Abstract
Chronic prurigo is a pruritic disease characterized by the development of pruriginous lesions due to scratching. The number of lesions is representative of the stage of the disease, while the presence of excoriations reflects the scratching activity. Aim of this study was to validate a new developed tool for the objective assessment of chronic prurigo. Investigator’s Global Assessment scales for stage and activity were completed for 187 patients with chronic prurigo, who also reported patient-reported outcomes for itch intensity and quality of life. To assess the reliability and objectivity of the Investigator’s Global Assessment, 5 independent raters completed the Investigator’s Global Assessment scales for 8 patients twice. The scores increased with increased intensity of pruritus. The Investigator’s Global Assessment stage scales correlated strongly with each other (Kendall’s-tau-b 0.62) and moderately with the Investigator’s Global Assessment activity scale (Kendall’s-tau-b 0.47). Intra-rater test–retest reliability was excellent for all items, while the congruence among raters was very good for Investigator’s Global Assessment – chronic prurigo activity (Kendall’s W 0.84) and good for Investigator’s Global Assessment stage scales (Kendall’s W 0.747). Investigator’s Global Assessment – chronic prurigo stage and activity are thus the best Investigator’s Global Assessment instruments for use in assessing chronic prurigo.
Key words: prurigo nodularis, chronic pruritus, itch
Chronic prurigo (CPG) is a burdensome, highly pruritic, chronic skin disease based on neuroimmune mechanisms (1–3). The presence of symmetrically distributed papular, nodular or other (plaques, umbilicated, linear) various pruriginous lesions is typical (1, 4, 5). The dominant subtype is chronic nodular prurigo (CNPG; also termed prurigo nodularis). Disease healing is characterized by flattening of the lesions until they disappear and leave behind a white or skin-coloured scar. In contrast to the reduced elevation during healing, the base of the lesions remains unchanged: a nodule shows the same circumference during regression and does not degrade into a papule. This observation makes monitoring the disease during clinical trials difficult, as investigators cannot memorize the stage of elevation or flattening for multiple lesions compared with previous visits. The flattening of individual lesions needs to be calculated by virtual methods, using imaging techniques for comparison; however, such techniques are currently unavailable (6). This observation prompted us to develop an alternative investigator assessment, based on the number of active lesions vs healed ones. We had previously developed and validated the Prurigo Activity and Severity Score (PAS), a comprehensive instrument to describe CPG (7). It was found that the estimated number of lesions on the whole body, corresponding to PAS item #2, is representative of the severity stage of the disease: an inter-item correlation analysis showed a high association with all other items (7). An early sign of CPG improvement, along with the interruption of scratching, is the disappearance of crusts and erosions from the top of the lesions (7, 8). Based on this, we developed 2 Investigator’s Global Assessments (IGA) for CPG; one for the current stage (estimated number of lesions) and one for the scratching activity. The first IGA was developed into two versions; a general version designed for all CPG subtypes, and a second version only for CNPG, the most frequent subtype (Table I). We report here the validation results for these novel instruments.
Fig. 1.
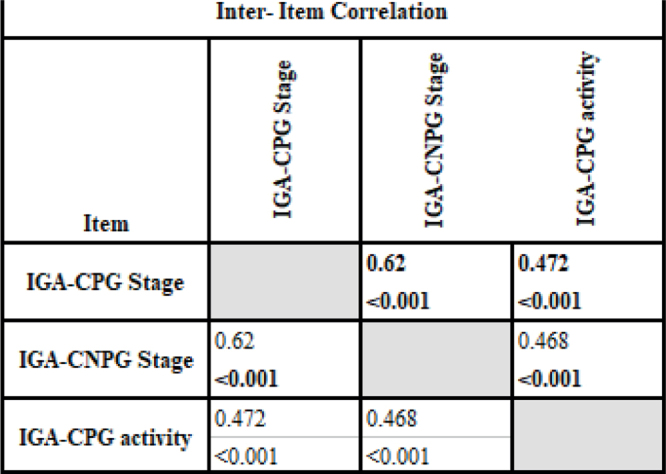
Inter-item correlation of Investigator Global Assessment (IGA). Medium grey: moderate correlation; darker grey: strong correlation. CPG: chronic prurigo; CNPG: chronic nodular prurigo.
