Abstract
We provide a game-theoretical epidemiological model for the COVID-19 pandemic that takes into account that: (1) asymptomatic individuals can be contagious, (2) contagion is behavior-dependent, (3) behavior is determined by a game that depends on beliefs and social interactions, (4) there can be systematic biases in the perceptions and beliefs about the pandemic. We incorporate lockdown decisions by the government into the model. The citizens’ and government’s beliefs can exhibit several biases that we discuss from the point of view of behavioral economics. We provide simulations to understand the effect of lockdown decisions and the possibility of “nudging” citizens in the right direction by improving the accuracy of their beliefs.
Keywords: COVID-19, epidemiology, game theory, behavioral economics, public health policy
1. Introduction
The 2019 coronavirus disease outbreak (COVID-19) has posed a significant threat to human health and the global economy, resulting in a global public health emergency. Access to approved treatments and vaccines for this disease had only recently become available when writing this article. That means that for several months during the pandemic, governments and organizations have had to rely on preventive measures such as lockdowns, social distancing, and hygienic behaviors, e.g., the use of face masks and hand-washing. As a result, a clear goal of public health policy during this outbreak has been to encourage people to practice responsible preventive behavior to limit the spread of COVID-19. Behavioral economics can help us understand how to design effective policies, implement them, and who the target population should be. This field applies insights from psychology and neuroscience to explain why people deviate from rational choice theory due to biases people may face during their decision-making process. Various scholars have pointed out that identifying these behavioral biases in the population can help predict how public health policies will be received and thus prevent them from backfiring in the current global situation [1,2,3]. Indeed, behavioral economics has been shown to produce highly effective and low-cost policies on health-related issues [4,5,6]. In addition, several articles have echoed the importance of policymakers taking into account individuals’ cognitive biases, as this allows for more efficient policy design, including policies related to public health [3,7,8].
We incorporate these insights of behavioral economics into a formal epidemiological model (SEIR-like). Our research hypothesis is that including those insights would change the predictions of SEIR-like models in relevant ways. In particular, we expect that “behavioral interventions” (that change the individual’s perceptions of the environment) can mitigate contagion. Therefore, such epidemiological models incorporating behavioral economics can be used to study how the dynamics of the pandemic (i.e., people infected and recovered) may change due to both individual and government behavior and their interaction as people’s behavior determines to some extent, the severity of the pandemic, and thus its economic consequences. We are the first, to the best of our knowledge, to combine epidemiological, game-theoretical, and behavioral assumptions to predict the progression of a pandemic. Indeed, ref. [9] argues that cooperation between economists and epidemiologists is required to tackle pandemics because it is a complex, cross-disciplinary issue that affects all aspects of society.
We build on two different kinds of literature. The first combines economics and epidemiology. Examples of this strand of literature are the studies on endogenizing economic behavior in a rational framework [10]; considering that the rate at which individuals change their sexual partner is endogenously determined by the prevalence of HIV [11]; a rational choice framework in which individuals decide on several aspects of their sexual relationships [12]; and allowing for forward-looking risky behavior [13]. More recently, this type of model has been applied to the study of COVID-19 [14,15,16]. The second literature incorporates game theory into epidemiological models, for example, considering myopic agents who can choose a continuous variable of protection [17]; and, more recently, addressing variants of the SIR model in which individuals reduce contacts as a function of the current or cumulative number of cases [18].
However, to the best of our knowledge, there has been no attempt to incorporate behavioral economics into a game-theoretical epidemiological model. This means that the analysis either comes from behavioral economics but with no formal epidemiological models or from epidemiological models that do not consider behavioral economics. In the present article, we aim to integrate behavioral economics into a game-theoretical epidemiological model with the goals of improving the predictions of the model and to better formalize some of the arguments that have been advanced from behavioral economics about the management of COVID-19.
2. Materials and Methods
2.1. SEIR Model, Game Theory, and Behavioral Economics
In this paper, we build upon the well-known compartmental epidemiological models as Susceptible-Exposed-Infectious-Removed (SEIR) that have been useful in studying pandemic dynamics. These models demonstrate how various public health strategies can influence the epidemic’s outcome. However, we believe that considering how behavioral biases can influence pandemic dynamics through individual actions can yield a wealth of information. Concerning this, we are the first, to our knowledge, to combine game theory and behavioral economics with an epidemiological model. This allows us to (1) endogenize the behavior of the population and, in particular, to allow agents to react to incentives and their perceptions of the progression of the pandemic; (2) to formalize how cognitive biases affect people’s perceptions, which in turn affect their behavior and, ultimately, the dynamics of contagion.
Our model has three components that, as we discussed, have never been jointly used before:
-
1.
A SEIR-type epidemiological model that, in particular, considers asymptomatic transmission for the case of COVID-19.
-
2.
A game-theoretical component in which individuals choose their level of responsible behavior (and thus the probability of contagion).
-
3.
Mechanisms from behavioral economics, considering that individuals’ perceptions and beliefs might be biased, especially as applied to COVID-19 [1,2,7,8,19]. In particular, we consider the following channels (we provide additional details about these channels in Online Appendix D).
-
(a)
Optimism bias and overconfidence, by which people tend to be excessively optimistic about future events and excessively confident in their own beliefs and skills to face those events [20].
-
(b)
Availability heuristic, in which the probability of an unknown event (a severe pandemic COVID-19) is estimated using the probability of a known event (a severe pandemic of seasonal influenza).
-
(c)
Fallacy of lack of evidence, whereby an absence of evidence for an event is interpreted as evidence for the absence of that event [21].
-
(d)
Status quo bias, by which people tend to prefer the current baseline (or status quo) over any change in such a way that there is a risk of doing nothing in the face of such a novel event as the pandemic [22].
-
(e)
Social influences have been extensively studied as a critical element in their effect on people’s choices and behaviors [23], especially on health-related outcomes.
-
(a)
2.2. Calibration
The simulations are all 360 periods long, e.g., , except those for the extended model, where we use 180 periods in the interest of computational time (included in the Online Appendix A). (However, this does not affect the shape of the dynamics, e.g., in terms of the evolution of cases, and therefore we can still compare the results across simulations.) To solve the system of non-linear differential equations, we have used a standard Runge-Kutta algorithm for the integration. Moreover, the parameters included in the model can be divided into two groups: medical-epidemiological parameters and behavioral parameters. The first group includes the subclinical infectious rate Asymptomatic vs. Infected, ; the (baseline) transmission rate, ; the recovery rate, ; the proportion of asymptomatic/subclinical cases, ; the mortality rate, ; and the incubation rate, . These parameters are summarized in Table 1, where the value used in the simulations and its corresponding reference can be seen. Some of these values are directly given by the SARS-CoV-2 characteristics themselves, such as the recovery rate (the inverse of the days needed for full recovery) and the incubation rate (the inverse of the days needed to incubate the virus). However, the remaining values are taken from the existing literature, which has estimated them using epidemiological models.
Table 1.
SEAIRD epidemiological parameter values.
| Parameter | Value Used | Range | Description | Reference |
|---|---|---|---|---|
| 0.5 | - | Subclinical infectious rate A vs. I | [24] | |
| 0.65 | 0.1–1 | (Baseline) Transmission rate | [25] | |
| 1/14 | - | Recovery rate for mild infections | [26] | |
| 1/3 | 0.05–0.6 | Proportion of subclinical cases | [27] | |
| 0.021 | 0.005–0.03 | Death rate | [28] | |
| 1/6.4 | - | Incubation rate | [29] |
Notes: This table shows the values of the parameters used for the model simulations. The first two parameters are taken from the epidemiology literature, being the baseline contagion rate a calibration. The last four are medically known parameters.
The set of behavioral parameters that are included in the model are summarized in Table 2, where the theoretical value in the model, the value used in the simulations, and a summary of its interpretation from a behavioral economics point of view are presented.
Table 2.
Relevant Behavioral and Economic parameters.
| Parameter | Value Used | Theoretical Range | Description | Behavioral Interpretation |
|---|---|---|---|---|
| 0.5 | Citizen’s and government’s prior |
|
||
| −0.5 | Disutility of contracting COVID-19 | – | ||
| c | Economic/psychological cost | – | ||
| 0 | Population mean of the cost c | |||
| 1 | Population variance of the cost c | |||
| 0.5 | Extra “moral” utility (for I) | – | ||
| , | Lockdown efficacy | – | ||
| 0.8 | Protective measures efficacy (for S and I) | Wrong beliefs : Availability heuristic | ||
| 0 | Strength of social norms | Social/Country norms |
Notes: These are the relevant values given to behavioral and economic parameters in the model. Each simulation in the model keeps these values constant while changing the parameter of interest analyzed.
