Abstract
Aims
Primary percutaneous coronary intervention (pPCI) is the preferred reperfusion strategy in patients with ST-segment elevation myocardial infarction (STEMI) provided it can be performed within 120 min from diagnosis. However, it is unclear whether pPCI or a pharmaco-invasive (P-I) strategy is the best choice in patients who cannot receive timely pPCI. The aim of the present study was to compare outcomes after delayed and late pPCI vs. a P-I strategy in STEMI patients who did not receive timely pPCI.
Methods and results
All patients with STEMI registered in the Norwegian Myocardial Infarction Registry (NORMI) between 2013 and 2019, with ≤12 h from symptom onset to first medical contact and available timelines were included in the study. The primary outcome was all-cause mortality, and follow-up was through 2019. A total of 21 121 (27% of 78 368) STEMI patients were registered in the NORMI. Among patients who met the inclusion criteria, 7238 (54%) patients underwent timely pPCI, 1537 (11%) delayed pPCI (121–180 min), 1012 (7%) late pPCI (>180 min), and 2338 (17%) patients were treated with a P-I strategy. After a median follow-up time of 2.5 years, mortality was higher in the delayed pPCI [adjusted hazard ratio (HR) 1.3, 95% confidence interval (CI) 1.0–1.5] and in the late pPCI group (adjusted HR 1.4, 95% CI 1.1–1.7) compared to the P-I strategy group, but bleeding complications were more frequent after P-I strategy.
Conclusions
In STEMI patients who did not receive timely percutaneous coronary intervention, a P-I strategy seemed to be associated with better long-term survival compared to delayed/late pPCI.
Keywords: Myocardial infarction, P-I strategy, Primary PCI, Outcome
Introduction
About one out of four myocardial infarctions (MI) is classified as ST-segment elevation myocardial infarction (STEMI).1 The outcome of patients with STEMI is influenced by several factors, including treatment strategy and delay to treatment. The European Society of Cardiology (ESC) recommend primary percutaneous coronary intervention (pPCI) as the preferred reperfusion strategy in STEMI, provided it can be performed in a timely manner.2,3 Timely pPCI has been shown to be superior to fibrinolysis in reducing mortality, re-infarction, and stroke.4–7 A pharmaco-invasive (P-I) strategy is recommend if a pPCI strategy cannot be performed within 120 min from STEMI diagnosis and there are no contraindications.3 A P-I strategy implies fibrinolysis followed by rescue percutaneous coronary intervention (PCI) in case of failed fibrinolysis or routine early PCI strategy (coronary angiography and PCI of infarct-related artery if indicated) in case of successful fibrinolysis.3 The Comparison of primary Angioplasty and Pre-hospital fibrinolysis In acute Myocardial infarction (CAPTIM) and the Strategic Reperfusion Early after Myocardial Infarction (STREAM) trials both reported similar rates of mortality between a pPCI strategy and a P-I strategy in patients who did not receive timely pPCI.8,9 However, the benefit of fibrinolytic therapy is greatest when it is given within 2 h after symptom onset, and as many as 30% of patients may have contraindications.10–12 The proportion of STEMI who receive fibrinolytic therapy has declined over the last decades and it is still discussed whether delayed pPCI or a P-I strategy is the best choice in patients who cannot receive pPCI in a timely manner.13–15 Recently published observational data from France suggest reduced mortality in patients treated with a P-I strategy compared to patients treated with delayed pPCI.16
Every year about 3600 patients in Norway are hospitalized with a STEMI.1 Norway has a scattered population, and in many areas, the distance to hospitals performing pPCI is long. STEMI management is organized in accordance with the hub-and spoke model. In most patients, STEMI diagnosis is made in the out-of-hospital setting via the emergency medical services or in a non-PCI centre (spoke hospital), and the patients transferred to the PCI-centre (hub hospital) when the treatment strategy has been decided.
The aim of the present nationwide study was to compare outcomes after delayed pPCI vs. a P-I strategy in patients with STEMI admitted to hospitals in Norway between 2013 and 2019.
