Abstract
Papillary thyroid microcarcinoma (PTMC) typically has an indolent course and excellent prognosis. Nonetheless, a subset of PTMC carries a risk of lymph node metastasis (LNM) and local recurrence. PTC from the Middle Eastern population is unique with respect to demographic and clinico-pathological characteristics as compared to other ethnicities of the world. The risk factors of LNM in PTMC patients of Middle Eastern ethnicity have not been fully explored. The present study aims to investigate the influencing factors of LNM in Middle Eastern PTMC patients and its predictive impact on patient’s outcome. A total of 226 confirmed PTMC cases were selected in this retrospective study. The correlation between clinico-pathological, as well as molecular, characteristics and LNM was evaluated. Multivariate analysis was performed by logistic regression and Cox proportional hazards models. Among the 226 patients, the rate of LNM was 43.8% (99/226). Bilaterality, multifocality, gross extrathyroidal extension (ETE), and intermediate-to-high American Thyroid Association (ATA) risk tumors were significantly associated with LNM in PTMC. Multivariate logistic regression analysis showed that bilaterality and gross ETE were independent predictive factors for LNM in PTMC. The recurrence-free survival (RFS) was shorter in PTMC with LNM compared to those without LNM (p = 0.0051) and was significant on multivariate analysis. In conclusion, our study showed that bilaterality and gross ETE were independent influencing factors of LNM in Saudi patients with PTMC. LNM was also associated with shorter RFS. The identification of risk factors for LNM in patients of Middle Eastern ethnicity could help the individualization of clinical management for PTMC patients.
Keywords: papillary thyroid microcarcinoma, lymph node metastasis, recurrence-free survival, risk factors
1. Introduction
The incidence of papillary thyroid carcinoma (PTC) has increased in the past decades [1,2,3]. In Saudi Arabia, thyroid cancer is the second most common cancer in women [4]. Papillary thyroid microcarcinoma (PTMC) is defined by the World Health Organization (WHO) as a tumor measuring up to 10 mm in its largest dimension [5]. The incidence of PTMC has also increased, primarily due to improved detection methods such as high-resolution sensitive cervical ultrasound and subsequent use of fine needle aspiration (FNA) biopsy [6,7,8,9]. Despite the increasing incidence of PTMC, it is indolent in nature, with patients usually having favorable prognosis [10]. However, a considerable subset of patients with PTMC have a tendency to develop aggressive disease and lymph node metastasis (LNM) [11,12].
According to several reports, LNM is considered one of the risk factors for aggressive PTMC [10,13,14,15,16]. Several clinico-pathological and molecular characteristics have been shown to increase the risk for LNM such as older age, gender, multifocality, bilaterality, extra-thyroidal extension, and the presence of Hashimoto’s thyroiditis [15,17,18]. In addition, the presence of BRAF mutations has been reported to be a significant risk factor for LNM [19,20].
Furthermore, the rate of LNM varies in frequency from one study to another, ranging between 14% to 40% [21,22,23]. Chow et al. [24] and others [25,26] have also documented the negative impact of LNM on recurrence of PTMC patients. However, at present, there are limited studies on the risk factors for LNM in PTMC in Middle Eastern populations. PTC in those of Middle Eastern ethnicity differs from other populations of the world with respect to several demographic and clinico-pathological features. The incidence of PTC is higher in Saudi Arabia compared to Western populations and it ranks as the second most common malignancy among females in this ethnicity, accounting for 14.3% of all cancers [4]. Further, as reported by this study and in other studies on Middle Eastern populations, the incidence of recurrence (18.4%) [27], lymph node metastasis (53.0%) [28], and distant metastasis (7.5%) [29] is higher compared to other ethnicities. Another important difference is the earlier age of onset for PTC in Middle Eastern populations. The median age of our study population is 40.4 years, which is similar to studies of other Middle Eastern ethnicities [30,31,32,33], but lower than that seen in studies of Western populations [34]. These findings likely reflect the inherent aggressive nature of PTC in this ethnicity.
Therefore, there is a compelling need to explore LNM in PTMC in this ethnicity to improve patient management. This study aims to explore the rate and clinico-pathological and molecular risk factors, as well as the impact of LNM, on patient outcomes in Middle Eastern PTMC.
