Abstract
Objectives
The objective of this study was to determine the level of type 2 diabetes (T2DM) and hypertension (HTN) in Vietnam and to assess the trend and recommend the future direction of prevention research efforts.
Design
We searched scientific literature, databases including PubMed, EMBASE, CINHAL and Google Scholar; grey literature and reference lists for primary research published, nation database websites between 1 January 2000 and 30 September 2020. We adapted the modified Newcastle Ottawa Scale for assessing the quality of the study, as recommended by the Cochrane Collaboration.
Results
In total, 83 studies met our inclusion criteria, representing data of approximately 239 034 population of more than 15 years of age in Vietnam. The findings show that prevalence rates varied widely across studies, from 1.0% to 29.0% for T2DM and 2.0% to 47.0% for HTN. For the total study period, pooled prevalence of T2DM and HTN in Vietnam for all studies was 6.0% (95% CI: 4.0% to 7.0%) and 25% (95% CI: 19% to 31%), respectively. Prevalence rate of both T2DM and HTN was higher among the male population compared with female counterpart.
Conclusion
There is evidence of a rising trend of HTN and T2DM prevalence in Vietnam. Future research should focus on the major drivers, incidence and prognosis of T2DM and HTN. Policy approaches should base upon the trends of T2DM and HTN in Vietnam over the last 20 years and pay more attention on the effective interventions to combat T2DM and HTN. In our study, we included both English and Vietnamese language articles and seems that majority of the articles came from Vietnamese language.
PROSPERO registration number
CRD42020182959.
Keywords: Health policy, DIABETES & ENDOCRINOLOGY, Hypertension, Ischaemic heart disease
Strengths and limitations of this study.
This is the first systematic review and meta-analysis on type 2 diabetes (T2DM) and hypertension (HTN) in Vietnam that collected data and documents over 20 years.
This is also the first review combining available documents published in both English and Vietnamese languages across domestic and international databases.
The study reported that prevalence of T2DM and HTN among adult population in Vietnam increased over the time.
While the current study followed the Meta-analyses Of Observational Studies in Epidemiology guideline, findings from the review were heterogeneous in nature due to the study design, the outcome measurement and the potential biases in identified documents. Additionally, the estimate prevalence by ethnicity and place of residence were not provided due to the data limitation.
Introduction
Globally, the non communicable diseases (NCDs) have become the leading cause of death.1 Due to the high number of deaths, non-communicable diseases,2 including cardiovascular diseases (CVDs), diabetes, cancer and chronic respiratory diseases, have appeared as key public health challenges worldwide.3 As a result, NCDs are included in sustainable development goal target 3.4, to by ‘2030 reduce by one-third premature mortality from NCDs through prevention and treatment and promote mental health and well-being’.2 4 NCD mortality rate, which was high in low middle-income countries (LMICs), nearly three-quarters of NCD deaths occurred in LMICs, expected to increase by 20% in coming years.5 Due to the increasing prevalence of fast food consumption and food insecurity,6–8 population of LMICs have a higher ability to purchase high-caloric foods, which are associated with higher intake of calories and fat. Such fast food consumption and food insecurity are responsible for increase in the prevalence of diabetes, hypertension (HTN) and other NCDs in LMICs. It is estimated that this condition is likely to increasing.
Like other LMICs, Vietnam has recently been facing the challenge of NCDs. The number of deaths due to NCDs in Vietnam rose from 296 900 in 2000 to 371 600 in 2010 and 424 000 in 2016.9 NCD were estimated to account for 73% of all deaths in Vietnam in 201410 and 77% in 2016.11 Of NCDs, CVDs represented 31% of all deaths in 2016; HTN, one of the main risk factors for CVDs, accounted for 21% of all deaths in the country.12 It was estimated in 2016 that about 17% of people aged 30–70 in Vietnam will suffer a premature death due to one of the four common NCDs (CVDs, cancer, chronic respiratory diseases and diabetes).13
The gross domestic product per capita was increased gradually in Vietnam, which is directly linked to increased behavioural risk factors for NCDs such as the harmful use of alcohol, unhealthy diets and physical inactivity.3 14 NCD risk factor survey in Vietnam (2015) revealed high prevalence of NCD risk factors among the adult population. For example, prevalence of overweight/obesity (BMI≥25) was 15.6%, HTN (systolic blood pressure (SBP)≥140 mm Hg and/or diastolic blood pressure (DBP)≥90 mm Hg or on medication) was 18.9%, raised cholesterol was 30.2%, physical inactivity 28.1%, lack of vegetable/fruit consumption 57.2%, the average population salt intake per day was 9.4 grams, which was almost double the WHO recommendation.14 These behavioural risk factors play a vital role of rising chronic disease burden including CVD and diabetes.
Over the past two decades, The Government of Vietnam has a number of policies, strategies, plans and programmes responding to NCDs. Two national programmes were implemented for the period 2002–2010 and 2012–2015 focusing on four disease groups of CVDs, diabetes, cancers and mental and neurological disorders13 and covering a component project of prevention and control of some dangerous diseases, which included some specific NCDs. Despite the efforts, these programmes did not have expected achievements due to lack of intersectoral coordination and direction for NCDs prevention as well as evidence-based research. An updated National Strategy on Prevention and Control of NCDs for the period of 2015–2025, which followed the WHO Global NCD Action plan 2013–2020 was developed in 2015, providing a strong basis for NCD prevention and control in Vietnam. Under the revised programme, the prevention and control of some dangerous infectious diseases and some common NCDs was included as a project component.15
In addition to these national policies and programmes targeting on HTN and type 2 diabetes (T2DM), over the last few decades, a number of studies have been undertaken in Vietnam to measure the prevalence of HTN and T2DM but none have assessed trend of T2DM and HTN except for a 2001–2009 time trends analysis, which showed an annual increase of HTN prevalence of 0.9%. Two reviews on prevalence of HTN and T2DM among adult population in Vietnam were published recently, yet these studies had their own limitations as (1) they were carried out based on the literature available in English16; (2) the review employed only surveys, which were conducted by a research institute, therefore the results may have some bias; (3) meta-analysis was not implemented to produce the pool estimation17; and (4) they are out of date assessment with regard to the rapid change of T2DM and HTN. There is a need for an updated systematic review and meta-analysis. It is important for both health professionals and policy-makers to better understand the trends of T2DM and HTN to develop effective policies and programmatic interventions. In this review, we conducted a systematic review and meta-analysis to comprehensively (1) determine the extent of research that has been done for HTN and T2DM and (2) to assess the trend and recommend the future direction of prevention research efforts.
Methods
We followed the Meta-analyses Of Observational Studies in Epidemiology (MOOSE) guidelines to identify studies.18The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was employed in this study.
Search strategy
We used the Population, Intervention, Comparison, Outcome, and Study design (PICOS) criteria to define the research question (table 1).19 Our search included studies published from 1 January 2000 to 30 September 2020 in both English and Vietnamese languages. We used a number of different search engines: PubMed, EMBASE, CINAHL, Google Scholar, Google and national website and database including the Database of National Agency for Science and Technology Information (vista.gov.vn) and some Vietnamese journals in the field, which are not included in the database. A full description of the electronic search strategy is available in online supplemental table S1.
Table 1.
PICOS criteria for inclusion and exclusion of studies
| Parameter | Inclusion criteria | Exclusion criteria |
| Population | Those were of age≥15 years | <15 |
| Intervention/exposure | Collection of data on T2DM and hypertension sociodemographic factors | Lack of data on T2DM and hypertension |
| Comparator | T2DM and hypertension status of Vietnamese adult | Lack of data on T2DM and hypertension |
| Outcome | Prevalence of T2DM and hypertension | No reported prevalence measure |
| Study design | Observational study Cross-sectional study Cohort study |
Editorial Methodological article |
PICOS, Population, Intervention, Comparison, Outcome, and Study design; T2DM, type 2 diabetes.
bmjopen-2021-052725supp001.pdf (1.7MB, pdf)
The keywords used in the search were ‘diabetes’, ‘diabetes mellitus’, ‘non-insulin dependent diabetes mellitus’, ‘NIDDM’, ‘type 2 diabetes’, ‘cardiovascular disease’, ‘CVD’, ‘myocardial infarction’, ischemic heart disease’, ‘hypertension’, ‘high blood pressure’, ‘coronary artery disease’, ‘Vietnam’, ‘đái tháo đường’, ‘tiểu đường’, ‘tăng đường huyết’, ‘tăng huyết áp’ ‘cao huyết áp’. We limited the search to studies that only involved human participants. We screened the studies using the following inclusion criteria: (1) had prevalence or incidence data available on either HTN or T2DM, (2) had selected a sample included those who are Vietnamese and are living in Vietnam and (3) had published results between 1 January 2000 to 30 September 2020. Once we identified the eligible studies, we made further exclusions based on sample, study design and publication type.
