Abstract
Coronary heart disease (CHD) mainly refers to coronary atherosclerotic heart disease and its pathogenesis is complex. Ginsenoside Rg1 (Rg1) has a wide range of pharmacological activities, such as antitumor effects, enhancing immunity and exerting protective effects on the vascular system. In the present study, the effect of Rg1 on vascular endothelial cells in CHD was investigated. Oxidized low-density lipoprotein (ox-LDL) was used to induce human umbilical vein endothelial cells (HUVECs) and cells were treated with 1, 5 or 10 µM Rg1. Cell Counting Kit-8 assay, TUNEL staining, western blot analysis of apoptosis-related proteins and senescence-related proteins, senescence-associated β-galactosidase staining, ELISA and other techniques including related kits of oxidative stress markers were used to detect the viability, apoptosis, oxidative stress, inflammatory cytokines including IL-1β, IL-6 and TNF-α and senescence of ox-LDL-induced HUVECs induced by Rg1. Western blot analysis was used to detect the expression levels of the AMP-activated protein kinase (AMPK)/sirtuin 3 (SIRT3)/p53 signaling pathway-related proteins. In addition, the associated mechanism was further determined using the AMPK pathway inhibitor compound C (CC). Rg1 increased the viability, and inhibited the apoptosis, senescence, oxidative stress and inflammation of ox-LDL-induced HUVECs. Pretreatment with CC partially reversed the protective effect of Rg1 on ox-LDL-induced HUVECs. In conclusion, Rg1 ameliorated apoptosis, senescence and oxidative stress of ox-LDL-induced HUVECs, at least in part, via the AMPK/SIRT3/p53 signaling pathway.
Keywords: ginsenoside Rg1, apoptosis, senescence, oxidative stress, oxidized low-density lipoprotein, vascular endothelial cell, AMP-activated protein kinase/sirtuin 3/p53 signaling pathway
Introduction
Coronary heart disease (CHD) mainly refers to coronary atherosclerotic heart disease. The basic pathological process of CHD is the lack of blood supply of the coronary artery caused by atherosclerosis (AS), which leads to ischemia and hypoxia of myocardial cells (1). There are numerous reasons for its occurrence. Lipid infiltration, oxidative stress and inflammation may all lead to the occurrence of AS (2). However, the specific mechanisms remain to be fully elucidated; thus, the treatment and prevention of CHD remain challenging.
A large number of clinical studies have demonstrated that vascular endothelial injury causes AS, which in turn leads to CHD, and CHD aggravates vascular endothelial injury (3-5). Vascular endothelial dysfunction and integrity destruction are the initial stages of AS, which may lead to a variety of cardiovascular diseases (6). Endothelial cells have high metabolic activity and endocrine regulation function to ensure normal blood flow in the vascular wall (7). In addition, endothelial cells are constantly affected by blood flow, inflammatory factors and their own metabolic disorders, including permeability and diffuse calcification that lead to structural and functional impairment, resulting in morphological and functional changes of endothelial cells (7). A previous study has demonstrated that microRNA-26a-5p promotes the proliferation and inhibits apoptosis of endothelial cells in mice with CHD by activating the PI3K/AKT signaling pathway targeting PTEN, thereby affecting the pathogenesis of CHD (8). In addition, several studies have investigated the severity of the disease by examining apoptosis, inflammation and senescence of vascular endothelial cells in CHD (9,10).
Ginsenosides are the main active substances of the Chinese herbal medicine ginseng, which have antitumor, immunity-enhancing and protective effects on the vascular system (11-13). Ginsenoside Rg1 (Rg1) has been widely used in cardiovascular and cerebrovascular diseases due to its unique therapeutic effects. For example, Rg1 is able to enhance myocardial contractility and maintain the integrity of the myocardial cell membrane, which has a marked effect on the protection of the cardiovascular system and the prevention and treatment of cardiovascular diseases, including AS and hypertension (14-16). Rg1 has been reported to alleviate high glucose-induced endothelial barrier dysfunction in human umbilical vein endothelial cells (HUVECs) by protecting the endothelial glycocalyx (17). However, to the best of our knowledge, the effect of Rg1 on vascular endothelial cells in CHD has remained elusive.
Therefore, in the present study, oxidized low-density lipoprotein (ox-LDL) was used to induce apoptosis, senescence and oxidative stress in vascular endothelial cells, and the effects of Rg1 on the ox-LDL-induced apoptosis, senescence and oxidative stress of vascular endothelial cells were explored and the associated mechanism was investigated. Therefore, the present study lays a foundation for the potential future treatment of CHD using Rg1.
Materials and methods
Reagents and cell culture
HUVECs (cat. no. BNCC337616), obtained from BeNa Culture Collection, were cultured in DMEM supplemented with 10% FBS (Gibco; Thermo Fisher Scientific, Inc.) and 1% penicillin/streptomycin in a humidified incubator with 5% CO2 at 37˚C. HUVECs were treated with different concentrations of Rg1 (1, 5 or 10 µM; Shanghai YaJi Biotechnology Co., Ltd.) for 24 h at 37˚C (18,19). The AMP-activated protein kinase (AMPK) inhibitor compound C (CC; 5 mM; MilliporeSigma) was used to pretreat HUVECs for 2 h at 37˚C. In addition, HUVECs were stimulated with 100 mg/l ox-LDL (Beijing Solarbio Science & Technology Co., Ltd.) for 48 h at 37˚C to construct an in vitro AS model. To evaluate the effects of Rg1 on ox-LDL-treated HUVECs, the cells were pretreated with Rg1 for 30 min prior to ox-LDL treatment. Untreated cells were regarded as the control group.
