Abstract
In a sample of 28 individuals cohabiting with a partner in NYC, Boston, or Chicago, this study tested whether implementation of stay-home orders to combat the spread of COVID-19 disrupted physical activity and whether high-quality romantic relationships buffered adverse effects. Participants provided FitBit data between February – October, 2020. Stay-home orders were associated with a reduction in daily step counts, B = −1,595.72, p = .018, increased sedentary minutes, B = 33.75, p = .002, and reduced daily minutes of light and moderate physical activity, B = −25.01, p = .011; B = −0.72, p = .021. No moderation effects emerged.
Keywords: relationships, couples, physical activity, sedentary behavior, COVID-19
The novel coronavirus SARS-CoV-2, or COVID-19, changed daily life to an unprecedented degree. Although stay-home orders and social distancing policies were instrumental in slowing the spread of COVID-19, they may also have adversely impacted individuals’ health and well-being due to disruption of daily routines and health-maintaining behaviors. However, studies examining health behavior consequences of these policies remains rare.
One health behavior particularly likely to suffer when sheltering in place and engaging in social distancing is physical activity. Stressors associated with COVID-19 could reduce psychological assets that enable individuals to make healthy decisions – particularly more effortful ones, such as choosing to exercise – and environmental changes (e.g., reduced opportunities for exercise following gym closures or inability to go outdoors, no longer commuting to work) remove more reflexive cues that stimulate less effortful engagement in these behaviors (Dunton et al., 2019). Indeed, one study found that self-reported physical activity dropped by nearly 20% during the pandemic (Yang & Koenigstorfer, 2020), with others finding similar self-reported declines (Gallè et al., 2020; Rhodes et al., 2020). A study examining steps recorded by physical activity trackers found similar declines in countries with total lockdown policies (Pépin et al., 2020). Reductions in physical activity are not without consequence: not only is physical activity essential for maintaining physical health, it is also consistently linked with better mental health outcomes (Landers & Arent, 2007), which is critical during times of stress such as the COVID-19 pandemic. Research is needed to better understand how implementing lockdowns impacts physical activity, how physical activity patterns rebound over time, and potential protective factors that may buffer any declines in activity.
Close relationships are one factor associated with physical activity (Aral & Nicolaides, 2017; Darlow & Xu, 2011) and supportive interpersonal environments can help buffer against the negative effects of stressors (Cohen & Wills, 1985). In addition to restricted access to exercise spaces due to shelter-in-place mandates, social isolation and loneliness associated with COVID-19 and related policies could undermine maintenance of health-promoting behaviors such as physical activity (Courtin & Knapp, 2017; House et al., 1988). When individuals have restricted access to their social networks and are also limited in available health activities, as during the COVID-19 pandemic, romantic partnerships may become the primary interpersonal source of support. It is not merely the presence of a romantic relationship that benefits health, however, but also the quality of the relationship (Kiecolt-Glaser & Wilson, 2017). High-quality relationships are consistently linked to better physical and mental health (Loving & Slatcher, 2013; Robles et al., 2014), and prior studies have shown that one’s own and one’s partner’s happiness are each associated with self-reported health and exercise (Chopik & O’Brien, 2017). In addition to buffering stressors that might otherwise undermine physical activity, a close and supportive romantic partner could also provide emotional resources (Afifi, Merrill, & Davis, 2016) to help individuals engage in effortful exercise behaviors when reflexive cues are no longer present in the environment (Dunton et al., 2019). Unfortunately, COVID-19 has placed unprecedented stress upon romantic relationships, leading to reductions in satisfaction (though effects are heterogeneous; Balzarini et al., 2020; Günther-Bel et al., 2020; Williamson, 2020).
It is unclear whether relationship benefits extend to the unique situation wherein couples are physically isolated from other potentially important support networks, such as friends, family, and workplace relationships. In pre-pandemic times, the association of high-quality relationships with well-being may have been confounded by a general tendency towards positive and health-promoting social relationships (e.g., overlap between different measures of social support; Gottlieb & Bergen, 2010; associations of different relational aspects with health; DiMatteo, 2004). The current COVID-19 pandemic and shelter-in-place mandate in response to the virus’ spread provide a unique opportunity to investigate the impact of isolation on health behaviors in couples and determine whether high-quality romantic relationships are protective against declines in physical activity – irrespective of tendencies towards positive relationships more broadly.
To address these gaps in knowledge, using objectively measured physical activity data collected between February and October of 2020, the present study tests whether physical activity was reduced from the month prior to the shelter-in-place to post-policy implementation in couples living in three metropolitan areas in the United States with similar climate and seasons (NYC, Boston, and Chicago). We further explore whether individuals who sheltered in place together with a romantic partner and who also have high-quality relationships were protected against any adverse impact of social isolation on physical activity. Specifically, we hypothesized that there would be a significant decrease in objectively measured physical activity from pre- to post-shelter-in-place policy implementation (i.e., during the time that these policies were in place), and that individuals in high quality relationships would experience less decrease in physical activity from pre- to post-shelter-in-place implementation.
Methods
Participants
Participants were a convenience sample of 50 cohabiting couples living in either NYC, Boston, or Chicago. Participants were recruited via online postings (e.g., ResearchMatch, Facebook advertisements) between May and September, 2020. Interested participants clicked a link in the recruitment script and completed an online screening survey to confirm that they met the following eligibility criteria: (1) they were 18+ years of age, (2) they were currently cohabitating with a romantic partner, (3) the participant and their partner were the only two members living in their household at the time of the study (e.g., no children or other family members resided in the household), (4) at least one partner must have been a consistent Fitbit user (i.e., they used Fitbit prior to shelter-in-place and continued to use Fitbit at the time of the study), (5) they engaged in some form of physical activity (e.g. running, walking, biking) at least once during the month prior to shelter-in-place, and (6) they were in self-reported good health. If an interested participant qualified, they were asked to provide an email address for themselves and their partner, and the partner was then sent the same screening survey. If both partners met the eligibility criteria, they were then invited to participate in the study. The requirement to own and regularly sync a FitBit was dropped due to slow recruitment in order to ensure that all couples were enrolled within a reasonable timeframe and because dyadic communication hypotheses (not reported here) were not dependent on FitBit data. Of the 40 couples screened during the time this requirement was in place, 24 couples with at least one FitBit user were enrolled for the present analysis (four couples where both partners linked a FitBit, for n = 28 individuals in total).
