Abstract
Background
The COVID-19 pandemic has heavily impacted social, economic and health systems worldwide. Necessary confinement measures have, in turn, contributed to the occurrence of several stress-related conditions and deterioration of pre-existing mental conditions, including insomnia.
Objective
The present study sought to investigate the occurrence and severity of insomnia during the COVID-19 lockdown among psychiatric patients and in the general population in the largest Italian sample examined to date. Potential factors associated with a risk of developing insomnia in the global sample were examined as well.
Methods
A sample of 20,720 people (5.5% of them being psychiatric patients) was assessed through an online survey conducted during lockdown between March and May 2020. To investigate the occurrence and severity of sleep related issues, the Insomnia Severity Index (ISI) was used. In order to evaluate factors associated with the severity of insomnia in the global sample, multivariate linear regression models were performed.
Results
During the lockdown, patients with pre-existing mental disorders reported a mean higher score on the ISI scale (p < 0.001) compared to the general population. According to the multivariate regression models, the first three weeks of lockdown were significantly associated with a higher risk of insomnia, but the risk disappeared in the fourth week. Other associated factors included: the presence of a pre-existing mental disorder, ages 24 to 64 years old, and/or being female (p < 0.001).
Conclusions
Although containment measures represent essential public health strategies to avoid the spread of the COVID-19 pandemic, sleep was one of the aspects affected during the early stages of the lockdown in both people with pre-existing mental disorders and general population. As an integral part of COVID-19 intervention, it is useful to raise awareness about these issues and to adopt both preventive and therapeutic interventions.
Keywords: COVID-19 pandemic, SARS-Cov-2, Sleep disorders, Lockdown, Psychiatric patients
1. Introduction
The COVID-19 pandemic has heavily influenced social, economic and health systems worldwide [1]. Due to the limited availability of specialised therapies and the high diffusion of the disease, affected countries have issued a variety of containment strategies that have radically changed people's lifestyle. Several studies showed the occurrence of high rates of anxiety, panic, stress and insomnia both among the COVID-19 affected individuals and within the general population [[2], [3], [4]].
Insomnia and sleep apnea are among the most common sleep disorders [5]. Previous investigation has examined the perception of sleep quality: in a prior study, between 10% and 18.1% of the population reported to be poor sleepers or insomniacs [6], while another study reported that a clinically valid diagnosis was available for only 6–15% of the sample [7]. Indeed, the association between mental disorders and insomnia is well-established: epidemiologic studies have shown that between 30 and 60% of people with mental disorders also reported insomnia. Furthermore, the persistence of insomnia was associated with a higher risk of developing a mental disorder. [[8], [9], [10]]
Among the various psychopathological aspects, sleep disorders and insomnia represent one of the main issues that emerged in the population that was exposed to COVID-19 pandemic and to the containment measures [[11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22]]. In fact, these measures have changed daily routines, with a potential impact on sleep patterns. The prevalence of sleep problems among the general population appeared to be larger than what had been reported in previous studies, with 35% reporting a sleep disorder, with higher rates in patients affected by COVID-19 (74.8%) compared to health workers and the general population (respectively, 36% and 32.3%) [23]. Another survey showed that COVID-19 lockdown was associated with poor sleep quality, shift in sleep cycle to delayed phase, sleep-deprivation, and depressive symptoms [24]. Another systematic review showed relatively high rates of insomnia, anxiety, depression, posttraumatic stress disorder and psychological distress symptoms within the population affected by COVID-19 in multiple countries [25]. In particular, subjects with pre-existing mental health disorders seemed to be more affected by the consequences of lockdown. Indeed, they reported significatively higher levels of clinical insomnia and change in sleep patterns compared to healthy controls [26,27]. However, a recent study suggests that there is no uniform effect of the lockdown on sleep. For instance, even though the majority of subjects in the general population showed worsened sleep patterns, a subset of individuals with pre-pandemic insomnia symptoms reported a subsequent meaningful improvement in sleep quality [28].
In Europe, Italy has been the first country severely hit by the pandemic, which led the adoption of a national lockdown (known as “Phase 1” of the sanitary emergency). This measure lasted 8 weeks, from March 8 to May 3, 2020, involving about 60 millions of people. During this period, 100,000 people have been quarantined, and >29,000 people have died from COVID-19. Only essential activities were allowed, and individuals were permitted to leave their houses only for necessities. In this dramatic scenario, several factors impacted the mental health of patients with pre-existing mental disorders, including delays in supplying psychotropic medications, difficulties in accessing primary care and outpatient clinics, fear of contracting COVID-19, and social isolation [26]. Even though several studies have evaluated the impact of pandemic and its related containment measures on subjects with pre-existing mental disorders [29], only a few studies analysed changes in sleep patterns and quality among patients with pre-existing mental disorders. A study investigating the prevalence of sleep disturbances in clinically stable older psychiatric patients (≥50 years), during the COVID-19 outbreak in China, found that over half of the participants suffered from sleep disturbances, which represented a higher prevalence compared to was the general population. [30] Another Chinese report showed that, during the peak of the COVID-19 epidemic with strict lockdown measures, psychiatric patients suffered from moderate to severe levels of insomnia. [26].
The COMET collaborative network study was one of the first to evaluate the impact of lockdown on the Italian general population as well as on patients with pre-existing mental disorders. The aims of the present study were: 1) to assess the prevalence of insomnia and sleep disorders during the different weeks of lockdown; 2) to identify prevalence and related factors of insomnia in a large sample of the Italian population, including psychiatric patients.