SIGNIFICANCE
Chronic prurigo is a skin disease characterized by the presence of severely itchy skin lesions, such as nodules or papules, which are caused by scratching over a long period. To date, there is no uniform documentation available for the skin lesions. “Investigator’s Global Assessments” are helpful for medical documentation of the skin lesions. For chronic prurigo, they are divided into 2 parts; one for the proportion of excoriations on the existing lesions and one for the total number of skin lesions. In this study we were able to validate the new tools for an objective assesment.
MATERIALS AND METHODS
Patient population and validation procedure
After providing written informed consent, 187 consecutive adult patients with CPG (clinically and histologically confirmed) were included in this prospective, longitudinal, uncontrolled, non-interventional study between November 2017 and February 2020. The ethics committee of the University of Münster approved the study, which was registered in the German Clinical Trials Register (DRKS00005383). Three trained investigators completed the IGA – chronic prurigo (IGA-CPG) stage, IGA – chronic nodular prurigo (IGA-CNPG) stage and IGA-CPG activity (Table I) and then counted all pruriginous lesions (papules, nodules, ulcers, plaques) in each patient. Patients completed electronically itch intensity scales (on a numerical rating scale (NRS): worst itch in the previous 24 h and in the previous 4 weeks) and instruments measuring the impairment in quality of life (Dermatology Quality of Life Index (DLQI) (9) and ItchyQoL).
Table I.
Investigator Global Assessment (IGA) for stage of chronic prurigo (CPG), chronic nodular prurigo (CNPG) and signs of activity in chronic prurigo
| Score | Category | Description |
|---|---|---|
| IGA-CPG stage | ||
| 0 | Clear | No pruriginous lesions (0 lesions) |
| 1 | Almost clear | Rare palpable pruriginous lesions (approximately 1–5 lesions) |
| 2 | Mild | Few palpable pruriginous lesions (approximately 6–19 lesions) |
| 3 | Moderate | Many palpable pruriginous lesions (approximately 20–100 lesions) |
| 4 | Severe | Abundant palpable pruriginous lesions (over 100 lesions) |
| IGA-CNPG stage | ||
| 0 | Clear | No nodules (0 nodules) |
| 1 | Almost clear | Rare palpable pruriginous nodules (approximately 1–5 nodules) |
| 2 | Mild | Few palpable pruriginous nodules (approximately 6–19 nodules) |
| 3 | Moderate | Many palpable pruriginous nodules (approximately 20–100 nodules) |
| 4 | Severe | Abundant palpable pruriginous nodules (over 100 nodules) |
| IGA-CPG activity | ||
| 0 | Clear | No pruriginous lesions have excoriations or crusts |
| 1 | Almost clear | Very small proportion of pruriginous lesions have excoriations or crusts (up to approximately 10% of all pruriginous lesions) |
| 2 | Mild | Minority of pruriginous lesions have excoriations or crusts (approximately 11–25% of all pruriginous lesions) |
| 3 | Moderate | Many pruriginous lesions have excoriations or crusts (approximately 26–75% of all pruriginous lesions) |
| 4 | Severe | Majority of pruriginous lesions have excoriations or crusts (approximately 76–100% of all pruriginous lesions) |
Test–retest procedure
In order to assess the reliability and objectivity of the IGA, 5 experienced dermatologists (“raters”) who were not involved in the validation data sampling completed the IGAs for 8 randomly chosen patients with CPG from the total study population twice within 1 h. The raters were asked to complete a feasibility questionnaire regarding the practicability and usefulness of the individual measuring instruments.
Statistical analysis
Statistical analyses were performed with SPSS 25.0 for Windows (IBM Corporation, Armonk, NY, USA). The level of significance was defined at p ≤ 0.05. The mean and medians, standard deviations (SD), quartiles, minimal, and maximal values, as well as frequencies, were calculated. The intraclass correlation coefficient (ICC) was calculated for test–retest reliability. Pearson’s χ2 test was used for inter-item correlation. Correlation coefficients were calculated between IGA and the external constructs NRS, DLQI, ItchyQoL, number of pruriginous lesions and items 2 and 5a/b from the PAS 1.0 to test for convergent validity. For concurrent validity testing, the NRS scores were grouped into bandings according to Reich et al. (10).