Inclusion and exclusion criteria
Studies eligible for inclusion met the following criteria: primary or secondary data, published in the English and Vietnamese languages, conducted in humans, studies that provide an estimate of prevalence of either HTN or T2DM and population age group 15 years or older. Studies were excluded if: (1) were reported in reviews, qualitative studies, editorials, abstracts, theses, books, case reports and letters to the editor; (2) the study had participants with type 1 diabetes, GDM, (3) only on the elderly (60 year old and over) and (4) studies employed RCT designs. HTN was defined as raised blood pressure was defined as an average (based on the WHO’s recommended tool for surveillance of NCDs and their risk factors (WHO STEPS survey)) SBP≥140 mm Hg and/or average DBP≥90 mm Hg and/or self-reported current medication for high blood pressure in the previous 2 weeks. T2DM was defined fasting plasma glucose≥7 mmol/L (≥126 mg/dL) or self-reporting having been diagnosed by a health professional.
Data extraction and quality assessment
Data extraction was carried out by at least two independent reviewers following a piloted version of the Cochrane Effective Practice and Organization of Care Group guidelines.18 They completed a standard data extraction form, summarising the study design and other relevant data for each article, including author name, sample size, survey year and reference standard (tables 2 and 3). Once article did not report survey year, publication year was listed. The main outcomes were prevalence of T2DM and HTN.
Table 2.
Summary of the reported prevalence rate of diabetes in Vietnam (2000–2020)
| SI | Author name | Publication year | Study conducted | Community/hospital based | Reference standard | Study design | Sample size | Age range | Prevalence of diabetes |
| 1 | Binh and Nhung58 | 2015 | 2010 | Community | The WHO and International Diabetes Federation diagnostic criteria | Cross-sectional | 892 | 35–70 | 7.60% |
| 2 | Miyakawa et al25 | 2017 | 2014 | Community | Elevated fasting plasma glucose (FPG) level≥7.0 mmol/L (126 mg/dL) or random elevated plasma glucose level≥11.1 mmol/L (200 mg/dL); or history of treatment for DM (lifestyle guidance including diet or exercise advice, oral medication or insulin) | Cross-sectional | 376 | 20–70 | 7.20% |
| 3 | Duc Son et al65 | 2004 | 2001 | Community | NM | Cross-sectional | 2932 | ≥15 | 6.6 |
| 4 | Binh et al48 | 2014 | Community | The glycaemic status was classified as normal glucose tolerance when FPG<5.6 mmol/L and 2-hour PG<7.8 mmol/L | Cross-sectional | 2443 | 48–57 | 14.30% | |
| 5 | Kien et al66 | 2013 | 2013 | Community | NM | Cross-sectional | 3736 | NM | 11% |
| 6 | Pham et al67 | 2015 | 2011–2013 | Community | Diabetes was diagnosed when FPG was≥7.0 mmol/L (126 mg/dL) or 2 hours post OGTT≥11.1 mmol/L (200 mg/dL) | Cross-sectional | 16 282 | 30–69 | 6.00% |
| 7 | Hoa et al44 | 2018 | 2016 | Facility-based | American Diabetes Association | Cross-sectional | 870 | >15 | 13.9% |
| 8 | Pham et al26 | 2015 | 2009 | Community | Based on STEPS rule | Cross-sectional | 1978 | 25–64 | 1.00% |
| 9 | National Hospital of Endocrinology27 | 2002 | 2002 | Hospital | WHO 1998: FPG≥7 mmol/L or 2-hour OGTT≥11.1 mmol/L | Cross-sectional | 9122 | 30–64 | 2.7 |
| 10 | Le et al34 | 2004 | NM | Community | WHO 1998/ADA 1997: FPG≥7 mmol/L or using | Cross-sectional | 2932 | >15 | 3.8 |
| 11 | Do and Le68 | 2008 | NM | Community | WHO 1998: FPG≥7 mmol/L or 2-hour OGTT≥11.1 mmol/L or self-report | Cross-sectional | 1456 | 30–69 | 7.0 |
| 12 | Ta et al36 | 2010 | NM | Community | WHO 1998: FPG≥7 mmol/L or 2-hour OGTT≥11.1 mmol/L | Cross-sectional | 2142 | 30–64 | 4 |
| 13 | Dao-Tran et al53 | 2012 | NM | Community | WHO 1998: FPG≥7 mmol/L or 2-hour OGTT≥11.1 mmol/L or self-report | Cross-sectional | 2710 | 40–64 | 3.7 |
| 14 | National Hospital of Endocrinology37 | 2012 | NM | Hospital | WHO 1998: FPG≥7 mmol/L or 2-hour OGTT≥11.1 mmol/L | Cross-sectional | 11 191 | 30–69 | 5.4 |
| 15 | Nguyen et al49 | 2008 | 2008 | Workplace | NM but not self-report | Cross-sectional | 383 | NM | 2% |
| 16 | Le et al69 | 2014 | 2011 | Community | NM but not self-report | Cross-sectional | 1401 | 40+ | 9.30% |
| 17 | Pham and Truong70 | 2019 | 2018 | Community | Decision 3319/QĐ-BYT, 19 July 2017—MOH | Cross-sectional | 3000 | 30–69 | 6.50% |
| 18 | Nguyen and Le71 | 2014 | 2014 | Community | NM but not self report | Cross-sectional | 5190 | 21–70 | 4.2% |
| 19 | Pham et al72 | 2019 | 2014–2015 | Workplace | Elevated FPG level≥7.0 mmol/L | Cross-sectional | 1595 | NM | 5.50% |
| 20 | Vu and Dang73 | 2018 | 2017 | Community | Capillary blood glucose by Accu-Chek D10-BIORAD: 2-hour OGTT≥11.1 mmol/L=diabetes; OGTT from 7.8 to 11.0=abnormal; WHO–IDF 2008 updated 2010: The glycaemic status was classified as abnormal when FPG range 5.6–6.9 mmol/L; FPG≥7 mmol/L=diabetes | Cross-sectional | 1.450 | ≥25 | 6.5 |
| 21 | Nguyen et al74 | 2017 | 2016 | Community | Diabetes prevention and control Project, National Institute of Endocrinology; using Onetouchverio machine (Johnson&Johnson) | Cross-sectional | 400 | 45–69 | 3.5 |
| 22 | Vo et al75 | 2017 | 2015–2016 | Community | ADA 2005: FPG≥7 mmol/L (≥126 mg/dL) or self-reporting having been diagnosed by a health professional | Cross-sectional | 758 | ≥40 | 14.5 |
| 23 | Hoang et al76 | 2016 | 2014 | Community | FPG and post OGTT: FPG≥7 mmol/L or 2-hour OGTT≥11.1 mmol/L (MoH 2011); IGT: FPG<7 mmol/L and 2-hour OGTT≥7.8–11.1 mmol/L or normal but self-report having been diagnosed | Cross-sectional | 2402 | 30–69 | 7.9 |
| 24 | Do et al77 | 2015 | 2013 | Community | FPG and post OGTT (WHO 1999: FPG≥7 mmol/L or 2-hour OGTT≥11.1 mmol/L or self-report and MoH 2011) | Cross-sectional | 1200 | 40–59 | 5.3 |
| 25 | Nguyen and Nguyen78 | 2013 | 2011 | Community | ADA/WHO 2010: FPG 100–126 mg/dL or 2-hour OGTT from 140 to 200 mg/dL or HbA1c≥6.5% | Cross-sectional | 1100 | ≥45 | 11.9 |
| 26 | Nguyen et al,79 | 2017 | Community | WHO STEPS: fasting blood glucose values>6.1 mmol/L or taking medications for diabetes; measured fasting blood glucose by Cardiocheck PA | Cross-sectional | 2440 | 18–69 | 6.7 | |
| 27 | Do et al80 | 2014 | 2013 | Community | MoH 2011 on screening diabetes in community | Cross-sectional | 1200 | 40–59 | 16.6 |
