Abstract
Introduction
Soft robotic wearable devices, referred to as exosuits, can be a valid alternative to rigid exoskeletons when it comes to daily upper limb support. Indeed, their inherent flexibility improves comfort, usability, and portability while not constraining the user’s natural degrees of freedom. This review is meant to guide the reader in understanding the current approaches across all design and production steps that might be exploited when developing an upper limb robotic exosuit.
Methods
The literature research regarding such devices was conducted in PubMed, Scopus, and Web of Science. The investigated features are the intended scenario, type of actuation, supported degrees of freedom, low-level control, high-level control with a focus on intention detection, technology readiness level, and type of experiments conducted to evaluate the device.
Results
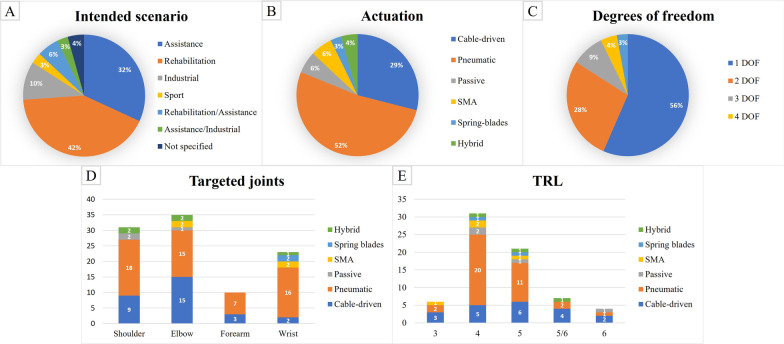
A total of 105 articles were collected, describing 69 different devices. Devices were grouped according to their actuation type. More than 80% of devices are meant either for rehabilitation, assistance, or both. The most exploited actuation types are pneumatic (52%) and DC motors with cable transmission (29%). Most devices actuate 1 (56%) or 2 (28%) degrees of freedom, and the most targeted joints are the elbow and the shoulder. Intention detection strategies are implemented in 33% of the suits and include the use of switches and buttons, IMUs, stretch and bending sensors, EMG and EEG measurements. Most devices (75%) score a technology readiness level of 4 or 5.
Conclusion
Although few devices can be considered ready to reach the market, exosuits show very high potential for the assistance of daily activities. Clinical trials exploiting shared evaluation metrics are needed to assess the effectiveness of upper limb exosuits on target users.
Keywords: Assistive technology, Exoskeletons, Exosuits, Rehabilitation robotics, Soft robotics, Upper limb
Background
Neuromuscular diseases (e.g., stroke, spinal cord injury, muscular dystrophy, etc.) and neurodegenerative diseases (e.g., multiple sclerosis, amyotrophic lateral sclerosis, etc.) can lead to severe motor impairment. On the one hand, this requires the patients to undertake a rehabilitation path to mitigate negative effects and improve motor functions and their general state of health. On the other hand, patients might become dependent on long-term care assistance for activities of daily living (ADLs).
Disabilities of the upper limb have a strong impact on the subject’s quality of life since they affect the possibility to independently perform basic activities [1, 2]. In this context, wearable rehabilitative and assistive devices, such as exoskeletons, may play an important role [3]. Exoskeletons are composed of rigid links, that are attached to the user’s limbs, and actuators, which exert torques at the joint level [4]. The main scenarios for which exoskeletons have been developed are: (i) motor rehabilitation of impaired limbs (rehabilitation scenario), (ii) assistance of subjects with disability with ADLs (assistive scenario), (iii) motor augmentation of healthy subjects in contexts such as factory work, military applications or sport (augmentation scenario).
In the rehabilitation scenario, wearable robots support the therapist in providing rehabilitative exercises. The advantage they bring with respect to traditional therapy lies in the higher number of repetitions that can be provided in a session, the possibility of objectively quantifying the subject’s performance, the relief of the therapist’s physical burden, and the possibility to monitor the patient’s involvement in the training. This makes it possible to increase the dose, personalize the intensity of the training, and stimulate the participation of the subject, which are all key factors in motor re-learning [5–7].
In the assistance scenario, wearable robots are meant to support movements typical of ADLs, such as drinking, eating, reaching, and personal hygiene [8, 9]. The use of assistive devices could help the user gain back part of his/her independence and facilitate participation, which is fundamental from a psychological and social point of view.
In the augmentation scenario, wearable robots provide high torques to improve the subject’s capabilities beyond the physiological level or to share and redistribute the load applied on the limbs. The main goal is to prevent musculoskeletal diseases typical of fatiguing and repetitive work and to reduce the metabolic cost [10].
A recent review written by Xiloyannis and colleagues [11] features a taxonomy useful to classify the different types of wearable robots to assist or augment the user’s movements. The first branching of their taxonomy classifies the devices between those that rely on a rigid frame to exert torques, referred to as “rigid exoskeletons”, and those that do not, referred to as “soft robotic suits”.
Although rigid exoskeletons can provide good trajectory tracking and can exert high torques, which are borne by the exoskeletal structure, they present numerous disadvantages: (i) they are heavy and bulky, which increases the inertia of the system and the metabolic cost of wearing; (ii) they are expensive; (iii) the rigid links constrain the natural degrees of freedom of the human joints and require careful alignment, which is time-consuming; (iv) even the smallest misalignment leads the exoskeleton to interfere with the physiological movements of the limb; (v) they have a low aesthetic quality. All these drawbacks prevent rigid exoskeletons to be widely adopted outside the clinical environment and to be used for home rehabilitation or daily assistance [12].
Therefore, soft robotic devices have been recently proposed as a valid alternative. Robotic suits are inherently compliant thanks to the lack of rigid links and the use of soft materials, such as fabric or soft polymers, as an interface with the subject’s limbs [13]. The use of such materials brings several advantages: (i) it supports the wearer’s movements without over-constraining the joints, thus maintaining their mobility and flexibility; (ii) precise joint alignment is not required, reducing the time needed to wear the device; (iii) it improves the comfort of wear and ease of donning and doffing, thus improving usability; (iv) it reduces the overall weight of the device, as well as the encumbrance, thus improving the portability; (v) it reduces the cost. These characteristics make this relatively new technology quite promising in delivering rehabilitation and providing assistance outside the clinical context.
However, despite the numerous advantages listed, robotic suits present some challenges that require further research. In particular, they act more as an external muscle, rather than an external skeleton [11]. This means that the actuation relies on the skeletal structure of the user, preventing the application of high torques, which may hurt the wearer. Moreover, their intrinsic compliance sacrifices the accuracy of the movements and the magnitude of the assistance, thus making the control quite complex. Indeed, the sleeve may slide, influencing the data collected by the sensors and making the force transmission unreliable [14, 15]. The shear forces acting on the skin could be increased as well. In addition, when it comes to upper limb assistance, a further challenge of soft robotic devices is represented by the control of upper limb movements. In fact, lower limb devices usually implement control strategies that rely upon the cyclicality of walking. In upper limb devices, instead, the number of dynamic tasks to be implemented, the unpredictable interaction with the environment, and the complexity of the biomechanics make their control a more complex operation [16].
Objective
In view of the growing research interest in the field, and given that no device has reached the market yet, we provide a complete and systematic literature review of soft robotic devices for upper limb assistance.
Xiloyannis and colleagues [11] provide an insightful narrative review on the modes of actuation, the physical human-robot interfaces, and the intention-detection strategies of some of the state-of-the-art soft devices, both for the upper and the lower limbs. However, they do not provide a complete list of all the devices. Another recent review [17] focuses only on the description of the different types of actuators for soft robotic devices.
The aim of this review is instead to provide a broad picture of the state of the art to help researchers that approach this field. Indeed, it investigates the possibilities for the application scenario, the actuation and the actuated joints, the design approaches, the intention detection strategies, and the validation experiments that might be exploited in the process of developing an upper limb robotic suit.
Methods
Search methods
We run a systematic review using the keywords in the electronic database search shown in Table 1. Keywords are subdivided into three categories: (1) the type of device, (2) the attributes of interest, and (3) the body section the devices interact with. The keywords were combined using Boolean operators (AND/OR) as follows: (1 OR 2 OR ... 7) AND (8 OR 9 OR ... 15) AND (16 OR 17 OR ... 22).
Table 1.
List of the keywords used for the electronic search
| Device | Attributes | Body section |
|---|---|---|
| 1. Exoskeleton | 8. Soft | 16. Upper limb |
| 2. Robot | 9. Flexible | 17. Arm |
| 3. Exosuit | 10. Wearable | 18. Shoulder |
| 4. Exosleeve | 11. Inflatable | 19. Elbow |
| 5. Sleeve | 12. Cable-driven | 20. Forearm |
| 6. Orthosis | 13. Pneumatic | 21. Wrist |
| 7. Suit | 14. Fabric-based | 22. Upper extremity |
| 15. Portable |
We restricted the research among papers written in English and published between 2000 and 2020. We searched the following bibliographic electronic databases: PubMed, Scopus, Web of Science. Furthermore, we performed backward and forward reference searching on the relevant articles identified from the electronic search to include the highest number of articles. We did not conduct any research among patents.
Data collection and analysis
The search results were screened by three reviewers (EB, MG, EA). The articles resulting from the database search were selected according to the following inclusion and exclusion criteria:
The device must be soft at the target joint level, meaning that there should be no rigid links that impose physical constraints on joint motions. Devices containing some rigid parts elsewhere are included.
The device must be intended to facilitate and support the movement of at least one degree of freedom of a joint among the shoulder, the elbow, or the wrist.
The device must be intended to be wearable and portable (if it is not portable when described in the literature document, it must be meant to be in next iterations).
The article is written in English and accessible as a full text by the Review Authors.
Hand devices were excluded from this review since they present particular design considerations and were already described by Chu and colleagues [18]. The Authors independently read the titles and the abstracts of retrieved articles and eliminated obviously irrelevant studies. The full texts of the remaining studies were examined and, according to the predetermined inclusion and exclusion criteria, they were independently ranked by at least two Authors as relevant and irrelevant. Discrepancies between Review Authors were resolved through discussion.
Data extraction
To provide a comprehensive summary of the identified devices, we investigated the following features of the included studies:
the intended application scenario, either rehabilitation, assistance, or augmentation, as previously classified;
the actuation characteristics in terms of the type of actuator(s) used and the number and type of implemented degree(s) of freedom (DOF) or supported movements;
the design approach followed with a focus on bio-inspired designs or other noteworthy design solutions;
the implemented intention-detection strategies;
the experiments conducted to validate the prototype.
The Technology Readiness Level (TRL) is also assessed for each device to provide a glimpse of the technological advancement in the field. The TRL is assigned according to the TRL definition provided by the HORIZON 2020 - Work Programme 2014-2015 and as explained in Table 2.
Table 2.
TRL definition.
| TRL | Definition | Explanation |
|---|---|---|
| 1 | Basic principle observed | The idea has been formulated |
| 2 | Technology concept formulated | The concept and the application have been formulated |
| 3 | Experimental proof of concept | The first prototype has been built but not tested |
| 4 | Technology validated in lab | The prototype has been tested in laboratory on a mannequin |
| 5 | Technology validated in relevant environment | The prototype is mature in terms of design and control and has been tested on healthy subjects |
| 6 | Technology demonstrated in relevant environment | The prototype has been tested for its efficacy on subjects with motor disability or healthy subjects according to the intended scenario |
| 7 | System prototype demonstration in operational environment | The system has been tested for its intended purpose in the clinic, at home, in the factory, in sport fields |
| 8 | System complete and qualified | The system is ready to be produced in large scale |
| 9 | Actual system proven in operational environment | The system is available in the market |
Results
Results of the electronic search
A flow chart outlining the studies selection process is shown in Fig. 1.