RESULTS
Between November 2017 and February 2020, 187 patients (104 females (55.6%); mean age 66.1 ± 13.1 years) were enrolled (Table II).
Table II.
Demographics, itch and prurigo characteristics
| Characteristics | |
|---|---|
| Number | 187 |
| Female, % | 55.6 |
| Age, years, mean (SD) | 66.11 (13.1) |
| Chronic prurigo underlying cause, % | |
| Dermatosis | 22.1 |
| Neurological | 41.4 |
| Systemic | 13.1 |
| Psychic | 0.7 |
| Multifactorial | 14.5 |
| Unclear | 8.3 |
| Exact number of all pruriginous lesions | |
| Range | 0–493 |
| Mean (SD) | 103.7 (96.5) |
| Median (IQR) | 79.0 (31.0–146.5) |
| Numerical rating scale worst 24 h | |
| Mean (SD) | 5.9 (2.3) |
| Median | 6.0 |
| Numerical rating scale worst 4 weeks | |
| Mean (SD) | 7.6 (2.7) |
| Median | 8.0 |
| Dermatology Life Quality Index | |
| Mean (SD) | 11.2 (6.8) |
| Median | 10.0 |
| ItchyQoL | |
| Mean (SD) | 72.4 (15.4) |
| Median | 74.8 |
| ItchyQoL-S | |
| Mean (SD) | 21.6 (4.5) |
| Median | 22.8 |
| ItchyQoL-E | |
| Mean (SD) | 28.8 (17.1) |
| Median | 27.9 |
| ItchyQoL-F | |
| Mean (SD) | 22.8 (6.5) |
| Median | 23.1 |
ItchyQoL-E: ItchyQoL subscore “Emotions”; ItchyQoL-F: ItchyQoL subscore “Functioning”; ItchyQoL-S: ItchyQoL subscore “Symptoms”; SD: standard deviation.
Test–retest reliability in the random sample of 8 patients and 5 raters
Based on the demographic characteristics, the reliability sample was representative of the total study population. The intra-rater test–retest reliability was excellent for all items (ICC IGA-CPG-stage 0.915; ICC IGA-CNPG stage 0.874; ICC IGA-CPG activity 0.972). Congruence among raters was very good in IGA-CPG activity (Kendall’s W 0.837) and good in the IGA-CPG (Kendall’s W 0.747) and IGA-CNPG stages (Kendall’s W 0.747).
Feasibility of 5 independent raters
No intelligibility problems were specified during the completion of all measuring instruments, which took less than 1 min per instrument. All raters considered the IGA-CPG activity and the IGA-CPG stage to be suitable tools for assessing the progress of CPG. Four examiners rated the IGA-CPG activity and IGA-CPG stage as 1 (“very good”). One rating was missing.
Four raters considered IGA-CNPG stage as a suitable instrument for follow-up of CNPG. One rater noted that it could be difficult to assess the course of CNPG without documenting the other concomitant pruriginous lesions. Three examiners rated the IGA-CNPG with a 2 (“good”), one with a grade of 1 (“very good”), and another gave no information.
Inter-item correlation of Investigator Global Assessment
The correlation between the IGA-CPG stage, IGA-CNPG stage and IGA-CPG activity was significant (p < 0.001). The IGA-CPG stage and IGA-CNPG stage correlated strongly with each other (Kendall’s-tau-b 0.62) and the IGA-CPG activity moderately with the IGA-CPG stage (Kendall’s-tau-b 0.472) and IGA-CNPG stage (Kendall’s-tau-b 0.468) (Fig. 1).
Convergent validity
Strong correlations were found between the IGA-CPG stage and PAS item #2 (estimation of the total number of pruriginous lesions; t = 0.794, p < 0.01), as well as the total counted number of all pruriginous lesions (t = 0.729, p < 0.01). The IGA-CPG activity also strongly correlated with the PAS item #5a (pruriginous lesions with excoriations and/or crusts on top; t = 0.759, p < 0.01). Very weak or weak correlations were found for IGA-CNPG and between the NRS worst and instruments for measuring quality of life (Fig. 2).
Fig. 2.