| 28 | Tran et al81 | 2013 | 2009 | Community | WHO–STEPS: fasting blood glucose values≥6.1 mmol/L) or on diabetes medication or having diagnosed by a healath professional | Cross-sectional | 1714 | 25–64 | 4.7 |
| 29 | Vo and Pham82 | 2017 | 2015–2016 | Community | NM but not self-report | Cross-sectional | 1114 | >40 | 16.10% |
| 30 | Nguyen83 | 2018 | 2015–2016 | Community | NM but not self-report | Cross-sectional | 1250 | 18–55 | 16.20% |
| 31 | Dang and Nguyen55 | 2016 | 2012 | Community | NM but not-self report | Cross-sectional | 2700 | >20 | 5.80% |
| 32 | Do50 | 2015 | 2012 | Community | Diabetes was diagnosed when FPG was≥7.0 mmol/L or 2 hours post OGTT≥11.1 mmol/L | Cross-sectional | 3500 | 30–96 | 3.10% |
| 33 | Duong84 | 2013 | 2011 | Community | WHO 2006 | Cross-sectional | 2000 | 30–69 | 4.30% |
| 34 | Tran and Dam45 | 2013 | 2011 | Community | WHO (not mentioned the year) | Cross-sectional | 2400 | 30–64 | 10.30% |
| 35 | Dao et al,46 | 2012 | 2010 | Community | WHO 1999 | Cross-sectional | 3100 | All age | 9.35% |
| 36 | Do and Nguyen85 | 2011 | 2010 | Community | OMS 1999, ADA 2005 | Cross-sectional | 3500 | 30–69 | 6.10% |
| 37 | Nguyen and Pham52 | 2011 | 2010 | Community | NM but not self-report | Cross-sectional | 1855 | 30–60 | 4.40% |
| 38 | Dzoan86 | 2011 | 2011 | Hospital based | Diabetes was diagnosed when FPG was ≥7.0 mmol/L or 2 hours post OGTT≥11.1 mmol/L | Cross-sectional | 2358 | 30–60 | 3.60% |
| 39 | Hoang43 | 2008 | 2005–2007 | Community | American Diabetes Association 1998 | Cross-sectional | 1335 | 18–70 | 3.1 |
| 40 | Vien and Phung87 | 2008 | 2008 | Community | NM but not self-report | Cross-sectional | 1620 | 18–60 | 2.60% |
| 41 | Do88 | 2004 | 2000 | Community | WHO 1999 | Cross-sectional | 212 | ≥16 | 1.42% |
| 42 | To et al89 | 2003 | May 2000 to September 2000 | Community | Diabetes was diagnosed when FPG was ≥7.0 mmol | Cross-sectional | 2017 | ≥16 | 3.62 |
| 43 | Do et al90 | 2003 | March 2002 to December 2002 | Community | Diabetes (WHO 1999) | Cross-sectional | 890 | 40–60 | 6.10% |
ADA, The American Diabetes Association; IDF, International Deiabetes Federation; IGT, Impaired Glucose Tolerance; MOH or MoH, Ministry of Health; OGTT, Oral Glucose Tolerance Test; QĐ-BYT, Quyết định - Bộ Y Tế (Decision - Ministry of Health); STEPS, WHO STEPS survey.
Table 3.
Summery of the reported prevalence rate of hypertension in Vietnam (2000–2020)
| SI | Author name | Publication year | Study conducted | Community/hospital based | Reference standard | Study design | Sample size | Age range | Prevalence of hypertension |
| 1 | Pham et al26 | 2009 | 2015 | Community | Raised blood pressure was defined as an average (based on STEPS rule) systolic blood pressure (SBP)≥140 mm Hg and/or average diastolic blood pressure (DBP)≥90 mm Hg and/or self-reported current medication for high blood pressure in the previous 2 weeks | Cross-sectional | 1978 | 25–64 | 18.9 |
| 2 | Bao et al91 | 2019 | 2019 | Community | SBP/DBP≥140/90 mm Hg or using antihypertensive medication | Cross-sectional | 2203 | ≥18 | 24.3 |
| 3 | Nam et al31 | 2018 | 2017 | Community | HTN was specified that SBP was 140 mm Hg or higher and/or DBP was 90 mm Hg or higher, if the medications used to treat HTN were used by the individuals for 2 weeks. ISH having an SBP≥140 mm Hg and DBP<90 mm Hg was used to diagnose | Cross-sectional | 675 | ≥18 | 47.3 |
| 4 | Hoang et al92 | 2019 | 2015 | Community | Raised blood pressure was defined as an average (based on STEPS rule) SBP≥140 mm Hg and/or average DBP≥90 mm Hg and/or self-reported current medication for high blood pressure in the previous 2 weeks | Cross-sectional | 3856 | 18–69 | 18.9 |
| 5 | Son et al93 | 2011 | 2002 | Community | Defined as BP≥140/90 mm Hg | Cross-sectional | 9832 | ≥25 | 25.1 |
| 6 | Do et al94 | 2014 | 2005 | Community | Hypertension was defined as SBP≥140 mm Hg and/or DBP≥90 mm Hg and/or self-reported current use of antihypertensive medication | Cross-sectional | 17 199 | 25–64 | 20.7 |
| 7 | Binh et al48 | 2014 | NM | Community | SBP≥130 mm Hg or DBP≥85 mm Hg or hypertension; | Cross-sectional | 2443 | 48–57 | 14.3 |
| 8 | Namet al31 | 2007 | 2005 | Community | SBP was at least 140 mm Hg, their DBP was at least 90 mm Hg, or they were being treated for hypertension | Cross-sectional | 2000 | 25 to 64 | 18.8 |
| 10 | Pham and Eggleston95 | 2015 | 2011–2013 | Community | Hypertension was defined as SBP 140 mm Hg and/or DBP 90 mm Hg or current use of antihypertensive medication | Cross-sectional | 5602 men and 10 680 women | 30–69 | 47.0 |
| 11 | Nam et al31 | 2005 | 2002 | Community | Hypertensive subjects were defined as those with SBP equal to or more than 140 mm Hg or DBP equal to or more than 90 mm Hg 18 or those being treated for hypertension | Cross-sectional | 2000 | 25–64 | 14.1 |
| 12 | Miyakawa et al25 | 2017 | 2014 | Community | Hypertension was defined as elevated BP, with SBP≥140 mm Hg and/or DBP≥90 mm Hg | Cross-sectional | 376 | 20–70 | 15 |
| 13 | Tran96 | 2007 | 2005 | Community | JNC VII (2003) | Cross-sectional | 1991 | 25–65 | 26.5 |
| 14 | Vo and Dang97 | 2007 | 2005 | Community | JNC VII | Cross-sectional | 1288 | 25 + | 28.4 |
| 15 | Le and Nguyen98 | 2011 | 2010 | Community | SBP≥140 mm Hg and/or DBP≥90 mm Hg | Cross-sectional | 1991 | 25–64 | 16.0 |
| 16 | Nguyen et al49 | 2008 | 2008 | Community (workplace) | NM but not self-report | Cross-sectional | 383 | NM | 16.0 |
| 17 | Vu et al99 | 2005 | 2004 | Community | SBP≥140 mm Hg and/or DBP≥90 mm Hg | Cross-sectional | 2366 | 18+ | 21.8 |
| 18 | Nguyen et al100 | 2013 | 2013 | Hospital based | NM but not self-report | Cross-sectional | 379 | NM | 13.3 |
| 19 | Tran and Nguyen101 | 2014 | 2012 | Community | SBP≥140 mm Hg and/or DBP≥90 mm Hg | Cross-sectional | 872 | 25–64 | 15.0 |
| 20 | Le et al69 | 2014 | 2011 | Community | Decision 3192/QĐ‐BYT dated 31 August 2010, Vietnam Ministry of Health | Cross-sectional | 1401 | 40+ | 30.6 |
| 21 | Nguyen102 | 2019 | 2016–2018 | Hospital based | NM but not self-report | Retrospective | 65 | NM | 49.2 |
| 22 | Lam and Lam103 | 2019 | 2012–2018 | Community | National hypertension programme: SBP≥140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 10 188 | ≥40 | 22.2 |
| 23 | Pham et al,72 | 2019 | 2014–2015 | Community (workplace) | NM (SBP≥140 mm Hg or DBP≥90 mm Hg) | Cross-sectional | 1595 | NM | 15.4 |
