Abstract
Biweekly county COVID-19 data were linked with Longitudinal Employer-Household Dynamics data to analyze population risk exposures enabled by pre-pandemic, country-wide commuter networks. Results from fixed-effects, spatial, and computational statistical approaches showed that commuting network exposure to COVID-19 predicted an area's COVID-19 cases and deaths, indicating spillovers. Commuting spillovers between counties were independent from geographic contiguity, pandemic-time mobility, or social media ties. Results suggest that commuting connections form enduring social linkages with effects on health that can withstand mobility disruptions. Findings contribute to a growing relational view of health and place, with implications for neighborhood effects research and place-based policies.
Keywords: Commuting networks, COVID-19, Fixed-effects, Spatial models, Computational statistics, Mobility data
1. Introduction
Research developments on how neighborhoods affect health (Arcaya et al., 2016; Diez Roux, 2001) offer great insights for understanding the community context of health behaviors and outcomes during the current COVID-19 pandemic. Community-level forces associated with COVID-19 include age structure (Dowd et al., 2020), population density (Sy et al., 2021), and racial composition (Millett et al., 2020). Such studies however, often treat places as bounded areas, separated by physical distance, and with largely stable residential communities. However, a growing relational turn in the literature on health and place sees places as nodes in broader networks, separated by socio-relational distances, and shaped by routine mobility of populations (Cummins et al., 2007, p. 1827; Sampson, 2012).
During the pandemic and long before, scholars of health, place, and neighborhoods effects have highlighted the need for a deeper understanding of place-to-place exposures to health risk through routine population mobility networks (Bavel et al., 2020; Block et al., 2020), based on activities located in non-residential environments (Browning et al., 2017; Krivo et al., 2013; Matthews and Yang, 2013; Sampson, 2012). The rapid spread of COVID-19 across the country painfully illustrates the significance of this critical, yet insufficiently understood, relational perspective. It underscores the urgent need for studies to move beyond local (within place) factors, and begin to prioritize the role of extra-local (between places) exposures to health risk (Berkman et al., 2014; Browning et al., 2017; Kuchler et al., 2021; Newmyer et al., 2022). The current study addresses this need and takes a relational approach to examining the role of place-to place commuting networks on an area's COVID-19 outcomes across space and time.
A growing number of COVID-19 studies have examined human mobility as a part of a community's risk exposures (Cartenì et al., 2020; Fazio et al., 2022; Pluchino et al., 2021; Weill et al., 2020), but data accessibility and computational costs greatly limit the ability of analyses to take a truly relational approach to understand place-to-place mobility that contributes to a community's exposures to high-risk areas across the country. Moreover, studies that examined the role of workplaces (e.g., Jay et al., 2020), have focused on the effects of distancing from work areas in general (vs. other types of sites). Yet, when people commute to specific high-risk workplace areas, their health behaviors and COVID-19 outcomes at home may be affected as well (Bavel et al., 2020; Kang et al., 2020). The current study thus seeks to contribute to the literature and address these gaps by first, taking an explicitly relational approach that allows for a more nuanced understanding of dyadic, county-to-county flows and their associations with local COVID-19. Second, it analyzes the role of commuting to workplace areas while accounting for the strengths of these flows and the levels of COVID-19 in the connected work areas.
Commuting represents an important place-to-place form of population mobility through which diseases can be transmitted to new populations (Balcan et al., 2009; Viboud et al., 2006). Millions of people commute every day in the US (McKenzie, 2015). The workplace, where people spend great portions of their days, is a key environment of exposure to risk and resources (Deziel et al., 2020; Lan et al., 2020), even when mobility is restricted through policies and interventions. For these reasons, local and state-level COVID-19 mitigation and prevention policies and guidelines have involved social and physical distancing recommendations, including telecommuting for work. As a result, many workers were able to switch to remote work; with some studies indicating about a third of workers doing so early in the pandemic (Rafiq et al., 2022). However, those who started telecommuting continued to communicate remotely. Moreover, a large share of the population continued to commute for work due to working in essential or frontline jobs or due to lack of access to remote resources such as high-speed internet (Chiou and Tucker, 2020; Tomer and Kane, 2020; Weill et al., 2020). Therefore, the predominant focus of prior research on the effects of stay-at-home policies and declines in mobility has been very important but has also left largely unanswered fundamental questions about the extent to which, despite disruptions in mobility, the commuting flows established before the pandemic continued, through enduring connections (direct or remote), to impact the spread of COVID-19.
This is an important gap because, without fully understanding the role of place-to-place commuting on health risk, the impact of local health promotion or risk prevention policies may be severely diluted through a place's exposures to high-risk in its connected communities. The current study aims to address this gap by examining the extent to which the roles of commuting ties, from before and during the pandemic, are unique from the influence of other neighboring areas, pandemic-time mobility disruptions, or social media links.
2. Theoretical and empirical background: pandemic and pre-pandemic commuting
Despite pandemic lockdowns, many people that commuted before the pandemic continued to travel to work due to the nature of their jobs or because they could not afford to work from home. Indeed, as the COVID-19 pandemic hit the US in 2020, about 60% of US workers found themselves in essential jobs and about 34% in frontline jobs that could not be performed from home (Tomer and Kane, 2020). Additionally, populations of lower socioeconomic status or with lower access to high-speed internet were less able to telecommute during the pandemic. (Chiou and Tucker, 2020; Jay et al., 2020; Weill et al., 2020). For these reasons, despite social distancing policies and other disruptions (De Vos, 2020) work-related transmission was found to account for close to half of COVID-19 outbreaks early in the pandemic (Lan et al., 2020).
Importantly, workplaces facilitate not only physical transmission of diseases through in person contacts but also the social transmission of health-relevant information and norms, which have been found to influence people's preventive behavior and health outcomes (Berkman et al., 2014; Zhang and Centola, 2019). As co-workers are often among people's close friends and confidants (Christakis and Fowler, 2008; Marks, 1994), social contacts at work have been shown to impact health behaviors, like quitting smoking (Christakis and Fowler, 2008), adopting a healthier diet (Buller et al., 2000), and risky behaviors in workers' households (Bolger et al., 1989; Taylor et al., 1997). Work environments where distancing and facemasks are normative may influence commuters to practice similar safe behaviors in home communities.
Therefore, to the extent that commuting networks facilitated in-person ties and risk exposures (physical or social) among those who continued to travel to work during the pandemic, we hypothesize that COVID-19 exposures through commuting ties (adjusted for pandemic disruptions) affected local COVID-19, net of local mobility or geographic contiguity.
Even in the absence of in-person contact among those who telecommuted during parts of the pandemic, work and personal ties were likely maintained using the Internet and social media platforms. Online communication and digital media was shown to facilitate the maintenance of in-person social contacts and the remote exchange of health information and social support (Bavel et al., 2020; Zhang and Centola, 2019). For instance, the spread of misinformation through social media has contributed to disease outbreaks such as Ebola (Allgaier and Svalastog, 2015) and to the adoption of unhealthy behaviors like vaping (Allem et al., 2017). Recently, Facebook connections were shown to be associated with county COVID-19 outbreaks (Kuchler et al., 2021). Prior studies that focused primarily on the effects of pandemic changes in physical mobility of populations (e.g., Weil et al., 2020; Jay et al., 2020) are, thus, likely to miss key dynamics of influence related to pre-existing in-person connections gone digital. The current study seeks to bridge these gaps by examining pre-pandemic commuting network patterns.