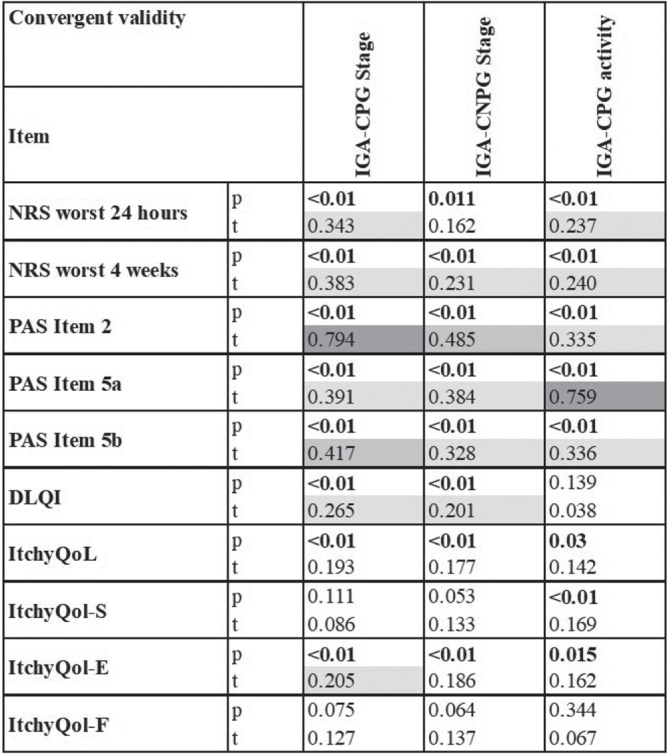
Convergent validity. Light grey: weak correlation; medium grey: moderate correlation; darker grey: strong correlation. DLQI: Dermatology Life Quality Index; ItchyQoL-E: ItchyQoL subscore “Emotions”; ItchyQoL-F: ItchyQoL subscore “Functioning”; ItchyQoL-S: ItchyQoL subscore “Symptoms”; NRS: numerical rating scale; p: p-value; PAS Item 2: estimation of the total number of pruriginous lesions; PAS Item 5a: percentage of pruriginous lesions with excoriations and/or crusts on top; PAS Item 5b: percentage of healed pruriginous; t: Kendall’s correlation coefficient.
Concurrent validity
With increasing pruritus intensity measured according to the worst NRS in the last 24 h and in the last 4 weeks, and categorized according to Reich et al. (10), the mean value of the different IGAs increased (Fig. 3).
Fig. 3.
Concurrent validity. Analysis in patients with no, mild, moderate, severe and very severe pruritus revealed differences. The Investigator Global Assessment (IGA) score increased with greater pruritus intensity. Significant differences between the characteristics of the groups were determined with the Kruskal–Wallis test. CPG: chronic prurigo; CNPG: chronic nodular prurigo; NRS: numerical rating scale.
DISCUSSION
A reliable assessment of CPG in routine care and, especially in clinical trials, is essential to document the disease course, treatment efficacy, and to capture, if present, the disease modifying potency of a drug. This study aims to describe and validate novel, short instruments to assess CPG, especially in clinical trials, as this indication is currently the focus of the pharmaceutical development (11). As such, the investigator assessment must be based on representative skin lesions. To date, CPG has not been assessed directly, but instead by instruments focusing on itch and impairment in quality of life (12). We excluded the subjective symptoms from this objective approach and suggest continuing to use specific itch intensity scales, such as the numerical rating scale (NRS), to make an assessment of the course of itch. CPG can be clinically characterized by multiple parameters, such as the type of lesions (papules, nodules, plaques), their individual size, individual quantity on a patient, elevation, distribution, stage of healing (resolution), and signs of scratch activity (excoriations/crusts). Previous studies (7, 8, 13) have shown that the estimated or total counted number of lesions is a representative marker for CPG disease severity and thus can serve as a reliable monitoring instrument. Other approaches, such as measuring the size (longitudinal or height) of individual pruriginous lesions, did not perform well in previous studies, and thus do not constitute representative items for an IGA (7, 8, 13, 14). For development of the IGA, we used a categorization and wording internationally accepted for the assessment of inflammatory dermatoses (15, 16). CPG is a relatively rare disease and patients are mostly treated in specialized centres (17, 18). Thus, it was decided to use the estimated number of lesions in order to describe the stage. This serves as a directory for non-experienced dermatologists to select the proper stage, which is especially essential in clinical trials. Analysis of the test–retest procedure showed excellent test–retest reliability in all IGAs (ICC all > 0.87). The inter-rater reliability was very good (Kendall’s W 0.837), especially in the IGA-CPG activity. However, the IGA-CPG stage and IGA-CNPG stage were also good (Kendall’s W 0.747).