2. Materials and methods
The COMET trial consisted of an online survey carried out between March and May 2020 in the Italian adult population. The online survey was set up through EUSurvey, a web platform promoted by the European Commission (2013). The survey was officially launched on March 30, 2020, taking approximately 30 min (range 15–45 min) to be completed.
The survey was disseminated by email invitation sent to health professionals and their patients; shared link on social media channels (Facebook, Twitter, Instagram) and on mailing lists of national psychiatric associations; involvement of national associations of stakeholders (e.g., associations of users/carers); official communication channels (e.g., university and hospital websites).
The survey addressed the Italian population aged over 18. The snowball sampling procedure - without defining strict inclusion/exclusion criteria (except age) – was used to recruit a large sample of the Italian population and to evaluate the effect of the studied variables on the outcome measures. Further details about the representativeness of the sample have been provided elsewhere [31].
The full study protocol has been described elsewhere [31], as the results of the primary outcomes [17]. The study has been approved by the Ethical Review Board of the University of Campania “L. Vanvitelli” (protocol number: 0007593/i).
For the purposes of the present paper, specifically focused on insomnia, the global sample was subdivided in two groups: patients with pre-existing mental disorders and people from the general population.
2.1. Assessment tools
Respondents' socio-demographic (e.g., gender, age, working and housing condition, etc.) and clinical variables (e.g., having a previous physical or mental disorder, use of illicit drugs or medications, etc.) were collected through a dedicated questionnaire.
The primary outcome was the Insomnia Severity Index (ISI). The ISI includes seven items assessing the characteristics and the severity of insomnia (i.e., sleep onset, sleep maintenance, and early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by the sleep difficulties) and its impact on daily functioning. Each item is rated on a 5-level Likert scale. The total score ranges from 0 to 28 [32].
As reported elsewhere [17,31], other assessment instruments included the Depression, Anxiety, Stress Scale (DASS-21) and the General Health Questionnaire (GHQ).
The DASS-21 evaluates the general distress [33] and is a reliable and valid tool assessing mental health in the general population [34]. The DASS consists of 21 items grouped in three subscales: depression, anxiety, and stress. Each item is rated on a 4-level Likert scale, from 0 (never) to 3 (almost always). The total score is calculated by adding the response values of each item, with higher scores indicating more severe levels of depressive, anxiety, and stress symptoms. The score at the DASS-depression subscale is divided into normal (0–9), mild (10−12), moderate (13−20), severe (21–27), and extremely severe depression (28–42). The score at the DASS-anxiety subscale is divided into normal (0–6), mild (7–9), moderate (10–14), severe (15–19), and extremely severe anxiety (20–42). The score at the DASS-stress subscale is divided into normal (0−10), mild (11–18), moderate (19–26), severe (27–34), and extremely severe stress (35–42).
The General Health Questionnaire (GHQ)-12 items version explores participants' mental health status through six positively worded items (e.g., “Have you been able to concentrate”?) and six negatively worded items (e.g., “Have you lost much sleep over worry?”). Threshold ≥4 at GHQ identifies people with a probability >80% of having a mental health problem [35].”
Other validated and reliable questionnaires were used in the study: the Obsessive-Compulsive Inventory-Revised version (OCI-R) [36], the Suicidal Ideation Attributes Scale (SIDAS) [37], the Severity-of-Acute-Stress-Symptoms-Adult scale (SASS) [38], the Impact of Event Scale-short version (IES) [39], the Connor-Davidson resilience scale [40], the brief-COPE [41], the short form of Post-Traumatic Growth Inventory (PTGI) [42], the Multidimensional Scale of Perceived Social Support (MSPPS) [43], and (only for healthcare professionals) the Maslach Burnout Inventory (MBI). [44]
Evaluating different psychopathological dimensions through specific scales, as described in the previous research [17], gave us the opportunity to better define the potential influence of those dimensions in the development of insomnia after exposure to lockdown.
2.2. Statistical analysis
Descriptive statistics were performed in order to describe the socio-demographic and clinical characteristics of the global sample and as well as any difference between patients with pre-existing mental disorders and the remaining sample.
In order to evaluate factors associated with the severity of insomnia in the global sample, a multivariate linear regression model has been implemented, using the total score at the ISI scale as main outcome measure and also including as independent variables: being infected by COVID-19, having a pre-existing mental disorder, and being a healthcare professional.
We used a propensity score in order to adjust for the likelihood of participants of being exposed to COVID infection in each week [45]. This methodological choice has been adopted considering that the propensity score produces a better adjustment for differences at baseline, rather than simply including potential confounders in the multivariable models. The propensity score was calculated using as independent variables age, gender, socioeconomic status and living in a severely impacted area [46].
Furthermore, in order to evaluate the impact of the lockdown duration and other related containment measures on the primary outcomes, the categorical variable “week” was also included in the regression models. The models were adjusted for the rate of new COVID cases and COVID-related mortality during the study period, as well as for several socio-demographic characteristics, such as gender, age, occupational status, having a physical comorbid condition, hours spent on the Internet, levels of perceived loneliness, health status, number of cohabiting people, level of satisfaction with one's own life, with cohabiting people, and with the housing condition. Missing data were handled using the multiple imputation approach [47], although the rate of missing data was <1%. For outcome variable considered in the present paper (i.e., ISI scale) the rate was <0.1%. All other variables were managed as previously reported [17].
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS), version 26.0 and STATA, version 15. For all analyses, the level of statistical significance was set at p < 0.05.