Therefore, to the extent that commuting networks forged before the pandemic facilitated remote social ties and exposures that bypassed physical distancing between residential and work communities, we hypothesize that pre-pandemic commuting ties functioned as significant pathways for the spread of COVID-19, independent of pandemic-time mobility disruptions.
3. Current study
Overall, the current study seeks to contribute theoretically and advance a relational perspective of health and place (Bavel et al., 2020; Berkman et al., 2014; Browning et al., 2017; Kuchler et al., 2021) by investigating how local COVID-19 cases and deaths are affected by commuters’ prior COVID-19 risk exposures in their specific work environments. It aims to understand the preexisting place-to-place transmission structures that enabled the fast and wide spread of COVID-19 across the country despite stay-at-home orders and increased remote work.
The study integrates methodological advances in population health, neighborhood effects, social epidemiology, and computational sociology (such as the operationalization of network measures and applications of negative binomial models, spatial-network regression models, permutation approaches, leave-one-out cross validation). These techniques allow us to account for spatial and the more complex, network dependencies within the data. The study uses origin-destination linkage information, i.e., comprehensive commuting flows between the residential and workplace locations and conceptualizes commuting as network ties of various strengths between counties, part of macro-level network systems forged before the pandemic. In addition, we draw on SafeGraph's smart-phone based mobility data, Google's Mobility Reports, and Facebook's Social Connectivity Index (SCI) to better understand the unique contributions of commuting-network diffusion to COVID-19 outcomes.
Among the COVID-19 studies so far, those that examined mobility flows have tended to rely on cell phone data (Chang et al., 2021; Jay et al., 2020; Weill et al., 2020). However, approaches using such data inevitably reflect only a small percentage of a community's population, over-representing young and affluent groups (Kang et al., 2020), and use rough estimates of workplace locations (Jay et al., 2020). Our study addresses these important limitations in several ways. First, we created measures based on a uniquely comprehensive commuting data that covers most US working population, of all ages and socioeconomic statuses. Moreover, we used formal workplace locations, as reported by the states to the Census Bureau - information from unemployment insurance forms submitted by businesses and organizations across the US.
4. Methods, data, and measures
4.1. COVID-19 network and spatial exposure measures
We examined COVID-19 confirmed cases and deaths from the USA Facts database, which integrates data from the Centers for Disease Control and Prevention (CDC), state-, and local-level public health agencies. We analyzed data based on twenty-three 2-week intervals between April 1st, 2020,1 and February 16th, 2021 (N = 62,445 county-time periods), within 2715 counties (those with complete data on relevant covariates), and 49 states (and Washington, D.C.).2 The outcomes are new COVID-19 cases and deaths within each county-time period.3
Network-weighted and spatially-weighted exposures to COVID-19 are based on case rates from the prior time period. In our study, these measures capture social and geographic proximity to COVID-19, respectively. Data on inter-county commuting, used to construct the network weighted average COVID-19 exposure risk index (or Network COVID-19), were based on the Longitudinal Employer-Household Dynamics (LEHD) Origin-Destination Employment Statistics (LODES) 2018 dataset,4 from the U.S. Census Bureau (Abowd et al., 2005).5 Formulas for the network and spatial exposure measures are shown in Equations (Eq. 1), (Eq. 2)).
| (Eq. 1) |
| (Eq. 2) |
Network COVID-19 exposure was based on Equation (1), where a given home county (h) is connected to W work counties. represents the number of commuters from county h who commute to county w, while represents the total number of outgoing commuters from county h. Within-county commuters is excluded from this measure. Spatially weighted exposure risk (Spatial COVID-19) was based on the average rate of COVID-19 cases of all queen-contiguous counties (e.g., Equation (2) for a county h that is queen-contiguous to B bordering counties). We incorporate a temporal lag into the construction of both exposure measures by using cases from the prior two-week period to account for both physical processes (e.g., COVID-19 case incubation) and social processes (e.g., time to observe and implement new behaviors).
4.2. Google-based measures of work-related mobility during the pandemic
We used the Community Mobility Reports (CMR) data from Google to control for local variation in mobility across the pandemic, likely driven both by government-enforced lockdowns and public health guidance. The CMR aggregate information about daily visits and length of stay, focusing on how mobility changed from a pre-pandemic baseline (here, January 3 – February 6), based on a sample of Google accounts, depending on location history settings, specific user settings, connectivity, and privacy requirements.6 We averaged the daily data both geographically (by county) and temporally, matching the same lagged, two-week units as the network and spatial exposure measures. When possible, missing data were interpolated using the time periods immediately before and after for the corresponding county. For comparability with the commuting data, we focused in on mobility trends for places of work. As such, this variable captures the level of work-related mobility throughout the study period, relative to a pre-pandemic baseline, and was included in all models as a control (“local work mobility”).7 More positive values convey greater mobility, while more negative values convey less mobility.
4.3. Cellphone mobility and social media ties measures
We also use measures of human mobility or intercounty social linkages based on independent data to assess the extent to which the role of commuting is unique from these.
Smart-phone based mobility and distancing measures. Using SafeGraph data,8 we capture intercounty visitor home-to-business travel flows for the entire US based on aggregations of over 6 million point-of-interest business locations combined with foot-traffic information anonymized from GPS location from smart phone applications. As such, in addition to capturing mobility changes over the course of the pandemic, a key benefit of the SafeGraph data is its inclusion of travel to locations not related to work (e.g., restaurants and gathering places) that may facilitate COVID-19 spread. First, we created a weighted network average of COVID-19 case rate based on proportion of outgoing travelers forming each tie to a home county (“SafeGraph network”). Next, we created a new, pandemic-adjusted version of the original LEHD network using the SafeGraph data by weighting each commuting tie (between county pairs, as used in the original network exposure to COVID-19) during a specific month by the % of the SafeGraph change in traffic that same month, relative to the SafeGraph mobility in the corresponding month one year before the pandemic.9 We then standardized and subtracted this dynamic network exposure measure from the pre-pandemic measure of COVID-19 network exposure (based on the LEHD commuting data also aggregated to the 10 months of our study). The resulting network exposure difference (pre-pandemic influence) estimates portions of the commuting network exposure effect related to enduring social ties of pre-pandemic origin (e.g., co-worker relationships that continued to influence health behaviors throughout COVID-19).
Social media connectivity measures. We utilize the Facebook Social Connectedness Index (SCI) is based on anonymized users of Facebook and their friendship links to other users who have interacted with Facebook over the 30 days prior to August 2020, all assigned to locations according to their Facebook activity and their device and connection data. The publicly available measures are aggregated and summarized as links across pairs of counties and include random noise to prevent user identification (Bailey et al., 2018; Facebook, 2018). We constructed a measure of county COVID-19 exposure through these social media ties data, applying a similar logic as that of the LEHD network exposure. For each county, we measured “outgoing” connections and weight each connected county's contribution based on the proportion of these outgoing ties it represents. More details on these measures and data are in the Methods Supplement.