Cell counting kit-8 (CCK-8) assay
Transfected HUVECs were seeded into 96-well plates with complete medium at a density of 2x104. Following treatment with Rg1 for 24 h, cell viability was detected using a CCK-8 assay (Beyotime Institute of Biotechnology). A total of 10 µl CCK-8 solution was added to each well of HUVECs. After incubation for 2 h, the absorbance value of each well was measured at 450 nm using a microplate reader (Bio-Rad Laboratories, Inc.).
TUNEL staining
Cells (1x104) were cultured on cover slips in a 24-well plate used for fluorescent detection. Following treatment with Rg1 for 24 h, cells were fixed in 4% paraformaldehyde for 30 min at room temperature and then incubated with TUNEL BrightGreen Apoptosis Detection kit (cat. no. A112-02; Vazyme Biotech Co., Ltd.) for 1 h. Cells were incubated with DAPI for 15 min at 37˚C in the dark, followed by fluorescence microscopy (magnification, x200). Images from 5 random fields were analyzed using ImageJ software (version 1.46; National Institutes of Health).
Western blot analysis
HUVECs were lysed in RIPA buffer (MilliporeSigma) and protein concentrations were measured using a BCA Protein Assay Kit (Beyotime Institute of Biotechnology). A total of 30 µg protein per lane was separated by SDS-PAGE using a 10% polyacrylamide gel and electroblotted onto a PVDF membrane. After blocking with 5% skimmed milk powder for 1.5 h at room temperature, the membrane was incubated at 4˚C with primary antibodies overnight. After three washes with TBS with 0.1% Tween-20, the membrane was incubated with a secondary goat antibody (dilution, 1:5,000; cat. no. ab6721; Abcam) for 1 h at room temperature. Signals were detected with Pierce™ Enhanced Chemiluminescence Western Blotting Substrate (Thermo Fisher Scientific, Inc.). The images were analyzed using ImageJ 1.8.0 software. The following antibodies were used (dilution, 1:5,000; all from Abcam): Anti-Bcl-2 (cat. no. ab32124, Abcam), anti-Bax (cat. no. ab32503), anti-cleaved caspase-3 (cat. no. ab32042), anti-caspase-3 (cat. no. ab32351), anti-p16 (cat. no. ab51243), anti-p21 (cat. no. ab109520), anti-AMPKα (cat. no. ab32047), anti-phosphorylated (p)-AMPKα (cat. no. ab133448), anti-sirtuin (SIRT)3 (cat. no. ab217319), anti-acetyl-p53 (cat. no. ab183544), anti-p53 (cat. no. ab179477) and anti-GAPDH (cat. no. ab9485). GAPDH was used as a loading control.
Senescence-associated β-galactosidase (SA-β-gal) staining
Cells were cultured in 24-well plates (1x104 cells/well). After treatment as aforementioned, the cells were washed with PBS and fixed in 3% formaldehyde at room temperature for 5 min. SA-β-gal staining was performed using a senescence β-galactosidase staining kit (cat. no. 9860; Cell Signaling Technology, Inc.) according to the manufacturer's instructions. A total of three fields of view were randomly selected and the number of senescent cells with blue staining was determined using a light microscope (magnification, x200).
Measurement of reactive oxygen species (ROS), malondialdehyde (MDA) and superoxide dismutase (SOD) levels
The levels of ROS (cat. no. ab139476; Abcam), MDA (cat. no. A003-1-2; Nanjing Jiancheng Bioengineering Institute) and SOD (cat. no. A001-3-2; Nanjing Jiancheng Bioengineering Institute) were detected using commercial kits according to the manufacturers' protocols.
ELISA
In brief, 100 µl cell culture supernatant was added into duplicate wells and incubated at 37˚C for 90 min. IL-1β (cat. no. H002), IL-6 (cat. no. H007-1-1) and TNF-α (cat. no. H052-1) levels were determined using ELISA (Nanjing Jiancheng Bioengineering Institute) according to the manufacturer's protocol. Photometric measurements were performed at 450 nm using a microplate reader (Varioskan Flash; Thermo Fisher Scientific, Inc.).
Statistical analysis
Values are expressed as the mean ± standard deviation. All experiments were repeated three times. All data were analyzed using SPSS version 16 (SPSS, Inc.). Significant differences among more groups were evaluated using one-way ANOVA followed by the Tukey-Kramer honest significant difference post-hoc test. P<0.05 was considered to indicate a statistically significant difference.
Results
Rg1 increases the viability of ox-LDL-induced HUVECs
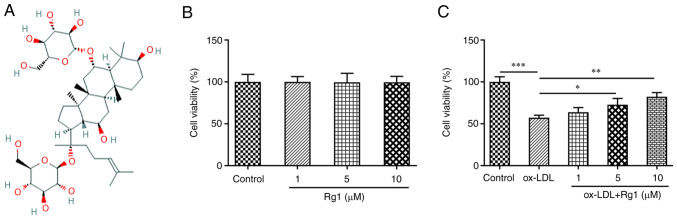
Fig. 1A presents the chemical structural formula of Rg1. CCK-8 assay revealed no significant change in cell viability after Rg1 administration (Fig. 1B). Subsequently, the effect of Rg1 on the viability of ox-LDL-induced cells was detected. The results demonstrated that the viability of ox-LDL-induced cells was markedly decreased compared with that of the control group. Compared with the ox-LDL group, the cell viability was enhanced with the increase of the Rg1 concentration (Fig. 1C).
Figure 1.