Methods
The Norwegian Myocardial Infarction Registry (NORMI)
The NORMI, a part of the Norwegian Cardiovascular Disease Registry, is a national quality register. Registration into NORMI is mandatory without requiring patient’s consent. The NORMI adhered to the Third Universal Definition of Myocardial Infarction during the study period.17 All MIs were classified as STEMI or non-STEMI according to the universal definition.17 The registry contains information on gender, age, cardiovascular risk factors, previous diseases and medication, symptoms and clinical findings, therapy and complications, drugs prescribed at discharge, and time of death. The registration and quality of the information in NORMI have been described previously.1,18
Study population
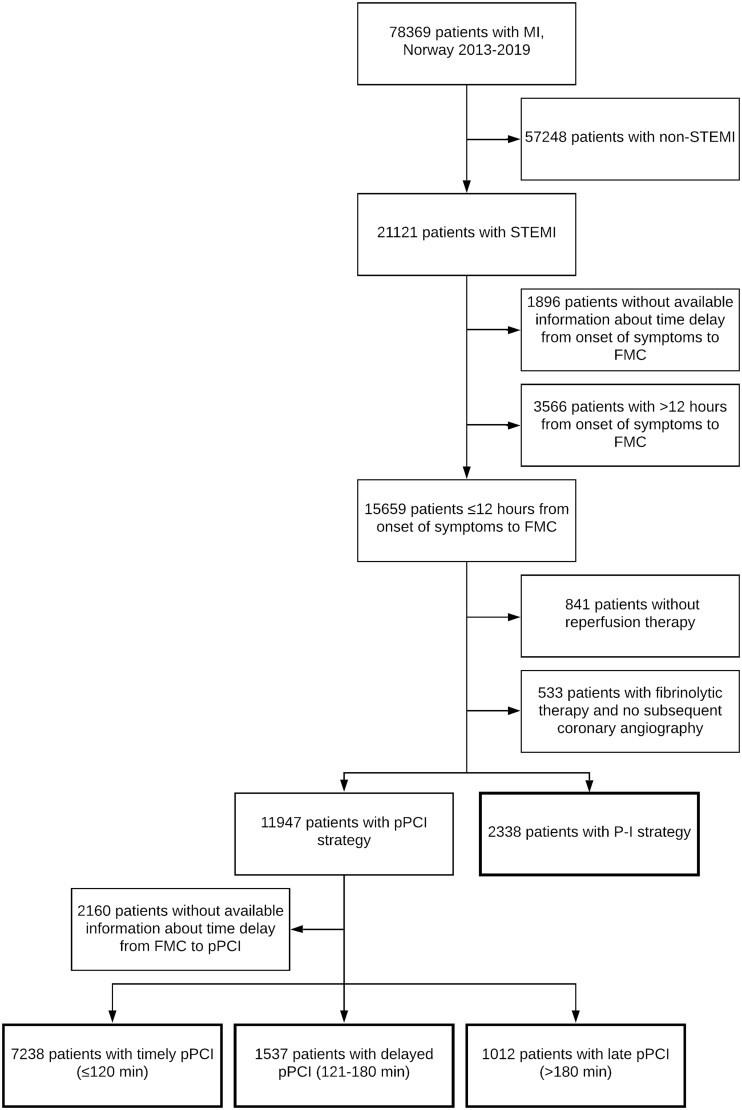
All patients admitted to hospitals in Norway with acute STEMI between 1 January 2013 and 31 December 2019 and registered in the NORMI were considered for inclusion in this study. In patients with more than one MI during the inclusion (study) period, only data from the first MI (index MI) were used. Patients presenting more than 12 h after symptom onset, patients without available timelines and patients without reperfusion therapy were excluded from the study (Figure 1).
Figure 1.
Patients admitted to hospitals in Norway with myocardial infarction from 2013 to 2019. FMC, first medical contact; MI, myocardial infarction; P-I strategy, pharmaco-invasive strategy; pPCI, primary percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
Outcomes
The primary outcome was all-cause mortality during follow-up. The secondary outcome was a composite of all-cause mortality, non-fatal stroke, or non-fatal MI. Follow-up data were available until 31 December 2019.
Definitions
Delay to reperfusion therapy
The time of STEMI diagnosis was not registered in NORMI, but time of first medical contact (FMC) was recorded. Therefore, we chose time from FMC to reperfusion as the best available estimate of system delay. If time from FMC to reperfusion therapy was missing, time from the diagnostic electrocardiogram (ECG) was used. If both time from FMC and time from diagnostic ECG were missing, time from hospital admission to reperfusion was used. NORMI used ‘balloon-time’ (first balloon inflation in the infarct related artery) as time of pPCI reperfusion.
We defined the following groups depending on the reperfusion strategy:
Timely pPCI: coronary angiography and PCI of infarct-related artery if indicated within 120 min from FMC.
Delayed pPCI: coronary angiography and PCI of infarct-related artery if indicated 121–180 min from FMC.
Late pPCI: coronary angiography and PCI of infarct-related artery if indicated >180 min from FMC.
P-I strategy: Fibrinolysis followed by coronary angiography and PCI of infarct-related artery if indicated regardless of time delays.
Major bleeding
NORMI defines major bleeding as (i) fatal bleeding, (ii) bleeding in a critical area or organ, such as intracranial, intraspinal, retroperitoneal, intraocular, intra-articular or pericardial, or intramuscular with compartment syndrome, and/or (iii) bleeding with haemoglobin drop >5 g/dL or ≥2 blood transfusions.
Patient and public involvement
This study used existing data from Norwegian national health registries. Registration into these registries is mandatory (the Norwegian Cardiovascular Disease Registry Regulation and the Norwegian Health Register Act), and consent by the patient was not required.
Statistics
Continuous variables are reported as means ± standard deviations or medians (25th percentile–75th percentile), and differences between groups were analysed using independent samples t-tests or Mann–Whitney non-parametric tests, as appropriate. Categorical variables are presented as numbers and percentages, and differences between groups were analysed by the chi-squared or Fisher’s exact tests. Kaplan–Meier curves for crude and event-free survival after hospital admission for the first MI in the study period were estimated, and Cox regression analyses were used to calculate hazard ratios (HRs) with 95% confidence intervals (CIs) for outcomes. The following covariates were included in the multivariable analyses: gender, age, smoking, previous stroke, previous MI, history of heart failure, diabetes, antihypertensive treatment, renal failure (estimated glomerular filtration rate < 60 mL/min), and out-of-hospital cardiac arrest (prior to hospitalization for index MI).
To account for confounding, three propensity score (PS) matched sets (timely pPCI matched with P-I strategy, delayed pPCI matched with P-I strategy, and late pPCI matched with P-I strategy) were constructed based on the following covariates: age, gender, smoking, previous stroke, previous MI, history of heart failure, diabetes, antihypertensive treatment, renal failure, and out-of-hospital cardiac arrest. The balance between the groups was assessed by investigating absolute standardized mean differences (SMDs) of all baseline covariates before and after the matching, using a threshold of 0.1 to indicate imbalance. Cox regression analyses using one-to-one nearest neighbour matching within 0.1 standard deviation of the PS were performed for timely pPCI vs. P-I strategy, delayed pPCI vs. P-I strategy, and late pPCI vs. P-I strategy.
