Abstract
The adipocyte fatty-acid binding protein (A-FABP) is predominantly expressed in macrophages and adipocytes and is an essential mediator of inflammation and atherosclerosis pathogenesis. Atherosclerosis is an aggravating factor for peripheral arterial disease (PAD). Our study intended to study the association between PAD and serum A-FABP levels in type-2 diabetes mellitus (T2DM) patients. One hundred and twenty T2DM subjects were enrolled in the study. Fasting blood samples were collected to determine biochemical data and A-FABP levels. By the automatic oscillometric method, the ankle–brachial index (ABI) was measured. Low ABI was defined as any value < 0.9. Twenty participants with T2DM (16.7%) were included in the low ABI group. Low ABI T2DM participants had an increased mean body mass index, body fat mass, systolic blood pressure, C-reactive protein, urine albumin–creatinine ratio, and A-FABP levels compared to those in the normal ABI group. After variables significantly associated with PAD were adjusted by multivariate logistic regression analyses, circulating A-FABP levels (odds ratio [OR]: 1.138; 95 percent confidence interval [CI]: 1.023–1.266; p = 0.017) were identified as the independent marker of PAD. In conclusion, fasting serum A-FABP value has positive association with PAD in T2DM patients.
Keywords: ankle–brachial index, peripheral arterial disease, adipocyte fatty-acid binding protein, diabetes mellitus
1. Introduction
Type-2 diabetes mellitus (T2DM) is associated with various complications. Cardiovascular disease (CVD) causes more than 60% of the life-years lost from DM and is the main cause of disability and mortality among populations with T2DM [1,2]. In DM patients, the most common cardiovascular manifestations include peripheral arterial disease (PAD), coronary heart disease, and heart failure [3]. PAD, a vascular disease caused by systemic atherosclerosis, can induce peripheral ischemia and has a strong association with the increased prevalence of cardiovascular events [4,5]. Ankle–brachial index (ABI) is not only a valuable tool in diagnosing PAD, but is also a surrogate marker of cardiovascular events in the general and diseased populations [6]. DM, an important aggravating factor for PAD, also increases the restenosis risk and can diminish the effectiveness of percutaneous endovascular revascularization in PAD patients [7]. Diabetic patients have a 1.5- to 4.0-fold higher risk of PAD occurrence than individuals without DM [8,9]. PAD in DM usually affects younger patients and is commonly associated with rapid progression, multilevel artery stenosis and occlusions, especially below the knee, as well as serious comorbidities and mortality, compared to that in the general population [10]. A longitudinal cohort study reported by Leibson et al. demonstrated that DM subjects with PAD have a higher mortality rate than subjects with either DM or PAD [11]. A recent review study also stated the prominent association between frailty syndrome in DM patients and PAD, especially in the geriatric populations or subjects after amputation [12].
The adipocyte fatty-acid binding protein (A-FABP, also called FABP4), a 15-kDa member of the intracellular fatty-acid binding protein mainly expressed in adipose cells or macrophages, is associated with arterial stiffness, dysmetabolic syndrome, and CVD [13,14]. In animal models, the proximal aorta atherosclerotic lesion size was ameliorated in A-FABP/apolipoprotein-E double-knockout mice compared to that in apolipoprotein-E-deficient controls [15,16]. Moreover, A-FABP deficiency limited to macrophages markedly reduced the atherosclerotic lesion size in vivo compared to total A-FABP deficiency [16]. In line with these animal study results, a ten-year prospective study revealed that circulating A-FABP concentration was the main pathophysiological mediator of atherosclerosis and had a positive association with the long-term outcome in coronary artery disease (CAD) populations [17].
The PAD prevalence of DM patients varies from 20% to 30% depending on the research population [18]. Cross-sectional studies have revealed a correlation between A-FABP expression and T2DM. The A-FABP value is positively associated with microalbuminuria even in T2DM populations with preserved renal function [19]. Our previous publications also demonstrated that the A-FABP level had a positive association with arterial stiffness in patients who had undergone renal transplant and were on hemodialysis [20,21]. However, publications on the A-FABP level and PAD among populations with DM are lacking. Therefore, we evaluated various predictors of PAD development and examined their correlation with the circulating A-FABP level in participants with T2DM. We also examined whether elevated serum A-FABP concentration was independently associated with PAD using the ABI.
2. Materials and Methods
2.1. Study Population
From November 2014 to March 2015, 140 patients with T2DM were enrolled at a medical center in Hualien, Taiwan. Twenty participants were excluded due to the use of protease-activated receptor-1 antagonists (n = 5), or warfarin (n = 3), or acute infection (n = 2) during blood sampling, and refusal to offer informed consent (n = 10). Finally, 120 patients with T2DM were invited to this study. The Research Ethics Committee of Hualien Tzu Chi Hospital approved this study (IRB103-136-B). Every participant provided written informed consent before entering this study. In the morning, after the participants had sat for ten minutes, the blood pressure (BP) was determined by standard mercury sphygmomanometers. Systolic BP (SBP) and diastolic BP (DBP) were obtained every 5 min, 3 times, and averaged for further analyses. Hypertension was defined as BP values ≥ 140/90 mmHg, or using any antihypertensive medication over the past two weeks.
2.2. Anthropometric and Body Composition Analysis
The height and body weight of each patient were recorded to the 0.50 cm and 0.50 kg, respectively. We calculated the body mass index (BMI) as a ratio of weight and height squared (kg/m2). Body fat mass was measured by bioimpedance analysis (Biodynamic-450; Biodynamics Corporation, Seattle, USA) in accordance with the standard tetrapolar whole-body (hand-foot) technique [13,22].
