Abstract
Introduction:
Acute kidney injury (AKI) can be a severe complication of the coronavirus 2019 (COVID-19) infection. Follow-up data of these AKI patients, including the rate of progression to chronic kidney disease (CKD), is limited.
Methods:
COVID-19 patients with AKI, admitted from June 1, 2020, to August 25, 2020, were enrolled prospectively. Their clinical profile, biochemical investigations, urine analysis, treatment, and outcome in terms of mortality or discharge were analyzed. The discharged patients were followed up 3 months later to determine their renal recovery status.
Results:
AKI was noted in 146 out of 4,613 COVID-19 patients with an incidence of 3.16%. The outcome was available for 111 patients. According to the KDIGO (Kidney Disease Improving Global Outcomes) AKI criteria, 20 (18%) patients were in Stage 1, 16 (14%) in Stage 2, and 75 (68%) in Stage 3 AKI. Proteinuria and hematuria were present in 66% and 41%, respectively. Renal replacement therapy (RRT) was required in 45 (40.5%) patients. A total of 53 (47.7%) patients turned RT-PCR negative and were discharged. The renal recovery at discharge was complete in 31 of 111 (28%), partial in 20 of 111 (18%), and none in two (2%) patients. At 3 months follow-up of discharged patients, total mortality rate was 55.85%. Twenty three of 53 (43%) recovered their renal functions to baseline and 26 of 53 (49%) had progressed to CKD. Diabetes mellitus, dyspnea, altered sensorium, severe acute respiratory distress syndrome, need for RRT, lymphopenia, high neutrophil–lymphocyte ratio, hyperglycemia, raised inflammatory markers, and hematuria were associated with high mortality rate and reached statistical significance.
Conclusion:
AKI in COVID-19 patients has a high mortality rate (55.85%) with a high CKD progression rate among survivors (49%).
Keywords: Acute kidney injury, chronic kidney disease, COVID-19, India, mortality
Introduction
Acute kidney injury (AKI) has been commonly described among coronavirus disease 2019 (COVID-19) patients. The initial studies, mainly from China, showed a much lower incidence rate of around 3.6%[1] to 5.1%.[2] However, later reports, especially from the West have shown higher AKI incidence rates. A study of 5,700 patients from New York[3] has shown AKI in COVID-19 patients to be around 22% among discharged and 67% among deceased patients.
The pathogenesis of AKI in COVID-19 is multifactorial with profoundly interconnected pathways of cytokine storm, organ cross-talk, systemic effects, and various mechanisms of renal involvement that include[4,5] prerenal azotemia, cytokine release (acute tubular necrosis [ATN], myoglobin cast nephropathy, collapsing glomerulopathy, and thrombotic microangiopathy), direct viral invasion, medication-induced effects (acute interstitial nephritis [AIN] with antiviral agents, oxalate nephropathy with vitamin C, and various antibiotics causing AIN/ATN). COVID-19 patients with AKI have high mortality ranging from 35% to 71%, and mortality is even higher in Stage 3 AKI ranging from 52% to 88% regardless of RRT usage.[6] AKI secondary to other causes is associated with an eightfold increased risk of developing the end-stage renal disease (ESRD).[7] It is, therefore, conceivable that survivors of COVID-19 AKI will be at increased risk of progression to CKD.
Mumbai was one of the initial hotspots of COVID-19 infection in India, and ours was the first fully COVID-19 dedicated tertiary government hospital in Mumbai. Information regarding incidence rate, the clinical course of AKI, and mortality among our population is extremely limited, and no long-term data regarding their follow-up and CKD progression are available till now. This study was undertaken to address the above points.
Methodology
This was a prospective, observational single-center study to assess the clinical profile and outcome of AKI in patients with COVID-19 disease admitted in a tertiary care hospital, from June 1, 2020, to August 25, 2020, after obtaining permission from the Institutional Ethics Committee. They were followed up telephonically 3 months later to determine if renal functions had returned to baseline or if they had progressed to CKD with available previous serum creatinine levels; the latest serum creatinine before admission was noted as the baseline serum creatinine. In patients with unknown previous renal function, imputation of baseline creatinine was done by entering back-calculated values using the MDRD (Modification of Diet in Renal Disease) formula with a target glomerular filtration rate of 75 mL/minute/1.73 m2. However, if the nadir creatinine during hospital admission or at 3 months follow-up was lesser than the imputed value, the baseline creatinine was corrected to the nadir creatinine value.
Inclusion criteria
Patients with the following features were included:
All patients of AKI or acute on CKD, with SARS-CoV-2 positive by RT-PCR, admitted to our hospital (including kidney transplant)
Those for whom outcome (discharge/death) was known
Patients in the age group ≥18 years
Those who gave written informed consent.