Fig. 1.
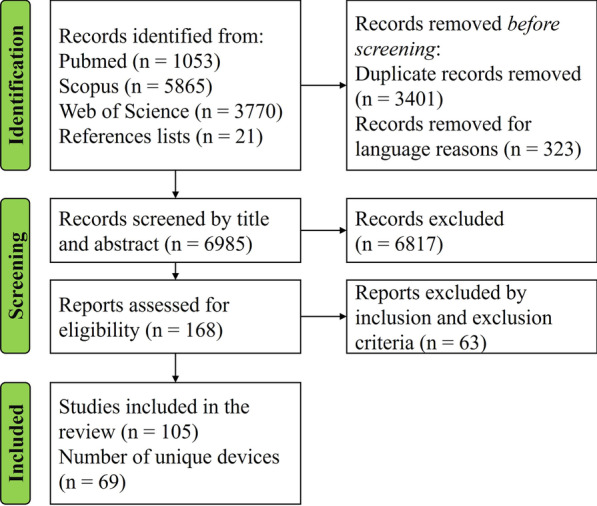
PRISMA flowchart of the literature search process.
The electronic databases’ search resulted in a total of 10688 identified studies. Searches through the reference lists resulted in 21 additional studies, reaching a total number of records of 10709. After the removal of 3401 duplicates and 323 articles that were not written in English, the titles and abstracts were pre-screened and irrelevant studies were eliminated. The full texts of 168 articles were analyzed and 105 articles, describing a total of 69 devices, were finally selected. Articles from the same research group were considered independently if the devices described were evidently different from each other, whereas articles regarding different iterations of the same device were grouped. For what concerns the design characteristics, the latest prototype iteration was considered, whereas, for what regards controllers, experiments, and evaluation metrics, the most representative across all papers concerning the same device were considered.
Overview of the identified devices
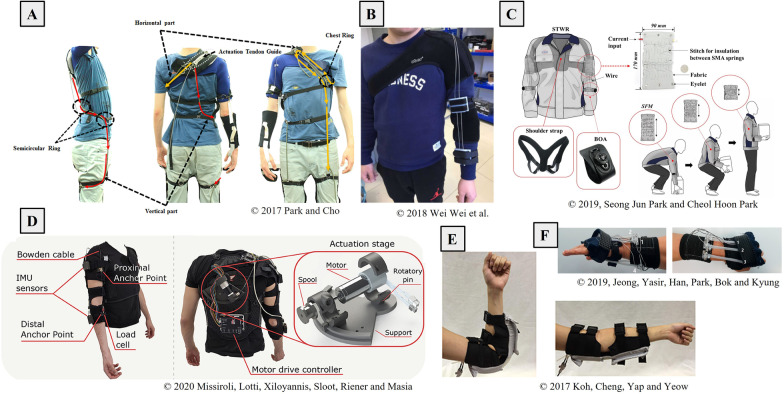
An overview of the identified devices is provided in Tables 3, 4, 5, 6, 7, where information on the intended application, actuation (degrees of freedom and type of actuators) and control strategy is provided. The assigned TRL is also reported for each device. Tables are organized grouping the prototypes according to their actuation strategy (i.e., cable-driven, passive, pneumatic, shape memory alloy, hybrid). Examples of soft robotic wearable devices for the upper limb are shown in Fig. 2.
Table 3.
Overview of the cable-driven devices.
| Scenario | DOF | Low-level Control | High-level Control | TRL | Year and Related Works |
|---|---|---|---|---|---|
| R | 1, S: abd/add | Position | – | 4 | 2012 [58, 89] |
| R | 1, E: flex/ext | - | – | 3 | 2015 [54] |
| A | 3, S: abd/add and flex/ext, E: flex/ext | Position | Mirroring the healthy limb | 5 | 2017 [62] |
| R/A | 7, S: humeral rot, abd/add, flex/ext, E: flex/ext, FA: pron/sup, wrist flex/ext and radial/ulnar dev | Position | Pre-determined joints trajectory | 5 | 2018 [43, 90] |
| R | 3, S: abd/add, flex/ext E: flex/ext | Speed | – | 4 | 2018 [34] |
| A | 1, E: flex/ext | Force | Arm dynamics compensation | 4 | 2018 [60] |
| R | 5, S: humeral rot, abd/add and flex/ext, E: flex/ext, FA: pron/sup | Position | Joystick or mirroring the healthy limb | 6/7 | 2019 [55, 79, 91] |
| A | 1, W: Dart throwing motion | Force | EMG-trigger | 5 | 2019 [48] |
| A | 2, E: flex/ext, FA: pron/sup | Position | – | 4 | 2019 [92] |
| R | 2, S: flex/ext, E: flex/ext | Position | Pre-determined joints trajectory | 5 | 2019 [93] |
| R | 1, E: flex/ext | Torque | Smartphone app. trigger | 3 | 2019 [66] |
| R | 1, E: flex/ext | Admittance | EMG-based neural-network torque estimation | 5 | 2019 [56, 57, 94] |
| R/A/I | 1, E: flex/ext | Admittance | IMU-based gravity compensation or EMG-based torque estimation | 5/6 | 2020 [28–32, 53, 74, 78, 95–101] |
| I | 2: bimanual lifting | Force | EMG trigger | 5/6 | 2020 [73, 102] |
| I | 4, S: elev, E: flex, bilateral | Position | Voice recognition | 5/6 | 2020 [52, 103] |
| I | 1, E: flex/ext | - | – | 3 | 2020 [59] |
| R | 1,W: flex/ext, ulnar/radial dev | Position | Pre-determined joints trajectory | 6 | 2020 [104] |
| - | 2, S: elev, E: flex/ext | Position | Pre-determined joints trajectory | 5/6 | 2020 [61, 105, 106] |
| A | 1, S: elev coupled with hum rot | Admittance | Gravity compensation | 5 | 2020 [33] |
| R | 1, E: flex/ext | Motion | - | 4 | 2020 [107] |
S = shoulder, E = elbow, FA = forearm, W = wrist, abd = abduction, add = adduction, flex = flexion, ext = extension, rot = rotation, pron = pronation, sup = supination, dev = deviation, elev = elevation, R = rehabilitation, A = assistance, I = industrial
Table 4.
Overview of the passive devices.
| Scenario | DOF | Low-level Control | High-level Control | TRL | Year and Related Works |
|---|---|---|---|---|---|
| I | 1, S: elev | – | – | 6 | 2017 [35] |
| I | 1, Weight lifting support | – | – | 4 | 2018 [36] |
| A | 1, E: flex/ext | – | – | 5 | 2019 [38] |
| A | 1, S: elev | - | – | 4 | 2020 [37] |
S = shoulder, E = elbow, flex = flexion, ext = extension, elev = elevation, A = assistance, I = industrial
Table 5.
Overview of the pneumatic devices.
| Scenario | DOF | Low-level Control | High-level Control | TRL | Year and Related works |
|---|---|---|---|---|---|
| A | 2, S: abd/add, E: flex/ext | Pressure | – | 4 | 2004 [108, 109] |
| A | 1, W: flex/ext | Pressure | Bending signal trigger | 5 | 2005 [25] |
| R | 4, E: flex/ext, FA: pron/sup, W: flex/ext, ulnar/radial dev | Force | Individual actuators control to induce muscle activation pattern | 5 | 2013 [110–115] |
| R | 3, FA: pron/sup, W: flex/ext, ulnar/radial dev | Pressure | – | 4/5 | 2015 [116] |
| R | 2, W: flex/ext radial/ulnar dev | Position | – | 5 | 2015 [76] |
| R | 1, E: flex/ext | Position | Pre-defined joint trajectory | 5 | 2015 [22] |
| A | 1, S: abd/add | Position | – | 4 | 2016 [15] |
| R | 2, W: flex/ext, radial/ulnar dev | Pressure | Manually defined setpoint | 4 | 2017 [117, 118] |
| R | 1, E: flex/ext | Pressure | Pre-defined or EMG triggered | 5 | 2017 [24] |
| A | 2, S: abd/add, flex/ext | Position | – | 4 | 2017 [14] |
| A | 1, S: abd/add | Position | – | 4 | 2017 [119] |
| R | 3, S: flex-ext, E: flex-ext, FA: pron-sup | Pressure | Manually defined setpoint | 4 | 2018 [26] |
| A/I | 1, E: flex/ext | - | – | 4 | 2018 [120, 121] |
| A | 1, E: flex/ext | Pressure | Bending signal trigger | 5 | 2018 [122, 123] |
| Sport | 1, S: Bat swing assistance in baseball | Pressure | Acceleration signal trigger | 5 | 2018 [50] |
| Sport | 1, S: forehand swing motion Medical | Pressure | Electric valve switch | 5 | 2018 [51] |
| R | 2, E: flex/ext, FA: pron/sup | Pressure | – | 4 | 2018 [124] |
| R | 2, W: flex/ext, radial/ulnar dev | Position | Mirroring the healthy limb | 5 | 2018 [70] |
| R | 2, S: Bimanual wheelchair push | Pressure | IMUs signal-based trigger | 5 | 2018 [69] |
| I | 1, E: flex/ext | Pressure | Manually defined setpoint | 4 | 2018 [20] |
| Medical | 3, S: abd/add, flex/ext, E: flex/ext | Pressure | – | 4 | 2019 [77, 125] |
| - | 1, E: flex/ext | Pressure | – | 4 | 2019 [126] |
| R/A | 2, S: abd/add, flex/ext | Pressure | Joystick | 4 | 2019 [21] |
| R | 1, S: abd/add | Pressure | Buttons trigger inflation and deflation | 4/5 | 2019 [63] |
| R | 1, E: flex/ext | Position | Pre-defined joint trajectory | 3 | 2019 [23, 127] |
| R | 2, W: flex/ext, radial/ulnar dev | Pressure | – | 4 | 2019 [128] |
| R | 1, FA: pron/sup | Position | Pre-defined joint trajectory | 4 | 2019 [129] |
| R | 2, S: elev, E: flex/ext | Position | Mirroring the healthy limb | 5 | 2019 [71] |
| R | 1, FA: pron/sup | Pressure | Pre-defined assistance levels | 4 | 2019 [130] |
| R | 1, S: abd/add | Pressure | Linear increase of pressure during abduction | 4 | 2019 [131] |
| R | 4, S: flex/ext, E: flex/ext, FA: pron/sup, W: flex/ext | Pressure | Button-triggered manually adjustable setpoint | 5/6 | 2020 [64, 132] |
| I/R | 3, S: flex/ext, E: flex/ext, W: flex/ext both single and dual arm | Force | Action and pose recognition | 6 | 2020 [65, 67] |
| R/A | 1 | Pressure | – | 4 | 2020 [133] |
| R | 1, S: abd/add | - | – | 3 | 2020 [27] |
| Medical | 1, S: abd/add | - | – | 4 | 2020 [134] |
| R | 1, S: elev | Pressure | Manually defined setpoint | 5/6 | 2020 [19] |
S = shoulder, E = elbow, FA = forearm, W = wrist, abd = abduction, add = adduction, flex = flexion, ext = extension, rot = rotation, pron = pronation, sup = supination, dev = deviation, elev = elevation, R = rehabilitation, A = assistance, I = industrial
Table 6.