2.3. Biochemical Analyses
An overnight-fasting 10 mL blood sample from each participant was collected and immediately centrifuged (3000× g, 10 min). Serum fasting glucose, glycated hemoglobin (HbA1c), total cholesterol, triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), blood urea nitrogen (BUN), creatinine, and C-reactive protein (CRP) levels were measured using a Siemens Advia 1800 autoanalyzer (Siemens Healthcare GmbH, Henkestr, Germany) [13,22,23]. In a random spot urine sample, we tested urine albumin–creatinine ratio (UACR). We measured serum A-FABP concentrations via commercially available enzyme immunoassay kits (SPI-BIO, Montigny-le-Bretonneux, France) [13,22]. The intra- and inter-assay coefficients of variation were 6.6% and 5.1%, respectively. Using the Chronic Kidney Disease Epidemiological Collaboration (CKD-EPI) equation, the estimated glomerular filtration rate was calculated [24].
2.4. Ankle–Brachial Index Measurements
We measured ABI values with an automatic machine (VaSera VS-1000, Fukuda Denshi Co., Ltd., Tokyo, Japan) which recorded both the arm and ankle BP simultaneously with the oscillometric method [23]. The occlusive monitoring cuffs were tightly placed on four limbs, and heart sound and electrocardiographic data were recorded in the rest supine position for 10 min during the ABI measurement. The ABI value was determined as the SBP ratio of ankle to brachial, while the lower ankle SBP value was used for data analysis. We recorded the parameters for both lower extremities of each patient repeatedly and calculated the mean value. An ABI threshold of 0.9 has been used for PAD diagnosis in a previous study [25]. In this study, the low ABI group consisted of patients with a right or left ABI value < 0.9, and those whose values ≥ 0.9 were defined as the control group, as in previous work [23].
2.5. Statistical Analysis
The Kolmogorov–Smirnov test was used to determine whether the data are normally distributed. Continuous variables with normal distribution were shown as the mean ± standard deviation and were compared by using Student’s t-test. Non-normally distributed variables were reported by the median (interquartile range) and examined via the Mann–Whitney U test (BUN, creatinine, fasting glucose, HbA1c, TG, and UACR). We used the χ2 test for categorical variables analysis. Variables significantly associated with PAD among T2DM populations were tested for multivariate logistical regression analysis (adopted factors: BMI, body fat mass, SBP, CRP, UACR, and A-FABP). The association between A-FABP concentrations and clinical variables was evaluated using the nonparametric Spearman’s rank correlation coefficient. The area under the receiver operating characteristic (ROC) curve was analyzed to identify the A-FABP level that predicts PAD in T2DM patients. We used SPSS Statistics 19.0 software for data analyses. A p-value of 0.05 or lower was considered significant.
3. Results
The demographic, clinical, and biochemical information of the 120 enrolled patients with T2DM is shown in Table 1. In total, 75 males and 45 female participated in the study, and 58 patients had hypertension (48.3%). Typical risk factors for CVD and atherosclerosis were highly prevalent in our study population. The low ABI group comprised 20 patients with T2DM (16.7%). DM subjects within the low ABI group had higher BMI (p = 0.037), body fat mass (p = 0.019), SBP (p = 0.002), CRP (p < 0.001), UACR (p = 0.001), and A-FABP (p < 0.001) values than those within the normal ABI group. Medications used by the study participants included statins (n = 56; 46.7%), fibrates (n = 4; 3.3%), metformin (n = 66; 55.0%), sulfonylurea (n = 68; 56.7%), dipeptidyl peptidase-4 inhibitor (n = 71; 59.2%), and insulin (n = 31; 25.8%). No statistically significant differences existed between the patients with low and normal ABI values regarding sex, comorbid conditions with hypertension, the use of anti-hyperlipidemic medications, or the anti-diabetic medications usage, such as statins, fibrates, metformin, sulfonylureas, dipeptidyl peptidase-4 inhibitors, and insulin.
Table 1.
Clinical variables at low ABI and control group in 120 type-2 diabetes mellitus patients.