Procedure
All study procedures were approved by the University of Connecticut Institutional Review Board. Participants and partners who met the above screening criteria were sent an initial email that provided an overview of the study, assigned study codes, and a link to the baseline survey. Participants provided informed consent by viewing the study information sheet on the first page of the baseline survey and confirming their agreement to participate. They then completed a baseline assessment comprising demographic information, measures of relationship quality, and other psychosocial measures (e.g., COVID-19-related anxiety, communication). The couple member with the FitBit additionally linked their device to Fitabase, a data management platform to support research using FitBit devices. Initially, participants granted permission to access data retrospectively from the month prior to shelter-in-place policy implementation (approximately February 20, 2020, through March 20, 2020) and prospectively during the month of study participation (e.g., during May of 2020). Post-hoc consent was obtained from 26 of the 28 participants to access all FitBit data from February 20, 2020, through October 19, 2020. There was no attrition.
Upon completing the baseline assessment, couples began seven days of daily diary assessments sent via Qualtrics. These were completed at the end of each day, and included questions on relationship processes (e.g., social support, communication). A final survey was sent via Qualtrics 28 days following enrollment, which concluded participation. FitBit data and baseline survey data were used for the present analysis.
Measures
Relationship quality.
Relationship quality was measured at baseline using the 7-item Relationship Assessment Scale (Hendrick, 1988; e.g., “How well does your partner meet your needs?” “In general, how satisfied are you with your relationship?”). Response options ranged from 1 to 5, with higher scores indicating greater relationship satisfaction. Internal consistency reliability was high (Cronbach’s α = 0.91).
Relationship quality was also measured in terms of closeness using a 3-item measure (Denes, 2015; e.g., “How emotionally connected do you feel to your partner?” “How close do you feel to your partner?”). Response options ranged from 1 to 5, with higher scores indicating greater closeness. Internal consistency reliability was high (Cronbach’s α = 0.85).
Physical activity.
Objectively measured physical activity data was obtained from Fitabase. For each social day (3am-3am), we calculated minutes of light, moderate, and vigorous physical activity, as well as sedentary time total steps. Data were censored for nonwear (defined as either minutes with zero activity count and no data on heart rate, or as more than 120 consecutive minutes with zero activity counts), and sleep times (extracted from Fitabase) were excluded from daily total calculations. Only days with at least 10 hours of wear time were included in the analysis (Burg et al., 2017). FitBit is a reliable and valid method for tracking physical activity (Diaz et al., 2015).
Demographics.
Self-reported demographic data included age, race/ethnicity, relationship status, relationship length, biological sex, gender, and sexual orientation.
Time variables.
Dummy codes were created to indicate the beginning of lockdown (i.e., when strict stay-home orders and social distancing policies were implemented; March 22, 2020 in NYC, March 20, 2020 in Chicago, and March 24, 2020 in Boston), and a count variable was created to indicate days since lockdown. Two variables were created to account for seasonal variations in physical activity, sine and cosine of the observation day, which together fit a 365-day sinusoidal curve to the pattern of physical activity (Ma et al., 2006). This technique (i.e., including sine and cosine) account for the intercept, phase, and amplitude of seasonal variations in physical activity, and was included because season is associated with both the primary predictor (date of lockdown) and the outcomes of interest. An indicator was also created for weekend v. weekday (Saturday and Sunday = 1).
Data Analysis Strategy
Data were nested within individuals over time, necessitating a multilevel framework to account for repeated measures. To account for similarity within the four couples where both partners linked a FitBit, a series of four dummy codes were created treating individuals [= 0] as the reference category with an indicator [= 1] for each of the couples. Multilevel models were estimated using PROC MIXED procedure in SAS v. 9.4. Histograms and preliminary analyses regressing the interquartile range of within-person activity on the median for within-person activity suggested no transformation was needed for total steps, sedentary minutes, or light physical activity, but that a square root transformation was appropriate for minutes of moderate and vigorous physical activity in order to promote homoscedasticity and reduce skewness for parametric testing (Emerson, 1983).
For steps, sedentary time, and light physical activity, random effects included a person-specific intercept, sine and cosine for seasonal variation, and the dummy code indicating the start of lockdown. A spatial power error structure with a local subcommand was specified. In practice, this error structure separates the residual into two components. The first component comprises error that is predictable within-person, such that exhibits serial autocorrelation over time, with higher correlations between observation days that are closer together in time (e.g., higher correlations between observations of steps or minutes that are 1 day v. 1 month apart). The other component is random error that remains uncorrelated within-person over time (i.e., it is not predictable; Schwartz & Stone, 2007). Due to collinearity between wear time and sedentary time (r = 0.85), we included hours of wear time and hours squared as fixed effects, and hours squared as a random effect. After detecting near-perfect or perfect correlations between seasonal variables and lockdown effects, we adjusted this for moderate and vigorous physical activity. In these models, random effects included a person-specific intercept and the dummy code indicating the start of lockdown (i.e., the pair of seasonality variables were removed from the equation), and the local command was removed from the repeated statement.
For each day-level outcome (steps, and minutes of sedentary, light, moderate, and vigorous physical activity), four models were tested. The first model included the indicator for couples, the indicator for weekend day, and sine and cosine as covariates. The primary predictor was lockdown date, and days since lockdown and the quadratic term for days since lockdown were also included to account for potential recovery to baseline activity over time as participants adjusted to stay-home orders and social distancing policies. The second and third model tested the multiplicative interactions of relationship satisfaction and closeness with the lockdown indicator. A final model included demographic covariates: age, sex, and race/ethnicity.
Data Sharing Statement
All materials necessary to replicate primary analyses are hosted on the SAGE Journals Figshare repository. Files include deidentified data, a data dictionary, SAS syntax, and complete SAS output.
Results
Participants were a mean of 34.43 years old (SD = 10.44; Range 24.00, 67.00) and had been in their present relationship for a mean of 7.74 years (SD = 8.77; Range 1.00, 46.00). Most were from NYC (21, 75.00%), followed by Chicago (6, 21.43%) and Boston (1, 3.57%). Only one participant reported having had COVID-19 (3.57%). Most were heterosexual (22, 78.57%) and reported both female sex and female gender (20, 71.43%). Most were White (21, 75.00%), two were Black (7.14%), and three were Hispanic (10.71%). More than half of the couples were married (18, 64.29%), and relationship satisfaction and closeness were high (Mean = 4.41, SD = 0.63; and Mean = 4.35, SD = 0.65, respectively).