3. Theory
3.1. SEAIRD Baseline Model
We describe a discrete-time SEAIRD model of COVID-19: Susceptible, Exposed, Asymptomatic (subclinical) infected, symptomatic (clinical) Infected, Recovered, and Deceased. (The SEAIRD model is an SEIR model with an additional category for infected but asymptomatic and another for deceased. Those in both E and A are unaware of their status. The implication of the model is that both exposed and asymptomatic individuals will behave as susceptible. However, asymptomatic infected individuals will have an infectious potential). We build our model following [30] (note that all variables depend implicitly on time t):
| (1) |
| (2) |
| (3) |
| (4) |
| (5) |
| (6) |
where represents the profile of actions taken by the population, which remains constant over time. Hence, we consider that the contagion rate depends on actions taken by citizens (such as protective measures) and take the rest of the medical parameters as independent from behavior. Following other models that consider asymptomatic individuals, e.g., [31], we consider that those in A and I have different infectious potential and behavior. In terms of the dynamics of the disease, successful individuals first become exposed with a certain probability that, as we have mentioned, depends on the behavior of asymptomatic and symptomatic infected individuals, which we explained below in more detail. (There is not a single “beta” parameter, but rather two: and , and they depend on the individual’s behavior. Indeed, it is precisely this dependence on behavior for the two categories that generate the need for two such parameters.) Those who are exposed will develop the disease with probability , and of those, they will either become infected asymptomatic (with probability ) or infected symptomatic (with probability ). Finally, individuals who are infected (either symptomatic or asymptomatic) will recover with probability , except for a fraction of those, who will die of the disease.
3.2. Individual Behavior
At each period of time, individuals decide whether to engage in responsible behavior or not. This responsible behavior (that we label “protect”) can include taking protective measures such as wearing a face mask, washing hands regularly, keeping social distance, etc. (Deceased individuals do not choose any action, and so from now on when we discuss behavior, we will refer exclusively to each of the other categories.) Moreover, individuals have a belief about the probability of the disease being capable of causing a pandemic. We argue that the several biases that we considered in Section 2, imply that , i.e., the individual undervalues the probability of a severe pandemic (in Online Appendix D we provide a detailed account about how these biases would affect ). This parameter allows us to capture several cognitive biases that could potentially happen at the beginning of the pandemic when individuals might underestimate the probability of the virus generating a pandemic. In addition, each individual has beliefs about the contagion that takes place (depending on the action she takes). While we give the explicit definition below, should be interpreted as the probability that an interaction between an individual who chooses a and another random individual in the population will result in contagion.
Individuals suffer a disutility from contracting the disease, and each individual has a private cost c of protecting oneself, normally distributed . Moreover, we assume that the psychological benefit or cost from protecting oneself depends only on the average action taken by the population. Function could be negative (i.e., at the beginning of the pandemic, when few people are engaging in protective measures, they can be ridiculed for doing so) or positive. We assume that those infected always have an extra “moral” utility when engaging in responsible behavior. Thus, the payoffs for taking a certain action depend on the individual’s status, as described in the table below (Table 3).
Table 3.
Payoff matrix.
| Protect | Don’t Protect | |
|---|---|---|
| I | 0 | |
| R | 0 |
There are several important details to consider. First, we follow the epidemiological literature that incorporates game theory, such as [17], assuming that individuals are not forward-looking but rather that they best respond to their incentives each period. Second, since we assumed that individuals in the categories , and A cannot differentiate between them (that is, individuals are unable to identify whether they are susceptible, exposed, or infected but asymptomatic), the incentives for individuals in those categories are identical. Note also that the government can influence the citizens’ perceptions, for example, by making them aware of the severity of the pandemic (hence making more accurate) or by using nudges that influence their perception over the contagion rate, something we discuss in Section 4.2.3.
As we noted in the Introduction, our model departs from many epidemiological models in having two distinct functions , , the rate at which susceptible agents become infected by asymptomatic and infected individuals, respectively. These rates are derived by assuming that each individual interacts randomly with another individual each period. Following [30], we assume that parameter measures the baseline contagion rate from those in I when there is no lockdown and no protective measures are taken. In contrast, for those in A, this rate is multiplied by a factor , willing to capture the biological difference in the contagion rate between asymptomatic and symptomatic individuals. Moreover, we assume that for any infectious individual (symptomatic or not), their contagion is reduced by a factor of when they use protective measures and by a factor that depends on whether lockdown is in effect (, a case that we discuss below in Section 3.3), or not . (In particular, if there is no lockdown , then . If there is a lockdown, then is an exogenous parameter determining how effective the lockdown is in reducing contagion when agents respect the lockdown. Ref. [32] consider instead the effectiveness of lockdown . Therefore, .) With these assumptions in place, we have that and are given by:
| (7) |
| (8) |
where the expectation is taken over behavior in each compartment (i.e., ), as the cost of choosing protective measures is idiosyncratic for each individual. Note that for a susceptible individual, the relevant rate is given by , that is a weighted sum of and , conditional on the action a chosen by the individual
However, we allow individuals to have a biased belief about , which we denote by , and therefore they might have a biased belief about , which we denote . ( would be defined as In other words, individuals understand the basic dynamics of the contagion rates when they compute the utility of choosing actions, but we allow for the possibility that they are biased in their estimation of the effectiveness of responsible behavior and, therefore, believe that it is given by . Obviously, if the individuals held correct beliefs about , then .)
Solving the Baseline Model with No Lockdown
From the game payoffs it follows immediately that an individual with cost c uses protective measures whenever if she is in I, and whenever if she is in R. Pre-symptomatic individuals (in ) with cost c use protective measures whenever
Therefore, for each category of individuals there is a threshold (with ), such that the individual protects herself if her cost is below the threshold. Hence, the fraction of individuals in S who protect themselves is (where is the standard normal CDF), and analogously for the other four categories. Note that at the beginning of the pandemic, we have , and, therefore, the incentives for susceptible individuals are approximately the same as for recovered individuals, namely those given by social norms.
3.3. Lockdown
Having mentioned the possibility of lockdown in the previous section, we now consider how it might occur. In our model, we assume that the government is the only player who can choose the lockdown. The government derives a disutility q from lockdown (as it reduces economic activity or increases criticism) per period that the lockdown is enforced. However, the government also derives a disutility from the deaths during the pandemic. Therefore, the expected utility of the government (we assume no time-discounting at this stage) at time T when a successful vaccination campaign is implemented and the pandemic ends is:
| (9) |
where is the probability the government assigns to the pandemic, and if there was a lockdown at time t, and 0 otherwise. As we assume that deaths can only be produced by the pandemic, we then have that .
Assumption A1.
The lockdown enacted by the government has the following restrictions: (1) the lockdown can only be approved in discrete segments of duration τ; (2) once a lockdown is not in place, the government must wait for a period τ to begin a new lockdown; and (3) the first time a decision about lockdown must be made is at time .
In practice, Assumption 1 means that the government can only enact lockdown at time ,⋯, until time T when a vaccine is discovered and implemented (for simplicity, we abstract away from considering the issues associated with implementing the vaccine). (In Online Appendix A, we consider an extension with a political economy model that allows for two types of government (authoritarian and democratic), as well as the possibility of declaring the state of alarm. We then explore the interaction between beliefs about the pandemic and the government’s response.)
4. Results
4.1. Theoretical Results
Asymptomatic individuals are biologically less contagious than symptomatic Infected individuals (because of in Equation (7)). However, they can be more contagious once we take into account their behavior. Let be the average action taken by Infected and Asymptomatic individuals, respectively.
Proposition 1.
Let be defined as
(10) Then, whenever , Asymptomatic individuals are more contagious than symptomatic Infected individuals.
While Asymptomatic individuals are biologically less infectious, Proposition 1 highlights the case when they are behaviorally more contagious than infected individuals, as they are not aware of transmitting the disease. Therefore, we have two opposing forces. In our model, when , the behavioral contagion channel is stronger than the biological channel, and that is why Asymptomatic are more contagious than symptomatic Infected individuals. This is a crucial insight to understanding the transmission of SARS-CoV-2: as asymptomatic individuals may not take precautions (e.g., by wearing face masks, washing hands), they become more contagious than symptomatic individuals, and they are then more likely to transmit the virus to the susceptible population.
Proposition 2.
The threshold is increasing in . A sufficient condition for to be increasing in ν and is that .
Proposition 2 shows that when the citizen’s perception of the efficacy of protective measures increases, it becomes more difficult for Asymptomatic individuals to be more contagious than symptomatic Infected individuals. The intuition for this is that when increases, Asymptomatic individuals (who behave as Susceptible, as they are not aware of being infected) are more willing to engage in protective behavior, which reduces their infectiousness. On the other hand, when the actual effectiveness of protective measures or lockdown increase, the effect on is a priori ambiguous; however, when , we can say with certainty that is increasing. Therefore, beyond the efforts that governments can make to improve the actual effectiveness of protective measures, it is essential to note that increasing citizens’ perceptions another helpful strategy for fighting COVID-19, something we discuss further in the next section. (We perform similar simulations for the efficacy of lockdown measures in Online Appendix C).