| Variables | All Patients (n = 120) |
Control Group (n = 100) |
Low ABI Group (n = 20) |
p Value |
|---|---|---|---|---|
| Age (years) | 61.50 ± 12.74 | 61.32 ± 11.96 | 62.40 ± 16.38 | 0.731 |
| Height (cm) | 162.97 ± 8.27 | 163.23 ± 8.40 | 161.68 ± 7.63 | 0.444 |
| BW (kg) | 71.88 ± 14.35 | 71.10 ± 13.36 | 75.75 ± 18.49 | 0.188 |
| Body mass index (kg/m2) | 26.94 ± 4.25 | 26.58 ± 3.90 | 28.75 ± 5.45 | 0.037 * |
| Body fat mass (%) | 30.23 ± 7.28 | 29.54 ± 7.21 | 33.70 ± 6.75 | 0.019 * |
| Left ABI | 1.06 (1.00–1.13) | 1.09 (1.03–1.14) | 0.89 (0.82–0.90) | <0.001 * |
| Right ABI | 1.08 (1.02–1.14) | 1.10 (1.06–1.15) | 0.92 (0.88–0.96) | <0.001 * |
| SBP (mmHg) | 139.31 ± 18.87 | 136.92 ± 16.85 | 151.25 ± 23.89 | 0.002 * |
| DBP (mmHg) | 81.32 ± 10.25 | 80.77 ± 9.36 | 84.05 ± 13.86 | 0.193 |
| Total cholesterol (mg/dL) | 160.54 ± 30.39 | 159.29 ± 29.51 | 166.80 ± 34.58 | 0.315 |
| Triglyceride (mg/dL) | 109.00 (78.50–182.00) | 110.50 (75.50–187.25) | 103.00 (86.75–172.50) | 0.863 |
| HDL-C (mg/dL) | 46.30 ± 12.36 | 46.43 ± 12.37 | 45.65 ± 12.63 | 0.798 |
| LDL-C (mg/dL) | 99.17 ± 26.99 | 98.66 ± 25.67 | 101.70 ± 33.50 | 0.648 |
| Fasting glucose (mg/dL) | 138.00 (119.50–171.75) | 138.00 (121.00–175.00) | 136.50 (102.00–169.00) | 0.481 |
| Glycated hemoglobin (%) | 7.20 (6.50–9.00) | 7.20 (6.50–8.88) | 7.25 (6.15–9.85) | 0.972 |
| BUN (mg/dL) | 15.00 (12.00–18.00) | 15.00 (12.00–18.00) | 18.00 (12.25–19.00) | 0.282 |
| Creatinine (mg/dL) | 0.8 (0.70–1.00) | 0.80 (0.70–1.00) | 0.80 (0.70–0.90) | 0.718 |
| eGFR (mL/min) | 91.12 ± 26.39 | 91.34 ± 26.00 | 90.00 ± 28.93 | 0.837 |
| C-reactive protein (mg/dL) | 0.08 (0.05–0.23) | 0.06 (0.05–0.15) | 0.51 (0.11–1.02) | <0.001 * |
| UACR (mg/g) | 14.00 (7.13–54.27) | 12.19 (6.06–33.55) | 67.68 (22.99–182.07) | 0.001 * |
| A-FABP (ng/mL) | 21.80 ± 9.02 | 19.88 ± 6.70 | 31.44 ± 12.61 | <0.001 * |
| Male, n (%) | 75 (62.5) | 65 (65.0) | 10 (50.0) | 0.206 |
| Hypertension, n (%) | 58 (48.3) | 46 (46.0) | 12 (60.0) | 0.253 |
| Statin usage, n (%) | 56 (46.7) | 45 (45.0) | 11 (55.0) | 0.413 |
| Fibrate usage, n (%) | 4 (3.3) | 4 (4.0) | 0 (0) | 0.363 |
| Metformin usage, n (%) | 66 (55.0) | 56 (56.0) | 10 (50.0) | 0.622 |
| Sulfonylurea usage, n (%) | 68 (56.7) | 54 (54.0) | 14 (70.0) | 0.187 |
| DDP-4 inhibitor usage, n (%) | 71 (59.2) | 60 (60.0) | 11 (55.0) | 0.678 |
| Insulin usage, n (%) | 31 (25.8) | 26 (26.0) | 5 (25.0) | 0.926 |
Continuous variables are shown as the mean ± standard deviation and tested by Student’s independent t-test. Non-normally distributed data were reported by the median (interquartile range); they were tested by the Mann–Whitney U test. Categorical variables were examed by the χ2 test and are reported as numbers (%). ABI, ankle–brachial index; BW, body weight; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; BUN, blood urea nitrogen; eGFR, estimated glomerulus filtration rate; UACR, urine albumin–creatinine ratio; A-FABP, adipocyte fatty-acid binding protein; DDP-4, dipeptidyl peptidase-4. * A p-value of 0.05 or lower was considered significant.
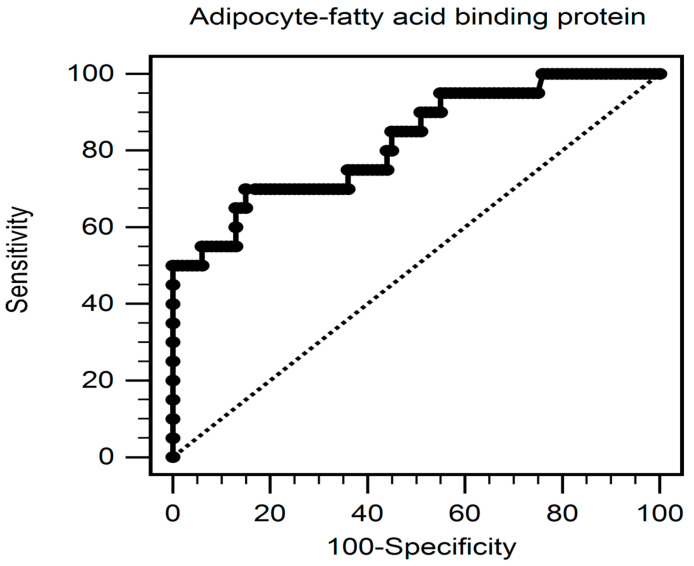
Adjustment was made for factors significantly associated with PAD (BMI, body fat mass, SBP, CRP, UACR, and A-FABP) in the multivariate logistic regression analysis. The analysis showed that elevated circulating A-FABP level (odds ratio [OR]: 1.138; 95% confidence interval [CI]: 1.023–1.266; p = 0.017), SBP (OR: 1.041; 95% CI: 1.004–1.079; p = 0.028), and CRP level (per 0.1 mg/dL increment, OR: 1.275; 95% CI: 1.067–1.523; p = 0.008) were risk factors for PAD in T2DM subjects (Table 2). The ROC curve diagram for the PAD prediction represented that the area under the ROC curve for the parameter A-FABP level was 0.823 (95% CI, 0.743–0.887; p < 0.001; Figure 1).
Table 2.