2. Materials and Methods
2.1. Patient Selection
A total of 226 PTMC patients diagnosed between 1988 and 2018 at King Faisal Specialist Hospital and Research Centre (Riyadh, Saudi Arabia) were included in the study. Cases were identified based on clinical history, followed by FNA biopsy for confirmation. The Institutional Review Board of the hospital approved this study, and since only retrospective patient data were used, the Research Advisory Council (RAC) provided a waiver of consent under project RAC # 221 1168 and # 2110 031. The study was conducted in accordance with the Declaration of Helsinki.
2.2. Clinico-Pathological and Follow-Up Data
Baseline clinico-pathological data were collected from case records and have been summarized in Table 1. A total thyroidectomy was performed in 81.4% (184/226) of PTMC cases in our cohort, whereas 18.6% (42/226) underwent lobectomy/hemithyroidectomy. Prophylactic central lymph node dissection was only performed in patients with clinically uninvolved central neck lymph nodes (cN0) who had advanced primary tumors (T3 or T4) or clinically involved lateral neck nodes (cN1b), or, if the information could be used to plan further steps in therapy, in accordance with the 2015 American Thyroid Association (ATA) guidelines [35]. Prophylactic lateral lymph node dissection was performed only if there was intra-operative evidence of lateral lymph node involvement. Extra-thyroidal extension (ETE) was further classified as follows: microscopic ETE was defined as a tumor extending beyond the thyroid capsule into the surrounding peri-thyroidal soft tissues of fat and/or skeletal muscle, without visual evidence of this invasion, and macroscopic ETE was defined as visual evidence of tumor invasion into strap muscles, subcutaneous soft tissue, larynx, trachea, esophagus, recurrent laryngeal nerve, or prevertebral fascia. Based on the 2015 ATA guidelines, tall cell, hobnail, columnar cell, diffuse sclerosing, and insular variants were classified as aggressive variants, whereas classical and follicular variants were classified as non-aggressive variants [35]. The staging of PTMC was performed using the eighth edition of American Joint Committee on Cancer (AJCC) staging system. Patients were stratified into low, intermediate, and high risk based on the 2015 ATA guidelines [35]. Following initial surgery, low-risk PTC patients were followed up annually, intermediate-risk patients were followed up at 6 months intervals, and high-risk patients were followed up at 3 months intervals. At each follow-up, neck ultrasound, thyroid function tests, thyroglobulin levels, and thyroglobulin antibodies were performed. In addition, for high-risk patients, radioiodine scans and PET CT scans were performed to identify tumor recurrence. Only structural recurrence (local, regional, or distant) was considered for analysis. Recurrence was defined as any newly detected tumor (local or distant) or metastatic regional lymph node based on ultrasound and/or imaging studies in patients who had been previously free of disease following initial treatment. Recurrence-free survival (RFS) was defined as the time (in months) from the date of initial surgery to the occurrence of any tumor recurrence (local, regional, or distant). In the case of no recurrence, the date of the last follow-up was the study endpoint for RFS.
Table 1.
Clinico-pathological and molecular characteristics of papillary thyroid microcarcinoma.