The proportional hazard assumptions were checked with the proportional-hazards assumption test based on Schoenfeld residuals and log–log plot of survival. A P-value of <0.05 was regarded as statistically significant. The data were analysed using STATA version 16 (StataCorp LLC, College Station, TX, USA) and PS analyses were conducted with the user-developed command ‘psmatch2’.
Ethics
The Regional Committee for Medical and Health Research Ethics North approved this study (REK 2016/170).
Results
From 1 January 2013, through 31 December 2019, a total of 78 369 patients with MI were registered in the NORMI (Figure 1). Of these, 21 121 (27%) were diagnosed with STEMI. pPCI was the major reperfusion strategy [n = 14 404 (68%)]. A P-I strategy was preferred in 2408 (11%) patients. Fibrinolytic therapy without later PCI was applied in 566 (3%) cases, while 3743 (18%) patients with STEMI were not offered any reperfusion therapy.
A total of 8996 (43%) STEMI patients were excluded from this study due to no reperfusion therapy, missing information on time delays or time delay >12 h from onset of symptoms to FMC, or no subsequent coronary angiography after fibrinolytic therapy (Figure 1, Supplementary material online, Table S1).
Of the remaining 12 125 patients, 7238 (60%) patients underwent timely pPCI, 1537 (13%) delayed pPCI, 1012 (8%) late pPCI, and 2338 (19%) patients were treated with a P-I strategy. A prehospital ECG was available in 8544 (70%) of these patients.
Clinical characteristics
Baseline characteristics of the included patients are described in Table 1. Patients treated with pPCI (all groups) were older than patients treated with a P-I strategy. Patients with delayed or late pPCI were more likely to have hypertension, diabetes, and previous cardiovascular diseases, while patients treated with a P-I strategy were more likely to smoke. We found only minor differences in clinical characteristics between patients treated with timely pPCI and patients treated with a P-I strategy. In the P-I strategy group, the median delay from prehospital diagnostic ECG to fibrinolytic therapy was 33 (25th–75th percentile 20–53) min, and the median delay from fibrinolytic therapy to coronary angiography was 255 (25th–75th percentile 145–833) min.
Table 1.
Clinical characteristics in patients with ST-elevation myocardial infarction receiving timely, delayed, and late pPCI compared to P-I strategy, Norway 2013–2019
| Timely pPCI (≤120 min) |
Delayed pPCI (121–180 min) |
Late pPCI (>180 min) |
P-I strategy | ||||
|---|---|---|---|---|---|---|---|
|
n = 7238 |
n = 1537 |
n = 1012 |
n = 2338 | ||||
| n | P a | n | P a | n | P a | n | |
| Age (years), mean (SD) | 63.3 (11.9) | 0.01 | 65.7 (12.9) | <0.001 | 65.9 (12.8) | <0.001 | 62.5 (11.1) |
| Male, n (%) | 5762 (77) | 0.56 | 1112 (72) | <0.001 | 727 (72) | <0.001 | 1823 (78) |
| Smoking | |||||||
| Previous smoking, n (%) | 2108 (29) | 0.09 | 444 (29) | 0.09 | 313 (31) | 0.28 | 698 (30) |
| Current smoking, n (%) | 2920 (40) | <0.001 | 607 (39) | 0.001 | 375 (37) | <0.001 | 1055 (45) |
| Obesity (BMI > 30 kg/m2), n (%) | 1980 (27) | 0.22 | 454 (30) | 0.55 | 304 (30) | 0.42 | 670 (29) |
| LDL-cholesterol (mmol/L) (SD) | 3.4 (1.1) | 0.02 | 3.3 (1.1) | 0.0001 | 3.3 (1.2) | 0.05 | 3.4 (1.1) |
| Antihypertensive therapy, n (%) | 2539 (35) | 0.81 | 645 (42) | <0.001 | 469 (46) | <0.001 | 828 (35) |
| Diabetes, n (%) | 886 (12) | 0.24 | 252 (16) | <0.001 | 180 (18) | <0.001 | 265 (11) |
| Previous coronary heart disease | |||||||
| Myocardial infarction, n (%) | 684 (9%) | 0.51 | 174 (11) | 0.16 | 155 (15) | <0.001 | 232 (10) |
| Percutaneous coronary intervention, n (%) | 701 (10) | 0.49 | 180 (12) | 0.13 | 136 (13) | 0.006 | 238 (10) |
| Coronary artery bypass grafting, n (%) | 127 (2) | 0.99 | 38 (2) | 0.12 | 50 (5) | <0.001 | 41 (2) |
| Previous stroke, n (%) | 233 (3) | 0.39 | 74 (5) | 0.002 | 61 (6) | <0.001 | 67 (3) |
| History of heart failure, n (%) | 74 (1) | 0.99 | 35 (2) | 0.002 | 22 (2) | 0.009 | 24 (1) |
| Chronic kidney disease (eGFR < 60 mL/min), n (%) | 932 (13) | 0.21 | 288 (19) | <0.001 | 220 (22) | <0.001 | 271 (14) |
| Medication prior to admittance | |||||||
| Acetylsalicylic acid, n (%) | 1278 (18) | 0.02 | 312 (20) | 0.56 | 265 (26) | <0.001 | 461 (20) |
| Lipid lowering therapy, n (%) | 1512 (21) | 0.66 | 341 (22) | 0.14 | 271 (27) | <0.001 | 476 (20) |
| Beta blocker, n (%) | 1054 (15) | 0.19 | 296 (19) | <0.001 | 240 (24) | <0.001 | 313 (13) |
| ACE/AII receptor inhibitor, n (%) | 1841 (25) | 0.002 | 417 (27) | <0.001 | 298 (29) | <0.001 | 515 (22) |
| Diuretics, n (%) | 830 (11) | <0.001 | 200 (13) | <0.001 | 135 (13) | <0.001 | 202 (9) |
| Anticoagulation therapy, n (%) | 280 (4) | <0.001 | 94 (6) | <0.001 | 91 (9) | <0.001 | 41 (2) |
| Out-of-hospital cardiac arrest, n (%) | 612 (8) | 0.73 | 154 (10) | 0.05 | 52 (5) | 0.002 | 192 (8) |
| Median time delay onset of symptoms to FMC, min (25th–75th percentile) | 54 (26–120) | <0.001 | 74 (30–155) | <0.001 | 90 (33–182) | 0.002 | 96 (60–160) |
| Median time delay from FMC to reperfusion therapy, min (25th–75th percentile) | 82 (65–100) | <0.001 | 140 (130–156) | <0.001 | 252 (206–365) | <0.001 | 48 (32–70) |
| Median time delay from admission PCI-hospital to reperfusion therapy, min (25th–75th percentile) | 20 (13–34) | 27 (16–51) | 47 (19–152) | NA | |||
Reference: pharmaco-invasive (P-I) strategy.
