788–95. 10.1001/jama.2012.9624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams MC, Moss AJ, Dweck M, et al. Coronary Artery Plaque Characteristics Associated With Adverse Outcomes in the SCOT-HEART Study. J Am Coll Cardiol 2019;73:291–301. 10.1016/j.jacc.2018.10.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee JM, Choi KH, Koo B-K, et al. Prognostic implications of plaque characteristics and stenosis severity in patients with coronary artery disease. J Am Coll Cardiol 2019;73:2413–24. 10.1016/j.jacc.2019.02.060 [DOI] [PubMed] [Google Scholar]
- 5.Williams MC, Newby DE, Dey D, et al. Response by Williams et al to Letter Regarding Article, “Low-Attenuation Noncalcified Plaque on Coronary Computed Tomography Angiography Predicts Myocardial Infarction: Results From the Multicenter SCOT-HEART Trial (Scottish Computed Tomography of the HEART)”. Circulation 2020;142. 10.1161/CIRCULATIONAHA.120.049840 [DOI] [PubMed] [Google Scholar]
- 6.Kay FU, Canan A, Abbara S. Common incidental findings on cardiac CT: a systematic review. Curr Cardiovasc Imaging Rep 2019;12. 10.1007/s12410-019-9494-4 [DOI] [Google Scholar]
- 7.Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407–77. 10.1093/eurheartj/ehz425 [DOI] [PubMed] [Google Scholar]
- 8.Excellence NIfHaC . Recent-Onset chest pain of suspected cardiac origin: assessment and diagnosis (clinical guideline 95). updated November 2016. National Institute for health and care excellence (NICE), 2010. Available: https://www.nice.org.uk/guidance/cg95 [Accessed 30 Mar 2020]. [PubMed]
- 9.Moss AJ, Williams MC, Newby DE, et al. The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep 2017;10:15. 10.1007/s12410-017-9412-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. J Am Coll Cardiol 2012;60:e44–164. 10.1016/j.jacc.2012.07.013 [DOI] [PubMed] [Google Scholar]
- 11.Narula J, Chandrashekhar Y, Ahmadi A, et al. SCCT 2021 expert consensus document on coronary computed tomographic angiography: a report of the Society of cardiovascular computed tomography. J Cardiovasc Comput Tomogr 2021;15:192–217. 10.1016/j.jcct.2020.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giusca S, Schütz M, Kronbach F, et al. Coronary computer tomography angiography in 2021-Acquisition protocols, tips and tricks and heading beyond the possible. Diagnostics 2021;11:1072. 10.3390/diagnostics11061072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ochs MM, Siepen FAdem, Fritz T, et al. Limits of the possible: diagnostic image quality in coronary angiography with third-generation dual-source CT. Clin Res Cardiol 2017;106:485–92. 10.1007/s00392-017-1077-2 [DOI] [PubMed] [Google Scholar]
- 14.ESoU R. ESUR guidelines on contrast agents 10.0, 2018. [Google Scholar]
- 15.ESoU R. ESUR guidelines on contrast media 9.0, 2014. [Google Scholar]
- 16.Ring J, Messmer K. Incidence and severity of anaphylactoid reactions to colloid volume substitutes. Lancet 1977;1:466–9. 10.1016/s0140-6736(77)91953-5 [DOI] [PubMed] [Google Scholar]
- 17.Ring J, Beyer K, Biedermann T, et al. Guideline for acute therapy and management of anaphylaxis: S2 guideline of the German Society for Allergology and clinical immunology (DGAKI), the association of German Allergologists (AeDA), the Society of pediatric allergy and environmental medicine (GpA), the German Academy of Allergology and environmental medicine (DAAU), the German professional association of pediatricians (BVKJ), the Austrian Society for Allergology and immunology (ÖGAI), the Swiss Society for allergy and immunology (SGAI), the German Society of Anaesthesiology and intensive care medicine (DGAI), the German Society of pharmacology (DGP), the German Society for psychosomatic medicine (DGPM), the German Working group of anaphylaxis training and education (AGATE) and the patient organization German allergy and asthma association (DAAB). Allergo J Int 2014;23:96–112. 10.1007/s40629-014-0009-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dean KE, Starikov A, Giambrone A, et al. Adverse reactions to intravenous contrast media: an unexpected discrepancy between inpatient and outpatient cohorts. Clin Imaging 2015;39:863–5. 10.1016/j.clinimag.2015.04.014 [DOI] [PubMed] [Google Scholar]