Overview of the SMA devices.
| Scenario | DOF | Low-level Control | High-level Control | TRL | Year and Related works |
|---|---|---|---|---|---|
| R | 1, W: flex/ext | Position-velocity | – | 3 | 2015 [39] |
| R | 1, E: flex/ext | Position | Pre-defined joint trajectory | 5 | 2017 [40] |
| R | 2, W: flex/ext, ulnar/radial dev | Temperature | – | 4 | 2019 [88] |
| - | 1, E: flex/ext | Position | Pre-defined joint trajectory | 4 | 2019 [41] |
E = elbow, W = wrist, flex = flexion, ext = extension, dev = deviation, R = rehabilitation
Table 7.
Overview of the spring-blades and hybrid devices.
| Scenario | DOF | Low-level Control | High-level Control | TRL | Year and Related works |
|---|---|---|---|---|---|
| R | 2, W: flex/ext, ulnar/radial dev | Motion | Buttons-triggered | 4 | 2018 [42] |
| R | 2, W: flex/ext, radial/ulnar dev | Position | EEG-based attention trigger | 5 | 2019 [72] |
| A | 2, S: flex/ext, E: flex/ext | Position | Reed switches trigger forward and backward driving | 5 | 2015 [46, 47] |
| I | 1, S: elev | Pressure | – | 4 | 2019 [44] |
| R | 2, E: flex/ext, W: flex/ext | Pulse-width (NMES), pressure | EMG trigger | 5/6 | 2020 [45] |
S = shoulder, E = elbow, W = wrist, flex = flexion, ext = extension, dev = deviation, elev = elevation, R = rehabilitation, A= assistance, I = industrial
Fig. 2.
Examples of soft robotic wearable devices for the upper limb: A passive suit for the assistance of the shoulder elevation from [35], B cable-driven suit for the assistance of the elbow flexion-extension from [60], C shape memory alloy (SMA) suit for the assistance of elbows flexion-extension from [41], D cable-driven suit for the assistance of the elbow flexion-extension from [74] E Pneumatic sleeve for the assistance of the elbow flexion-extension from [24], F SMA glove for the assistance of the wrist flexion-extension and ulnar and radial deviation from [88]. All images are under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited (https://creativecommons.org/licenses/by/4.0/).
Application scenario
The first step in the process of designing a device to support limb movements is the definition of the intended application. This is fundamental since it influences all the subsequent design choices: types and number of actuators, materials, intention detection strategy, and controller architecture.
The three possible scenarios we identified in the selected works are: (i) rehabilitation, (ii) assistance with ADLs, (iii) augmentation of healthy subjects in environments such as industry or sport. The majority of devices (81%) are meant for medical applications, either for assistance (32%) or rehabilitation (42%) or both (6%), as shown in Fig. 3A.
Fig. 3.
Results of the electronic search in terms of A intended application scenario of the device, B actuation type, C implemented degrees of freedom, D joints actuated by the device with respect to the actuation type, E technology readiness level with respect to the actuation type, where devices scoring half-levels were grouped with the lowest level, except for category 5/6 which was numerous.
The low number of augmentation devices for healthy subjects, either for industrial (13%) or sport (3%) applications, is probably because soft robots are not the best choice to provide the forces required to carry out arduous work. Indeed, the fact that they rely on the skeletal structure of the wearer to transfer the forces prevents them to apply high torques. Moreover, their intrinsic compliance does not guarantee precision in trajectory tracking. On the other hand, the compliance of such devices is the key feature to guarantee comfort and safety, thus making them good candidates to provide prolonged assistance.
Actuation
The second step to be accomplished when designing a soft exoskeleton is the choice of the actuators. Each actuation type has its own advantages and disadvantages, thus the selection should be made according to the requirements of the device, possibly based on the application scenario. Moreover, it should be considered that the device is meant to be portable and, therefore, the shape and the weight become critical features. The actuation types we identified in the literature analysis are pneumatic (52%), cable-driven (29%), passive (6%), Shape Memory Alloy (SMA) (6%), spring blades with linear actuators (3%), and hybrid actuation systems (4%), as shown in Fig. 3B.
Despite the characteristics and the pros and cons of the different types of actuators were deeply discussed by Thalman and colleagues [17], we will provide a brief summary hereafter for completeness.
Pneumatic actuation
Pneumatic actuators use compressed air to actuate a system. An example of a pneumatic suit is shown in Fig.2E. They can contract, expand, elongate, and even bend upon inflation. They are compliant and can be placed along the limb to distribute the contact pressure [19–22]. The main disadvantages of pneumatic actuation lie in the low bandwidth and in the non-linearity [23–27]. Moreover, they need compressors and tanks, which impact the portability of the system.
Cable-driven actuation
Cable-driven transmission relies on the use of cables that are wound up on a spool by the action of electric motors. Examples of cable-driven exosuits are shown in Fig. 2E and D. The shortening of the cables produces a positive tension that acts on the anchor points. The use of electric motors brings advantages such as ease of control with respect to other actuators, higher power, and higher bandwidth. Cables are inserted into sheaths (Bowden cables) to reduce friction and protect the wearer. Indeed, cable transmission presents disadvantages in terms of friction and backlash phenomena [28, 29] which must be considered when designing the suit and the control architecture [30–34].
Passive systems
Three types of passive mechanisms were identified among the selected devices: (i) spring and cable transmission [35–37], (ii) locking mechanisms [36], (iii) elastic bands [38]. An example of a passive exosuit is shown in Fig. 2A. The advantage of using passive systems is that they do not require any source of power, thus reducing the weight of the device, solving battery duration issues, and being cost-effective [37]. The disadvantage is that they may only provide either gravity compensation or help to maintain a posture, without being able to adapt to external conditions.
Shape Memory Alloy actuation
Shape Memory Alloys (SMA) can be used in those applications where small and slow movements are required due to their limited stroke and bandwidth [39]. Examples of SMA eoxsuit are shown in Fig. 2C and F. They have a low weight and small dimensions, they are noiseless, and are relatively cheap [40, 41]. However, they present a highly non-linear behavior due to hysteresis and their control depends on room temperature [40].
Spring blades actuation
This type of actuation is based on the use of linear electric motors and elastic metallic strips. The linear motors pull or push the metallic blades which actuate the joint. The actuation unit is placed directly on the limb which needs support [42, 43]. This is advantageous in terms of transmission but increases the weight of the arm, at the expense of portability.
Hybrid actuation
Hybrid systems combine different types of actuators in a single device. One device combines pneumatic actuators and cable-driven transmission [44]. The authors claim that this solution combines the strength and compliance of the pneumatic actuators, with the convenience of the Bowden transmission. In another device, pneumatic actuators and neuromuscular electrical stimulation (NMES) were combined to boost the rehabilitative potential of the device [45]. Finally, one device includes passive springs in an active cable-driven device to reduce the motor power consumption [46, 47]. The authors proved that the passive spring system decreased the motor power consumption by 17.5%.
Actuated joints
The majority of the identified devices actuate only one (56%) or two (28%) DOFs, as shown in Fig. 3C. Few works have actuated more than two DOFs. This may be because a large number of actuators is required to actuate multiple DOFs, which could in turn make the device cumbersome and heavy, while also making the control challenging.
Among the human arm joints, the shoulder is actuated in 45% of the identified devices, the elbow in 51%, the forearm in 10%, and the wrist in 33%. In Fig. 3D, the number of devices actuating each joint with respect to the type of actuation is shown.
With regards to shoulder actuation, it was mainly implemented with pneumatic actuators (58%). The actuation of the elbow is instead equally distributed between pneumatic actuation and cable-driven transmission (43%). The forearm pronation/supination and the wrist movements are mainly supported by pneumatic actuators (70%).
Some research has been undertaken to combine multiple DOFs by exploiting arm kinematic couplings to simplify the design. Choi and colleagues [48] implemented the Dart Throwing Motion for the wrist, whereas Georgarakis and co-workers [49] proposed the coupled elevation and external rotation of the shoulder in the frontal plane. Other combined movements that were implemented are the bat swing assistance for baseball augmentation [50] and the forehand swing assistance for tennis augmentation [51].
Similarly, attempts were conducted to actuate different DOFs in series. Kim and colleagues [52] implemented a locking mechanism, which allows actuating both elbow and shoulder in consecutive phases. Xiloyannis and co-workers [53] developed a modular one-to-many actuator, which allows for the independent control of two elbows with a single actuator.
Design approach
To improve the design phase, some works undertook a “bio-inspired” approach, taking inspiration from the human musculoskeletal structure to design the device.
In the case of cable-driven devices, cable routing can be bio-inspired in the sense that it mimics muscle insertions and tendon positions. Moreover, cable guides can reproduce the function of important skeletal structures. An example is the elbow cable guide, which can be used to mimic the olecranon function, which acts as a lever for the extensor muscle [34, 54]. A different approach used to perform cable routing is the identification of lines of minimal extension to place rigid parts such as cable guides and Bowden sheaths, as was proposed by Lessard et al. [55]. Lines of minimal extension are defined as those where the skin shears less.
Similarly, pneumatic actuators can be placed in the same position as the target muscles in a bio-inspired fashion. Moreover, pneumatic actuators could be shaped to fit the curvature of the arm, as in [20]. In analogy with what can be done for cable-driven systems, pneumatic devices can include mechanisms that mimic the musculoskeletal structure. An example is given by O’Neill and colleagues [14], who mimicked the shoulder cruciate ligament with a four-bar linkage system.
An example of a bio-inspired approach in passive systems is the one proposed by Phan and co-workers [38], who placed the passive elastic bands so as to emulate the ligaments’ structure of the elbow. Bio-inspiration may also apply to the design of the actuator itself. Indeed, a cable-driven compliant tendon sheath actuator based on the Hill muscle-tendon model was designed by Lu and colleagues [56, 57].
In addition to the bio-inspired approaches, other significant design solutions, which are aimed at improving ergonomics and energy-saving, have been proposed in the literature.
Galiana and colleagues [58] used redundant collinear cables to solve misalignment problems and to reduce off-axis torques of the shoulder. They proposed to insert the cables anchor points in such a way to minimize the motor torque required to perform the movement and to minimize the non-targeted joints torques. The goal was to achieve transparency with respect to the non-assisted DOFs, bringing advantages both in terms of energy savings and ergonomics. Another approach to deal with alignment problems has been proposed by Harbauer and colleagues [59]. They secured the cable at the wrist in a loop, so that in case there is a slight offset between the motors or the upper arm is rotated, it can be compensated. This approach also allows an even distribution of forces between both sides of the arm to be achieved.
For what concerns pressure distribution on the limb, Wei and colleagues [60] increased the number of Bowden cables from the minimum necessary to reduce pressure. Samper-Escudero and co-workers [61] proposed an exosuit coupling system based on fibers compliance: the textile pattern was designed to efficiently transmit forces. The coupling transforms the pulling force from the cable into a pushing force over the anterior part of the limb. When the cable tightens, the clamp adheres to the anterior part of the arm, creating a push-force in the area, and the fabric self-adapts to the user’s anatomy.