4.4. County-level covariates
We include a number of sociodemographic control variables likely relevant to COVID-19 outcomes.10 These county-level measures were largely drawn from the 2014–2018 American Community Survey (ACS) 5-year estimates and are considered to be time-invariant for the study period. They include economic disadvantage, measured as the first principal component transformation produced from a principal components analysis of unemployment rate, median income, percent in poverty, percent single female-headed family households, percent college graduates (aged at least 25), percent occupied housing units that are owner-occupied, and percent vacant housing units (eigenvalue = 3.2 among all US counties). Communities with lower socioeconomic status can have more pre-existing health conditions, less access to healthcare, less access to high-speed internet that could enable remote work, and are less able to engage in social distancing (Chiou and Tucker, 2020; Weill et al., 2020). We also control the percent of residents 65 years or older and binary indicators of whether the county is above average, compared to all counties in the ACS, regarding (1) percentage of the population that is non-Hispanic White, (2) percentage of the population that is non-Hispanic Black, and (3) percentage of the population that is Hispanic. Finally, we include a measure of the percent of the county population with urban residence, as measured in the 2010 US Census. Table 1 displays descriptive statistics for all variables.
Table 1.
Descriptive statistics for entire analytic sample (unstandardized).
| Mean | SD | Min. | Max. | |
|---|---|---|---|---|
| Outcomes | ||||
| COVID-19 confirmed cases (count) | 429.6 | 2148.9 | .0 | 189592.0 |
| COVID-19 deaths (count) | 7.5 | 41.9 | .0 | 3086.0 |
| COVID-19 confirmed cases (rate) | 374.6 | 451.9 | .0 | 13726.1 |
| COVID-19 deaths (rate) | 7.0 | 12.1 | .0 | 283.3 |
| Predictors | ||||
| Network lagged confirmed case rate | 364.2 | 368.7 | 1.8 | 3016.4 |
| Spatially lagged confirmed case rate | 355.2 | 397.4 | .0 | 4464.8 |
| Change in local work mobility | −24.9 | 9.5 | −77.0 | 40.2 |
| Economic disadvantage | .0 | 1.7 | −6.2 | 8.4 |
| % 65 and older | 17.9 | 4.2 | 3.8 | 55.6 |
| Above avg. non-Hispanic White | .63 | – | .0 | 1.0 |
| Above avg. non-Hispanic Black | .30 | – | .0 | 1.0 |
| Above avg. Hispanic | .21 | – | .0 | 1.0 |
| % Urban population | 46.6 | 29.6 | .0 | 100.0 |
Notes: N = 62,445 county-time periods, nested within 2715 counties, in 50 states (includes DC, excludes Alaska).
4.5. Analytic strategy
Fixed and mixed effects models. We utilize fixed effects negative binomial models and two-level mixed effects negative binomial models. Negative binomial models, as opposed to Poisson, are useful in modeling over-dispersed count outcomes, especially when outcomes are relatively rare. First, we estimate fixed effects models to focus only on within-county variation in COVID-19 outcomes, as predicted by each county's network exposure, spatial exposure, and local work mobility. Next, we estimate two-level mixed effects models to incorporate between-county variation as well, allowing for the inclusion of theoretically relevant, county-level predictors. Further details are provided in the Methods Supplement. Convergent results across these two modeling strategies with regard to the influence of network exposure, described in the following section, strengthen our confidence in the study's findings.
Due to the high correlation between commuting network COVID-19 exposure and spatial COVID-19 exposure (see Equations (Eq. 1), (Eq. 2))), we also replicate each model using a “split network” approach in which the network exposure measure is constructed two different ways: (a) using only commuting ties between counties that are spatially queen-contiguous and (b) using only commuting ties between counties that are not spatially queen-contiguous. These models help to separate network effects from possible unmeasured spatial confounders. Consistency in network spillover estimates across network configurations lends confidence that our results are not unduly influenced by collinearity between spatial and network COVID-19 spillovers.
Permutations and model fit comparisons. We next utilize permutation testing of predictor significance, a flexible, simulation-based approach (Breiman, 2001). This strategy avoids distributional and independence assumptions about model error, on which traditional statistical tests of significance rely. Due to the multiple interdependencies inherent to our data (network exposure to COVID-19, cf. Equation (1), and spatial exposure to COVID-19, cf. Equation (2)), permutation tests serve as a useful robustness check of the regression-based results. For each predictor, we conduct a set of permutations in which the values of the predictor are randomly permuted across all observations, breaking any association with COVID-19 outcomes and generating a distribution of what model error would look like if the predictor had no effect. The observed error is then compared to this distribution in order to assess that predictor's contribution to model fit. We use mean arctangent absolute percentage error (MAAPE) to measure average model error. To assess the contribution of the network measure to overall model performance, we also compare models using fit statistics like AIC, BIC, and MAAPE calculated with leave-one-out cross validation (LOOCV-MAAPE). Further details are in the Methods Supplement.
Spatial autoregressive panel models with county fixed effects. Additionally, we estimate spatially lagged autoregressive panel models with county fixed effects. These employ maximum likelihood estimation and predict COVID-19 confirmed case and death rates (i.e., counts per 100,000 population). This approach has the advantage of accounting for interdependence among counties in the model structure while focusing on within-county variance over time to estimate spillovers. We estimate these models using the spxtregress command in Stata 16 and a spatial dependence structure defined by (a) only queen-contiguity, (b) queen-contiguity OR counties which are linked by more than 1% outgoing commuters, and (c) queen-contiguity OR counties which are linked by more than 0.5% outgoing commuters.
Appendix 1 shows the different steps utilized throughout our analyses, as well as the locations of corresponding results.
5. Results
5.1. Visualizing commuting networks and COVID-19
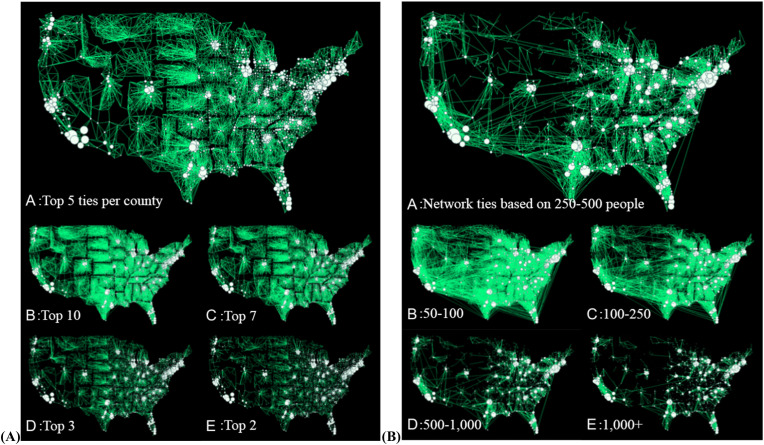
Fig. 1 shows the inter-county commuting networks based on LEHD-LODES home-to-work location data. County nodes are located based on geographical coordinates of their centroids. In Fig. 1A, node size is based on the number of commuters who work outside the county. For simplicity, the first mapped network graph shows only ties that are in the top 5 out of every node, followed by graphs with corresponding ties in the top 10, 7, 3, and 2 respectively. Across these maps, network ties tend to be clustered within states and large metropolitan areas, as expected given the tie definition. Network density depends on the number of ties included. Fig. 1B shows mobility ties based on different flow strength. Many ties show clustering within states and more of the weaker ties (under 250 commuters each) cross state boundaries. The maps in Fig. 1 illustrate the socially interconnected nature of US counties, above and beyond geographic contiguity.