| No. | % | |
|---|---|---|
| Total | 226 | |
| Age, median (range) | 40.4 (11.5–84.0) | |
| <55 | 191 | 84.5 |
| ≥55 | 35 | 15.5 |
| Gender | ||
| Female | 181 | 80.1 |
| Male | 45 | 19.9 |
| Histologic subtype | ||
| Aggressive variants | 29 | 12.8 |
| Non-aggressive variants | 197 | 87.2 |
| Tumor laterality | ||
| Unilateral | 154 | 68.1 |
| Bilateral | 72 | 31.9 |
| Multifocality | ||
| Yes | 91 | 40.3 |
| No | 135 | 59.7 |
| Extrathyroidal extension | ||
| Gross | 15 | 6.7 |
| Microscopic | 48 | 21.2 |
| Absent | 163 | 72.1 |
| Lymphovascular invasion | ||
| Present | 42 | 18.6 |
| Absent | 184 | 81.4 |
| Tumor size | ||
| <0.5 cm | 54 | 23.9 |
| 0.5–1.0 cm | 172 | 76.1 |
| pN | ||
| N0 | 103 | 45.6 |
| N1 | 99 | 43.8 |
| Central only | 40 | 17.7 |
| Central + lateral | 8 | 3.5 |
| Lateral only | 51 | 22.6 |
| Nx | 24 | 10.6 |
| pM | ||
| M0 | 220 | 97.3 |
| M1 | 6 | 2.7 |
| TNM Stage | ||
| I | 206 | 91.2 |
| II | 11 | 4.8 |
| III | 3 | 1.3 |
| IV | 4 | 1.8 |
| Unknown | 2 | 0.9 |
| Hashimoto’s thyroiditis | ||
| Present | 46 | 20.4 |
| Absent | 180 | 79.6 |
| BRAF mutation | ||
| Present | 103 | 45.6 |
| Absent | 117 | 51.8 |
| Unknown | 6 | 2.6 |
| NRAS mutation | ||
| Present | 16 | 7.1 |
| Absent | 203 | 89.8 |
| Unknown | 7 | 3.1 |
| HRAS mutation | ||
| Present | 3 | 1.3 |
| Absent | 217 | 96.0 |
| Unknown | 6 | 2.7 |
| KRAS mutation | ||
| Present | 2 | 0.9 |
| Absent | 218 | 96.4 |
| Unknown | 6 | 2.7 |
| TERT mutation | ||
| Present | 16 | 7.1 |
| Absent | 184 | 81.4 |
| Unknown | 26 | 11.5 |
| Recurrence | ||
| Yes | 33 | 14.6 |
| No | 193 | 85.4 |
| ATA risk category | ||
| Low | 67 | 29.6 |
| Intermediate | 92 | 40.8 |
| High | 67 | 29.6 |
| Total follow-up duration (mean ± S.D.) (in years) | 9.8 ± 6.9 | |
TNM—Tumor-Node-Metastasis; BRAF—B-Raf Proto-Oncogene; NRAS—Neuroblastoma RAS Viral Oncogene Homolog; HRAS—Harvey Rat Sarcoma Viral Oncogene Homolog; KRAS—Kirsten rat sarcoma virus; TERT—Telomerase Reverse Transcriptase.
2.3. BRAF and TERT Mutation Analysis
BRAF and TERT mutation data for the entire PTMC cohort were available from our previous studies [36,37].
2.4. Statistical Analsysis
The associations between clinico-pathological variables and tumor recurrence were determined using contingency table analysis and Chi-square tests. Logistic regression analysis was used for multivariate analysis. The Mantel–Cox log rank test was used to evaluate RFS. Survival curves were generated using the Kaplan–Meier method. Two-sided tests were used for statistical analyses with a limit of significance defined as a p value of <0.05. Data analyses were performed using the JMP14.0 (SAS Institute, Inc., Cary, NC, USA) software package.
3. Results
3.1. Patient Characteristics
The median age of the study cohort was 40.4 years (range: 11.5–84 years), with a male to female ratio of 1:4. A majority of the tumors were non-aggressive variants (classical variant–71.2%; 161/226, follicular variant–16.0%; 36/226). Tumors were bilateral in 31.9% (72/226) of cases, whereas multifocality was noted in 40.3% (91/226). Extrathyroidal extension was seen in 27.9% (63/226) of PTMCs. The incidence of BRAF mutation in PTMC was 46.8% (103/220) and that of TERT mutation was 8.0% (16/200). On ATA risk stratification, 29.6% (67/226) were found to be low risk, 40.8% (92/226) intermediate risk, and 29.6% (67/226) high risk. Of the patients, 72.6% (164/226) received radioactive iodine therapy (Table 1).
3.2. Incidence of Lymph Node Metastasis (LNM) in PTMC and Its Clinico-Pathological Associations
LNM was noted in 43.8% (99/226) of PTMCs in our cohort, of which central LNM (CLNM) was 17.7%, and lateral LNM (LLNM) was 26.1%. The rate of occult CLNM (clinical N0 with pathologic N1a) was 5.3% and the rate of occult LLNM (clinical N0 with pathologic N1b) was 7.5%. A total of 24 (10.6%) patients had Nx status and, hence, were not included for further analysis. LNM was significantly associated with bilateral tumors (p < 0.0001), multifocality (p = 0.0019), gross extrathyroidal extension (p = 0.0034), tumor recurrence (p = 0.0025), and ATA intermediate/high risk tumors (p < 0.0001). However, no association with molecular markers (RAF/RAS genes and TERT) was noted (Table 2).