FMC, first medical contact; pPCI, primary percutaneous coronary intervention.
In-hospital complications
The rate of in-hospital complications is shown in Table 2.
Table 2.
In-hospital complications in patients with ST-elevation myocardial infarction receiving timely, delayed, and late pPCI compared to P-I strategy, Norway 2013-2019
| Timely pPCI (≤120 min) | Delayed pPCI (121–180 min) | Late pPCI (>180 min) | P-I strategy | |
|---|---|---|---|---|
| n = 7238 | n = 1537 | n = 1012 | n = 2338 | |
| n | n | n | n | |
| Recurrent myocardial infarction, n (%) | 74 (1.0) | 16 (1.0) | 5 (0.5) | 11 (0.9) |
| Stroke, n (%) | 10 (0.1) | 6 (0.4) | 4 (0.4) | 18 (0.8) |
| Major bleeding, n (%) | 78 (1.1) | 21 (1.4) | 12 (1.2) | 57 (2.4) |
| Atrial fibrillation (new), n (%) | 233 (3.2) | 68 (4.4) | 44 (4.4) | 83 (3.6) |
| Ventricular tachycardia/fibrillation, n (%) | 408 (5.6) | 89 (5.8) | 60 (5.9) | 99 (4.2) |
| Cardiogenic shock, n (%) | 280 (3.9) | 99 (6.4) | 66 (6.5) | 129 (5.5) |
| In-hospital death, n (%) | 239 (3.3) | 99 (6.4) | 68 (6.7) | 93 (4.0) |
P-I strategy, pharmaco-invasive strategy; pPCI, primary percutaneous coronary intervention.
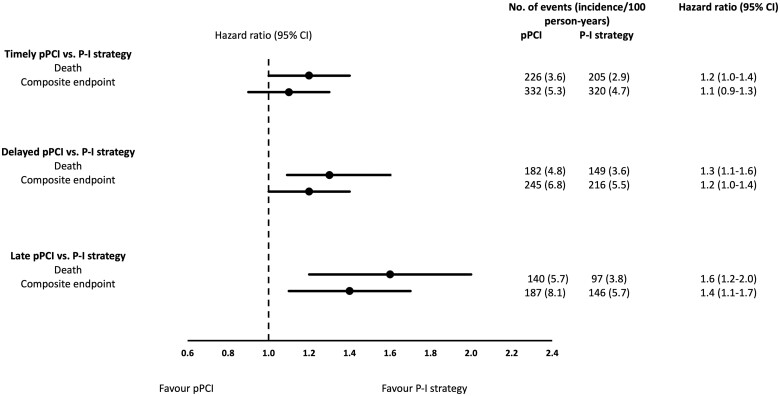
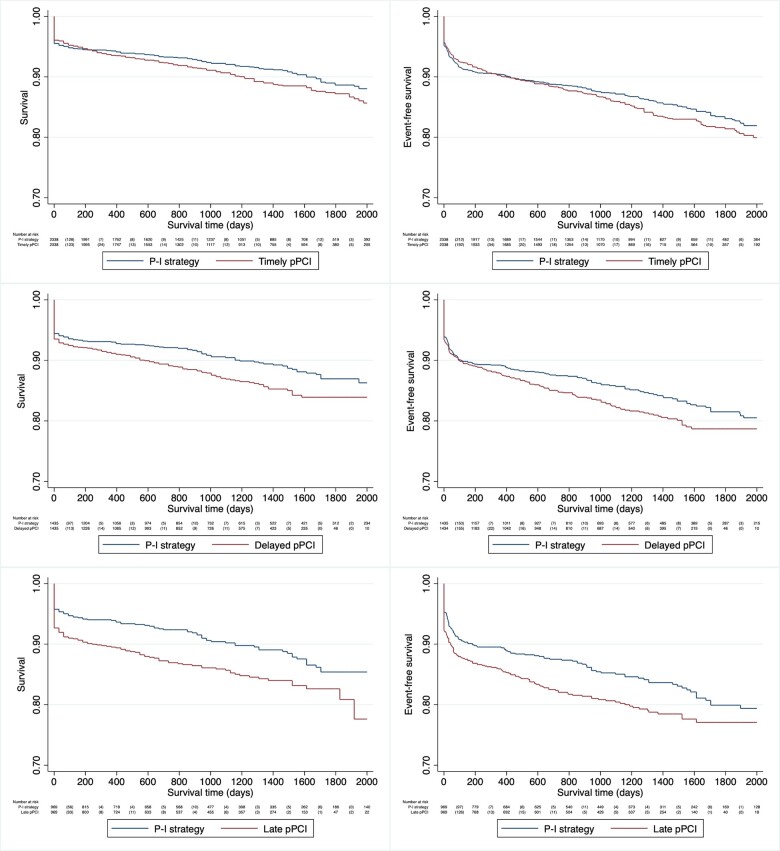
Outcomes
After a median follow-up time of 944 days (25th–75th percentile 396–1583), 1328 (11%) patients had died. Both the crude and the adjusted risk of all-cause mortality was higher in the delayed and late pPCI groups compared to the P-I strategy group (Table 3, Figure 2). For the composite endpoint death, non-fatal stroke or non-fatal MI, the patients were followed for a median time of 913 days (25th–75th percentile 335–1522). Event-free survival was higher in patients treated with a P-I strategy compared to patients treated with delayed and late pPCI (Table 3, Figure 2).