Multivariate logistic regression analysis of the variables associated with peripheral arterial disease in 120 patients with diabetes mellitus.
| Variables | Odds Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|
| Adipocyte fatty-acid binding protein, 1 ng/mL | 1.138 | 1.023–1.266 | 0.017 * |
| Systolic blood pressure, 1 mmHg | 1.041 | 1.004–1.079 | 0.028 * |
| C-reactive protein, 0.1 mg/dL | 1.275 | 1.067–1.523 | 0.008 * |
| Body mass index, 1 kg/m2 | 0.974 | 0.808–1.174 | 0.780 |
| Body fat mass, 1 % | 1.012 | 0.912–1.123 | 0.823 |
| Urine albumin-to-creatinine ratio, 1 mg/g | 0.999 | 0.998–1.001 | 0.287 |
Data were analyzed using multivariate logistic regression (adopted factors: body fat mass, body mass index, C-reactive protein, systolic blood pressure, urine albumin–creatinine ratio, and adipocyte fatty-acid binding protein). * p < 0.05 was statistically significant.
Figure 1.
The area under the receiver operating characteristic curve represents the diagnostic power of the adipocyte fatty-acid binding protein value for predicting peripheral artery disease in type-2 diabetes mellitus subjects.
Table 3 shows the correlation between serum A-FABP and clinical variables by Spearman’s correlation analysis. First, left, and right ABI were negative correlated with A-FABP (r = –0.418 and –0.474, respectively, both p < 0.001). Second, serum A-FABP was found to be positively correlated with BMI (r = 0.271, p = 0.003), body fat mass (r = 0.379, p < 0.001), SBP (r = 0.249, p = 0.006), TG (r = 0.319, p < 0.001), CRP (r = 0.382, p < 0.001), and UACR (r = 0.362, p < 0.001) but negatively associated with HDL-C (r = −0.186, p = 0.006), and eGFR (r = −0.442, p < 0.001).
Table 3.
Spearman correlation coefficients between adipocyte fatty-acid binding protein and clinical variables in 120 type-2 diabetes mellitus patients.
| Variables | Spearman Coefficient of Correlation | p Value |
|---|---|---|
| Age (years) | 0.088 | 0.340 |
| Body mass index (kg/m2) | 0.271 | 0.003 * |
| Body fat mass (%) | 0.379 | <0.001 * |
| Left ankle–brachial index | –0.418 | <0.001 * |
| Right ankle–brachial index | −0.474 | <0.001 * |
| Systolic blood pressure (mmHg) | 0.249 | 0.006 * |
| Diastolic blood pressure (mmHg) | 0.116 | 0.208 |
| Total cholesterol (mg/dL) | 0.081 | 0.378 |
| Triglyceride (mg/dL) | 0.319 | <0.001 * |
| HDL-C (mg/dL) | –0.186 | 0.042 * |
| LDL-C (mg/dL) | 0.048 | 0.606 |
| Fasting glucose (mg/dL) | 0.165 | 0.072 |
| eGFR (mL/min) | –0.249 | 0.006 * |
| C-reactive protein (mg/dL) | 0.382 | <0.001 * |
| UACR (mg/g) | 0.362 | <0.001 * |
Analysis of data was performed using the Spearman correlation analysis. HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; eGFR, estimated glomerulus filtration rate; UACR, urine albumin–creatinine ratio. * p < 0.05 was considered statistically significant.
4. Discussion
Our cross-sectional study of 120 patients with T2DM showed that serum A-FABP concentrations, together with SBP and CRP, were independent predictors of PAD diagnosed based on ABI values.
Systemic atherosclerosis events are the most important factor determining PAD prevalence and are increasing in number. It is estimated that 200 million patients are affected by PAD around the world [26]. PAD can be detected by various methods; however, ABI measurement is the noninvasive, standard approach for the diagnosis of PAD [27]. In the general population, ABI values less than 0.9 has been regarded as a predictor to diagnose PAD with 95% sensitivity [28]. PAD has high prevalence and morbidity rates and is characterized by high risk of CVD, amputation, and even death [5].
Studies have identified many established risk factors for PAD development, including smoking, DM, hypertension, obesity, dyslipidemia, aging, and chronic kidney disease [8,29,30], all of which induce a chronic inflammatory response, thereby aggravating the progression of atherosclerosis. DM is the main risk factor for PAD, and according to the Framingham Heart Study, twenty percent of patients with PAD symptoms are diagnosed with DM [31]. A positive association has been indicated between obesity and PAD in both the general population and hemodialysis patients [32], and it has even been reported that obesity is associated with PAD severity [33]. Previous researchers have also found that SBP value is significantly increased in PAD compared to non-PAD groups [34]. This finding likely stems from changes in the Windkessel effect, which explains arterial blood perfusion toward the periphery. With the progression of atherosclerosis, hardening of the vascular wall leads to elevated SBP and reduces the Windkessel effect [35]. Recently, a meta-analysis reported that even mild-to-moderate chronic kidney disease might increase the risk of PAD. Besides, UACR significantly improves PAD risk discrimination and prediction of amputation in addition to traditional parameters [30]. In line with these publications, our current study also provides clinical evidence that higher BMI, body fat mass, SBP, and UACR values in T2DM patients with low ABI are associated with PAD.