3. Results
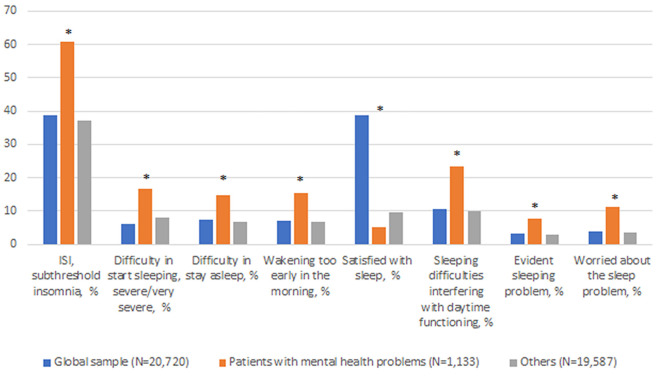
The global sample consisted of 20,720 people, 5.5% (N = 1133) of them being represented by patients with pre-existing mental disorders. Patients with mental disorders were mainly females (72.4%, N = 820), mid-age adults (40.3 ± 13.9 years) and mostly affected by anxiety (34.3%) and depressive disorders (35.3%)(See Table 1 ). Among of patients with pre-existing mental disorders, 60.8% reported a subthreshold level of insomnia (ISI mean 9.8, sd = 6.1). This rate was significantly higher compared to the general population (ISI mean score 6.6, sd = 5.1; prevalence rate: 38.8%) (p < 0.001) (see Fig. 1 ).
Table 1.
Socio-demographic and clinical characteristics of the study sample (N = 20,720).
| Global sample (N = 20,720) | Patients with mental disorders (N = 1133) | Others (N = 19,587) | |
|---|---|---|---|
| Age, years, mean ± SD | 40.4 ± 14.3 | 40.31 ± 13.9 | 40.43 ± 14.34 |
| Gender, F, % (N) | 71.0 (14,720) | 72.4 (820) | 71.0 (13,900) |
| Living with partner, yes, % (N) | 52.2 (10,808) | 43.8 (496) | 52.6 (10,312) |
| University degree, yes, % (N) | 62.0 (12,844) | 54.9 (622) | 62.4 (12,222) |
| Employed, yes, % (N) | 70.0 (14,518) | 58.5 (663) | 70.7 (13,855) |
| Lost job due the pandemic, yes, % (N) | 6.3 (1302) | 8.5 (96) | 6.2 (1206) |
| Are you practicing smart working, yes, % (N) | 34.2 (7089) | 26.4 (299) | 34.7 (6790) |
| Spending more time on Internet, yes, % (N) | 80.1 (16,598) | 79.0 (906) | 80.0 (15,670) |
| Any comorbid physical condition (s), yes, % (N) | 14.5 (3012) | 31.7 (359) | 13.5 (2653) |
| Any mental health problem (s), yes, % (N) | 5.5 (1133) | ||
| Have you been infected by COVID-19, yes, % (N) | 1.4 (296) | 1.6 (18) | 1.4 (278) |
| Have you been isolated due to COVID-19 infection, yes, % (N) | 1.5 (316) | 1.9 (22) | 1.5 (294) |
| Have you been in contact with someone affected by COVID-19, yes, % (N) | 4.2 (866) | 4.7 (53) | 4.2 (813) |
Fig. 1.
Levels of ISI global score in the total sample.
Abbreviation: ISI = Insomnia Severity Index. *p < 0.001.
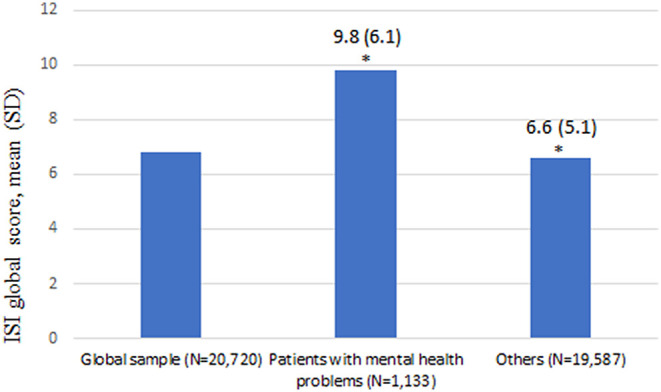
In patients with pre-existing mental disorders, the most frequent problems were related to sleeping difficulties interfering with daytime functioning (23.3%, N = 263), severe/very severe difficulties in start sleeping (16.7%, N = 188) and waking up too early in the morning (15.4%, N = 175) (p < 0.001) (see Table 2 , Fig. 2 ).
Table 2.
Levels of insomnia during the lockdown period.
| Global sample (N = 20,720) | Patients with mental disorders (N = 1133) | Others (N = 19,587) | p-value | |
|---|---|---|---|---|
| ISI global score, M (SD) | 6.8 (5.2) | 9.8 (6.1) | 6.6 (5.1) | <0.001 |
| ISI, subthreshold insomnia, yes, % (N) | 38.8 (8031) | 60.8 (688) | 37.3 (5815) | <0.001 |
| Difficulty in start sleeping, severe/very severe, yes, % (N) | 6.1 | 16.7 (188) | 7.9 (1540) | <0.001 |
| Difficulty in stay asleep, yes, % (N) | 7.4 | 14.8 (168) | 6.9 (1346) | <0.001 |
| Wakening too early in the morning, yes, % (N) | 7.2 | 15.4 (175) | 6.9 (1346) | <0.001 |
| Satisfied with sleep, yes, % (N) | 38.7 | 5.1 (58) | 9.6 (1871) | <0.001 |
| Sleeping difficulties interfering with daytime functioning, yes, % (N) | 10.7 | 23.3 (263) | 10.0 (1966) | <0.001 |
| Evident sleeping problem, yes, % (N) | 3.1 | 7.7 (88) | 2.8 (537) | <0.001 |
| Worried about the sleep problem, yes, % (N) | 3.8 | 11.2 (127) | 3.4 (668) | <0.001 |
Abbreviations: ISI = Insomnia Severity Index; M = mean; DS = standard deviation. Bold characters indicate significant values.