Table 3.
Outcomesa in patients with ST-elevation myocardial infarction receiving timely, delayed, and late pPCI compared to P-I strategy, Norway 2013–2019
| Timely pPCI (≤120 min) |
Delayed pPCI (121–180 min) |
Late pPCI (>180 min) |
P-I strategy | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
n = 7238 |
n = 1537 |
n = 1012 |
n = 2338 | |||||||
| n | Hazard ratio (95% CI)b | Adjusted HR (95% CI)b,c | n | Hazard ratio (95% CI)b | Adjusted HR (95% CI)b,c | n | Hazard ratio (95% CI)b | Adjusted HR (95% CI)b,c | n | |
| Death | 742 (10.3%) | 1.3 (1.1–1.5) | 1.1 (1.0–1.3) | 224 (14.6%) | 1.9 (1.5–2.3) | 1.3 (1.0–1.5) | 157 (15.5%) | 2.1 (1.6–2.5) | 1.4 (1.1–1.7) | 205 (8.9%) |
| Composite endpoint (death, non-fatal stroke, and non-fatal MI) | 1015 (14.0%) | 1.1 (1.0–1.2) | 1.0 (0.9–1.2) | 290 (18.9%) | 1.5 (1.3–1.8) | 1.2 (1.0–1.4) | 206 (20.4%) | 1.7 (1.4–2.0) | 1.3 (1.1–1.5) | 320 (13.7%) |
Follow-up to 31 December 2019. Death: median follow-up 944 days (25th–75th percentile 396–1583). Composite endpoint: median follow-up 913 days (25th–75th percentile 335–1522).
Reference: Pharmaco-invasive (P-I) strategy.
Gender, age, smoking, previous stroke, previous AMI, history of heart failure, diabetes, antihypertensive treatment, renal failure (eGFR < 60 mL/min), and out-of-hospital cardiac arrest.
P-I strategy, pharmaco-invasive strategy; pPCI, primary percutaneous coronary intervention.
Figure 2.
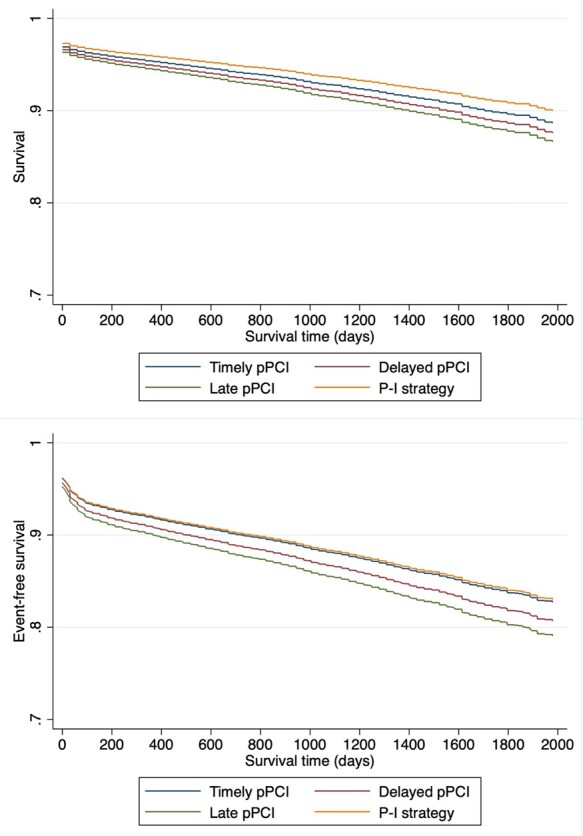
Adjusteda survival and event-free survival in patients with ST-elevation myocardial infarction receiving timely, delayed, and late pPCI compared to P-I strategy, Norway 2013–2019. aGender, age, smoking, previous stroke, previous myocardial infarction, history of heart failure, diabetes, antihypertensive treatment, renal failure (estimated glomerular filtration rate < 60 mL/min), and out-of-hospital cardiac arrest.
A total of 1276 (55%) patients in the P-I strategy group received fibrinolytic therapy within 120 min from onset of symptoms. Event-free survival did not differ from fibrinolytic therapy after 120 min from onset of symptoms (adjusted HR 1.0, 95% CI 0.8–1.3).
The proportional hazard assumption was fulfilled for all analyses.
Propensity score-matched cohorts
After the PS matching, 4676 patients were included in the timely pPCI—P-I strategy cohort, 2870 in the delayed pPCI—P-I strategy cohort, and 1938 in the late pPCI—P-I strategy cohort. Baseline characteristics of the three PS-matched cohorts were balanced with SMD below 0.1 in the delayed pPCI—P-I strategy cohort and the late pPCI—P-I strategy cohort. In the timely pPCI—P-I strategy cohort, the SMD was between 0.1 and 0.2 for male, previous MI, diabetes and smoking, but still acceptable (Supplementary material online, TableS2).