4.2. Numerical Results
In this section, we present the results of the model simulations for each of the six categories contained in the SEAIRD behavioral epidemiology model. We want to stress the fact that there is great uncertainty about the key parameters for the COVID-19 epidemic [33]. This uncertainty extends to the design of an optimal policy, as these parameters are extremely sensitive to changes [34,35,36]. Moreover, simulations are often performed under strong assumptions about the impact of social distance policies without connecting to the necessary data [37]. As a result, since the exact numbers in terms of economic cost and public health are affected by this [38], our analysis will focus solely on assessing the effects on the relative change in pandemic dynamics. For example, comparing the evolution of the number of infected between various scenarios rather than in absolute terms (e.g., the total number of infected). These results should then be interpreted as changes in the dynamics (evolution) between categories. Concerning this, any policy that has focused on containing the spread of the virus has aimed to “flatten the curve”, and thus reduce the rate at which society as a whole goes from Susceptible to Exposed, that is, the contagion rate. Based on the model and the results presented below, any policymaker should consider several factors that may influence the dynamics of the pandemic. In this regard, two factors that have a major effect on this evolution and have a direct link to behavioral economics are (1) the effectiveness of preventive measures (as well as the perception that individuals have of them, ), and (2) the social norms that prevail in the country or “country” norms. In the following subsections, we will further analyze the two factors mentioned above.
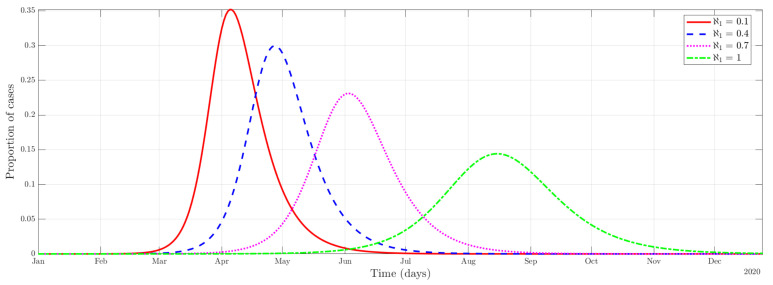
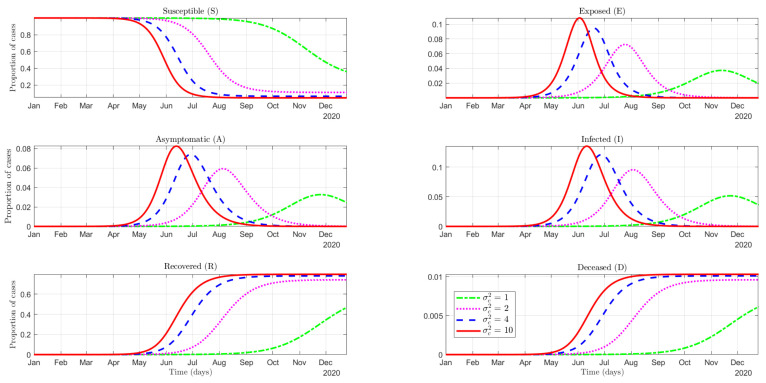
4.2.1. Effectiveness of the Use of Protective Measures
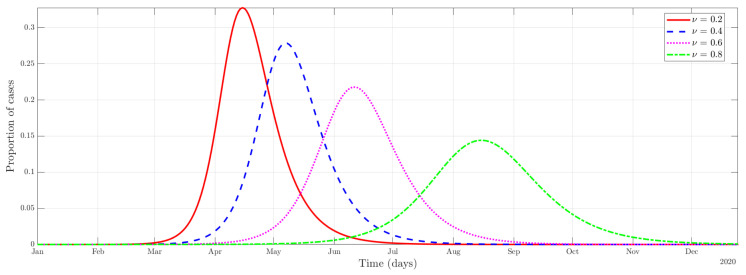
As we can see in Figure 1, an increase in efficacy translates into a slowing down of the outbreak. (Other factors that affect the time-course of the outbreak. The graph for the efficacy of lockdown is similar to that in Figure 1 and can be found in the Online Appendix C. These parameters directly affect the contagion rate of A (), and I (), decreasing the rate at which individuals in S flow to the E category.) That is to say, as the efficacy increases, the number of infected cases becomes more homogeneously distributed during the period of time considered in the simulation. In other words, a public health policy aimed at increasing the effectiveness of the use of protective measures will produce a flattening of the curve in terms of the proportion of cases. Examples of such policies could be an introduction of mandatory face mask use, the use of hydroalcoholic gel in establishments, or a policy that establishes social distance.
Figure 1.
Disease dynamics of the combined infectious category () with different protective measures effectiveness.
4.2.2. Social Norms
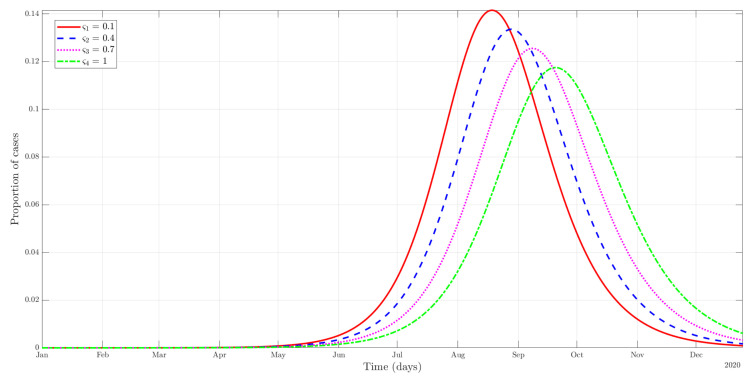
Social norms have been emphasized as one of the key factors in determining behavior during the pandemic, and, therefore, effective rates of contagion [3,7,39,40,41,42,43,44,45]. We have modeled social norms by including as a payoff for engaging in protective measures for all individuals (symptomatic individuals derive an extra ). For the sake of deriving numerical results, we model function , where is a sigmoid function, and is a constant that is intended to capture “shifts” in the importance of social norms across differences societies (thus, is also a “behavioral” parameter).
As we can see in Figure 2, an increase of has the expected effect on the evolution of the number of cases in terms of flattening the curve over the time period. Higher values of reflect stronger norms (possibly country-specific), which translates into a higher proportion of individuals being protected from the onset of the pandemic. For instance, in the case of face masks, those countries that started their widespread use (mask-wearing culture) have been able to contain the virus better in terms of the rate of contagion. This is because public mask-wearing is most effective at preventing virus spread when compliance is high [46]. Concerning this, in the absence of widespread vaccination for COVID-19, governments and public health institutions have ended up being advocated for individuals to use preventive measures during the pandemic. Therefore, developing public health policies that affect (in this case, social norms) is vital to slow down the time-course of the outbreak. In addition, policymakers must also take into account potential free-riding behavior. In the case of face masks, a greater use of them in the community may encourage others to follow the norm. However, it also creates incentives for others not to assume the cost of protecting themselves since others already do so [45].
Figure 2.
Evolution in the number of cases of the combined infectious category () depends on the strength of social norms ().
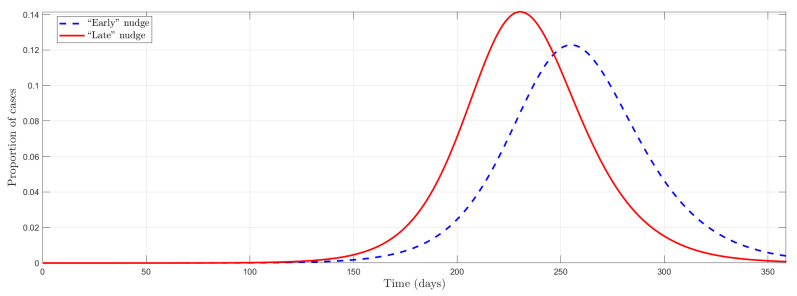
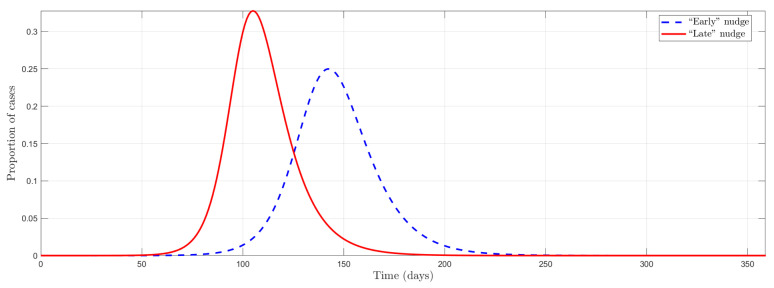
Additionally, it is different to start at an early stage of the pandemic in a country with a culture of preventive measures from another society that promotes this social norm in more advanced pandemic stages. Thus, in the following simulation, we exploit the timing of a policy aimed at shifting social norms in two different periods. We can see in Figure 3 that the model captures well this “timing effect” or anticipation in the public policies. This is of great importance since nudges that directly affect social norms by inducing a change in behavior at the beginning of the pandemic have a more significant effect at “flattening the curve” than when it is at a more advanced stage.
Figure 3.
Timing effect in a nudge on social norms.
