Abstract
Past psychiatric diagnoses are central to patient case formulation and prognosis. Recently, alternative classification models such as the Hierarchical Taxonomy of Psychopathology (HiTOP) proposed to assess traits to predict clinically-relevant outcomes. The current study directly compared personality traits and past diagnoses as predictors of future mental health and functioning in three independent, prospective samples. Regression analyses found that personality traits significantly predicted future first onsets of psychiatric disorders (ΔR2=06–.15), symptom chronicity (ΔR2=.03–.06), and functioning (ΔR2=.02–.07), beyond past and current psychiatric diagnoses. Conversely, past psychiatric diagnoses did not provide an incremental prediction of outcomes when personality traits and other concurrent predictors were already included in the model. Overall, personality traits predicted a variety of outcomes in diverse settings, beyond diagnoses. Past diagnoses were generally not informative about future outcomes when personality was considered. Together, these findings support the added value of personality traits assessment in case formulation, consistent with HiTOP model.
Keywords: Diagnosis, Functioning, Personality traits, Psychopathology
Diagnostic assessment typically includes evaluation of past (i.e., remitted) diagnoses. Although past diagnoses serve various functions in clinical practice, one of the key reasons for their assessment is to inform prognosis (Croft et al., 2015; Kendell & Jablensky, 2003; Koerner, Hood, & Antony, 2011). Indeed, studies have demonstrated that after adjusting for current diagnoses, past diagnoses predicted psychiatric and functional outcomes, including financial difficulties, loneliness, and substance use (Copeland, Wolke, Shanahan, & Costello, 2015; Ormel et al., 2017). However, assessment of past diagnoses usually relies on retrospective recall of episodes that happened decades earlier. This approach often leads to symptom underreporting and inconsistency over time (Andrews, Anstey, Brodaty, Issakidis, & Luscombe, 1999; Bromet, Dunn, Connell, Dew, & Schulberg, 1986; Copeland, Shanahan, Costello, & Angold, 2011; Moffitt et al., 2010; Olino et al., 2012; Takayanagi et al., 2014). These limitations may lower prognostic value of past diagnoses.
Personality traits constitute enduring dispositions to a pattern of thoughts, feelings, and behaviors that underlie mental health (Hur, Stockbridge, Fox, & Shackman, 2018; Krueger & Tackett, 2006; Shackman et al., 2016; Widiger, 2011). Personality traits are established as major predictors of future psychopathology, related functional impairment, and life and treatment outcomes (Bucher, Suzuki, & Samuel, 2019; Jeronimus, Kotov, Riese, & Ormel, 2016; Karsten, Penninx, Verboom, Nolen, & Hartman, 2013; Lahey, 2009; Ozer & Benet-Martinez, 2006; Roberts, Kuncel, Shiner, Caspi, & Goldberg, 2007; Waszczuk et al., 2018). For example, Roberts et al. (2007) found that the association of personality with future outcomes was as strong as that of cognitive ability and socioeconomic status. Neuroticism in particular is known to be a major predictor of poor mental health and functioning, however, all broad personality dimensions have shown robust associations with future outcomes (Bucher et al., 2019; Ozer & Benet-Martinez, 2006).
When compared directly to psychiatric diagnoses, personality traits were superior in predicting future functioning outcomes (Morey et al., 2007; Morey et al., 2012), in line with the broader evidence of clinical utility of personality traits in assessment of functional status (Hopwood et al., 2011; Hopwood et al., 2007). Moreover, one study has found that after accounting for personality traits, past psychiatric diagnoses were no longer predictive of new onsets and recurrences of internalizing disorders (Conway, Craske, Zinbarg, & Mineka, 2016). Overall, the evidence indicates that the assessment of personality traits is informative for predicting future outcomes, and might fully account for the prognostic ability of past psychiatric diagnoses. Specifically, to date the predictive utility of personality traits has been demonstrated in direct comparison to past diagnoses of internalizing disorders.
Recently, the Hierarchical Taxonomy of Psychopathology (HiTOP) model has emerged as an alternative approach to classifying and conceptualizing psychopathology (Kotov, Krueger, & Watson, 2018; Kotov et al., 2017; Krueger et al., 2018). Importantly, HiTOP does not focus on past symptoms or diagnoses, and instead includes traits. In particular, personality traits form the base of HiTOP alongside psychopathology (Widiger et al., 2018). The classification proposed by the HiTOP model demonstrates research and clinical utility, with the model postulating inclusion of personality traits assessment for patient outcome prediction (Kotov et al., 2021; Ruggero et al., 2019; Widiger et al., 2018).
The aim of the current study was to directly compare prognostic utility of personality traits and past diagnoses in predicting a wide range of future mental health outcomes. The majority of the diagnoses investigated in the study were from the internalizing domain. Specifically, using three independent, longitudinal samples, we compared predictions of future first onsets of internalizing and externalizing psychiatric disorders (Sample 1), symptom chronicity (Sample 2), and long-term functional outcomes (Sample 3). We hypothesized that for all future outcomes studied in this paper, personality traits will provide an additional prediction over and above current and past psychiatric diagnoses, supporting the view that personality traits should be routinely assessed in clinical practice alongside diagnostic interviews. Furthermore, we report associations between individual personality traits and future outcomes, to inform about incremental contributions of specific traits.
Methods
Sample 1 – Community adolescents
Participants
Participants came from the Adolescent Development of Emotions and Personality Traits (ADEPT) study. The ADEPT cohort at enrollment consisted of 550 adolescent females from Suffolk County, New York, USA (mean age=14.39, SD=.63, range=13–15 years, 88.5% Caucasian, 67.6% with at least one college educated parent) (Michelini et al., 2020). Exclusion criteria were history of DSM-IV Major Depressive Disorder (MDD) or Dysthymia prior to enrollment, an intellectual disability, an absence of a biological parent willing to participate, an inability to read or understand questionnaires, and a lack of fluency in English. Both adolescents and parents provided written informed consents and the study was approved by the Stony Brook University’s IRB.
The current study focuses on N=469 participants for whom personality traits and both past and current diagnoses were available at waves 3 (hereon referred to as baseline) and wave 5 (hereon referred to as 20-month follow-up). Wave 3 was selected as a baseline to ensure a sufficient number of past diagnoses. The analytic sample had baseline mean age=15.85 years old (SD=0.63, range=15–17) and was 87.8% Caucasian.
Diagnoses
DSM-IV diagnoses were assessed at baseline and 20-month follow-up, using the semi-structured diagnostic interview Kiddie Scheduled for Affective Disorders and Schizophrenia for School-Aged Children, Present and Lifetime Version (KSADS-PL) (Kaufman et al., 1997). Interviews were conducted by extensively trained research staff under the supervision of clinical psychologists. The KSADS-PL has excellent reliability and validity in diagnosing adolescent psychopathology (Kaufman et al., 1997). The analyses focused on five diagnostic classes: Any depressive disorder, Any anxiety disorder, Any eating disorder, Any substance use disorder, and Any behavioral disorder. The inter-rater reliability was good [κ range: .68 (Depression NOS) to .94 (Any Anxiety Disorder) based on 25 interviews].
Personality traits
Adolescents completed the 44-item self-report Big Five Inventory (BFI) at baseline (John, Donahue, & Kentle, 1991). The BFI measures five personality traits: extraversion, agreeableness, conscientiousness, neuroticism, and openness to new experiences, using a Likert scale ranging from 1 (disagree strongly) to 5 (agree strongly). This measure is commonly used to assess personality in adults and adolescents (Soto, John, Gosling, & Potter, 2011) and demonstrates good reliability and validity (John & Srivastava, 1999), including in our sample (α=.76–86).
Functioning
Adolescents completed two age-appropriate measures of functioning. The revised version of School Attitude Assessment Survey (SAAS-R) (McCoach & Siegle, 2003) was used to measure factors associated with students’ academic achievement. Three subscales were assessed and combined into a total score: Attitudes Toward Teachers, Attitudes Toward School, and Motivation/Self-Regulation. The response scale ranges from 1 (strongly disagree) to 7 (strongly agree). The scale demonstrates sound psychometric properties in youth (Dedrick, Shaunessy-Dedrick, Suldo, & Ferron, 2015; Suldo, Shaffer, & Shaunessy, 2008). The Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet, Dahlem, Zimet, & Farley, 1988) was used to measure adolescents’ subjective social support from three sources: family, friends, and a significant other. Reponses ranged from 1 (very strongly disagree) to 7 (very strongly agree). Good psychometric properties have been found with the MSPSS in several studies with adolescents and young adults (Canty-Mitchell & Zimet, 2000; Zimet, Powell, Farley, Werkman, & Berkoff, 1990).
Sample 2 - Trauma-exposed primary care patients
Participants
Participants were recruited from the World Trade Center (WTC) Health Program in the USA between October 2014 and February 2016, where they were receiving health monitoring or treatment (medical or psychiatric) (Dasaro et al., 2015). All participants were exposed to the 9/11 disaster and were recruited for a study (N=202) focused on the daily relationships between PTSD and physical health, and oversampled for high PTSD symptoms (Dornbach-Bender et al., 2019). The current study focuses on N=133 participants who completed optional baseline personality trait assessments (mean age=53.72, SD=8.85, range=35–85, 85% male, 85% Caucasian, 76% completed at least some college education). The analysis subsample did not differ from the total sample on any baseline demographic characteristics, symptoms, and diagnoses (Table S1 in the Supplementary Materials). The 1-year follow-up symptom data were available from the monitoring records of the WTC Health Program. The study was approved by the Stony Brook University IRB, and all participants provided a written informed consent.