Fig. 1.
County-to-county commuting networks across the US. Counties are represented as network nodes located based on the geographical coordinates of their centroids. Across the graphs, the size of the nodes is based on weighted outdegree. (A). Interconnected communities. The maps show only ties that represent a) the top 5 flows out of every node, b) the top 10, c) top 7, d) top 3, and e) top 2 outflows. (B). Ties of different strengths. The maps show ties that represent a) flows between 250 and 500 people each b) 50 to 100 people; c) 100 to 250 people; d) 500 to 1000 people; and e) more than 1000 people.
In Fig. 2 , panels A and B display the concentrations of new COVID-19 cases and deaths, respectively, measured as population rates, at time periods 1, 8, 16, and 23 in our study. The polygons represent counties, with darker shades for higher new COVID-19 rates based on time specific deciles. Panel C shows the geographic and temporal variation in network COVID-19 exposure. Counties are shaded by concentration of network-lagged COVID-19 case rate (see Equation (1)), based on new cases at the prior time period. As shown, the network exposure concentration at each time follows and amplifies patterns overlapping with those of local COVID-19 cases and deaths shown in panels A and B. Panel C thus highlights the predominance of Northeast and Northwest regions and many Rocky Mountain counties in the top rank of network COVID-19 exposure in the early period of the pandemic, followed by an amplification of Southern network exposures in the next periods, continuing to a strong emergence of Northcentral exposures, and a return to the top deciles among the Southern counties during the later periods. Taken together, the maps of Fig. 2 illustrate the strong links between COVID-19 exposure via intercounty commuting and COVID-19 outcomes in the following two weeks. As illustrated, this congruence exists across the duration of the study period.
Fig. 2.
Geographic distribution of COVID-19 cases, deaths, and network exposures across time. N = 2715 counties in each time. Polygons (counties) are colored in different shades by decile categories at each time period (lightest to darkest shades for bottom to top deciles). (A) New COVID-19 cases during a selection of four time periods, at the beginning, middle, and last time periods out of the study's 23 time periods. Polygons (counties) are colored in different shades by decile categories at each time period (lightest to darkest shades reflect gradation from bottom to top deciles). (B) New COVID-19 deaths at the same time periods. (C) Network weighted COVID-19 exposure, based on prior new cases for the same time periods.
5.2. Fixed and mixed effects results
Fig. 3 displays estimates from fixed-effects and multilevel mixed-effects models. In the fixed effects models, new COVID-19 cases and deaths were regressed on network and spatial exposure, time-lagged COVID-19 case rate, and dummy variables for each of the 23 time periods. Network exposure to COVID-19 consistently shows a positive association with both COVID-19 cases and deaths, even after controlling for spatial exposure and local work mobility.
Fig. 3.
Estimates and 95% Confidence intervals from fixed effects models.
N = 62,445 county-time periods (though counties with no variation of the outcome are dropped). Continuous predictors are standardized. All models also include time period fixed-effects, exposure term of total county population (2014–2018, ACS 5-year population estimates).
We next estimated the fixed effects models using split network measures based on commuting between (a) only spatially contiguous counties and (b) only spatially non-contiguous counties. The results (lower panel of Fig. 3) show that network effects persist in both cases, indicating that network exposures matter for the spread of COVID-19 independent of spatial proximity. The reversed sign of the spatial exposure effect between the main and split network models suggests that partially de-confounding the network and spatial exposure measures by splitting the commuting network allowed for the estimation of spatial spillovers, net of commuting.
The fixed effects results are consistent with those obtained using multilevel mixed-effects negative binomial models, as shown in Fig. 4 . Adjusting for spatial exposure and all other controls, the count of new COVID-19 confirmed cases per county population is estimated to increase by a factor of 3.66 (95% CI = 2.90, 4.61) for each unit increase in standardized network exposure, while the count of new COVID-19 deaths per county population is estimated to increase by a factor of 2.96 (95% CI = 2.23, 3.94) per unit increase in standardized network exposure (exponentiated changes in logged count). The mixed effects analyses showed that population exposure to COVID-19 in a county's commuting network increased local COVID–19 cases and deaths in the subsequent time period, above and beyond the area's socioeconomic disadvantage, age composition, urban status, and racial and ethnic composition. The effect of network exposure to COVID–19 cases on cases and deaths was also robust to controlling for exposure to COVID-19 cases through spatial contiguity and to controlling for prior local work mobility.
Fig. 4.
Estimates and 95% Confidence intervals from fixed effects models.
N = 62,445 county-time periods. Continuous predictors are standardized. All models also include time period fixed-effects, exposure term of total county population (2014–2018, ACS 5-year population estimates), and clustered standard errors by state.
As expected, an area's socioeconomic disadvantage contributed to both higher death rates and cases relative to the local population. The area's concentration of non-Hispanic white residents was negatively associated with infection cases (marginally statistically significant) but had no significant association with COVID-19 deaths. The concentration of non-Hispanic Black residents was associated with higher cases and deaths, while the concentration of Hispanic residents was associated with higher cases. These findings are consistent with a large body of work on the health challenges and social vulnerabilities linked to COVID-19 risk that burden minority communities, including a disproportionate likelihood to be in frontline occupations and in low-paid jobs with little flexibility in transitioning to a remote format (Tomer and Kane, 2020).
Multilevel mixed effects model estimates (for network and spatial exposures) using the split network approach are shown in the lower panel of Fig. 4. As shown, network effects persist in both cases, indicating that network exposures matter for the spread of COVID-19 independent of spatial proximity.
5.3. Model fit comparisons and permutations
Table 2a, Table 2b (panel A) shows a comparison of model fit statistics across multilevel mixed effects models, which included (a) spatial exposure, (b) network exposure, and (c) both as predictors. Local work mobility, sociodemographic covariates, and time-period fixed effects were included in all models. As shown, the table compares BIC, AIC, and MAAPE fit results. Also included is a set of MAAPE results which was calculated with a leave-one-out algorithm for comparable models estimated using cumulative (rather than panel) data. As shown, models including the network-based exposure show consistently better fit than those which only account for spatial exposure.
Table 2a.
Fit statistics across multilevel mixed effects negative binomial models, including local mobility, county-level covariates, and time period fixed effects.
| AIC | BIC | MAAPE | LOO-MAAPE* | ||
|---|---|---|---|---|---|
| Cases | |||||
| Spatial only | 685519 | 685817 | .57641 | .16686 | |
| Network only | 683299 | 683597 | .56950 | .16556 | |
| Spatial and network | 683300 | 683608 | .56948 | .15935 | |
| Deaths | |||||
| Spatial only | 250229 | 250528 | .94104 | .39540 | |
| Network only | 249482 | 249780 | .94095 | .39304 | |
| Spatial and network | 249443 | 249750 | .94071 | .39242 | |
Table 2b.