Rg1 increases the viability of ox-LDL-induced HUVECs. (A) Chemical structure of Rg1. (B) CCK-8 assay was used to detect the viability of HUVECs treated with Rg1. (C) CCK-8 assay was used to examine the viability of ox-LDL-induced HUVECs treated with Rg1. *P<0.05, **P<0.01, ***P<0.001. CCK-8, Cell Counting Kit-8; ox-LDL, oxidized low-density lipoprotein; HUVEC, human umbilical vein endothelial cell; Rg1, ginsenoside Rg1.
Rg1 inhibits the apoptosis of ox-LDL-induced HUVECs
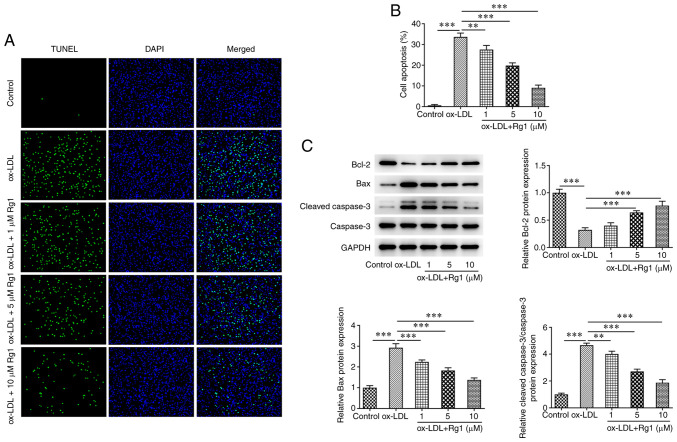
TUNEL assay results demonstrated that apoptosis was markedly increased following treatment with ox-LDL compared with the control group. Compared with that in the ox-LDL group, apoptosis decreased in cells treated with Rg1 in a dose-dependent manner (Fig. 2A and B). Subsequently, western blot analysis was used to detect the expression levels of apoptosis-related proteins. The results revealed that, compared with those in the control group, the expression levels of Bcl-2 were decreased and the expression levels of Bax and cleaved caspase-3 were increased after ox-LDL induction. Compared with the ox-LDL group, Rg1 was able to markedly inhibit the expression of Bax and cleaved caspase-3, while it increased the expression levels of Bcl-2 and caspase-3 expression remained unchanged (Fig. 2C).
Figure 2.
Rg1 inhibits the apoptosis of ox-LDL-induced HUVECs. (A) TUNEL assay was used to detect the apoptosis of ox-LDL-induced HUVECs treated by Rg1 (magnification, x200). (B) Quantified proportion of apoptotic cells. (C) Western blot analysis was performed to detect the expression of apoptosis-related proteins. **P<0.01, ***P<0.001. ox-LDL, oxidized low-density lipoprotein; HUVEC, human umbilical vein endothelial cell; Rg1, ginsenoside Rg1.
Rg1 inhibits the senescence of ox-LDL-induced HUVECs
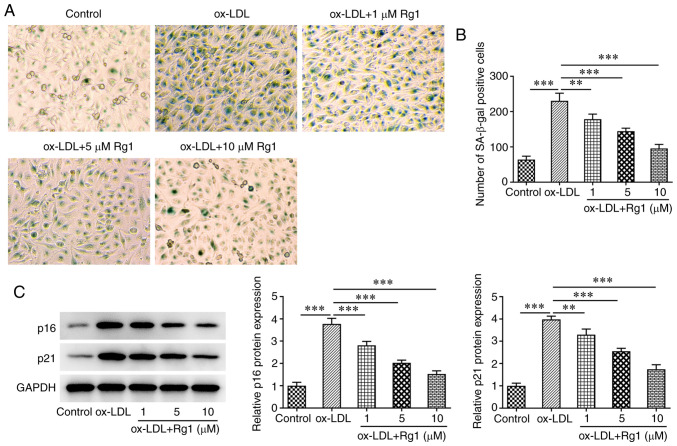
SA-β-gal staining was used to detect cell senescence. The results revealed that ox-LDL markedly promoted cell senescence compared with the control group. Rg1 markedly reduced the senescence of ox-LDL-induced cells (Fig. 3A and B). Subsequently, western blot analysis was used to detect the expression levels of the senescence-related proteins p16 and p21. The results demonstrated that, compared with those in the control group, the expression levels of p16 and p21 were markedly increased following challenge with ox-LDL. Of note, compared with the ox-LDL group, the expression levels of p16 and p21 were decreased in a dose-dependent manner after Rg1 administration (Fig. 3C).
Figure 3.
Rg1 inhibits the senescence of ox-LDL-induced HUVECs. (A) SA-β-gal staining was used to detect the senescence of ox-LDL-induced HUVECs (magnification, x200). (B) Quantified number of senescent cells. (C) Western blot analysis was used to detect the expression of senescence-related proteins. **P<0.01, ***P<0.001. ox-LDL, oxidized low-density lipoprotein; HUVEC, human umbilical vein endothelial cell; Rg1, ginsenoside Rg1; SA-β-gal, senescence-associated β-galactosidase.