Exclusion criteria
All patients who had the following features were excluded:
Patients who had CKD Stage 5D
Those in the age grouP <18 years
Their demographic data, comorbidities, drug history, investigation details including hematologic and biochemical reports, inflammatory markers, urine microscopy reports, radiography (X-ray chest and/or computed tomography chest), and treatment details were noted. Clinical parameters such as blood pressure, pulse rate, arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FiO2) value, and urine output were noted. Clinical course in terms of inotrope requirement, need for oxygen therapy by invasive/noninvasive ventilation, and need for RRT or any other organ dysfunction were recorded. Dialysis in all our patients was provided as SLED (sustained low-efficiency dialysis)/HD (hemodialysis). They were discharged if they were asymptomatic for at least 3 days with either recovering AKI or continued hemodialysis (if no recovery occurred) along with negative RT-PCR report. The final outcomes, that is, mortality or renal recovery (complete, partial, or none) at discharge, were noted. All discharged patients were followed up telephonically and their latest renal function test reports, which were done at local laboratories, were noted to determine renal recovery or progression to CKD.
Definitions
1. The Kidney Disease: Improving Global Outcomes (KDIGO) Criteria for AKI (2012)
AKI was defined as any of the following:
An increase in serum creatinine by >0.3 mg/dL within 48 hours
An increase in serum creatinine to >1.5 times baseline, which is known or presumed to have occurred within the prior 7 days
Urine volume <0.5 mL/kg/hour for 6 hours
2.AKI staging was calculated as follows:
AKI Stage 1: An increase in serum creatinine > 0.3 mg/dL in 48 hours or 1.5 to 1.9 times baseline or urine output <0.5 mL/kg/hour (6–12 hours)
AKI Stage 2: An increase in serum creatinine 2 to 2.9 times from baseline or <0.5 mL/kg/hour (>12 hours
AKI Stage 3: An increase in serum creatinine more than 3 times baseline or to ≥4 mg/dL or the initiation of RRT or urine output <0.3 mL/kg/hour (>24 hours) or anuria (>12 hours)
3.Berlin Criteria for Acute Respiratory Distress Syndrome (ARDS)
Mild ARDS: PaO2/FiO2 ratio ≤300 and >200
Moderate ARSD: PaO2/FiO2 ratio 100–200
Severe ARDS: PaO2/FiO2 ratio <100
4.AKI Recovery (at discharge)[8]:
Complete recovery: A difference in creatinine of <0.3 mg/dL and creatinine change in percentage <25%
Partial recovery: A decrease in serum creatinine from the peak value of >33% but still above 25% of normal/baseline value
No recovery: Persistent need for hemodialysis or decrease in serum creatinine of less than 33% from peak values.
5.Progression to CKD as per the KDIGO 2012 guidelines[9]
It was defined for AKI patients as eGFR <60 mL/minute/1.73 m2 after 3 months or for patients with underlying CKD as a decline of eGFR >25% from baseline at 3 months.
Statistical analysis
The gathered data were analyzed by SPSS (Statistical Package for the Social Sciences, Version 21) software (IBM, Chicago, IL, USA). The categorical variables were described as frequency or percentages and compared with the Chi-square test or Fisher's exact test as appropriate. The continuous variables were described as mean ± standard deviation or mean rank and compared with Mann–Whitney U test. Graphical representation was done whenever necessary. A P value < 0.05 was considered statistically significant.
Results
A total of 4,613 patients with SARS-CoV-2 infection were admitted to the hospital from June 1, 2020, to August 25, 2020, of which 146 (3.16%) patients had AKI [Table 1]. The outcomes were available for 111 patients at the end of the study period; 35 patients were without outcome (discharge/mortality) and hence not included in the data set. Limited manpower availability during the pandemic made it difficult to collect their data retrospectively.
Table 1.
AKI in COVID
| All (n=111) | Discharged (n=53) | In-hospital mortality (n=58) | P | |
|---|---|---|---|---|
| AKI | ||||
| Stage 1 | 20 (18%) | 13 (25%) | 7 (12%) | 0.139 |
| Stage 2 | 16 (14%) | 9 (17%) | 7 (12%) | |
| Stage 3 | 75 (68%) | 31 (58%) | 44 (76%) | |
| Need for RRT | 45 (40.5%) | 15 (28.3%) | 30 (50%) | 0.022 |
| AKI on CKD | 23 (20.7%) | 13 (24.5%) | 10 (17%) | 0.360 |
| Duration of RRT (days) | ||||
| <4 | 22 (49%) | 1 (7%) | 21 (70%) | <0.001 |
| 5-9 | 16 (35.5%) | 9 (60%) | 7 (23%) | |
| >10 | 7 (15.5%) | 5 (34%) | 2 (7%) | |
| Renal recovery at discharge | ||||
| Complete | 31 (28%) | 31 (58%) | 0 | <0.001 |
| Partial | 20 (18%) | 20 (38%) | 0 | |
| No recovery | 2 (2%) | 2 (4%) | 0 | |
| Expired | 58 (52%) | 0 | 58 (100%) | |
| Renal Recovery at 3 months | ||||
| Recovered | 23 (20.7%) | 23 (43%) | 0 | |
| CKD Progression | 26 (23.4%) | 26 (49%) | 0 | |
| Expired | 62 (55.85%) | 4 (8%) | 58 (100%) |
AKI=acute kidney injury; RRT=renal replacement therapy; CKD=chronic kidney disease. P value less than 0.5 is considered significant and has been highlighted in bold
While most of these patients had severe COVID-19 disease, 18.9% of patients developed AKI despite having mild COVID symptoms, without any features of ARDS. Our patient set was from the early phase of the pandemic, wherein 4,613 COVID-19 patients were admitted in 86 days, with resources limited comparatively; thus kidney biopsy was logistically not possible. Baseline details of subjects are shown in Table 2. At admission, the patients had been symptomatic for a mean of 6.29 ± 3.09 days. Most patients were nonoliguric (57.7%) at diagnosis of AKI. About 37% of patients had hypotension and needed inotropes.
