Hidradenitis suppurativa (HS) is a chronic skin disease, which manifests as painful abscesses, fistulas and scarring lesions (1). The estimated prevalence of HS is approximately 1% of the general population (2, 3).
HS-related quality of life (QoL) is significantly impaired due to the physical and psychological symptoms, resulting in depression, anxiety, stigmatization and fatigue (4, 5). QoL among patients with HS is also reduced, especially in extremely severe cases, due to various complications, such as contractures of the limbs, lesion-related squamous cell carcinomas, fistulas into the joints and urinary tract, and genital lymphoedema (1).
Massive scrotal lymphoedema, resulting in genital deformation, was initially termed penoscrotal elephantiasis (6). Genital elephantiasis includes congenital and acquired (secondary) cases (6–8). The incidence of this syndrome in association with HS is not fully known; only a few cases have been reported, with scarring as a main considered pathogenetic factor. Massive genital lymphoedema could obstruct personal hygiene and lead to urinary incontinence, non-aesthetic appearance, loss of libido, and interfere with sexual intercourse, negatively influencing QoL.
The aim of this study was to report and assess the outcomes of surgical management of genital elephantiasis in patients with HS, with regard to improvements in their QoL.
MATERIALS AND METHODS
Ethical approval was obtained from the Bioethics Committee at the Medical University of Wroclaw, Pasteura 1 (No 432/2015) and a total of 7 patients (4 men and 3 women) were recruited from our clinic for prospective study during two years’ time (2017–2018). Inclusion criteria were: adults with Hurley stage III HS with presentation of genital elephantiasis. Other diseases that could result in genital elephantiasis were ruled out.
The diagnosis of HS was made accordingly to well-established clinical criteria (1). All patients with any significant co-morbidities or abnormalities, such as anxiety disorders, depression, and other mental disorders that might jeopardize the results, were excluded. Moreover, patients with HS were screened for metabolic disorders, which might affect the healing process. Clinical manifestation of disease staging was based on Hurley’s 3-degree scale (1). Patients did not receive any concomitant anti-inflammatory treatment.
The age range of study participants was 32–58 years (mean 41.0 ± 8.6 years), and the mean disease duration was 14.0 ± 7.3 years. All included patients were heavy smokers (mean 22.4 ± 9.1 pack-years) and all were overweight (mean body mass index (BMI) 31.6 ± 3.5 kg/m2).
The surgical approach was tailored to each individual and aimed to restore the best possible functional and visual effect. All surgeries were performed under general and/or tumescent local anaesthesia.
The genital elephantiasis was treated by the wide excision of the affected genital areas encompassing all lesions or the whole area of the given body region – in which the disease may possibly spread. The margins of the excised unaffected tissues were established individually. Surgical reconstruction was then performed, using the following combined surgical modalities: partial suture with secondary intention healing (SIH); partial suture with graft; or local flap techniques with partial SIH.
Demographic data and disease history were collected from all participants. The wide spectrum of psychophysical aspects was evaluated, with Polish language versions of multiple questionnaires, including the Dermatology Life Quality Index (DLQI), 13-item Beck Depression Inventory (BDI), Functional Assessment of Chronic Illness Therapy – Fatigue scale (FACIT-F), the scale of stigmatization assessment by A. Evers (6-Item Stigmatization Scale) and the Euro-QoL-5D (EQ-5D) health questionnaire.
In addition, 3 months after surgery a questionnaire assessing the cosmetic and functional effects of the surgical treatment was applied, in which patients scored the effects as: 1: unacceptable, 2: acceptable, 3: good, or 4: perfect. Moreover, in a subsequent questionnaire assessing symptoms accompanying the perioperative period, patients were asked to indicate the incidence of complications, such as pain, infection and contracture.
The assessments were performed before and 3 months after the surgical interventions.
Statistical analysis
All data were assessed for parametric or non-parametric distribution. Differences between groups were determined using the Wilcoxon signed-rank test and Student’s t-test with reference to the distribution of evaluated variables (abnormal or normal, respectively). A p-value < 0.05 was considered statistically significant. Statistical analyses were performed using Statistica 12 software (StatSoft, Tulsa, OK, USA).
