Abstract
Introduction Periodontal diseases are widespread in women of reproductive potential. Although their treatment of these disorders contributes to oral health, there is still no conclusive evidence that this intervention has a beneficial effect on the course of pregnancy, in particular the rate of premature births. On the one hand, the aim of the paper is a systematic assessment of the association between periodontal diseases and pregnancy complications, based on the current literature. On the other hand, the efficacy of periodontal treatments vs. no treatment in pregnant women should be assessed with the target criterion of premature birth or other pregnancy complications.
Materials and methods The narrative review was based on the PRISMA statement. Premature births were defined as primary endpoints, while various perinatal and maternal outcomes were grouped together as secondary endpoints. An electronic database search for relevant meta-analyses and systematic reviews was carried out in PubMed and the Cochrane database. Methodological characteristics and the results of the included studies were extracted. The RR or OR (95% CI) was used to measure the result. The quality of the included studies was assessed according to the AMSTAR checklist.
Results Seven publications were included (total number of subjects n = 56755). The majority of included studies do not demonstrate a significant association of periodontal disease and/or periodontal treatment with certain childhood and/or maternal outcomes. The quality of the included studies was deemed to be sufficient.
Conclusion Even today, there is insufficient evidence to confirm the correlation between periodontal disease and certain maternal and/or infantile outcomes. Periodontal treatment during pregnancy also does not seem to affect the risks of pregnancy. Nevertheless, it is recommended that all pregnant women are advised to improve their daily oral hygiene in order to prevent inflammatory diseases, regardless of the progress of the pregnancy.
Keywords: periodontal diseases, premature birth, adverse birth outcomes, pregnancy, evidence
Background
Premature birth: Epidemiology and etiology
Birth before the 37th week of pregnancy is the second leading cause of death for children under the age of five, according to data from the WHO, and is also the leading cause of neonatal mortality and severe early and long-term morbidity 1 2 3 4 5 . Every year, about 15 million children are born prematurely worldwide 6 . In 50% of all spontaneous premature births, the etiology is uncertain 5 . Despite intensive efforts and advances in medicine, the rate of premature births has not seen a significant global decrease 5 6 7 . That means that each year nearly one million premature babies die in the first 28 days after birth 2 . Developing countries account for a large part of this figure 6 . The rate of premature birth in Germany was 7.99% in 2020. Thus, Germany is among the lowest in Europe. Preterm infants face particular health risks due to the immaturity of their organ systems 2 3 . Among other things, the immaturity of the central nervous system causes apnea, bradycardia and temperature regulation disorders 3 . They often suffer from long-term physical and mental limitations, developmental disorders of the nervous system and breathing problems 2 5 . Last but not least, risks of clinical treatment, such as nosocomial infections, must be taken into account. Causal therapy for an impending premature birth is not yet possible. For medical reasons, planned premature birth plays an important role in reducing the premature birth rate 2 . A further starting point is risk-based prevention, which is of particular importance, especially in the outpatient sector 2 7 . This includes, in particular, discussion of maternal dental health in pregnancy.
Periodontitis in pregnancy
For many years, periodontology has been concerned with the potential connection between the inflammatory foci in the oral cavity and systemic diseases such as diabetes, arthritis, dementia and cardiovascular diseases. Similarly, an association with undesirable consequences for pregnancy such as premature birth, low birth weight and preeclampsia is discussed 4 5 8 . Inflammation of the periodontal bed (periodontitis) and gums (gingivitis) are common in women of reproductive potential 5 8 . The risk of periodontal inflammation is increased especially during pregnancy, and pre-existing gum disease tends to worsen during pregnancy 4 5 8 9 . The occurrence of chronic periodontitis in pregnancy is reported in the literature as 5% to 20%, and gingivitis as 30% to 100% 5 8 9 . The susceptibility of pregnant women to inflammation in the oral cavity could be explained by the significantly altered hormonal balance in pregnancy, which changes the tissue morphology in the oral cavity 4 5 8 . Increased vascular permeability, vascular proliferation and dilatation may contribute to susceptibility to inflammation. However, immunological mechanisms could also play a role, since the maternal immune system is suppressed during pregnancy in order to prevent premature delivery (rejection) of the fetus 5 8 .
Periodontitis and risk of premature birth
With regard to premature birth, a much-discussed mechanism is the rise of bacteria via the vagina and cervix into the uterine cavity 2 5 8 . This obvious mechanism has been relatively marginalized in the scientific discussion in recent years in favor of other pathological mechanisms in its weighting. Among other hypotheses, the question arises of a connection between inflammation in the oral cavity and pregnancy complications. One mechanism would be, for example, the hematogenic spread of microorganisms in the oral cavity 5 8 . In the case of a periodontal infection, bacteria can pass via the pocket epithelium into blood vessels and from there reach the fetal placental unit 5 8 . Thus, Katz et al. 2009 detected the periodontal bacterium Porphyromonas gingivalis in the placenta of women with increased concentration of chorioamnionitis 5 . Indirect biological mechanisms could also explain a possible correlation between inflammation of the oral cavity and premature births. Through the oral infection, endogenous inflammatory mediators are increasingly excreted, such as the tumor necrosis factor-α (TNF-α) 5 8 . The result is increased prostaglandin synthesis, which can lead to uterine contractions, cervical dilatations and premature rupture of membranes. Additively, bacteria and their products can reach the liver and likewise cause an increased release of inflammatory mediators there 5 . Kumar et al. 2014 were able to show that the serum level of TNF-α was statistically significantly higher in women with periodontitis and preeclampsia than in pregnant women with inconspicuous oral hygiene and preeclampsia 5 . However, an alternative explanation could also be that pregnant women who get a periodontal disease have a genetic predisposition to an excessive local or systemic inflammatory response to a certain stimulus (e.g., bacteria) 5 8 . In addition to this explanation, it would also be conceivable to increase the production of cytokines after contact with bacteria, which, for example, can lead to premature labor or a rupture of membranes 5 8 . It remains to be seen whether the presumed association between dental health and the risk of premature birth and the association with other pregnancy complications can be confirmed epidemiologically.