Table 2.
Clinico-pathological associations of lymph node metastasis in papillary thyroid microcarcinoma.
| Total | LNM Present | LNM Absent | p Value | ||||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Total | 202 | 99 | 49.0 | 103 | 51.0 | ||
| Age (years) | |||||||
| <55 | 171 | 84.6 | 88 | 88.9 | 83 | 80.6 | 0.0992 |
| ≥55 | 31 | 15.4 | 11 | 11.1 | 20 | 19.4 | |
| Gender | |||||||
| Female | 165 | 81.7 | 77 | 77.8 | 88 | 85.4 | 0.1587 |
| Male | 37 | 18.3 | 22 | 22.2 | 15 | 14.6 | |
| Histologic subtype | |||||||
| Aggressive variants | 26 | 12.9 | 12 | 12.1 | 14 | 13.6 | 0.7548 |
| Non-aggressive variants | 176 | 87.1 | 87 | 87.9 | 89 | 86.4 | |
| Tumor laterality | |||||||
| Unilateral | 132 | 65.3 | 51 | 51.5 | 81 | 78.6 | <0.0001 |
| Bilateral | 70 | 34.7 | 48 | 48.5 | 22 | 21.4 | |
| Multifocality | |||||||
| Yes | 84 | 41.6 | 52 | 52.5 | 32 | 31.1 | 0.0019 |
| No | 118 | 58.4 | 47 | 47.5 | 71 | 68.9 | |
| Extrathyroidal extension | |||||||
| None | 145 | 71.8 | 61 | 61.6 | 84 | 81.5 | 0.0034 |
| Microscopic | 42 | 20.8 | 26 | 26.2 | 16 | 15.6 | |
| Gross | 15 | 7.4 | 12 | 12.2 | 3 | 2.9 | |
| Lymphovascular invasion | |||||||
| Present | 35 | 17.3 | 17 | 17.2 | 18 | 17.5 | 0.9545 |
| Absent | 167 | 82.7 | 82 | 82.8 | 85 | 82.5 | |
| Tumor size | |||||||
| ≤0.5 cm | 47 | 23.3 | 24 | 24.2 | 23 | 22.3 | 0.7478 |
| 0.6–1.0 | 155 | 76.7 | 75 | 75.8 | 80 | 77.7 | |
| Distant metastasis | |||||||
| Yes | 12 | 5.9 | 9 | 9.1 | 3 | 2.9 | 0.0582 |
| No | 190 | 94.1 | 90 | 90.9 | 100 | 97.1 | |
| TNM stage | |||||||
| I–II | 195 | 96.5 | 94 | 94.9 | 101 | 98.1 | 0.2155 |
| III–IV | 7 | 3.5 | 5 | 5.1 | 2 | 1.9 | |
| Hashimoto’s thyroiditis | |||||||
| Yes | 40 | 19.8 | 19 | 19.2 | 21 | 20.4 | 0.8310 |
| No | 162 | 80.2 | 80 | 80.8 | 82 | 79.6 | |
| BRAF mutation | |||||||
| Present | 95 | 47.0 | 53 | 53.5 | 42 | 40.8 | 0.0693 |
| Absent | 107 | 53.0 | 46 | 46.5 | 61 | 59.2 | |
| NRAS mutation | |||||||
| Present | 15 | 7.7 | 4 | 4.2 | 11 | 11.0 | 0.1061 |
| Absent | 180 | 92.3 | 91 | 95.8 | 89 | 89.0 | |
| HRAS mutation | |||||||
| Present | 3 | 1.5 | 1 | 1.0 | 2 | 2.0 | 0.5809 |
| Absent | 193 | 98.5 | 95 | 99.0 | 98 | 98.0 | |
| KRAS mutation | |||||||
| Present | 1 | 0.5 | 0 | 0.0 | 1 | 1.0 | 0.2451 |
| Absent | 195 | 99.5 | 96 | 100.0 | 99 | 99.0 | |
| TERT mutation | |||||||
| Present | 15 | 8.5 | 8 | 9.0 | 7 | 8.1 | 0.8227 |
| Absent | 161 | 91.5 | 81 | 91.0 | 80 | 91.9 | |
| Tumor recurrence | |||||||
| Yes | 33 | 16.3 | 24 | 24.2 | 9 | 8.7 | 0.0025 |
| No | 169 | 83.7 | 75 | 75.8 | 94 | 91.3 | |
| ATA risk category | |||||||
| Low | 63 | 31.2 | 2 | 2.0 | 61 | 59.2 | <0.0001 |
| Intermediate/high | 139 | 68.8 | 97 | 98.0 | 42 | 40.8 | |
TNM—Tumor-Node-Metastasis; BRAF—B-Raf Proto-Oncogene; NRAS—Neuroblastoma RAS Viral Oncogene Homolog; HRAS—Harvey Rat Sarcoma Viral Oncogene Homolog; KRAS—Kirsten rat sarcoma virus; TERT—Telomerase Reverse Transcriptase.