RESULTS
Overall improvement in QoL occurred in all patients after surgery for genital elephantiasis. According to the DLQI, the mean score before and after treatment differed significantly and was assessed as 16.7 ± 3.9 points (range 10–22 points) and 13.7 ± 4.7 points (range 7–20 points), respectively (p < 0.05). Health-related QoL, assessed with the EQ-5D questionnaire, was also considerably higher after surgery (p < 0.05); however, according to the EQ-5D-VAS no statistical differences were observed among patients before and after surgery (59.9 ± 10.5 vs 62.1 ± 9.6 points). The mean result of the 13-item BDI in patients with HS was significantly lower (p < 0.05) after surgery and was estimated as 5.6 ± 2.38 points (range 3–10 points) vs an initial 8.6 ± 2.06 points (range 6–12 points). Furthermore, the outcome of surgery among 3 patients with initial scoring above 10 points (indicating the possibility of depression) resulted in a reduction in BDI scoring to below 10 points in 2 of them (10 points vs 8 points and 10 points vs 5 points). Regarding the FACIT-F, clinically significant fatigue was observed in 85.7% and 57.1% of patients with HS before and after treatment, respectively (p < 0.05). Moreover, stigmatization levels among patients with HS were markedly lower after surgical treatment (6.3 ± 1.91 vs 4.7 ± 1.58 points, p < 0.05).
The cosmetic effects of conducted surgical therapy were assessed as good or acceptable (43% in both groups), whereas only 14% of patients did not accept the cosmetic outcome (Fig. 1). Regarding functional effects, all of the patients assessed them positively (71% acceptable, 29% good). With reference to post-operative complications, it is notable that a group of patients did not experience any side-effects (43%). Some of the patients with HS experienced pain, contracture or infection (29%, 14%, 14%, respectively).
Fig. 1.
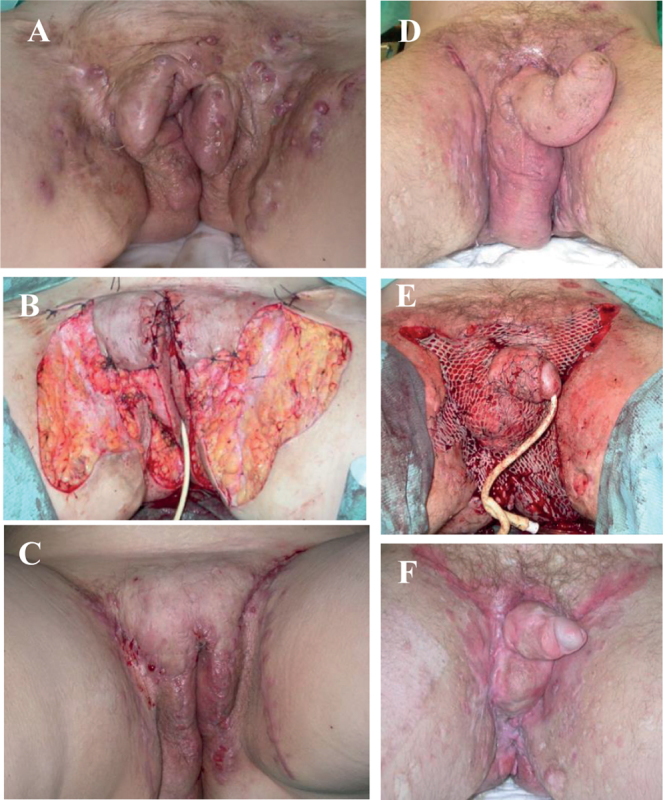
Representative clinical images of patients with genital elephantiasis. (A, D) Pre-surgery; (B) pubic flaps with secondary intention healing; (E) wide excision with split thickness skin graft; (C, F) postsurgical outcomes.
DISCUSSION
The enormous impact of HS on QoL has been shown in numerous studies. The majority of patients experience impairment in both everyday life (90–97%) and professional life (60%) (9, 10). Thus, current guidelines for treatment of HS state that surgery is one of the best options, especially in severe cases connected with scarring in the affected areas. Depending on the severity of the disease, the disease localization, patients’ general condition, and the surgeon’s experience, numerous surgical techniques can be recommended. Moreover, in a recent study by a Dutch group (11), major surgery significantly reduced patients’ impairments in overall work and daily activity.