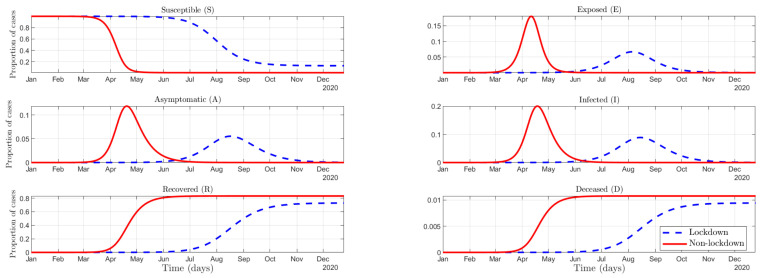
4.2.3. Mandates vs. Nudges to Fight COVID
Individuals’ decisions to use preventive measures are greatly affected by both their beliefs about their efficacy as well as the prevalence of their behavior, e.g., the use of face masks in public [45]. As part of these preventive measures, wearing a mask is highly effective. It may protect both the user and those around them from contracting COVID-19 [40,46,47,48,49,50]. Moreover, the effectiveness of other measures, such as hand-washing or social distancing, is also decisive in influencing the number of reported daily cases, for instance, in Thailand, ref. [51]. Thus, the effectiveness of any preventive measures against the transmission of the virus can be very high. However, if citizens believe that it is not effective, that will guide their beliefs and, therefore, their actions (they might fail to protect themselves). Instead of trying to change individuals’ beliefs, the government might use mandates that increase the effectiveness of protective measures, corresponding to an increase in in our model (imposing mandatory use of masks, use of hydroalcoholic gel in establishments, social distancing, etc.), as discussed in Section 4.2.1. (In our model, mandates have a qualitatively similar effect to a change in social norms, leading to a flattening of the curve.)
In terms of changing not only the actual effectiveness , but also the perception about it , a policy maker might at first think that both would have the same effect on the evolution of cases (although not in proportion). However, the intuition is not straightforward. In our model, a shift in perception has minimal effect on the dynamics of the pandemic, which is striking because it is the perceptions that guide, to some extent, individuals’ behavior. To better understand this phenomenon, note that at the beginning of the pandemic, the number of cases is so small that a change in perception does not generate sufficient incentives to move the average behavior of society (behavioral force). However, when the number of cases grows sufficiently enough so that perceptions can cause such incentives, it is “too late” because then a nudge on perception does not achieve the desired objective due to the sheer inertia of the dynamics (epidemiological force). Indeed, ref. [52] find using a causal structural model that in the US, a nationwide mandate on the use of face masks for employees in the early stages of the pandemic could have resulted in a reduction of weekly case growth by more than ten percentage points in late April.
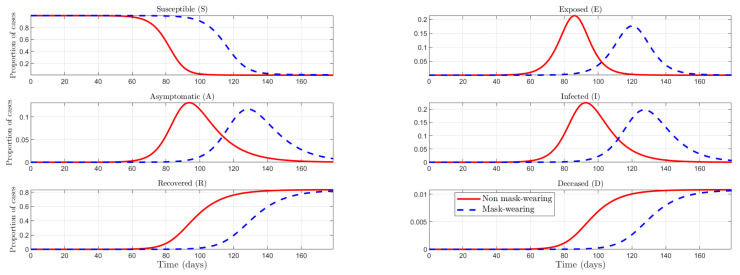
About a mandate forcing individuals to wear face masks in the early stages of the pandemic versus later stages, we find the same timing effect as with social norms. (As was the case with social norms, the timing of behavioral policies also matters. In the Online Appendix C, we include an exercise similar to that in Figure 3 and find a similar result: implementing the nudge earlier is more effective in flattening the curve.) This emphasizes the importance of taking direct and unhesitating action even when the number of cases is low, as the number of cases is growing exponentially. As [53] noted, there are two main reasons why countries like Taiwan have been able to control the virus much more quickly: first, Taiwan had a robust public health infrastructure in place before COVID-19, allowing for faster and more coordinated responses; and second, widespread use of face masks to reduce transmission from infected people (regardless of symptoms) while also protecting wearers (mass wearing). This leads us to propose the exercise of comparing two scenarios: one in which a mask-wearing culture with citizens with greater accuracy in their beliefs about the actual effectiveness of protective measures, against the opposite scenario. As we can see in Figure 4, a country with higher social norms and more accurate beliefs about the effectiveness of protection can flatten the curve, reducing then the incidence of the pandemic.
Figure 4.
Mask wearing vs. non-mask-wearing culture comparison: the effect of social norms and efficient use of protection.
5. Conclusions
As stated in the Introduction, our research hypothesis was that introducing behavioral insights and game theory into an SEIR-like epidemiological model would change the predictions of those models in relevant ways. We have validated this hypothesis by providing a series of novel results. We provide here a summary of those results.
A relevant finding is that, even if asymptomatic infected individuals are biologically less contagious than symptomatic individuals, for example, due to a lower virus load, ref. [54], they can be effectively more contagious (Proposition 1), the reason being that those with no symptoms might not take preventive measures against COVID-19 with enough intensity. However, we show that this is less likely to happen if the perceived effectiveness of protecting oneself increases (Proposition 2), as this in turn increases the perceived incentives for asymptomatic individuals to engage in protective behavior, thus reducing their infectiousness and lowering contagion. Theoretically, this means that governments can then mitigate the pandemic not only through lockdowns or by making it mandatory to wear face masks but also by “nudging” people to protect themselves and the rest of society [3].
Concerning our numerical results, we show that an increase in the effectiveness of protective measures “flattens the curve” of contagion, as is to be expected. However, an interesting result is that, perhaps surprisingly, improving citizen’s beliefs about the effectiveness of protective measures has a small effect on the pandemic dynamics. This is because at the start of the pandemic, improving citizens’ perceptions about protective measures has a small effect because there are few cases (and thus individual incentives are small), and by the time there are enough cases, it is “too late” to affect the dynamics of contagion meaningfully. The same is true for social norms which, by themselves, might not be enough to stop the spread of the pandemic in countries in which the initial social norm is not to engage in protective behavior, for a similar reason as the one discussed for nudges about preventive measures effectiveness. For these reasons, mandates might be more effective at the beginning of the pandemic, in terms of reducing contagion, than nudges or a sudden increase in social pressure. (However, as we argue in [55], nudges are also easier and faster to implement, and thus governments might be better off by implementing nudges in the interim while mandates are being approved.) This is one of the reasons why, in coherence with our results, mask-wearing societies with populations used to the use of protective measures have had a faster control of the pandemic [46]: the more normalized in society the use of protective measures is, the higher the probability of adopting them initially and thus when it matters most for controlling contagion and flattening the curve.
These results show that our research hypothesis was correct, and our model has produced meaningful insights that could not have been derived without considering the behavioral biases of the individuals in their decision on whether to take preventive measures. This is obviously one of the strengths of our model. However, our framework has some limitations that we would like to discuss, as well as future research directions that can solve these limitations and provide new results.
One of the limitations of our framework is that we use a “reduced form” approach, where several biases are mapped to the same behavioral parameters: a future research direction is to incorporate specific biases explicitly into the model, for example, present bias through models of hyperbolic discounting, ref. [56]. Another limitation is that the action space is small, with only two possible actions for individuals to take; an immediate avenue for future research consists of enriching the action space to include multidimensional actions (to allow for the possibility that wearing face masks may relax other protective measures), as well as heterogeneity by age and other characteristics, in such a way that the payoffs of the game depend on such characteristics. (As older people have a demonstrated higher risk of suffering the consequences of COVID-19 [57], public health policies would also affect them heterogeneously depending on age.) In addition, social networks could be included together in the epidemiological-behavioral model.
We view our paper as the first step in a research agenda that combines epidemiological models, game theory, and behavioral economics, and we believe that it opens the possibility of incorporating interesting extensions. For example, we have included a political economy model in the Appendix A, in which the government must decide how to react to the pandemic. However, there are many other economic applications that can be incorporated, among others, vaccine R&D, vaccination campaigns, etc. We view all of these as fruitful extensions that can be incorporated into our framework.
The codes needed to replicate the results obtained in the article are provided as Supplementary Materials. In particular, they replicate all the figures included.
Abbreviations
The following abbreviations are used in this manuscript:
| SEIR | Susceptible-Exposed-Infectious-Removed |
| SEAIRD | Susceptible-Exposed-Asymptomatic-Infectious-Recovered-Deceased |
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19159557/s1, the codes needed to replicate the results obtained in the article.
Appendix A. Initial Reaction to the Pandemic
This section expands the model that we presented to include the initial reaction to the pandemic. If one thing has become clear, the government plays an important role in the course of the pandemic. In addition, it may suffer from biases that undermine its initial ability to react to the outbreak. In this new context, the players are the government and a continuum of mass 1 of citizens. There are two states of the world, ; for no pandemic and pandemic, respectively. (If there is no pandemic, no measures will be required; if there is a pandemic, then protective measures will be needed to reduce contagion. One possibility is that when there is no pandemic, the , and when the state there is pandemic, .) The objective probability that is p; however, the government assigns probability , and the citizens’ probability (and this is common knowledge). (Since these probabilities can be different, we are implicitly assuming that government and citizens have different priors [58].) We assume that , due to the behavioral biases discussed in Section 2, and explained in detail in Online Appendix D.