Objectives of the paper
This paper is based on two research questions.
How can the correlation between periodontal disease in pregnant women and pregnancy complications be assessed using meta-analyses and systematic reviews?
How can the efficacy of periodontal treatment vs. no treatment in pregnant women with periodontal disease be assessed in terms of premature birth and other negative birth outcomes (see definition below) using meta-analyses and systematic reviews?
In this way, conclusions can be drawn for evidence-based midwifery in terms of proper counselling during pregnancy, and gynecologists and midwives in private practice can be supported in clinical decision-making when caring for pregnant women.
Materials and Methods
Study design
The present study sees itself as a narrative review, which provides a broad overview of a specific topic 10 .
The PRISMA statement (Preferred Reporting Items for Systematic reviews and Meta-analyses) is to be used to improve reporting of systematic reviews and meta-analyses. Consisting of a checklist and a flow chart, which is divided into four phases of a systematic overview 11 , the PRISMA statement was applied in some parts due to its high relevance in the present study.
Primary and secondary outcomes
This narrative review examined the correlation between periodontal diseases and certain outcomes. The primary outcome of the present narrative review is premature birth up to a maximum of 36+6 weeks of pregnancy. Perinatal outcomes (low birth weight below 2500 g, very low birth weight below 1500 g, low premature birth weight, low gestational age, premature birth before 35 weeks of pregnancy or < 35 weeks of pregnancy [up to 34+6 weeks of pregnancy] or before 32 weeks of pregnancy or < 32 weeks of pregnancy [up to 31+6 weeks of pregnancy], stillbirths) and maternal outcomes (mortality, preeclampsia, undesirable effect of therapy, plaque values, gum health, change in the depth of probing, change in the clinical attachment values) were defined as secondary outcomes.
Selection of studies
In February 2021, an electronic database search (PubMed and Cochrane database) was conducted after relevant meta-analyses and systematic reviews, which was updated in February 2022. Three independent authors (AK, NF, DS) searched for relevant articles on the basis of the previously defined inclusion and exclusion criteria. Finally, the search results of all three authors were combined as part of a collegial scientific exchange.
Search terms
In the studies used, the treatment of inflammatory gum diseases such as gingivitis and periodontitis was mostly analyzed. No classification of the severity of the periodontal disease has been established.
The databases used for research were PubMed and the Cochrane database. For the research on PubMed, the filters “Systematic Review” and “Meta-analysis” have been activated. Another filter was the inclusion of the publication of the studies in the period between January 1, 2010, and February 1, 2022. The search strategy was to connect relevant search terms by the Boolean operators. One search term describes the primary outcome of the present paper (“preterm birth”), while another search term describes the intervention to be investigated (“periodontal treatment”). These search terms were linked by the Boolean operators (e.g., “preterm birth” AND “periodontal treatment”). Likewise, the search term of the primary outcome (“preterm birth”) was combined with the search term “periodontal disease” (e.g., “preterm birth” AND “periodontal disease”). In the Cochrane database, the search term “periodontal disease” was researched with the filter of the “Cochrane Reviews”. The last search took place on February 14, 2022.
Inclusion criteria and exclusion criteria
One inclusion criterion was the study design of the meta-analysis. Studies that carried out both a meta-analysis and a systematic review were also accepted. Only studies that were written in English and published between January 1, 2010, and February 1, 2022, were included. The participants of the studies should represent women in pregnancy. In addition, studies were included that looked at the gestational age at birth in connection with periodontal diseases. Another inclusion criterion was perinatal and maternal outcomes in the context of periodontal diseases, which are related to negative birth events. Studies analyzing the correlation between premature birth and the treatment of periodontal disease were also included. All study designs (e.g., observational or interventional study) as well as other literature (e.g., textbooks or grey literature) apart from the systematic reviews and meta-analyses were excluded. Studies which exclusively represented the study design of systematic review work (not in combination with meta-analyses) were also excluded.
Data extraction
The methodological characteristics of the included studies were analyzed and presented. These presented the study type, country and intervention of the examined studies, the characteristics of the subjects, the study objective, the endpoints/outcomes as well as the inclusion/exclusion criteria of the selected studies. The results of the included studies were also considered. The endpoints and results of the studies were extracted. The relative risk (RR) or odds ratio (OR) (95% confidence interval) was considered as an outcome measure of the included meta-analyses.
Evaluation of the quality of the included studies
High-quality review papers systematically identify the evidence, evaluate it methodically, and summarize it descriptively or meta-analytically. Systematic distortions of systematic reviews should be evaluated 12 . To assess the quality of the included systematic reviews and meta-analyses, the validated and frequently used AMSTAR checklist was applied, which contains 11 key questions. The answer options Yes, No, Uncertain and Not applicable were available for each key question. However, no cut-off was planned for the overall assessment. For this review, the AMSTAR checklist (A MeaSurement Tool to Assess Systematic Reviews) was applied in German, and with a slightly modified translation, taking into account the current standards – and was presented in tabular form 12 .