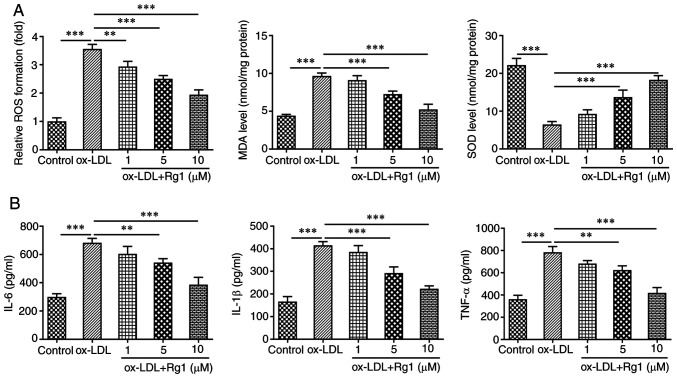
Rg1 inhibits oxidative stress and inflammation in ox-LDL-induced HUVECs
The levels of oxidative stress-related indicators, including ROS, MDA and SOD, were subsequently detected. The results revealed that compared with the control group, the levels of ROS and MDA in ox-LDL-induced cells were markedly increased, while the levels of SOD were markedly decreased. The effects of ox-LDL induction on ROS, MDA and SOD levels were reversed after Rg1 administration (Fig. 4A). ELISA kits were used to detect the expression levels of inflammatory cytokines, including IL-6, IL-1β and TNF-α. It was revealed that IL-6, IL-1β and TNF-α levels were markedly increased in the ox-LDL group compared with the control group. Compared with those in the ox-LDL group, the expression levels of IL-6, IL-1β and TNF-α in the ox-LDL + Rg1 group were markedly decreased (Fig. 4B).
Figure 4.
Rg1 inhibits oxidative stress and inflammation in ox-LDL-induced human umbilical vein endothelial cells. (A) Kits were used to detect the expression of oxidative stress indicators. (B) ELISA was used to detect the release of inflammatory cytokines. **P<0.01, ***P<0.001. ox-LDL, oxidized low-density lipoprotein; Rg1, ginsenoside Rg1; ROS, reactive oxygen species; MDA, malondialdehyde; SOD, superoxide dismutase.
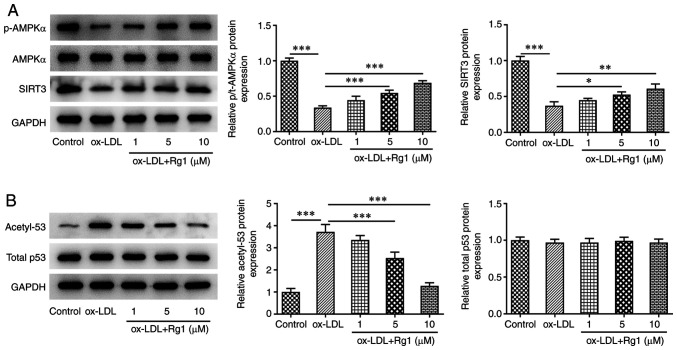
Rg1 regulates the AMPK/SIRT3/p53 signaling pathway
After ox-LDL induction, the levels of p-AMPK and SIRT3 were markedly decreased, the expression of acetyl-p53 was markedly increased and no apparent changes were observed in total AMPK and total p53 expression, compared with the control group. After Rg1 administration, compared with those in the ox-LDL group, the levels of p-AMPK and SIRT3 increased, while acetyl-p53 levels decreased in a dose-dependent manner (Fig. 5A and B). It was thus indicated that the AMPK/SIRT3/p53 signaling pathway was abnormally regulated after ox-LDL induction. The results suggested that 10 µM Rg1 exhibited the most marked effect on this pathway, and therefore this concentration was selected for subsequent experiments.
Figure 5.
Rg1 regulates the AMPK/SIRT3/p53 signaling pathway. Western blot analysis was used to detect the expression of (A) AMPK/SIRT3 and (B) p53 signaling pathway-related proteins. *P<0.05, **P<0.01, ***P<0.001. ox-LDL, oxidized low-density lipoprotein; Rg1, ginsenoside Rg1; p, phosphorylated; t, total; AMPK, AMP-activated protein kinase; SIRT, sirtuin.
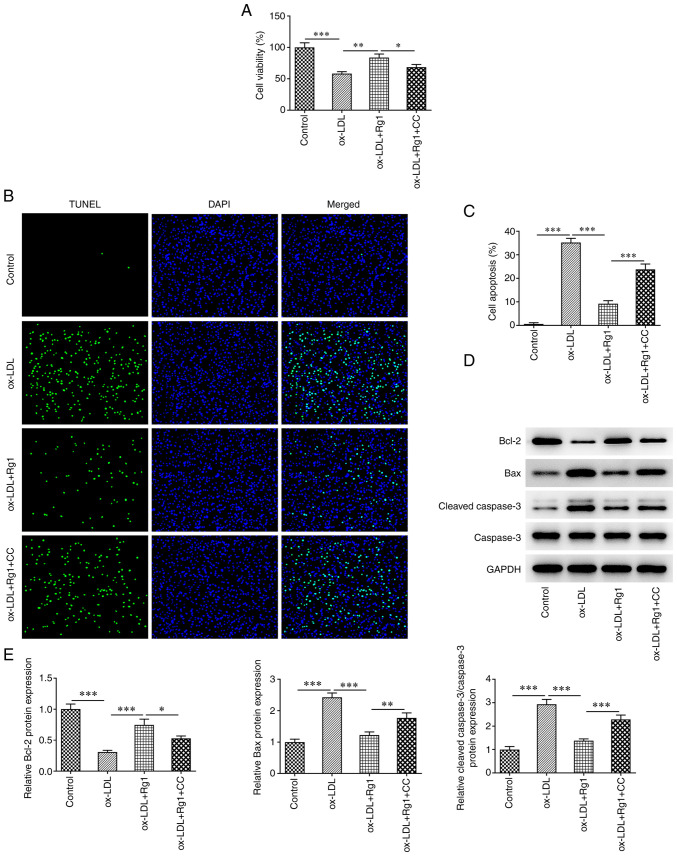
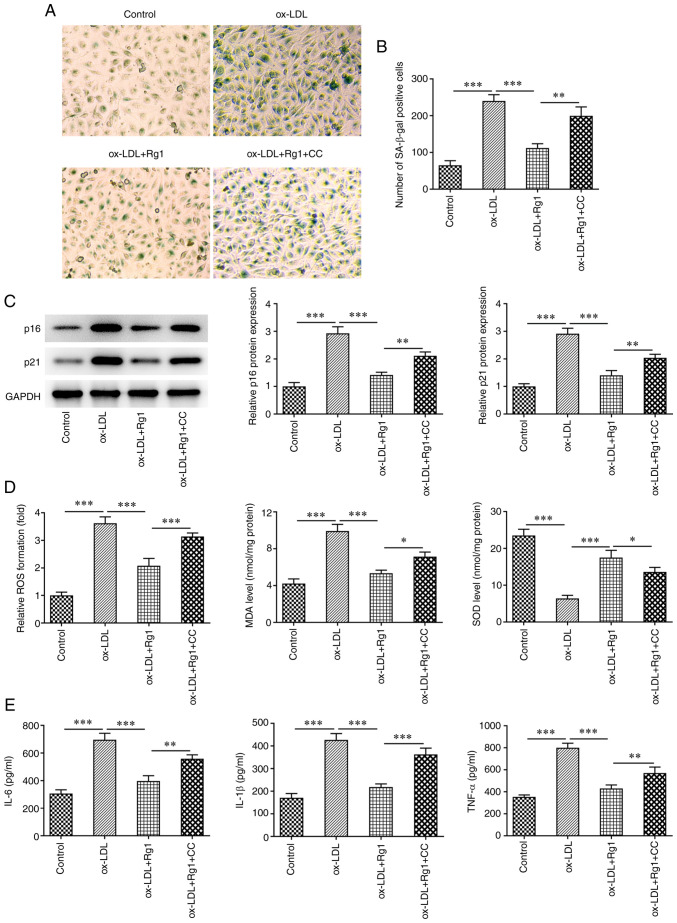
Pretreatment with CC partially reverses the protective effect of Rg1 on ox-LDL-induced HUVECs
The mechanism of Rg1 acting on ox-LDL-induced HUVECs was further explored by pretreating the cells with the AMPK inhibitor CC. The results of the CCK-8 assay demonstrated that cell viability in the ox-LDL +Rg1 + CC group was markedly decreased compared with that in the ox-LDL + Rg1 group (Fig. 6A). TUNEL staining revealed that apoptosis was markedly increased in the ox-LDL + Rg1 + CC group compared with the ox-LDL + Rg1 group (Fig. 6B and C). Western blot analysis demonstrated that compared with those in the ox-LDL + Rg1 group, Bax and cleaved