Participants provided a median of 191 valid observation days (Mean = 170.39, SD = 72.42, Range 13.00, 243.00). Observations were spread consistently across months. The lowest number of observations were in February (4.22%) and October (7.36%), which is expected given that these months only had partial data collection. The remaining months (March – September) had a relatively even 11.30% – 14.38% of observations. At the minute-level, 31.88% of observations were removed due to nonwear during waking hours; at the person-level, the mean number of observations removed was 31.62% (SD = 28.76%; Range 0.18%, 91.33%). Separate spaghetti plots for each individual’s steps and physical activity over time are shown in Electronic Supplementary Figures 1–5, and unadjusted model results are available in Table 1.
Table 1.
Unadjusted model results.
| Stepsa | Sedentary Minutes | Light Physical Activity | Moderate Physical Activityb | Vigorous Physical Activityb | |
|---|---|---|---|---|---|
|
| |||||
| Fixed Effects c | |||||
|
|
|||||
| B (se) | B (se) | B (se) | B (se) | B (se) | |
|
| |||||
| Intercept | 49.14 (11.52)** | 724.91 (22.36)** | 186.93 (22.40)** | 2.07 (0.61)** | 2.68 (0.78)** |
| Weekend (v. Weekday) | 6.50 (1.16)** | −16.62 (2.17)** | 798 (1.76)** | 0.12 (0.07) | 0.06 (0.09) |
| sin(X) | −27.82 (12.28)* | 27.16 (22.55) | −35.93 *21.93) | −0.69 (0.66) | −0.01 (0.79) |
| cos(X) | 21.04 (8.06)* | −10.69 (14.64) | 1.23 (14.19) | 0.89 (0.42)* | 1.02 (0.50)* |
| Lockdown | −15.96 (6.30)* | 33.75 (9.94)** | −25.01 (9.11)* | −0.72 (0.29)* | −0.17 (0.38) |
| Days Since Lockdown | 1.15 (0.35)** | −1.13 (0.64) | 1.04 (0.63) | 0.05 (0.02)** | 0.04 (0.02) |
| Days Since Lockdown*unDays Since Lockdown | −0.00 (0.00)** | 0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00)* | −0.00 (0.00) |
|
| |||||
| Random Effects d | |||||
|
|
|||||
| Estimate (se) | Estimate (se) | Estimate (se) | Estimate (se) | Estimate (se) | |
|
| |||||
| Intercept Variance | 983.90 (312.38)** | 4,577.52 (1,466.02)** | 4,963.79 (1,679.12)** | 2.14 (0.68)** | 4.83 (1.44)** |
| Lockdown Variance | 527.27 (211.85)** | 895.41 (498.44)* | 717.95 (430.90)* | 0.70 (0.30)* | 1.66 (0.60)** |
| Intercept and lockdown correlation | 0.01 (0.27)** | −0.35 (0.28) | −0.81 (0.17)** | −0.32 (0.23) | −0.41 (0.19)* |
p < .05
p < .01
Divided by 100
Square root transformed
Fixed effects for couples not shown; For sedentary minutes, fixed effects for hours of wear time not shown.
Only intercept variance, lockdown variance, and their correlation are shown for brevity
Steps.
In the first model, the effect of “lockdown” was significant, suggesting that implementing stay-home orders and social distancing policies significantly reduced daily step counts by about 1,600 steps, B = −1,595.72, 95% CI −2,892.84, −298.59 p = .018. There was a significant recovery over time of approximately 100 steps each day, B = 114.82, 95% CI 47.02, 182.62, p < .001, though this attenuated with time, B = −0.45, 95% CI −0.74, −0.15, p = .003. The predicted temporal pattern of steps for the “average participant” is portrayed in Figure 1, random intercept and slope coefficients are in Electronic Supplementary Figure 6, and conditional residual plots for this model are provided in Electronic Supplementary Figure 7.
Figure 1.
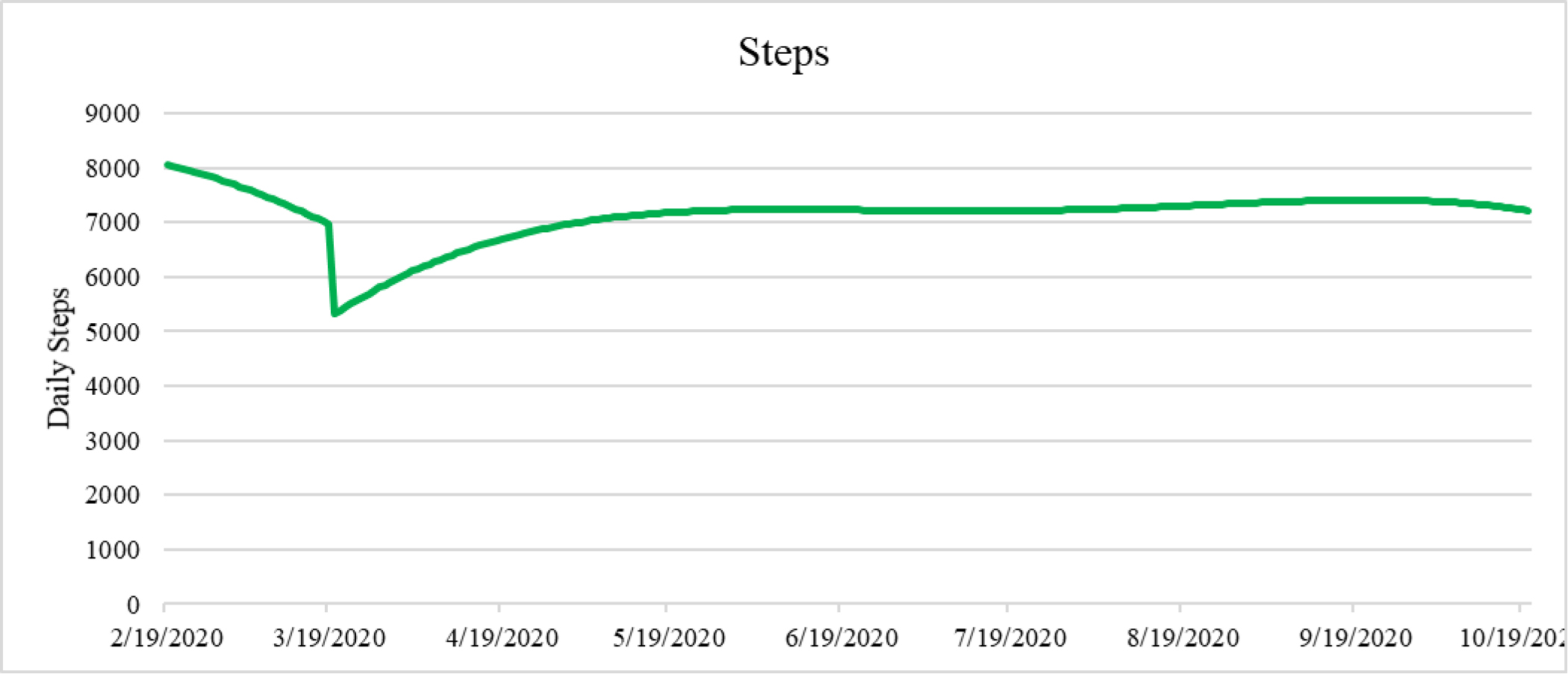
Model-predicted daily steps.