Interestingly, in the convergent and concurrent validity assessments, the IGA-CPG performed better in comparison with the IGA-CNPG. The IGA-CPG allows a broader assessment, since all other non-nodular pruriginous lesions can also be included. In general, most patients show a mixture of different CPG lesions, although one lesion may predominate (Fig. 4) (1, 4). The advantage of the IGA-CPG is that a clear assessment can be made without uncertainty as to whether lesions shall be included and without a loss of information. Moreover, our raters preferred the IGA-CPG over the IGA-CNPG.
Fig. 4.

Clinical example of chronic nodular prurigo. A patient with chronic nodular prurigo showing nodules (blue arrow) and papules (yellow arrow; lesions less than 1 cm in diameter).
The IGA-CPG for assessment of activity showed good reliability amongst the raters. Similar to the IGA-CPG stage, the IGA-CPG activity showed better concurrent validity data. The IGA-CPG activity was also graded as very good by the raters and considered feasible and acceptable for determining CPG activity. The IGAs for stage and activity only moderately correlate with one another, clearly showing that they assess different aspects of the disease.
In conclusion, the use of IGAs can simplify the objective clinical assessment of CPG. This study found IGA-CPG stage and activity to be the most suitable IGA instruments currently available, especially for inclusion of patients in clinical trials.
ACKNOWLEDGEMENTS
The authors thank Sina Niemeyer, Linda Baus and Louisa Oste for their contribution towards recruitment and the dean’s office for CZ’s exemption.
We acknowledge the support provided by the European Academy of Dermatology and Venereology (EADV, number 2016-012 to MP).
Footnotes
Conflicts of interest. CZ reports personal fees from Beiersdorf and Dermasence and is a investigator for Sanofi, Abbvie, Boerhinger Ingelheim, Novartis, MSD, Pfizer outside the submitted work. MPP reports personal fees from Galderma, personal fees from Menlo Therapeutics, personal fees from Trevi Therapeutics, personal fees from Novartis outside the submitted work. MA reports grants and personal fees from Abbott/AbbVie, Amgen, Biogen Idec, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly, Forward Pharma, Galderma, GSK, Hexal, Janssen, LEO Pharma, Medac, MSD, Novartis, Pfizer, Sandoz, Teva, TK, Trevi, and Xenoport. outside the submitted work. SS reports personal fees from Almirall, personal fees from Beiersdorf, personal fees from Bellus Health, personal fees from Cara Therapeutics, personal fees from Celgene, personal fees from Galderma Laboratorium, personal fees from Clexio Biosciences, personal fees from LEO, personal fees from Menlo Therapeutics, personal fees from Novartis, personal fees from Sienna Biopharmaceuticals, personal fees from Trevi Therapeutics, personal fees from Vanda Pharmaceuticals, other from Dermasence, other from Kiniksa, other from Galderma, personal fees from Galderma S.A., other from Menlo Therapeutics, other from Novartis, other from Trevi Therapeutics, outside the submitted work. MS has no conflicts of interest to declare.