Fig. 2.
Differences in sleep quality between subjects with pre-existing mental disorders and the general population.
Abbreviation: ISI = Insomnia Severity Index. *p < 0.001.
According to the multivariate regression models, weighted for the propensity score, weeks of exposure to the pandemic and to the related containment measures were significantly associated with risk of insomnia with Beta coefficient (B) ranging from 1.3 (95% CI: 1.06–1.73) during the week April 9–15 to 1.2 (95% CI: 1.0–1.4) in the week April 16–April 22, even after controlling for the potential role of confounders, such as infection rate and mortality rate for COVID-19 in Italy (see Table 3 ). Otherwise, in the week April 30th- May 4th analysed data were not significantly associated with risk of insomnia (p = 0.205). Other factors associated with a risk of developing insomnia included being affected by a pre-existing mental disorder (B: 1.511; 95% CI: 1.294–1.765; p < 0.001), female gender (B: 0.908; 95% CI: 0.847–0.974; p < 0.007), being aged between 24 and 54 years (B: 1.351; 95% CI:1.155–1.581; p < 0.001) and being aged 54 to 64 years (B: 1.246: 95% CI: 1.080–1.437; p < 0.003), even after controlling for the severity of depressive, anxiety and stress symptoms as well as the general health status (see Table 3).
Table 3.
Regression models weighted by propensity score.
| Logistic regression: predictors of insomnia | ||||
|---|---|---|---|---|
| Sign. | Exp(B) | 95% C.I.per EXP(B) |
||
| Inferiore | Superiore | |||
| Being in one of the most affected Italian regions, yes | 0.832 | 1.007 | 0.942 | 1.077 |
| Age groups, up to 24 years (ref) | <0.001 | |||
| 24 to 54 years | 0.001 | 1.351 | 1.155 | 1.581 |
| 55 to 64 years | 0.003 | 1.246 | 1.080 | 1.437 |
| Over 65 years | 0.224 | 1.105 | 0.941 | 1.298 |
| Cases COVID | 0.981 | 1.000 | 1.000 | 1.000 |
| Death COVID | 0.780 | 1.000 | 0.999 | 1.000 |
| Mental health problem, yes | 0.001 | 1.511 | 1.294 | 1.765 |
| COVID+ | 0.410 | 0.937 | 0.801 | 1.094 |
| Quarantine | 0.074 | 1.092 | 0.992 | 1.203 |
| Time to exposure, ref. week March 30 – April 8 | 0.186 | |||
| Week April 15 – April 9 | 0.016 | 1.355 | 1.058 | 1.735 |
| Week April 16–April 22 | 0.041 | 1.214 | 1.008 | 1.462 |
| Week April 23 – April 29 | 0.050 | 1.171 | 0.997 | 1.375 |
| Week April 30 – May 4 | 0.205 | 1.072 | 0.963 | 1.193 |
| Lost job due to the pandemic | 0.001 | 0.749 | 0.663 | 0.848 |
| GHQ TOT | <0.001 | 1.039 | 1.029 | 1.050 |
| Gender, male ref. | 0.007 | 0.908 | 0.847 | 0.974 |
| DASS ANX | <0.001 | 1.080 | 1.075 | 1.085 |
| DASS DEP | <0.001 | 1.050 | 1.045 | 1.055 |
| DASS STRESS | <0.001 | 1.018 | 1.013 | 1.024 |
| Constant | ,000 | 0.075 | ||
Abbreviations: COVID = Coronavirus disease; GHQ = General Health Questionnaire; DASS = Depression, Anxiety, Stress Scale. Bold characters indicate significant values.
4. Discussion
COMET has been one of the first studies assessing the influence of COVID-19 pandemic on insomnia in a large sample of patients with pre-existing mental disorders compared to the general population. In addition, socio-demographic and clinical correlates of insomnia during lockdown were investigated.
Our first finding was that patients with pre-existing mental disorders had significantly higher scores at the ISI scale compared to the general population. This result is consistent with other recent findings indicating that patients with mental disorders are at a high risk of experiencing high levels of symptoms of depression, anxiety, stress and insomnia compared to healthy subjects [26,48].
In this study we also examined the different items of the ISI scale in the two sub-groups, showing that people with pre-existing mental disorders showed a global worsening in sleep quality compared to the general population, although longitudinal data is needed to confirm this finding. In particular, they had higher rates of difficulty falling asleep, early awakenings, and impairment in overall daily activities. To our knowledge, our study is the first to quantitatively and qualitatively evaluate insomnia through the various ISI items in psychiatric patients, comparing them to the general population.
During the pandemic, the exposure time to lockdown might have been a potential predictor of developing insomnia, with a significantly increased risk during the three central weeks (from April 9th to April 29th, 2020). These findings suggest that the duration of containment measures might significantly influence mental health and well-being of the general population, as also found by Sibley and colleagues in a sample of the general population in New Zealand [49]. Indeed, in the final week that was measured (April 30th - May 4th), the relationship between week of exposure to the pandemic and the likelihood of developing insomnia was not significant. Thus, these results seem to suggest that insomnia due to the pandemic was acute and temporary, rather than of continued relevance. Moreover, these findings may suggest that people showed some degree of resilience to the negative – likely short-term - effects the pandemic had on sleep. However, previous research showed that lockdown changed daily routines worldwide with an impact on sleep patterns and an increased risk of developing other mental health problems, such as depressive and anxiety disorders [48,50]. Furthermore, in the general population, we found a prevalence rate of 38.8% of subthreshold insomnia, similarly to a study conducted by Shi and coworkers in China [51]. As the observation was limited to the short-term, we do not know whether an unstable, waning and waxing course could follow: preventive interventions may include a close follow up.