There was significant variability in the effect of lockdown on daily steps. However, neither closeness to partner nor relationship satisfaction explained this variability (i.e., the interactions of these variables with the indicator for lockdown were not significant, p = .89 and .95, respectively).
Sedentary time.
In the first model, the effect of “lockdown” was significant, suggesting slightly more than a 30-minute increase per day in sedentary time, B = 33.75, 95% CI 13.28, 54.22, p = .002. There was no significant effect of days since lockdown, p = .077; neither was the quadratic term significant, p = .106. In a joint test of these effects, conclusions were unaltered, χ2(2) = 3.4, p = .19. The predicted temporal pattern of sedentary time for the “average participant” is portrayed in Figure 2, random intercept and slope coefficients are in Electronic Supplementary Figure 8, and conditional residual plots for this model are provided in Electronic Supplementary Figure 9.
Figure 2.
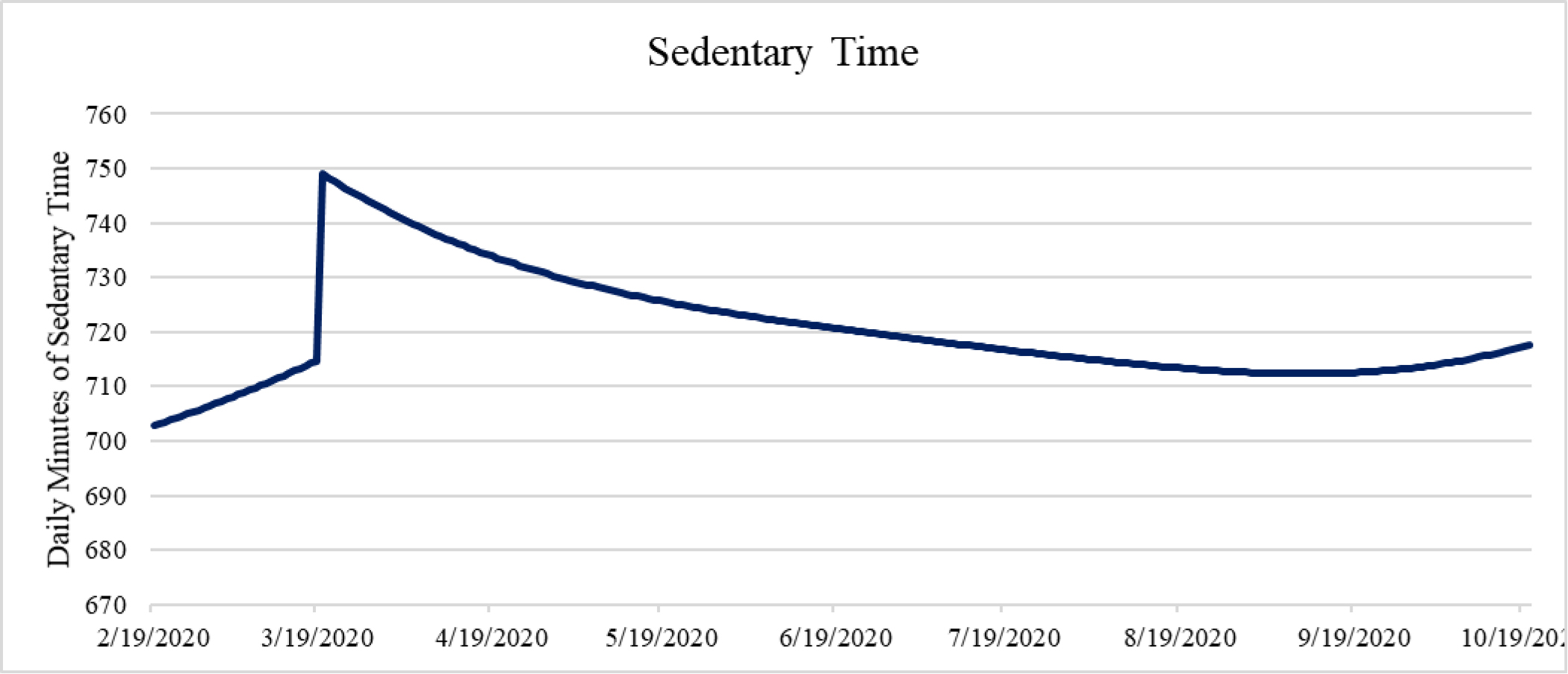
Model-predicted daily minutes of sedentary time.
There was significant variability in the effect of lockdown on daily steps. However, neither closeness to partner nor relationship satisfaction explained this variability (i.e., the interaction of these variables with the indicator for lockdown was not significant, p = .39 and .77, respectively). Including demographic covariates did not alter conclusions.
Light physical activity.
In the first model, the effect of “lockdown” was significant, suggesting a decrease of about 25 minutes per day in light physical activity, B = −25.01, 95% CI −43.77, −6.26, p = .011. There was no significant effect of days since lockdown, p = .097; nor was the quadratic term significant, p = .083. In a joint test of these effects, conclusions were unaltered, χ2(2) = 3.0, p = .22. The predicted temporal pattern of light physical activity for the “average participant” is portrayed in Figure 3, random intercept and slope coefficients are in Electronic Supplementary Figure 10, and conditional residual plots for this model are provided in Electronic Supplementary Figure 11.