Results
Results of the narrative literature search
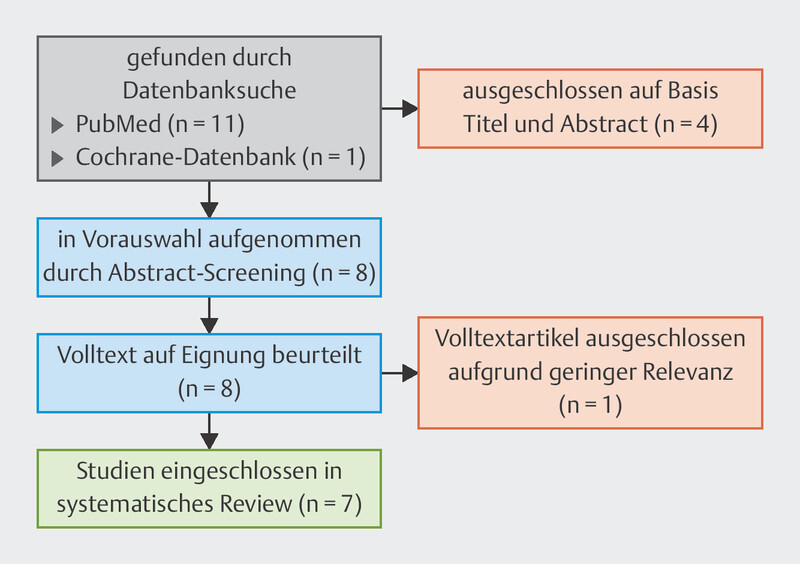
The electronic search in the databases yielded 13 results. After screening the abstract, four articles were excluded. The eight remaining articles were evaluated in full text, whereby one article was excluded due to its low relevance for the question focused here. Finally, seven articles 4 8 13 14 15 16 17 were included in this narrative review (cf. Fig. 1 ). The seven meta-analyses and systematic reviews come from Great Britain, Spain, Poland, Brazil, Canada and Greece.
Fig. 1.
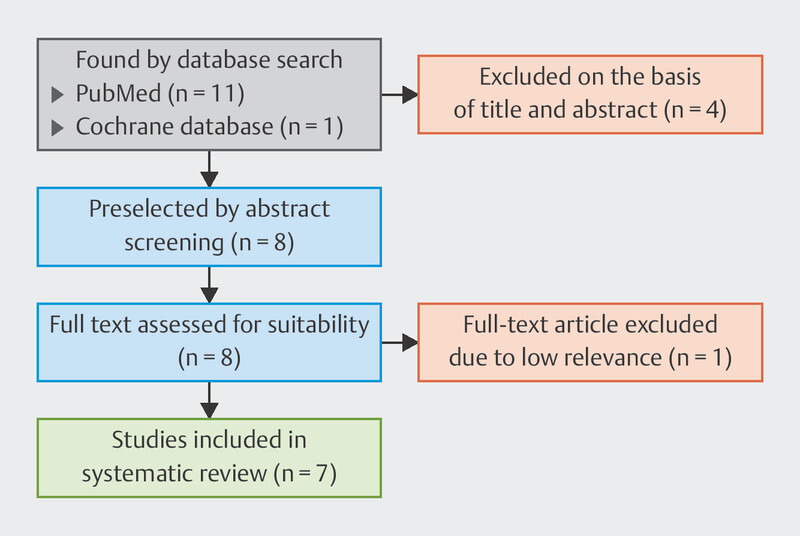
Fig. Flow chart for narrative literature research according to the PRISMA Schema 11 .
Methodological characteristics of the included studies
A total of seven studies were included in this narrative review. These studies presented meta-analyses and systematic reviews. Four meta-analyses and systematic reviews 4 13 14 17 looked at randomized and controlled intervention studies (intervention periodontal treatment vs. no treatment), whereas three meta-analyses and systematic reviews included observational studies that analyzed the association of negative birth outcomes with periodontal diseases 8 15 16 . The meta-analyses include studies from five different continents (America, Europe, Asia, Australia, Africa) and seven different countries (Chile, Iraq, India, Brazil, Malaysia, Madagascar, Canada). The number of subjects in the included studies varied between n = 6558 and n = 12047. For all the studies considered here, the total number of female subjects was n = 56755. In all studies, pregnant women represented the subjects and the exposure was periodontal disease. In all the meta-analyses and systematic reviews examined, the primary outcome was premature birth (< 37 weeks) 4 8 13 14 15 16 17 . In addition, in six of the seven 4 8 13 14 15 17 meta-analyses and systematic reviews, the low birth weight in SGA (< 2500 g) was considered a primary outcome. The secondary outcomes of the studies represented different maternal or perinatal outcomes. The methodological characteristics of the studies are shown in detail in Table 1 .
Table 1 Methodological characteristics of the included studies.
| Study | Study type | Country and intervention of the examined studies | Identification of subjects | Study objective | Endpoints/outcomes | Inclusion/exclusion criteria |
| Iheozor-Ejiofor et al., 2017 4 | Cochrane Review |
Countries of the examined studies:
5 from North America, 4 from South America, 3 from Europe, 2 from Asia and 1 from Australia.
Intervention of the examined studies: The intervention was periodontal treatment (any combination of mechanical treatment) vs. no treatment in 11 studies and periodontal treatment vs. alternative periodontal treatment in 4 studies. |
Subjects:
7161 pregnant women
Exposure: Subjects with periodontitis or gingivitis Further features: Subjects in the first or second trimester of pregnancy (except in 2 studies); severity of periodontitis from moderate to severe |
Goal: Investigation of whether the treatment of gum disease can prevent unfavorable birth outcomes in pregnant women. |
Primary outcomes:
Perinatal outcomes (gestational age at birth, birth weight, low gestational age); maternal outcomes (mortality, preeclampsia, adverse effect of
therapy).
Secondary outcomes: Maternal outcomes (plaque values, gum health, changes in probing depth; changes in clinical attachment values) |
Inclusion criteria:
All randomized controlled trials investigating the effects of periodontal treatment on the prevention or reduction of perinatal and maternal morbidity
and mortality.