The government can be democratic (with probability ) and authoritarian (with probability ). The government can take two actions: Alarm or Wait. An authoritarian government derives extra utility from choosing Alarm. Moreover, these states are connected to the possibility of enforcing a lockdown.
Assumption A1.
At period , the government must choose Alarm if it decides to enforce a lockdown.
In other words, at , no lockdown can be enforced unless the government chooses alarm. After the government decides whether to choose Alarm or Wait, each citizen decides whether to Protest or Not protest. (We must not overlook the importance of political economy in the current pandemic. Ref. [59] show, for instance that countries under more significant electoral pressure took less stringent public health measures to prevent the spread of COVID-19. The effect of such policies is more likely to harm the economy. Moreover, in the early stages of the pandemic, protests against the lockdown erupted all over the world [60].) We assume for simplicity that this decision only happens during the initial period (although the model could be easily extended to allow for multiple protests). The government derives a disutility , where and f is the fraction of citizens that protest. The payoffs for citizen i, depending on the type of government, are as follows:
| Protest | No Protest | |
| Democratic | 0 | |
| Authoritarian | 0 |
Here k is to be interpreted as the private cost the individual must bear to protest, and we assume that , for some constant b, and is distributed i.i.d. , what makes this subgame a global game. The interpretation is that the individuals derive a benefit from protesting against an authoritarian government. However, this benefit depends on the fraction of citizens who participate in the protest (we consider these as reduced-form payoffs, although they could be microfounded). The payoff for the government for choosing Alarm is:
| (A1) |
( is the indicator function), and for choosing Wait:
| (A2) |
where and are the continuation payoffs for the government from choosing either action, as determined by Equation (9), and are the fractions of citizens that protest when the government chooses either action. Note that in Equation (9), both and depend implicitly on the action y selected by the government (Alarm vs. Wait), as that action determines the entire path of lockdown decisions until time T, that in turn determines the death rate, and hence the total disutility to the government.
Appendix A.1. Government Equilibrium Behavior
We consider the concept of Sequential Equilibrium. First, we solve the behavior of the citizens, and then we “backward induct” the behavior of the government. Let be the posterior that the government is democratic after it has chosen a particular action y. First, note that if , i.e., there is a certainty that the government is democratic, it is a dominant strategy for every citizen not to protest. Let be the fraction of citizens who oppose. Using standard techniques in global games [61], we know that a threshold will give the solution , such that a citizen chooses to protest whenever , as proved in Proposition A2 in Online Appendix B (note that the threshold depends on the action y chosen by the government, that in turn influences the citizens’ posterior that the government is democratic). (Note that appears in the government’s payoffs in Equations (A1) and (A2), and depends on the posterior , that in turn depends on the behavior of each of the two types of government.) We need to consider four possibilities: two pooling equilibria, in which both types choose the same action, and two separating equilibria.
Proposition A1.
There exist three sequential equilibria.
- 1.
Pooling equilibrium with Alarm, when: .
- 2.
Separating equilibrium in which the democratic government chooses Wait, and the authoritarian government chooses Alarm, when:
- 3.
Pooling equilibrium with Waiting, when
Appendix A.2. The Economic versus Health Trade-Off
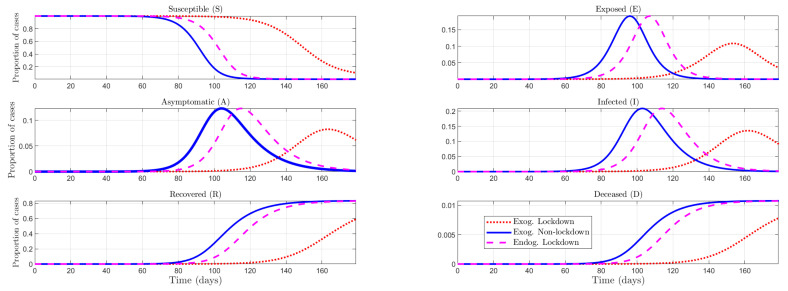
Most actions during COVID-19 have highlighted the uncomfortable trade-offs that societies suffer or will suffer in the future in response to the pandemic. As noted above, the immediate response of governments has focused primarily on “managing” the pandemic with the objective of “flattening the curve” or simply saving lives. In this appendix we have presented a conceptual framework that allows us to account for this feature: in the model, the government faces such trade-offs. It can impose lockdowns, but these policies come at a cost [62]. Figure A1 represents three scenarios: two of them in which the lockdown is imposed or not in an exogenous way for all the periods against a scenario in which the government chooses endogenously whether to impose or not a lockdown. The results of the model are predictable, yet it matches the reality. Any government has a trade-off between public health and the economy. This trade-off is represented in the government’s utility function in Equation (9). Thus, a policymaker would choose in between a permanent lockdown and no lockdown. Concerning this, lockdown policies are highly effective: in the U.S. and using a causal structural model framework, Chernozhukov2021 show that without stay-at-home orders, cases would have been higher by 6 to 63 percent, and without business closures, the number of infected cases would have been higher at 17 to 78 percent.
Figure A1.
Exogenous lockdown and Non-lockdown vs. endogenous lockdown (Alarm pooling equilibrium).
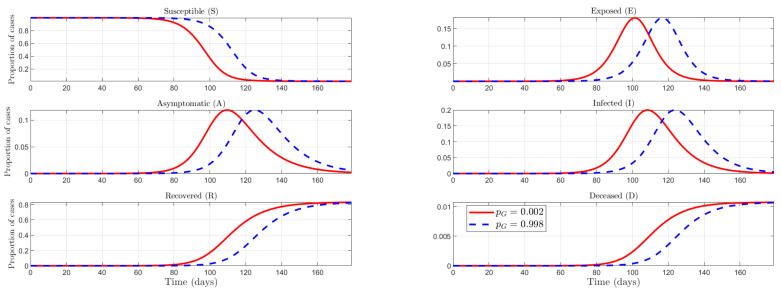
Appendix A.3. Unexpected versus Expected Pandemic
Just as crucial as the trade-off faced by governments in establishing policies that have an economic cost, the initial reaction to the pandemic by governments was decisive for its evolution in the early stages [52]. Figure A2 shows the effect on pandemic dynamics of a government that fully expects it to occur versus one that does not expect it to happen. As can be seen, not expecting it to be realized ends up delaying decision-making on the policymaker. Even China took a long time to respond to the outbreak: it took 51 days from 1 December 2019 to 20 January 2020 for the Chinese central government to take complete control. Despite this, disease control strategies were quickly centralized by the government [63]. Including these strategies, early detection and isolation of cases were more effective in preventing more infections than travel restrictions and contact reductions [64]. On the other hand, we perform the same simulation to test the effect of citizens’ anticipation on the dynamics of the pandemic. However, there is no change large enough to be graphically perceived. This points to the conclusion that expectations about the realization of the pandemic are of vital importance when it comes to the government since its initial reaction depends on it.
Figure A2.
Unexpected vs. Expected Pandemic.
Appendix B. Mathematical Proofs
Proof of Proposition 1.
We want to find that makes contagion for A and I equal, therefore , that is:
or equivalently
(A3) However, since , for Equation (A3) to hold, it must be that
and that is precisely Equation (10). □
Proof of Proposition 2.
From the definition of in Equation (10):
(A4) and assuming that , i.e., that a higher actual effectiveness makes the perceive effectiveness weakly higher, then a sufficient condition for the expression in Equation (A4) to be positive is . Finally, note that the proof for the comparative statics of is completely analogous to that of , what concludes the proof. □
Proposition A2.
The threshold and fraction are given, respectively, by
(A5)
(A6)
Proof of Proposition A2.
Note that the threshold must be such that the agent is indifferent between the two actions, i.e.,
But of course, is endogenous, as it depends on the citizens’ behavior. Therefore, we have that
Therefore, is the solution to:
what in turn pins down in Equation (A6). □
Proof of Proposition A1.
First, we will prove that the two proposed equilibria are indeed sequential equilibria.
- (1)
Pooling equilibrium with Alarm: in this case, , and therefore and it must be the case that This is the condition for the democratic government, which implies the condition for the authoritarian government.
- (2)
Separating equilibrium in which the democratic government chooses Wait, and the authoritarian government chooses Alarm. In this case and , what implies :
- (3)
Pooling equilibrium in Waiting. In this case, , . The type that has the most incentives to deviate is authoritarian, so this equilibrium exists whenever
Moreover, we can rule out the separating equilibrium in which a democratic government chooses Alarm and an authoritarian government chooses Wait. In that case, the authoritarian government would benefit from deviating to Alarm (as that would induce citizens to believe it is a democratic government and protest with lower probability) and would derive the extra payoff of B. □
Appendix C. Additional Simulations
This appendix contains some additional simulations to those presented in the main text. Figure A3 shows then the variation in the proportion of cases (symptomatic and asymptomatic infected) in response to variations in the effectiveness of the lockdown measure, . As can be seen, an increase in efficiency translates into a “flattening” of the curve, reducing the rate at which the number of cases grows by affecting the infection rate.