caspase-3 levels were increased, and Bcl-2 expression was decreased in the ox-LDL + Rg1 + CC group (Fig. 6D and E). These results indicated that CC was able to reverse the promoting effect of Rg1 on the viability of ox-LDL-induced HUVECs. Subsequently, cell senescence was assessed, and it was revealed that SA-β-gal-positive cells were markedly increased in the ox-LDL + Rg1 + CC group compared with the ox-LDL + Rg1 group (Fig. 7A and B). Furthermore, the expression levels of p16 and p21 in cells were markedly increased after CC treatment compared with the ox-LDL + Rg1 group (Fig. 7C). Next, oxidative stress and inflammation were detected, and the results demonstrated that compared with those in the ox-LDL + Rg1 group, the levels of ROS and MDA in the ox-LDL + Rg1 + CC group were increased, while the levels of SOD were decreased (Fig. 7D). Furthermore, the expression levels of the inflammatory cytokines IL-6, IL-1β and TNF-α were also increased after CC treatment compared with those in the ox-LDL + Rg1 group (Fig. 7E). These results suggested that pretreatment with CC partially reversed the protective effect of Rg1 on ox-LDL-induced HUVECs.
Figure 6.
Pretreatment with CC partially reverses the effect of Rg1 on the viability of ox-LDL-induced human umbilical vein endothelial cells. (A) CCK-8 assay was used to detect cell viability. (B) TUNEL assay was employed to detect apoptosis (magnification, x200). (C) Quantified proportion of apoptotic cells. (D and E) Western blot analysis was used to detect the expression of apoptosis-related proteins. *P<0.05, **P<0.01, ***P<0.001. ox-LDL, oxidized low-density lipoprotein; Rg1, ginsenoside Rg1; CC, compound C.
Figure 7.
Pretreatment with CC partially reverses the protective effect of Rg1 on ox-LDL-induced HUVECs. (A) SA-β-gal staining was used to detect the senescence of HUVECs (magnification, x200). (B) Quantified number of senescent cells. (C) Western blot analysis was used to detect the expression of senescence-related proteins. (D) Related kits were used to detect the expression of oxidative stress indicators. (E) ELISA was performed to detect the release of inflammatory cytokines. *P<0.05, **P<0.01, ***P<0.001. ox-LDL, oxidized low-density lipoprotein; HUVEC, human umbilical vein endothelial cell; Rg1, ginsenoside Rg1; CC, compound C; SA-β-gal, senescence-associated β-galactosidase.
Discussion
Injury to the coronary artery endothelium is a key initiating factor in the formation of coronary AS (20). Oxidative modification of LDL may promote the formation of atherosclerotic plaque, which is the most important factor causing AS (21). It is also the main factor leading to injury of endothelial cells and smooth muscle cells (22). In in vitro studies, ox-LDL was used to induce injury to HUVECs to simulate an AS model (23-25). In the present study, ox-LDL was used to treat HUVECs and induce injury, simulating the damage of ox-LDL to blood vessels in the process of coronary AS. The present results demonstrated that after ox-LDL induction, the viability of HUVECs decreased, apoptosis and senescence occurred, and oxidative stress and inflammation in cells increased, indicating successful model establishment in vitro.