3.3. Risk Factors Predicting LNM in PTMC
Since we found LNM to be associated with adverse clinico-pathological factors in PTMC, we sought to further assess the risk factors that could independently predict LNM. On multivariate logistic regression analysis, we found gross extrathyroidal extension (HR = 3.20; 95% CI = 1.36–7.53; p = 0.0077) and tumor bilaterality (HR = 3.31; 95% CI = 1.43–7.62; p = 0.0050) to be independent predictors for LNM (Table 3).
Table 3.
Multivariate analysis using a logistic regression model for predictors of lymph node metastasis (LNM) in PTMC.
| Multivariate (LNM) | ||
|---|---|---|
| Clinico-Pathological Variables | HR (95% CI) |
p Value |
| Age | ||
| ≥55 years (vs. <55years) | 0.44 (0.18–1.09) | 0.0747 |
| Gender | ||
| Male (vs. female) | 1.45 (0.63–3.31) | 0.3794 |
| Histology | ||
| Aggressive variants (vs. non-aggressive variants) | 0.96 (0.38–2.45) | 0.9322 |
| Tumor laterality | ||
| Bilateral (vs. unilateral) | 3.31 (1.43–7.62) | 0.0050 |
| Tumor focality | ||
| Multifocal (vs. unifocal) | 0.91 (0.40–2.06) | 0.8261 |
| Extrathyroidal extension | ||
| Absent | Reference | |
| Microscopic | 1.25 (0.36–4.31) | 0.7240 |
| Gross | 3.20 (1.36–7.53) | 0.0077 |
| Lymphovascular invasion | ||
| Present (vs. absent) | 0.73 (0.30–1.76) | 0.4804 |
| Tumor size | ||
| 0.5–1.0 cm (vs. <0.5 cm) | 0.95 (0.46–1.95) | 0.8848 |
| Distant metastasis | ||
| Present (vs. absent) | 2.44 (0.50–11.99) | 0.2728 |
HR—hazard ratio; CI—confidence interval.
3.4. LNM and Clinical Outcome in PTMC
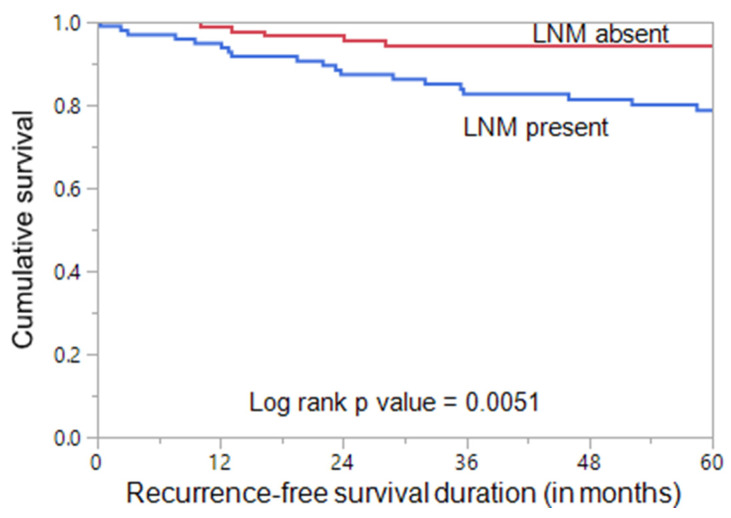
As previously stated, LNM was significantly associated with tumor recurrence. Using the Mantel–Cox log rank test, we found that PTMC patients with LNM had a significantly shorter RFS compared to patients without LNM (p = 0.0051; Figure 1). On multivariate analysis using Cox proportional hazards model, LNM was found to be an independent predictor of shorter RFS (HR = 2.97; 95% CI = 1.23–7.99; p = 0.0149) (Table 4).