Exclusion criteria: Studies in which the obstetric results were not reported were excluded. |
| Manrique-Corredor et al., 2019 16 | Systematic review and meta-analysis |
Countries of the examined studies:
8 studies from America, 6 from Europe, 5 from Asia and 1 from Africa.
Intervention of the examined studies: – |
Subjects:
10215 pregnant women
Exposure: Periodontitis in pregnant woman |
Goal: Examination of the correlation between periodontitis and premature birth in women of childbearing potential. | Primary outcomes: Premature birth or no premature birth | Inclusion criteria: Inclusion of analytical case-control studies and prospective cohort studies. Studies had to express associations with ORs. English or Spanish articles have been taken into account. WHO definition of premature births. |
| Konopka et al., 2012 15 | Meta-analysis |
Countries of the examined studies:
8 studies from Europe, 7 from South America, 4 from North America and 3 from Asia.
Intervention of the examined studies: – |
Subjects:
12047 pregnant women
Exposure: Periodontitis in pregnant woman |
Goal: Examination of the influence of periodontitis on premature birth and low birth weight. | Primary outcomes: Premature birth before the 37th week of pregnancy; low birth weight below 2500 g | Inclusion criteria: Non-experimental, case-control prospective or cohort studies; exposure defined as maternal periodontitis; cases with premature birth prior to the 37th week of pregnancy or low birth weight below 2500 g; studies conducted in humans; only case parameters were used in periodontal studies; only one (earliest) study conducted by the same group of authors was considered. |
| Da Rosa et al., 2012 14 | Systematic review and meta-analysis |
Countries of the examined studies:
Studies come from Chile, USA, Iraq, India, Australia and Brazil.
Intervention of the examined studies: Treatment of periodontal disease compared to usual care. |
Subjects:
6988 pregnant women
Exposure: Pregnant women with gingivitis in which ≥ 25% of areas bleed during probing and areas with a clinical attachment loss of > 2 mm. Further features: Women over 18 years of age with a single pregnancy of 22 weeks or less. |
Goal: Examination of the correlation between periodontal effects, premature birth and low birth weight as well as the reasons for the ongoing controversy in this field. | Primary outcomes: Premature birth (< 37 weeks), low birth weight (< 2500 g) and/or low premature birth weight | Inclusion criteria: Studies had to specifically investigate treatments for periodontal diseases during pregnancy, compare the results of the usual treatment and the specific treatment, and report at least one outcome of interest. Including only randomized studies whose subjects met certain criteria. |
| Boutin et al., 2013 13 | Systematic review and meta-analysis |
Countries of the examined studies:
5 studies from the United States, 1 from Australia and 2 from Chile, 2 from Brazil, 1 from Iran and 1 from India.
Intervention of the examined studies: The intervention (periodontal treatment) consisted of root planing and superficial tartar removal (scaling) and was initiated in all studies prior to week 28 of pregnancy. |
Subjects:
7018 pregnant women
Exposure: Periodontal disease of the pregnant woman |
Goal: To investigate the effects of periodontal treatment on the risk of premature birth and to research the heterogeneity between studies. |
Primary outcome:
Premature birth, defined as a delivery before the 37th week of pregnancy.
Secondary outcome: Childbirth before the 35th and 32nd week of pregnancy, gestational age at birth, birth weight, low birth weight, defined as a birth weight below 2500 g, and very low birth weight, defined as a birth weight below 1500 g. |
Inclusion criteria:
RCTs in pregnant women with periodontal disease (all degrees of severity, including gingivitis) who received either periodontal treatment (scaling and
root planing) or no treatment. All comparators have been accepted.
Exclusion criteria: Studies that selected participants from a population of women with systematic or pregnancy-related health issues or who are at high risk of premature birth. |
| Polyzos et al., 2010 17 | Systematic review and meta-analysis |
Countries of the examined studies:
Studies from Chile, USA, Iran, India, Australia and Brazil.
Intervention of the examined studies: Pregnant women have been treated with scaling and root planing compared to no treatment or prophylaxis. |
Subjects:
6558 pregnant women
Exposure: Periodontal disease of the pregnant woman |
Goal: To investigate whether the treatment of periodontal disease is associated with scaling and root planing during pregnancy with a reduction in the rate of premature births. |
Primary outcome:
Premature birth (< 37 weeks)
Secondary outcomes: Low birth weight (< 2500 g), spontaneous abortions/stillbirths and overall adverse pregnancy outcomes (premature birth < 37 weeks and spontaneous abortions/stillbirths). |
Inclusion criteria:
Studies in which pregnant women were treated with scaling and root planing compared to no treatment or prophylaxis. Studies involving patients with
documented periodontal disease, regardless of the intensity and severity of the disease.
Exclusion criteria: Randomized studies that included patients at risk of premature birth who received labor inhibitors, and non-randomized and pseudo-randomized studies. |
| Moliner-Sánchez et al., 2020 8 | Systematic review and meta-analysis |
Countries of the examined studies:
Studies from Chile, USA, Malaysia, Brazil, Madagascar, India, Canada.