Park and co-workers [35] were able to decouple the horizontal movement of the shoulder from the vertical movement by using a hook tendon, which is free to move from the anterior to the medial part of the arm. This strategy allows the actuation tendon to only slightly change length when the horizontal movement is performed, so that elevation of the arm can be effectively assisted in any configuration. Moreover, the hook detaches when the applied torque exceeds 10% of the maximum torque required. Something similar was done by Kim and colleagues [52], who introduced a rotating anchor point above the shoulder to allow for passive internal/external rotation of the shoulder.
To relieve compression forces and shear stresses from the shoulder, Gaponov and colleagues [62] and Li and colleagues [34] applied an offset to the shoulder.
To reduce the weight of the air supply in their pneumatic actuated tennis augmentation device, Ogawa and colleagues [51] exploited the weight of the tennis player to supply pressure from a pump placed in his/her shoes.
Intention detection
Among the 69 identified works, only 23 implement an intention detection strategy. In the next paragraphs, the solutions adopted are briefly described. The remaining works either defined a trajectory to be tracked or manually adjusted the support provided by the suit.
Switches, buttons, joysticks
As for electric motors, buttons and/or switches can be used to trigger forward and backward driving of the actuators [42, 46, 47, 51]. The motors are usually actuated at a constant speed and the switches are used to control position. In the case of pneumatic actuators, instead, one button can be employed for inflation and another for deflation [63–65].
Similarly, a joystick [21, 55] can be used to perform position control of the limb. Seth and colleagues [66] implemented a smartphone application to be used as a touch trigger, which initiates flexion and extension at constant torque.
The main drawback of all these approaches lies in the need to use the controlateral arm to trigger the assistance. Therefore, this strategy interferes with the normal execution of ADLs, requires some residual capability of the controlateral arm, and can assist only mono-lateral movements.
An approach that would solve this problem is voice recognition [52]. However, this type of strategy can be used in almost noise-free environments only.
Kinematic and dynamic measurements
If the user is healthy or she/he has residual motor capabilities, it is possible to implement IMU-based torque estimation. The control action can be computed by estimating the torque necessary to compensate for gravity [33, 56, 67, 68] or by implementing a dynamic torque estimator [30], which takes also the dynamics of the arm into account.
IMUs can also be used to trigger assistance when the acceleration signals overcome a threshold [50] or to detect the phase of cyclic movements, such as pushing the wheelchair, and to provide assistance in the appropriate phase [69].
Similarly, it is possible to exploit the signal coming from bending sensors [25].
Another popular approach is mimetic control, or mirror position control [55, 62, 70, 71]. Assuming that one of the two arms is healthy, it is possible to track its movements and reproduce them on the impaired limb thanks to the device. This technique, however, only allows the suit to provide support with bimanual and symmetric tasks.
EEG measurements
To make sure the patient is highly involved in the training, Li et al. [72] implemented assistance triggered by measuring the electroencephalography (EEG) attention level. The amplitude of the wrist movement was pre-determined. Attention levels were calculated according to the EEG band power values.
EMG measurements
In case the subject preserved some residual muscular activity, surface electromyographic (sEMG) signals can be used to trigger the assistance. Different modalities have been implemented. The easiest way to use it is by imposing a threshold that the signal must overcome to trigger assistance. The threshold can be single [45, 48] or double [73]. It is also possible to impose a time-over-threshold parameter which is useful to reject artifacts [24].
EMG signals can be used to estimate the muscle torque [57, 74], thus determining the level of assistance. The advantage of this approach is that the user’s intention is detected before the actual execution of the movement, and therefore the assistance is provided in a timely manner [75]. Moreover, using EMG signals allows the monitoring of the user’s active involvement in the execution of the task, improving rehabilitation outcomes. The main drawback of using such strategies is the need for performing a calibration procedure for each user and each session, due to the replacement of the electrodes.
Lotti and colleagues [32] made a comparison between IMU-based and EMG-based assistance. They concluded that the two strategies show similar performances in terms of position tracking accuracy and muscular effort reduction. However, EMG-based intention detection is capable of adapting when dynamic conditions change, thus making the use of the device more symbiotic with respect to the IMU-based approach.
Validation
To test the efficacy of the device in supporting the user’s motion, validation tests were conducted on most of the identified devices. In particular, 7 devices were tested on subjects with disability (either post-stroke or elderly), 50 devices were tested on healthy subjects, and the remaining were either tested on test benches or on a mannequin. Experiments carried out solely to evaluate the performance of the actuators will not be described. The validation tests identified in this literature review can be grouped into four main categories: i) kinematics evaluation, ii) user’s effort evaluation, iii) comfort and ergonomics evaluations, iv) clinical assessment.
Kinematics evaluation
Concerning kinematics, the main outcome measures are trajectory tracking performance, range of motion (ROM), and movement execution velocity.
Trajectory tracking performance tests are conducted in case the control strategy relies on a reference trajectory to evaluate whether the suit can achieve the reference movement and with which accuracy.
For what regards cable-driven devices, Gaponov and co-workers [62] tested a possible rehabilitation scenario on four healthy subjects in which mirror therapy was delivered. They obtained an angle root mean squared error (RMSE) of 2.12, 3.05, 4.9 for the shoulder flexion, shoulder abduction, and elbow flexion, respectively. Li and colleagues [34] tested their device on healthy subjects and obtained an angle RMSE of 2.3 and of 2.9 for the shoulder movement and the elbow flexion, respectively. Choi and colleagues [48] achieved an angle RMSE lower than 3 for the wrist dart-throwing motion of three healthy subjects. With respect to pneumatic devices, Andrikopoulos and colleagues [76] achieved mean absolute errors of 1.43 and 1.51 for the flexion/extension and radial/ulnar deviation of the wrist, respectively, for one healthy subject.
When the range of motion is tested, this is mainly done in three different conditions: i) without the suit, to understand the natural ROM of the user, ii) with the suit but without assistance, to understand the effects of the suit design, iii) and with the suit and assistance provided, to understand the augmentation properties of the device.
To cite a few examples, Choi and colleagues [48] achieved a ROM higher than 50 for the wrist flexion of one healthy subject. They also proved that their wrist-assistive device did not influence the ROM of non-targeted joints, such as the fingers, obtaining no significant change with respect to the natural ROM. Similarly, Lessard and colleagues [55] proved that their prototype does not significantly influence the ROM of healthy subjects. Koh and co-workers’ elbow sleeve [24], instead, achieved approximately 50% of the active ROM when no contribution was provided by the healthy user.
The velocity of the movement was evaluated by Sakoda and colleagues [50] who achieved an improvement in bat swing speed by 3 km/h in experienced subjects. Similarly, Ogawa and co-workers [51] proved that their suit could significantly improve tennis swing velocity in healthy subjects. Xiloyannis and colleagues [28] instead observed that the use of the exosuit decreases the movement velocity and smoothness in healthy subjects.
User’s effort evaluation
The effort of the user in performing a certain movement is evaluated to test the efficacy of the device in providing support. Typically, sEMG signals are evaluated while performing dynamic or static tasks with different loads, both on targeted and non-targeted muscles. Comparisons are made when performing the task without wearing the device, wearing it but without assistance, and with assistance. Isometric tests are also conducted to assess the effect of the suit on muscle fatigue. Xiloyannis and co-workers provided a nice overview of the results obtained by different research groups in terms of sEMG signal in their recent review article [11]. In general, exosuits prove to be effective in decreasing muscular effort.
Another option to test muscular endurance with and without assistance is explored by Sasaki and co-workers [25] with Mosso’s ergograph, obtaining a clear improvement in muscular endurance for healthy subjects. The measurement of body sway is instead used as an indicator of muscle fatigue by Abe and colleagues [77], whose suit was could suppress body sway by 5% for one healthy subject. The maximum load holding time is exploited by Goppold and colleagues [65] to test the ability of their device to extend it. The maximum holding time was extended by approximately 50%, when support was provided by the suit to six healthy subjects.
An alternative to assess the user’s effort is to estimate the metabolic consumption from the heart rate (HR), as done by Lessard and colleagues [55]. They proved that the suit could reduce the HR increase of subjects with single-arm weakness, when exercising, from 12.4% to 3%. O’Neill and colleagues [19] measured the change in HR of the therapist when delivering stretching exercises with and without the assistance of the suit and obtained a decrease between 3.2% and 8.6%.
Comfort and ergonomics evaluation
Regarding comfort and ergonomics, this is evaluated by measuring contact forces between the limb and the device, as done by Andrikopoulos and colleagues [76] while performing flexion-extension and ulnar-radial deviation of the elbow. The forces generated by the device on the hand and palm did not exceed 2.2 N. Similarly, Xiloyannis and co-workers [78] evaluated the pressure distribution at the human-suit interface of the anchor point achieving peak pressure ranging from 20 to 40kPa.
Other methods of assessing comfort are checking skin redness [19] or providing questionnaires directly to the user for a self-evaluation [65].
Clinical assessment
Only one study [45] evaluated the effect of using a hybrid exosuit, integrating NMES and soft pneumatic muscle, on upper limb motor recovery of a group of 15 stroke survivors. The study showed that a 20-session training significantly improved voluntary motor functions, released muscle spasticity at the elbow, wrist, and fingers, and improved muscular coordination of the entire upper limb.
Technology Readiness Level
As can be observed in Fig. 3E, most of the devices have a TRL of 4 or 5. In particular, 9% of the devices score level 3, 45% score level 4, 30% score level 5, 10% were assigned between level 5 and level 6, 6% score level 6. The majority of pneumatic devices (55%) score level 4, whereas the majority of cable-driven devices (33%) score level 5.
Level 3 means that the experimental proof of concept or the prototype has been built but not tested. Level 4 means that the prototype has been tested in the laboratory on a mannequin. Level 5 means that the prototype is mature in terms of design and control and has been tested on healthy subjects. Level 6 means that the prototype has been tested for its efficacy on subjects with motor disabilities or healthy subjects according to the intended scenario. Level 7 means that the system has been tested for its intended purpose in the clinic, at home, in the factory, or in sports fields.
Few devices reached maturity, in terms of design, control, and safety, for being tested on end-users (level 6).
Among the 9 devices with the highest TRL (5/6-7), only three actuate more than 2 DOFs. The first one is a cable-driven device developed by Lessard and co-workers [79], it actuates 6 DOFs and was tested in a clinical environment on 9 subjects with upper limb impairment. However, it only supports symmetric tasks, since it relies on a mimetic control strategy. The second one, a pneumatic exosuit, was developed by Das and co-workers [64]. It supports 4 DOFs but, at the current state, it is not portable and the support is changed by employing a potentiometer, which makes the support not dynamic. The third one, a pneumatically actuated exosuit, was designed by Goppold and colleagues [65]. It actuates 3 DOFs and automatically recognizes the action and the pose of the user. However, some critical aspects were found to be the high weight (6.5 kg) and the low intuitiveness of the device to be worn and used.