Table 2.
Baseline demographics
| All (n=111) | Discharged (n=53) | In-hospital mortality (n=58) | P | |
|---|---|---|---|---|
| Age (Mean±SD) | 62.02±12.13 | 61.23±12.02 | 62.74±12.28 | 0.367 |
| Gender | ||||
| Male | 75 (67.6%) | 39 (74%) | 36 (62%) | 0.227 |
| Female | 36 (32.4%) | 14 (26%) | 22 (38%) | |
| Comorbidity | ||||
| CKD | 23 (20.7%) | 13 (24.5%) | 10 (17.2%) | 0.360 |
| Transplant | 2 (1.8%) | 1 (1.8%) | 1 (1.7%) | 1.00 |
| Hypertension | 72 (64.9%) | 35 (66%) | 37 (63.8%) | 0.844 |
| Diabetes | 71 (64.0%) | 27 (51%) | 44 (75.9%) | 0.011 |
| CAD | 19 (17.1%) | 10 (19%) | 9 (15.5%) | 0.802 |
| Underlying respiratory illness | 5 (4.5%) | 4 (7.5%) | 1 (1.7%) | 0.191 |
| CVA | 6 (5.4%) | 3 (5.6%) | 3 (5.2%) | 0.814 |
| Others (HIV, malignancy, Kochs, MN, SS) | 15 (13.5%) | 6 (11.3%) | 9 (15.5%) | 0.582 |
| Drugs | ||||
| ACE inhibitors/ARBs | 13 (11.7%) | 8 (15%) | 5 (9%) | 0.379 |
| NSAIDs | 5 (4.5%) | 1 (2%) | 4 (7%) | 0.366 |
| Immunosuppression | 3 (2.7%) | 2 (4%) | 1 (2%) | 0.605 |
| Tenofovir | 2 (1.8%) | 2 (4%) | 0 (0%) | 0.226 |
| Duration of symptoms at admission (days) | ||||
| 1-4 | 33 (29.7%) | 17 (32%) | 16 (27.6%) | 0.476 |
| 5-9 | 63 (56.8%) | 31 (58.5%) | 32 (55.2%) | |
| >9 | 15 (13.5%) | 5 (9.5%) | 10 (17.2%) | |
| Clinical symptoms | ||||
| Fever | 87 (78.4%) | 39 (74%) | 48 (83%) | 0.258 |
| Cough | 59 (53.2%) | 24 (45%) | 35 (60%) | 0.130 |
| Fatigue | 53 (47.7%) | 27 (50.9%) | 26 (45%) | 0.571 |
| Breathlessness | 96 (86.5%) | 41 (77%) | 55 (95%) | 0.011 |
| Altered sensorium | 59 (53.2%) | 11 (21%) | 48 (83%) | <0.0001 |
| Fluid overload | 14 (12.6%) | 2 (3.8%) | 12 (21%) | 0.016 |
| Vomiting | 5 (4.5%) | 3 (5.7%) | 2 (3%) | 0.534 |
| Loose motions | 15 (13.5%) | 5 (9.4%) | 10 (17%) | 0.234 |
| Clinical course | ||||
| Pulse (mean) | 95.50±18.19 | 86.96±15.64 | 103.29±16.91 | <0.001 |
| Need of ionotropes | 41 (37%) | 1 (1.9%) | 40 (68.9%) | <0.001 |
| Bleeding | 4 (3.6%) | 0 | 4 (6.9%) | 0.058 |
| ARDS | ||||
| No | 21 (18.9%) | 21 (39.6%) | 0 | <0.001 |
| Mild | 18 (16.2%) | 15 (28.3%) | 3 (5.2%) | |
| Moderate | 21 (18.9%) | 11 (20.8%) | 10 (17.2%) | |
| Severe | 51 (45.9%) | 6 (11.3%) | 45 (77.6%) | |
| Need of oxygen | ||||
| No | 21 (18.9%) | 21 (39.6%) | 0 | |
| High Flow Nasal Oxygen/Bag and Mask Ventilation | 54 (48.6%) | 25 (47.2%) | 29 (50%) | <0.001 |
| CPAP/BIPAP | 24 (21.6%) | 7 (13.2%) | 17 (29.3%) | |
| Invasive | 12 (10.8%) | 0 | 12 (20.7%) | |
| Bacterial Infections | ||||
| Cellulitis | 5 (4.5%) | 4 (7.5%) | 1 (1.7%) | 0.487 |
| Urinary tract Infection | 3 (2.7%) | 2 (3.7%) | 1 (1.7%) | 0.605 |
| Pneumonia | 3 (2.7%) | 1 (1.9%) | 2 (3.4%) | 0.792 |
SD=standard deviation; CKD=chronic kidney disease; ARDS=Acute respiratory distress syndrome; CAD=coronary artery disease; MN=Membranous Nephropathy; SS=Systemic sclerosis; CVA=cerebrovascular accident; HIV=human immunodeficiency virus; ACE=angiotensin-converting enzyme; ARB=angiotensin receptor blocker; NSAID=nonsteroidal anti-inflammatory drugs; CPAP=continuous positive airway pressure; BPAP=bilevel positive airway pressure. P Value of less than 0.5 is considered significant and has been highlighted in bold
Overall, out of 111 patients, 20 (18%) patients were Stage 1 AKI, 16 (14%) were Stage 2 AKI, and 75 (68%) were Stage 3 AKI. Out of 111 patients, 45 (40.54%) patients needed RRT [Table 1]. The patients were dialyzed for clinical and biochemical indications such as uremia, fluid overload, hyperkalemia, or metabolic acidosis. The increasing stage of AKI was not associated with increased mortality. However, hemodialysis initiation was a poor prognostic marker (P = 0.022) with two-thirds of patients eventually dying, and the majority (70%) of them dying within 4 days of initiation (P < 0.001) of hemodialysis. Dialysis in all our patients was provided as SLED/HD. Acute peritoneal dialysis was not done in any patients.