Diagnoses
The past and current PTSD, MDD, and Panic disorder diagnoses were derived at baseline using the Structured Interview for the DSM-IV (SCID) (First, Spitzer, Gibbon, & Williams, 1997). The assessment was administered by trained interviewers under the close supervision of clinical psychologists. Previous assessments of reliability of the trained interviewers in independent studies in this population demonstrated good inter-rater agreement for Axis I diagnoses, including κ=.82 for current PTSD diagnosis (Bromet et al., 2016; Gonzalez et al., 2017).
Personality traits
The Personality Inventory for DSM-5 (PID-5) (Krueger, Derringer, Markon, Watson, & Skodol, 2012), a 220-item questionnaire with a four-point response scale (0=very false to 3=very true), was used to measure five higher-order maladaptive personality traits (Krueger et al., 2012). The PID-5 domains broadly map on domains of normal personality: negative affectivity corresponds to neuroticism, detachment to low extraversion, disinhibition to low conscientiousness, and antagonism to low agreeableness, with the PID-5 including an additional psychoticism domain instead of openness to experience (Krueger & Markon, 2014; Thomas et al., 2012). Psychometric properties of the PID-5 are well-documented (Krueger et al., 2012; Krueger & Markon, 2014), and internal consistencies were very high in the current sample (α=.91–.95).
Symptoms and functioning
PTSD symptoms were measured at baseline and 1-year follow-up using the Posttraumatic Stress Disorder Checklist-Specific Version (Weathers, Litz, Herman, Huska, & Keane, 1993), a 17-item self-report questionnaire assessing, on a five point scale (1=not at all to 5=extremely), the severity of WTC-related DSM-IV PTSD symptoms in the past month. The scale demonstrates excellent psychometric properties (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Dobie et al., 2002; Wilkins, Lang, & Norman, 2011), and had an excellent internal consistency in the current sample (α=.95).
Depression symptoms were assessed at baseline using the 20-item General Depression scale of the Inventory of Depression and Anxiety Symptoms, expanded version (IDAS-II) (Watson et al., 2012). The IDAS-II measures symptoms in the past two weeks, rated on a 5-point scale (1=not at all to 5=extremely). Depression symptoms at 1-year follow-up were assessed using the Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer, & Williams, 2001), a 9-item questionnaire on a 4-point scale (0=not at all to 4=nearly every day). The internal consistency was very high (α=.92).
Global mental health functioning was assessed at baseline and 1-year follow-up using the mental subscale from a 12-item Short-Form Health Survey (Ware, Keller, & Kosinski, 1998; Ware, Kosinski, & Keller, 1996). The mental subscale taps the vitality, social functioning, and role functioning difficulties caused by mental health problems. The scale is normed to a general USA population mean of 50 and a SD of 10; higher scores represent better mental health functioning.
Family life impairment was assessed using the Sheehan Disability Scale (SDS) (Sheehan, 1986). Participants rated the extent to which their symptoms interfered with family life or home responsibilities during the last month, using a 10-point Likert scale (0=Not at all impaired, 5=Moderately impaired, 10=Very severely impaired). The measure is well validated (Leon, Olfson, Portera, Farber, & Sheehan, 1997).
Sample 3 – Psychiatric patients
Participants
Participants were drawn from the Collaborative Longitudinal Personality Disorders Study (CLPS) (Gunderson et al., 2000), a multisite, naturalistic longitudinal study. The CLPS enrolled 668 participants in Northeastern USA aged between 18 to 45 years old, who had either personality disorders or current depression without any personality disorder. The current study focuses on N=604 participants for whom both past and current diagnoses were available at baseline for Axis I disorders (mean age=32.72, SD=8.09, range=18–45 years old; 65% female, 70.1% Caucasian). Written informed consent was provided by all participants. The study was approved by each collaborating site’s IRB.
Diagnoses
The past and current Axis I diagnoses were assessed at baseline using the SCID for DSM-IV (First et al., 1997). Participants were interviewed in person by experienced interviewers with master’s or doctoral degrees in mental health disciplines, who underwent extensive standardized training and received regular supervision (Zanarini et al., 2000). The current study focuses on Axis I diagnoses of MDD, PTSD, Panic, Other Anxiety disorders, OCD, and Eating disorders. The inter-rater reliability ranged from fair to excellent [κ range: .56 (OCD) to .88 (PTSD)] (Zanarini et al., 2000).
Personality traits
Participants completed the 240-item NEO Personality Inventory–Revised (Costa & McCrae, 1992), which was designed to assess dimensions of the five-factor model of personality: neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness. Internal consistency reliabilities for the five domains in this sample at the baseline assessment ranged from .87 to .92.
Functioning
Functioning was assessed at baseline, 2-year, and 10-year follow-ups. The Global Assessment of Functioning (GAF) (Endicott, Spitzer, Fleiss, & Cohen, 1976) is a commonly used clinician-rated single item score, ranging from 1 to 100, that indicates an overall symptom severity and level of functioning. The Longitudinal Interval Follow-Up Evaluation (LIFE) (Keller et al., 1987) is a semi-structured interview that was used to assess psychosocial functioning. Three domains of functioning were assessed: interpersonal, work, and recreation. Both outcome measures are well validated (Jones, Thornicroft, Coffey, & Dunn, 1995; Startup, Jackson, & Bendix, 2002; Warshaw, Keller, & Stout, 1994).
Analytic approach
The incremental prediction of future outcomes by personality traits vs. past diagnoses was evaluated using regression models. Analyses controlled for current diagnoses at baseline and, where needed, baseline levels of the outcome variables (entered first in the model as covariates). Next, two sets of regressions were conducted for each outcome. In the first set, past diagnoses at baseline were included as the first block of predictors, and the incremental validity of baseline personality traits entered as the second block of predictors was tested. In the second set, baseline personality traits were included as the first block, and the incremental validity of the block of past diagnoses was tested. Each outcome constituted a dependent variable in a separate regression model. The incremental prediction of past diagnoses vs personality traits was compared using ΔR2 analysis of deviance chi-square tests. All analyses were conducted in SPSS version 25.
Specifically, in Sample 1, logistic regressions were used to prospectively predict 20-months psychiatric disorder first onsets, grouped by domain. Blocks were all current baseline diagnoses (i.e., from all domains), all past diagnoses, and personality traits at baseline. Moreover, linear regression analyses were used to prospectively predict the 20-month functioning outcomes. Blocks were baseline functioning, all current baseline diagnoses, all past diagnoses, and personality traits at baseline. In Sample 2, linear regression analyses were used to prospectively predict the 1-year course of psychiatric symptoms. Blocks were baseline psychiatric symptoms, current baseline internalizing diagnoses, past internalizing diagnoses, and personality traits at baseline. In Sample 3, linear regression analyses were used to prospectively predict 2- and 10-year functioning outcomes. Blocks were baseline functioning, current baseline internalizing diagnoses, past internalizing diagnoses, and personality traits at baseline.
Sensitivity analyses
Finally, to ensure that covariates, in particular current diagnoses, do not affect the pattern of results, analyses were repeated including only the two predictor blocks: past psychiatric diagnoses and baseline personality traits (entered in both orders). Second, to compare the prediction of lifetime diagnoses vs. personality traits, past and current diagnoses were collapsed into lifetime diagnoses. The main regression analyses were repeated with lifetime diagnoses as a predictor block and without including current diagnoses. For example, in Sample 2, baseline psychiatric symptoms were entered first, followed by lifetime diagnoses and personality traits at baseline (entered in both orders).
Results
Incremental predictions
Descriptive statistics for measures included in three samples are reported in Table 1. The incremental predictions by personality traits and past diagnoses across all outcomes are summarized in Figure 1.