The exosuit designed by Samper-Escudero and co-workers [61], supports 2 DOFs (shoulder elevation and elbow flexion) but relies on pre-determined joint trajectories. The device developed by Xiloyannis and colleagues [28, 74] instead was used with a variety of intuitive controllers that do not require the user’s input (EMG-based torque estimation or IMU-based gravity compensation) but only supports the elbow. Similarly, the exosuit developed by Hosseini and colleagues [73] implements an EMG-based controller, but only supports bimanual lifting. Another exosuit meant for industrial work, developed by Kim and co-workers [52], supports bimanual lifting, with shoulder elevation and elbow flexion coupled, with the assistance activated via voice recognition.
Finally, O’Neill and colleagues [19] developed a pneumatic exosuit to support the patient’s arm against gravity so as to relieve the therapist’s burden during the exercise. However, the support level is manually adjusted according to the user’s and therapist’s needs.
Discussion
The results of this review show that research in the field of upper limb soft devices has been quite active in the last two decades. The main applications for which they have been developed are related to the assistance of fragile people, either for rehabilitation, or assistance, or both. Cable-driven transmission and soft pneumatic actuators are the most common choices for the actuation unit.
In particular, pneumatic actuators seem to be the preferred choice to actuate the shoulder. This may be because to actuate the shoulder one must deal with the whole weight of the arm. Indeed, they may be placed below the arm and inflated to push the arm, evenly distributing contact pressure. The use of cable-driven transmission might be sub-optimal since it could result in pressure peaks around the anchor points. Spring blades and SMA may not be indicated due to the relatively limited stroke they are capable of, making them more suitable for supporting wrist movements.
Nevertheless, research on soft pneumatic actuated devices is still mainly focused on the development of the actuators themselves, whereas cable-driven devices can be considered more advanced in terms of control strategies and intention detection.
The assistance of the elbow joint is the most explored, followed by the shoulder and the wrist. Few works have implemented more than 2 DOFs, due to the complexity of the control. Those who have, indeed, either do not implement advanced controllers, including intention-detection strategies appropriate for the intended scenario, or did not test a great variety of movements.
Regarding design solutions, even though many attempts were conducted to improve ergonomics and energy saving, we believe there is still scope for improvement. Effort should be put into designing the suit to optimize pressure distribution and joint reaction forces. Simulation software, such as OpenSim (SimTK) [80, 81], could be a useful resource in this view. Moreover, few works have achieved real portability at the latest iteration.
A common problem in soft devices is the inability to apply high forces because of the deformability of the soft materials and the fact that the device relies on the skeletal structure of the user. Optimization of the comfort and ergonomics should go in parallel with the improvements in force transmission. Research should also be devoted to making the devices adaptable to different users according to the their physical characteristics.
We believe that the integration of passive systems such as springs, clutches, and brakes in active devices could be beneficial in the decrease of energy consumption and weight of the device. Although only preliminary results were found in this review, this suggestion can be supported by literature on upper limb stiff exoskeletons that include passive elements in their design [9, 82, 83].
Hybrid actuation should be better explored as well, since it may allow the combination of the benefits of different actuation types, also according to the different joints to be supported. This might apply, in particular, to NMES hybrid devices. Indeed, NMES used in combination with rigid exoskeletons has proven to bring beneficial effects in upper-limb rehabilitation [84, 85]. We believe that, starting from the work of Nam and colleagues [45], this approach should be investigated with soft robotic suits as well.
Few prototypes implement intention detection strategies, which make the device effectively cooperate with the user. This, however, is a fundamental aspect of a device for motion support, especially if it is meant to assist with ADLs or arduous work. The development of effective intention detection strategies, which do not require long calibration procedures, and which are able to adapt to different dynamic conditions, is fundamental in view of the development and diffusion of soft devices for the upper limb, whose movements are various and hardly predictable.
Many works tested the device at a preliminary stage (actuation characterization), but few tests were conducted to assess the efficacy of the support. Experiments were conducted mainly to evaluate the accuracy of the device in tracking a certain trajectory, achieving full range of motion, and being effective in decreasing muscle effort when worn. However, proposed experimental protocols are various and differ from each other so that comparison among different works is difficult.
Few research groups tested their devices on end-users and performed a complete meaningful clinical assessment. For the rehabilitation scenario, in the future, other metrics commonly used for the evaluation of upper limb robotic devices such as movement time, hand-path ratio, and inter-joint correlation, should be included [86, 87]. In the assistance scenario, externally-assessed functional scales, such as the Performance of the Upper Limb-PUL-module, self-perceived scales, such as the Abilhand questionnaire, and usability scales, such as the System Usability Scale should be used to assess the effectiveness and usability of the device [3].
In this view, carefully designed pilot clinical trials should be conducted to prove the effectiveness of such devices to provide support to the wearer. The lack of clinical trials has also prevented to identify a precise target population.
It is worth noticing that most cable-driven devices score level 5, whereas most pneumatic devices score level 4. This suggests that cable-driven devices are more technologically advanced with respect to pneumatic ones. Moreover, the devices showing the highest TRL, either support only one DOF or implement control strategies that make them unsuitable for daily assistance with different activities (e.g. predefined trajectories, mimetic control, manual support adjustment, voice control). In the future, we would expect more suits to reach levels 6 and 7 and finally be ready for commercialization. Clinical trials will be also mandatory to prove that the devices meet the safety, health, and environmental protection requirements needed to reach the market.
Conclusion
In conclusion, we confirm that soft exoskeletons might show a very high potential despite none of the analyzed devices having reached the market yet. We could infer that there is a lack of soft devices implementing multiple DOFs with appropriate control strategies including intention detection. The movements supported by the prototypes are few and do not include a great variety of actions that would allow the user to perform daily life activities. Ergonomics, user experience, and portability should be further explored in future studies, as well as the design of devices that support multiple DOFs. Finally, clinical trials are needed to assess the effectiveness of upper limb exosuits and to identify the category of subjects who can benefit the most from these types of devices.
Overall, we think that the development of soft wearable devices for the support of daily life activities of the upper limbs is a promising and growing research field for which we have great hopes in the next years.
Abbreviations
- ADL
Ativities of daily living
- DOF
Degree of freedom
- EEG
Electroencephalography
- HR
Heart rate
- IMU
Inertial measurement unit
- RMSE
Root mean square error
- ROM
Range of motion
- sEMG
Surface electromyography
- SMA
Shape memory alloy
- TRL
Technology readiness level
- NMES
Neuromuscular electrical stimulation
Author contributions
EB performed data collection and the review of papers, processed the data, and drafted the manuscript. EA and MG conceived the study, supervised the project, contributed to the paper selection process, provided guidance for the structure of the review and made critical revisions to the manuscript. AP, FB and FR supervised the work, and made critical revisions to the manuscript. All authors read and approved the final manuscript.
Funding
This work was not funded by any organization.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Declarations
Competing interests
The authors declare that Marta Gandolla, Francesco Braghin and Alessandra Pedrocchi hold shares of Agade SRL.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Elena Bardi, Email: elena.bardi@polimi.it.
Marta Gandolla, Email: marta.gandolla@polimi.it.
Francesco Braghin, Email: francesco.braghin@polimi.it.
Ferruccio Resta, Email: ferruccio.resta@polimi.it.
Alessandra L. G. Pedrocchi, Email: alessandra.pedrocchi@polimi.it
Emilia Ambrosini, Email: emilia.ambrosini@polimi.it.
References
- 1.Faria-Fortini I, Michaelsen SM, Cassiano JG, Teixeira-Salmela LF. Upper extremity function in stroke subjects: relationships between the international classification of functioning, disability, and health domains. J Hand Ther. 2011;24(3):257–265. doi: 10.1016/j.jht.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Janssen MMHP, Bergsma A, Geurts ACH, De Groot IJM. Patterns of decline in upper limb function of boys and men with DMD: an international survey. J Neurol. 2014;261(7):1269–1288. doi: 10.1007/s00415-014-7316-9. [DOI] [PubMed] [Google Scholar]
- 3.Longatelli V, Antonietti A, Biffi E, Diella E, D’Angelo MG, Rossini M, et al. User-centred assistive SystEm for arm Functions in neUromuscuLar subjects (USEFUL): a randomized controlled study. J Neuroeng Rehabil. 2021;18(1):1–17. doi: 10.1186/s12984-020-00794-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perry JC, Rosen J, Burns S. Upper-limb powered exoskeleton design. IEEE/ASME Trans Mechatron. 2007;12(4):408–417. doi: 10.1109/TMECH.2007.901934. [DOI] [Google Scholar]
- 5.Gassert R, Dietz V. Rehabilitation robots for the treatment of sensorimotor deficits: a neurophysiological perspective. J Neuroeng Rehabil. 2018;15(1):1–15. doi: 10.1186/s12984-018-0383-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krebs HI, Volpe BT. Rehabilitation robotics. 1. Amsterdam: Elsevier B.V.; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weber LM, Stein J. The use of robots in stroke rehabilitation: a narrative review. NeuroRehabilitation. 2018;43(1):99–110. doi: 10.3233/NRE-172408. [DOI] [PubMed] [Google Scholar]
- 8.Kapsalyamov A, Hussain S, Jamwal PK. State-of-the-art assistive powered upper limb exoskeletons for elderly. IEEE Access. 2020;8:178991–179001. doi: 10.1109/ACCESS.2020.3026641. [DOI] [Google Scholar]
- 9.Gandolla M, Dalla Gasperina S, Longatelli V, Manti A, Aquilante L, D’Angelo MG, et al. An assistive upper-limb exoskeleton controlled by multi-modal interfaces for severely impaired patients: development and experimental assessment. Rob Auton Syst. 2021;143:103822. doi: 10.1016/j.robot.2021.103822. [DOI] [Google Scholar]
- 10.Bogue R. Exoskeletons - a review of industrial applications. Ind Rob. 2018;45(5):585–590. doi: 10.1108/IR-05-2018-0109. [DOI] [Google Scholar]
- 11.Xiloyannis M, Alicea R, Georgarakis AM, Haufe FL, Wolf P, Masia L, et al. Soft robotic exosuits: state of the art, core technologies and open challenges. IEEE Trans Robot. 2021 doi: 10.1109/TRO.2021.3084466. [DOI] [Google Scholar]
- 12.Gorgey AS. Robotic exoskeletons: the current pros and cons. World J Orthop. 2018;9(9):112–119. doi: 10.5312/wjo.v9.i9.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asbeck AT, Rossi SMMD, Galiana I, Ding Y, Walsh CJ. Stronger, smarter, softer: next-generation wearable robots. IEEE Robot Autom Mag. 2014 doi: 10.1109/MRA.2014.2360283. [DOI] [Google Scholar]
- 14.O’Neill CT, Phipps NS, Cappello L, Paganoni S, Walsh CJA. soft wearable robot for the shoulder: design, characterization, and preliminary testing. IEEE Int Conf Rehabil Robot. 2017;2017:1672–8. doi: 10.1109/ICORR.2017.8009488. [DOI] [PubMed] [Google Scholar]
- 15.Natividad RF, Yeow CH. Development of a soft robotic shoulder assistive device for shoulder abduction. In: 6th IEEE RAS EMBS International Conference on Biomedical Robotics and Biomechatronics. IEEE; 2016:989–993.