PAD reflects systemic atherosclerosis, a complicated process involving oxidative stress, endothelial dysfunction, vascular smooth muscle cell activation, changes in matrix metabolism, platelet activation, and lipid disturbances [36]. The ABI, a widely used, non-invasive, standard tool for PAD diagnosis, is a reliable and highly reproducable method to detect asymptomatic PAD in the early stage. Low ABI values are associated with many CVD risks in the general population and T2DM subjects [6]. A-FABP is traditionally regarded as a biomarker expressed predominantly in adipose tissue and macrophages. It is derived from monocytes activated by PPAR agonists and oxidized LDL. A-FABP is an important mediator of inflammation and is involved in the pathogenesis of obesity-related insulin resistance, as well as the development of metabolic syndrome and T2DM [37]. Previous reports demonstrated that elevated circulating A-FABP values positively correlated with the low HDL-C level and high BMI, waist circumference, BP, total cholesterol, TG, LDL-C, insulin levels, and homeostasis model assessment-estimated insulin resistance (HOMA-IR) values [38]. Our present study also revealed that A-FABP was positively correlated with BMI, body fat mass, SBP, triglyceride, CRP, and UACR but negatively associated with HDL-C and eGFR. This may explain the effect of A-FABP leading to metabolic deterioration, thereby aggravating atherosclerosis [39]. Results from pharmacological intervention studies in animal models indicate that the serum A-FABP level is a central player in inducing insulin resistance, increasing plasma lipid levels, and promoting the formation of vulnerable atherosclerotic plaques via multiple mechanisms such as autocrine or systemic endocrine pathways in macrophages [40]. A study using different mouse models demonstrated that a specific orally administered A-FABP antagonist was highly effective in the T2DM and atherosclerosis treatment [41]. Recent publications in humans also revealed an association between A-FABP and atherosclerotic diseases and the inflammatory status of the arterial system [42,43]. Administration of an A-FABP antagonist also contributes to the elimination and reduced development of atherosclerotic plaques in vitro and in vivo [41]. A-FABP has been linked to increased atherosclerotic plaque burden in CAD patients and has a positive association with the intima–media thickness of carotid artery in Chinese adults, as assessed by ultrasound [44,45]. Likewise, the study by Bao and his colleagues revealed that circulating A-FABP level is positively correlated with the severity of atherosclerotic disease and a prominent aggravating factor for the CAD occurrence in Chinese women [46]. Inflammation measured by CRP levels as a parameter of PAD occurrence has been reported in the inter-scientific consensus on PAD management [42]. Consistent with prior published data, we found that CRP concentrations have a positive correlation with low ABI values in T2DM patients. Serum CRP represents the primary cause of increased inflammation, which may be a causal predictor of plaque formation and arterial atherosclerotic disease. Our study revealed that circulating A-FABP and CRP levels were independent predictors of PAD in T2DM populations in multivariate logistic regression analyses even after adjusting for variables significantly associated with PAD. Moreover, a significant negative correlation between A-FABP and bilateral ABI values was noted by Spearman’s correlation analysis. These data indicate that A-FABP-related inflammatory responses may aggravate atherosclerotic progression in PAD. Thus, A-FABP levels could be a more specific PAD marker to evaluate ABI in patients with T2DM [47].
Our research has limitations. First, this research was conducted as a single-center, cross-sectional study without the control group, and various lifestyle habits that may affect PAD occurrence, such as smoking and alcohol consumption, were not recorded [48,49]. This lack of information may bias our research, and further longitudinal studies are required to validate our results. Second, the sample of 120 patients with DM in one medical center does not represent of the whole population of Taiwan or all ethnicities. Although a previous study by Ding et al. also investigated the relationship between circulating A-FABP levels and PAD in 488 Chinese T2DM subjects with a larger sample size than our present study, they used ultrasound examination for diagnosing PAD stenosis [47]. Operator-dependent ultrasound data may influence the study result. Our study used ABI, the widely used and valuable diagnostic tool for PAD diagnosis, which is more reproducible and reliable than ultrasound examination and can detect PAD in the early stage. Further studies with larger sample sizes including hospitals across multiple cities or even multiple countries are warranted to establish a more definite conclusion. Third, according to review articles, antilipidemic agents like statins and new antidiabetic drugs such as DPP4i decrease the prevalence of arterial stiffness and cardiovascular risk [50,51]. However, no significant differences between groups with low and normal ABI values were found in our study in relation to the drugs used, though this may be related to the small sample size and poor drug compliance of some patients. Thus, further investigations of the relationship between the abovementioned medications and PAD in patients with T2DM are needed. Fourth, although the ABI plays a vital role in the diagnosis of PAD, ABI may be falsely elevated due to calcification of the artery’s middle layer wall in the DM population. Some studies had recommended using the to–-brachial index (TBI) instead of the ABI for the PAD diagnosis in DM patients [12]. However, the TBI value of PAD diagnosed among DM subjects is still unclear. More research is needed to evaluate the application of TBI in the DM population.
5. Conclusions
Our present study showed, for the first time, that the fasting serum A-FABP level is positively associated with PAD. Moreover, in T2DM populations, fasting serum A-FABP levels are regarded as a consistent and significant predictor associated with PAD determined by ABI.
Author Contributions
Conceptualization, B.-G.H. and M.-C.C.; data curation, C.-Y.M. and D.-A.W.; formal analysis, B.-G.H. and M.-C.C.; funding acquisition, M.-C.C.; investigation, C.-Y.M. and D.-A.W.; methodology, B.-G.H. and M.-C.C.; supervision, M.-C.C.; writing—original draft, C.-Y.M.; writing—review and editing, B.-G.H. and M.-C.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The Protection of the Human Subjects Institutional Review Board, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation approved this study on 1 January 2015 (REC No.: IRB103-136-B).
Informed Consent Statement
Written informed consent was obtained from all patients enrolled in this research.
Data Availability Statement
All data which support the findings of our study are included in this article.
Conflicts of Interest
The authors declare no conflict to interest.