At the time of discharge, AKI recovered completely in 31 of 53 (58%) patients and partially in 20 of 53 (38%) patients. AKI did not recover in two of 53 (4%) patients [Figure 1]. Patients with underlying CKD fared like AKI patients in terms of recovery of renal functions at discharge (66% vs. 56%). Investigations are mentioned in detail in Table 3. Urine abnormalities [Table 4] were seen in most patients.
Figure 1.
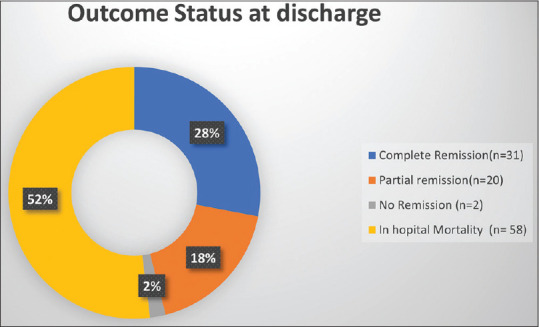
Of 111 patients, 58 patients died in the hospital. A total of 53 patients of COVID-19 with acute kidney injury were discharged, of whom 31 (28%) patients had complete remission, 20 (18%) patients had partial remission, and two (2%) patients had no remission of acute kidney injury
Table 3.
Investigations
| All (n=111) | Discharged (n=53) | In-hospital mortality (n=58) | P | |
|---|---|---|---|---|
| Hb (g/dL) (12-18) | 11.05±2.50 | 10.59±2.12 | 11.47±2.76 | 0.107 |
| WBC (cells/mm3) (4,000-11,000) | 14857.48±8531.83 | 12433.58±9257.50 | 15406.90±7883.84 | 0.081 |
| Neutrophils (cells/mm3) (1,500-8,000) | 13063.81±7867.98 | 12433.58±8533.48 | 13639.71±7233.72 | 0.057 |
| PMN (%) (42%-85%) | 87.51±7.77 | 86.37±7.84 | 88.56±7.63 | 0.012 |
| Lymphocyte count (1,000-4,000) | 1236.16±1336.85 | 1358.57±1075.30 | 1124.31±1538.65 | 0.003 |
| Lymphocyte (%) (20-40) | 8.61±6.43 | 9.99±6.38 | 7.36±6.27 | 0.001 |
| NLR (<5) | 17.13±16.76 | 13.20±12.59 | 20.72±19.24 | 0.004 |
| Platelet count (/mm3) (150,000-350,000/µL) | 213.53±148.00 | 236.09±170.72 | 192.91±121.56 | 0.308 |
| Serum creatinine (mg/dL) on admission (0.8-1.5) | 4.01±3.70 | 3.82±3.39 | 4.19±3.99 | 0.985 |
| Peak serum creatinine (mg/dL) | 6.37±3.81 | 5.65±3.65 | 7.02±3.86 | 0.024 |
| BUN (mg%) (5-20) | 82.53±42.87 | 78.42±39.72 | 86.29±45.58 | 0.308 |
| Na (meq/L) (135-145) | 139.15±16.50 | 135.46±19.81 | 142.52±11.96 | 0.016 |
| Hypernatremia (>145 meq/L) | 26 (23.4%) | 6 (11.3%) | 20 (34.5%) | 0.016 |
| K (mEq/L) (3.5-5.5) | 4.52±1.0 | 4.32±0.83 | 4.72±1.09 | 0.13926 |
| Blood sugar (mg/dL) | 250.92±169.73 | 186.26±143.98 | 310.00±171.01 | <0.0001 |
| ESR (mm/hour) (Male: 0-15 ; Female: 0-20) | 69.50±38.45 | 57.25±39.00 | 80.69±34.61 | <0.0001 |
| CRP (mg/L) (<5) | 58.30±49.31 | 45.70±40.21 | 69.82±54.17 | 0.008 |
| LDH (U/L) (220-430) | 1030.59±587.48 | 777.39±532.97 | 1261.97±541.13 | <0.0001 |
| Bilirubin (up to 1 mg%) | 0.76±2.01 | 1.13±2.88 | 0.43±0.21 | 0.317 |
| SGOT (U/L) (5-40) | 50.02±59.93 | 40.60±50.92 | 58.64±66.40 | 0.013 |
| SGPT (U/L) (5-40) | 40.10±58.47 | 36.08±67.51 | 43.78±49.11 | 0.008 |