The rate of in-hospital complications in the PS matched cohorts is shown in Supplementary material online, TableS3. Major in-hospital bleeding was more frequent in the P-I strategy group compared to timely and delayed pPCI.
Using the P-I strategy as the reference group in all three cohorts, the HR and 95% CI for death were 1.2 (1.0–1.4) for timely pPCI, 1.3 (1.1–1.6) for delayed pPCI, and 1.6 (1.2–2.0) for late pPCI. For the composite of all-cause death, MI, or stroke, the HR for timely pPCI was 1.1 (0.9–1.3), for delayed pPCI 1.2 (1.0–1.4), and for late pPCI 1.4 (1.1–1.7) (Figures 3 and4).
Figure 3.
Outcomes in propensity score-matched patient cohorts with ST-elevation myocardial infarction receiving timely, delayed, and late pPCI compared to P-I strategy, Norway 2013–2019. P-I strategy: pharmaco-invasive strategy; pPCI, primary percutaneous coronary intervention (delayed: 121–180 min, late: >180 min).
Figure 4.
Survival and survival free of non-fatal stroke and non-fatal myocardial infarction in propensity score-matched cohorts of patients with ST-elevation myocardial infarction receiving timely, delayed, and late pPCI compared to P-I strategy, Norway 2013–2019. P-I strategy: pharmaco-invasive strategy; pPCI, primary percutaneous coronary intervention (delayed: 121–180 min, late: >180 min).
Discussion
In this nationwide study including all patients with STEMI admitted to hospitals in Norway from 2013 to 2019, 68% of the patients underwent pPCI, while 11% of patients were treated with a P-I strategy. As many as 18% of the patients with STEMI were not offered any reperfusion therapy at all. Only 61% of the patients treated with a pPCI strategy underwent pPCI within recommended timelines. In patients who did not have pPCI performed within 120 min, a P-I strategy was associated with better survival compared to delayed or late pPCI. However, major bleeding was more frequent in patients treated with P-I strategy compared to pPCI.
Early restoration of coronary blood flow is essential to optimize myocardial salvage and to reduce mortality in patients with MI.19 The ESC guidelines recommend early reperfusion with pPCI or a P-I strategy for all patients with STEMI.3 Nonetheless, this study showed that many patients in Norway were not offered reperfusion treatment. High age, comorbidities (e.g. high proportion smokers) and prehospital cardiac arrest and/or cardiogenic shock in some patients with STEMI, and consequently greater risk of complications to the treatment, may partly explain the finding. Geographical differences have previously been demonstrated in the treatment of MI in Norway, and more patients with MI were invasively assessed if they were admitted to hospitals with easy access to PCI facilities.20,21 In this study, we did not investigate whether there were geographical differences.
Achieving timely performance of pPCI is often more difficult than expected, and a large proportion of patients with STEMI in Norway were not offered reperfusion therapy within guideline-recommended time frames. Similar findings have been reported from other European countries.22–24 Potential causes are prehospital transportation delay, in-hospital delay at PCI-centres, or lack of fibrinolytic agents in the emergency medical services. Since in-hospital delay was short, and fibrinolytic agents available in most ambulances in the rural areas, transportation delay was the most probable reason for the treatment delay in our study population. Consequently, a P-I approach might have been a better option in many patients according to current guidelines.3
The STREAM trial showed effective reperfusion with prehospital fibrinolysis followed by timely coronary angiography in patients with STEMI who could not undergo primary PCI within 1 h after FMC, but no difference in survival between the P-I strategy and delayed pPCI groups.9 From the French registry of Acute ST-elevation and non-ST-elevation Myocardial Infarction (FAST-MI), Danchin et al.25 recently reported better long-term survival in patients treated with P-I therapy compared to delayed pPCI. The results of our study are in accordance with the findings from France, supporting a P-I strategy as an alternative strategy in patients who cannot receive timely pPCI.
Patients treated with P-I therapy were more likely to have a major bleeding complication during hospitalization compared to patients treated with pPCI. The increased risk of bleeding, especially intracranial bleeding, associated with fibrinolytic therapy is well known.5,26 The location of the bleeding is unfortunately not specified in NORMI. The additional risk of bleeding may be reduced by the dose reduction of tenecteplase for patients over 75 years as recommended in the recent ESC guidelines.3
The main strengths of this study are the large and unselected population comprising nearly all patients hospitalized with STEMI in Norway from 2013 to 2019 and a nearly complete follow-up. However, there are several important limitations associated with the study design and the NORMI. The study was an observational study, making it difficult to demonstrate causal associations between treatment and outcomes. Only STEMIs that led to hospitalization were registered in the NORMI. A few hospitals did not deliver complete data for the whole period, but the coverage compared with the Norwegian Patient Register was >90%.1 Information about time delay from symptom onset to FMC was missing in a proportion of patients. Furthermore, in 3566 patients (17%), more than 12 h had passed from symptom onset to FMC. In accordance with the exclusion criteria, these patients were excluded. This may however represent a potential selection bias since the excluded patients were older and had more comorbidity. We only obtained deidentified data from the NORMI and the Norwegian Patient Registry and could not verify the information through medical records at the individual patient level. Consequently, we have only been able to adjust for a limited number of covariates. Nevertheless, the degree of completeness and correctness of most variables in the NORMI have been shown to be high.27 However, unmeasured confounders still exist. NORMI used balloon time as reperfusion time for pPCI, despite ESC guidelines recommending use of wire passage time. We did not have the opportunity to correct for this. Parts of Norway have very scattered settlements with long distances to invasive hospitals. Generalization of the findings to other countries must therefore be done with great caution.