- 16.Jarrassé N, Proietti T, Crocher V, Robertson O, Sahbani A, Morel G, et al. Robotic exoskeletons: a perspective for the rehabilitation of arm coordination in stroke patients. Front Hum Neurosci. 2014;8:1–13. doi: 10.3389/fnhum.2014.00947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thalman C, Artemiadis P. A review of soft wearable robots that provide active assistance: trends, common actuation methods, fabrication, and applications. Wearable Technol. 2020;1:1–27. doi: 10.1017/wtc.2020.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chu CY, Patterson RM. Soft robotic devices for hand rehabilitation and assistance: a narrative review. J Neuroeng Rehabil. 2018;15:1–14. doi: 10.1186/s12984-018-0350-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Neill C, Proietti T, Nuckols K, Clarke ME, Hohimer CJ, Cloutier A, et al. Inflatable soft wearable robot for reducing therapist fatigue during upper extremity rehabilitation in severe stroke. IEEE Robot Autom Lett. 2020;5(3):3899–3906. doi: 10.1109/LRA.2020.2982861. [DOI] [Google Scholar]
- 20.Thalman CM, Lam QP, Nguyen PH, Sridar S, Novel Polygerinos PA. Exosuit soft elbow, to supplement bicep lifting capacity. IEEE/RJS Int Conf Intell Robot Syst. 2018;2018:6965–71. [Google Scholar]
- 21.Arellano FJL, Roquemore B, Gandhi S, Maruyama T, Patil D, Polygerinos P. Soft wearable deltoid assistive device. In: Proceedings 2019 esign of Medical Devices Conference Minneapolis, Minnesota, USA; 2019:1–4.
- 22.Oguntosin V, Harwin WS, Kawamura S, Nasuto SJ, Hayashi Y. Development of a wearable assistive soft robotic device for elbow rehabilitation. IEEE Int Conf Rehabil Robot. 2015;2015:747–752. [Google Scholar]
- 23.Irshaidat M, Soufian M, Al-Ibadi A, Nefti-Meziani SA. novel elbow pneumatic muscle actuator for exoskeleton arm in post-stroke rehabilitation. IEEE Int Conf Soft Robot. 2019;2019:630–5. [Google Scholar]
- 24.Koh TH, Cheng N, Yap HK, Yeow CH. Design of a soft robotic elbow sleeve with passive and intent-controlled actuation. Front Neurosci. 2017;11:1–12. doi: 10.3389/fnins.2017.00597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sasaki D, Noritsugu T, Takaiwa M. Development of active support splint driven by pneumatic soft actuator (ASSIST) Proc 2005 IEEE Int Conf Robot Autom. 2005 doi: 10.1109/ROBOT.2005.1570171. [DOI] [Google Scholar]
- 26.Belforte G, Eula G, Ivanov A, Raparelli T, Sirolli S. Presentation of textile pneumatic muscle prototypes applied in an upper limb active suit experimental model. J Text Inst. 2018;109(6):757–766. doi: 10.1080/00405000.2017.1368111. [DOI] [Google Scholar]
- 27.Tschiersky M, Hekman EEG, Brouwer DM, Herder JL, Suzumori K. A compact mckibben muscle based bending actuator for close-to-body application in assistive wearable robots. IEEE Robot Autom Lett. 2020;5(2):3042–3049. doi: 10.1109/LRA.2020.2975732. [DOI] [Google Scholar]
- 28.Xiloyannis M, Chiaradia D, Frisoli A, Masia L. Physiological and kinematic effects of a soft exosuit on arm movements. J Neuroeng Rehabil. 2019;16(1):1–15. doi: 10.1186/s12984-019-0495-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cappello L, Binh DK, Yen SC, Masia L. Design and preliminary characterization of a soft wearable exoskeleton for upper limb. Proc IEEE RAS EMBS Int Conf Biomed Robot Biomechatron. 2016;2016:623–630. [Google Scholar]
- 30.Dinh BK, Xiloyannis M, Antuvan CW, Cappello L, Masia L. Hierarchical cascade controller for assistance modulation in a soft wearable arm exoskeleton. IEEE Robot Autom Lett. 2017;2(3):1786–1793. doi: 10.1109/LRA.2017.2668473. [DOI] [Google Scholar]
- 31.Dinh BK, Xiloyannis M, Cappello L, Antuvan CW, Yen SC, Masia L. Adaptive backlash compensation in upper limb soft wearable exoskeletons. Rob Auton Syst. 2017;92:173–186. doi: 10.1016/j.robot.2017.03.012. [DOI] [Google Scholar]
- 32.Lotti N, Xiloyannis M, Missiroli F, Chiaradia D, Frisoli A, Sanguineti V. Intention-detection strategies for upper limb exosuits: model-based myoelectric vs dynamic-based control. 8th IEEE Int Conf Biomed Robot Biomechatron. 2020;2020:410–5. [Google Scholar]
- 33.Georgarakis AM, Song J, Wolf P, Riener R, Xiloyannis M. Control for gravity compensation in tendon-driven upper limb exosuits. Proc IEEE RAS EMBS Int Conf Biomed Robot Biomechatron. 2020;2020:340–345. [Google Scholar]
- 34.Li M, Guo W, Xu G, Jia Y, Xie J, Zhang X. A Tendon-driven upper-limb rehabilitation robot. In: 2018 15th International Conference Ubiquitous Robot. Hawaii Convention Center, Hawai’i, USA,: IEEE; 2018;303–308.
- 35.Park D, Cho KJ. Development and evaluation of a soft wearable weight support device for reducing muscle fatigue on shoulder. PLoS One. 2017;12(3):1–24. doi: 10.1371/journal.pone.0173730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang Y, Arakelian V. Design of a passive robotic exosuit for carrying heavy loads. IEEE-RAS Int Conf Humanoid Robot. 2018;2018:860–5. [Google Scholar]
- 37.Asgari M, Hall PT, Moore BS, Crouch DL. Wearable shoulder exoskeleton with spring-cam mechanism for customizable, nonlinear gravity compensation. Proc Annu Int Conf IEEE Eng Med Biol Soc EMBS. 2020;2020:4926–4929. doi: 10.1109/EMBC44109.2020.9175633. [DOI] [PubMed] [Google Scholar]
- 38.Phan TQ, Nguyen H, Vermillion B, Lee SW. Passive elbow movement assistant (PEMA): a portable exoskeleton to compensate angle-dependent tone profile of the elbow joint post-stroke. 2019 IEEE 16th Int Conf Rehabil Robot. 2019;2019:1209–1214. doi: 10.1109/ICORR.2019.8779365. [DOI] [PubMed] [Google Scholar]
- 39.Villoslada A, Flores A, Copaci D, Blanco D, Moreno L. High-displacement flexible Shape Memory Alloy actuator for soft wearable robots. Rob Auton Syst. 2015;73:91–101. doi: 10.1016/j.robot.2014.09.026. [DOI] [Google Scholar]
- 40.Copaci D, Cano E, Moreno L, Blanco D. New design of a soft robotics wearable elbow exoskeleton based on shape memory alloy wire actuators. Appl Bionics Biomech. 2017;2017:1–11. doi: 10.1155/2017/1605101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park SJ, Park CH. Suit-type wearable robot powered by shape-memory-alloy-based fabric muscle. Sci Rep. 2019;9(1):1–8. doi: 10.1038/s41598-018-37186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Higuma T, Kiguchi K, Arata J. Low-profile two-degree-of-freedom wrist exoskeleton device using multiple spring blades. IEEE Robot Autom Lett. 2018;3(1):305–311. doi: 10.1109/LRA.2017.2739802. [DOI] [Google Scholar]
- 43.Li N, Yu P, Yang T, Zhao L, Liu Z, Xi N, et al. Bio-inspired wearable soft upper-limb exoskeleton robot for stroke survivors. 2017 IEEE Int Conf Robot Biomimetics ROBIO. 2017;2018:2693–2698. doi: 10.1109/ROBIO.2017.8324826. [DOI] [Google Scholar]
- 44.Thompson N, Sinha A, Krishnan G. Characterizing architectures of soft pneumatic actuators for a cable-driven shoulder exoskeleton. IEEE Int Conf Robot Autom. 2019;2019:570–6. [Google Scholar]
- 45.Nam C, Rong W, Li W, Cheung C, Ngai W, Cheung T, et al. An exoneuromusculoskeleton for self-help upper limb rehabilitation after stroke. Soft Robot. 2020;00(00):1–22. doi: 10.1089/soro.2020.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koo I, Yun C, Costa MVO, Scognamiglio JVF, Yangali TA, Park D, et al. Development of a meal assistive exoskeleton made of soft materials for polymyositis patients. IEEE/RSJ Int Conf Intell Robot Syst (IROS) 2014;2014:542–547. [Google Scholar]
- 47.Park D, Koo I, Cho KJ. Evaluation of an improved soft meal assistive exoskeleton with an adjustable weight-bearing system for people with disability. IEEE Int Conf Rehabil Robot. 2015;2015:79–84. [Google Scholar]
- 48.Choi H, Kang BB, Jung BK, Cho KJ. Exo-Wrist: a soft tendon-driven wrist-wearable robot with active anchor for dart-throwing motion in hemiplegic patients. IEEE Robot Autom Lett. 2019;4(4):4499–4506. doi: 10.1109/LRA.2019.2931607. [DOI] [Google Scholar]
- 49.Georgarakis AM, Wolf P, Riener R. Simplifying exosuits: kinematic couplings in the upper extremity during daily living tasks. IEEE International Conference on Rehabilitation Robotics Toronto, Canada: IEEE; 2019;423–428. [DOI] [PubMed]
- 50.Sakoda W, Ramirez AV, Ogawa K, Tsuji T, Kurita Y. Reinforced suit using low pressure driven artificial muscles for baseball bat swing. ACM Int Conf Proc Ser. 2018 doi: 10.1145/3174910.3174932. [DOI] [Google Scholar]
- 51.Ogawa K, Ikeda T, Unplugged Kurita Y. Suit Powered Suit powered, for superhuman tennis. 10th Fr 12th Eur Congr Mechatron. 2018;2018:361–4. [Google Scholar]
- 52.Kim YG, Little K, Noronha B, Xiloyannis M, Masia L, Accoto D. A voice activated bi-articular exosuit for upper limb assistance during lifting tasks. Robot Comput Integr Manuf. 2020;66:1–9. doi: 10.1016/j.rcim.2020.101995. [DOI] [Google Scholar]
- 53.Xiloyannis M, Annese E, Canesi M, Kodiyan A, Bicchi A, Micera S, et al. Design and validation of a modular one-to-many actuator for a soft wearable exosuit. Front Neurorobot. 2019;13(June):1–14. doi: 10.3389/fnbot.2019.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nycz CJ, Delph MA, Modeling Fischer GS. design of a tendon actuated soft robotic exoskeleton for hemiparetic upper limb rehabilitation. 37th Annu In Conf IEEE Eng Med Biol Soc. 2015;2015:3889–92. doi: 10.1109/EMBC.2015.7319243. [DOI] [PubMed] [Google Scholar]
- 55.Lessard S, Pansodtee P, Robbins A, Trombadore JM, Kurniawan S, Teodorescu M. A Soft Exosuit for Flexible Upper-Extremity Rehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2018;26(8):1604–1617. doi: 10.1109/TNSRE.2018.2854219. [DOI] [PubMed] [Google Scholar]
- 56.Wu Q, Chen B, Wu H. Neural-network-enhanced torque estimation control of a soft wearable exoskeleton for elbow assistance. Mechatronics. 2019;63(March):102279. doi: 10.1016/j.mechatronics.2019.102279. [DOI] [Google Scholar]
- 57.Lu L, Wu Q, Chen X, Shao Z, Chen B, Wu H. Development of a sEMG-based torque estimation control strategy for a soft elbow exoskeleton. Rob Auton Syst. 2019;111:88–98. doi: 10.1016/j.robot.2018.10.017. [DOI] [Google Scholar]
- 58.Galiana I, Hammond FL, Howe RD, Popovic MB. Wearable soft robotic device for post-stroke shoulder rehabilitation: identifying misalignments. In: ms Vilamoura, Algarve, Portugal: IEEE; 2012; 317–322.