| CPK (IU/L) (0-120) | 189.45±251.94 | 140.66±166.11 | 234.03±305.09 | 0.007 |
| D-dimer (µg/mL) (<0.80) | 10.18±9.78 | 9.29±9.42 | 11.00±10.11 | 0.241 |
| IL-6 (pg/mL) (<7) | 1386.50±1724.12 | 753.84±1155.05 | 1964.63±1951.21 | <0.0001 |
| Ferritin (ng/mL) (Male: 22-322 Female: 10-201) | 1246.14±1330.62 | 1048.18±1135.62 | 1427.03±1473.29 | 0.019 |
Hb=hemoglobin; WBC=white blood cell; PMN=polymorphonuclear leukocyte; NLR=neutrophil–leucocyte ratio; BUN=blood urea nitrogen; Na=sodium; K=potassium; ESR=erythrocyte sedimentation rate; CRP=C-reactive protein; SGOT=serum glutamic-oxaloacetic transaminase; SGPT=serum glutamic-pyruvic transaminase; CPK=creatine phosphokinase; IL-6=interleukin-6. P Value of less than 0.5 is considered significant and has been highlighted in bold
Table 4.
Urine abnormalities
| All (n=111) | Discharged (n=53) | In-hospital mortality (n=58) | P | |
|---|---|---|---|---|
| Urine dipstick | ||||
| Protein | ||||
| None | 38 (34.2%) | 20 (38%) | 18 (31%) | 0.352 |
| 1 | 18 (16.2%) | 11 (21%) | 7 (12%) | |
| 2 | 22 (19.8%) | 11 (21%) | 11 (19%) | |
| 3 | 22 (19.8%) | 7 (13%) | 15 (26%) | |
| 4 | 11 (9.9%) | 4 (7.5%) | 7 (12%) | |
| WBC | ||||
| No | 69 (62.2%) | 35 (66.0%) | 34 (58.6%) | 0.217 |
| 1+ | 27 (23.4%) | 8 (15.1%) | 19 (32.7%) | |
| 2+ | 10 (9.0%) | 6 (11.3%) | 4 (6.9%) | |
| 3+ | 4 (3.6%) | 3 (5.7%) | 1 (1.7%) | |
| 4+ | 1 (0.9%) | 1 (1.9%) | 0 (0.0%) | |
| Blood | ||||
| None | 65 (58.6%) | 39 (74%) | 26 (45%) | 0.003 |
| 1 | 13 (11.7%) | 7 (13%) | 6 (10%) | |
| 2 | 23 (20.7%) | 5 (9.4%) | 18 (31%) | |
| 3 | 10 (9.0%) | 2 (4%) | 8 (14%) | |
| Ketones | 18 (16.2%) | 2 (4%) | 16 (28%) | 0.001 |
| Nitrite | 4 (3.6%) | 2 (4%) | 2 (3.4%) | 1.00 |
| Glucose | 27 (24.3%) | 4 (7.5%) | 23 (40%) | <0.0001 |
| Urobilinogen | 1 (0.9%) | 1 (2%) | 0 (0.0%) | 0.477 |
WBC=white blood cell P Value of less than 0.5 is considered significant and has been highlighted in bold
Over the 3 months, treatment protocols changed with gathering evidence [Table 5]. Steroids were given as methylprednisolone 80 mg/day for 7 to 14 days or dexamethasone 6 mg tablet once daily. All patients received antibiotics. Patients of AKI were switched to unfractionated heparin (81.1%) from low-molecular-weight heparin. Three months follow-up outcome is shown in Table 6. The mortality of AKI patients with COVID-19 at 3 months was found to be 55.85%. Similarly, eight out of 20 (40%) patients who had partial recovery of renal functions at discharge progressed to CKD at 3 months [Figure 2].
Table 5.