Intervention of the examined studies: – |
Subjects:
6768 pregnant women
Exposure: Periodontal disease of the pregnant woman Further features: Age of subjects between 18 and 40 years, participation in the study started between the 6th and 24th week of pregnancy. |
Goal: Analyze all evidence available in the scientific literature on the risk of premature birth and/or a low-birth-weight newborn in pregnant women with periodontal disease. | Primary outcomes: Premature birth and/or low birth weight. | Inclusion criteria: Cohort studies analyzing the relative risk of premature birth and/or low birth weight in pregnant women with periodontal disease. Studies that only describe the possible correlation between these variables, as well as those in which periodontal treatment was carried out during pregnancy. Periodontitis had to be clinically diagnosed in the women examined during pregnancy. |
Correlation between periodontal diseases, their treatment and birth outcomes
The meta-analyses and systematic reviews lead to heterogeneous results. Five of the seven examined meta-analyses and systematic reviews 4 13 14 15 17 found no significant correlation between periodontal disease and/or periodontal treatment with certain maternal and perinatal outcomes. For example, Iheozor-Ejiofor et al. 4 found that there is insufficient evidence to determine which periodontal treatment is best suited to prevent unfavorable obstetric consequences. Konopka et al. 15 also explained that the hypothesis that periodontitis is an independent risk factor for premature abortion and/or low birth weight had to be further examined. Rosa et al. 14 , on the other hand, found that the treatment of periodontal diseases during pregnancy cannot offer general protection against premature birth and low birth weight. Similar results were obtained by Boutin et al. 13 , who found that there was no significant reduction in the risk of premature birth due to periodontal treatment. Polyzos et al. 17 also confirmed this by showing that the treatment of periodontitis in pregnant women has no significant effect on the frequency of premature births. Two of the seven meta-analyses and systematic reviews examined, on the other hand, came to complementary results, since they showed correlations between periodontal diseases and certain maternal and/or perinatal outcomes. Thus, Manrique-Corredor et al. 16 found that the risk of premature birth is doubled by maternal periodontitis. Moliner-Sánchez et al. 8 showed a statistically significant correlation between periodontitis and the evaluated outcomes when the results were examined in connection with the per capita income of the countries. A detailed description of the central results of the studies can be found in Table 2 .
Table 2 Key results of the studies.
| Study | Endpoints | Results/conclusion |
| Iheozor-Ejiofor et al., 2017 4 | No clear difference in premature births < 37 weeks (RR 0.87, 95% CI 0.70–1.10) between periodontal treatment and no treatment. Low-quality evidence that periodontal treatment may reduce low birth weight < 2500 g (RR 0.67, 95% CI 0.48–0.95). It is uncertain whether periodontal treatment may result in a difference in premature birth < 35 weeks (RR 1.19, 95% CI 0.81–1.76) and < 32 weeks (RR 1.35, 95% CI 0.78–2.32), low birth weight < 1500 g (RR 0.80, 95% CI 0.38–1.70), perinatal mortality (including fetal and neonatal deaths up to the first 28 days after birth) (RR 0.85, 95% CI 0.51–1.43) and preeclampsia (RR 1.10, 95% CI 0.74–1.62). |
Total included studies:
15 RCTs
Results: When comparing pregnant women with periodontal gum disease who receive treatment to those who do not, there is no clear difference in the number of women receiving periodontal treatment before the 37th week of pregnancy, and fewer babies may be born weighing less than 2500 g (low-quality evidence). Conclusion: There is insufficient evidence to determine which periodontal treatment is better suited to prevent adverse obstetric outcomes. |
| Manrique-Corredor et al., 2019 16 | The meta-analysis gives an OR of 2.01 (95% CI 1.71, 2.36), which represents a significant positive correlation between the explanatory and the result variables. |
Total included studies:
20 studies
Results: The risk of premature birth is doubled by maternal periodontitis. Conclusion: Health and education centers should prioritize this risk factor and implement preventive measures for all women of childbearing potential in order to reduce the frequency of premature births. |
| Konopka et al., 2012 15 | The overall odds ratio for premature birth with a low-weight infant for mothers with periodontitis is 2.35 (1.88–2.93, p < 0.0001). For low birth weight, the total OR is 1.5 (95% CI: 1.26–1.79, p = 0.001), for premature births −2.73 (95% CI: 2.06–3.6, p < 0.0001). |
Total included studies:
15 case-control studies, 1 cross-sectional study and 6 cohorts of studies
Results: The hypothesis that periodontitis is an independent risk factor for premature termination of pregnancy and/or low body weight in newborns needs to be further examined. Conclusion: Dental care for pregnant women should be established as an integral part of the prenatal care program. |
| Da Rosa et al., 2012 14 | Treatment of periodontal disease during pregnancy has no significant effect on the overall birth rate of premature birth < 37 weeks (RR = 0.90, 95% CI: 0.68–1.19; p = 0.45; I2: 74%). There is a weak correlation between the treatment of periodontal disease during pregnancy and the reduction of low birth weight < 2500 g, and without a significant effect (RR = 0.92, 95% CI: 0.71–1.20; p = 0.55; I2: 56%). |
Total included studies:
Outcome premature births: 13 studies included; outcome low birth weight: 9 studies.