Coefficient estimates, 95% confidence, and MAAPE-based permutation test results from mixed-effects models predicting COVID-19 confirmed cases and deaths.
| Confirmed cases | Deaths | |||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | P-test proportion | Coef. | 95% CI | P-test proportion | |
| Network exposure | 1.30 | [1.07,1.53] | 0.000 | 1.09 | [0.8,1.37] | 0.000 |
| Spatial exposure | .02 | [-0.18,0.23] | 0.09 | .22 | [-0.06,0.5] | 0.00 |
| Local change in work mobility | .01 | [-0.12,0.14] | 0.77 | −.53 | [-0.73,-0.33] | 0.00 |
| Economic disadvantage | .15 | [0.08,0.21] | 0.00 | .49 | [0.33,0.64] | 0.00 |
| Percent 65 and older | −.23 | [-0.32,-0.14] | 0.17 | .24 | [0.11,0.36] | 0.00 |
| Above average non-Hispanic White | −.07 | [-0.15,0.01] | 1.00 | −.02 | [-0.19,0.15] | 0.91 |
| Above average non-Hispanic Black | .25 | [0.17,0.33] | 1.00 | .27 | [0.09,0.45] | 1.00 |
| Above average Hispanic | .13 | [0.03,0.23] | 1.00 | .08 | [-0.04,0.21] | 0.00 |
| Percent urban | .02 | [-0.04,0.09] | 0.96 | −.03 | [-0.14,0.08] | 0.00 |
Notes: N = 62,445 county-time periods for panel data; N = 2715 counties for cumulative data. Statistics are based on multilevel mixed effects models which include all sociodemographic controls.
*LOO-MAAPE are based on cumulative data.
Results from the permutation tests (Table 2a, Table 2b panel B) show the robust importance of COVID-19 network exposure. The network-based measure improved model fit in all trials predicting deaths and cases (i.e., no model in which this measure was randomly permuted outperformed the original model based on observed data).
5.4. Spatial autoregressive panel models with county fixed effects
Estimates from the spatial autoregressive panel analyses are displayed in Table 3 . Models 1 and 3 include only a spatial or a combined spatial and commuting network lag, while Models 2 and 4 also control for local work mobility. All models include time period fixed effects. As shown, spatial and network lag coefficients are consistently positive and statistically significant, suggesting inter-county spillovers of COVID-19 case and death rates. Adding commuting network ties to the weight matrix increases the estimated magnitude of this coefficient (i.e., spillovers become more pronounced), and improves model fit. These results show the salience of human mobility to the spread of COVID-19 above and beyond geographic contiguity.
Table 3.
Spatial autoregressive panel models with county fixed effects, predicting COVID-19 confirmed case rate and death rate.
| COVID-19 Case Rate (per 100,000) |
COVID-19 Death Rate (per 100,000) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 (N = 71,553) |
M2 (N = 62,445) |
M3 (N = 71,553) |
M4 (N = 62,445) |
||||||||||
| Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | ||||||
| Only spatial contiguity | |||||||||||||
| Lag | .68 | *** | (.003) | .67 | *** | (.003) | .36 | *** | (.005) | .42 | *** | (.005) | |
| Local work mobility | Yes | Yes | |||||||||||
| AIC | 971671.1 | 833201.5 | 543004.7 | 444574.8 | |||||||||
| BIC | 971891.4 | 833427.6 | 543225.0 | 444800.9 | |||||||||
| Spatial contiguity with 1% commuting ties | |||||||||||||
| Lag | .89 | *** | (.004) | .89 | *** | (.004) | .68 | *** | (.007) | .73 | *** | (.006) | |
| Local work mobility | Yes | Yes | |||||||||||
| AIC | 968008.9 | 828009.8 | 540567.8 | 442122.6 | |||||||||
| BIC | 968229.2 | 828235.9 | 540788.0 | 442348.7 | |||||||||
| Spatial contiguity with 0.5% commuting ties | |||||||||||||
| Lag | .92 | *** | (.004) | .92 | *** | (.003) | .74 | *** | (.007) | .78 | *** | (.007) | |
| Local work mobility | Yes | Yes | |||||||||||
| AIC | 967923.8 | 827967.8 | 540128.2 | 442029.2 | |||||||||
| BIC | 968144.1 | 828193.9 | 540348.4 | 442255.3 | |||||||||
***p < .001; **p < .01; *p < .05; †p < .10; all models include time and county fixed effects.
5.5. Cell phone mobility results
The upper panel of Fig. 5 shows coefficient estimates from multilevel mixed-effects models predicting cases and deaths with (a) the SafeGraph-based measure of pandemic-adjusted commuting network exposure, (b) pre-pandemic influence, (c) spatial exposure, and (d) all controls. As shown, both the pandemic-adjusted commuting exposure and the measure of pre-pandemic influence are positively associated with both cases and deaths. This result suggests that pre-pandemic commuting ties encapsulate social linkages which continue to influence COVID-19 spillovers beyond pandemic-related changes to daily mobility. Model fit comparisons using these new measures are shown in the upper panel of Table 4 . As shown, the model including both the pandemic-adjusted network exposure and pre-pandemic influence (M4) best predicts cases, while the model using an exposure measure based entirely on the SafeGraph mobility data (M2) slightly outperforms M4 at predicting deaths.
Fig. 5.
Summary of coefficient estimates and 95% confidence intervals from multilevel mixed effects negative binomial models; controls included spatial COVID-19 exposure and county-level sociodemographic factors; Exposure is total county population; Standard errors clustered by state.
Table 4.
Comparison of model fit statistics across models, using additional pandemic-time datasets.
| Confirmed Cases | Deaths | |||
|---|---|---|---|---|
| AIC | BIC | AIC | BIC | |
| Adjusting for pandemic-time, in-person mobility changes (LEHD and SafeGraph data; N = 27,300 county-time periods; 2730 counties) | ||||
| M1: Baseline (only spatial exposure + local work mobility + controls) | 342934.4 | 343098.7 | 141319.6 | 141483.8 |
| M2: Pandemic-time phone mobility network exposures (SafeGraph) | 342593.9 | 342766.4 | 140942.0 | 141114.5 |
| M3: Pre-pandemic commuting network exposure (LEHD) | 342592.6 | 342765.1 | 140965.2 | 141137.7 |
| M4: Commuting networks (pandemic adjusted + pre-pandemic) (SafeGraph + LEHD) | 342582.0 | 342762.7 | 140957.0 | 141137.7 |
| Adjusting for pandemic-time online social ties (LEHD and Facebook SCI Data; 62,445 county-time periods; 2715 counties) | ||||
| M1: Baseline (only spatial exposure + local work mobility + controls) | 685518.9 | 685817.3 | 250229.4 | 250527.8 |
| M2: Pre-pandemic commuting network exposures (LEHD) | 683300.3 | 683607.7 | 249442.9 | 249750.3 |
| M3: Social media ties network (Facebook SCI) | 685336.1 | 685643.5 | 250226.5 | 250533.9 |
| M4: Social media ties + Pre-pandemic commuting networks (Facebook SCI + LEHD) | 683295.7 | 683612.2 | 249392.1 | 249708.5 |
Fit statistics are based on multilevel mixed effects negative binomial regression models; all models included the baseline measures: spatial COVID-19 exposure, local work mobility, and all sociodemographic county-level covariates; SE clustered by state.