In conclusion, many patients still received reperfusion therapy later than the guideline-recommended timelines. Efforts should be made to reduce the time delay. In patients with long transfer distances to pPCI, this study has shown that a P-I strategy may be associated with improved outcomes compared to delayed/late pPCI. In accordance with current guidelines,3 a P-I strategy should be considered as an alternative reperfusion strategy in patients with long transfer distances to pPCI.
Supplementary material
Supplementary material is available at European Heart Journal – Cardiovascular Pharmacotherapy online.
Data availability
Raw data were generated at the Norwegian Institute of Public Health. Derived data supporting the findings of this study are available from the corresponding author on request.
Funding
This work was supported by the South-Eastern Norway Regional Health Authority, Hamar, Norway. The funder had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, or approval of the manuscript.
Conflict of interest: J.J. has received speaking fees from Amgen, AstraZeneca, BMS, Boehringer Ingelheim, Novartis, Pfizer and Sanofi.
S.H. has received speaking fees from Boehringer Ingelheim, BMS/Pfizer and Sanofi.
A.H.P. has no conflicts of interest.
Supplementary Material
Contributor Information
Jarle Jortveit, Department of Cardiology, Sørlandet Hospital, Arendal, Box 783, Stoa, 4809 Arendal, Norway.
Are Hugo Pripp, Oslo Centre of Biostatistics and Epidemiology, Oslo University Hospital, Oslo, Norway.
Sigrun Halvorsen, Department of Cardiology, Oslo University Hospital, Postboks 4956 Nydalen, 0424 Oslo, Norway.
References
- 1. Jortveit J, Govatsmark RE, Digre TA, Risoe C, Hole T, Mannsverk J, Slordahl SA, Halvorsen S.. Myocardial infarction in Norway in 2013. Tidsskr Nor Laegeforen 2014;134:1841–1846. [DOI] [PubMed] [Google Scholar]
- 2. Steg PG, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van 't Hof A, Widimsky P, Zahger D; Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569–2619. [DOI] [PubMed] [Google Scholar]
- 3. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119–177. [DOI] [PubMed] [Google Scholar]
- 4. Zijlstra F, Hoorntje JC, de Boer MJ, Reiffers S, Miedema K, Ottervanger JP, van 't Hof AW, Suryapranata H.. Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med 1999;341:1413–1419. [DOI] [PubMed] [Google Scholar]
- 5. Keeley EC, Boura JA, Grines CL.. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361:13–20. [DOI] [PubMed] [Google Scholar]
- 6. Widimsky P, Budesinsky T, Vorac D, Groch L, Zelizko M, Aschermann M, Branny M, St'asek J, Formanek P; ‘PRAGUE’ Study Group Investigators. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Final results of the randomized national multicentre trial–PRAGUE-2. Eur Heart J 2003;24:94–104. [DOI] [PubMed] [Google Scholar]
- 7. Andersen HR, Nielsen TT, Rasmussen K, Thuesen L, Kelbaek H, Thayssen P, Abildgaard U, Pedersen F, Madsen JK, Grande P, Villadsen AB, Krusell LR, Haghfelt T, Lomholt P, Husted SE, Vigholt E, Kjaergard HK, Mortensen LS; DANAMI-2 Investigators. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med 2003;349:733–742. [DOI] [PubMed] [Google Scholar]
- 8. Bonnefoy E, Lapostolle F, Leizorovicz A, Steg G, McFadden EP, Dubien PY, Cattan S, Boullenger E, Machecourt J, Lacroute JM, Cassagnes J, Dissait F, Touboul P; Comparison of Angioplasty and Prehospital Thromboysis in Acute Myocardial Infarction study group. Primary angioplasty versus prehospital fibrinolysis in acute myocardial infarction: a randomised study. Lancet 2002;360:825–829. [DOI] [PubMed] [Google Scholar]
- 9. Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Danays T, Lambert Y, Sulimov V, Rosell Ortiz F, Ostojic M, Welsh RC, Carvalho AC, Nanas J, Arntz HR, Halvorsen S, Huber K, Grajek S, Fresco C, Bluhmki E, Regelin A, Vandenberghe K, Bogaerts K, Van de Werf F, Team SI; STREAM Investigative Team. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med 2013;368:1379–1387. [DOI] [PubMed] [Google Scholar]
- 10. Boersma E, Maas AC, Deckers JW, Simoons ML.. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet 1996;348:771–775. [DOI] [PubMed] [Google Scholar]
- 11. Weaver WD, Cerqueira M, Hallstrom AP, Litwin PE, Martin JS, Kudenchuk PJ, Eisenberg M.. Prehospital-initiated vs hospital-initiated thrombolytic therapy. The Myocardial Infarction Triage and Intervention Trial. JAMA 1993;270:1211–1216. [PubMed] [Google Scholar]
- 12. Cannon CP, Bahit MC, Haugland JM, Henry TD, Schweiger MJ, McKendall GR, Shah PK, Murphy S, Gibson CM, McCabe CH, Antman EM, Braunwald E.. Underutilization of evidence-based medications in acute ST elevation myocardial infarction: results of the Thrombolysis in Myocardial Infarction (TIMI) 9 Registry. Crit Pathw Cardiol 2002;1:44–52. [DOI] [PubMed] [Google Scholar]
- 13. Puymirat E, Simon T, Cayla G, Cottin Y, Elbaz M, Coste P, Lemesle G, Motreff P, Popovic B, Khalife K, Labeque JN, Perret T, Le Ray C, Orion L, Jouve B, Blanchard D, Peycher P, Silvain J, Steg PG, Goldstein P, Gueret PJ, Belle L, Aissaoui N, Ferrieres J, Schiele F, Danchin N, Usik U; FAST-MI Investigators. Acute myocardial infarction: changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI Program (French Registry of Acute ST-Elevation or Non-ST-elevation Myocardial Infarction) 1995 to 2015. Circulation 2017;136:1908–1919. [DOI] [PubMed] [Google Scholar]