In our sample, job loss and unemployment seemed to significatively influence the risk of developing insomnia. This finding is consistent with other international studies carried out in the U.S. and in South Africa, which found that job loss due to the nationwide lockdown was particularly associated with poorer mental health, with a higher risk of developing insomnia [50,52]. Conversely, unemployed subjects in Belgium were less affected by the restrictions [53]. These differences could be due to the presence of different welfare systems that were able to moderate the socio-economic impact of the pandemic. Therefore, it may be useful to identify the most appropriate and effective policy measures to protect the mental and physical health of the general population.
In our sample, the COVID-19 pandemic and its related containment measures had a negative impact on the young and adult population (i.e., those aged 24 to 64 years), but not on the eldery. The negative effects on young people's mental health is an expected result, due to the rapid change in lifestyle habits [16,54,55]. However, other studies recognize the elderly as the most fragile and at-risk individuals due to the physical distancing and the difficulties in receiving adequate care and interventions [56,57]. This finding has not been confirmed in our sample, although the participation rate in the present online survey of eldery people has been quite limited, probably due to the difficulties in accessing online tools.
Female participants were found to be at a higher risk of developing insomnia, in line with previous research conducted in Italy [[57], [58], [59]] and in other countries [14,60,61]. This finding may be due to the higher incidence of anxiety and depressive disorders in women [[62], [63], [64], [65], [66]].
The presence of a pre-existing mental health disorder was found to be a significant independent risk factor for the development of insomnia and related disorders, in line with previous data [26,67,68]. Therefore, our results confirmed the well-established relationship between sleep disorders and the whole spectrum of mental disorders [27,69,70]. Given these findings, additional studies comparing, when available, measures of sleep disorders in patients with psychiatric disorders before and after lockdown measures should be encouraged in order to ultimately assess potential differences compared to the general population and to develop and disseminate personalized supportive interventions [[71], [72], [73]]. Psychological interventions focused on sleep hygiene, planning of routine activities, adaptive coping strategies and relaxation exercises can be useful for patients with sleep disorders [27,74]. In addition, some useful recommendations adapted from cognitive-behavioral therapy for insomnia (CBT—I) have been developed by the European Academy for Cognitive-Behavioral Treatment of the Insomnia to manage the risks of sleep related problem during home confinement due to COVID-19 pandemic [[75], [76], [77]]. Some of those recommendations focused on the importance of maintaining regular sleep schedules, getting a daily dose of daylight exposure and staying away from electronics in the bedroom. Indeed, CBT-I showed to be useful in the treatment of acute insomnia due to stressful events, such as isolation and containment measures due to COVID-19 [78,79]. Of note, these strategies could be made more widely accessible via telemedicine, dedicated apps and wearable devices [80]. In respect to pharmacological treatment, general insomnia treatment guidelines should be considered. Benzodiazepines (BZ) and hypnotic BZ receptor agonists (Z-drugs; HBRA) are recommended by the current European guideline for the diagnosis and treatment of insomnia for short-term use as a second-line treatment if CBT-I treatment is ineffective or unavailable [81]. In this respect, among study's limitations it must be acknowledged that we had no information regarding the therapeutic regimens of patients with pre-existing mental disorders. In this perspective, there is the possibility that patients showed only subclinical levels of insomnia due to the presence of a specific hypnotic therapy. Ultimately, further studies to evaluate the long-term presence of insomnia in patients with mental disorders with versus without a specific pharmacological treatment are needed.
Although we found that pre-existing mental disorders, young and adult ages, as well as female gender might represent potential predictors of insomnia in our sample, these relationships and associations have been already reported before the pandemic, thus leaving open the possibility they might be not directly related to lockdown measures. However, we do not know the levels of insomnia before the lockdown to confirm the possible increase of the issue during the containment measures. Nonetheless, the exposure weeks were always compared to the first week, with data suggesting an initial negative effects on insomnia due to lockdown measures, followed by a progressive normalization of sleep just before the easing of containment measures. In addition, the lack of a test to assess a potential interaction effect of week*pre-existing problems represents a limitation to our study.
Furthermore, the cross-sectional nature of the study allowed only a single time assessment, without the possibility to analyze insomnia in participants in the pre-lockdown period, nor when the containment measures were reduced. Second, due to lockdown measures, only an online dissemination of the anonymous survey was feasible. Therefore, participants were asked whether they suffer from any mental and/or physical disorder, without any confirmation by licensed psychiatrist/clinicians, using a structured assessment tool such as the SCID-5. This aspect should have biased our findings, and research studies using robust recruitment procedure and appropriate assessment tools should be promoted in order to further confirm the findings of the present study. Nonetheless, this format could have limited the participation of elderly people or those living in socially disadvantaged contexts [82]. Moreover, the global sample cannot be considered fully representative of the Italian population. In particular, this is due to the fact that people in our sample are mainly females, who have obtained university degree, and with a mean age lower than Italian general population, as compared with socio-demographic population data available at ISTAT website. Therefore, these aspects can limit the generalizability of our findings. Indeed, our study has some strengths. In particular, it is one of the first studies carried out in different geographic Italian regions with a large sample of the general population during the lockdown period, including people with pre-existing mental disorders. Validated and reliable assessment tools were used to characterise insomnia, according to a propensity score analysis.