Figure A3.
Endogenous lockdown efficacy. The role of the the relative contagion in the evolution of cases when the agent respects lockdown.
Figure A4 depicts two extreme scenarios taking government actions as exogenous: imposing lockdown during the entire pandemic or not imposing it at all during any period. In terms of health and social welfare, the first measure has a positive effect on the proportion of infected in reducing its upward trend.
Figure A4.
Exogenous lockdown vs. Non-lockdown.
Figure A5 depicts the effect of an increase in the cost heterogeneity of protective measures, c. It can be seen that an increase in cost dispersion results in a more rapid increase in the number of infected people when the mean population cost is low enough ( as, for the simulations, we have assumed that the cost follows a standard normal). The effect is mechanical since, with a higher dispersion, there are more people with a higher cost (the tails of the distribution widen) and fewer people end up being protected in comparison to a situation in which the dispersion is smaller.
Figure A5.
Disease dynamics with an increase in cost heterogeneity.
Figure A6 is similar to Figure 3 in the main text. However, in the first, the “timing effect” of a nudge on the effectiveness of protective measures is evaluated rather than its effect on a ‘shift’ in social norms. From both, we can draw the same conclusion: measures taken in the early stages of the pandemic have a greater effect in reducing the increase in cases.
Figure A6.
Timing effect in a nudge on protection efficacy.
Appendix D. Behavioral Channels
As we discussed in the paper, several factors studied in behavioral economics contributed to the scope and magnitude of the SARS-CoV-2 pandemic as we discussed in the Introduction. We provide here a detailed explanation of the channels we considered.
Optimism bias and overconfidence. People tend to be excessively optimistic about future events. Moreover, people are excessively confident in their own beliefs and skills to face future events [20]. In particular, citizens and politicians might believe that a serious and uncontrollable pandemic is less likely to occur than it is. This, in relation to our model, implies that , and . That is, both citizens and the government assign the pandemic a lower probability than it has. This, in turn, will affect the timing of public health policies to contain the spread of the virus. As we have seen in Section 4.2.3, the timing of policies is crucial to stop the evolution of cases. Therefore, a government who has more accurate beliefs about the objective probability of a pandemic will have a greater initial capacity to react. We could include another related bias within this behavioral bias: anumerism/failure to understand exponential growth. This implies that citizens and governments underestimate the potential of the pandemic to grow exponentially. As we can see in Equation (9), a lower value of implies giving less weight to the total number of deaths during the pandemic in the government’s utility. On the other hand, from a citizen’s point of view, this leads to the belief that both the severity of contracting the virus and the rate of contagion is lower than they are (see Table 3). In other words, the severity of the pandemic is again underestimated, causing citizens to protect themselves less than they should. As Soofi2020 noted, providing peer comparison feedback or communicating risks accurately are potentially helpful ways to tackle optimism and overconfidence in this context. In addition, emphasizing an adverse outcome resulting from COVID-19 that has occurred to individuals or a population similar to the target population could increase the tendency of citizens to protect themselves [65]. The use of role models such as celebrities could help promote preventive measures in adolescents because, although their risk of severe symptoms from COVID-19 is reduced [57], they still play a role in the transmission of the virus.
Availability heuristic, in which the probability of an unknown event (a severe pandemic COVID-19) is estimated using the probability of a known event (a severe pandemic of seasonal influenza). It has been proved that this behavioral bias affects the information that people refer to when deciding whether to engage in certain health-related behaviors. An example would be how recall of a drug advertisement affects the perceived prevalence of that disease [66], just as a physician diagnosing a patient might increase the likelihood of diagnosing the subsequent patient with the same illness [67]. In the present model, this bias could affect the citizens’ perceptions of the effectiveness of responsible behavior for oneself (), as well as and . Concerning the former, from the individuals’ point of view, COVID-19 preventive measures may be affected by their perception of their effectiveness. In this sense, lower values of this perception lead to a lower use of protection (Proposition 2). Therefore, the information people receive about a particular type of behavior becomes vital because it influences their health decisions. This behavioral bias suggests that creating a negative sentiment about adherence to COVID-19-related preventive measures may increase the perceived risk of non-adherence [1]. In Section 4.2.3, we further explore the comparison in terms of the effectiveness of public health policies that may affect this perception that individuals may have about the efficacy of the use of preventive measures versus government mandates. For the effect that the availability heuristic bias may have in terms of the model, we should also mention the consequent underestimation of the objective probability that the pandemic will occur. For example, despite initial fears that the H1N1 pandemic of 2009 had the same intensity as the Spanish flu, it turned out to be relatively mild, with an estimate of fewer than 300,000 deaths worldwide [68]. However, as far as the current pandemic is concerned, the opposite is true (it was initially underestimated).
Fallacy of lack of evidence, by which an absence of evidence for an event is interpreted as evidence for the absence of that event [21]. Again, this could lead to underestimating and .
Status quo bias, by which people tend to prefer the current baseline (or status quo) over any change in such a way that there is a risk of doing nothing in the face of such a novel event as the pandemic [22]. There are other connected biases such as anchoring and insufficient adjustment and loss aversion. These predict that people take the status quo as a reference point and any change from that reference point is either undervalued (reflected typically in an insufficient adjustment to the new situation) or perceived as a loss (which stimulates doing nothing), ref. [69]. In all the cases and are underestimated. Related to this, we have the omission bias, which is people’s tendency to prefer that if harm must happen, it does so because of a lack of action on their part, rather than due to an active choice they made [8].
Social influences have been extensively studied as a critical element in their effect on people’s choices and behaviors [23]. In particular, social norms are a significant determinant in the engagement of health-related decision-making, e.g., starting to drink alcohol and smoke cigarettes [70,71,72,73]. In the present model, social norms also influence the actions of individuals since they constitute a decisive factor in the take-up rate for COVID-19 preventive measures. A direct implication of this result is that when designing public policy to increase the number of people using protective measures, policymakers should consider that peers such as work colleagues, friends, and family affect the individual’s behavior. This effect is related to the status quo bias. For example, in the early stages of the pandemic, in those societies where the social norm did not contemplate the use of face masks, individuals were in an equilibrium in which there were insufficient incentives to start protecting themselves. (Spain, for example, is among those countries with a non-mask-wearing culture. In this country, evidence has been found that there is a profile of individuals who are more resistant to mask-wearing: young, educated, unconcerned with being infected, and with an introverted personality. On the other hand, the propensity to use masks is incredibly high among the elderly living in localities where mask-wearing behavior is popular [44].) This status quo was in part affected by social norms. (There is evidence that we can consider wearing a face mask as part of a social norm. For example, in Germany, a recent survey suggests that people who wear face masks in public view others who also wear them more favorably than those who do not [42]. In addition, those who report that their immediate circle, e.g., friends and family, wear masks at a higher rate are more likely to wear them as well [43].) However, as the authorities emphasized its use, behavior moved away from this equilibrium. Indeed, there is evidence that nudges (in the form of persuasive health communication) are effective when appealing to protect others. For example, in this regard, a message that emphasizes how COVID-19 threatens “your community” increases people’s intentions to wear a face mask [41]. About our model, this type of public policy would provoke a strengthening of social norms, which would be reflected in the parameter . As we have seen in Section 4.2.2, changes in the value of this parameter have a significant impact on the dynamics of the pandemic in terms, i.e., of the evolution of cases.
From these behavioral channels, we can group them according to the parameter they affect in our model: (1) the probability that citizens and government assign to the pandemic that we claim is smaller than the actual probability p; (2) the citizens’ perceptions of the effectiveness of responsible behavior: , might also be smaller than the actual effectiveness ; and (3) the social norm parameter that determines how strong social norms are (included in function , that depends implicitly on ) is a function on the social perception of the pandemic.