- 14. Aliprandi-Costa B, Morgan L, Snell L-C, D Souza M, Kritharides L, French J, Brieger D, Ranasinghe I.. ST-elevation acute myocardial infarction in Australia-temporal trends in patient management and outcomes 1999-2016. Heart Lung Circ 2019;28:1000–1008. [DOI] [PubMed] [Google Scholar]
- 15. Jernberg T, Johanson P, Held C, Svennblad B, Lindback J, Wallentin L; SWEDEHEART/RIKS-HIA. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA 2011;305:1677–1684. [DOI] [PubMed] [Google Scholar]
- 16. Danchin N, Puymirat E, Steg PG, Goldstein P, Schiele F, Belle L, Cottin Y, Fajadet J, Khalife K, Coste P, Ferrieres J, Simon T; FAST-MI 2005 Investigators. Five-year survival in patients with ST-segment-elevation myocardial infarction according to modalities of reperfusion therapy: the French Registry on Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) 2005 Cohort. Circulation 2014;129:1629–1636. [DOI] [PubMed] [Google Scholar]
- 17. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand J-P, Menasché P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon J-L, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S; ESC Committee for Practice Guidelines (CPG). Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551–2567. [DOI] [PubMed] [Google Scholar]
- 18. Govatsmark RE, Sneeggen S, Karlsaune H, Slordahl SA, Bonaa KH.. Interrater reliability of a national acute myocardial infarction register. Clin Epidemiol 2016;8:305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Anderson JL, Karagounis LA, Califf RM.. Metaanalysis of five reported studies on the relation of early coronary patency grades with mortality and outcomes after acute myocardial infarction. Am J Cardiol 1996;78:1–8. [DOI] [PubMed] [Google Scholar]
- 20. Melberg T, Thoresen M, Hansen JB, Westheim A.. [How are patients with acute coronary syndromes treated in Norwegian hospitals?]. Tidsskr Nor Laegeforen 2005;125:2925–2928. [PubMed] [Google Scholar]
- 21. Jortveit J, Halvorsen S.. Geographical differences in prescription of secondary preventive drug therapy after acute myocardial infarction in Norway. Eur Heart J Cardiovasc Pharmacother 2017;3:132–133. [DOI] [PubMed] [Google Scholar]
- 22. Authors/Task Force M, Ryden L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes HP, Huikuri H, Marre M, Marx N, Mellbin L, Ostergren J, Patrono C, Seferovic P, Uva MS, Taskinen MR, Tendera M, Tuomilehto J, Valensi P, Zamorano JL, Guidelines E, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Document R, De Backer G, Sirnes PA, Ezquerra EA, Avogaro A, Badimon L, Baranova E, Baumgartner H, Betteridge J, Ceriello A, Fagard R, Funck-Brentano C, Gulba DC, Hasdai D, Hoes AW, Kjekshus JK, Knuuti J, Kolh P, Lev E, Mueller C, Neyses L, Nilsson PM, Perk J, Ponikowski P, Reiner Z, Sattar N, Schachinger V, Scheen A, Schirmer H, Stromberg A, Sudzhaeva S, Tamargo JL, Viigimaa M, Vlachopoulos C, Xuereb RG.. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 2013;34:3035–3087. [DOI] [PubMed] [Google Scholar]
- 23. Puymirat E, Battler A, Birkhead J, Bueno H, Clemmensen P, Cottin Y, Fox KA, Gorenek B, Hamm C, Huber K, Lettino M, Lindahl B, Muller C, Parkhomenko A, Price S, Quinn T, Schiele F, Simoons M, Tatu-Chitoiu G, Tubaro M, Vrints C, Zahger D, Zeymer U, Danchin N;. EHS 2009 snapshot participants. Euro Heart Survey 2009 Snapshot: regional variations in presentation and management of patients with AMI in 47 countries. Eur Heart J Acute Cardiovasc Care 2013;2:359–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jager B, Haller PM, Piackova E, Kaff A, Christ G, Schreiber W, Weidinger F, Stefenelli T, Delle-Karth G, Maurer G, Huber K, Vienna SRG; for the Vienna STEMI Registry Group. Predictors of transportation delay in patients with suspected ST-elevation-myocardial infarction in the VIENNA-STEMI network. Clin Res Cardiol 2020;109:393–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Danchin N, Popovic B, Puymirat E, Goldstein P, Belle L, Cayla G, Roubille F, Lemesle G, Ferrieres J, Schiele F, Simon T; the FAST-MI Investigators. Five-year outcomes following timely primary percutaneous intervention, late primary percutaneous intervention, or a pharmaco-invasive strategy in ST-segment elevation myocardial infarction: the FAST-MI programme. Eur Heart J 2020;41:858–866. [DOI] [PubMed] [Google Scholar]
- 26. Gurwitz JH, Gore JM, Goldberg RJ, Barron HV, Breen T, Rundle AC, Sloan MA, French W, Rogers WJ.. Risk for intracranial hemorrhage after tissue plasminogen activator treatment for acute myocardial infarction. Participants in the National Registry of Myocardial Infarction 2. Ann Intern Med 1998;129:597–604. [DOI] [PubMed] [Google Scholar]
- 27. Govatsmark RES, Janszky I, Slordahl SA, Ebbing M, Wiseth R, Grenne B, Vesterbekkmo E, Bonaa KH.. Completeness and correctness of acute myocardial infarction diagnoses in a medical quality register and an administrative health register. Scand J Public Health 2020;48:5–13. 1403494818803256. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Raw data were generated at the Norwegian Institute of Public Health. Derived data supporting the findings of this study are available from the corresponding author on request.