5.6. Social media ties results
The lower panel of Fig. 5 shows coefficient estimates from multilevel mixed-effects models predicting cases and deaths using (a) the original pre-pandemic commuting based network exposure measure, (b) the exposure measure based on Facebook SCI data, (c) spatial exposure, and (d) all controls. As shown, Facebook SCI exposure has no significant effect after controlling for commuting network exposure. The results of these analyses, when taken together with the set of SafeGraph models described above, show that commuting ties represent a composite of social and physical influences, both of which have important implications for the spread of COVID-19 across space. That said, the lower panel of Table 4 suggests that Facebook-based exposure may make some contributions to model fit beyond commuting, especially in predicting deaths. For this outcome, the best model fit resulted from the inclusion of both pre-pandemic commuting network exposure and Facebook SCI-based exposure.
Taken together, results from the SafeGraph and Facebook data supporting analyses showed that (a) our findings are robust to controls capturing intercounty changes in mobility during the pandemic, and (b) COVID-19 exposure based on the pre-pandemic commuting network captures both physical and social intercounty influences and has predictive value beyond alternative measures and additional controls based on SafeGraph mobility data and Facebook social connectivity.
5.7. Supplementary analyses
We conducted several additional analyses to check the robustness of our results.11 In order to assess whether are results were biased due to regression linearity assumptions, we constructed a 10-categorical measure of network exposure based on deciles and incorporated this into the full multilevel mixed effects models in place of the continuous measure of network exposure. These models allow for a nonlinear effect of network exposure by estimating a separate coefficient for each decile category, referenced against the lowest category. Even without the linearity constraint, these models still estimated near linear relationships between network exposure and the study's outcomes. Appendix 2 shows predicted values from these models.
As is a frequent challenge in COVID-19 analyses, our study relies on recent data compiled by numerous agencies, and may be influenced by factors such as regional testing capabilities and reporting standards. To test whether our results are robust to alternative measures of COVID-19, we aggregated county-level COVID-19 data from the New York Times database (via Social Explorer) to the time periods in our study period. Appendix 3a shows a correlation between this measure and our USA Facts-based measure, especially for later time periods (lower correlation in the earlier periods was likely due to higher data missingness during those times). Appendix 3b shows coefficient estimates from fixed effects and multilevel mixed effects models predicting cases and deaths from the New York Times database (with exposure measures based on the USA Facts data). As shown, results are substantively similar.
6. Discussion
The current analyses found that, during the COVID-19 pandemic, US counties have been significantly affected by their populations' exposures to COVID-19 in their commuting networks. The results are robust to adjusting for changes in mobility during the pandemic using independent mobility data from smart phone records. This finding supports our first proposed hypothesis and is consistent with the fact that millions of US workers, like bus drivers, postal and health workers, and grocery and meatpacking workers, are in occupations deemed “essential” with little possibility of working from home (Tomer and Kane, 2020). Our unique relational exposure measure capitalizes on the most comprehensive commuting data available, which allows us to capture the mobile population irrespective of age or socioeconomic status, an important contribution that extends on studies using phone and digital app data (Chiou and Tucker, 2020; Jay et al., 2020; Weill et al., 2020). These results are consistent with prior work indicating both workplace transmission of diseases and resources (Deziel et al., 2020; Lan et al., 2020) as well as social influences of health behaviors among co-workers and peers (Buller et al., 2000; Christakis and Fowler, 2008) that can also carry over to workers’ households (Bolger et al., 1989; Taylor et al., 1997). Importantly, this finding contributes to advancing the theoretical and conceptual thinking with new insights in support of the growing relational perspective on health and place (Bavel et al., 2020; Berkman et al., 2014; Block et al., 2020; Browning et al., 2017; Cummins et al., 2007; Kuchler et al., 2021; Matthews and Yang, 2013; Sampson, 2012).
In contrast to studies focused on short-term fluctuations in mobility of smart phone users during the pandemic, our findings highlight first-time evidence on the importance of the enduring effects of the pre-pandemic commuting ties for the spread of COVID-19 across space and time. The findings suggest that these pre-pandemic network influences operate above and beyond short-term distancing related to “stay-at-home” guidelines and worker layoffs. This supports our second hypothesis and in line with ideas that COVID-19 exposures, like other health risk exposures, entail remote ties and influence among people and groups, whether they work from home or not (Allem et al., 2017; Allgaier and Svalastog, 2015; Bavel et al., 2020; Zhang and Centola, 2019). Indeed, prior evidence suggests that social influence through digital communication apps like Facebook, Twitter, or text messaging affects crisis preparedness (Afzalan et al., 2015) and predicts COVID-19 outbreaks (Kuchler et al., 2021). Our results similarly indicated that, consistent with prior evidence (Kuchler et al., 2021), Facebook connectivity exposures contribute to improvements in COVID-19 model fit. Still, it is instructive that exposures through the commuting network had additional predictive value beyond the social media network exposure, contributing further improvement to model fit. The results of these analyses together with findings that adjusted for pandemic-times mobility from smart phone and applications data, further support the idea that commuting ties combined both social and physical influences, with important implications for the spread of COVID-19 across space.
7. Conclusions and implications for research and policy
In sum, the current study found that commuting networks across the country shaped COVID-19 cases and deaths, above and beyond spillovers between geographically contiguous areas, mobility changes during the pandemic, or social media connections. Both pre-pandemic commuting networks as well as pandemic-adjusted commuting mattered beyond pandemic-time mobility disruptions. The findings indicate that connections across places forged through population-level commuting networks, set in place before the pandemic, operate as significant channels of COVID-19 exposures. This is consistent with important insights in prior work that health risk, such as COVID-19 exposures, entail not just disease transmission risk but also the social transfer of information, attitudes, and resources (Bavel et al., 2020; Browning et al., 2017; Newmyer et al., 2022) that can contribute to prevention and mitigation.
As this pandemic has demonstrated, physical distancing from work is not an option for many vulnerable groups. Our findings move the academic and public discussions beyond debates around individual responsibility and stay-at-home policies toward a macro-level level relational view of public health that acknowledges the durable place-to-place interdependent systems of linkages and influence that bridge across space and time (Berkman et al., 2014; Cummins et al., 2007). Understanding the value of treating places and neighborhoods as parts of broader, inter-connected networks of places has important implications for advancing neighborhood effects research and for better understanding the mixed effects of costly interventions that moved families away from poor places while ignoring the poverty of areas nearby (Graif et al., 2016).
The current results indicates several additional directions for future research and policy. They suggest that outcomes following a policy intervention in one place may be substantially hindered by influences from places connected to it when they take more lax approaches. Conversely, the results also suggest that place-based policies designed to lower COVID-19 outbreaks in a highly interconnected place may spillover to lower COVID-19 spread in other areas across its commuting network. For instance, as masks or vaccine mandates are implemented in highly connected communities, they may contribute to key protection spillovers in other connected areas in the network. Still, disinformation campaigns against mask wearing or vaccines that affect a highly connected work hub may also influence health risk behaviors across workers’ home communities. On the bright side, the current findings also suggest that access to policies and provisions such as paid sick leave, health safety equipment, and affordable health that may help the lives and health of the workers and families, may also spillover and save lives, improving the health and wellbeing of the communities in which the workers live.