Table 1 –
Diagnoses, personality traits, symptoms, and functioning measures in each study
| Sample 1, Community adolescents (ADEPT study), N=469 | |
|---|---|
| Current diagnoses at baseline | N (%) |
| Any depressive disorder | 18 (3.8%) |
| Any anxiety disorder | 105 (22.4%) |
| Any eating disorder | 11 (2.3%) |
| Any substance use | 11 (2.3%) |
| Any behavioral disorder | 29 (6.2%) |
| Past diagnoses at baseline | |
| Any depressive disorder | 49 (10.4%) |
| Any anxiety disorder | 82 (17.5%) |
| Any eating disorder | 6 (1.3%) |
| Any substance use | 9 (1.9%) |
| Any behavioral disorder | 18 (3.8%) |
| First onsets by 20-month follow-up | |
| Any depressive disorder | 36 (7.7%) |
| Any anxiety disorder | 24 (7.2%) |
| Any eating disorder | 22 (4.7%) |
| Any behavioral disorder | 15 (3.2%) |
| Any substance use | 34 (7.2%) |
| Personality traits (BFI) at baseline | Mean (SD) |
| Neuroticism | 2.82 (.85) |
| Extraversion | 3.67 (.86) |
| Conscientiousness | 3.68 (.71) |
| Agreeableness | 4.06 (.67) |
| Openness to experience | 3.89 (.57) |
| Functioning at baseline | |
| School attitude | 15.82 (3.27) |
| Perceived social support | 17.21 (3.08) |
| Functioning at 20-month follow up | |
| School attitude | 16.34 (3.18) |
| Perceived social support | 17.45 (3.09) |
| Sample 2, Trauma-exposed primary care adult patients (WTC study), N=133 | |
| Current diagnoses at baseline | N (%) |
| PTSD | 26 (18.8%) |
| MDD | 21 (15.1%) |
| Panic | 9 (6.5%) |
| Past diagnoses at baseline | |
| PTSD | 27 (20.3%) |
| MDD | 34 (25.6%) |
| Panic | 5 (3.8%) |
| Personality traits (PID-5) at baseline | Mean (SD) |
| Negative Affectivity | 46.9 (8.97) |
| Detachment | 48.49 (9.53) |
| Disinhibition | 49.28 (10.52) |
| Antagonism | 46.15 (8.19) |
| Psychoticism | 46.08 (8.31) |
| Current symptoms/functioning at baseline | |
| PTSD symptoms | 35.02 (14.86) |
| Depression symptoms | 40.49 (13.86) |
| Mental health functioning | 43.95 (12.25) |
| Family life impairment | 3.34 (3.07) |
| Current symptoms/functioning at 1 year follow-up | |
| PTSD symptoms | 39.38 (17.28) |
| Depression symptoms | 8.18 (7.04) |
| Mental health functioning | 43.71 (12.24) |
| Family life impairment | 3.61 (3.06) |
| Sample 3, Adult psychiatric patients (CLPS study), N=604 | |
| Current diagnoses at baseline | N (%) |
| MDD | 279 (46.2%) |
| PTSD | 138 (22.8%) |
| Panic | 123 (20.4%) |
| Other Anxiety disorders | 235 (38.9%) |
| OCD | 78 (12.9%) |
| Eating disorders | 106 (17.5%) |
| Past diagnoses at baseline | |
| MDD | 241 (39.9%) |
| PTSD | 52 (8.6%) |
| Panic | 43 (7.1%) |
| Other Anxiety disorders | 28 (4.6%) |
| OCD | 18 (3.0%) |
| Eating disorders | 63 (10.4%) |
| Personality traits (NEO-PI-R) at baseline | Mean (SD) |
| Neuroticism | 119.86 (24.14) |
| Extraversion | 93.15 (22.29) |
| Conscientiousness | 101.01 (24.88) |
| Agreeableness | 114.70 (19.24) |
| Openness to experience | 117.97 (21.63) |
| Functioning at baseline | |
| GAF | 57.73 (10.71) |
| LIFE interpersonal | 2.75 (.90) |
| LIFE work | 1.91 (.96) |
| LIFE recreation | 3.03 (1.20) |
| Functioning at 2-year follow-up | |
| GAF | 59.86 (13.08) |
| LIFE interpersonal | 2.45 (.86) |
| LIFE work | 2.32 (1.02) |
| LIFE recreation | 2.46 (1.19) |
| Functioning at 10-year follow-up | |
| GAF | 61.36 (13.33) |
| LIFE interpersonal | 2.47 (.89) |
| LIFE work | 2.73 (1.06) |
| LIFE recreation | 2.56 (1.09) |
Notes: GAF – The Global Assessment of Functioning; LIFE - The Longitudinal Interval Follow-up Evaluation
Figure 1 – Incremental predictions of mental health outcomes by personality traits and past diagnoses.
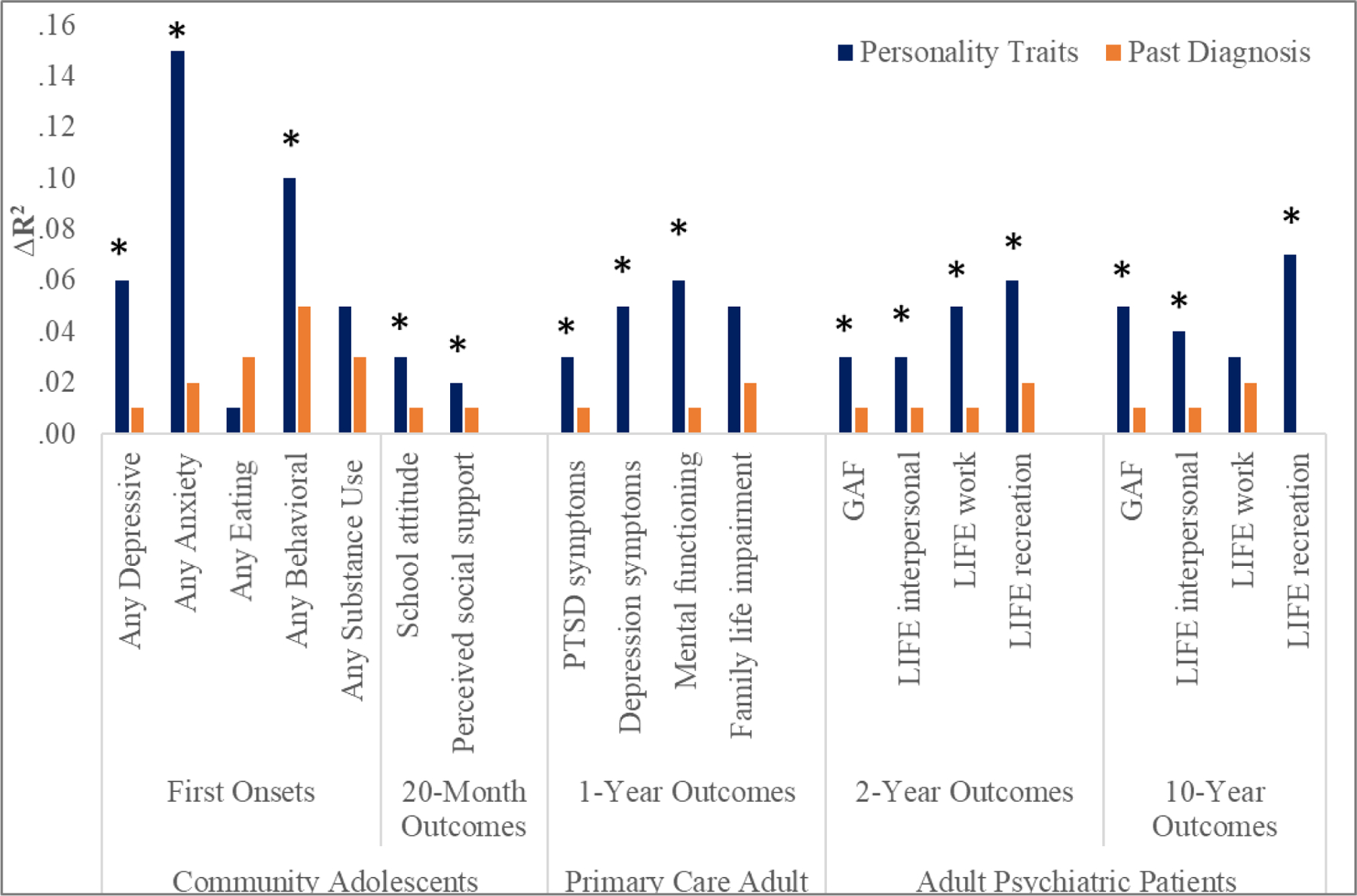
Notes: Asterisk denotes significant ΔR2 at p<.05 when the predictor was added to the model in the final regression block, after accounting for all other predictors.
In the community adolescents sample, the effect size for analyses of first onsets is reported as Nagelkerke pseudo R2.
In Sample 1, after adjusting for current and past baseline diagnoses, personality traits provided a significant incremental prediction of the first onsets of depressive (ΔR2=.06), anxiety (ΔR2=.15), and behavioral disorders (ΔR2=.10) at 20-month follow-up, but not of the first onsets of substance use and eating disorders (Table 2). Conversely, after adjusting for current baseline diagnoses and personality traits, past diagnoses provided no significant incremental prediction of first onsets. Jointly, baseline diagnoses and personality traits accounted for R2=.18–.34 in first onsets of disorders, with personality accounting for 17.6% to 62.5% of the total variance explained by the models.
Table 2 –
Incremental prediction by past diagnoses vs personality traits of disorder first onsets and functional outcomes in community adolescents (Sample 1)
| 20-month Outcomes | Model 1 | Model 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor added | R2 | ΔR2 | %R2 | p | Predictor added | R2 | ΔR2 | %R2 | p | |
| Current diagnoses | .27 | Current diagnoses | .27 | |||||||
| Past diagnoses | .28 | .01 | 3.6% | .07 | Personality | .33 | .06 | 18.2% | <.01* | |
| Personality | .34 | .06 | 17.6% | <.01* | Past diagnoses | .34 | .01 | 2.9% | .29 | |
| Any Anxiety diagnoses first onsets | Current diagnoses | .07 | Current diagnoses | .07 | ||||||
| Past diagnoses | .08 | .01 | 12.5% | .79 | Personality | .22 | .15 | 68.2% | <.01* | |
| Personality | .24 | .15 | 62.5% | <.01* | Past diagnoses | .24 | .02 | 8.3% | .54 | |
| Any Eating diagnoses first onsets | Current diagnoses | .06 | Current diagnoses | .06 | ||||||
| Past diagnoses | .09 | .03 | 33.3% | .29 | Personality | .08 | .02 | 25.0% | .72 | |
| Personality | .11 | .01 | 9.1% | .83 | Past diagnoses | .11 | .03 | 27.3% | .38 | |
| Any Behavioral diagnoses first onsets | Current diagnoses | .03 | Current diagnoses | .03 | ||||||
| Past diagnoses | .08 | .05 | 62.5% | .19 | Personality | .13 | .11 | 84.6% | .04* | |
| Personality | .19 | .10 | 52.6% | .04* | Past diagnoses | .19 | .05 | 26.3% | .19 | |
| Any Substance use diagnoses first onsets | Current diagnoses | .10 | Current diagnoses | .10 | ||||||
| Past diagnoses | .14 | .04 | 28.6% | .10 | Personality | .16 | .06 | 37.5% | .04* | |
| Personality | .18 | .05 | 27.8% | .09 | Past diagnoses | .18 | .03 | 16.7% | .26 | |
| School attitude | Current school attitude | .29 | Current school attitude | .29 | ||||||
| Current diagnoses | .31 | .02 | 6.5% | .03* | Current diagnoses | .31 | .02 | 6.5% | .03* | |
| Past diagnoses | .31 | .00 | 0.0% | .28 | Personality | .33 | .03 | 9.1% | .01* | |
| Personality | .34 | .03 | 8.8% | .01* | Past diagnoses | .34 | .01 | 2.9% | .28 | |
| Perceived social support | Current perceived social support | .22 | Current perceived social support | .22 | ||||||
| Current diagnoses | .24 | .02 | 8.3% | .08 | Current diagnoses | .24 | .02 | 8.3% | .08 | |
| Past diagnoses | .25 | .01 | 4.0% | .10 | Personality | .26 | .02 | 7.7% | .03* | |
| Personality | .27 | .02 | 7.4% | .04* | Past diagnoses | .27 | .01 | 3.7% | .14 | |
Notes: Current and past diagnoses included: any depressive disorders, any anxiety disorders, any eating disorders, any substance use, and behavioral disorders. Personality traits included: neuroticism, extraversion, conscientiousness, agreeableness, and openness to experience.