Figure 1.
Recurrence-free survival (RFS) in papillary thyroid microcarcinoma (PTMC). Kaplan–Meier survival curve showing a shorter recurrence-free survival in PTMC patients with lymph node metastasis (LNM) than in those without LNM (p = 0.0051).
Table 4.
Multivariate analysis using a Cox proportional hazards model for predictors of recurrence-free survival (RFS) in PTMC.
| Multivariate (RFS) | ||
|---|---|---|
| Clinico-Pathological Variables | HR (95% CI) |
p Value |
| Age | ||
| ≥55 years (vs. <55 years) | 1.89 (0.57–5.19) | 0.2760 |
| Gender | ||
| Male (vs. female) | 2.92 (1.28–6.48) | 0.0116 |
| Histology | ||
| Aggressive variants (vs. non-aggressive variants) | 0.52 (0.07–2.27) | 0.4238 |
| Tumor laterality | ||
| Bilateral (vs. unilateral) | 1.21 (0.35–5.63) | 0.7766 |
| Tumor focality | ||
| Multifocal (vs. unifocal) | 0.52 (0.11–1.78) | 0.3139 |
| Extrathyroidal extension | ||
| Absent | Reference | |
| Microscopic | 2.40 (0.86–6.47) | 0.0937 |
| Gross | 3.29 (0.70–16.72) | 0.1325 |
| Lymphovascular invasion | ||
| Present (vs. absent) | 0.58 (0.09–2.10) | 0.4436 |
| Tumor size | ||
| 0.5–1.0 cm (vs. <0.5 cm) | 0.81 (0.17–3.02) | 0.7658 |
| Distant metastasis | ||
| Present (vs. absent) | 4.37 (1.08–18.16) | 0.0389 |
| Lymph node metastasis | ||
| Present (vs. absent) | 2.97 (1.23–7.99) | 0.0149 |
HR—hazard ratio; CI—confidence interval.
4. Discussion
PTMC has become a health concern due to its increase in incidence over recent decades [19,20]. Although cases of PTMC usually have favorable outcomes, there is a subset of PTMC patients that present with aggressive disease and a high risk of recurrence. Identifying risk factors of LNM and recurrence is very important to decide the best therapeutic management for these patients.
In the present study, we analyzed the retrospective data of 226 patients with PTMC. The results revealed that the rate of LNM was 43.8%, which is within the range previously reported [15,38]. The rate of CLNM was 17.7% and LLNM was 26%. Interestingly, the rate of occult CLNM was 5.3%, whereas it was 7.5% for occult LLNM. This suggests that lateral LNs are more commonly involved, especially for occult metastasis. This is different from previous studies, where central LNs were the most common area for LNM [15,21,39]. This result of a high rate of LLNM and occult LLNM could help surgeons in the decision of performing prophylactic lateral lymph node dissections to reduce recurrence. However, a larger cohort from this ethnic group is required to validate our findings.
This study shows the presence of bilateral foci and gross extra-thyroid extension as the only independent risk factors for LNM in Middle Eastern patients with PTMC. This is similar to other studies which also found extrathyroidal extension and bilaterality as predictors of lymph node metastasis [14,17,21,40]. However, our study differs from larger studies of other Western and far Eastern ethnicities in that we did not find any other clinico-pathological parameters as potential predictors of lymph node metastasis, whereas male gender, age, tumor size, multifocality, lymphovascular invasion, and presence of Hashimoto’s thyroiditis were reported in these ethnicities as predictors of lymph node metastasis in PTMC [14,15,17,21,40,41,42,43,44,45,46,47]. The cohort size, ethnicity, and study design (including lateral LNM or central LNM) might contribute to these differences.