| 24 | Vo et al75 | 2017 | 2015–2016 | Community | SBP≥140 mm Hg or DBP≥90 mm Hg or reporting having diagnosed and on medication by a health professional | Cross-sectional | 1153 | ≥18 | 33.8 |
| 25 | Nguyen et al104 | 2017 | 2011–2015 | Community | MoH 2010, SBP≥140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 20 000 | ≥25 | 28.5 |
| 26 | Pham et al105 | 2017 | 2014 | Community | STEPS, SBP≥140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 459 | 45–64 | 35.5 |
| 28 | Nguyen et al106 | 2017 | 2016 | Community | SBP≥140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 2699 | 18–69 | 18.97 |
| 29 | Tran et al107 | 2017 | 2016 | Workplace | NM but not self-report | Cross-sectional | 1930 | NM | 2.3 |
| 30 | Do et al77 | 2015 | 2013 | Community | JNC7, MoH 2010, SBP≥140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 1200 | 40–59 | 19.7 |
| 31 | Hong108 | 2015 | 2013 | Community | NM (must be SBP≥140 mm Hg or DBP≥90 mm Hg be because this was a baseline survey of an intervention with control group) | Cross-sectional | 1619 | ≥25 | 20.7 |
| 32 | Le et al109 | 2015 | 2013 | Community | WHO—SBP≥140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 800 | ≥18 | 16.8 |
| 33 | Do et al80 | 2014 | 2012 | Community | JNC-7—SBP≥140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 1200 | 40–59 | 19.7 |
| 34 | Chu110 | 2014 | 2014 | Community | MOH, 2010: 140 mm Hg or DBP≥90 mm Hg | Cross-sectional | 2085 | ≥25 | 18.0 |
| 35 | Nguyen111 | 2014 | 2011 | Community | 140 mm Hg or DBP≥80 mm Hg | Cross-sectional | 1833 | ≥25 | 11.8 |
| 37 | Tran et al81 | 2013 | 2009 | Community | WHO–STEPS: 140 mm Hg or DBP≥90 mm Hg or on medication | Cross-sectional | 1714 | 25–64 | 17.8 |
| 38 | Vien and Phung87 | 2008 | 2008 | Community | NM but not self-report | Cross-sectional | 1620 | 18–60 | 15.8 |
| 39 | Do et al90 | 2003 | March 2002 to December 2002 | Community | Hypertension diagnosis (>140/90) Diabetes (WHO 1999) |
Cross-sectional | 890 | 40–60 | 12.7 |
HTN, Hypertension; ISH, International Society of Hypertension; JNC VII, The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; MoH, Ministry of Health; NM, Not mentioned; QĐ-BYT, Quyết định - Bộ Y Tế (Decision - Ministry of Health); STEPS, WHO STEPS survey.
Data analysis
All meta-analyses were performed using MetaXL V.1.4.20 We calculated pooled prevalence of T2DM and HTN. In addition, we also assessed the pooled prevalence of T2DM and HTN by year interval and sex. We also assessed publication bias using both a graphical (Doi plot) and quantitative (Luis Furuya-Kanamori index) examination for potential small study effects.21 The methodology that we followed for the meta-analysis was described in details by Neyeloff et al.22 Briefly, for each study, we calculated the following variables: (1) SE of the prevalence, (2) variance, (3) study weights (inversed variance), (4) study weight*prevalence estimate, (5) study weight* (prevalence estimate)2 and (6) (study weight)2. We used these variables to estimate Q measure. We adapted the modified Newcastle Ottawa Scale for assessing the quality of the study, as recommended by the Cochrane Collaboration.23 Four criteria were used to score studies as ‘high quality’ (4 points), ‘moderate quality’ (2–3 points) and ‘poor quality’ (0–1 points). Criteria included: target population a close representation of the national population (yes=1, no=0), sufficient sample size (yes=1, no=0), random sampling (yes=1, no=0) and ascertainment of T2DM and HTN measure (yes=1, no=0). The cut-off for a sufficient sample size was set at 500 participants.20 24
We checked for statistical heterogeneity and inconsistency using the Q and I2 statistics, respectively, of heterogeneity among studies) and I2 (per cent between-studies variability). Based on Q and I2 values, we chose quality effects models to report pooled prevalence estimates (HTN, T2DM) and the associated 95% CI to minimise the heterogeneity. We followed the same procedures to calculate the pooled prevalence of T2DM and HTN by time periods (2000–2004; 2005–2010; 2011–2015; 2016–2020) and sex. We checked for statistical heterogeneity and inconsistency using the Q and I2 statistics, respectively.
Patient and public involvement
No patient involved
Result
Study characteristics and quality
Our literature search yielded 4054 records. After exclusion of duplicates and review of titles and abstracts, articles were included for further evaluation. Of these, full texts could not be found for 43 articles. The full text of the remaining 341 articles were examined and a total of 259 articles excluded after abstract screening. We were unable to access the full text of these documents at the time we searched for relevant papers across databases. These papers were published in Vietnamese language. Of them, about two-thirds were government-funded project reports, which require fees for archived access; the remaining papers were not available on the Vietnamese journal websites. We included 82 articles in the final synthesis (figure 1). These articles presenting data for 239 034 individuals. Out of these, 44 articles reported prevalence of T2DM and 39 articles reported prevalence of HTN. For T2DM, all were cross-sectional in nature (table 2). Majority of the studies (92.4%) were community based and only three studies were facility based (7.6%). For HTN, all were cross-sectional in nature (table 3). Majority of the studies (90%) were community based and only four studies were facility based (10%). Quality score of each study presented in (online supplemental tables S2 and S3. Majority of the articles came from Vietnamese language.
Figure 1.
Consort diagram: search strategy and selection of studies included in this review.
Estimation of prevalence rates
Prevalence rates varied widely across studies, from 1.0% to 29.0% for T2DM and 2.0% to 47.0% for HTN. The pooled prevalence of T2DM and HTN in Vietnam for all studies was 6.0% (95% CI: 4.0% to 7.0%) and 25% (95% CI: 19% to 31%), respectively (figures 2 and 3).
Figure 2.
Pooled prevalence of diabetes in Vietnam.
Figure 3.
Pooled prevalence of hypertension in Vietnam.
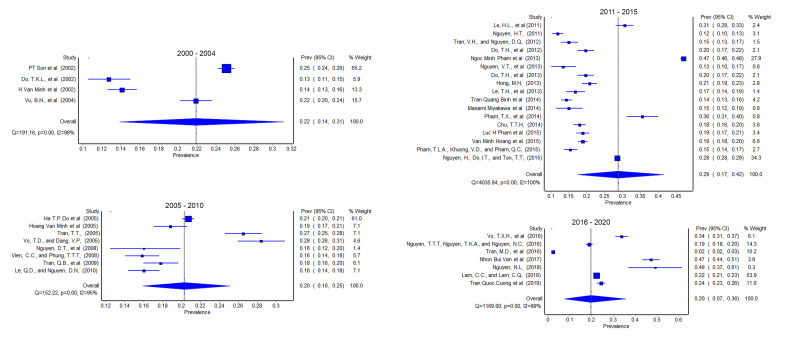
Prevalence rates by year of study
To investigate T2DM and HTN prevalence over time, we arranged outcomes by time of study in four aggregated intervals (i) 2000–2004, (ii) 2005–2010, (iii) 2011–2015 and (iv) 2016–2020.