The effect size for analyses of first onsets is Nagelkerke pseudo R2. Percentage R2 denotes the proportion of the total variance explained by the predictor added. P-value denotes significant ΔR2 at p<.05.
Furthermore, in Sample 1, after adjusting for current functioning, and current and past baseline diagnoses, personality traits provided a significant incremental prediction of functional outcomes at 20-month follow up (ΔR2=.02–.03) and uniquely accounted for 7.4% to 8.8% of the total variance in functional outcomes. Conversely, after adjusting for current functioning, current baseline diagnoses and personality traits, past diagnoses provided no significant incremental prediction of future functioning. Notably, after adjusting for baseline functioning, current diagnoses predicted social attitudes (ΔR2=.02), but not perceived social support at 20-month follow up.
In Sample 2, after adjusting for baseline symptoms, and both current and past internalizing diagnoses, personality traits provided significant incremental prediction of change in PTSD symptoms (ΔR2=.03), depression symptoms (ΔR2=.05), and mental health functioning (ΔR2=.06) a year later, but not family life impairment (Table 3). Conversely, past internalizing diagnoses did not provide any significant incremental prediction when baseline symptoms, current internalizing diagnoses, and personality traits were included in the model. Notably, after adjusting for baseline symptoms, current internalizing diagnoses did not provide any incremental prediction of 1-year PTSD and depression symptoms, but predicted 1-year mental health functioning and family life impairment (ΔR2=.05–.06). Jointly, baseline symptoms, internalizing diagnoses and personality traits accounted for R2=.54–.80 in 1-year symptom course, with personality accounting for 3.8% to 9.7% of the total variance explained by the models.
Table 3 –
Incremental prediction by past diagnoses vs personality traits of symptom course in trauma-exposed primary care adult patients (Sample 2)
| 1-year Outcomes | Model 1 | Model 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor added | R2 | ΔR2 | %R2 | p | Predictor added | R2 | ΔR2 | %R2 | p | |
| Current PTSD symptoms | .75 | Current PTSD symptoms | .75 | |||||||
| Current diagnoses | .76 | .01 | 1.3% | .44 | Current diagnoses | .76 | .01 | 1.3% | .44 | |
| Past diagnoses | .77 | .02 | 2.6% | .10 | Personality | .79 | .03 | 3.8% | .01* | |
| Personality | .80 | .03 | 3.8% | .02* | Past diagnoses | .80 | .01 | 1.3% | .25 | |
| Depression symptoms | Current Depression symptoms | .52 | Current Depression symptoms | .52 | ||||||
| Current diagnoses | .56 | .03 | 5.4% | .07 | Current diagnoses | .56 | .03 | 5.4% | .07 | |
| Past diagnoses | .57 | .01 | 1.8% | .71 | Personality | .61 | .05 | 8.2% | .02* | |
| Personality | .61 | .05 | 8.2% | .03* | Past diagnoses | .61 | .00 | 0.0% | .90 | |
| Mental function | Current Mental function | .50 | Current Mental function | .50 | ||||||
| Current diagnoses | .55 | .05 | 9.1% | .03* | Current diagnoses | .55 | .05 | 9.1% | .02* | |
| Past diagnoses | .56 | .01 | 1.8% | .50 | Personality | .61 | .06 | 9.8% | .01* | |
| Personality | .62 | .06 | 9.7% | .01* | Past diagnoses | .62 | .01 | 1.6% | .56 | |
| Family life impairment | Current Family life impairment | .41 | Current Family life impairment | .41 | ||||||
| Current diagnoses | .47 | .06 | 12.8% | .02* | Current diagnoses | .47 | .06 | 12.8% | .02* | |
| Past diagnoses | .49 | .02 | 4.1% | .31 | Personality | .52 | .05 | 9.6% | .04* | |
| Personality | .54 | .05 | 9.3% | .07 | Past diagnoses | .54 | .02 | 3.7% | .35 | |
Notes: Current and past diagnoses included PTSD, MDD, and panic disorders. Personality traits included negative affectivity, detachment, disinhibition, antagonism, and psychoticism.
Percentage R2 denotes the proportion of the total variance explained by the predictor added. P-value denotes significant ΔR2 at p<.05.
In Sample 3, after adjusting for baseline functioning, and both current and past internalizing diagnoses, personality traits provided significant incremental prediction of 2-year and 10-year outcomes on GAF (ΔR2=.03) and LIFE ratings (ΔR2=.03–.07), except the 10-year LIFE work functioning (Table 4). Conversely, past internalizing diagnoses did not provide any significant incremental prediction when baseline functioning, current internalizing diagnoses, and personality traits were included in the model. Moreover, for 2-year and 10-year LIFE outcomes, current internalizing diagnoses also did not provide any incremental prediction over and above the baseline functioning, but they predicted GAF outcomes (ΔR2=.03 and .04 at follow-up years 2 and 10, respectively). Jointly, baseline functioning, internalizing diagnoses, and personality traits accounted for R2=.14–.35 in 2-year functioning outcomes, and R2=.12–.28 in 10-year functioning outcomes. Personality accounted for 8.6% to 35.7% of the total variance explained by the models predicting 2-year outcomes, and 17.9% to 50.0%. of the total variance explained in 10-year outcomes.
Table 4 –
Incremental prediction by past diagnoses vs personality traits of long-term functioning outcomes in adult psychiatric patients (Sample 3)
| 2-year Outcomes | Model 1 | Model 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor added | R2 | ΔR2 | %R2 | p | Predictor added | R2 | ΔR2 | %R2 | p | |
| Current GAF | .28 | Current GAF | .28 | |||||||
| Current diagnoses | .31 | .03 | 9.7% | <.01* | Current diagnoses | .31 | .03 | 9.7% | <.01* | |
| Past diagnoses | .32 | .01 | 3.1% | .48 | Personality | .34 | .03 | 8.8% | <.01* | |
| Personality | .35 | .03 | 8.6% | <.01* | Past diagnoses | .35 | .01 | 2.9% | .32 | |
| LIFE interpersonal | Current LIFE interpersonal | .27 | Current LIFE interpersonal | .27 | ||||||
| Current diagnoses | .29 | .02 | 6.9% | .07 | Current diagnoses | .29 | .02 | 6.9% | .07 | |
| Past diagnoses | .30 | .01 | 3.3% | .20 | Personality | .31 | .02 | 6.5% | <.01* | |
| Personality | .32 | .03 | 9.4% | <.01* | Past diagnoses | .32 | .01 | 3.1% | .10 | |
| LIFE work | Current LIFE work | .06 | Current LIFE work | .06 | ||||||
| Current diagnoses | .08 | .02 | 25.0% | .10 | Current diagnoses | .08 | .02 | 25.0% | .10 | |
| Past diagnoses | .09 | .01 | 11.1% | .69 | Personality | .13 | .05 | 38.5% | <.01* | |
| Personality | .14 | .05 | 35.7% | <.01* | Past diagnoses | .14 | .01 | 7.1% | .72 | |
| LIFE recreation | Current LIFE recreation | .08 | Current LIFE recreation | .08 | ||||||
| Current diagnoses | .09 | .01 | 11.1% | .44 | Current diagnoses | .09 | .01 | 11.1% | .44 | |
| Past diagnoses | .11 | .02 | 18.2% | .08 | Personality | .15 | .06 | 40.0% | <.01* | |
| Personality | .17 | .06 | 35.3% | <.01* | Past diagnoses | .17 | .02 | 11.8% | .07 | |
| 10-year Outcomes | ||||||||||
| GAF | Current GAF | .18 | Current GAF | .22 | ||||||
| Current diagnoses | .22 | .04 | 18.2% | .01* | Current diagnoses | .27 | .04 | 14.8% | .01* | |
| Past diagnoses | .23 | .01 | 4.3% | .40 | Personality | .28 | .05 | 17.9% | <.01* | |
| Personality | .28 | .05 | 17.9% | <.01* | Past diagnoses | .22 | .01 | 4.5% | .39 | |
| LIFE interpersonal | Current LIFE interpersonal | .11 | Current LIFE interpersonal | .11 | ||||||
| Current diagnoses | .12 | .01 | 8.3% | .47 | Current diagnoses | .12 | .01 | 8.3% | .47 | |
| Past diagnoses | .13 | .01 | 7.7% | .78 | Personality | .16 | .04 | 25.0% | <.01* | |
| Personality | .17 | .04 | 23.5% | .01* | Past diagnoses | .17 | .01 | 5.9% | .83 | |
| LIFE work | Current LIFE work | .04 | Current LIFE work | .04 | ||||||
| Current diagnoses | .05 | .02 | 40.0% | .80 | Current diagnoses | .05 | .02 | 40.0% | .80 | |
| Past diagnoses | .08 | .03 | 37.5% | .55 | Personality | .10 | .04 | 40.0% | .23 | |
| Personality | .12 | .03 | 25.0% | .35 | Past diagnoses | .12 | .02 | 16.7% | .72 | |
| LIFE recreation | Current LIFE recreation | .05 | Current LIFE recreation | .05 | ||||||
| Current diagnoses | .07 | .02 | 28.6% | .30 | Current diagnoses | .07 | .02 | 28.6% | .30 | |
| Past diagnoses | .07 | .00 | 0.0% | .93 | Personality | .14 | .07 | 50.0% | <.01* | |
| Personality | .14 | .07 | 50.0% | <.01* | Past diagnoses | .14 | .00 | 0.0% | .97 | |
Notes: GAF – The Global Assessment of Functioning; LIFE - The Longitudinal Interval Follow-up Evaluation
Current and past diagnoses included MDD, PTSD, panic, anxiety disorders, OCD, and eating disorders. Personality traits included: neuroticism, extraversion, conscientiousness, agreeableness, and openness to experience.