Author Contributions
Conceptualization, B.A.M.-L., D.J.-G. and J.-M.A.-P.; methodology, B.A.M.-L. and D.J.-G.; software, B.A.M.-L. and D.J.-G.; formal analysis, B.A.M.-L. and D.J.-G.; investigation, B.A.M.-L., D.J.-G. and J.-M.A.-P.; writing—original draft preparation, B.A.M.-L.; writing—review and editing, B.A.M.-L., D.J.-G. and J.-M.A.-P. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
The authors are making the code publicly available.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Blas A. Marin-Lopez gratefully acknowledges the financial support of the Spanish Ministry of Science, Innovation, and Universities (ECO2017-87069-P). David Jimenez-Gomez is grateful for the funding from the Ministry of Science and Innovation and the European Regional Development Fund (FEDER), through the PID2019-107081GB-I00 project; from the Ministry of Science and Innovation, through the project “Nudging applied to the improvement of regulation” (RED2018-102761-T); from the Valencian Community, through the Prometeo program PROMETEO/2021/073. José-María Abellán-Perpiñán is grateful for the funding from the Ministry of Science and Innovation and the European Regional Development Fund (FEDER) through the PID2019-104907GB-I00 project. He is also grateful for funding from Fundacion Seneca through the 20825/PI/18 project.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Soofi M., Najafi F., Karami-Matin B. Using Insights from Behavioral Economics to Mitigate the Spread of COVID-19. Appl. Health Econ. Health Policy. 2020;18:345–350. doi: 10.1007/s40258-020-00595-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haushofer J., Metcalf J.C.E. Combining Behavioral Economics and Infectious Disease Epidemiology to Mitigate the COVID-19 Outbreak. Volume 6. Princeton University; Princeton, NJ, USA: 2020. pp. 1–10. [Google Scholar]
- 3.Abellán Perpiñán J.M., Jimenez-Gomez D., del Llano-Señarís J. Economía de la Salud (y más) de la COVID-19. Asociación de Economía de la Salud (Barcelona); Barcelona, Spain: 2020. La gestión de la pandemia de SARS-CoV-2 según la economía del comportamiento. [Google Scholar]
- 4.Karing A. Social signaling and childhood immunization: A field experiment in Sierra Leone. University of California Berkeley. 2018. [(accessed on 1 May 2020)]. Available online: https://economics.yale.edu/sites/default/files/jmp_socialsignaling.pdf.
- 5.Pop-Eleches C., Thirumurthy H., Habyarimana J.P., Zivin J.G., Goldstein M.P., De Walque D., MacKeen L., Haberer J., Kimaiyo S., Sidle J., et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: A randomized controlled trial of text message reminders. Aids. 2011;25:825–834. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banerjee A.V., Duflo E., Glennerster R., Kothari D. Improving immunisation coverage in rural India: Clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ. 2010;340 doi: 10.1136/bmj.c2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Bavel J.J., Boggio P., Capraro V., Cichocka A., Cikara M., Crockett M., Crum A., Douglas K., Druckman J., Drury J., et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 8.Halpern S.D., Miller F.G. The Urge to Build More Intensive Care Unit Beds and Ventilators: Intuitive but Errant. Ann. Int. Med. 2020;173:302–303. doi: 10.7326/M20-2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray E.J. Epidemiology’s Time of Need: COVID-19 Calls for Epidemic-Related Economics. J. Econ. Perspect. 2020;34:105–120. doi: 10.1257/jep.34.4.105. [DOI] [Google Scholar]
- 10.Geoffard P.Y., Philipson T. Rational epidemics and their public control. Int. Econ. Rev. 1996;37:603–624. doi: 10.2307/2527443. [DOI] [Google Scholar]
- 11.Kremer M. Integrating behavioral choice into epidemiological models of AIDS. Q. J. Econ. 1996;111:549–573. doi: 10.2307/2946687. [DOI] [Google Scholar]
- 12.Greenwood J., Kircher P., Santos C., Tertilt M. An equilibrium model of the African HIV/AIDS epidemic. Econometrica. 2019;87:1081–1113. doi: 10.3982/ECTA11530. [DOI] [Google Scholar]
- 13.Auld M.C. Choices, beliefs, and infectious disease dynamics. J. Health Econ. 2003;22:361–377. doi: 10.1016/S0167-6296(02)00103-0. [DOI] [PubMed] [Google Scholar]
- 14.Eichenbaum M.S., Rebelo S., Trabandt M. The Macroeconomics of Epidemics. National Bureau of Economic Research; Cambridge, MA, USA: 2020. Technical Report. [Google Scholar]
- 15.Garibaldi P., Moen E.R., Pissarides C.A. Modelling contacts and transitions in the SIR epidemics model. Covid Econ. 2020;5:1–21. [Google Scholar]
- 16.Jones C.J., Philippon T., Venkateswaran V. Optimal Mitigation Policies in a Pandemic: Social Distancing and Working from Home. National Bureau of Economic Research; Cambridge, MA, USA: 2020. Technical Report. [Google Scholar]
- 17.Reluga T.C. Game Theory of Social Distancing in Response to an Epidemic. PLoS Comput. Biol. 2010;6:e1000793. doi: 10.1371/journal.pcbi.1000793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eksin C., Paarporn K., Weitz J.S. Systematic biases in disease forecasting—The role of behavior change. Epidemics. 2019;27:96–105. doi: 10.1016/j.epidem.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 19.OECD Regulatory Policy and COVID-19: Behavioural Insights for Fast-Paced Decision Making; Technical Report November; 2020. [(accessed on 14 April 2021)]. Available online: https://www.oecd.org/coronavirus/policy-responses/regulatory-policy-and-covid-19-behavioural-insights-for-fast-paced-decision-making-7a521805/
- 20.Lovallo D., Kahneman D. Delusions of success. Harv. Bus. Rev. 2003;81:56–63. [PubMed] [Google Scholar]
- 21.Altman D.G., Bland J.M. Statistics notes: Absence of evidence is not evidence of absence. BMJ. 1995;311:485. doi: 10.1136/bmj.311.7003.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Redelmeier D.A., Shafir E. Pitfalls of judgment during the COVID-19 pandemic. Lancet Public Health. 2020;5:e306–e308. doi: 10.1016/S2468-2667(20)30096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Becker G.S., Murphy K.M. Social Economics. Harvard University Press; Cambridge, MA, USA: 2009. [Google Scholar]
- 24.Davies N.G., Kucharski A.J., Eggo R.M., Gimma A., Edmunds W.J., Jombart T., O’Reilly K., Endo A., Hellewell J., Nightingale E.S., et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: A modelling study. Lancet Public Health. 2020;5:E375–E385. doi: 10.1016/S2468-2667(20)30133-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iwata K., Miyakoshi C. A Simulation on Potential Secondary Spread of Novel Coronavirus in an Exported Country Using a Stochastic Epidemic SEIR Model. J. Clin. Med. 2020;9:944. doi: 10.3390/jcm9040944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO . Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. World Health Organization; Geneve, Switzerland: 2020. Technical Report. [Google Scholar]
- 27.Nishiura H., Kobayashi T., Miyama T., Suzuki A., mok Jung S., Hayashi K., Kinoshita R., Yang Y., Yuan B., Akhmetzhanov A.R., et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int. J. Infect. Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peng L., Yang W., Zhang D., Zhuge C., Hong L. Epidemic Analysis of COVID-19 in China by Dynamical Modeling. medRxiv. 2020 doi: 10.1101/2020.02.16.20023465. [DOI] [Google Scholar]
- 29.Backer J.A., Klinkenberg D., Wallinga J. Incubation period of 2019 novel coronavirus (2019- nCoV) infections among travellers from Wuhan, China, 20 28 January 2020. Eurosurveillance. 2020;25:2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N., Flasche S., Clifford S., Pearson C.A., Munday J.D., et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giannitsarou C., Kissler S., Toxvaerd F. Waning immunity and the second wave: Some projections for SARS-CoV-2. Am. Econ. Rev. Insights. 2021;3:321–338. doi: 10.1257/aeri.20200343. [DOI] [Google Scholar]
- 32.Berger D.W., Herkenhoff K.F., Mongey S. An SEIR Infectious Disease Model with Testing and Conditional Quarantine. National Bureau of Economic Research; Cambridge, MA, USA: 2020. Technical Report. [Google Scholar]
- 33.Manski C.F., Molinari F. Estimating the COVID-19 infection rate: Anatomy of an inference problem. J. Econ. 2021;220:181–192. doi: 10.1016/j.jeconom.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Atkeson A. What Will Be the Economic Impact of COVID-19 in the US? Rough Estimates of Disease Scenarios. National Bureau of Economic Research; Cambridge, MA, USA: 2020. p. 25. (NBER Working Paper Series). Technical Report. [Google Scholar]
- 35.Stock J.H. Data Gaps and the Policy Response to the Novel Coronavirus. National Bureau of Economic Research; Cambridge, MA, USA: 2020. Technical Report. [Google Scholar]
- 36.Avery C., Bossert W., Clark A., Ellison G., Ellison S.F. An Economist’s Guide to Epidemiology Models of Infectious Disease. J. Econ. Perspect. 2020;34:79–104. doi: 10.1257/jep.34.4.79. [DOI] [Google Scholar]