2000–2004
We included nine studies from 2000 to 2004 in our analysis, six of these studies presented findings for T2DM25–30 and three for HTN.29 31 32 The pooled estimate of T2DM was 3.0% (95% CI: 1.0% to 5.0%), whereas for HTN it was 22.0% (95% CI: 14.0% to 31.0%) (figures 4 and 5).
Figure 4.
Prevalence of diabetes in Vietnam by year of study.
Figure 5.
Prevalence of hypertension in Vietnam by year of study.
2005–2010
Nineteen studies between 2005 and 2010 presented both prevalence of T2DM and HTN in Vietnam in which ten studies30 33–41 presented prevalence of T2DM and ten studies focused on HTN.33 34 37 41–47 The pooled estimate of T2DM was 5.0% (95% CI: 3.0% to 7.0%), whereas for HTN it was 20.0% (95% CI: 16.0% to 25.0%) (figures 4 and 5).
2011–2015
We identified 37 studies that presented findings for T2DM between the years 2011 and 2015. These resulted in a pooled estimate of T2DM 6.0% (95% CI: 4.0% to 9.0%) from 20 studies.36 39–41 48–59 We identified 18 studies for the same period in Vietnam that presented findings for HTN25 31–33 40 41 43 45 46 50–52 54 58–61 resulting in a pooled estimate of 29% (95% CI: 17% to 42%).
2016–2020
For the most recent interval, we identified eight studies31 44 47–49 53 57 for T2DM in Vietnam with a pooled estimate of 9.0% (95% CI: 5.0% to 14.0%). We also identified eight studies34 44 47–49 53 56 57 for HTN in the region with a pooled estimate of 20.0% (95% CI: 7.0% to 36.0%).
Gender-specific prevalence
We identified six studies for type T2DM and nineteen for HTN for use in gender-specific prevalence analysis (figures 6 and 7). Pooled estimate for T2DM slightly higher among the male (5.0%, 95% CI: 4.0% to 7.0%) compared with female (4.0%, 95% CI: 3.0% to 5.0%). For HTN, pooled estimate also higher among the male (25.0%, 95% CI: 22.0% to 28.0%) compared with female (18.0%, 95% CI: 15.0% to 22.0%).
Figure 6.
Prevalence diabetes in Vietnam by gender.
Figure 7.
Prevalence hypertension in Vietnam by gender.
Publication bias
The funnel plots for the T2DM and HTN were presented in online supplemental figures S1a-d and S2a-d. According to these figures, large heterogeneity was observed both for the T2DM and HTN prevalence estimation.
Discussion
This is the first systematic evaluation and meta-analysis of the scientific literature on the pooled prevalence trend of T2DM and HTN among the adult population in Vietnam. In our study, we found the pooled prevalence of T2DM has increased around three times from 2000 to 2004 (3%) and 2016 to 2020 (9%). A systematic review study by Nguyen et al reported that prevalence estimates of T2DM were 2.7% in 2002 and 5.4% in 2012.17 To our knowledge, this is the updated systematic review and meta-analysis paper on T2DM and HTN in Vietnam. The growing trend of T2DM in Vietnam in the present review is consistent with secular trends in several Asian countries such as China,62 India,61 Sri Lanka and Bangladesh63 where researchers also observed the similar magnitudes of a 10-year increase in T2DM prevalence. It is already well know that older age, urban residence, overweight, increased central adiposity, and physical inactivity, genetic factors, HTN, and high intake of animal protein may contribute to enhanced diabetes.17 In our study, due to data limitation, we were not able to assess the major drivers of T2DM in Vietnam; however, we expect Vietnam shares similar characteristics such as others in LMICs.
The pooled analysis from this study found that the prevalence of HTN has increased dramatically in Vietnam since 2000–2004. In another systematic review and meta-analysis study, Meiqari et al reported that pooled prevalence of measured HTN in Vietnam was 21.1%.16 In that study, they included the only English language studies but in our study, we included both English and Vietnamese studies, which we believe it gives a proper scenario of HTN in Vietnam. A review study by Hoy et al reported that high blood pressure is common among the Vietnamese population and they had knowledge that they have high blood pressure may be low.64
The main strength of the current study is that we followed a systematic and comprehensive approach to identify studies on both T2DM and HTN following MOOSE guidelines and a registered protocol. Risk of bias was assessed using well-established criteria. Within the study, we also investigated the sex-specific prevalence and as well as time trend. The main weakness of this study comes from the research this review identified. Although the majority of studies included in this review were graded as moderate-to-high quality, many were cross-sectional in nature and followed a survey-based approach. In addition, findings of this study were extremely heterogeneous in nature, not only in study design and data collection but also in outcome. To minimise the heterogeneity, we chose the quality effect model, which is now well established. As with all systematic reviews, there is the potential for publication bias in the identified studies, with some not initially designed to report on the T2DM and HTN. The reference standards for determining T2DM and HTN were not consistent between all studies. In addition, we attempted to explore factors associated with T2DM and HTN but insufficient studies reported this information. Another limitation, we searched PubMed, EMBASE, CINAHL, Google Scholar, Google and national website and database. There may be some other relevant data base we may miss it. But in our study, we included articles from Vietnamese journals. Moreover, information on certain groups, such as ethnicity and place of residence, were not available in enough studies to be included in subgroup analysis.
Although an adequate number of T2DM and HTN prevalence studies have been conducted, they were mostly reported the overall prevalence. Little data exist on the place of residence specific, education specific, wealth index and geographic location-specific prevalence of T2DM and HTN. We did not find any longitudinal cohort studies on T2DM and HTN. This is a significant gap in the knowledge and understanding of these chronic diseases in the context of Vietnam. Such studies would provide essential information on the incidence of these diseases, their associated risk factors, and the groups that are at higher risk of developing them. Further, longitudinal data are necessary to understand disease progression and prognosis.
Conclusion
We found increase in the prevalence T2DM and HTN among the adult population in Vietnam over the study period. We also found T2DM and HTN higher among the male compared than female. Future research should investigate the driving force behind the increasing rates of T2DM and HTN and explain the major drivers in both conditions. Policy approaches should base upon the trends of T2DM and HTN in Vietnam over the last 20 years and pay more attention on the effective interventions to combat T2DM and HTN.
Supplementary Material
Acknowledgments
The authors are grateful for the generous and helpful comments of the reviewers. We thank The Institute for Social Science Research, The University of Queensland and The Health Strategy and Policy Institute, Vietnam Ministry of Health for their support.
Footnotes
Contributors: All authors made a substantial contribution to this work. NT, AM, and TTMO conceptualised the review. NT, TB, TTMO, and AM designed the research. TB, NT, HTMH, PHV, PVH, NTTC, and KTA collected data, read, screened abstracts and titles of potentially relevant studies and took responsibilities for extracting data and rating their quality independently. TB and NT analysed and interpreted the data. TB, NT, and AM drafted manuscript with all the authors critically reviewing it and suggesting amendments prior to submission. NT is acting as guarantor.
Funding: This work was funded by The University of Queensland (UQ) Global Strategy and Partnership Seed Funding Scheme 2018 and The Institute for Social Science Research for strengthening the collaboration between UQ researchers and Vietnamese researchers (grant number not applicable). NT, TB, and AM are also supported by the Australian Government through the Australian Research Council's Centre of Excellence for Children and Families over the Life Course (Project ID CE200100025).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Bukhman G, Mocumbi AO, Atun R, et al. The Lancet NCDI poverty Commission: bridging a gap in universal health coverage for the poorest billion. Lancet 2020;396:991–1044. 10.1016/S0140-6736(20)31907-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bennett JE, Stevens GA, Mathers CD, et al. Ncd countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. The Lancet 2018;392:1072–88. 10.1016/S0140-6736(18)31992-5 [DOI] [PubMed] [Google Scholar]
- 3.Pham BD, Kim BG, Nguyen TTH, et al. Exposure to messages on risk factors for noncommunicable diseases in a rural Province of Vietnam. Biomed Res Int 2019;2019:1–8. 10.1155/2019/7962947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Diabetes and hypertension in India. JAMA Intern Med 2018;178:363–72. 10.1001/jamainternmed.2017.8094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization , 2021. Noncommunicable diseases. Available: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases [Accessed 7 July 2022].