Percentage R2 denotes the proportion of the total variance explained by the predictor added. P-value denotes significant ΔR2 at p<.05.
Associations with individual personality traits
The associations between individual personality traits at baseline and future outcomes are reported in Table S2 in the Supplemental Materials. Across the three Samples, in unadjusted models personality traits were in general significantly associated with all outcomes. Specifically, neuroticism/negative affectivity and conscientiousness/disinhibition demonstrated the largest number of associations with outcomes. In final regression models adjusted for covariates, past and current diagnoses, and other personality traits, only a handful of significant unique associations remained. Most prominently, agreeableness was uniquely associated with the first onsets of any behavioral (OR=.54) and any substance use disorders (OR=.66) in Sample 1, as well as GAF at 2-year follow up (β=.11) and GAF and LIFE interpersonal at 10-year follow up (β=.13 and .14, respectively) in Sample 3. Extraversion was uniquely associated with the first onsets of any anxiety diagnoses (OR=.65) in Sample 1, 2-year LIFE interpersonal (β=.13) and 10-year LIFE recreation (β=.19) outcomes in Sample 3, while detachment was uniquely associated with PTSD and Depression symptoms (β=.15 and .07, respectively) in Sample 2. Openness to experience was uniquely associated with positive school attitude in Sample 1 (β=.09), and 2-year LIFE recreation (β=.18) and 10-year GAF and LIFE recreation (β=.10 and .12, respectively) outcomes in Sample 3. Neuroticism was uniquely associated with the first onsets of any depressive (OR=1.52) and any anxiety disorders (OR=2.40) in Sample 1, family life impairment (β=.21) in Sample 2, and GAF at 10-year follow up (β=−.13) in Sample 3. Finally, conscientiousness was only associated with positive school attitude (β=.15) outcome in Sample 1 and 2-year LIFE work (β=.13) outcome in Sample 3 in fully adjusted models.
Sensitivity analyses
The sensitivity analyses found that past diagnoses were generally not predictive over and above personality traits when current diagnoses and other concurrent covariates were not accounted for, with five exceptions. In Sample 1, when current diagnoses were excluded from the models, past diagnoses predicted first onsets of substance use and school attitude at 20-months follow up, over and above personality (ΔR2=.08 and .02, respectively, Table 5). In Sample 3, when baseline functioning and current internalizing diagnoses were excluded from the models, past internalizing diagnoses were significant predictors of 2-year and 10-year functional outcomes on GAF, and 2-year LIFE recreation, over and above personality (ΔR2=.03–.04, Table 5). Conversely, past internalizing diagnoses were not predictive of symptoms change over and above personality traits in Sample 2.
Table 5 -.
Incremental prediction by past diagnoses vs personality traits of (a) disorder first onsets and functioning in community adolescents in Sample 1, (b) symptoms and functioning in trauma-exposed primary care adult patients in Sample 2, and (c) long-term functioning outcomes in adult psychiatric patients in Sample 3
| Model 1 | Model 2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor added | R2 | ΔR2 | %R2 | p | Predictor added | R2 | ΔR2 | %R2 | p | |
| (a) 20-month Outcomes in Sample 1, Community adolescents | ||||||||||
| Any Depressive diagnoses first onsets | Past diagnoses | .10 | Personality | .18 | ||||||
| Personality | .20 | .11 | 55.0% | <.01* | Past diagnoses | .20 | .02 | 10.0% | .10 | |
| Any Anxiety diagnoses first onsets | Past diagnoses | .07 | Personality | .19 | ||||||
| Personality | .23 | .16 | 69.6% | <.01* | Past diagnoses | .23 | .04 | 17.4% | .20 | |
| Any Eating diagnoses first onsets | Past diagnoses | .08 | Personality | .05 | ||||||
| Personality | .10 | .02 | 20.0% | .72 | Past diagnoses | .10 | .05 | 50.0% | .12 | |
| Any Behavioral diagnoses first onsets | Past diagnoses | .06 | Personality | .11 | ||||||
| Personality | .15 | .10 | 66.7% | .04* | Past diagnoses | .15 | .05 | 33.3% | .24 | |
| Any Substance use diagnoses first onsets | Past diagnoses | .13 | Personality | .09 | ||||||
| Personality | .17 | .04 | 23.5% | .15 | Past diagnoses | .17 | .08 | 47.1% | <.01* | |
| School attitude | Past diagnoses | .09 | Personality | .22 | ||||||
| Personality | .24 | .15 | 62.5% | <.01* | Past diagnoses | .24 | .02 | 8.3% | .02* | |
| Perceived social support | Past diagnoses | .04 | Personality | .12 | ||||||
| Personality | .13 | .09 | 69.2% | <.01* | Past diagnoses | .13 | .01 | 7.7% | .23 | |
| (b) 1-year Outcomes in Sample 2, Trauma-exposed primary care adult patients | ||||||||||
| PTSD symptoms | Past diagnoses | .05 | Personality | .48 | ||||||
| Personality | .50 | .45 | 90.0% | <.01* | Past diagnoses | .50 | .02 | 4.0% | .29 | |
| Depression symptoms | Past diagnoses | .03 | Personality | .48 | ||||||
| Personality | .48 | .45 | 93.8% | <.01* | Past diagnoses | .48 | .00 | 0.0% | .86 | |
| Mental function | Past diagnoses | .01 | Personality | .45 | ||||||
| Personality | .46 | .45 | 97.8% | <.01* | Past diagnoses | .46 | .01 | 2.2% | .52 | |
| Family life impairment | Past diagnoses | .02 | Personality | .35 | ||||||
| Personality | .36 | .34 | 94.4% | <.01* | Past diagnoses | .36 | .01 | 2.8% | .93 | |
| (c) Outcomes in Sample 3, Adult psychiatric patients | ||||||||||
| 2-year Outcomes | ||||||||||
| GAF | Past diagnoses | .04 | Personality | .11 | ||||||
| Personality | .15 | .11 | 73.3% | <.01* | Past diagnoses | .15 | .04 | 26.7% | <.01* | |
| LIFE interpersonal | Past diagnoses | .02 | Personality | .08 | ||||||
| Personality | .10 | .08 | 80.0% | <.01* | Past diagnoses | .10 | .02 | 20.0% | .23 | |
| LIFE work | Past diagnoses | .02 | Personality | .08 | ||||||
| Personality | .07 | .05 | 71.4% | <.01* | Past diagnoses | .09 | .01 | 11.1% | .16 | |
| LIFE recreation | Past diagnoses | .04 | Personality | .11 | ||||||
| Personality | .14 | .10 | 71.4% | <.01* | Past diagnoses | .14 | .03 | 21.4% | .02* | |
| 10-year Outcomes | ||||||||||
| GAF | Past diagnoses | .04 | Personality | .13 | ||||||
| Personality | .16 | .12 | 75.0% | <.01* | Past diagnoses | .16 | .03 | 18.8% | .02* | |
| LIFE interpersonal | Past diagnoses | .01 | Personality | .08 | ||||||
| Personality | .09 | .08 | 88.9% | <.01* | Past diagnoses | .09 | .01 | 11.1% | .77 | |
| LIFE work | Past diagnoses | .05 | Personality | .05 | ||||||
| Personality | .19 | .04 | 21.1% | .24 | Past diagnoses | .09 | .04 | 44.4% | .38 | |
| LIFE recreation | Past diagnoses | .01 | Personality | .12 | ||||||
| Personality | .12 | .11 | 91.7% | <.01* | Past diagnoses | .12 | .00 | 0.0% | .91 | |
Notes: GAF – The Global Assessment of Functioning; LIFE - The Longitudinal Interval Follow-up Evaluation
In Sample 1, past diagnoses included: any depressive disorders, any anxiety disorders, any eating disorders, any substance use, and behavioral disorders. In Sample 2, past diagnoses included PTSD, MDD, and panic disorders. In Sample 3, past diagnoses included MDD, PTSD, panic, anxiety disorders, OCD, and eating disorders.
In Samples 1 and 3, personality traits included: neuroticism, extraversion, conscientiousness, agreeableness, and openness to experience. In Sample 2, personality traits included negative affectivity, detachment, disinhibition, antagonism, and psychoticism.
In Sample 1, the effect size for analyses of first onsets is Nagelkerke pseudo R2.
Percentage R2 denotes the proportion of the total variance explained by the predictor added. P-value denotes significant ΔR2 at p<.05.