- 59.Harbauer CM, Fleischer M, Nguyen T, Bos F, Bengler K. Too close to comfort? A new approach of designing a soft cable-driven exoskeleton for lifting tasks under ergonomic aspects. 2020 3rd Int Conf Intell Robot Control Eng. 2020 doi: 10.1109/IRCE50905.2020.9199238. [DOI] [Google Scholar]
- 60.Wei W, Qu Z, Wang W, Zhang P, Hao F. Design on the bowden cable-driven upper limb soft exoskeleton. Appl Bionics Biomech. 2018;2018:1–9. doi: 10.1155/2018/1925694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Samper-Escudero JL, Gimenez-Fernandez A, Sanchez-Uran MA, Ferre M. A cable-driven exosuit for upper limb flexion based on fibres compliance. IEEE Access. 2020;8:153297–153310. doi: 10.1109/ACCESS.2020.3018418. [DOI] [Google Scholar]
- 62.Gaponov I, Popov D, Lee SJ, Ryu JH. Auxilio: A portable cable-driven exosuit for upper extremity assistance. Int J Control Autom Syst. 2016;15(1):73–84. doi: 10.1007/s12555-016-0487-7. [DOI] [Google Scholar]
- 63.Li B, Greenspan B, Mascitelli T, Raccuglia M, Denner K, Duda R, et al. Design of the Playskin Air: a user-controlled, soft pneumatic exoskeleton. In: Proceeding 2019 Design Of Medical Devices Conference ASME; 2019;1–4.
- 64.Das S, Kurita Y. ForceArm: a wearable pneumatic gel muscle (PGM)-based assistive suit for the upper limb. IEEE Trans Med Robot Bionics. 2020;2(2):269–281. doi: 10.1109/TMRB.2020.2990436. [DOI] [Google Scholar]
- 65.Goppold JP, Kuschan J, Thiele G, Schmidt H, Krüger J, Hackbart R, et al. PowerGrasp - Design and evaluation of a modular soft-robotic arm exosuit for industrial applications. 52nd Int Symp Robot. 2020;2020:107–114. [Google Scholar]
- 66.Seth D, Vardhan Varma VKH, Anirudh P, Kalyan P. Preliminary design of soft exo-suit for arm rehabilitation. In: HCII 2019 Digital Human Modeling and Applications in Health, Safety, Ergonomics and Risk Management. Springer International Publishing; 2019:284–294.
- 67.Kuschan J, Goppold JP, Schmidt H, Krüger J. Powergrasp: concept for a novel soft-robotic arm support system. 50th Int Symp Robot. 2018;2018:269–274. [Google Scholar]
- 68.Little K, Antuvan CW, Xiloyannis M, De Noronha B, Kim YG, Masia L, et al. IMU-based assistance modulation in upper limb soft wearable exosuits. IEEE 16th Int Conf Rehabil Robot. 2019 doi: 10.1109/ICORR.2019.8779362. [DOI] [PubMed] [Google Scholar]
- 69.Sridar S, Narasimha RG, Gadagi AM, Taduru V, Strzelczyk C, Maruyama T. Soft Robotic Shoulder Assist Device - Towards Prevention Of Shoulder Overuse Syndrome In Wheelchair Users. Proceedings 2018 Design of Medical Devices Conference, Minneapolis, Minnesota, USA.: ASME; 2018;1–3.
- 70.Gobee S, Durairajah V, Mugilan G. Design and development of upper limb soft exoskeleton for rehabilitation. In: 2nd International Conference for Innovation in Biomedical Engineering and Life Science IFMBE Proceedings vol. 67. Singapore: Springer; 2018; 111–116.
- 71.Vega Ramirez A, Kurita Y. A soft exoskeleton jacket with pneumatic gel muscles for human motion interaction. In: Universal Access in Human-Computer Interaction Multimodality Assistant Environment. Springer International Publishing; 2019;587–603.
- 72.Li M, Liang Z, He B, Zhao CG, Yao W, Xu G, et al. Attention-controlled assistive wrist rehabilitation using a low-cost EEG sensor. IEEE Sens J. 2019;19(15):6497–6507. doi: 10.1109/JSEN.2019.2910318. [DOI] [Google Scholar]
- 73.Hosseini M, Meattini R, San-Millan A, Palli G, Melchiorri C, Paik J. A sEMG-driven soft exosuit based on twisted string actuators for elbow assistive applications. IEEE Robot Autom Lett. 2020;5(3):4094–4101. doi: 10.1109/LRA.2020.2988152. [DOI] [Google Scholar]
- 74.Missiroli F, Lotti N, Xiloyannis M, Sloot LH, Riener R, Masia L. Relationship between muscular activity and assistance magnitude for a myoelectric model based controlled exosuit. Front Robot AI. 2020;7(December):1–13. doi: 10.3389/frobt.2020.595844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gandolla M, Ferrante S, Ferrigno G, Baldassini D, Molteni F, Guanziroli E, et al. Artificial neural network EMG classifier for functional hand grasp movements prediction. J Int Med Res. 2017;45(6):1831–1847. doi: 10.1177/0300060516656689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Andrikopoulos G, Nikolakopoulos G, Manesis S. Motion control of a novel robotic wrist exoskeleton via pneumatic muscle actuators. In: IEEE International Conference on Emerging Technologies and Factory IEEE; 2015;1–8.
- 77.Abe T, Koizumi S, Nabae H, Endo G, Suzumori K. Muscle textile to implement soft suit to shift balancing posture of the body. IEEE Int Conf Soft Robot RoboSoft 2018. 2018;2018:572–8.
- 78.Xiloyannis M, Chiaradia D, Frisoli A, Masia L. Characterisation of pressure distribution at the interface of a soft exosuit: towards a more comfortable wear. In: Carrozza MC, Micera S, Pons JL, editors. Wearable robotics: challenges and trends. Cham: Springer International Publishing; 2019. pp. 35–38. [Google Scholar]
- 79.Lessard S, Pansodtee P, Robbins A, Baltaxe-Admony LB, Trombadore JM, Teodorescu M. CRUX: A compliant robotic upper-extremity exosuit for lightweight, portable, multi-joint muscular augmentation. Int Conf Rehabil Robot. 2017;2017:1633–8. doi: 10.1109/ICORR.2017.8009482. [DOI] [PubMed] [Google Scholar]
- 80.Delp SL, Anderson FC, Arnold AS, Loan P, Habib A, John CT, et al. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Trans Biomed Eng. 2007;54(11):1940–1950. doi: 10.1109/TBME.2007.901024. [DOI] [PubMed] [Google Scholar]
- 81.Seth A, Hicks JL, Uchida TK, Habib A, Dembia CL, Dunne JJ, et al. OpenSim: Simulating musculoskeletal dynamics and neuromuscular control to study human and animal movement. Plos Comput Biol. 2018 doi: 10.1371/journal.pcbi.1006223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bilancia P, Berselli G. Conceptual design and virtual prototyping of a wearable upper limb exoskeleton for assisted operations. Int J Interact Des Manuf. 2021;15(4):525–539. doi: 10.1007/s12008-021-00779-9. [DOI] [Google Scholar]
- 83.Kaneishi D, Matthew RP, Tomizuka M. Active/passive switching control framework for assistive devices with variable stiffness actuator. In: Proceedings of American Control Conference Philadelphia, PA; 2019;5240–5246.
- 84.Ambrosini E, Ferrante S, Zajc J, Bulgheroni M, Baccinelli W, D’Amico E, et al. The combined action of a passive exoskeleton and an EMG-controlled neuroprosthesis for upper limb stroke rehabilitation: first results of the RETRAINER project. IEEE Int Conf Rehabil Robot. 2017 doi: 10.1109/ICORR.2017.8009221. [DOI] [PubMed] [Google Scholar]
- 85.Ambrosini E, Gasperini G, Zajc J, Immick N, Augsten A, Rossini M, et al. A robotic system with emg-triggered functional eletrical stimulation for restoring arm functions in stroke survivors. Neurorehabil Neural Repair. 2021;35(4):334–345. doi: 10.1177/1545968321997769. [DOI] [PubMed] [Google Scholar]
- 86.De Los Reyes-Guzmán A, Dimbwadyo-Terrer I, Trincado-Alonso F, Monasterio-Huelin F, Torricelli D, Gil-Agudo A. Quantitative assessment based on kinematic measures of functional impairments during upper extremity movements: A review. Clin Biomech. 2014;29(7):719–727. doi: 10.1016/j.clinbiomech.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 87.Nordin N, Xie SQ, Wünsche B. Assessment of movement quality in robot- assisted upper limb rehabilitation after stroke: a review. J Neuroeng Rehabil. 2014 doi: 10.1186/1743-0003-11-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jeong J, Yasir IB, Han J, Park CH, Bok SK, Kyung KU. Design of shape memory alloy-based soft wearable robot for assistingwrist motion. Appl Sci. 2019 doi: 10.3390/app9194025. [DOI] [Google Scholar]
- 89.Kesner SB, Jentoft L, Hammond FL, Howe RD, Popovic M. Design considerations for an active soft orthotic system for shoulder rehabilitation. Annu Int Conf IEEE Eng Med Biol Soc. 2011 doi: 10.1109/IEMBS.2011.6092006. [DOI] [PubMed] [Google Scholar]
- 90.Li N, Yang T, Yu P, Chang J, Zhao L, Zhao X, et al. Bio-inspired upper limb soft exoskeleton to reduce stroke-induced complications. Bioinspir Biomim. 2018;13:1–20. doi: 10.1088/1748-3190/aad8d4. [DOI] [PubMed] [Google Scholar]
- 91.Elor A, Lessard S, Teodorescu M, Kurniawan S. Project butterfly: Synergizing immersive virtual reality with actuated soft exosuit for upper-extremity rehabilitation. In: IEEE Conference on Virtual Reality and 3D User Interfaces, VR 2019. Osaka. Japan. 2019;2019:1448–56.