- 6.Farrell P, Thow AM, Abimbola S, et al. How food insecurity could lead to obesity in LMICs: when not enough is too much: a realist review of how food insecurity could lead to obesity in low- and middle-income countries. Health Promot Int 2018;33:812–26. 10.1093/heapro/dax026 [DOI] [PubMed] [Google Scholar]
- 7.Li L, Sun N, Zhang L, et al. Fast food consumption among young adolescents aged 12-15 years in 54 low- and middle-income countries. Glob Health Action 2020;13:1795438. 10.1080/16549716.2020.1795438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Umberger WJ, Rupa JA, Zeng D. Understanding food westernisation and other contemporary drivers of adult, adolescent and child nutrition quality in urban Vietnam. Public Health Nutr 2020;23:2571–83. 10.1017/S1368980020001354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . Global health estimate 2016: deaths by cause, Age, Sex, by country and by region, 2000 - 2016. Geneva; 2018. [Google Scholar]
- 10.Institute for Health Metrics and Evaluation , 2017. Global burden of disease. top 10 causes of years of life lost (YLLs) in 2017 and percent change, 2007-2017, all ages, number. Available: https://www.healthdata.org/vietnam [Accessed 7 July 2022].
- 11.Girum T, Shumbej T, Shewangizaw M. Burden of malaria in Ethiopia, 2000-2016: findings from the global health estimates 2016. Trop Dis Travel Med Vaccines 2019;5:1–7. 10.1186/s40794-019-0090-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alex K . Tackling high blood pressure in Vietnam - in pictures, 2018. The guardian. Available: https://www.theguardian.com/healthcare-network/gallery/2018/may/17/high-blood-pressure-vietnam-world-hypertension-day [Accessed 7 July 2022].
- 13.Organization WH. Noncommunicable diseases country profiles 2018; 2018. https://apps.who.int/iris/handle/10665/274512 [Accessed 7 July 2022].
- 14.Bui TV, Blizzard CL, Luong KN, et al. National survey of risk factors for non-communicable disease in Vietnam: prevalence estimates and an assessment of their validity. BMC Public Health 2016;16:1–12. 10.1186/s12889-016-3160-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thuy Duyen N, Van Minh H, Van Huy N, et al. Patterns of behavioral risk factors for non-communicable diseases in Vietnam: a narrative scoping review. Health Psychol Open 2020;7:2055102920967248:205510292096724. 10.1177/2055102920967248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meiqari L, Essink D, Wright P, et al. Prevalence of hypertension in Vietnam: a systematic review and meta-analysis. Asia Pac J Public Health 2019;31:101–12. 10.1177/1010539518824810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen CT, Pham NM, Lee AH, et al. Prevalence of and risk factors for type 2 diabetes mellitus in Vietnam: a systematic review. Asia Pac J Public Health 2015;27:588–600. 10.1177/1010539515595860 [DOI] [PubMed] [Google Scholar]
- 18.Cochrane Effective Practice and Organisation of Care Group . Data collection checklist. EPOC, 2015. [Google Scholar]
- 19.Hoque ME, Long KZ, Niessen LW, et al. Rapid shift toward overweight from double burden of underweight and overweight among Bangladeshi women: a systematic review and pooled analysis. Nutr Rev 2015;73:438–47. 10.1093/nutrit/nuv003 [DOI] [PubMed] [Google Scholar]
- 20.Biswas T, Magalhaes RJS, Townsend N, et al. Double burden of underweight and overweight among women in South and Southeast Asia: a systematic review and meta-analysis. Adv Nutr 2020;11:128–43. 10.1093/advances/nmz078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Furuya-Kanamori L, Barendregt JJ, Doi SAR. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc 2018;16:195–203. 10.1097/XEB.0000000000000141 [DOI] [PubMed] [Google Scholar]
- 22.Neyeloff JL, Fuchs SC, Moreira LB. Meta-Analyses and forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes 2012;5:1–6. 10.1186/1756-0500-5-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JPT DJ, Altman DG, Higgins JPT, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, 2011. www.handbook.cochrane.org [Google Scholar]
- 24.Saquib N, Saquib J, Ahmed T, et al. Cardiovascular diseases and type 2 diabetes in Bangladesh: a systematic review and meta-analysis of studies between 1995 and 2010. BMC Public Health 2012;12:434. 10.1186/1471-2458-12-434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miyakawa M, Shimizu T, Van Dat N, et al. Prevalence, perception and factors associated with diabetes mellitus among the adult population in central Vietnam: a population-based, cross-sectional seroepidemiological survey. BMC Public Health 2017;17:1–8. 10.1186/s12889-017-4208-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pham LH, Au TB, Blizzard L, et al. Prevalence of risk factors for non-communicable diseases in the Mekong delta, Vietnam: results from a steps survey. BMC Public Health 2009;9:1–8. 10.1186/1471-2458-9-291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Hospital of Endocrinology . National program on diabetes control and prevention [in Vietnamese. 1st ed, 2002. [Google Scholar]
- 28.Vien CC, Phung TTT. Survey on overweight, hypertension, and diabetes among workers in middle region Vietnam. J Employ Prote 2008:17–21. [Google Scholar]
- 29.Do TT. Prevalence of diabetes and decreased blood sugar in Tan DAN and Thai son communes, an Lao district, HAI Phong. Viet Medi J 2004;11:128–32. [Google Scholar]
- 30.To VH, Vu MH, Nguyen VH. Epidemiological survey on diabetes among population aged 16 and older in three districts in Hanoi. Viet Medi J 2003;6:p. 58–64. [Google Scholar]
- 31.Nam KD, Van NB, Hoang LV, et al. Hypertension in a mountainous Province of Vietnam: prevalence and risk factors. Heliyon 2020;6:e03383. 10.1016/j.heliyon.2020.e03383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vo TD, Dang VP. Hypertension in long an Province in 2005: prevalence and risk factors. J Medi Pharm 2007;11:122–8. [Google Scholar]
- 33.Hoy D, Rao C, Nhung NTT, et al. Risk factors for chronic disease in Viet Nam: a review of the literature. Prev Chronic Dis 2013;10:120067. 10.5888/pcd10.120067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Le NTD, Dinh Pham L, Quang Vo T. Type 2 diabetes in Vietnam: a cross-sectional, prevalence-based cost-of-illness study. Diabetes Metab Syndr Obes 2017;10:363. 10.2147/DMSO.S145152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Do TaNL. Investigation for associated factors and epidemiology of type 2 diabetes in Hochiminh City [in Vietnamese]. Vietn J Food Nutrit Scien 2008. [Google Scholar]
- 36.Ta MTT, Nguyen KT, Nguyen ND, et al. Identification of undiagnosed type 2 diabetes by systolic blood pressure and waist-to-hip ratio. Diabetologia 2010;53:2139–46. 10.1007/s00125-010-1841-6 [DOI] [PubMed] [Google Scholar]
- 37.National Hospital of Endocrinology . N.H.o.E.N.p.o.d.c.a.p.i.V.n.e.H.M.P. evaluation of the effectiveness of preventative intervention programs on diabetes in community. Hanoi: Ministry of Science and Technology; 2012. [Google Scholar]
- 38.Pham VBa, Truong QD. Prevalence of diabetes and its related factors among people aged 30 - 69 in Binh Dinh province in 2018 Ho Chi Minh City. J Medic Pharm 2019;23:58–62. [Google Scholar]