Medications
| Medications | All (n=111) | Discharged (n=53) | In-hospital mortality (n=58) |
|---|---|---|---|
| Hydroxychloroquine | 47 (42.34%) | 22 (41.5%) | 25 (43.1%) |
| Azithromycin | 72 (64.9%) | 30 (56.6%) | 42 (72.4%) |
| Iveremctin | 74 (66.7%) | 35 (66.03%) | 39 (67.2%) |
| Ritonavir/lopinavir | 11 (10%) | 4 (7.54%) | 7 (12.1%) |
| Antibiotics | 111 (100%) | 53 (100%) | 58 (100%) |
| Steroids | 108 (97.3%) | 50 (94.3%) | 58 (100%) |
| Anticoagulation | 90 (81.1%) | 39 (73.6%) | 51 (87.9%) |
| Tocilizumab | 15 (13.5%) | 3 (5.6%) | 12 (20.7%) |
| Remdesivir | 12 (10.8%) | 7 (13.2%) | 5 (8.62%) |
Table 6.
Renal recovery, CKD progression and mortality of patients at discharge and 3 months.
| Complete recovery at discharge | Partial recovery at discharge | No recovery at discharge | Total | |
|---|---|---|---|---|
| Complete recovery of AKI at 3 months | 14 | 9 | 0 | 23 |
| CKD progression at 3 months | 16 | 8 | 2 | 26 |
| Expired at 3 months | 1 | 3 | 0 | 4 |
| Total | 31 | 20 | 2 | 53 |
AKI=acute kidney injury; CKD=chronic kidney disease
Figure 2.
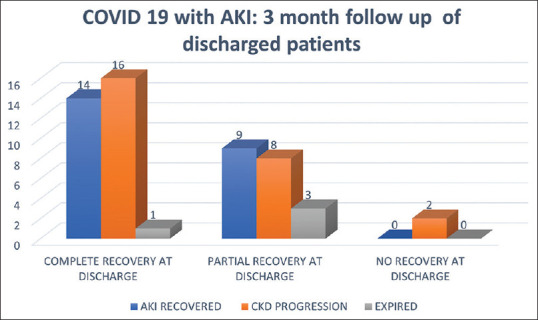
A total of 53 out of 111 COVID-19 patients who had AKI were discharged. Thirty-one had complete recovery, 20 had partial and, two out of 53 had no recovery. After 3 months follow-up, among patients with complete recovery (n = 31), 16 progressed to CKD, 14 recovered renal functions, and one died. Among patients with partial renal recovery at discharge (n = 20), eight progressed to CKD, nine recovered renal functions, and three expired. Both patients with no renal recovery at discharge progressed to CKD AKI: Acute kidney Injury; CKD: chronic kidney disease
Comparison of discharged versus in-hospital mortality group
There was no difference in terms of age and gender between the survivors and the deceased.
Diabetes, even after adjusting for age and other comorbid conditions, was more commonly seen in the mortality group versus discharged (76% vs. 51%: P = 0.010)[Table 2]. The patients who were sicker at the time of admission with symptoms such as breathlessness (95% vs. 77%: deceased vs. discharged group), altered sensorium (83% vs. 21%), and features of fluid overload (20.7% vs. 3.8%) were more likely to have a significantly poor outcome in terms of mortality (P values 0.011, 0.0001, 0.016, respectively)[Table 2]. Hypotension was a much more common feature among the deceased group as compared with the discharged group (68.9% vs. 1.9%)[Table 2]. Thirty hemodialysis slots per day were made available for the COVID-19 patients during the pandemic. An adequate number of slots for the AKI patients helped us provide adequate dialysis, as per the requirement, whenever needed. The dialysis provided was SLED/intermittent HD.
All patients of COVID-19 with AKI who died had underlying ARDS requiring oxygen therapy. Severe ARDS as per the Berlin criteria was present in 77.6% of deceased as compared with 11.32% in discharged. All patients who required intubation and mechanical ventilation expired in our cohort. The need for oxygen therapy/mechanical ventilation reached a statistical significance between the discharged and deceased groups [Table 2].
Overall, all COVID-19 patients with AKI had leukocytosis (14857.48 ± 8531.83), but differential counts of patients in the mortality group showed them to have more neutrophilia (polymorphonuclear leukocytes percentage 88.56 ± 7.63 vs. 86.37 ± 7.84; P = 0.012), lymphopenia (lymphocytes percentage 7.36 ± 6.27 vs. 9.99 ± 6.38, P = 0.001) with a higher NLR ratio (20.72 ± 19.24 vs. 13.20 ± 12.59, P = 0.004). The value of inflammatory markers was statistically higher among patients who died in the hospital compared with discharged patients (ESR 80.69 ± 34.61 vs. 57.25 ± 39.00, P < 0.001; CRP 69.82 ± 54.17 vs. 45.70 ± 40.21, P = 0.008; IL-6 1964.63 ± 1951.21 vs. 753.84 ± 1155.05, P < 0.001; ferritin 1427.03 ± 1473.29 vs. 1048.18 ± 1135.62, P = 0.019)[Table 3].
Serum lactose dehydrogenase (LDH), CPK, and IL-6 values were also statistically higher among the mortality group [Table 3]. Transaminitis was overall mild in this cohort, but still the SGOT (serum glutamic-oxaloacetic transaminase) and SGPT (serum glutamic-pyruvic transaminase) values were found to be higher among the deceased. High blood sugars and even diabetic ketoacidosis (DKA) were frequent findings among our patients. It could be attributed to a large proportion of them being diabetic (64%) along with the use of steroids in the majority of them (97.3%). The deceased group had statistically higher blood sugar levels (310.00 ± 171.01 vs. 186.26 ± 143.98, P < 0.001). Hypernatremia was more commonly seen in the mortality group (34.5% vs. 11.3%, P = 0.016)Table 3.