- 92.Ismail R, Ariyanto M, Perkasa IA, Adirianto R, Putri FT, Glowacz A, et al. Soft elbow exoskeleton for upper limb assistance incorporating dual motor-tendon actuator. Electron. 2019;8(1–20):1184. doi: 10.3390/electronics8101184. [DOI] [Google Scholar]
- 93.Pont D, Contreras AF, Samper JL, Saez FJ, Ferre M, Sanchez MA, et al. ExoFlex: an upper-limb cable-driven exosuit. Robot 2019 Fourth Iber Robot Conf Adv Intell Syst Comput. 2020 doi: 10.1007/978-3-030-36150-1_34. [DOI] [Google Scholar]
- 94.Wu Q, Wang X, Chen B, Wu H. Design and fuzzy sliding mode admittance control of a soft wearable exoskeleton for elbow rehabilitation. IEEE Access. 2018;6:60249–60263. doi: 10.1109/ACCESS.2018.2875550. [DOI] [Google Scholar]
- 95.Cappello L, Pirrera A, Weaver P, Masia L. A series elastic composite actuator for soft arm exosuits. IEEE Int Conf Rehabil Robot. 2015 doi: 10.1109/ICORR.2015.7281176. [DOI] [Google Scholar]
- 96.Canesi M, Xiloyannis M, Ajoudani A, Biechi A, Masia L. Modular one-to-many clutchable actuator for a soft elbow exosuit. IEEE Int Conf Rehabil Robot. 2017 doi: 10.1109/ICORR.2017.8009489. [DOI] [PubMed] [Google Scholar]
- 97.Chiaradia D, Xiloyannis M, Antuvan CW, Frisoli A, Masia L. Design and embedded control of a soft elbow exosuit. 2018 IEEE Int Conf Soft Robot. 2018;2018:565–571. doi: 10.1109/ROBOSOFT.2018.8405386. [DOI] [Google Scholar]
- 98.Dinh BK, Cappello L, Masia L. Localized Extreme Learning Machine for online inverse dynamic model estimation in soft wearable exoskeleton. In: 6th IEEE/RAS-EMBS International Conference on Biomedical Robotics and Biomechatronics UTown, Singapore: IEEE; 2016;580–587.
- 99.Xiloyannis M, Cappello L, Khanh Dinh B, Antuvan CW, Masia L. Design and preliminary testing of a soft exosuit for assisting elbow movements and hand grasping. In: Ibáñez J, González-Vargas J, Azorín JM, Akay M, Pons JL, editors. Converging clinical and engineering research on neurorehabilitation II. Cham: Springer International Publishing; 2017. pp. 557–561. [Google Scholar]
- 100.Xiloyannis M, Cappello L, Binh KD, Antuvan CW, Masia L. Preliminary design and control of a soft exosuit for assisting elbow movements and hand grasping in activities of daily living. J Rehabil Assist Technol Eng. 2017;4:205566831668031. doi: 10.1177/2055668316680315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lotti N, Xiloyannis M, Durandau G, Galofaro E, Sanguineti V, Masia L, et al. Adaptive model-based myoelectric control for a soft wearable arm exosuit: A new generation of wearable robot control. IEEE Robot Autom Mag. 2020 doi: 10.1109/MRA.2019.2955669. [DOI] [Google Scholar]
- 102.Hosseini M, Meattini R, Palli G, Melchiorri C. Development of sEMG-driven assistive devices based on twisted string actuation. 3rd Int Conf Control. Autom Robo. 2017;2017:115–20. [Google Scholar]
- 103.Kim YG, Xiloyannis M, Accoto D, Masia L. Development of a SoftExosuit for Industrial Applications. In: 2018 Development of as soft Exosuit for Industrial Applications 7th International Conference for Biomedical Robotics and Biomechatronics. IEEE. 2018;2018:324–9.
- 104.Li N, Yang T, Yang Y, Yu P, Xue X, Zhao X, et al. Bioinspired Musculoskeletal Model-based Soft Wrist Exoskeleton for Stroke Rehabilitation. J Bionic Eng. 2020;17(6):1163–1174. doi: 10.1007/s42235-020-0101-9. [DOI] [Google Scholar]
- 105.Samper-Escudero JL, Contreras-González AF, Pont-Esteban D, Sáez-Sáez FJ, Sanchez-Urán MA, Ferre MÁ. Assessment of an upper limb exosuit with textile coupling. In: 2020 IEEE International Conference on Human-Machine Systems (ICHMS); 2020;1–6.
- 106.Samper-Escudero JL, Contreras-González AF, Ferre M, Sánchez-Urán MA, Pont-Esteban D. Efficient multiaxial shoulder-motion tracking based on flexible resistive sensors applied to exosuits. Soft Robot. 2020;7(3):370–385. doi: 10.1089/soro.2019.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zuccon G, Bottin M, Ceccarelli M, Rosati G. Design and performance of an elbow assisting mechanism. Machines. 2020;8(4):1–15. doi: 10.3390/machines8040068. [DOI] [Google Scholar]
- 108.Kobayashi H, Hiramatsu K. Development of muscle suit for upper limb. Proc 2004 IEEE Int Conf Robot Autom. 2004 doi: 10.1109/ROBOT.2004.1307433. [DOI] [Google Scholar]
- 109.Kobayashi H, Ishida Y, Suzuki H. Realization of all motion for the upper limb by a muscle suit. Proc 2004 IEEE Int Work Robot Hum Interact Commun. 2004 doi: 10.1109/ROMAN.2004.1374835. [DOI] [Google Scholar]
- 110.Ueda J, Ding M, Matsugashita M, Oya R, Ogasawara T. Pinpointed control of muscles by using power-assisting device. 2007 IEEE Int Conf Robot Autom. 2007 doi: 10.1109/BIOROB.2008.4762829. [DOI] [Google Scholar]
- 111.Ueda J, Matsugashita M, Oya R, Ogasawara T. Control of muscle force during exercise using a musculoskeletal-exoskeletal integrated human model. Springer Tracts Adv Robot. 2008;39:143–152. doi: 10.1007/978-3-540-77457-0_14. [DOI] [Google Scholar]
- 112.Ding M, Ueda J, Ogasawara T. Pinpointed muscle force control using a power-assisting device: System configuration and experiment. Proc 2nd Bienn IEEE/RAS-EMBS Int Conf Biomed Robot Biomechatron. 2008;2008:181–186. [Google Scholar]
- 113.Ueda J, Hyderabadwala M, Krishnamoorthy V, Shinohara M. Motor task planning for neuromuscular function tests using an individual muscle control technique. ICORR. 2009;2009:133–8. [Google Scholar]
- 114.Ueda J, Ming D, Krishnamoorthy V, Shinohara M, Ogasawara T. Individual muscle control using an exoskeleton robot for muscle function testing. IEEE Trans Neural Syst Rehabil Eng. 2010;18(4):339–350. doi: 10.1109/TNSRE.2010.2047116. [DOI] [PubMed] [Google Scholar]
- 115.Gallagher W, Ding M, Ueda J. Relaxed individual control of skeletal muscle forces via physical human-robot interaction. Multibody Syst Dyn. 2013;30:77–99. doi: 10.1007/s11044-013-9362-y. [DOI] [Google Scholar]
- 116.Bartlett NW, Lyau V, Raiford WA, Holland D, Gafford JB, Ellis TD, et al. A soft robotic orthosis for wrist rehabilitation. J Med Devices Trans ASME. 2015;9(3):1–3. [Google Scholar]
- 117.Al-Fahaam H, Davis S, Nefti Meziani S. A novel, soft, bending actuator for use in power assist and rehabilitation exoskeletons. In: IEEE International Conference on Intelligent Robots and Systems, Vancouver: IEEE; 2017;533–538.
- 118.Al-Fahaam H, Davis S, Nefti-Meziani S. Wrist rehabilitation exoskeleton robot based on pneumatic soft actuators. In: 2016 International Conference for Students on Applied Engineering 2016. School of Mechanical and Systems Engineering; 2017;491–496.
- 119.Simpson CS, Okamura AM, Hawkes EW. Exomuscle: an inflatable device for shoulder abduction support. IEEE Int Conf Robot Autom. 2017;2017:6651–7. [Google Scholar]
- 120.Zhang X, Singh G, Krishnan GA. soft wearable sleeve for joint stiffness modulation. IEEE Int Conf Adv Intell Mechatron. 2016;2016:264–9. [Google Scholar]
- 121.Thompson N, Zhang X, Ayala F, Hsiao-Wecksler ET, Augmented Krishnan G, Stiffness joint, actuation using architectures of soft pneumatic actuators. In: International Conference on Robotics and Automation Brisbane, Australia. 2018;2018:1533–8.
- 122.Gao X, Sun Y, Hao L, Xiang C, Cheng HA. new type of soft pneumatic elbow. IEEE Int Conf Robot Biomimetics. 2017;2018:2681–6. [Google Scholar]
- 123.Gao X, Sun Y, Hao L, Yang H, Chen Y, Xiang C. A new soft pneumatic elbow pad for joint assistance with application to smart campus. IEEE Access. 2018;6:38967–38976. doi: 10.1109/ACCESS.2018.2852757. [DOI] [Google Scholar]
- 124.Zhang G, Lin M. Design of a soft robot using pneumatic muscles for elbow rehabilitation. 3rd Int Conf Robot Autom Eng. 2018;2018:14–8. [Google Scholar]
- 125.Abe T, Koizumi S, Nabae H, Endo G, Suzumori K, Sato N, et al. Fabrication of 18 weave muscles and their application to soft power support suit for upper limbs using Thin McKibben Muscle. IEEE Robot Autom Lett. 2019;4(3):2532–8. doi: 10.1109/LRA.2019.2907433. [DOI] [Google Scholar]
- 126.Nassour J, Vaghani S, Hamker FH. Design of soft exosuit for elbow assistance using butyl rubber tubes and textile. Cham: Springer International Publishing; 2019. [Google Scholar]
- 127.Irshaidat M, Soufian M, Elkurdi A, Nefti-Meziani S. Soft and hard robotics for movement rehabilitation, analysis and modelling. Proc Int Conf Dev eSystems Eng. 2019 doi: 10.1109/DeSE.2019.00179. [DOI] [Google Scholar]
- 128.Ang BWK, Yeow CH. Design and characterization of a 3d printed soft robotic wrist sleeve with 2 DoF for stroke rehabilitation. In: 2019 IEEE International Conference on Soft Robotics Seoul, Korea: IEEE; 2019;577–582.
- 129.Park SH, Yi J, Kim D, Lee Y, Koo HS, Park YLA, lightweight, soft wearable sleeve for rehabilitation of forearm pronation and supination. In: IEEE International Conference on Soft Robotics, IEEE. 2019;2019:636–41.
- 130.Realmuto J, Sanger TA. Robotic forearm orthosis using soft fabric-based helical actuators. 2nd IEEE Int Conf Soft Robot. 2019;2019:591–6. [Google Scholar]
- 131.Natividad RF, Hong SW, Miller-Jackson TM, Yeow CH. The exosleeve: a soft robotic exoskeleton for assisting in activities of daily living. Cham: Springer International Publishing; 2019. [Google Scholar]
- 132.Goto T, Kurita Y, Das S, Kunze K. Artificial motion guidance: an intuitive device based on pneumatic gel muscle (PGM). In: 31st Annual ACM Symposium on User Interface Software and Technology, Berlin, Germany; 2018;182–184.
- 133.Ang BWK, Yeow CH. Design and modeling of a high force soft actuator for assisted elbow flexion. IEEE Robot Autom Lett. 2020;5(2):3731–3736. doi: 10.1109/LRA.2020.2980990. [DOI] [Google Scholar]
- 134.Simpson C, Huerta B, Sketch S, Lansberg M, Hawkes E, Okamura A. Upper Extremity Exomuscle for Shoulder Abduction Support. IEEE Trans Med Robot Bionics. 2020;2(3):474–484. doi: 10.1109/TMRB.2020.3012471. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.