Finally, the sensitivity analyses comparing lifetime (past and current) diagnoses and personality traits, while controlling for baseline covariates, are reported in Supplementary Table S3, available online. In Sample 1, lifetime diagnoses predicted first onsets of depressive disorders and substance use, over and above personality traits (ΔR2=.16 and .10, respectively). In Sample 2, lifetime internalizing diagnoses did not predict outcomes beyond personality and baseline traits. Finally, in Sample 3, lifetime internalizing psychiatric diagnoses demonstrated prediction of functional outcomes over and above baseline functioning and personality traits for 2-year GAF and LIFE interpersonal (both ΔR2=.03).
Discussion
The current multi-sample study found that personality traits significantly predicted future first onsets of psychiatric disorders, symptom chronicity, and functional impairment, over and above past psychiatric diagnoses. Moreover, past psychiatric diagnoses, which were largely from the internalizing domain, did not provide incremental prediction of the majority of these important outcomes when personality traits were already included in the model. This suggests that traits may capture relevant prognostic information contained in past diagnoses, in addition to other features that are important for prognostic predictions. Overall, personality traits are informative for patient prognosis and should be routinely assessed in clinical practice alongside diagnostic interviews.
Personality traits constituted a significant predictor of almost all future outcomes assessed in this study. The results complement earlier findings in the CLPS sample, which demonstrated significant contributions of personality traits to predicting future patient functioning, over and above personality disorder diagnoses (Morey et al., 2007; Morey et al., 2012). However, here we extended these findings to Axis I diagnoses, mainly from the internalizing domain, and investigated predictions separately for past and present diagnoses. Moreover, when predicting future outcomes, personality traits were predictive beyond corresponding baseline self-reported symptoms and clinician-rated functioning. This is consistent with previous findings demonstrating that personality traits predict future psychopathology even when baseline symptoms are already included in the models (Jeronimus et al., 2016; Karsten et al., 2013; Klein, Kotov, & Bufferd, 2011; Ormel et al., 2013; Waszczuk et al., 2018).
Traits may be predictive of future outcomes because they capture the general disposition to experience certain symptoms and states, as evidenced by their good correspondence to the average levels of symptoms and experiences captured by ecological momentary assessments (DeYoung et al., 2020). Moreover, personality traits, symptoms, and disorders share etiological mechanisms, and traits might index common vulnerabilities (Durbin & Hicks, 2014; Klein et al., 2011). Notably, the current pattern of results was consistent across measures of both normal and maladaptive personality traits, in line with the evidence that they largely map onto the same latent dimensions (Widiger & Presnall, 2013; Widiger et al., 2018).
Conversely, past diagnoses, which were largely from the internalizing domain, contributed little prognostic utility when personality traits were included in the models. Specifically, past diagnoses contributed no incremental predictions when both current diagnoses and personality traits were included in the models, and predicted only five outcomes over and above personality traits in models without current diagnoses. This pattern of results is consistent with one previous study demonstrating that after accounting for personality traits, past internalizing disorder diagnoses were no longer predictive of new onsets and recurrences of internalizing disorders (Conway et al., 2016). The current study extends this work by predicting symptoms chronicity and various forms of functioning in three independent samples.
This pattern of findings could be due to several possible factors that challenge the validity of past diagnostic data, in particular biases in retrospective recall (Andrews et al., 1999; Bromet et al., 1986; Copeland et al., 2011; Moffitt et al., 2010; Olino et al., 2012; Takayanagi et al., 2014). For example, half of individuals hospitalized due to depression did not receive a past depression diagnosis when interviewed 25 years later (Andrews et al., 1999). This might be caused by forgetting past symptoms, especially if they occurred during a single episode, or due to cognitive reframing of past experiences, so that they are no longer recounted in a way that supports the assignment of a diagnosis (Streiner, Patten, Anthony, & Cairney, 2009). Moreover, it is possible that in a proportion of participants, in particular in community settings, diagnoses reflect an isolated episode of psychiatric illness followed by a full recovery (Glazer et al., 2019; Monroe & Harkness, 2011; Spencer, Biederman, & Mick, 2007), contributing little prognostic value for future outcomes. As such, the results are consistent with the idea that past episodes predict future outcomes if they reflect or make a lasting impact on person’s traits. These possibilities remain to be tested directly.
Past diagnoses predicted substance use first onsets and four functional outcomes over and above personality traits in models without current diagnoses. Similarly, when past and current diagnoses were combined into lifetime diagnoses, they were predictive of first onsets of depressive disorders and substance use, as well as several future functional outcomes, over and above personality traits. This is consistent with the assessment of functioning being integral to deriving psychiatric diagnoses. However, diagnoses did not contribute an incremental prediction of future PTSD and depression symptoms, over and above baseline symptoms. This finding compliments previous literature demonstrating that symptoms outperform diagnoses in predicting patients’ functioning and medication prescriptions (Conway et al., 2018; Waszczuk, Kotov, Ruggero, Gamez, & Watson, 2017; Waszczuk, Zimmerman, et al., 2017).
The current results might to some degree be driven by differences in statistical properties between traits and categorical diagnoses. Specifically, traits might serve as better predictors in statistical models due to their dimensional assessments that capture a full range of severity. Conversely, diagnostic interviews contain skip-out rules and don’t routinely support scoring disorder criteria continuously, but it is possible to modify SCID administration to achieve reliable dimensional symptom counts (Shankman et al., 2018). It is also possible that imperfect inter-rater reliabilities and other psychometric limitations affected predictions by diagnoses. Field trails demonstrated that categorical diagnoses routinely do not meet accepted inter-rater reliability standards (Regier et al., 2013), but the same disorders often showed excellent reliability when conceptualized dimensionally (Markon, Chmielewski, & Miller, 2011; Shea et al., 2002).
The results support HiTOP’s core focus on traits and symptoms in the present, and its assertion that personality traits are informative for prognostic decision-making (Ruggero et al., 2019; Widiger et al., 2018). The integration of personality traits assessment into clinical practice is feasible and in line with the DSM-5 inclusion of the self-report Personality Inventory for DSM-5 as an alternative to categorical personality disorders (Bach, Markon, Simonsen, & Krueger, 2015; Krueger et al., 2012; Krueger & Markon, 2014; Rodriguez-Seijas, Eaton, & Krueger, 2015). Moreover, mental health clinicians surveyed on this issue have usually been supportive and rated personality traits as clinically useful, in particular for patient communication purposes (Glover, Crego, & Widiger, 2012; Morey, Skodol, & Oldham, 2014).
Although the current study demonstrates the incremental utility of personality traits in aggregate, agreeableness and extraversion emerged as top unique predictors of future outcomes, beyond covariates, diagnoses, and other personality traits. Agreeableness and extraversion have previously been shown to prospectively associate with mental health and functioning (Bucher et al., 2019; Hakulinen et al., 2015; Laursen, Pulkkinen, & Adams, 2002; Ozer & Benet-Martinez, 2006; Tackett, Hernández, & Eisenberg, 2019). Both traits appear to capture information that is not included in diagnoses, possibly pertaining to the quality of interpersonal relationships (Braveman, Egerter, & Williams, 2011; Swickert, 2009; Tackett et al., 2019). Nonetheless, even personality traits thought to correspond more directly to internalizing psychopathology, such as neuroticism, showed unique associations with future disorder first onsets and functioning. This might be due to traits better capturing general underlying vulnerability, across the entire dimension of risk. Overall, the results support previous calls for assessments of all personality traits simultaneously in clinical practice (Bucher et al., 2019).
Limitations
Strengths of the current study include a comprehensive personality trait and clinical outcomes assessment that was collected alongside a structured diagnostic interview of past and present psychopathology in three independent, longitudinal samples. However, several limitations are notable. First, shared methods variance might explain why self-reported traits outperform interview-derived diagnoses in predicting future symptom outcomes. However, this confound cannot account for the findings that personality is also a better predictor of interviewer-derived future disorder onsets and long-term functioning. Moreover, the majority of diagnoses in the study come from the internalizing domain, thus it is possible that diagnoses from other domains would demonstrate a better incremental prediction. Relatedly, in Sample 2, the use of different measures of depression symptoms at baseline and 1-year follow up might have limited the precision of adjusting for baseline symptoms.
Second, prediction in statistical models cannot tell us about clinician prognosis in real-life clinical settings. In particular, while statistically significant, some of the incremental effect sizes achieved by adding personality traits to the prediction models might not be clinically meaningful. Third, the community adolescent sample did not present with a high number of past eating disorders and substance use diagnoses, which might have contributed to the low prognostic utility of past diagnoses for future disorder incidents in this sample. Moreover, the exclusion of adolescents with a history of MDD or dysthymia at enrollment (approximately 18 months prior to the baseline time point of the current study) might have impacted the ability of any past depressive diagnoses to predict future first onsets. However, onset of many disorders occur in adulthood, so psychiatric history in youth can have limited prognostic information (Kessler et al., 2007; Kessler et al., 2005). Personality traits can provide a more comprehensive indication of vulnerability in developmental populations than past diagnoses.
Fifth, the current study does not explicate the mechanisms though which personality is associated with future psychiatric outcomes. Many pathways are plausible, including personality sharing an underlying vulnerability, or constituting an indirect or direct causal factor, for future outcomes (Durbin & Hicks, 2014; Klein et al., 2011; Krueger & Tackett, 2003). Overall, a mechanistic understanding of complex personality-psychopathology relationships is needed for extending the current clinical implications beyond the outcome prediction, towards informing intervention approaches that target personality vulnerabilities directly.
Conclusions
The current multi-sample study demonstrated that personality traits predict future mental health outcomes, over and above diagnoses. Past psychiatric diagnoses, which were largely from the internalizing domain, were generally no longer informative about future outcomes when personality traits were included in predictive models. Together, these findings suggest that in order to improve the prediction of future psychiatric outcomes, clinicians should consider incorporating personality traits in patients’ assessments and case formulations.