Funding
Graif is also thankful for funding from NICHD (K01 HD093863) and support from the Population Research Institute funded by NICHD (P2C HD041025). Honavar is thankful for funding from the NSF (IIS 2041759, 1636795) and NIH NCATS (UL1 TR002014).
Acknowledgments
We thank John Iceland, Scott Yabiku, Barry Lee, Charles Boynton, Brittany Freelin, Leif Jensen and other participants in the Population Research Institute's Communities and Place working group and Population Association of America meeting participants, for feedback on earlier drafts.
Footnotes
Because March counts were low and sparsely distributed across space compared to the later months, this study period started on April 1st. This enabled more reasonable variation across space in COVID-19 cases and deaths.
Out of 3143 US counties and equivalents, we omitted observations with missing data on key variables, including all of Alaska (missing commuting data) leading to an analytical sample of N = 2715 counties. Note that we also estimated primary models without controlling for local work mobility, allowing for an analytic sample of 3111 counties, with substantively similar results (available on request).
A small number of county-times had negative counts of either new cases or new deaths recorded, due to reporting errors or corrections. These counts were coded as 0 for the construction of lagged variables and subsequent analyses.
The most recent available data at the time of the analysis, as updated on an annual basis, with a delay in release by the Census Bureau. Supplemental analyses revealed a high degree of network stability for each of the five prior years (available upon request), suggesting that even more recent data would yield substantively similar findings.
Data on Unemployment Insurance earning records from states and other local institutions were collected and matched by the US Census Bureau to other administrative records, census data, and survey data on firms, workers, and households. About 95% of salary and wage jobs are covered by the Unemployment Insurance records (Graham et al., 2014). The commuting flow statistics are created based on matching the location of employers' establishments (work destination location) to the residential location of employees (home origin locations). We aggregated the LEHD-LODES data to create an origin-destination, inter-county weighted network among US counties.
The data and more documentation details are available here: https://www.google.com/covid19/mobility/.
During the study period, governmental measures to mitigate the spread of COVID-19 primarily took the form of lockdowns, stay at home orders, and mandated business closures. As such, controlling for local work mobility is helps to adjust for spatial and temporal variation in governmental pandemic response measures.
SafeGraph data was obtained from https://www.safegraph.com.
The weights were log-transformed to adjust for undue influence of extreme outliers.
Although it is possible that other county-level characteristics could influence COVID-19 outcomes, we focused on controlling for those that we believed most likely to confound the effects of network exposure. We address the possibility of unmeasured, county-level confounders through our fixed effects models, described subsequently.
In addition to the tests described here, we also estimated a set of models in which the local work mobility control was replaced by local, time-lagged COVID-19 case rate. Results were substantively similar to those presented, available upon request. These alternative models offer an especially conservative robustness check by adjusting for any spatial or temporal factors that might influence past COVID-19 incidence, such as governmental pandemic response measures.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.healthplace.2022.102891.
Appendix 1. Flow chart of analyses, data used, and location of results within manuscript
Appendix 2. Predicted counts of COVID-19 confirmed cases and deaths, based on multilevel mixed effects models in which COVID-19 network exposure was modeled using decile categories; controls included spatial COVID-19 exposure and county-level sociodemographic factors; Exposure is total county population; Standard errors clustered by state
Appendix 3a. Correlation coefficients between USA Facts COVID-19 database and The New York Times coronavirus data
Appendix 3b. Estimates and 95% Confidence intervals from fixed effects and multilevel mixed effects models predicting confirmed cases and deaths from the New York Times coronavirus database.N = 62,445 county-time periods in main mixed effects models (counties with no variation of the outcome are dropped from fixed effects models). Continuous predictors are standardized. All models also include time period fixed-effects, exposure term of total county population (2014–2018, ACS 5-year population estimates). Mixed effects models have clustered standard errors by state
Appendix ASupplementary data
The following is the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Abowd J.M., Stephens B.E., Vilhuber L., Andersson F., McKinney K.L., Roemer M., Woodcock S. 2005. The LEHD Infrastructure Files and the Creation of the Quarterly Workforce Indicators. [Google Scholar]
- Afzalan N., Evans-Cowley J.S., Barijough M. From big to little data for natural disaster recovery: how online and on-the-ground activities are connected? ISJLP. 2015;11:153–180. [Google Scholar]
- Allem J.-P., Ferrara E., Uppu S.P., Cruz T.B., Unger J.B. E-cigarette surveillance with social media data: social bots, emerging topics, and trends. JMIR Public Heal. Surveill. 2017;3:e98. doi: 10.2196/publichealth.8641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allgaier J., Svalastog A.L. The communication aspects of the Ebola virus disease outbreak in Western Africa - do we need to counter one, two, or many epidemics? Croat. Med. J. 2015;56:496–499. doi: 10.3325/cmj.2015.56.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcaya M.C., Tucker-Seeley R.D., Kim R., Schnake-Mahl A., So M., Subramanian S.V. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc. Sci. Med. 2016;168 doi: 10.1016/j.socscimed.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey M., Cao R., Kuchler T., Stroebel J., Wong A. Social connectedness: measurement, determinants, and effects. J. Econ. Perspect. 2018;32:259–280. doi: 10.1257/jep.32.3.259. [DOI] [PubMed] [Google Scholar]
- Balcan D., Colizza V., Gonçalves B., Hud H., Ramasco J.J., Vespignani A. Multiscale mobility networks and the spatial spreading of infectious diseases. Proc. Natl. Acad. Sci. U.S.A. 2009;106:21484–21489. doi: 10.1073/pnas.0906910106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bavel J.J.V., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N., Drury J., Dube O., Ellemers N., Finkel E.J., Fowler J.H., Gelfand M., Han S., Haslam S.A., Jetten J., Kitayama S., Mobbs D., Napper L.E., Packer D.J., Pennycook G., Peters E., Petty R.E., Rand D.G., Reicher S.D., Schnall S., Shariff A., Skitka L.J., Smith S.S., Sunstein C.R., Tabri N., Tucker J.A., Linden S. van der, Lange P. van, Weeden K.A., Wohl M.J.A., Zaki J., Zion S.R., Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nat. Human Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Berkman L.F., Kawachi I., Glymour M.M., editors. Social Epidemiology. Oxford University Press; Oxford: 2014. [Google Scholar]
- Block P., Hoffman M., Raabe I.J., Dowd J.B., Rahal C., Kashyap R., Mills M.C. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nat. Human Behav. 2020;4 doi: 10.1038/s41562-020-0898-6. [DOI] [PubMed] [Google Scholar]