Discussion
AKI incidence rate (3.16%) in our hospitalized study population of COVID-19 patients was comparable with other eastern countries such as China[10] even though the Western countries have much higher incidence rates of around 22% to 40%.[3,11] AKI incidence of 8.6% has been noted by a South Asian country in intensive care unit COVID-19 admissions.[12] Greater age; comorbidities, mainly diabetes; and need for mechanical ventilation are some of the important factors associated with increased AKI incidence. The wide variation in incidence is probably related to population demographics, variable inclusion criteria, and AKI risk factors.[13] Comorbidities were present in around two-thirds of our patients. Diabetes was present in 64% of our population and was associated with high in-hospital mortality. These patients often were found to have DKA on admission and secondary infections such as cellulitis. Control of blood sugar levels was especially challenging considering all of them were given steroids for 14 days and most patients requiring continuous insulin infusions. In a Spanish study of 11,312 patients with COVID-19 disease, regardless of the previous history of diabetes, admission hyperglycemia was found to be an independent risk factor for mortality.[14]
AKI is more common in severe COVID-19 disease. Patients of AKI who died in our cohort had a statistically significantly higher incidence of dyspnea (95%), encephalopathy (83%), fluid overload (20.7%), and hypotension needing inotrope support (68.9%) and oxygen support (100%) when compared with survivors. Patients needing mechanical ventilation had the worst prognosis with no patients surviving in our study. Although most patients of AKI (80%) had underlying ARDS, up to 20% of patients developed AKI despite having a milder disease and no ARDS suggesting different mechanisms from organ cross-talk, sepsis, cytokine storm, and maybe direct viral nephrotoxicity.
The mortality rate of AKI in our cohort was high with 52.25% of patients dying in the hospital and an additional 3.6% of patients at home after discharge, amounting to a total mortality rate of 55.85%. This is much higher than the COVID-19 mortality rate in the general population, which is estimated to be around 2% to 9% the world over.[15] AKI is an independent risk factor for mortality in COVID patients. COVID-19 patients with AKI have high mortality ranging from 35% to 71%, and mortality is even higher in Stage 3 AKI patients ranging from 52% to 88%, regardless of RRT usage.[6]
Of all the COVID-19 AKI patients in our study, less than one-third of patients (28%) were discharged to home with complete recovery of renal functions, and at 3 months only 21% were alive with fully recovered AKI. Among patients who survived post-COVID-19 AKI, almost half (49%) progressed to CKD. A similar study of follow-up of COVID-19 AKI patients from New York[16] studied 1,835 patients of COVID-19 AKI and followed them up for a median of 21 days post-discharge. A total of 832 patients were discharged, of which 65% had complete recovery of renal functions, and 35% had acute kidney disease (AKD). Follow-up creatinine values were available for 212 patients. Around 18% of patients with complete recovery and 64% of AKD patients on follow-up had persistent renal dysfunction. The SARS-CoV-2 virus enters the host cell via membrane-bound ACE2, which is also present on podocytes and renal tubular cells. Autopsy studies and renal biopsy series have found most patients to have diffuse acute tubular injury along with other findings such as collapsing glomerulopathy, thrombotic microangiopathy, and myoglobin cast nephropathy. Electron microscopy in some, but not all, studies has shown the presence of SARS-CoV-2 viral particles in the kidney.[17,18,19] Direct viral effects with collapsing glomerulopathy, endothelial damage, coagulopathy, and complement activation may be responsible for incomplete recovery. Given that COVID-19 is a pandemic that has already affected millions of people worldwide with a high incidence of AKI and potentially higher incomplete recovery, as seen in our study, close surveillance after discharge in this group is essential.
In some studies, CKD was found to be an independent risk factor for mortality.[2] Although AKI was associated with high mortality overall, patients with underlying CKD were similarly distributed among the survivor and mortality groups in our cohort.
In our study, proteinuria was seen in 66%, leukocyturia in 38%, and hematuria in 42% as per urine dipstick findings. Of these, hematuria and leukocyturia were seen in significantly higher numbers in the mortality group. A study by Cheng et al.[2] revealed hematuria and proteinuria in 43.9% and 26.7% COVID-19 AKI patients, respectively, and the presence of these both was associated with a higher risk of mortality. Another study by Hirsch et al.[20] from New York noted proteinuria, hematuria, and WBC in urine in 64%, 74%, and 36.5% of AKI patients, respectively. Inflammatory markers including ESR, ferritin, IL-6, and LDH were all raised in our whole cohort, and the difference between the survivors and deceased was statistically significant. As with other studies, lymphopenia with a high NLR ratio (P = 0.004) was also seen in a higher proportion of patients who died.[21]
Rhabdomyolysis has been associated with AKI in some studies.[22,23] In our study, higher CPK levels were associated with increased risk of mortality, but they were not quantitatively as high as seen in diagnosed cases of rhabdomyolysis, which are typically >1,000 units/L.