- 37.Ferguson N., Laydon D., Nedjati Gilani G., Imai N., Ainslie K., Baguelin M., Bhatia S., Boonyasiri A., Cucunuba Perez Z., Cuomo-Dannenburg G., et al. Report 9: Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID19 Mortality and Healthcare Demand. Imperial College COVID-19 Response Team London; London, UK: 2020. [Google Scholar]
- 38.Acemoglu D., Chernozhukov V., Werning I., Whinston M.D. A Multi-Risk SIR Model with Optimally Targeted Lockdown. Am. Econ. Rev. Insights. 2021;3:487–502. doi: 10.1257/aeri.20200590. [DOI] [Google Scholar]
- 39.Bonell C., Michie S., Reicher S., West R., Bear L., Yardley L., Curtis V., Amlôt R., Rubin G.J. Harnessing behavioural science in public health campaigns to maintain ’social distancing’ in response to the COVID-19 pandemic: Key principles. J. Epidemiol. Community Health. 2020;74:617–619. doi: 10.1136/jech-2020-214290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mitze T., Kosfeld R., Rode J., Wälde K. Face masks considerably reduce COVID-19 cases in Germany. Proc. Natl. Acad. Sci. USA. 2020;117:32293–32301. doi: 10.1073/pnas.2015954117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pfattheicher S., Nockur L., Böhm R., Sassenrath C., Petersen M.B. The emotional path to action: Empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol. Sci. 2020;31:1363–1373. doi: 10.1177/0956797620964422. [DOI] [PubMed] [Google Scholar]
- 42.Betsch C., Korn L., Sprengholz P., Felgendreff L., Eitze S., Schmid P., Böhm R. Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proc. Natl. Acad. Sci. USA. 2020;117:21851–21853. doi: 10.1073/pnas.2011674117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goldberg M., Gustafson A., Maibach E., van der Linden S., Ballew M.T., Bergquist P., Kotcher J., Marlon J.R., Rosenthal S., Leiserowitz A. Social norms motivate COVID-19 preventive behaviors. PsyArXiv. 2020 doi: 10.31234/osf.io/9whp4. [DOI] [Google Scholar]
- 44.Barceló J., Sheen G.C.H. Voluntary adoption of social welfare-enhancing behavior: Mask-wearing in Spain during the COVID-19 outbreak. PLoS ONE. 2020;15:e0242764. doi: 10.1371/journal.pone.0242764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bokemper S.E., Cucciniello M., Rotesi T.E., Pin P., Malik A.A., Willebrand K., Paintsil E.E., Omer S.B., Huber G.A., Melegaro A. Beliefs about Mask Efficacy and the Effect of Social Norms on Mask Wearing Intentions for COVID-19 Risk Reduction. PLoS ONE. 2021;16:e0258282. doi: 10.1371/journal.pone.0258282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Howard J., Huang A., Li Z., Tufekci Z., Zdimal V., van der Westhuizen H.M., von Delft A., Price A., Fridman L., Tang L.H., et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA. 2021;118:e2014564118. doi: 10.1073/pnas.2014564118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang X., Ferro E.G., Zhou G., Hashimoto D., Bhatt D.L. Association between universal masking in a health care system and SARS-CoV-2 positivity among health care workers. JAMA. 2020;324:703–704. doi: 10.1001/jama.2020.12897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Y., Tian H., Zhang L., Zhang M., Guo D., Wu W., Zhang X., Kan G.L., Jia L., Huo D., et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: A cohort study in Beijing, China. BMJ Glob. Health. 2020;5:e002794. doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clapp P.W., Sickbert-Bennett E.E., Samet J.M., Berntsen J., Zeman K.L., Anderson D.J., Weber D.J., Bennett W.D. Evaluation of cloth masks and modified procedure masks as personal protective equipment for the public during the COVID-19 pandemic. JAMA Int. Med. 2021;181:463–469. doi: 10.1001/jamainternmed.2020.8168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization . Advice on the Use of Masks in the Context of COVID-19: Interim Guidance. World Health Organization; Geneve, Switzerland: 2020. [(accessed on 26 May 2022)]. Technical Report. Available online: https://apps.who.int/iris/handle/10665/332293. [Google Scholar]
- 51.Mahikul W., Chotsiri P., Ploddi K., Pan-Ngum W. Evaluating the impact of intervention strategies on the first wave and predicting the second wave of COVID-19 in thailand: A mathematical modeling study. Biology. 2021;10:80. doi: 10.3390/biology10020080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chernozhukov V., Kasahara H., Schrimpf P. Causal impact of masks, policies, behavior on early covid-19 pandemic in the U.S. J. Econ. 2021;220:23–62. doi: 10.1016/j.jeconom.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Summers J., Cheng H.Y., Lin H.H., Barnard L.T., Kvalsvig A., Wilson N., Baker M.G. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lancet Reg. Health West. Pac. 2020;4:100044. doi: 10.1016/j.lanwpc.2020.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhou R., Li F., Chen F., Liu H., Zheng J., Lei C., Wu X. Viral dynamics in asymptomatic patients with COVID-19. Int. J. Infect. Dis. 2020;96:288–290. doi: 10.1016/j.ijid.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abellán Perpiñán J.M., Cierco C., Jimenez-Gomez D. Nudges y la pandemia: Un análisis desde la economía y el derecho conductual. Gac. Sanit. 2022;36:93–96. doi: 10.1016/j.gaceta.2022.03.004. [DOI] [PubMed] [Google Scholar]
- 56.Laibson D. Golden eggs and hyperbolic discounting. Q. J. Econ. 1997;112:443–478. doi: 10.1162/003355397555253. [DOI] [Google Scholar]
- 57.European Centre for Disease Prevention and Control Risk Factors and Risk Groups. 2021. [(accessed on 1 May 2021)]. Available online: https://www.ecdc.europa.eu/en/covid-19/latest-evidence/risk-factors-risk-groups.
- 58.Aumann R.J. Agreeing to Disagree. Ann. Stat. 1976;4:1236–1239. doi: 10.1214/aos/1176343654. [DOI] [Google Scholar]
- 59.Pulejo, Massimo; Querubín, Pablo Electoral concerns reduce restrictive measures during the COVID-19 pandemic. J. Public Econ. 2021;198:104387. doi: 10.1016/j.jpubeco.2021.104387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sly L. Stirrings of Unrest around the World could Portend Turmoil as Economies Collapse. 2020. [(accessed on 17 May 2021)]. Available online: https://www.washingtonpost.com/world/coronavirus-protests-lebanon-india-iraq/2020/04/19/1581dde4-7e5f-11ea-84c2-0792d8591911_story.html.
- 61.Morris S., Shin H.S. Global Games: Theory and Applications. In: Dewatripont M., Hansen L.P., Turnovsky S.J., editors. Advances in Economics and Econometrics. Theory and Applications, Eighth World Congress (Seattle 2000) Volume 1. Econometric Society; Cambridge University Press; Cambridge, UK: 2003. pp. 56–103. Chapter 3. [Google Scholar]
- 62.Chilton S., Nielsen J.S., Wildman J. Beyond COVID-19: How the “dismal science” can prepare us for the future. Health Econ. 2020;29:851–853. doi: 10.1002/hec.4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu Y., Saltman R.B. Policy lessons from early reactions to the COVID-19 virus in China. Am. J. Public Health. 2020;110:1145–1148. doi: 10.2105/AJPH.2020.305732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lai S., Ruktanonchai N.W., Zhou L., Prosper O., Luo W., Floyd J.R., Wesolowski A., Santillana M., Zhang C., Du X., et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585:410–413. doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Matjasko J.L., Cawley J.H., Baker-Goering M.M., Yokum D.V. Applying behavioral economics to public health policy: Illustrative examples and promising directions. Am. J. Prevent. Med. 2016;50:S13–S19. doi: 10.1016/j.amepre.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.An S. Antidepressant direct-to-consumer advertising and social perception of the prevalence of depression: Application of the availability heuristic. Health Commun. 2008;23:499–505. doi: 10.1080/10410230802342127. [DOI] [PubMed] [Google Scholar]
- 67.Folkes V.S. The availability heuristic and perceived risk. J. Consum. Res. 1988;15:13–23. doi: 10.1086/209141. [DOI] [Google Scholar]
- 68.Esparza J. Lessons From History: What Can We Learn From 300 Years of Pandemic Flu That Could Inform the Response to COVID-19? Am. J. Public Health. 2020;110:1160–1161. doi: 10.2105/AJPH.2020.305761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kahneman D., Knetsch J.L., Thaler R.H. The endowment effect, loss aversion, and status quo bias. J. Econ. Perspect. 1991;5:193–206. doi: 10.1257/jep.5.1.193. [DOI] [Google Scholar]
- 70.DeCicca P., Kenkel D., Mathios A., Shin Y.J., Lim J.Y. Youth smoking, cigarette prices, and anti-smoking sentiment. Health Econ. 2008;17:733–749. doi: 10.1002/hec.1293. [DOI] [PubMed] [Google Scholar]
- 71.Hsieh C.S., van Kippersluis H. Smoking initiation: Peers and personality. Quant. Econ. 2018;9:825–863. doi: 10.3982/QE615. [DOI] [Google Scholar]
- 72.Fletcher J.M., Ross S.L. Estimating the effects of friends on health behaviors of adolescents. Health Econ. 2018;27:1450–1483. doi: 10.1002/hec.3780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marin-Lopez B.A. Risky Behavior Initiation with Behavioral Agents and Social Interactions. 2021. [(accessed on 17 May 2021)]. Available online: https://ssrn.com/abstract=3915368.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors are making the code publicly available.