Funding Statement
This work was supported by Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan, Grant Number TCRD109-71.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harding J.L., Pavkov M.E., Magliano D.J., Shaw J.E., Gregg E.W. Global trends in diabetes complications: A review of current evidence. Diabetologia. 2019;62:3–16. doi: 10.1007/s00125-018-4711-2. [DOI] [PubMed] [Google Scholar]
- 2.Rao Kondapally Seshasai S., Kaptoge S., Thompson A., Di Angelantonio E., Gao P., Sarwar N., Whincup P.H., Mukamal K.J., Gillum R.F., Holme I., et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 2011;364:829–841. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glovaci D., Fan W., Wong N.D. Epidemiology of diabetes mellitus and cardiovascular disease. Curr. Cardiol. Rep. 2019;21:21. doi: 10.1007/s11886-019-1107-y. [DOI] [PubMed] [Google Scholar]
- 4.Fowkes F.G., Murray G.D., Butcher I., Heald C.L., Lee R.J., Chambless L.E., Folsom A.R., Hirsch A.T., Dramaix M., deBacker G., et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: A meta-analysis. JAMA. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marone E.M., Cozzolino P., Ciampichini R., Chiodini V., Ferraresi R., Rinaldi L.F., Mantovani L.G., Cesana G. Peripheral arterial disease in diabetic patients: A long-term population-based study on occurrence, outcomes and cost. J. Cardiovasc. Surg. 2018;59:572–579. doi: 10.23736/S0021-9509.18.10405-8. [DOI] [PubMed] [Google Scholar]
- 6.Lia A.C., Maria G.G., Marc C.C., Jordi B., Anna P., Ruth M.L., Marc E.B., Dídac P., Lourdes C., Rafel R. Role of low ankle-brachial index in cardiovascular and mortality risk compared with major risk conditions. J. Clin. Med. 2019;8:870. doi: 10.3390/jcm8060870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grzegorz K.J., Natalia P., Grzegorz C., Agata S. Pathogenesis and clinical significance of in-stent restenosis in patients with diabetes. Int. J. Environ. Res. Public Health. 2021;18:11970. doi: 10.3390/ijerph182211970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tavintharan S., Cheung N., Lim S.C., Tay W., Shankar A., Shyong Tai E., Wong T.Y. Prevalence and risk factors for peripheral artery disease in an Asian population with diabetes mellitus. Diab. Vasc. Dis. Res. 2009;6:80–86. doi: 10.1177/1479164109336043. [DOI] [PubMed] [Google Scholar]
- 9.Criqui M.H., Aboyans V. Epidemiology of peripheral artery disease. Circ. Res. 2015;116:1509–1526. doi: 10.1161/CIRCRESAHA.116.303849. [DOI] [PubMed] [Google Scholar]
- 10.Thejasvi T., Caitlin E.K., Ehrin J.A. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J. Diabetes. 2015;6:961–969. doi: 10.4239/wjd.v6.i7.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leibson C.L., Ransom J.E., Olson W., Zimmerman B.R., O’Fallon W.M., Palumbo P.J. Peripheral arterial disease, diabetes, and mortality. Diabetes Care. 2004;27:2843–2849. doi: 10.2337/diacare.27.12.2843. [DOI] [PubMed] [Google Scholar]
- 12.Grzegorz K.J., Natalia P., Grzegorz C., Agata S. Chronic Lower extremity ischemia and its association with the frailty syndrome in patients with diabetes. Int. J. Environ. Res. Public Health. 2020;17:9339. doi: 10.3390/ijerph17249339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen M.C., Hsu B.G., Lee C.J., Yang C.F., Wang J.H. High serum adipocyte fatty acid binding protein level as a potential biomarker of aortic arterial stiffness in hypertensive patients with metabolic syndrome. Clin. Chim. Acta. 2017;473:166–172. doi: 10.1016/j.cca.2017.08.030. [DOI] [PubMed] [Google Scholar]
- 14.Furuhashi M., Saitoh S., Shimamoto K., Miura T. Fatty acid-binding protein 4 (FABP4): Pathophysiological insights and potent clinical biomarker of metabolic and cardiovascular diseases. Clin. Med. Insights Cardiol. 2014;8:23–33. doi: 10.4137/CMC.S17067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boord J.B., Maeda K., Makowski L., Babaev V.R., Fazio S., Linton M.F., Hotamisligil G.S. Adipocyte fatty acid-binding protein, aP2, alters late atherosclerotic lesion formation in severe hypercholesterolemia. Arterioscler. Thromb. Vasc. Biol. 2002;22:1686–1691. doi: 10.1161/01.ATV.0000033090.81345.E6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makowski L., Boord J.B., Maeda K., Babaev V.R., Uysal K.T., Morgan M.A., Parker R.A., Suttles J., Fazio S., Hotamisligil G.S., et al. Lack of macrophage fatty-acid-binding protein aP2 protects mice deficient in apolipoprotein E against atherosclerosis. Nat. Med. 2001;7:699–705. doi: 10.1038/89076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Eynatten M., Breitling L.P., Roos M., Baumann M., Rothenbacher D., Brenner H. Circulating adipocyte fatty acid-binding protein levels and cardiovascular morbidity and mortality in patients with coronary heart disease: A 10-year prospective study. Arterioscler. Thromb. Vasc. Biol. 2012;32:2327–2335. doi: 10.1161/ATVBAHA.112.248609. [DOI] [PubMed] [Google Scholar]
- 18.Yang S.L., Zhu L.Y., Han R., Sun L.L., Li J.X., Dou J.T. Pathophysiology of peripheral arterial disease in diabetes mellitus. J. Diabetes. 2017;9:133–140. doi: 10.1111/1753-0407.12474. [DOI] [PubMed] [Google Scholar]