Figure 3.
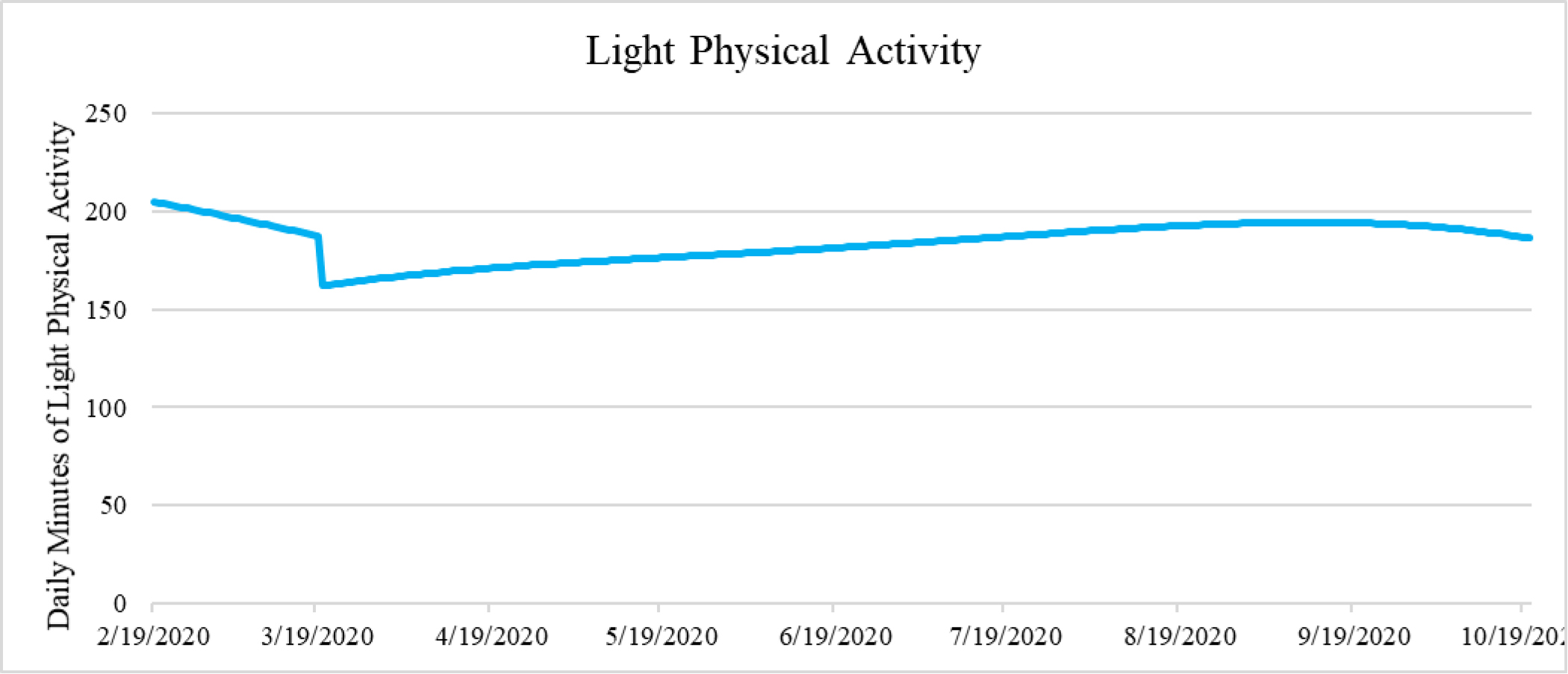
Model-predicted daily minutes of light physical activity.
Although there was significant variability in the effect of lockdown on daily minutes of light physical activity, neither closeness to partner nor relationship satisfaction explained this variability, p = .18 and .29, respectively. Including demographic covariates did not alter conclusions.
Moderate physical activity.
In the first model, the effect of “lockdown” was significant, B = −0.72, 95% CI −1.32, −0.12, p = .021 (a decrease of approximately 3.5 minutes). There was a significant effect of days since lockdown, B = 0.05, 95% CI 0.02, 0.09, p = .005. The quadratic term was significant, suggesting that this recovery attenuated with time, B = −0.00, 95% CI −0.00, −0.00, p = .016. The predicted temporal pattern of moderate physical activity for the “average participant” is portrayed in Figure 4, random intercept and slope coefficients are in Electronic Supplementary Figure 12, and conditional residual plots for this model are provided in Electronic Supplementary Figure 13.
Figure 4.