Supplementary Material
Acknowledgements:
We gratefully acknowledge the support of participants in each study for generously contributing their time and energy.
Funding/Support:
The ADEPT study constituting Sample 1 was supported by the National Institute of Mental Health (RO1MH093479). The study in World Trade Center responders constituting Sample 2 was supported by the National Institute for Occupational Safety and Health (U01OH010712). The CLPS study constituting Sample 3 was supported by RO1 MH080221, RO1 MH01654, RO1 MH50837, RO150838, RO1 MH50839, RO1 50840, RO1 MH50850, RO1 MH69904, and RO1 MH 73708 from the National Institute of Mental Health.
Role of the sponsor:
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or decision to submit the manuscript for publication.
References
- Andrews G, Anstey K, Brodaty H, Issakidis C, & Luscombe G (1999). Recall of depressive episode 25 years previously. Psychological medicine, 29(4), 787–791. [DOI] [PubMed] [Google Scholar]
- Bach B, Markon K, Simonsen E, & Krueger RF (2015). Clinical utility of the DSM-5 alternative model of personality disorders: Six cases from practice. Journal of Psychiatric Practice®, 21(1), 3–25. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour research and therapy, 34(8), 669–673. [DOI] [PubMed] [Google Scholar]
- Braveman P, Egerter S, & Williams DR (2011). The social determinants of health: coming of age. Annual review of public health, 32. [DOI] [PubMed] [Google Scholar]
- Bromet E, Dunn LO, Connell MM, Dew MA, & Schulberg HC (1986). Long-term reliability of diagnosing lifetime major depression in a community sample. Archives of General Psychiatry, 43(5), 435–440. [DOI] [PubMed] [Google Scholar]
- Bromet E, Hobbs M, Clouston S, Gonzalez A, Kotov R, & Luft B (2016). DSM-IV post-traumatic stress disorder among World Trade Center responders 11–13 years after the disaster of 11 September 2001 (9/11). Psychological medicine, 46(4), 771–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucher MA, Suzuki T, & Samuel DB (2019). A meta-analytic review of personality traits and their associations with mental health treatment outcomes. Clinical psychology review, 70, 51–63. [DOI] [PubMed] [Google Scholar]
- Canty-Mitchell J, & Zimet GD (2000). Psychometric properties of the Multidimensional Scale of Perceived Social Support in urban adolescents. American journal of community psychology, 28(3), 391–400. [DOI] [PubMed] [Google Scholar]
- Conway CC, Craske MG, Zinbarg RE, & Mineka S (2016). Pathological personality traits and the naturalistic course of internalizing disorders among high-risk young adults. Depression and anxiety, 33(1), 84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, … South SC (2018). A hierarchical taxonomy of psychopathology can transform mental health research. Perspectives on Psychological Science, 14(3), 419–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, & Angold A (2011). Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry, 50(3), 252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Wolke D, Shanahan L, & Costello EJ (2015). Adult functional outcomes of common childhood psychiatric problems: a prospective, longitudinal study. JAMA psychiatry, 72(9), 892–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). Professional manual: revised NEO personality inventory (NEO-PI-R) and NEO five-factor inventory (NEO-FFI). Odessa, FL: Psychological Assessment Resources, 61. [Google Scholar]
- Croft P, Altman DG, Deeks JJ, Dunn KM, Hay AD, Hemingway H, … Petersen SE (2015). The science of clinical practice: disease diagnosis or patient prognosis? Evidence about “what is likely to happen” should shape clinical practice. BMC medicine, 13(1), 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasaro CR, Holden WL, Berman KD, Crane MA, Kaplan JR, Lucchini RG, … Tirunagari US (2015). Cohort Profile: World Trade Center Health Program General Responder Cohort. International journal of epidemiology, dyv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedrick RF, Shaunessy-Dedrick E, Suldo SM, & Ferron JM (2015). Psychometric properties of the school attitude assessment survey–revised with international baccalaureate high school students. Gifted Child Quarterly, 59(1), 38–54. [Google Scholar]
- DeYoung CG, Chmielewski M, Clark LA, Condon DM, Kotov R, Krueger RF, … Mullins‐Sweatt SN (2020). The distinction between symptoms and traits in the Hierarchical Taxonomy of Psychopathology (HiTOP). Journal of Personality. [DOI] [PubMed] [Google Scholar]
- Dobie DJ, Kivlahan DR, Maynard C, Bush KR, McFall M, Epler AJ, & Bradley KA (2002). Screening for post-traumatic stress disorder in female Veteran’s Affairs patients: validation of the PTSD checklist. General Hospital Psychiatry, 24(6), 367–374. [DOI] [PubMed] [Google Scholar]
- Dornbach-Bender A, Ruggero CJ, Schuler K, Contractor AA, Waszczuk MA, Kleva CS, … Kotov R (2019). Positive and negative affect in the daily life of world trade center responders with PTSD: An ecological momentary assessment study. Psychological trauma: theory, research, practice and policy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durbin CE, & Hicks BM (2014). Personality and psychopathology: A stagnant field in need of development. European journal of personality, 28(4), 362–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, & Cohen J (1976). The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry, 33(6), 766–771. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1997). Structured clinical interview for DSM-IV Axis 1 Disorders—Non-patient edition (version 2.0). New York State Psychiatric Institute, Biometrics Research Department. [Google Scholar]
- Glazer KB, Sonneville KR, Micali N, Swanson SA, Crosby R, Horton NJ, … Field AE (2019). The course of eating disorders involving bingeing and purging Among adolescent girls: prevalence, stability, and transitions. Journal of Adolescent Health, 64(2), 165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover NG, Crego C, & Widiger TA (2012). The clinical utility of the Five Factor Model of personality disorder. Personality Disorders: Theory, Research, and Treatment, 3(2), 176. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Friedberg F, Li X, Zvolensky MJ, Bromet EJ, Mahaffey BL, … Kotov R (2017). Trauma-focused smoking cessation for smokers exposed to the World Trade Center Disaster: A randomized clinical trial. Nicotine & Tobacco Research, 19(8), 968–975. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Shea MT, Skodol AE, McGlashan TH, Morey LC, Stout RL, … Keller MB (2000). The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. Journal of personality disorders, 14(4), 300–315. [DOI] [PubMed] [Google Scholar]
- Hakulinen C, Elovainio M, Pulkki ‐ Råback L, Virtanen M, Kivimäki M, & Jokela M (2015). Personality and depressive symptoms: Individual participant meta-analysis of 10 cohort studies. Depression and anxiety, 32(7), 461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Malone JC, Ansell EB, Sanislow CA, Grilo CM, McGlashan TH, … Skodol AE (2011). Personality assessment in DSM-5: Empirical support for rating severity, style, and traits. Journal of personality disorders, 25(3), 305–320. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Morey LC, Shea MT, McGlashan TH, Sanislow CA, Grilo CM, … Skodol AE (2007). Personality traits predict current and future functioning comparably for individuals with major depressive and personality disorders. The Journal of nervous and mental disease, 195(3), 266–269. [DOI] [PubMed] [Google Scholar]
- Hur J, Stockbridge MD, Fox AS, & Shackman AJ (2018). Dispositional negativity, cognition, and anxiety disorders: An integrative translational neuroscience framework. Progress in Brain Research, 247, 375–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeronimus B, Kotov R, Riese H, & Ormel J (2016). Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants. Psychological medicine, 46(14), 2883–2906. [DOI] [PubMed] [Google Scholar]
- John OP, Donahue EM, & Kentle RL (1991). The big five inventory—versions 4a and 54. In: Berkeley, CA: University of California, Berkeley, Institute of Personality; …. [Google Scholar]
- John OP, & Srivastava S (1999). The Big Five trait taxonomy: History, measurement, and theoretical perspectives. Handbook of personality: Theory and research, 2(1999), 102–138. [Google Scholar]
- Jones SH, Thornicroft G, Coffey M, & Dunn G (1995). A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). The British Journal of Psychiatry, 166(5), 654–659. [DOI] [PubMed] [Google Scholar]
- Karsten J, Penninx BW, Verboom CE, Nolen WA, & Hartman CA (2013). Course and risk factors of functional impairment in subthreshold depression and anxiety. Depression and anxiety, 30(4), 386–394. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, … Ryan N (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 980–988. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, & Andreasen NC (1987). The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry, 44(6), 540–548. [DOI] [PubMed] [Google Scholar]
- Kendell R, & Jablensky A (2003). Distinguishing between the validity and utility of psychiatric diagnoses. American journal of psychiatry, 160(1), 4–12. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Amminger GP, Aguilar ‐ Gaxiola S, Alonso J, Lee S, & Ustun TB (2007). Age of onset of mental disorders: a review of recent literature. Current opinion in psychiatry, 20(4), 359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Klein DN, Kotov R, & Bufferd SJ (2011). Personality and depression: explanatory models and review of the evidence. Annual Review of Clinical Psychology, 7, 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koerner N, Hood HK, & Antony MM (2011). Interviewing and case formulation. The Oxford handbook of clinical psychology, 225–252. [Google Scholar]
- Kotov R, Krueger RF, & Watson D (2018). A paradigm shift in psychiatric classification: the Hierarchical Taxonomy Of Psychopathology (HiTOP). World Psychiatry, 17(1), 24–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby M, … Zimmerman M (2017). The Hierarchical Taxonomy Of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of abnormal psychology, 126(4), 454. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Cicero DC, Conway CC, DeYoung CG, … Wright AG (2021). The Hierarchical Taxonomy of Psychopathology (HiTOP): A Quantitative Nosology Based on Consensus of Evidence. Annual Review of Clinical Psychology, 17. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The Phq-9. Journal of general internal medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, & Skodol AE (2012). Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological medicine, 42(09), 1879–1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Kotov R, Watson D, Forbes MK, Eaton NR, Ruggero CJ, … Zimmerman J (2018). Progress in achieving empirical classification of psychopathology. World Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, & Markon KE (2014). The role of the DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. Annual Review of Clinical Psychology, 10, 477–501. [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Tackett JL (2003). Personality and psychopathology: Working toward the bigger picture. Journal of personality disorders, 17(2: Special issue), 109–128. [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Tackett JL (2006). Personality and psychopathology: Guilford Press. [Google Scholar]