- 19.Seo D.H., Nam M., Jung M., Suh Y.J., Ahn S.H., Hong S., Kim S.H. Serum levels of adipocyte fatty acid-binding protein are associated with rapid renal function decline in patients with type 2 diabetes mellitus and preserved renal function. Diabetes Metab. J. 2020;44:875–886. doi: 10.4093/dmj.2019.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen Y.C., Hsu B.G., Lee C.J., Ho C.C., Ho G.J., Lee M.C. Serum adipocyte fatty acid-binding protein level is associated with arterial stiffness quantified with cardio-ankle vascular index in kidney transplant patients. Clin. Exp. Nephrol. 2018;22:188–195. doi: 10.1007/s10157-017-1438-1. [DOI] [PubMed] [Google Scholar]
- 21.Lai Y.H., Lin Y.L., Wang C.H., Kuo C.H., Hsu B.G. Positive association of serum adipocyte fatty acid binding protein level with peripheral artery disease in hemodialysis patients. Ther. Apher. Dial. 2020;24:300–306. doi: 10.1111/1744-9987.13431. [DOI] [PubMed] [Google Scholar]
- 22.Li J.C., Wu D.A., Hou J.S., Subeq Y.M., Chen H.D., Hsu B.G. High serum adipocyte fatty acid binding protein is associated with metabolic syndrome in patients with type 2 diabetes. J. Diabetes Res. 2016;2016:8380279. doi: 10.1155/2016/8380279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsu B.G., Lee C.J., Yang C.F., Chen Y.C., Wang J.H. High serum resistin levels are associated with peripheral artery disease in the hypertensive patients. BMC Cardiovasc. Disord. 2017;17:80. doi: 10.1186/s12872-017-0517-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levey A.S., Stevens L.A., Schmid C.H., Zhang Y.L., Castro A.F., III, Feldman H.I., Kusek J.W., Eggers P., Van Lente F., Greene T., et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferreira A.C., Macedo F.Y.B. A review of simple, non-invasive means of assessing peripheral arterial disease and implications for medical management. Ann. Med. 2010;42:139–150. doi: 10.3109/07853890903521070. [DOI] [PubMed] [Google Scholar]
- 26.Fowkes F.G., Rudan D., Rudan I., Aboyans V., Denenberg J.O., McDermott M.M., Norman P.E., Sampson U.K., Williams L.J., Mensah G.A., et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet. 2013;382:1329–1340. doi: 10.1016/S0140-6736(13)61249-0. [DOI] [PubMed] [Google Scholar]
- 27.Duprez D.A., De Buyzere M.M., De Bruyne L., Clement D.L., Cohn J.N. Small and large artery elasticity indices in peripheral arterial occlusive disease (PAOD) Vasc. Med. 2001;6:211–214. doi: 10.1177/1358836X0100600402. [DOI] [PubMed] [Google Scholar]
- 28.Lai Y.H., Lin Y.L., Wang C.H., Kuo C.H., Hsu B.G. Negative correlation of serum adiponectin level with peripheral artery occlusive disease in hemodialysis patients. Tzu Chi Med. J. 2020;32:70–74. doi: 10.4103/tcmj.tcmj_19_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norgren L., Hiatt W.R., Dormandy J.A., Nehler M.R., Harris K.A., Fowkes F.G., Bell K., Caporusso J., Durand-Zaleski I., Komori K., et al. Inter-society consensus for the management of peripheral arterial disease (TASC II) J. Vasc. Surg. 2007;45((Suppl. S)):S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 30.Matsushita K., Ballew S.H., Coresh J., Arima H., Ärnlöv J., Cirillo M., Ebert N., Hiramoto J.S., Kimm H., Shlipak M.G., et al. Measures of chronic kidney disease and risk of incident peripheral artery disease: A collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 2017;5:718–728. doi: 10.1016/S2213-8587(17)30183-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murabito J.M., D’Agostino R.B., Silbershatz H., Wilson W.F. Intermittent claudication. A risk profile from The Framingham Heart Study. Circulation. 1997;96:44–49. doi: 10.1161/01.CIR.96.1.44. [DOI] [PubMed] [Google Scholar]
- 32.Hung P.H., Tsai H.B., Lin C.H., Hung K.Y. Abdominal obesity is associated with peripheral artery disease in hemodialysis patients. PLoS ONE. 2013;8:e67555. doi: 10.1371/journal.pone.0067555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zeymer U., Parhofer K.G., Pittrow D., Binz C., Schwertfeger M., Limbourg T., Röther J. Risk factor profile, management and prognosis of patients with peripheral arterial disease with or without coronary artery disease: Results of the prospective German REACH registry cohort. Clin. Res. Cardiol. 2009;98:249–256. doi: 10.1007/s00392-009-0754-1. [DOI] [PubMed] [Google Scholar]
- 34.Kiuchi S., Hisatake S., Watanabe I., Toda M., Kabuki T., Oka T., Dobashi S., Ikeda T., Kiuchi S., Hisatake S., et al. Pulse pressure and upstroke time are useful parameters for the diagnosis of peripheral artery disease in patients with normal ankle brachial index. Cardiol. Res. 2016;7:161–166. doi: 10.14740/cr508e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reymond P., Westerhof N., Stergiopulos N. Systolic hypertension mechanisms: Effect of global and local proximal aorta stiffening on pulse pressure. Ann. Biomed. Eng. 2012;40:742–749. doi: 10.1007/s10439-011-0443-x. [DOI] [PubMed] [Google Scholar]