REFERENCES
- 1.Pereira MP, Steinke S, Zeidler C, Forner C, Riepe C, Augustin M, et al. European academy of dermatology and venereology European prurigo project: expert consensus on the definition, classification and terminology of chronic prurigo. J Eur Acad Dermatol Venereol 2018; 32: 1059–1065. [DOI] [PubMed] [Google Scholar]
- 2.Pereira MP, Hoffmann V, Weisshaar E, Wallengren J, Halvorsen JA, Garcovich S, et al. Chronic nodular prurigo: clinical profile and burden. A European cross-sectional study. J Eur Acad Dermatol Venereol 2020; 34: 2373–2383. [DOI] [PubMed] [Google Scholar]
- 3.Zeidler C, Stander S. The pathogenesis of prurigo nodularis – ‘super-itch’ in exploration. Eur J Pain 2016; 20: 37–40. [DOI] [PubMed] [Google Scholar]
- 4.Pereira MP, Zeidler C, Nau T, Bobko S, Evers AWM, Garcovich S, et al. Position statement: linear prurigo is a subtype of chronic prurigo. J Eur Acad Dermatol Venereol 2019; 33: 263–266. [DOI] [PubMed] [Google Scholar]
- 5.Schedel F, Schurmann C, Metze D, Stander S. Prurigo. Klinische Definition und Klassifikation. Hautarzt 2014; 65: 684–690. [DOI] [PubMed] [Google Scholar]
- 6.Bruland P, Hanse W, Schedel F, Stander S, Fritz F. PIACS: A system for the automatic detection, categorization and comparison of scratch-related skin lesions in dermatology. Stud Health Technol Inform 2015; 216: 1042. [PubMed] [Google Scholar]
- 7.Polking J, Zeidler C, Schedel F, Osada N, Augustin M, Metze D, et al. Prurigo Activity Score (PAS): validity and reliability of a new instrument to monitor chronic prurigo. J Eur Acad Dermatol Venereol 2018; 32: 1754–1760. [DOI] [PubMed] [Google Scholar]
- 8.Siepmann D, Lotts T, Blome C, Braeutigam M, Phan NQ, Butterfass-Bahloul T, et al. Evaluation of the antipruritic effects of topical pimecrolimus in non-atopic prurigo nodularis: results of a randomized, hydrocortisone-controlled, double-blind phase II trial. Dermatology 2013; 227: 353–360. [DOI] [PubMed] [Google Scholar]
- 9.Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) – a simple practical measure for routine clinical use. Clin Exp Dermatol 1994; 19: 210–216. [DOI] [PubMed] [Google Scholar]
- 10.Reich A, Chatzigeorkidis E, Zeidler C, Osada N, Furue M, Takamori K, et al. Tailoring the cut-off values of the visual analogue scale and numeric rating scale in itch assessment. Acta Derm Venereol 2017; 97: 759–760. [DOI] [PubMed] [Google Scholar]
- 11.Pereira MP, Mittal A, Ständer S. Current treatment strategies in refractory chronic pruritus. Curr Opin Pharmacol 2018; 46: 1–6. [DOI] [PubMed] [Google Scholar]
- 12.Steinke S, Zeidler C, Riepe C, Bruland P, Soto-Rey I, Storck Met al. Humanistic burden of chronic pruritus in patients with inflammatory dermatoses: results of the European Academy of Dermatology and Venereology Network on Assessment of Severity and Burden of Pruritus (PruNet) cross-sectional trial. J Am Acad Dermatol 2018; 79: 457–463.e5. [DOI] [PubMed] [Google Scholar]
- 13.Schedel F, Schürmann C, Augustin M. Prurigo nodularis: introduction of a re-defined classification and Prurigo Activity Score (PAS). Acta Derm Venereol 2013; 93: 610. [Google Scholar]
- 14.Wong SS, Goh CL. Double-blind, right/left comparison of calcipotriol ointment and betamethasone ointment in the treatment of prurigo nodularis. Arch Dermatol 2000; 136: 807–808. [DOI] [PubMed] [Google Scholar]
- 15.Breuer K, Braeutigam M, Kapp A, Werfel T. Influence of pimecrolimus cream 1% on different morphological signs of eczema in infants with atopic dermatitis. Dermatology 2004; 209: 314–320. [DOI] [PubMed] [Google Scholar]
- 16.Simpson E, Bissonnette R, Eichenfield LF. The validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD): The development and reliability testing of a novel clinical outcome measurement instrument for the severity of atopic dermatitis. J Am Acad Dermatol 2020; 83: 839–846. [DOI] [PubMed] [Google Scholar]
- 17.Pereira MP, Steinke S, Bruland P, Ständer HF, Dugas M, Augustin Met al. Management of chronic pruritus: from the dermatological office to the specialized itch center. A review. Itch 2017; 2: e06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dantas LD, Bakos L, Balbinot G, Drechsler CE, Eidt LM. Prevalence of dermatoses in dermatologic evaluation requests from patients admitted to a tertiary hospital for 10 years. An Bras Dermatol 2015; 90: 762–764. [DOI] [PMC free article] [PubMed] [Google Scholar]



