Complementary and alternative medicine (CAM) use is common in the United States [1, 2]. However, certain herbal supplements have immunostimulatory effects, including Spirulina platensis, Aphanizomenon flos-aquae, Chlorella, Echinacea, and alfalfa [1]. Patients may consume immunostimulatory CAM for their purported health effects [3, 4]. However, this poses a potential risk for patients with autoimmune skin disease [1]. To characterize the frequency of immunostimulatory CAM use in such patients, we performed a single-center case-control study of herbal supplement use (Spirulina, Echinacea, Chlorella, Aphanizomenon, and alfalfa) among adults with dermatomyositis (DM), cutaneous lupus erythematosus (CLE), autoimmune blistering disease (AIBD), and healthy controls without autoimmune disease.
Patients in the principal investigator’s clinics were systematically surveyed about herbal supplement use at any point prior to their disease flare. To ensure standardization and minimize recall bias, patients were asked about CAM use in a stepwise manner (Supplementary Material). Healthy controls were surveyed in general dermatology clinics. Chart review information included disease cohort, CAM use history, and demographics. Demographics were analyzed with descriptive statistics. Fisher’s exact tests were performed to compare the frequency of CAM use among the DM, CLE, and AIBD cohorts to healthy controls. Results were reported as odds ratios at a significance level of 0.05.
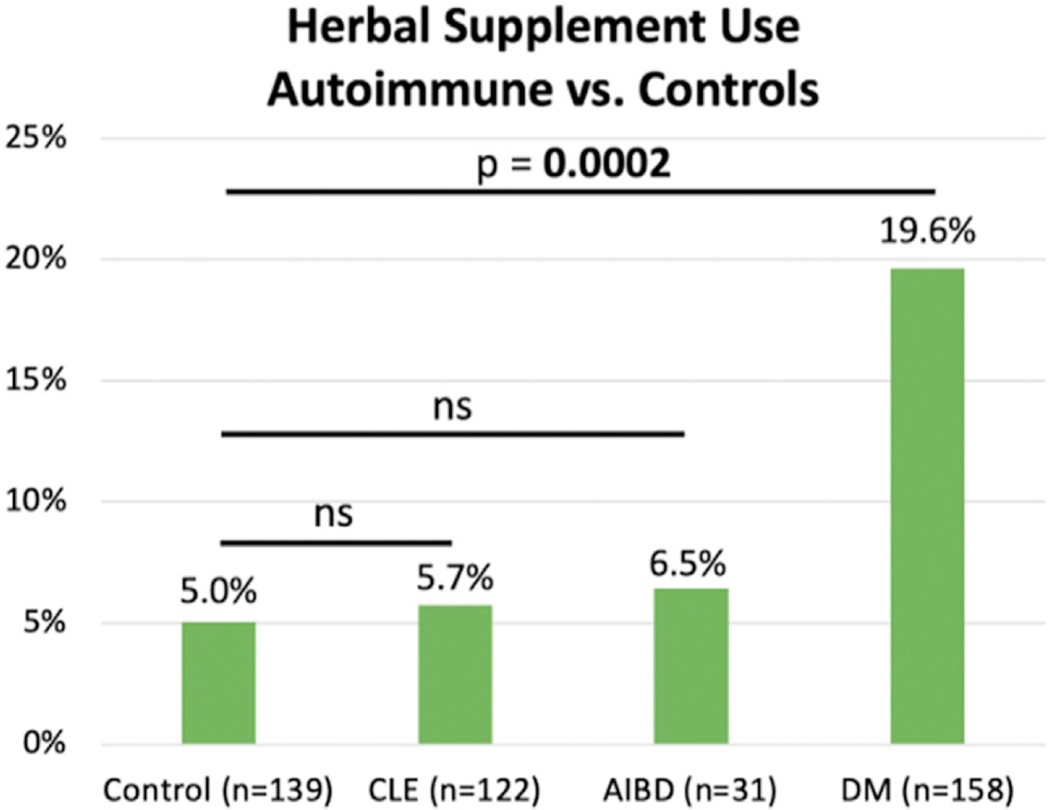
450 patients were included in this study (158 DM, 122 CLE, 31 AIBD, 139 controls) (Table 1). CAM use was reported in 19.6% of the DM cohort, 5.7% of CLE, 6.5% of AIBD, and 5.0% of controls (Figure 1, Table 1). Spirulina was the most frequently used CAM, with 14.6% of DM patients in the cohort reporting Spirulina use, 4.1% of CLE, 0% of AIBD, and 4.3% of controls (Table 1). Chlorella (7.6%), Aphanizomenon flos-aquae (2.5%), alfalfa (1.9%), and Echinacea (2.5%) use were reported in a smaller proportion of DM patients (Table 1). DM patients were significantly more likely to have used immunostimulatory CAMs compared to controls (OR 4.58, p=0.0002), in contrast to CLE (p=0.0956) or AIBD (p=0.6688). Spirulina was significantly more likely to be used by DM patients compared to controls (OR 3.76, p=0.0031) (Table 1). Echinacea, Aphanizomenon flos-aquae, Chlorella, and Alfalfa were not significantly associated with any autoimmune cohort.