- 36.Faxon D.P., Fuster V., Libby P., Beckman J.A., Hiatt W.R., Thompson R.W., Topper J.N., Annex B.H., Rundback J.H., Fabunmi R.P., et al. Atherosclerotic vascular disease conference: Writing group III: Pathophysiology. Circulation. 2004;109:2617–2625. doi: 10.1161/01.CIR.0000128520.37674.EF. [DOI] [PubMed] [Google Scholar]
- 37.Peeters W., de Kleijn D.P., Vink A., van de Weg S., Schoneveld A.H., Sze S.K., van der Spek P.J., de Vries J.P., Moll F.L., Pasterkamp G. Adipocyte fatty acid binding protein in atherosclerotic plaques is associated with local vulnerability and is predictive for the occurrence of adverse cardiovascular events. Eur. Heart J. 2011;32:1758–1768. doi: 10.1093/eurheartj/ehq387. [DOI] [PubMed] [Google Scholar]
- 38.Park S.E., Rhee E.J., Lee W.Y., Kim W.J., Yoo S.H., Bae J.C., Choi E.S., Park C.Y., Oh K.W., Park S.W., et al. The role of serum adipocyte fatty acid-binding protein on the development of metabolic syndrome is independent of pro-inflammatory cytokines. Nutr. Metab. Cardiovasc. Dis. 2012;22:525–532. doi: 10.1016/j.numecd.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 39.Flink L., Mochari-Greenberger H., Mosca L. Gender differences in clinical outcomes among diabetic patients hospitalized for cardiovascular disease. Am. Heart J. 2013;165:972–978. doi: 10.1016/j.ahj.2013.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaman D., Ilhan N., Akbulut M. Adipocyte fatty acid binding protein levels in patients with coronary artery disease and its relationship to alternative biomarkers. Kardiol. Pol. 2015;73:94–100. doi: 10.5603/KP.a2014.0152. [DOI] [PubMed] [Google Scholar]
- 41.Furuhashi M., Tuncman G., Görgün C.Z., Makowski L., Atsumi G., Vaillancourt E., Kono K., Babaev V.R., Fazio S., Linton M.F., et al. Treatment of diabetes and atherosclerosis by inhibiting fatty-acid-binding protein aP2. Nature. 2007;447:959–965. doi: 10.1038/nature05844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Höbaus C., Herz C.T., Pesau G., Wrba T., Koppensteiner R., Schernthaner G.H. FABP4 and cardiovascular events in peripheral arterial disease. Angiology. 2018;69:424–430. doi: 10.1177/0003319717728226. [DOI] [PubMed] [Google Scholar]
- 43.Furuhashi M., Hotamisligil G.S. Fatty acid-binding proteins: Role in metabolic diseases and potential as drug targets. Nat. Rev. Drug Discov. 2008;7:489–503. doi: 10.1038/nrd2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miyoshi T., Onoue G., Hirohata A., Hirohata S., Usui S., Hina K., Kawamura H., Doi M., Kusano K.F., Kusachi S., et al. Serum adipocyte fatty acid-binding protein is independently associated with coronary atherosclerotic burden measured by intravascular ultrasound. Atherosclerosis. 2010;211:164–169. doi: 10.1016/j.atherosclerosis.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 45.Yeung D.C., Xu A., Cheung C.W., Wat N.M., Yau M.H., Fong C.H., Chau M.T., Lam K.S. Serum adipocyte fatty acid-binding protein levels were independently associated with carotid atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2007;27:1796–1802. doi: 10.1161/ATVBAHA.107.146274. [DOI] [PubMed] [Google Scholar]
- 46.Bao Y., Lu Z., Zhou M., Li H., Wang Y., Gao M., Wei M., Jia W. Serum levels of adipocyte fatty acid-binding protein are associated with the severity of coronary artery disease in Chinese women. PLoS ONE. 2011;6:e19115. doi: 10.1371/journal.pone.0019115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ding M., Shi J.Y., Xing Y.Z., Sun B., Fang Q.H., Zhang J.Y., Zhang Q.M., Chen L.M., Yu D.M., Li C.J. Serum adipocyte fatty acid-binding protein levels are associated with peripheral arterial disease in women, but not men, with type 2 diabetes mellitus. J. Diabetes. 2018;10:478–486. doi: 10.1111/1753-0407.12549. [DOI] [PubMed] [Google Scholar]
- 48.Camplain R., Meyer M.L., Tanaka H., Palta P., Agarwal S.K., Aguilar D., Butler K.R., Heiss G. Smoking behaviors and arterial stiffness measured by pulse wave velocity in older adults: The Atherosclerosis Risk in Communities (ARIC) study. Am. J. Hypertens. 2016;29:1268–1275. doi: 10.1093/ajh/hpv189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bell S., Daskalopoulou M., Rapsomaniki E., George J., Britton A., Bobak M., Casas J.P., Dale C.E., Denaxas S., Shah A.D., et al. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: Population based cohort study using linked health records. BMJ. 2017;356:j909. doi: 10.1136/bmj.j909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Batzias K., Antonopoulos A.S., Oikonomou E., Siasos G., Bletsa E., Stampouloglou P.K., Mistakidi C.V., Noutsou M., Katsiki N., Karopoulos P., et al. Effects of newer antidiabetic drugs on endothelial function and arterial stiffness: A systematic review and meta-analysis. J. Diabetes Res. 2018;2018:1232583. doi: 10.1155/2018/1232583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Upala S., Wirunsawanya K., Jaruvongvanich V., Sanguankeo A. Effects of statin therapy on arterial stiffness: A systematic review and meta-analysis of randomized controlled trial. Int. J. Cardiol. 2017;227:338–341. doi: 10.1016/j.ijcard.2016.11.073. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data which support the findings of our study are included in this article.