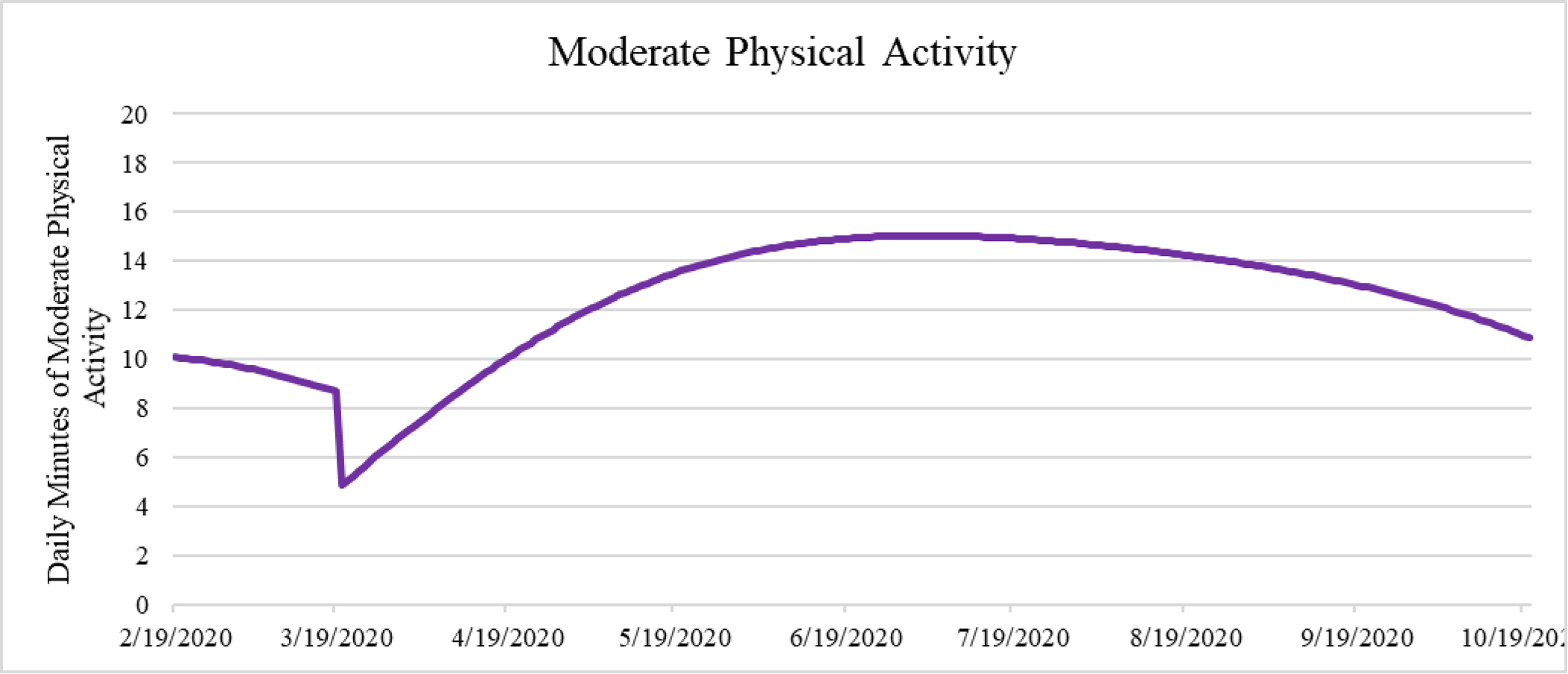
Model-predicted daily minutes of moderate physical activity.
There was significant variability in the effect of lockdown on daily minutes of moderate physical activity. However, neither closeness to partner nor relationship satisfaction explained this variability, p = .64 and .46, respectively. Including demographic covariates did not alter conclusions.
Vigorous physical activity.
In the first model, the effect of “lockdown” on the square root of minutes of vigorous physical activity was not significant, B = −0.17, 95% CI −0.96, 0.62, p = .45. There was no significant effect of days since lockdown, p = .095; nor was the quadratic term significant, p = .16. In a joint test of these effects, conclusions were unaltered, χ2(2) = 4.1, p = .13. The predicted temporal pattern of vigorous physical activity for the “average participant” is portrayed in Figure 5, random intercept and slope coefficients are in Electronic Supplementary Figure 14, and conditional residual plots for this model are provided in Electronic Supplementary Figure 15.
Figure 5.
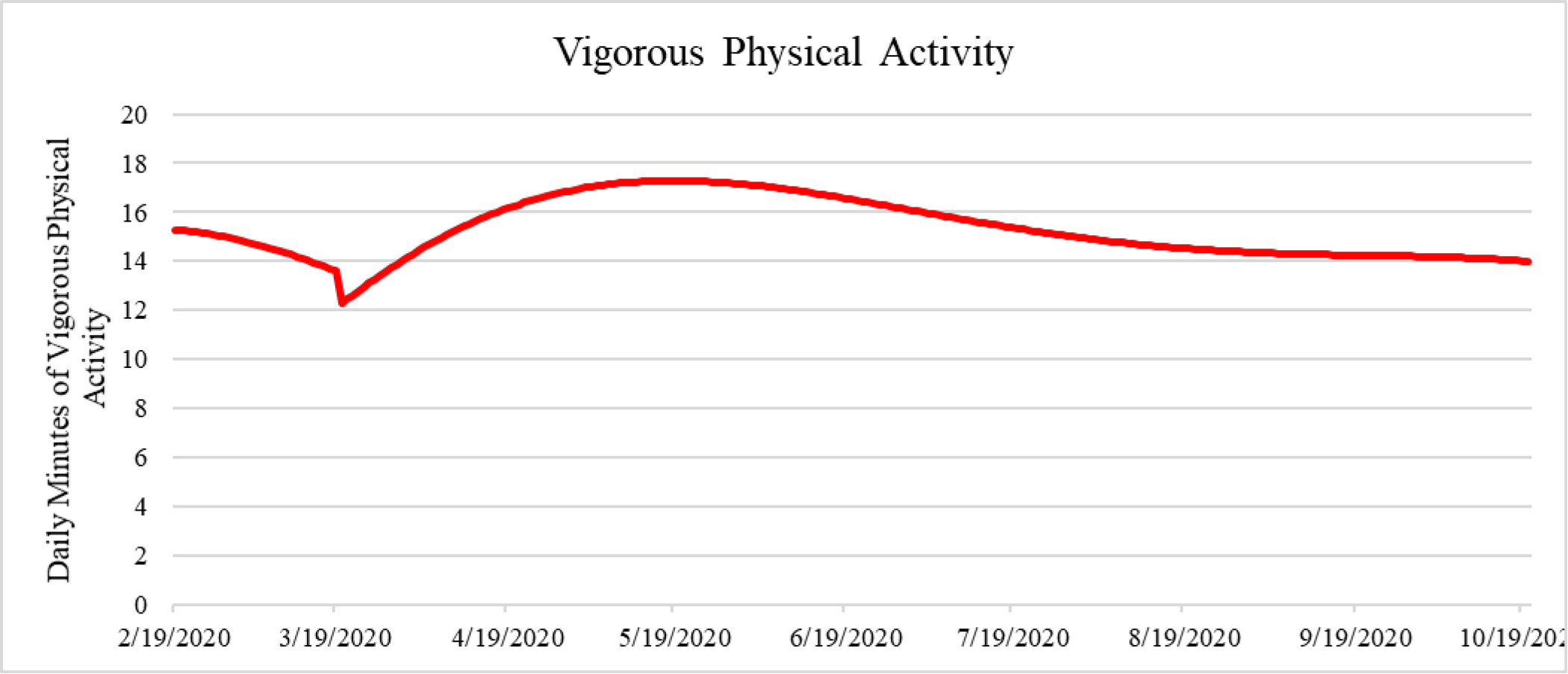
Model-predicted daily minutes of vigorous physical activity.