Results: Treatment of periodontal disease during pregnancy cannot provide general protection against premature birth and low birth weight. Conclusion: Primary periodontal treatment during pregnancy cannot reduce the rate of premature birth or low birth weight. |
| Boutin et al., 2013 13 | A non-significant correlation between periodontal treatment and premature birth (RR: 0.89; 95% CI: 0.73–1.08) can be determined. Daily use of chlorhexidine mouthwashes is associated with a reduction in premature birth rate (RR: 0.69, 95% CI 0.50–0.95). |
Total included studies:
12 studies
Results: No significant reduction in the risk of premature birth due to periodontal treatment with tartar removal (scaling) and root planing. However, the mean gestational age and mean birth weight in the intervention groups is significantly higher than in the comparison groups. Conclusion: Chlorhexidine mouthwash as a preventive agent should be further examined. |
| Polyzos et al., 2010 17 | In the high-quality studies, the treatment has no significant effect on the overall rate of premature births (OR 1.15, 95% CI 0.95–1.40; p = 0.15). Treatment does not result in a reduction in the rate of low birth weight infants (OR 1.07, 0.85–1.36; p = 0.55), spontaneous abortions/stillbirths (0.79, 0.51–1.22; p = 0.28) or overall adverse pregnancy outcomes (premature births < 37 weeks and spontaneous abortions/stillbirths) (1.09, 0.91–1.30; p = 0.34). |
Total included studies:
11 studies
Results: Treatment of periodontitis with tartar removal (scaling) and root planing in pregnant women has no significant effect on the incidence of premature births. Low-quality studies indicated a positive effect of the treatment, while high-quality studies clearly show that there is no such effect. Conclusion: Treatment of periodontal disease with tartar removal (scaling) and root planing cannot be considered an effective means of reducing premature birth rates. |
| Moliner-Sánchez et al., 2020 8 | Statistically significant values (RR = 1.67 [1.17–2.38], 95% CI) and low birth weight (RR = 2.53 [1.61–3.98], 95% CI) are determined for the risk of premature birth in pregnant women with periodontitis. A meta-regression, in which these results are related to the income level of the individual countries, gives statistically significant values for premature birth RR = 1.8 (1.43–2.27) 95% CI and for low birth weight RR = 2.9 (1.98–4.26) 95% CI. The risk of premature birth in women with periodontitis is increased by 1.67 times and the risk of a newborn with low birth weight by 1.42 times (evidence level 2a). |
Total included studies:
11 studies
Results: A statistically significant correlation between periodontitis and the two birth complications studied is found when examining the relationship between these results and the country’s per capita income. Conclusion: These results may not only be due to income, but also due to other factors such as educational attainment, and should therefore be examined in more detail in future studies. |
Evaluation of the quality of the included studies
The quality of the included meta-analyses and systematic reviews can be classified as sufficient according to the AMSTAR checklist, resulting in an average level of evidence. The questions of the checklist can in some cases be answered with yes . Weaknesses in the quality of the included studies result from a priori planning/definition (classified as Uncertain in 6 studies) as well as grey and unpublished literature included in the studies (classified as Uncertain in all studies). Similarly, six studies present only the references of the included studies, but not of the excluded studies. In addition, three out of seven studies do not provide information on a potential conflict of interest. All other seven questions of the checklist could be consistently assessed as yes in all included studies. The results of this evaluation are shown in Table 3 .
Table 3 Evaluation of the quality of the included studies according to the AMSTAR checklist.
| Study | A priori planning/definition | Study selection/extraction of 2 independent persons | Comprehensive systematic literature search | Unpublished and grey literature included | References of the included and excluded literature | Study characteristics indicated | Risk of distortion assessed | Risk of distortion taken into account in the interpretation of results | Statistically adequate evaluation | Potential publication bias addressed | Potential conflicts of interest addressed |
| Iheozor-Ejiofor et al., 2017 4 | Yes | Yes | Yes | Uncertain | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Manrique-Corredor et al., 2019 16 | Uncertain | Yes | Yes | Uncertain | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Konopka et al., 2012 15 | Uncertain | Yes | Yes | Uncertain | No | Yes | Yes | Yes | Yes | Yes | No |
| Da Rosa et al., 2012 14 | Uncertain | Yes | Yes | Uncertain | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Boutin et al., 2013 13 | Uncertain | Yes | Yes | Uncertain | No | Yes | Yes | Yes | Yes | Yes | No |
| Polyzos et al., 2010 17 | Uncertain | Yes | Yes | Uncertain | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Moliner-Sánchez et al., 2020 8 | Uncertain | Yes | Yes | Uncertain | No | Yes | Yes | Yes | Yes | Yes | Yes |
Discussion
Summary of results
A total of seven meta-analyses and systematic reviews 4 8 13 14 15 16 17 were included in the narrative review (n = 56755). The examined studies of the meta-analyses and systematic reviews used periodontal treatment vs. no treatment as an intervention, or they investigated the correlation between periodontal diseases and negative birth results. The studies came to heterogeneous results, whereby the majority of the examined meta-analyses and systematic reviews 4 13 14 15 17 do not find a significant correlation between periodontal disease and/or periodontal treatment with certain maternal and/or perinatal outcomes. A medium level of evidence may be assumed based on the AMSTAR assessment.
Embedding in the state of research
Periodontal diseases are discussed as a risk factor for premature births and/or low birth weight. Nevertheless, there is little consensus on the extent to which periodontal treatment in pregnancy can prevent or reduce negative birth outcomes 14 . However, most of the studies included here did not confirm the correlation between periodontal health and risk of premature birth or risk of negative maternal or perinatal outcomes. It should be noted that only two of the seven meta-analyses examined indicated significant correlations with regard to an increase in risk in the case of deficient oral health 8 16 . Both studies were published in 2019 and 2020, and were therefore younger than those meta-analyses (including the included Cochrane review 4 ), which did not postulate any significant correlations. For the benefit of periodontal treatment in terms of risk reduction for premature birth and negative outcomes, there was no clear evidence of efficacy 13 14 17 . According to the AMSTAR assessment, a medium quality is indicated for all included studies, so whether oral health influences the risk of premature birth or the risk of negative outcomes cannot be conclusively assessed.
Other reviews arrive at similar results: Teshome and Yitayeh also conducted a systematic review, which analyzed the correlation between periodontal disease and low premature birth weight. It was found that periodontal disease could be a possible risk factor for premature births with low birth weight, but further studies would be necessary 18 . Ide and Papapanou also show that maternal periodontitis is slightly but significantly related to low birth weight and premature birth. However, the results are influenced by the exposure definition of periodontitis 19 . The same can be found in the present narrative review. The heterogeneity of the classifications of the severity of periodontal disease causes difficulties, both in the meta-analyses and systematic reviews themselves, as well as in the studies considered therein. López et al. also reported something similar in a review. They found that those people included in studies who showed a positive effect of the treatment of periodontitis on premature birth were not based on consistent scientific findings 20 . Rangel-Rincón et al. also showed in their review that the different findings are not sufficient to demonstrate that the frequency of undesirable pregnancy outcomes in pregnant women receiving periodontal treatment decreases significantly 21 .