- Lahey BB (2009). Public health significance of neuroticism. American Psychologist, 64(4), 241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen B, Pulkkinen L, & Adams R (2002). The antecedents and correlates of agreeableness in adulthood. Developmental psychology, 38(4), 591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Olfson M, Portera L, Farber L, & Sheehan DV (1997). Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. The international journal of psychiatry in medicine, 27(2), 93–105. [DOI] [PubMed] [Google Scholar]
- Markon KE, Chmielewski M, & Miller CJ (2011). The reliability and validity of discrete and continuous measures of psychopathology: a quantitative review. Psychological Bulletin, 137(5), 856. [DOI] [PubMed] [Google Scholar]
- McCoach DB, & Siegle D (2003). The school attitude assessment survey-revised: A new instrument to identify academically able students who underachieve. Educational and Psychological Measurement, 63(3), 414–429. [Google Scholar]
- Michelini G, Perlman G, Tian Y, Mackin D, Nelson B, Klein D, & Kotov R (2020). Multiple domains of risk factors for first onset of depression in adolescent girls. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, & Poulton R (2010). How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological medicine, 40(6), 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, & Harkness KL (2011). Recurrence in major depression: a conceptual analysis. Psychological Review, 118(4), 655. [DOI] [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ, Gunderson JG, Skodol AE, Shea MT, Yen S, … Sanislow CA (2007). Comparison of alternative models for personality disorders. Psychological medicine, 37(7), 983. [DOI] [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ, Markowitz JC, Gunderson JG, Grilo CM, McGlashan TH, … Ansell EB (2012). Comparison of alternative models for personality disorders, II: 6-, 8-, and 10-year follow-up. Psychological medicine, 42(8), 1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC, Skodol AE, & Oldham JM (2014). Clinician judgments of clinical utility: A comparison of DSM-IV-TR personality disorders and the alternative model for DSM-5 personality disorders. Journal of abnormal psychology, 123(2), 398. [DOI] [PubMed] [Google Scholar]
- Olino TM, Shankman SA, Klein DN, Seeley JR, Pettit JW, Farmer RF, & Lewinsohn PM (2012). Lifetime rates of psychopathology in single versus multiple diagnostic assessments: Comparison in a community sample of probands and siblings. Journal of psychiatric research, 46(9), 1217–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Jeronimus BF, Kotov R, Riese H, Bos EH, Hankin B, … Oldehinkel AJ (2013). Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clinical psychology review, 33(5), 686–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Oerlemans AM, Raven D, Laceulle OM, Hartman CA, Veenstra R, … Reijneveld SA (2017). Functional outcomes of child and adolescent mental disorders. Current disorder most important but psychiatric history matters as well. Psychol Med, 47(7), 1271–1282. [DOI] [PubMed] [Google Scholar]
- Ozer DJ, & Benet-Martinez V (2006). Personality and the prediction of consequential outcomes. Annu. Rev. Psychol, 57, 401–421. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Clarke DE, Kraemer HC, Kuramoto SJ, Kuhl EA, & Kupfer DJ (2013). DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. American Journal of Psychiatry, 170(1), 59–70. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Kuncel NR, Shiner R, Caspi A, & Goldberg LR (2007). The power of personality: The comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science, 2(4), 313–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, & Krueger RF (2015). How transdiagnostic factors of personality and psychopathology can inform clinical assessment and intervention. Journal of personality assessment, 97(5), 425–435. [DOI] [PubMed] [Google Scholar]
- Ruggero CJ, Kotov R, Hopwood CJ, First M, Clark LA, Skodol AE, … Cicero DC (2019). Integrating the Hierarchical Taxonomy of Psychopathology (HiTOP) into clinical practice. Journal of consulting and clinical psychology, 87(12), 1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shackman AJ, Tromp DP, Stockbridge MD, Kaplan CM, Tillman RM, & Fox AS (2016). Dispositional negativity: An integrative psychological and neurobiological perspective. Psychological bulletin, 142(12), 1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankman SA, Funkhouser CJ, Klein DN, Davila J, Lerner D, & Hee D (2018). Reliability and validity of severity dimensions of psychopathology assessed using the Structured Clinical Interview for DSM-5 (SCID). International journal of methods in psychiatric research, 27(1), e1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea MT, Stout R, Gunderson J, Morey LC, Grilo CM, McGlashan T, … Zanarini MC (2002). Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. American Journal of Psychiatry, 159(12), 2036–2041. [DOI] [PubMed] [Google Scholar]
- Sheehan DV (1986). The anxiety disease: Bantam. [Google Scholar]
- Soto CJ, John OP, Gosling SD, & Potter J (2011). Age differences in personality traits from 10 to 65: Big Five domains and facets in a large cross-sectional sample. Journal of personality and social psychology, 100(2), 330. [DOI] [PubMed] [Google Scholar]
- Spencer TJ, Biederman J, & Mick E (2007). Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. Journal of pediatric psychology, 32(6), 631–642. [DOI] [PubMed] [Google Scholar]
- Startup M, Jackson MC, & Bendix S (2002). The concurrent validity of the Global Assessment of Functioning (GAF). British Journal of Clinical Psychology, 41(4), 417–422. [DOI] [PubMed] [Google Scholar]
- Streiner DL, Patten SB, Anthony JC, & Cairney J (2009). Has ‘lifetime prevalence’reached the end of its life? An examination of the concept. International journal of methods in psychiatric research, 18(4), 221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suldo SM, Shaffer EJ, & Shaunessy E (2008). An independent investigation of the validity of the School Attitude Assessment Survey—Revised. Journal of Psychoeducational Assessment, 26(1), 69–82. [Google Scholar]
- Swickert R (2009). 30 Personality and social support processes. The Cambridge handbook of personality psychology, 524. [Google Scholar]
- Tackett JL, Hernández MM, & Eisenberg N (2019). Agreeableness. In McAdams D, Shiner R, & Tackett JL (Eds.), The Handbook of Personality Development. [Google Scholar]
- Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, & Mojtabai R (2014). Accuracy of reports of lifetime mental and physical disorders: results from the Baltimore Epidemiological Catchment Area study. JAMA psychiatry, 71(3), 273–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KM, Yalch MM, Krueger RF, Wright AG, Markon KE, & Hopwood CJ (2012). The convergent structure of DSM-5 personality trait facets and five-factor model trait domains. Assessment, 1073191112457589. [DOI] [PubMed] [Google Scholar]
- Ware JE, Keller SD, & Kosinski M (1998). Sf-12: How to Score the Sf-12 Physcial and Mental Health Summary Scales: QualityMetric Incorporated. [Google Scholar]
- Ware JE, Kosinski M, & Keller SD (1996). A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care, 34(3), 220–233. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, & Stout RL (1994). Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of psychiatric research, 28(6), 531–545. [DOI] [PubMed] [Google Scholar]
- Waszczuk MA, Kotov R, Ruggero CJ, Gamez W, & Watson D (2017). Hierarchical Structure of Emotional Disorders: From Individual Symptoms to the Spectrum Journal of abnormal psychology. [DOI] [PubMed] [Google Scholar]
- Waszczuk MA, Li K, Ruggero CJ, Clouston SA, Luft BJ, & Kotov R (2018). Maladaptive Personality Traits and 10-Year Course of Psychiatric and Medical Symptoms and Functional Impairment Following Trauma. Annals of Behavioral Medicine, 52(8), 697–712. [DOI] [PubMed] [Google Scholar]
- Waszczuk MA, Zimmerman M, Ruggero C, Li K, MacNamara A, Weinberg A, … Kotov R (2017). What do clinicians treat: diagnoses or symptoms? The incremental validity of a symptom-based, dimensional characterization of emotional disorders in predicting medication prescription patterns. Comprehensive Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Naragon-Gainey K, Koffel E, Chmielewski M, Kotov R, … Ruggero CJ (2012). Development and validation of new anxiety and bipolar symptom scales for an expanded version of the IDAS (the IDAS-II). Assessment, 19(4), 399–420. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies. [Google Scholar]
- Widiger TA (2011). Personality and psychopathology. World Psychiatry, 10(2), 103–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiger TA, & Presnall JR (2013). Clinical Application of the F ive-F actor M odel. Journal of Personality, 81(6), 515–527. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Sellbom M, Chmielewski M, Clark LA, DeYoung CG, Kotov R, … Mullins-Sweatt S (2018). Personality in a Hierarchical Model of Psychopathology. Clinical Psychological Science, 2167702618797105. [Google Scholar]
- Wilkins KC, Lang AJ, & Norman SB (2011). Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and anxiety, 28(7), 596–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, … McGlashan TH (2000). The collaborative longitudinal personality disorders study: Reliability of axis I and II diagnoses. Journal of personality disorders, 14(4), 291–299. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The multidimensional scale of perceived social support. Journal of personality assessment, 52(1), 30–41. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, & Berkoff KA (1990). Psychometric characteristics of the multidimensional scale of perceived social support. Journal of personality assessment, 55(3–4), 610–617. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