There was significant variability in the effect of lockdown on daily minutes of light physical activity. However, neither closeness to partner nor relationship satisfaction explained this variability, p = .59 and .48, respectively. Including demographic covariates did not alter conclusions.
Discussion
In a sample of 28 individuals living in three major metropolitan areas in the United States during the peak of the COVID-19 pandemic, the present study found significant decreases in objectively measured steps and minutes of light and moderate physical activity, and an increase in sedentary time, immediately following the implementation of stay-home orders and social distancing policies. Decreases in step and moderate physical activity recovered over time. There was no change in vigorous physical activity from pre- to post-policy implementation, and, counter to study hypotheses, neither relationship closeness nor relationship satisfaction buffered against decreases in activity.
Implementation of policies to stem the spread of COVID-19 resulted in significantly lower objective measures of daily step counts and minutes of light and moderate physical activity and increased sedentary time. This aligns with research showing a decline in steps (Pépin et al., 2020) and in self-reported moderate and vigorous physical activity during this same time (Rhodes et al., 2020; Yang & Koenigstorfer, 2020), as well as increases in self-reported sedentary time (Gallè et al., 2020). Differences between the present study and prior literature may be due to differences in assessment (i.e., objectively measured v. self-reported activity), but may also be due to differences in the sample. For example, apps that promote physical activity buffered against declines in activity (Yang & Koenigstorfer, 2020) as did home equipment and formulating exercise plans (Rhodes et al., 2020). The present sample comprised active FitBit users only. It may be that individuals who use activity trackers are less likely to forego exercise during stressful times, or may even increase activity as a coping mechanism (Faulkner et al., 2020; this may be why we did not find any significant decline in vigorous physical activity – ostensibly a purposeful exercise session). Also, these individuals may not have lost the same reflexive cues to exercise (Dunton et al., 2019): a FitBit is worn constantly, even if a gym closes, for example.
Having a highly satisfying or close relationship did not buffer declines in physical activity. It may be that people who are more likely to have a satisfying relationship are also more likely to engage in positive health behaviors, such as physical activity. This lack of moderation could also be due to range restriction, such that all participants were able to glean stress-buffering benefits from their romantic relationship (Cohen & Wills, 1985). Indeed, most couples were quite close and satisfied, with the lowest reported values still exceeding the midpoint of the scale. Given that stressors associated with the pandemic have presented a challenge to many relationships, those people remaining satisfied with their romantic partner during the implementation of stay-home-orders could be particularly resilient (Balzarini et al., 2020; Günther-Bel et al., 2020; Williamson, 2020). This is not surprising and represents a challenge in couples-based research more broadly, whereby satisfied couples are more likely to enroll in a study together. Another possibility is that declines in physical activity were not due to stressors, which have the potential to be buffered, but to sudden environmental changes (e.g., inability to access gyms, disruption of normal exercise routines). That being said, problem-solving directed towards overcoming these disruptions together with a close partner could still help to reduce adverse impacts by, for example, providing support for effortful engagement (rather than relying on reflexive cues; Dunton et al., 2019) or by more quickly identifying an alternative (e.g., running by the river instead of on a treadmill at the gym, buying at-home videos instead of going to an exercise class).
This study has numerous strengths, most importantly 8 months of objectively measured continuous physical activity data using a validated accelerometer (Diaz et al., 2015). However, there are also several limitations. The sample size is small, limiting power to detect significant moderation effects. Range restriction (i.e., a sample of highly close and satisfied couples) could also undermine our ability to detect such effects. The sample was self-selected (satisfied couples) and highly active, which could limit generalizability. It is likely that consistent FitBit users may be more active or less likely to stop exercising due to stay-home orders because they have a greater focus on maintaining fitness. Results may not generalize to individuals living outside of metropolitan areas, where the effect of lockdown may have had less of an impact (e.g., due to greater outdoor access) or areas with more temperate winter climates. Similarly, there may have been differences in the impact of lockdown on physical activity in different cities due to differences in enforcement or culture, but we were underpowered to test such effects. However, NYC, Boston, and Chicago were selected due to similarities in the timing of shelter-in-place mandates, urban environments, and weather patterns, so differences between cities were not anticipated. Finally, closeness and satisfaction assessments occurred mid-pandemic (and in the middle of FitBit data collection), and so it is hard to establish temporal associations.
Conclusions
This study found a short-term decrease in objectively assessed steps, light physical activity, and moderate physical activity, as well as an increase in sedentary time, following implementation of “stay-home” orders in three metropolitan areas in the United States. However, these decreases in steps and moderate physical activity recovered relatively quickly, and there was no decrease in vigorous physical activity. This suggests that individuals are resilient in adapting their physical activity routines to the confines of “lockdown.” To inform future efforts at intervention development, future studies should recruit couples with a broader range of relationship satisfaction, should include individuals who do not already own physical activity trackers, and should consider alternative forms of social connection (e.g., FaceTime, virtual workouts with friends) that may buffer unintended health consequences of policies designed to mitigate the spread of COVID-19.
Supplementary Material
Funding:
This study was supported by InCHIP (Rapid Response Proposals to Address COVID-19; co-PIs: Cornelius, Denes). Dr. Cornelius receives support from NIH/NCATS (KL2 TR001874). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH.
Footnotes
Conflict of interest: Dr. Gorin is the director of the Institute for Collaboration on Health, Intervention, and Policy (InCHIP). There are no other potential conflicts of interest.