It should also be noted that premature birth and other outcomes considered here represent multifactorial events. Risk factors such as smoking, low socio-economic status, maternal age and ethnicity can promote both periodontitis and premature birth. This can lead to misinterpretation of the data, as there may be no causal relationship between the outcomes examined and periodontitis 4 . The results of this narrative review underline the results of some systematic reviews, which focus on the same topic. There is insufficient evidence to conclusively assess the correlation between periodontal disease and negative birth outcomes.
Limitations
The present study also showed some limitations, which resulted, on the one hand, from the methodological approach and, on the other hand, from the included studies. One limitation was that only English-language articles were included in the review, which can lead to distortion. Despite the independent search of three authors, it remains uncertain whether all relevant studies could really be identified. With regard to the limitations of the included studies, reference should be made to the heterogeneity of the included meta-analyses and systematic reviews. This was calculated in all meta-analyses, which in some cases led to significant values and considerably restricted the comparability of the results. Many of the meta-analyses examined here also demonstrate publication distortion. In addition, there is no consensus about which time of the dental examination is considered suitable in pregnancy 4 . It is also critical to note that in some studies, subjects who have experienced premature birth were also included during a previous birth, which was insufficiently taken into account in the examinations from a statistical standpoint 4 . In addition, the periodontal treatments in the studies are very diverse, which makes comparability difficult. The meta-analyses and systematic reviews also include different study designs. For example, in some papers, only randomized studies were considered 4 13 14 17 , while others also included observational studies 8 15 16 . It should also be noted that some of the included meta-analyses partially evaluated the same studies. However, the meta-analyses each examine further, differing studies, which is why these were nevertheless included separately in this narrative review. It should be noted that Polyzos et al. 17 and Boutin et al. 13 investigated similar studies and presented similar results. Despite the limitations, the results outlined here can be described as an extension of the state of research due to the overall high total number of subjects (n = 56755) and the inclusion criterion of the meta-analyses and systematic reviews.
Answering the research questions
Based on the results, the above research questions can be answered as follows:
How can the correlation between periodontal disease in pregnant women and pregnancy complications be assessed using meta-analyses and systematic reviews? Periodontitis as a risk factor for premature birth must be further examined, since heterogeneous study results are available, some of them of inadequate quality. However, one of the examined studies indicates that the risk of premature birth doubles in the presence of maternal periodontitis 16 . Another examined study shows a significant correlation between periodontitis and certain maternal and perinatal outcomes when the results are analyzed in relation to the countries’ per capita income 8 . Here, however, it remains uncertain whether periodontitis really has an influence on the risk of premature birth, or an existing low socio-economic status, which as a risk factor influences both the risk of premature birth and the risk of poor dental health 22 23 .
How can the efficacy of periodontal treatment vs. no treatment in pregnant women with periodontal disease be assessed in terms of premature birth and other negative birth outcomes (see definition below) using meta-analyses and systematic reviews? The majority of the examined meta-analyses and systematic reviews show that there is no significant correlation between periodontal treatment and certain maternal and perinatal outcomes 4 13 14 17 . There is insufficient evidence 4 to determine which periodontal treatment is best suited to avoid negative obstetric consequences. Periodontal treatment during pregnancy does not significantly reduce the risk or frequency of premature birth 13 14 17 and low birth weight 14 .
Conclusion
Most of the included studies indicate that there is no significant correlation between dental health and the risk of premature birth or negative maternal and perinatal outcomes or between periodontal treatments during pregnancy and the reduction of the risk of premature birth. However, the quality of the studies is not high enough to be able to record this with a high level of evidence. To improve the evidence level, further randomized controlled trials must be conducted to systematically control the bias. Nevertheless, it is recommended that all pregnant women be advised to improve daily oral hygiene, so that this is promoted and inflammatory diseases can be counteracted by preventive efforts. This should be a routine part of health advice, irrespective of pregnancy. In the context of a benefit/harm assessment, the treatment of periodontitis based on an individualized risk assessment is recommended in pregnant women, since in many cases periodontal treatment leads to an improvement in periodontal health. Since, as part of the reformulation of the German Midwifery Act, midwives will also be asked to provide evidence-based advice and care in future, the results of the present paper are equally relevant for both gynecologists and midwives 24 .