5. Conclusions
The COVID-19 pandemic had a major impact on the lifestyle and mental health of the general population worldwide. In particular, sleep was one of the aspects affected during the early stages of the lockdown (results for other clinical variables have been published elsewhere), as an event that abruptly subverted everyday life and the normal functioning of both people with pre-existing mental disorders and general population. Consequently, psychiatrists as well as all other mental health professionals should be aware about this phenomenon and its recognition through the use of adequate assessment tools in order to consider to adopt prompt preventive and therapeutic strategies in the initial phases of future pandemics, and avoid possible negative consequences [[83], [84], [85]]. Future studies should evaluate the long-term impact of lockdown and its containment measures on insomnia.
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
Acknowledgements
Fondazione Romeo ed Enrica Invernizzi.
References
- 1.Unützer J., Kimmel R.J., Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. 2020;19(2):130–131. doi: 10.1002/wps.20766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dutheil F., Mondillon L., Navel V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol Med. 2021;51(10):1773–1774. doi: 10.1017/S0033291720001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marazziti D., Stahl S.M. The relevance of COVID-19 pandemic to psychiatry. World Psychiatry. 2020;19(2):261. doi: 10.1002/wps.20764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Partinen M., Hublin C. Principles and practice of sleep medicine. 4th ed. Elsevier, Saunders; Philadelphia: 2005. Epidemiology of sleep disorders; pp. 626–647. [Google Scholar]
- 6.Ohayon M.M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 7.Ohayon M.M. Epidemiological overview of sleep disorders in the general population. Sleep Med Res. 2011;2(1):1–9. [Google Scholar]
- 8.Mellinger G.D., Balter M.B., Uhlenhuth E.H. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 9.Ohayon M.M., Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;37:9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 10.Ohayon M.M. Prevalence of DSM-IV diagnostic criteria of insomnia: distinguishing insomnia related to mental disorders from sleep disorders. J Psychiatr Res. 1997;31:333–346. doi: 10.1016/s0022-3956(97)00002-2. [DOI] [PubMed] [Google Scholar]
- 11.Ubara A., Sumi Y., Ito K., Matsuda A., Matsuo M., Miyamoto T., et al. Self-isolation due to COVID-19 is linked to small one-year changes in depression, sleepiness, and insomnia: results from a clinic for sleep disorders in Shiga prefecture, Japan. Int J Environ Res Public Health. 2020;17(23):8971. doi: 10.3390/ijerph17238971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020;17(13):4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. 2020;19(2):249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29(4) doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beck F., Leger D., Cortaredona S., Verger P., Peretti-Watel P., COCONEL Group Would we recover better sleep at the end of Covid-19? A relative improvement observed at the population level with the end of the lockdown in France. Sleep Med. 2021;78:115–119. doi: 10.1016/j.sleep.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fiorillo A., Sampogna G., Giallonardo V., Del Vecchio V., Luciano M., Albert U., et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: results from the COMET collaborative network. Eur Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sampogna G., Del Vecchio V., Giallonardo V., Luciano M., Albert U., Carmassi C., et al. What is the role of resilience and coping strategies on the mental health of the general population during the COVID-19 pandemic? Results from the Italian multicentric COMET study. Brain Sci. 2021;11(9):1231. doi: 10.3390/brainsci11091231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pompili M., Innamorati M., Sampogna G., Albert U., Carmassi C., Carrà G., et al. The impact of Covid-19 on unemployment across Italy: consequences for those affected by psychiatric conditions. J Affect Disord. 2021;296:59–66. doi: 10.1016/j.jad.2021.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qiu D., Li Y., Li L., He J., Ouyang F., Xiao S. Prevalence of post-traumatic stress symptoms among people influenced by coronavirus disease 2019 outbreak: a meta-analysis. Eur Psychiatry. 2021;64(1) doi: 10.1192/j.eurpsy.2021.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. Psychological impact of COVID-19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rooksby M., Furuhashi T., McLeod H.J. Hikikomori: a hidden mental health need following the COVID-19 pandemic. World Psychiatry. 2020;19(3):399–400. doi: 10.1002/wps.20804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jahrami H., BaHammam A.S., Bragazzi N.L., Saif Z., Faris M., Vitiello M.V. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta R., Grover S., Basu A., Krishnan V., Tripathi A., Subramanyam A., et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62(4):370–378. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Solé B., Verdolini N., Amoretti S., Montejo L., Rosa A.R., Hogg B., et al. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC study. J Affect Disord. 2021;281:13–23. doi: 10.1016/j.jad.2020.11.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kocevska D., Blanken T.F., Van Someren E.J.W., Rösler L. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 2020;76:86–88. doi: 10.1016/j.sleep.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20(1):124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu X., Li W., Zou S., Li Y., Wang H., Yan X., et al. Sleep disturbances and their association with quality of life in older psychiatric patients during the COVID-19 pandemic. J Geriatr Psychiatry Neurol. 2022 Mar;35(2):229–236. doi: 10.1177/08919887221078565. PMID: 35245994; PMCID: PMC8899840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giallonardo V., Sampogna G., Del Vecchio V., Luciano M., Albert U., Carmassi C., et al. The impact of quarantine and physical distancing following COVID-19 on mental health: study protocol of a multicentric Italian population trial. Front Psych. 2020;11:533. doi: 10.3389/fpsyt.2020.00533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morin C.M., Belleville G., Bélanger L., Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lovibond S.H., Lovibond P.F. 2nd ed. Psychology Foundation; Sydney: 1995. Manual for the depression anxiety & stress scales. [Google Scholar]