Rg1 has a wide range of pharmacological effects including neurotrophic, neuroprotective and effects (26,27). In the present study, it was indicated that Rg1 was able to enhance ox-LDL-induced cell viability and inhibit apoptosis. A previous study has reported that Rg1 inhibits myocardial apoptosis and inflammation through the Toll-like receptor 4/NF-κB/NLR family pyrin domain containing 3 signaling pathway (28). In addition, the present study revealed that Rg1 inhibited the senescence of ox-LDL-induced HUVECs. Rg1 has been indicated to inhibit senescence and promotes differentiation of human bone marrow mesenchymal stem cells through GSK-3β and β-catenin (29). The present study demonstrated that Rg1 inhibited ox-LDL-induced oxidative stress and the inflammatory response in HUVECs. This is consistent with the study of Qin et al (30), which demonstrated that Rg1 improved cardiac oxidative stress and inflammation in streptozotocin-induced diabetic rats. At present, only one study has investigated the utility Rg1 in AS. For example, Rg1-notoginsenoside R1-protocatechuic aldehyde was observed to reduce AS and attenuate low-shear stress-induced vascular endothelial cell dysfunction in apolipoprotein E-knockout mice (31). The novelty of the present study lied to the demonstration that Rg1 ameliorates ox-LDL-induced apoptosis, senescence and oxidative stress in HUVECs.
The present study revealed that the AMPK/SIRT3/p53 signaling pathway was inhibited in ox-LDL-induced HUVECs, while Rg1 was able to activate the AMPK/SIRT3/p53 signaling pathway after ox-LDL induction. A previous study has demonstrated that Rg1 exerts anti-senescence effects by inhibiting mitochondrial pathway-mediated apoptosis of hematopoietic stem/progenitor cells and activating the SIRT3/SOD2 signaling pathway (32). SIRT3 protects endothelial cells from high glucose-induced senescence and dysfunction through the p53 signaling pathway (33). In addition, activation of the AMPK/SIRT3 signaling pathway may reduce the levels of vascular endothelial mitochondrial ROS, and thus increase the mitochondrial antioxidant capacity of vascular endothelial cells (34). Therefore, it was hypothesized that Rg1 exerts its role through the AMPK/SIRT3/p53 signaling pathway. In the present study, CC was added to further explore the associated mechanism. It was revealed that CC inhibited cell viability, increased apoptosis, accelerated cell senescence and increased oxidative stress and inflammatory response in cells treated with ox-LDL + Rg1. It was able to reverse the protective effect of Rg1 on ox-LDL-induced HUVECs. Therefore, it was preliminarily concluded that Rg1 ameliorated ox-LDL-induced apoptosis, senescence and oxidative stress of HUVECs at least partially through the AMPK/SIRT3/p53 signaling pathway. The specific mechanisms are illustrated in Fig. 8.
Figure 8.
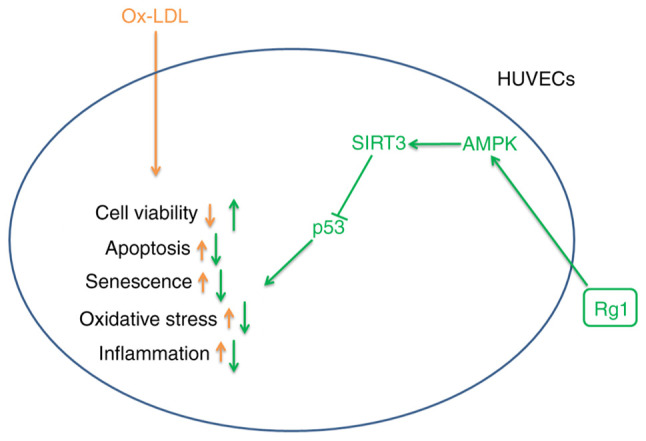
Schematic presenting the specific mechanisms of the protective effect of Rg1 on ox-LDL-induced HUVECs. Green arrows pointing upwards indicate increased activity and orange arrows pointing downwards indicate decreased activity. ox-LDL, oxidized low-density lipoprotein; Rg1, ginsenoside Rg1; AMPK, AMP-activated protein kinase; SIRT, sirtuin; HUVEC, human umbilical vein endothelial cell.
Of note, the present study presents certain limitations. The effect of Rg1 on coronary AS and its mechanism were only investigated at the cellular level, but not further verified in animals, which will be performed in future studies. An adequate dose of Rg1 for AS would also be required to be determined in animal models in future studies. In addition, the mechanism was only investigated using the AMPK pathway inhibitor CC and the mechanism was not further verified with pathway agonists, which is also one of the limitations of the present study. The conclusions of the present study will be further verified with the use of pathway agonists in future experiments. In addition, in the present study, the effect of Rg1 was only assessed on vascular endothelial cells. The effects on other cell types, such as the ventricular cardiomyocyte cell line H9c2, remain to be examined.
In conclusion, the present study revealed that Rg1 ameliorates apoptosis, senescence and oxidative stress in ox-LDL-induced HUVECs via the AMPK/SIRT3/p53 signaling pathway. The present study provided an important theoretical basis for the potential use of Rg1 in the clinical treatment of CHD.
Acknowledgements
Not applicable.