To the best of our knowledge this is the first prospective single-centre study on the influence of surgery on the psychosocial status of patients with genital elephantiasis due to HS. All patient-reported outcomes demonstrated similar trends to previous studies assessing the impact of general surgical management in HS (2, 11, 12).
The current study confirms that wide local excision followed by reconstruction improves QoL in the vast majority of patients, and reduces stigmatization and fatigue levels. Moreover, there was a statistically significant reduction in depression scores. It is important to highlight that 29% of patients after the performed treatment were no longer in the group of clinically suspected depression. Patients with HS also evaluated the cosmetic and functional aspects of surgical treatment as positive.
Genital elephantiasis secondary to HS is a challenging disease, which can be extensive, and causes both physical and psychosocial distress. A multidisciplinary approach, with an excisional surgery and appropriate reconstructive procedure, should be tailored to individual patients in order to achieve a good outcome.
This study has some limitations. It has a single-centre design. Hence, the number of cases was limited as genital elephantiasis due to HS is a rare phenomenon.
In conclusion, surgery for genital elephantiasis secondary to HS can be considered as an efficacious treatment modality for this complication. As surgical treatment requires experience, we suggest grouping suitable patients in specialized centres in order to provide the best possible care.
ACKNOWLEDGEMENTS
The study was carried out as a part of the project “Young Researcher” (number STM.C260.20.08).
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Zouboulis CC, Desai N, Emtestam L, Hunger RE, Ioannides D, Juhász I, et al. European S1 guideline for treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol 2015; 29: 619–644. [DOI] [PubMed] [Google Scholar]
- 2.Jemec GB, Heidenheim M, Nielsen NH. The prevalence of hidradenitis suppurativa and its potential precursor lesions. J Am Acad Dermatol 1996; 35: 191–194. [DOI] [PubMed] [Google Scholar]
- 3.Revuz JE, Canoui-Poitrine F, Wolkenstein P, Viallette C, Gabison G, Pouget F, et al. Prevalence and factors associated with hidradenitis suppurativa: results from two case-control studies. J Am Acad Dermatol 2008; 59: 596–601. [DOI] [PubMed] [Google Scholar]
- 4.von der Werth JM, Jemec GB. Morbidity in patients with hidradenitis suppurativa. Br J Dermatol 2001; 144: 809–813. [DOI] [PubMed] [Google Scholar]
- 5.Matusiak L, Bieniek A, Szepietowski JC. Psychophysical aspects of hidradenitis suppurativa. Acta Derm Venereol 2010; 90: 264–268. [DOI] [PubMed] [Google Scholar]
- 6.Cook G: Manson’s Tropical Diseases, 20th edn. (International student edition). London: WB Saunders, 1998: 1322–1338. [Google Scholar]
- 7.Nelson RA, Alberts GL, King LE Jr. Penile and scrotal elephantiasis caused by indolent Chlamydia trachomatis infection. Urology 2003; 61: 224. [DOI] [PubMed] [Google Scholar]
- 8.Horinaga M, Masuda T, and Jitsukawa S. A case of scrotal elephantiasis 30 years after treatment of penile carcinoma. Hinyokika Kiyo 1998; 44: 839–841. [PubMed] [Google Scholar]
- 9.Kofler L, Schweinzer K, Heister M, Kohler M, Breuninger H, Häfner HM. Surgical treatment of hidradenitis suppurativa: an analysis of postoperative outcome, cosmetic results and quality of life in 255 patients. J Eur Acad Dermatol Venereol 2018; 32: 1570–1574. [DOI] [PubMed] [Google Scholar]
- 10.Posch C, Monshi B, Quint T, Vujic I, Lilgenau N, Rappersberger K. The role of wide local excision for the treatment of severe hidradenitis suppurativa (Hurley grade III): retrospective analysis of 74 patients. J Am Acad Dermatol 2017; 77: 123–129. [DOI] [PubMed] [Google Scholar]
- 11.Prens LM, Huizinga J, Janse IC, Horváth B. Surgical outcomes and the impact of major surgery on quality of life, activity impairment and sexual health in hidradenitis suppurativa patients: a prospective single center study. J Eur Acad Dermatol Venereol. 2019; 33: 1941–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thornton JP, Abcarian H. Surgical treatment of perianal and perineal hidradenitis suppurativa. Dis Colon Rectum 1978; 21: 573. [DOI] [PubMed] [Google Scholar]