- 34.Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020;49:1–3. [PubMed] [Google Scholar]
- 35.Goldberg D.P., Gater R., Sartorius N., Ustun T.B., Piccinelli M., Gureje O., et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–197. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 36.Foa E.B., Huppert J.D., Leiberg S., Langner R., Kichic R., Hajcak G., et al. The obsessive-compulsive inventory: development and validation of a short version. Psychol Assess. 2002;14:485–496. doi: 10.1037/1040-3590.14.4.485. [DOI] [PubMed] [Google Scholar]
- 37.van Spijker B.A., Batterham P.J., Calear A.L., Farrer L., Christensen H., Reynolds J., et al. The suicidal ideation attributes scale (SIDAS): community-based validation study of a new scale for the measurement of suicidal ideation. Suicide Life Threat Behav. 2014;44:408–419. doi: 10.1111/sltb.12084. [DOI] [PubMed] [Google Scholar]
- 38.Kilpatrick D.G., Resnick H.S., Friedman M.J. American Psychiatric Association; Washington, DC: 2013. Severity of acute stress symptoms-adult (national stressful events survey acute stress disorder short scale [NSESSS]) [Google Scholar]
- 39.Thoresen S., Tambs K., Hussain A., Heir T., Johansen V.A., Bisson J.I. Brief measure of posttraumatic stress reactions: impact of event scale-6. Soc Psychiatry Psychiatr Epidemiol. 2010;45:405–412. doi: 10.1007/s00127-009-0073-x. [DOI] [PubMed] [Google Scholar]
- 40.Connor K.M., Davidson J.R.T. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC) depress. Anxiety. 2003;18:71–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 41.Carver C.S., Connor-Smith J. Personality and coping. Annu Rev Psychol. 2010;61:679–704. doi: 10.1146/annurev.psych.093008.100352. [DOI] [PubMed] [Google Scholar]
- 42.Cann A., Calhoun L.G., Tedeschi R.G., Taku K., Vishnevsky T., Triplett K.N., et al. A short form of the posttraumatic growth inventory. Anxiety Stress Coping. 2010;23:127–137. doi: 10.1080/10615800903094273. [DOI] [PubMed] [Google Scholar]
- 43.Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. J Pers Assess. 1988;1:30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]
- 44.Maslach C., Jackson S.E. Consulting Psychologists Press; Palo Alto, CA: 1981. MBI: maslach burnout inventory. [Google Scholar]
- 45.Haukoos J.S., Lewis R.J. The propensity score. JAMA. 2015;314:1637–1638. doi: 10.1001/jama.2015.13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raad H., Cornelius V., Chan S., Williamson E., Cro S. An evaluation of inverse probability weighting using the propensity score for baseline covariate adjustment in smaller population randomised controlled trials with a continuous outcome. BMC Med Res Methodol. 2020;20:70. doi: 10.1186/s12874-020-00947-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rubin D.B. Wiley; New York: 1977. Multiple imputation for nonresponse in surveys. [Google Scholar]
- 48.Mandelkorn U., Genzer S., Choshen-Hillel S., Reiter J., Meira E., Cruz M., et al. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med. 2021;17(1):45–53. doi: 10.5664/jcsm.8800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sibley C.G., Greaves L.M., Satherley N., Wilson M.S., Overall N.C., Lee C.H.J., et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am Psychol. 2020;75:618–630. doi: 10.1037/amp0000662. [DOI] [PubMed] [Google Scholar]
- 50.Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Mental health during the first weeks of the COVID-19 pandemic in the United States. Front Psych. 2021;12 doi: 10.3389/fpsyt.2021.561898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shi L., Lu Z.A., Que J.Y., Huang X.L., Liu L., Ran M.S., et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davy J.P., Scheuermaier K., Roden L.C., Christie C.J., Bentley A., Gomez-Olive F.X., et al. The COVID-19 lockdown and changes in routine-oriented lifestyle behaviors and symptoms of depression, anxiety, and insomnia in South Africa. J Phys Act Health. 2021:1–12. doi: 10.1123/jpah.2020-0863. [DOI] [PubMed] [Google Scholar]
- 53.Cellini N., Conte F., De Rosa O., Giganti F., Malloggi S., Reyt M., et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021;77:112–119. doi: 10.1016/j.sleep.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. Erratum in: J Psychosom Res 2020;139:110278. PMID: 32682159; PMCID: PMC7832650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Glowacz F., Schmits E. Psychological distress during the COVID-19 lockdown: the young adults most at risk. Psychiatry Res. 2020;293:113486. doi: 10.1016/j.psychres.2020.113486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salfi F., Lauriola M., D’Atri A., Amicucci G., Viselli L., Tempesta D., et al. Demographic, psychological, chronobiological, and work-related predictors of sleep disturbances during the COVID-19 lockdown in Italy. Sci Rep. 2021;11(1):11416. doi: 10.1038/s41598-021-90993-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Somma A., Gialdi G., Krueger R.F., Markon K.E., Frau C., Lovallo S., et al. Dysfunctional personality features, non-scientifically supported causal beliefs, and emotional problems during the first month of the COVID-19 pandemic in Italy. Pers Individ Differ. 2020;165 doi: 10.1016/j.paid.2020.110139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alonzi S., La Torre A., Silverstein M.W. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychol Trauma. 2020;12:S236–S238. doi: 10.1037/tra0000840. [DOI] [PubMed] [Google Scholar]