Table 1:
Demographics
| DM (n = 158) | CLE (n = 122) | AIBD (n = 31) | Control (n = 139) | ||
|---|---|---|---|---|---|
| Sex – n (%) | Female | 138 (87.3) | 102 (83.6) | 22 (71.0) | 108 (77.7) |
| Male | 20 (12.6) | 20 (16.4) | 9 (29.0) | 31 (22.3) | |
| Race – n (%) | White | 129 (81.6) | 64 (52.5) | 19 (61.3) | 113 (81.3) |
| Black | 13 (8.2) | 39 (32.0) | 1 (3.2) | 7 (5.0) | |
| Asian | 5 (3.2) | 9 (7.4) | 4 (12.9) | 10 (7.2) | |
| Other | 11 (7.0) | 10 (8.2) | 7 (22.6) | 9 (6.5) | |
| Age at Disease Onset – Median (IQR) | 50.0 (40.1 – 58.2) | 34.8 (26.0 –47.5) | 55.3 (49.6 – 65.2) | N/A | |
| Age at Clinic Visit – Median (IQR) | 56.0 (48.1 – 67.1) | 51.5 (40.6 – 62.4) | 64.9 (56.8 – 76.9) | 55.1 (35.1 – 66.0) | |
| Spirulina | n (%) | 23 (14.6) | 5 (4.1) | 0 (0) | 6 (4.3) |
| OR | 3.76 | 0.95 | 0 | N/A | |
| p-value | 0.0031 | NS | NS | N/A | |
| Echinacea | n (%) | 4 (2.5) | 2 (1.6) | 1 (3.2) | 2 (1.4) |
| OR | 1.78 | 1.14 | 2.27 | N/A | |
| p-value | NS | NS | NS | N/A | |
| Aphanizomenon | n (%) | 4 (2.5) | 0 (0) | 2 (6.5) | 1 (0.7) |
| OR | 3.57 | 0 | 9.33 | N/A | |
| p-value | NS | NS | NS | N/A | |
| Chlorella | n (%) | 12 (7.6) | 2 (1.6) | 1 (3.2) | 4 (2.9) |
| OR | 2.77 | 0.56 | 1.12 | N/A | |
| p-value | NS | NS | NS | N/A | |
| Alfalfa | n (%) | 3 (1.9) | 2 (1.6) | 0 (0) | 2 (1.4) |
| OR | 1.32 | 1.14 | 0 | N/A | |
| p-value | NS | NS | NS | N/A | |
| Any Herbal | n (%) | 31 (19.6) | 7 (5.7) | 2 (6.5) | 7 (5.0) |
| OR | 4.58 | 1.15 | 1.30 | N/A | |
| p-value | 0.0002 | NS | NS | N/A | |
DM – Dermatomyositis; CLE – Cutaneous Lupus Erythematosus; AIBD – Autoimmune Blistering Disease; N/A – Not Applicable; OR – Odds Ratio; IQR – Interquartile Range; NS – Not Statistically Significant (p > 0.05)
Figure 1: Herbal Supplement Use among Autoimmune Cohorts versus Controls.
DM – Dermatomyositis; CLE – Cutaneous Lupus Erythematosus; AIBD – Autoimmune Blistering Disease; ns – Not Statistically Significant (P > 0.05)
These results demonstrate that immunostimulatory CAM use may be more common among DM patients compared to CLE, AIBD, and controls in this cohort. Among the DM cohort, Spirulina was the most common CAM. Limitations include recall bias, the case-control study design, and the single-center nature of this study. This study does not account for timing between CAM use and disease onset, or history of flares. It is unknown whether Spirulina affects the course of DM, or whether patients with DM flares were likely to take Spirulina. Prospective blinded studies are needed to ascertain the link between Spirulina and DM. Although the effects of immunostimulatory CAM on autoimmune skin disease are not currently understood, our work shows that they are used by some dermatology patients. Clinicians should inquire about supplement use in patients with autoimmune skin disease, and assess the potential impact on their patients’ clinical course and wellbeing.
Supplementary Material
Acknowledgements:
William D. James, MD
Funding/Support:
United States Department of Veterans Affairs (Veterans Health Administration, Office of Research and Development and Biomedical Laboratory Research and Development) (VPW). Center for Advancing Translational Sciences of the National Institutes of Health, TL1TR001880 (CEB).
Footnotes
Conflict of Interest:
The authors of this manuscript have no conflicts of interest to disclose.
IRB Approval:
IRB approval has been obtained for this study (University of Pennsylvania IRB # 833981)
References
- 1.Chakka S, et al. , The effects of immunostimulatory herbal supplements on autoimmune skin diseases. Journal of the American Academy of Dermatology, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falci L, Shi Z, and Greenlee H, Multiple Chronic Conditions and Use of Complementary and Alternative Medicine Among US Adults: Results From the 2012 National Health Interview Survey. Prev Chronic Dis, 2016. 13: p. E61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deng R. and Chow T-J, Hypolipidemic, antioxidant, and antiinflammatory activities of microalgae Spirulina. Cardiovascular therapeutics, 2010. 28(4): p. e33–e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karkos PD, et al. , Spirulina in clinical practice: evidence-based human applications. Evidence-based complementary and alternative medicine : eCAM, 2011. 2011: p. 531053–531053. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.