Funding Statement
Funding: The present study was supported by the Shanghai Putuo District Xinglin Excellence Program (grant no. ptxlyq2101), the Clinical Advantage Discipline of Health System of Putuo District in Shanghai (grant no. 2019ysxk01), the Shanghai Key Medical Specialties Construction Project (grant no. ZK2019A11) and the National Health Commission of Yangpu District ‘good doctor’ construction project.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
TJL and ZXZ conceived and designed the study. JC and ZJL performed the experiments. ZXZ and JC analyzed the experimental data. TJL and ZJL wrote and revised the manuscript. ZXZ and JC confirm the authenticity of all the raw data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Liang F, Wang Y. Coronary heart disease and atrial fibrillation: A vicious cycle. Am J Physiol Heart Circ Physiol. 2021;320:H1–H12. doi: 10.1152/ajpheart.00702.2020. [DOI] [PubMed] [Google Scholar]
- 2.Wirtz PH, von Känel R. Psychological stress, inflammation, and coronary heart disease. Curr Cardiol Rep. 2017;19(111) doi: 10.1007/s11886-017-0919-x. [DOI] [PubMed] [Google Scholar]
- 3.Gimbrone MA Jr, Garcia-Cardeña G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ Res. 2016;118:620–636. doi: 10.1161/CIRCRESAHA.115.306301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction: Testing and clinical relevance. Circulation. 2007;115:1285–1295. doi: 10.1161/CIRCULATIONAHA.106.652859. [DOI] [PubMed] [Google Scholar]
- 5.Palombo C, Kozakova M. Arterial stiffness, atherosclerosis and cardiovascular risk: Pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol. 2016;77:1–7. doi: 10.1016/j.vph.2015.11.083. [DOI] [PubMed] [Google Scholar]
- 6.Balta S. Endothelial dysfunction and inflammatory markers of vascular disease. Curr Vasc Pharmacol. 2021;19:243–249. doi: 10.2174/1570161118666200421142542. [DOI] [PubMed] [Google Scholar]
- 7.Tesauro M, Mauriello A, Rovella V, Annicchiarico-Petruzzelli M, Cardillo C, Melino G, Di Daniele N. Arterial ageing: From endothelial dysfunction to vascular calcification. J Intern Med. 2017;281:471–482. doi: 10.1111/joim.12605. [DOI] [PubMed] [Google Scholar]
- 8.Jing R, Zhong QQ, Long TY, Pan W, Qian ZX. Downregulated miRNA-26a-5p induces the apoptosis of endothelial cells in coronary heart disease by inhibiting PI3K/AKT pathway. Eur Rev Med Pharmacol Sci. 2019;23:4940–4947. doi: 10.26355/eurrev_201906_18084. [DOI] [PubMed] [Google Scholar]
- 9.Gao ZF, Ji XL, Gu J, Wang XY, Ding L, Zhang H. microRNA-107 protects against inflammation and endoplasmic reticulum stress of vascular endothelial cells via KRT1-dependent Notch signaling pathway in a mouse model of coronary atherosclerosis. J Cell Physiol. 2019;234:12029–12041. doi: 10.1002/jcp.27864. [DOI] [PubMed] [Google Scholar]
- 10.Wu X, Zheng W, Jin P, Hu J, Zhou Q. Role of IGFBP1 in the senescence of vascular endothelial cells and severity of aging-related coronary atherosclerosis. Int J Mol Med. 2019;44:1921–1931. doi: 10.3892/ijmm.2019.4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li H, Huang N, Zhu W, Wu J, Yang X, Teng W, Tian J, Fang Z, Luo Y, Chen M, Li Y. Modulation the crosstalk between tumor-associated macrophages and non-small cell lung cancer to inhibit tumor migration and invasion by ginsenoside Rh2. BMC Cancer. 2018;18(579) doi: 10.1186/s12885-018-4299-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun M, Ye Y, Xiao L, Duan X, Zhang Y, Zhang H. Anticancer effects of ginsenoside Rg3 (review) Int J Mol Med. 2017;39:507–518. doi: 10.3892/ijmm.2017.2857. [DOI] [PubMed] [Google Scholar]
- 13.Zhou P, Xie W, He S, Sun Y, Meng X, Sun G, Sun X. Ginsenoside Rb1 as an anti-diabetic agent and its underlying mechanism analysis. Cells. 2019;8(204) doi: 10.3390/cells8030204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang R, Yin D, Yang D, Liu X, Zhou Q, Pan Y, Li J, Li S. Xinnaokang improves cecal microbiota and lipid metabolism to target atherosclerosis. Lett Appl Microbiol. 2021;73:779–792. doi: 10.1111/lam.13573. [DOI] [PubMed] [Google Scholar]
- 15.Yang P, Ling L, Sun W, Yang J, Zhang L, Chang G, Guo J, Sun J, Sun L, Lu D. Ginsenoside Rg1 inhibits apoptosis by increasing autophagy via the AMPK/mTOR signaling in serum deprivation macrophages. Acta Biochim Biophys Sin (Shanghai) 2018;50:144–155. doi: 10.1093/abbs/gmx136. [DOI] [PubMed] [Google Scholar]