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References/Literatur
- 1.Berens N. Marburg: Medizinisches Zentrum für Zahn-, Mund- und Kieferheilkunde der Philipps-Universität Marburg; 2018. Mundgesundheit von Patientinnen mit Schwangerschaftskomplikationen und Anzeichen einer Frühgeburt: Klinische und mikrobiologische Kohortenstudie [Dissertation] [Google Scholar]
- 2.Deutsche Gesellschaft für Gynäkologie und Geburtshilfe ; Österreichische Gesellschaft für Gynäkologie und Geburtshilfe ; Schweizerische Gesellschaft für Gynäkologie und Geburtshilfe . S2k-Leitlinie Prävention und Therapie der Frühgeburt (Version 1.1. 02/2020) 2020. https://www.awmf.org/uploads/tx_szleitlinien/015–025l_S2k_Praevention-Therapie_Fruehgeburt_2020–02.pdf https://www.awmf.org/uploads/tx_szleitlinien/015–025l_S2k_Praevention-Therapie_Fruehgeburt_2020–02.pdf
- 3.Gätje R, Eberle C, Scholz C, Lübke M, Solbach C, Muschel K, Kissler S, Siedentopf F, Weißenbacher T, Debus G, Schuhmacher I, Sänger N. 2. Stuttgart: Thieme; 2011. Kurzlehrbuch Gynäkologie und Geburtshilfe. [Google Scholar]
- 4.Iheozor-Ejiofor Z, Middleton P, Esposito M et al. Treating periodontal disease for preventing adverse birth outcomes in pregnant women. Cochrane Database Syst Rev. 2017;(06):CD005297. doi: 10.1002/14651858.CD005297.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Opacic J, Maldonado A, Ramseier CA et al. Einfluss der Parodontitis auf Schwangerschaft und Geburt. Swiss Dental Journal SSO. 2019;129:581–589. doi: 10.61872/sdj-2019-07-08-03. [DOI] [PubMed] [Google Scholar]
- 6.Ärzteblatt . Weltweit mehr als 15 Millionen Frühgeborene – Tendenz steigend. 2012. https://www.aerzteblatt.de/nachrichten/50057/Weltweit-mehr-als-15-Millionen-Fruehgeborene-Tendenz-steigend https://www.aerzteblatt.de/nachrichten/50057/Weltweit-mehr-als-15-Millionen-Fruehgeborene-Tendenz-steigend
- 7.Rath W, Schmidt S. Iatrogene Frühgeburt. Z Geburtshilfe Neonatol. 2011;215:131–132. doi: 10.1055/s-0031-1285843. [DOI] [PubMed] [Google Scholar]
- 8.Moliner-Sánchez CA, Iranzo-Cortés JE, Almerich-Silla JM et al. Effect of per Capita Income on the Relationship between Periodontal Disease during Pregnancy and the Risk of Preterm Birth and Low Birth Weight Newborn. Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2020;17:8015. doi: 10.3390/ijerph17218015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daalderop LA, Wieland BV, Tomsin K et al. Periodontal Disease and Pregnancy Outcomes: Overview of Systematic Reviews. JDR Clin Trans Res. 2018;3:10–27. doi: 10.1177/2380084417731097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ressing M, Blettner M, Klug S.Systematische Übersichtsarbeiten und Metaanalysen. Teil 6 der Serie zur Bewertung wissenschaftlicher Publikationen Dtsch Arztebl Int 2009106456–463.19652768 [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J et al. Bevorzugte Report Items für systematische Übersichten und Meta-Analysen: Das PRISMA-Statement. Dtsch Med Wochenschr. 2011;136:e9–e15. [Google Scholar]
- 12.Schmucker C, Nothacker M, Möhler R, Kopp I, Meerpohl JJ. Freiburg, Marburg: Cochrane Deutschland, Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften – Institut für Medizinisches Wissensmanagement; 2017. Bewertung von systematischen Übersichtsarbeiten: ein Manual für die Leitlinienerstellung. [DOI]
- 13.Boutin A, Demers S, Roberge S et al. Treatment of periodontal disease and prevention of preterm birth: systematic review and meta-analysis. Am J Perinatol. 2013;30:537–544. doi: 10.1055/s-0032-1329687. [DOI] [PubMed] [Google Scholar]
- 14.Da Rosa MI, Pires PDS, Medeiros LR et al. Periodontal disease treatment and risk of preterm birth: a systematic review and meta-analysis. Cadernos de Saúde Pública. 2012;28:1823–1833. doi: 10.1590/s0102-311×2012001000002. [DOI] [PubMed] [Google Scholar]
- 15.Konopka T, Paradowska-Stolarz A. Periodontitis and risk of preterm birth and low birthweight – a meta-analysis. Ginekologia Polska. 2012;83:446–453. [PubMed] [Google Scholar]
- 16.Manrique-Corredor E, Orozco-Beltran D, Lopez-Pineda A et al. Maternal periodontitis and preterm birth: Systematic review and meta-analysis. Community Dent Oral Epidemiol. 2019;47:243–251. doi: 10.1111/cdoe.12450. [DOI] [PubMed] [Google Scholar]
- 17.Polyzos NP, Polyzos IP, Zavos A et al. Obstetric outcomes after treatment of periodontal disease during pregnancy: systematic review and meta-analysis. BMJ. 2010;341:c7017. doi: 10.1136/bmj.c7017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Teshome A, Yitayeh A. Relationship between periodontal disease and preterm low birth weight: systematic review. Pan Afr Med J. 2016;24:215. doi: 10.11604/pamj.2016.24.215.8727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ide M, Papapanou P. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes – systematic review. J Periodontol. 2013;84:181–194. doi: 10.1902/jop.2013.134009. [DOI] [PubMed] [Google Scholar]
- 20.López NJ, Uribe S, Martinez B. Effect of periodontal treatment on preterm birth rate: a systematic review of meta-analyses. Periodontol 2000. 2015;67:87–130. doi: 10.1111/prd.12073. [DOI] [PubMed] [Google Scholar]
- 21.Rangel-Rincón LJ, Vivares-Builes AM, Botero JE et al. An Umbrella Review Exploring the Effect of Periodontal Treatment in Pregnant Women on the Frequency of Adverse Obstetric Outcomes. J Evid Based Dent Pract. 2018;18:218–239. doi: 10.1016/j.jebdp.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Hidalgo-Lopezosa P, Jiménez-Ruz A, Carmona-Torres JM et al. Sociodemographic factors associated with preterm birth and low birth weight: A cross-sectional study. Women Birth. 2019;32:e538–e543. doi: 10.1016/j.wombi.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 23.Lee JH, Lee JS, Choi JK et al. National dental policies and socio-demographic factors affecting changes in the incidence of periodontal treatments in Korean: A nationwide population-based retrospective cohort study from 2002–2013. BMC Oral Health. 2016;16:118. doi: 10.1186/s12903-016-0310-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graf J, Weinert K, Plappert CF et al. Evidenzbasierte Hebammenkunde: Implikationen für Lehre, Praxis und Wissenschaft. HebammenWissen. 2021;2:50–53. [Google Scholar]