- 59.Amerio A., Lugo A., Stival C., Fanucchi T., Gorini G., Pacifici R., et al. COVID-19 lockdown impact on mental health in a large representative sample of Italian adults. J Affect Disord. 2021;292:398–404. doi: 10.1016/j.jad.2021.05.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meitei S.Y., Pao P.S.V., Baite K.D., Konjengbam H. Prevalence of insomnia and internet dependence amidst the COVID 19 among the northeast Indian population: a preliminary study. Sleep Vigil. 2021:1–6. doi: 10.1007/s41782-021-00153-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alharbi A.S., Alshahrani S.M., Alsaadi M.M., Al-Jahdali H.H., Wali S.O., BaHammam A.S. Sleep quality and insomnia during the COVID-19 lockdown among the Saudi public: a cross-sectional study. Saudi Med J. 2021;42(4):384–390. doi: 10.15537/smj.2021.42.4.20200735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McLean C.P., Asnaani A., Litz B.T., Hofmann S.G. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schuch J.J., Roest A.M., Nolen W.A., Penninx B.W., de Jonge P. Gender differences in major depressive disorder: results from the Netherlands study of depression and anxiety. J Affect Disord. 2014 Mar;156:156–163. doi: 10.1016/j.jad.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 64.Steel Z., Marnane C., Iranpour C., Chey T., Jackson J.W., Patel V., et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43(2):476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang B., Wing Y.K. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29(1):85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 66.Charles J., Harrison C., Britt H. Insomnia. Aust Fam Physician. 2009;38(5):283. [PubMed] [Google Scholar]
- 67.Pérez-Carbonell L., Meurling I.J., Wassermann D., Gnoni V., Leschziner G., Weighall A., et al. Impact of the novel coronavirus (COVID-19) pandemic on sleep. J Thorac Dis. 2020;12(Suppl. 2):S163–S175. doi: 10.21037/jtd-cus-2020-015. Erratum in: J Thorac Dis 2021;13(2):1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Plunkett R., Costello S., McGovern M., McDonald C., Hallahan B. Impact of the COVID-19 pandemic on patients with pre-existing anxiety disorders attending secondary care. Ir J Psychol Med. 2021;38(2):123–131. doi: 10.1017/ipm.2020.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kokou-Kpolou C.K., Megalakaki O., Laimou D., Kousouri M. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bartoszek A., Walkowiak D., Bartoszek A., Kardas G. Mental well-being (depression, loneliness, insomnia, daily life fatigue) during COVID-19 related home-confinement-a study from Poland. Int J Environ Res Public Health. 2020;17(20):7417. doi: 10.3390/ijerph17207417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Goldman M.L., Druss B.G., Horvitz-Lennon M., Norquist G.S., Kroeger Ptakowski K., Brinkley A., et al. Mental health policy in the era of COVID-19. Psychiatr Serv. 2020;10 doi: 10.1176/appi.ps.202000219. [DOI] [PubMed] [Google Scholar]
- 72.Kaufman K.R., Petkova E., Bhui K.S., Schulze T.G. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open. 2020;6(3) doi: 10.1192/bjo.2020.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Greenberg N., Brooks S.K., Wessely S., Tracy D.K. How might the NHS protect the mental health of health-care workers after the COVID-19 crisis? Lancet Psychiatry. 2020;7 doi: 10.1016/S2215-0366(20)30224-8. doi: S2215-0366(20)30224-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stefana A., Youngstrom E.A., Jun C., Hinshaw S., Maxwell V., Michalak E., et al. The COVID-19 pandemic is a crisis and opportunity for bipolar disorder. Bipolar Disord. 2020 doi: 10.1111/bdi.12949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Krystal A.D., Prather A.A., Ashbrook L.H. The assessment and management of insomnia: an update. World Psychiatry. 2019;18(3):337–352. doi: 10.1002/wps.20674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B., et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I academy. J Sleep Res. 2020;29(4) doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 77.Baglioni C., Altena E., Bjorvatn B., Blom K., Bothelius K., Devoto A., et al. The European academy for cognitive behavioural therapy for insomnia: an initiative of the European insomnia network to promote implementation and dissemination of treatment. J Sleep Res. 2020;29(2) doi: 10.1111/jsr.12967. [DOI] [PubMed] [Google Scholar]
- 78.Boullin P., Ellwood C., Ellis J.G. Group vs. individual treatment for acute insomnia: a pilot study evaluating a “one-shot” treatment strategy. Brain Sci. 2016;7:E1. doi: 10.3390/brainsci7010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Randall C., Nowakowski S., Ellis J.G. Managing acute insomnia in prison: evaluation of a “one-shot” cognitive behavioral therapy for insomnia (CBT-I) intervention. Behav Sleep Med. 2019;17(6):827–836. doi: 10.1080/15402002.2018.1518227. [DOI] [PubMed] [Google Scholar]
- 80.Morin C.M., Carrier J., Bastien C., Godbout R. Canadian sleep and circadian network. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can J Public Health. 2020;111(5):654–657. doi: 10.17269/s41997-020-00382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Riemann D., Baglioni C., Bassetti C., Bjorvatn B., Dolenc Groselj L., Ellis J.G., et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. doi: 10.1111/jsr.12594. [DOI] [PubMed] [Google Scholar]
- 82.Shah S.G.S., Nogueras D., van Woerden H.C., Kiparoglou V. The COVID-19 pandemic: a pandemic of lockdown loneliness and the role of digital technology. J Med Internet Res. 2020;22(11) doi: 10.2196/22287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stewart D.E., Appelbaum P.S. COVID-19 and psychiatrists’ responsibilities: a WPA position paper. World Psychiatry. 2020;19(3):406–407. doi: 10.1002/wps.20803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kuzman M.R., Curkovic M., Wasserman D. Principles of mental health care during the COVID-19 pandemic. Eur Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]