Limitation
It is possible that a few cases of mild AKI were missed out due to nonreferral to the nephrology department. Those who were without outcome at the end of the study could not be included in the data set. Kidney biopsy could not be done in those who did not recover. While admission serum creatinine value was done at our center's central laboratory using Jaffe's method, post-discharge patients were allowed to get investigations from the local laboratory; hence, standardization of testing method could not be ensured.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to thank Dnyaneshwar Gajbhare and Walmik Suresh Mistari for their help.
References
- 1.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–38. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323:2052–9. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng JH, Bijol V, Sparks MA, Sise ME, Izzedine H, Jhaveri KD. Pathophysiology and Pathology of acute kidney injury in patients with COVID-19. Adv Chronic Kidney Dis. 2020;27:365–76. doi: 10.1053/j.ackd.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ronco C, Reis T. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat Rev Nephrol. 2020;16:308–10. doi: 10.1038/s41581-020-0284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michel RR, Rachel H. Acute kidney injury, another challenge for nephrology. Am J Nephrology. 2020;51:761–3. doi: 10.1159/000511161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ishani A, Xue JL, Himmelfarb J, Eggers PW, Kimmel PL, Molitoris BA, et al. Acute kidney injury increases risk of ESRD among elderly. J Am Soc Nephrol. 2009;20:223–8. doi: 10.1681/ASN.2007080837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schrijvers D, Gunst J, Van den Berghe G, Schetz M. Recovery from AKI by KDIGO criteria. Crit Care. 2014;18((Suppl 1)):P386. [Google Scholar]
- 9.Kidney Disease: Improving Global Outcomes (KDIGO) CKD work group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150. [Google Scholar]
- 10.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19: Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng JH, Hirsch JS, Hazzan A, Wanchoo R, Shah HH, Malieckal DA, et al. Outcomes among patients hospitalized with COVID-19 and acute kidney injury. Am J Kidney Dis. 2021;77:204–15. doi: 10.1053/j.ajkd.2020.09.002. e1. doi: 10.1053/j.ajkd. 2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhadade R, Harde M, deSouza R, Kasbe A, Deshpande C, Dave S, et al. Appraisal of critically ill COVID-19 patients at a dedicated COVID hospital. J Assoc Physicians India. 2020;68:14–9. [PubMed] [Google Scholar]
- 13.Kolhe NV, Fluck RJ, Selby NM, Taal MW. Acute kidney injury associated with COVID- 19: A retrospective cohort study? PLoS Med. 2020;17:e1003406. doi: 10.1371/journal.pmed.1003406. doi: 10.1371/journal.pmed. 1003406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carrasco-Sánchez FJ, López-Carmona MD, Martínez-Marcos FJ, Pérez-Belmonte LM, Hidalgo-Jiménez A, Buonaiuto V, et al. Admission hyperglycaemia as a predictor of mortality in patients hospitalized with COVID-19 regardless of diabetes status: Data from the Spanish SEMI-COVID-19 Registry. Ann Med. 2021;53:103–16. doi: 10.1080/07853890.2020.1836566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Available from: https://coronavirus.jhu.edu/data/mortality .
- 16.Chan L, Chaudhary K, Saha A, Chauhan K, Vaid A, Baweja M, et al. Acute kidney injury in hospitalized patients with COVID-19. medRxiv 2020. 2020.05.04.20090944. doi: 10.1101/2020.05.04.20090944. [Google Scholar]
- 17.Sharma P, Uppal NN, Wanchoo R, Shah HH, Yang Y, Parikh R, et al. COVID-19-associated kidney injury: A case series of kidney biopsy findings. J Am Soc Nephrol. 2020;31:1948–58. doi: 10.1681/ASN.2020050699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su H, Yang M, Wan C, Yi LX, Tang F, Zhu HY, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98:219–27. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Santoriello D, Khairallah P, Bomback AS, Xu K, Kudose S, Batal I, et al. Postmortem kidney pathology findings in patients with COVID-19. J Am Soc Nephrol. 2020;31:2158–67. doi: 10.1681/ASN.2020050744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98:209–18. doi: 10.1016/j.kint.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li X, Liu C, Mao Z, Xiao M, Wang L, Qi S, et al. Predictive values of neutrophil-to-lymphocyte ratio on disease severity and mortality in COVID-19 patients: A systematic review and meta-analysis. Crit Care. 2020;24:647. doi: 10.1186/s13054-020-03374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin M, Tong Q. Rhabdomyolysis as potential late complication associated with COVID-19. Emerg Infect Dis. 2020;26:1618–20. doi: 10.3201/eid2607.200445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taxbro K, Kahlow H, Wulcan H, Fornarve A. Rhabdomyolysis and acute kidney injury in severe COVID-19 infection? BMJ Case Rep. 2020;13:e237616. doi: 10.1136/bcr-2020-237616. doi: 10.1136/bcr-2020-237616. [DOI] [PMC free article] [PubMed] [Google Scholar]