- Bolger N., DeLongis A., Kessler R.C., Wethington E. The contagion of stress across multiple roles. J. Marriage Fam. 1989;51:175. doi: 10.2307/352378. [DOI] [Google Scholar]
- Breiman L. Random forests. Mach. Learn. 2001;45:5–32. [Google Scholar]
- Browning C.R., Calder C.A., Soller B., Jackson A.L., Dirlam J. Ecological networks and neighborhood social organization. Am. J. Sociol. 2017;122:1939–1988. doi: 10.1086/691261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buller D., Buller M.K., Larkey L., Sennott-Miller L., Taren D., Aickin M., Wentzel T.M., Morrill C. Implementing a 5-a-Day peer health educator program for public sector labor and trades employees. Health Educ. Behav. 2000;27:232–240. doi: 10.1177/109019810002700209. [DOI] [PubMed] [Google Scholar]
- Cartenì A., Di Francesco L., Martino M. How mobility habits influenced the spread of the COVID-19 pandemic: results from the Italian case study. Sci. Total Environ. 2020;741 doi: 10.1016/j.scitotenv.2020.140489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S., Pierson E., Koh P.W., Gerardin J., Redbird B., Grusky D., Leskovec J. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2021;589:82–87. doi: 10.1038/s41586-020-2923-3. [DOI] [PubMed] [Google Scholar]
- Chiou L., Tucker C. 2020. Social Distancing, Internet Access and Inequality. [Google Scholar]
- Christakis N.A., Fowler J.H. The collective dynamics of smoking in a large social network. N. Engl. J. Med. 2008;358:2249–2258. doi: 10.1056/nejmsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S., Curtis S., Diez-Roux A.V., Macintyre S. Understanding and representing ‘place’ in health research: a relational approach. Soc. Sci. Med. 2007;65:1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- De Vos J. The effect of COVID-19 and subsequent social distancing on travel behavior. Transp. Res. Interdiscip. Perspect. 2020;5 doi: 10.1016/j.trip.2020.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deziel N.C., Allen J.G., Scheepers P.T.J., Levy J.I. The COVID-19 pandemic: a moment for exposure science. J. Expo. Sci. Environ. Epidemiol. 2020;30 doi: 10.1038/s41370-020-0225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A.V. Investigating neighborhood and area effects on health. Am. J. Publ. Health. 2001;91 doi: 10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd J.B., Andriano L., Brazel D.M., Rotondi V., Block P., Ding X., Liu Y., Mills M.C. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc. Natl. Acad. Sci. U.S.A. 2020;117:9696–9698. doi: 10.1073/pnas.2004911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facebook . 2018. Social Connectedness Index (SCI)https://dataforgood.facebook.com/ [WWW Document]. Faceb. Data Good Progr. URL. accessed 2.22.22. [Google Scholar]
- Fazio M., Pluchino A., Inturri G., Le Pira M., Giuffrida N., Ignaccolo M. Exploring the impact of mobility restrictions on the COVID-19 spreading through an agent-based approach. J. Transport Health. 2022;25 doi: 10.1016/j.jth.2022.101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham M.R., Kutzbach M.J., McKenzie B. 2014. Design Comparison of LODES and ACS Commuting Data Products. [Google Scholar]
- Graif C., Arcaya M.C., Diez Roux A.V. Moving to opportunity and mental health: exploring the spatial context of neighborhood effects. Soc. Sci. Med. 2016;162:50–58. doi: 10.1016/j.socscimed.2016.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jay J., Bor J., Nsoesie E.O., Lipson S.K., Jones D.K., Galea S., Raifman J. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat. Human Behav. 2020;4:1294–1302. doi: 10.1038/s41562-020-00998-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y., Gao S., Liang Y., Li M., Rao J., Kruse J. Multiscale dynamic human mobility flow dataset in the U.S. during the COVID-19 epidemic. Sci. Data. 2020;7:1–13. doi: 10.1038/s41597-020-00734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krivo L.J., Washington H.M., Peterson R.D., Browning C.R., Calder C.A., Kwan M.-P. Social isolation of disadvantage and advantage: the reproduction of inequality in urban space. Soc. Forces. 2013;92 doi: 10.1093/sf/sot043. [DOI] [Google Scholar]
- Kuchler T., Russel D., Stroebel J. The geographic spread of COVID-19 correlates with the structure of social networks as measured by Facebook. J. Urban Econ. 2021;127:103314. doi: 10.1016/j.jue.2020.103314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan F.Y., Wei C.F., Hsu Y.T., Christiani D.C., Kales S.N. Work-related COVID-19 transmission in six Asian countries/areas: a follow-up study. PLoS One. 2020;15:1–12. doi: 10.1371/journal.pone.0233588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks S.R. Intimacy in the public realm: the case of co-workers. Soc. Forces. 1994;72:843–858. [Google Scholar]
- Matthews S.A., Yang T.-C. Spatial polygamy and contextual exposures (SPACEs) Am. Behav. Sci. 2013;57 doi: 10.1177/0002764213487345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie B. 2015. Who drives to work?: Commuting by automobile in the United States: 2013. [Google Scholar]
- Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C., Honermann B., Lankiewicz E., Mena L., Crowley J.S., Sherwood J., Sullivan P. Assessing differential impacts of COVID-19 on Black communities. Ann. Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newmyer L., Evans M., Graif C. 2022. Socially Connected Neighborhoods and the Spread of Sexually Transmitted Infections. Demography. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pluchino A., Biondo A.E., Giuffrida N., Inturri G., Latora V., Le Moli R., Rapisarda A., Russo G., Zappalà C. A novel methodology for epidemic risk assessment of COVID-19 outbreak. Sci. Rep. 2021;11:5304. doi: 10.1038/s41598-021-82310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafiq R., McNally M.G., Sarwar Uddin Y., Ahmed T. Impact of working from home on activity-travel behavior during the COVID-19 Pandemic: an aggregate structural analysis. Transport. Res. Part A Policy Pract. 2022;159:35–54. doi: 10.1016/j.tra.2022.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson R. University of Chicago Press; Chicago: 2012. Great American City: Chicago and the Enduring Neighborhood Effect. [Google Scholar]
- Sy K.T.L., White L.F., Nichols B.E. Population density and basic reproductive number of COVID-19 across United States counties. PLoS One. 2021;16 doi: 10.1371/journal.pone.0249271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.E., Repetti R.L., Seeman T. Health psychology: what is an unhealthy environment and how does it get under the skin? Annu. Rev. Psychol. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- Tomer A., Kane J.W. 2020. To Protect Frontline Workers during and after COVID-19, We Must Define Who They Are. (Washington, DC) [Google Scholar]
- Viboud C., Bjørnstad O.N., Smith D.L., Simonsen L., Miller M.A., Grenfell B.T. Synchrony, waves, and spatial hierarchies in the spread of influenza. Science. 2006;312(80):447–451. doi: 10.1126/science.1125237. [DOI] [PubMed] [Google Scholar]
- Weill J.A., Stigler M., Deschenes O., Springborn M.R. Social distancing responses to COVID-19 emergency declarations strongly differentiated by income. Proc. Natl. Acad. Sci. U.S.A. 2020;117 doi: 10.1073/PNAS.2009412117. 19658–19660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Centola D. Social networks and health: new developments in diffusion, online and offline. Annu. Rev. Sociol. 2019;45:91–109. doi: 10.1146/annurev-soc-073117-041421. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.