- 16.Pan C, Huo Y, An X, Singh G, Chen M, Yang Z, Pu J, Li J. Panax notoginseng and its components decreased hypertension via stimulation of endothelial-dependent vessel dilatation. Vascul Pharmacol. 2012;56:150–158. doi: 10.1016/j.vph.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 17.Zhu T, Wang H, Wang L, Zhong X, Huang W, Deng X, Guo H, Xiong J, Xu Y, Fan J. Ginsenoside Rg1 attenuates high glucose-induced endothelial barrier dysfunction in human umbilical vein endothelial cells by protecting the endothelial glycocalyx. Exp Ther Med. 2019;17:3727–3733. doi: 10.3892/etm.2019.7378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen J, Zhang X, Liu X, Zhang C, Shang W, Xue J, Chen R, Xing Y, Song D, Xu R. Ginsenoside Rg1 promotes cerebral angiogenesis via the PI3K/Akt/mTOR signaling pathway in ischemic mice. Eur J Pharmacol. 2019;856(172418) doi: 10.1016/j.ejphar.2019.172418. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y, Ding S, Chen Y, Sun Z, Zhang J, Han Y, Dong X, Fang Z, Li W. Ginsenoside Rg1 alleviates lipopolysaccharide-induced neuronal damage by inhibiting NLRP1 inflammasomes in HT22 cells. Exp Ther Med. 2021;22(782) doi: 10.3892/etm.2021.10214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krankel N, Luscher TF, Landmesser U. Novel insights into vascular repair mechanisms. Curr Pharm Des. 2014;20:2430–2438. doi: 10.2174/13816128113199990478. [DOI] [PubMed] [Google Scholar]
- 21.Jin JL, Zhang HW, Cao YX, Liu HH, Hua Q, Li YF, Zhang Y, Guo YL, Wu NQ, Zhu CG, et al. Long-term prognostic utility of low-density lipoprotein (LDL) triglyceride in real-world patients with coronary artery disease and diabetes or prediabetes. Cardiovasc Diabetol. 2020;19(152) doi: 10.1186/s12933-020-01125-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kattoor AJ, Kanuri SH, Mehta JL. Role of Ox-LDL and LOX-1 in atherogenesis. Curr Med Chem. 2019;26:1693–1700. doi: 10.2174/0929867325666180508100950. [DOI] [PubMed] [Google Scholar]
- 23.Chen L, Yang W, Guo Y, Chen W, Zheng P, Zeng J, Tong W. Exosomal lncRNA GAS5 regulates the apoptosis of macrophages and vascular endothelial cells in atherosclerosis. PLoS One. 2017;12(e0185406) doi: 10.1371/journal.pone.0185406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, Che J, Zhao H, Tang J, Shi G. Paeoniflorin attenuates oxidized low-density lipoprotein-induced apoptosis and adhesion molecule expression by autophagy enhancement in human umbilical vein endothelial cells. J Cell Biochem. 2019;120:9291–9299. doi: 10.1002/jcb.28204. [DOI] [PubMed] [Google Scholar]
- 25.Zhang D, Bi Z, Li Y, Zheng H, Li L, Ouyang J, Wang B, Bi Y. Sodium ferulate modified gene expression profile of oxidized low-density lipoprotein-stimulated human umbilical vein endothelial cells. J Cardiovasc Pharmacol Ther. 2009;14:302–313. doi: 10.1177/1074248409347986. [DOI] [PubMed] [Google Scholar]
- 26.Xie W, Zhou P, Sun Y, Meng X, Dai Z, Sun G, Sun X. Protective effects and target network analysis of ginsenoside Rg1 in cerebral ischemia and reperfusion injury: A comprehensive overview of experimental studies. Cells. 2018;7(270) doi: 10.3390/cells7120270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gao Y, Chu S, Zhang Z, Chen N. Hepataprotective effects of ginsenoside Rg1-a review. J Ethnopharmacol. 2017;206:178–183. doi: 10.1016/j.jep.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 28.Luo M, Yan D, Sun Q, Tao J, Xu L, Sun H, Zhao H. Ginsenoside Rg1 attenuates cardiomyocyte apoptosis and inflammation via the TLR4/NF-kB/NLRP3 pathway. J Cell Biochem. 2020;121:2994–3004. doi: 10.1002/jcb.29556. [DOI] [PubMed] [Google Scholar]
- 29.Wang Z, Jiang R, Wang L, Chen X, Xiang Y, Chen L, Xiao M, Ling L, Wang Y. Ginsenoside Rg1 improves differentiation by inhibiting senescence of human bone marrow mesenchymal stem cell via GSK-3β and β-catenin. Stem Cells Int. 2020;2020(2365814) doi: 10.1155/2020/2365814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qin Q, Lin N, Huang H, Zhang X, Cao X, Wang Y, Li P. Ginsenoside Rg1 ameliorates cardiac oxidative stress and inflammation in streptozotocin-induced diabetic rats. Diabetes Metab Syndr Obes. 2019;12:1091–1103. doi: 10.2147/DMSO.S208989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang L, Li Y, Ma X, Liu J, Wang X, Zhang L, Li C, Li Y, Yang W. Ginsenoside Rg1-notoginsenoside R1-protocatechuic aldehyde reduces atherosclerosis and attenuates low-shear stress-induced vascular endothelial cell dysfunction. Front Pharmacol. 2020;11(588259) doi: 10.3389/fphar.2020.588259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou Y, Wang YP, He YH, Ding JC. Ginsenoside Rg1 performs anti-aging functions by suppressing mitochondrial pathway-mediated apoptosis and activating sirtuin 3 (SIRT3)/superoxide dismutase 2 (SOD2) pathway in Sca-1(+) HSC/HPC cells of an aging rat model. Med Sci Monit. 2020;26(e920666) doi: 10.12659/MSM.920666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen T, Ma C, Fan G, Liu H, Lin X, Li J, Li N, Wang S, Zeng M, Zhang Y, Bu P. SIRT3 protects endothelial cells from high glucose-induced senescence and dysfunction via the p53 pathway. Life Sci. 2021;264(118724) doi: 10.1016/j.lfs.2020.118724. [DOI] [PubMed] [Google Scholar]
- 34.Han L, Li J, Li J, Pan C, Xiao Y, Lan X, Wang M. Activation of AMPK/Sirt3 pathway by phloretin reduces mitochondrial ROS in vascular endothelium by increasing the activity of MnSOD via deacetylation. Food Funct. 2020;11:3073–3083. doi: 10.1039/c9fo02334h. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.