- 39.Vo TXH, NHT C, Phan TKH, et al. Prevalence of hypertension and diabetes among adults in Ho Chi Minh city - a community - based study in an urban district. J Prev Med 2017;27:79–87. [Google Scholar]
- 40.Hoang DH, Chu TTH, Bui CD. Prevalence of diabetes type 2 and prediabetes of people age 30 - 69 in Hanoi 2014. J Prev Med 2016;26:94–101. [Google Scholar]
- 41.Do TH, Truong VD, Nguyen TL, et al. Prevalence of hypertension, hyperglycemia and certain related factors in middle age group in Dong son district, Thanh Hoa Province 2013. J Prev Med 2014;24:30–6. [Google Scholar]
- 42.Dzoan TTV. Some risk factors of diabetes type 2 in subjects aged 30 - 60 years in the hospital 198. J Food Nutr Scien 2011;7:51–60. [Google Scholar]
- 43.Hoang DM. Studying on prevalence of diabetes in HAI Phong. VMJ 2008;1:1–4. [Google Scholar]
- 44.Hoa NB, Phuc PD, Hien NT, et al. Prevalence and associated factors of diabetes mellitus among tuberculosis patients in Hanoi, Vietnam. BMC Infect Dis 2018;18:1–9. 10.1186/s12879-018-3519-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tran VH, Dam VC. Research on diabetes and knowledge, practice on complication prevention of population 30 - 64 years old in Hau Giang province in 2011. J Pract Med 2013;4:23–7. [Google Scholar]
- 46.Dao TMA, Tran ML, Tran TPN. Diabetes type II at age group of 30 - 69 in Nghe An population in 2010. J Med Res 2012;79:186–93. [Google Scholar]
- 47.Do MC, Nguyen TH. Assessment prevalence of diabetes, glucose tolerance (IGT) and risk factors in the age 30 - 69 in suburbs of Hai Phong 2010. JMPDC 2011;4:70–8. [Google Scholar]
- 48.Binh TQ, Phuong PT, Nhung BT, et al. Metabolic syndrome among a middle-aged population in the red River delta region of Vietnam. BMC Endocr Disord 2014;14:1–9. 10.1186/1472-6823-14-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nguyen DT, HN L, Phung DN, et al. Health situation and behavioural factors related to health of Saigon brewery workers in 2008 HO Chi Minh City. J Med Pharm 2008;12:229–33. [Google Scholar]
- 50.Do MC. Research on the level of relevance between some risk factors and diabetes and glycemia disorder of people from 30 - 69 years old in three urban districts of Hai Phong in 2012. VJM 2015;2:103–8. [Google Scholar]
- 51.Duong TH. Early diagnosis of diabetes and glucose disorder among adults in HAI Phong 2011 Vietnam. J Medicine 2013. [Google Scholar]
- 52.Nguyen VQ, Pham TH. Survey on prevalence of diabetes and prediabetes in HAI Hau distric, Nam Dinh Province 2010. VMJ 2011;1:5–10. [Google Scholar]
- 53.Dao-Tran T-H, Anderson D, Chang A, et al. Factors associated with self-management among Vietnamese adults with type 2 diabetes. Nurs Open 2018;5:507–16. 10.1002/nop2.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nguyen VL. Hypertension increase and its risk factors among labor- aged population in Hau Giang Province in 2016. J Com Med 2018;1:84–91. [Google Scholar]
- 55.Dang HC, Nguyen VL. Prevalence of diabetes type 2 and its risk factors in Ca mau Province: solutions for management and prevention. J Comm Med 2016;32:30–5. [Google Scholar]
- 56.Nguyen TTT, Nguyen TQ, Nguyen NC. Raised blood glucose situation among adults 18 - 69 years old in Hanoi 2016. J Prev Med 2017;27:92–8. [Google Scholar]
- 57.Kien VD, Van Minh H, Giang KB, et al. Socioeconomic inequalities in catastrophic health expenditure and impoverishment associated with non-communicable diseases in urban Hanoi, Vietnam. Int J Equity Health 2016;15:p. 1–11. 10.1186/s12939-016-0460-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Binh TQ, Nhung BT. Prevalence and risk factors of type 2 diabetes in middle-aged women in northern Vietnam. Int J Diabetes Dev Ctries 2016;36:150–7. 10.1007/s13410-015-0372-6 [DOI] [Google Scholar]
- 59.Nguyen QV, NN L. Prevalence and correlates of pre-diabetes, diabetes in some provinces in southern Vietnam: a cross-sectional study HO Chi Minh City. J Med Pharm 2014;18:451–7. [Google Scholar]
- 60.Do TT. Diabetes prevalence and glucose desreased tolerance at Tan Dan & Thai Son communes, An Lao District-Hai Phong. JVM 2004:128–32. [Google Scholar]
- 61.Ramachandran A, Snehalatha C, Shetty AS, et al. Trends in prevalence of diabetes in Asian countries. World J Diabetes 2012;3:110–7. 10.4239/wjd.v3.i6.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zuo H, Shi Z, Hussain A. Prevalence, trends and risk factors for the diabetes epidemic in China: a systematic review and meta-analysis. Diabetes Res Clin Pract 2014;104:63–72. 10.1016/j.diabres.2014.01.002 [DOI] [PubMed] [Google Scholar]
- 63.Ramachandran A, Wan Ma RC, Snehalatha C. Diabetes in Asia. The Lancet 2010;375:408–18. 10.1016/S0140-6736(09)60937-5 [DOI] [PubMed] [Google Scholar]
- 64.Hoy D, Rao C, Nhung NTT, et al. Risk factors for chronic disease in Viet Nam: a review of the literature. Prev Chronic Dis;10. 10.5888/pcd10.120067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Duc Son LNT, Kusama K, Hung NTK, et al. Prevalence and risk factors for diabetes in Ho Chi Minh City, Vietnam. Diabet Med 2004;21:371–6. 10.1111/j.1464-5491.2004.01159.x [DOI] [PubMed] [Google Scholar]
- 66.Kien VD, Van Minh H, Giang KB, et al. Socioeconomic inequalities in catastrophic health expenditure and impoverishment associated with non-communicable diseases in urban Hanoi, Vietnam. Int J Equity Health 2016;15:1–11. 10.1186/s12939-016-0460-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pham NM, Eggleston K. Diabetes prevalence and risk factors among Vietnamese adults: findings from community-based screening programs. Diabetes Care 2015;38:e77–8. 10.2337/dc14-3093 [DOI] [PubMed] [Google Scholar]
- 68.Do T, Le N. Investigation for associated factors and epidemiology of type 2 diabetes in Hochiminh City [in Vietnamese]. Viet J Food Nutri Sci 2008. [Google Scholar]
- 69.Le HN, Nguyen TH, TL V, et al. The prevalence of non-communicable disease and its related factors among individuals aged 40 years and older living in long Thuan commune, BEN Cau district, Tay Ninh Province HO Chi Minh City. J Med Pharm 2014;18:746–54. [Google Scholar]
- 70.Pham VB, Truong QD. Prevalence of diabetes and its related factors among people aged 30 - 69 in Binh Dinh province in 2018 Ho Chi Minh City. J Med Pharm 2019;23:58–62. [Google Scholar]
- 71.Nguyen QV, Le NN. Prevalence and correlates of pre-diabetes, diabetes in some provinces in southern Vietnam: a cross-sectional study HO Chi Minh City. J Med Pharm 2014;18:451–7. [Google Scholar]
- 72.Pham TLA, Khuong VD, Pham QC. Current situation of health and diseases of the traffic police between 2014 - 2015. J Med Pharm 2019;29:55–63. [Google Scholar]
- 73.Vu DT, Dang BT. The prevalence of type 2 diabetes in people aged ≥25 years in Thai Binh Province 2017. J Med Pharm 2018;28:33–8. [Google Scholar]
- 74.Nguyen BT, TK L, Dao DK, et al. Diabetes mellitus prevalence of people aged from 45 to 69 and some related factors in SA Thay town, SA Thay district, Kon tum Province 2016. J Med Pharm 2017;27:146–53. [Google Scholar]