References
- Afifi TD, Merrill AF, & Davis S (2016). The theory of resilience and relational load. Personal Relationships, 23(4), 63–683. doi: 10.1111/pere.12159 [DOI] [Google Scholar]
- Aral S & Nicolaides C (2017). Exercise contagion in a global social network. Nature Communications, 8(1), 1–8. doi: 10.1038/ncomms14753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balzarini RN, Muise A, Zoppolat G, Di Bartolomeo A, Rodrigues DL, Alonso-Ferres M, Urganci B, Debrot A, Bock Pichayayothin N, Dharma C, Chi P, Karremans J, Schoebi D, & Slatcher RB (2020). Love in the time of COVID: perceived partner responsiveness buffers people from lower relationship quality associated with COVID-related stressors. PsyArXiv. doi: 10.31234/osf.io/e3fh4 [DOI] [Google Scholar]
- Burg MM, Schwartz JE, Kronish IM, Diaz KM, Alcantara C, Duer-Hefele J, & Davidson KW (2017). Does stress result in you exercising less? Or does exercising result in you being less stressed? Or is it both? Testing the bi-directional stress-exercise association at the group and person (N of 1) level. Annals of Behavioral Medicine, 51(6), 799–809. doi: 10.1007/s12160-017-9902-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopik WJ & O’Brien E (2017). Happy you, healthy me? Having a happy partner is independently associated with better health in oneself. Health Psychology, 36(1), 21–30. doi: 10.1037/hea0000432 [DOI] [PubMed] [Google Scholar]
- Cohen S & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. doi: 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- Courtin E & Knapp M (2017). Social isolation, loneliness and health in old age: a scoping review. Health & Social Care in the Community, 25(3), 799–812. doi: 10.1111/hsc.12311 [DOI] [PubMed] [Google Scholar]
- Darlow SD & Xu X (2011). The influence of close others’ exercise habits and perceived social support on exercise. Psychology of Sport and Exercise, 12(5), 575–578. doi: 10.1016/j.psychsport.2011.04.004 [DOI] [Google Scholar]
- Denes A (2015). Genetic and individual influences on predictors of disclosure: Exploring variation in the oxytocin receptor gene and attachment security. Communication Monograph, 82(1), 113–133. doi: 10.1080/03637751.2014.993544 [DOI] [Google Scholar]
- Diaz KM, Krupka DJ, Chang MJ, Peacock J, Ma Y, Goldsmith J, Schwartz JE, & Davidson KW (2015). Fitbit®: An accurate and reliable device for wireless physical activity tracking. International Journal of Cardiology, 185, 138–140. doi: 10.1016/j.ijcard.2015.03.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR (2004) Social support and patient adherence to medical treatment: a meta-analysis. Health Psychology, 23(2), 207–218. doi: 10.1037/0278-6133.23.2.207 [DOI] [PubMed] [Google Scholar]
- Dunton GF, Rothman AJ, Leventhal AM, & Intille SS (2019). How intensive longitudinal data can stimulate advances in health behavior maintenance theories and interventions. Translational Behavioral Medicine, 11, 281–286. doi: 10.1093/tbm/ibz165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson JD (1983). Mathematical Aspects of Transformation. In Hoaglin DC, Mosteller F, & Tukey JW (Eds.). Understanding robust and exploratory data analysis, Vol. 3 (p. 247–282). John Wiley & Sons. [Google Scholar]
- Faulkner G, Rhodes RE, Vanderloo LM, Chulak-Bozer T, O’Reilly N, Ferguson L, & Spence JC (2020). Physical activity as a coping strategy for mental health due to the COVID-19 virus: a potential disconnect among Canadian adults?. Frontiers in Communication, 5, 74. doi: 10.3389/fcomm.2020.571833 [DOI] [Google Scholar]
- Gallè F, Sabella EA, Ferracuti S, De Giglio O, Caggiano G, Protano C, Valeriani F, Parisi EA, Valerio G, & Liguori G (2020). Sedentary behaviors and physical activity of Italian undergraduate students during lockdown at the time of CoViD−19 pandemic. International Journal of Environmental Research and Public Health, 17(17), 6171. doi: 10.3390/ijerph17176171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb BH & Bergen AE (2010). Social support concepts and measures. Journal of Psychosomatic Research, 69(5):511–20. doi: 10.1016/j.jpsychores.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Günther-Bel C, Vilaregut A, Carratala E, Torras-Garat S, & Pérez-Testor C (2020). A mixed-method study of individual, couple, and parental functioning during the state-regulated COVID-19 lockdown in Spain. Family Process, 59(3), 1060–1079. doi: 10.1111/famp.12585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrick SS (1988). A generic measure of relationship satisfaction. Journal of Marriage and the Family, 50(1), 93–98. doi: 10.2307/352430 [DOI] [Google Scholar]
- House JS, Landis KR, & Umberson D (1988). Social relationships and health. Science, 241(4865), 540–545. doi: 10.1126/science.3399889 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK & Wilson SJ (2017). Lovesick: How couples’ relationships influence health. Annual Review of Clinical Psychology, 13, 421–443. doi: 10.1146/annurev-clinpsy-032816-045111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landers DM & Arent SM (2007). Physical activity and mental health. In Tenenbaum G & Eklund RC (Eds.), Handbook of sport psychology (p. 469–491). John Wiley & Sons, Inc. [Google Scholar]
- Loving TJ & Slatcher RB (2013). Romantic relationships and health. In Simpson JA & Campbell L (Eds.). Oxford library of psychology. The Oxford handbook of close relationships (p. 617–637). Oxford University Press. [Google Scholar]
- Ma Y, Olendzki BC, Li W, Hafner AR, Chiriboga D, Hebert JR, Campbell M, Sarnie M, & Ockene IS (2006). Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population. European Journal of Clinical Nutrition, 60(4), 519–528. doi: 10.1038/sj.ejcn.1602346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pépin JL, Bruno RM, Yang RY, Vercamer V, Jouhaud P, Escourrou P, & Boutouyrie P (2020). Wearable activity trackers for monitoring adherence to home confinement during the COVID-19 pandemic worldwide: data aggregation and analysis. Journal of Medical Internet Research, 22(6), e19787. doi: 10.2196/19787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes RE, Liu S, Lithopoulos A, Zhang CQ, & Garcia-Barrera MA (2020). Correlates of perceived physical activity transitions during the COVID-19 pandemic among canadian adults. Applied Psychology: Health and Well-Being, 12(4), 1157–1182. doi: 10.1111/aphw.12236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, & McGinn MM (2014). Marital quality and health: a meta-analytic review. Psychological Bulletin, 140(1), 140–187. doi: 10.1037/a0031859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz JE & Stone AA (2007). The analysis of real-time momentary data: a practical guide. The science of real-time data capture: self-reports in health research (p. 76–113). Oxford University Press. [Google Scholar]
- Williamson HC (2020). Early effects of the COVID-19 pandemic on relationship satisfaction and attributions. Psychological Science, 31(12), 1479–1487. doi: 10.1177/0956797620972688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y & Koenigstorfer J (2020). Determinants of physical activity maintenance during the Covid-19 pandemic: a focus on fitness apps. Translational Behavioral Medicine, 10(4), 835–842. doi: 10.1093/tbm/ibaa086 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