- 19.Kim YS, Yoon SH, Choi YH, et al. Nausea and vomiting after exposure to non-ionic contrast media: incidence and risk factors focusing on preparatory fasting. Br J Radiol 2018;91:20180107. 10.1259/bjr.20180107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gomi T, Nagamoto M, Hasegawa M, et al. Are there any differences in acute adverse reactions among five low-osmolar non-ionic iodinated contrast media? Eur Radiol 2010;20:1631–5. 10.1007/s00330-009-1698-6 [DOI] [PubMed] [Google Scholar]
- 21.Vijayalakshmi K, Kunadian B, Wright RA, et al. A prospective randomised controlled trial to determine the early and late reactions after the use of iopamidol 340 (Niopam) and iomeprol 350 (Iomeron) in cardiac catheterisation. Eur J Radiol 2007;61:342–50. 10.1016/j.ejrad.2006.09.013 [DOI] [PubMed] [Google Scholar]
- 22.Andreucci M, Solomon R, Tasanarong A. Side effects of radiographic contrast media: pathogenesis, risk factors, and prevention. Biomed Res Int 2014;2014:1–20. 10.1155/2014/741018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu MT, Douglas PS, Udelson JE, et al. Safety of coronary CT angiography and functional testing for stable chest pain in the promise trial: a randomized comparison of test complications, incidental findings, and radiation dose. J Cardiovasc Comput Tomogr 2017;11:373–82. 10.1016/j.jcct.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abbara S, Blanke P, Maroules CD, et al. SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: a report of the Society of cardiovascular computed tomography guidelines Committee: endorsed by the North American Society for cardiovascular imaging (NASCI). J Cardiovasc Comput Tomogr 2016;10:435–49. 10.1016/j.jcct.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 25.Maffei E, Palumbo AA, Martini C, et al. "In-house" pharmacological management for computed tomography coronary angiography: heart rate reduction, timing and safety of different drugs used during patient preparation. Eur Radiol 2009;19:2931–40. 10.1007/s00330-009-1509-0 [DOI] [PubMed] [Google Scholar]
- 26.Kassamali RH, Kim DH, Patel H, et al. Safety of an i.v. β-adrenergic blockade protocol for heart rate optimization before coronary CT angiography. AJR Am J Roentgenol 2014;203:759–62. 10.2214/AJR.13.11492 [DOI] [PubMed] [Google Scholar]
- 27.Bell GW, Edwardes M, Dunning AM, et al. Periprocedural safety of 64-detector row coronary computed tomographic angiography: results from the prospective multicenter accuracy trial. J Cardiovasc Comput Tomogr 2010;4:375–80. 10.1016/j.jcct.2010.08.003 [DOI] [PubMed] [Google Scholar]
- 28.Hashimoto S, Kobayashi A. Clinical pharmacokinetics and pharmacodynamics of glyceryl trinitrate and its metabolites. Clin Pharmacokinet 2003;42:205–21. 10.2165/00003088-200342030-00001 [DOI] [PubMed] [Google Scholar]
- 29.Bellin M-F, Stacul F, Webb JAW, et al. Late adverse reactions to intravascular iodine based contrast media: an update. Eur Radiol 2011;21:2305–10. 10.1007/s00330-011-2200-9 [DOI] [PubMed] [Google Scholar]
- 30.Bednarczuk T, Brix TH, Schima W, et al. 2021 European thyroid association guidelines for the management of Iodine-Based contrast media-induced thyroid dysfunction. Eur Thyroid J 2021;10:269–84. 10.1159/000517175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Solomon R. Contrast-Induced acute kidney injury: is there a risk after intravenous contrast? Clin J Am Soc Nephrol 2008;3:1242–3. 10.2215/CJN.03470708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weisbord SD, Mor MK, Resnick AL, et al. Incidence and outcomes of contrast-induced AKI following computed tomography. Clin J Am Soc Nephrol 2008;3:1274–81. 10.2215/CJN.01260308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DISCHARGE Trial Group, Maurovich-Horvat P, Bosserdt M, et al. Ct or invasive coronary angiography in stable chest pain. N Engl J Med 2022;386:1591–602. 10.1056/NEJMoa2200963 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The data set analysed in this study is not publicly available due to data protection regulations. It is available on reasonable request from the corresponding author.