- 75.Vo TXH, NHT C, Phan TKH, et al. Prevalence of hypertension and diabetes among adults in Ho Chi Minh city - a community - based study in an urban district. J Med Pharm 2017;27:79–87. [Google Scholar]
- 76.Hoang DH, Chu TTH, Bui CD. Prevalence of diabetes type 2 and prediabetes of people age 30 - 69 in Hanoi 2014. J Med Pharm 2016;26:94–101. [Google Scholar]
- 77.Do TH, Nguyen TTD, Nguyen TL, et al. Actual situation on hypertension, diabetes and the health care requirement status among people of the middle-age group (from 40 - 59) at Dong Son district, Thanh Hoa province 2013. J Med Pharm 2015;25:381–90. [Google Scholar]
- 78.Nguyen VL, Nguyen VT. The rate of diabetes and some factors related to the Khmer ethnic minority people who are 45 years and over in Hau Giang Province. J Med Pharm 2013;23:142–9. [Google Scholar]
- 79.Nguyen TTT, Nguyen TQ, Nguyen NC. Raised blood glucose situation among adults 18 - 69 years old in Hanoi 2016. J Med Pharm 2017;27:92–8. [Google Scholar]
- 80.Do TH, Truong VD, Nguyen TL, et al. Prevalence of hypertension, hyperglycemia and certain related factors in middle age group in Dong son district, Thanh Hoa Province 2013. J Med Pharm 2014;24:30–6. [Google Scholar]
- 81.Tran QB, Phan TL, Truong DB, et al. Steps survey on risk factors for non-communicable diseases in Can Tho city 2009 - 2010. J Med Pharm 2013;23:72–9. [Google Scholar]
- 82.Vo TD, Pham TT. Study on status of diabetes type 2 and assessment of intervention results on adults aged from 40 years old at My Xuyen, Soc Trang in 2015 - 2016. J Med Pharm 2017;9:138–45. [Google Scholar]
- 83.Nguyen VL. Hypertension increase and its risk factors among labor- aged population in Hau Giang Province in 2016. J Comm Med 2018;1:84–91. [Google Scholar]
- 84.Duong TH. Early Diagnosis of Diabetes and Glucose Disorder among Adults in Hai Phong 2011 Vietnam. J Medicine 2013. [Google Scholar]
- 85.Do MC, Nguyen TH. Assessment prevalence of diabetes, glucose tolerance (IGT) and risk factors in the age 30 - 69 in suburbs Haoi city 2010. J Malaria and Paras Dis Cont 2011;4:70–8. [Google Scholar]
- 86.Dzoan TTV. Some risk factors of diabetes type 2 in subjects aged 30 - 60 years in the hospital 198. J Food and Nutr Sci 2011;7:51–60. [Google Scholar]
- 87.Vien CC, Phung TTT. Survey on overweight, hypertension, and diabetes among workers in middle region Vietnam. J Employ Prot 2008:17–21. [Google Scholar]
- 88.Do TT. Prevalence of diabetes and decreased blood sugar in Tan DAN and Thai son communes, an Lao district, HAI Phong. VMJ 2004;11:128–32. [Google Scholar]
- 89.To VH, Vu MH, Nguyen VH. Epidemiological survey on diabetes among population aged 16 and older in three districts in Hanoi. VMJ 2003;6:58–64. [Google Scholar]
- 90.Do TKL, Nguyen DVA, Nguyen QD, et al. A study on nutritional status, related factors and high blood glucoza level of adults aged 40 to 60 living in a center district of Hanoi City. VMJ 2003;9:78–84. [Google Scholar]
- 91.Bao LV, Cuong TQ, Tuan NA. Associated factors of hypertension in women and men in Vietnam: a cross-sectional study. Int J Environ Res Public Health 2019;16:4714. 10.3390/ijerph16234714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hoang VM, Tran QB, Vu THL, et al. Patterns of raised blood pressure in Vietnam: findings from the who steps survey 2015. Int J Hypertens 2019;2019:1–7. 10.1155/2019/1219783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Son PT, Quang NN, Viet NL, et al. Prevalence, awareness, treatment and control of hypertension in Vietnam-results from a national survey. J Hum Hypertens 2012;26:268–80. 10.1038/jhh.2011.18 [DOI] [PubMed] [Google Scholar]
- 94.Do HTP, Geleijnse JM, Le MB, et al. National prevalence and associated risk factors of hypertension and prehypertension among Vietnamese adults. Am J Hypertens 2015;28:89–97. 10.1093/ajh/hpu092 [DOI] [PubMed] [Google Scholar]
- 95.Pham NM, Eggleston K. Prevalence and determinants of diabetes and prediabetes among Vietnamese adults. Diabetes Res Clin Pract 2016;113:116–24. 10.1016/j.diabres.2015.12.009 [DOI] [PubMed] [Google Scholar]
- 96.Tran TT. The influence factors involve knowledge and practice in adult about high blood pressure in Ho Chi Minh City 2005 HO Chi Minh City. J Med Pharm 2007;11:118–26. [Google Scholar]
- 97.Vo TD, Dang VP. Hypertension in long an Province in 2005: prevalence and risk factors HO Chi Minh City. J Med Pharm 2007;11:122–8. [Google Scholar]
- 98.Le QD, Nguyen DN. The prevalence of hypertension and body mass index among adults aged 25 - 64 years at Lam Dong in 2010 Ho Chi Minh City. J Med Pharm 2011;15:158–64. [Google Scholar]
- 99.Vu BN, HN L, Cao MN, et al. Prevalence of hypertension among adults living in district 4 - Ho Chi Minh city 2004 Ho Chi Minh City. J Med Pharm 2005;9:93–9. [Google Scholar]
- 100.Nguyen VT, Trang MHY, VT V, et al. Disease model in advanced bureaucrats who are monitored by the health care department of long an Province HO Chi Minh City. J Med Pharm 2013;17:331–4. [Google Scholar]
- 101.Tran VH, Nguyen DN. Prevalence of hypertension and its risk behaviours at the population among 25 - 64 years old in Ninh Hai district, Ninh Thuan province Ho Chi Minh City. J Med Pharm 2014;18:709–16. [Google Scholar]
- 102.Nguyen NL. Evaluating the effectiveness of management, protection and health care of cadres in Vinh Long province in 3 years 2016 - 2018 Ho Chi Minh City. J Med Pharm 2019;23:124–9. [Google Scholar]
- 103.Lam CC, Lam CQ. The status of hypertension and relevance between risk factors with hypertension in people aged ≥40 years old at Ninh Hoa town, Khanh Hoa province, 2012 - 2018. J Prev Med 2019;29:100–5. [Google Scholar]
- 104.Nguyen H, Do IT, Ton TT. Prevalence trend of hypertension and risk factors of cardiovascular disease among people aged 25 and older in dA Nang City between 2011 and 2015. J Prev Med 2017;27:55–64. [Google Scholar]
- 105.Pham TX, Nguyen TBY, Duong TH, et al. Reality of hypertension in aged of 45 - 64 year in Dien Bien district in 2014. J Prev Med 2017;27:67–73. [Google Scholar]
- 106.Nguyen TT, Nguyen TKA, Nguyen NC. Hypertension status among adults 18 - 69 years old in Hanoi 2016. J Prev Med 2017;27:84–91. [Google Scholar]
- 107.Tran MD, et al. Workers health conditions of the automobile and motorcycle brake manufacturing company in Vietnam in 2016. J Prev Med 2017;27:126–33. [Google Scholar]
- 108.Hong MH. Research on the high blood pressure in person from 25 years or older and results of intervention at Phu Tan district in Ca Mau province in 2014. J Prev Med 2015;25:333–41. [Google Scholar]
- 109.Le TH, Tran TMH, TTX L, et al. Prevalence of hypertension among adults in two rural communes, Quang Trach district, Quang Binh Province 2013. J Prev Med 2015;XXV:77–84. [Google Scholar]
- 110.Chu TTH. Prevalence of hypertension in Hanoi City in 2012. J Prev Med 2014;24:91–5. [Google Scholar]
- 111.Nguyen HT. Current status of hypertension of the adult population aged 25 years and older who living in Trang HA commune, Tu son town, BAC Ninh Province in 2011. J Prev Med 2014;24:80–5. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-052725supp001.pdf (1.7MB, pdf)
Data Availability Statement
Data are available upon reasonable request.