The presence of bilateral foci has been reported in the literature as an independent risk factor for LNM [23,48]. Although gross ETE has not been reported as an independent risk factor of LNM in patients with PTMC, its strong association with aggressive PTMC and its impact on patient survival have been well documented [10,49,50].
Furthermore, we found that the proportion of intermediate/high ATA risk of recurrence stratification is significantly higher in LNM PTMC patients, which suggests a higher risk of recurrence. Therefore, we have investigated the impact of LNM on PTMC patient outcome. The result revealed a 2.8-fold higher recurrence rate in PTMC patients with LNM than in PTMC patients without LNM. In addition, the recurrence-free survival was significantly shorter (p = 0.0051) in LNM PTMC patients. This is in agreement with other previous studies, where LNM was found to be a predictor of patient outcome [51,52]. While some studies have shown that LNM can affect a patient’s recurrence-free survival only in combination with other risk factors, such as number and diameter of LNM [53,54], this study shows LNM alone to be an independent risk factor for recurrence-free survival, irrespective of the number and diameter of LNM in PTMC.
This study has some limitations. It is a retrospective study from a single tertiary care center, and so selection bias cannot be ignored. The study has a limited number of PTMC patients of Middle Eastern ethnicity, and so the conclusions need to be read with caution.
5. Conclusions
Bilateral tumors and gross ETE are independent risk factors for LNM in Middle Eastern PTMC patients. The presence of lateral LNM is apparently higher than central LNM in this study cohort, which should be considered carefully by surgeons for therapeutic and preventive plans for this PTMC patient group. Finally, we identified that LNM in PTMC increases the risk of recurrence and affects the prognosis by being an independent risk factor for recurrence-free survival. These data could help to extend our understanding about the risk of LNM and recurrence in PTMC in patients of Middle Eastern ethnicity and support the importance of individualized management of PTMC patients.
Acknowledgments
The authors would like to thank Felisa DeVera for her technical assistance.
Author Contributions
Conceptualization, K.S.A.-K. and A.K.S.; methodology, S.K.P. and A.K.S.; software, S.K.P.; validation, S.K.P. and P.A.; formal analysis, S.K.P. and A.K.S.; investigation, P.A. and N.S.; resources, S.S.A.-S. and F.A.-D.; data curation, S.K.P.; writing—original draft preparation, K.S.A.-K.; writing—review and editing, S.K.P. and A.K.S.; visualization, A.K.S. and S.K.P.; supervision, K.S.A.-K.; project administration, K.S.A.-K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of King Faisal Specialist Hospital and Research Centre (protocol code 2211168; 16 September 2021 and 2110031; 6 February 2012).
Informed Consent Statement
Patient consent was waived since only retrospective patient data were used for the study.
Data Availability Statement
The data presented in this study are available in the article.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pellegriti G., Frasca F., Regalbuto C., Squatrito S., Vigneri R. Worldwide Increasing Incidence of Thyroid Cancer: Update on Epidemiology and Risk Factors. J. Cancer Epidemiol. 2013;2013:965212. doi: 10.1155/2013/965212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pereira M., Williams V.L., Johnson J.H., Valderrabano P. Thyroid Cancer Incidence Trends in the United States: Association with Changes in Professional Guideline Recommendations. Thyroid. 2020;30:1132–1140. doi: 10.1089/thy.2019.0415. [DOI] [PubMed] [Google Scholar]
- 3.Baldini E., Tuccilli C., Pironi D., Catania A., Tartaglia F., Di Matteo F.M., Palumbo P., Arcieri S., Mascagni D., Palazzini G., et al. Expression and Clinical Utility of Transcription Factors Involved in Epithelial–Mesenchymal Transition during Thyroid Cancer Progression. J. Clin. Med. 2021;10:4076. doi: 10.3390/jcm10184076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alrawaji A., Alshahrani Z., Alzahrani W., Alomran F., Almadouj A. Cancer Incidence Report Saudi Arabia 2015. Saudi Health Council, Saudi Cancer Registry; Riyadh, Saudi Arabia: 2018. [Google Scholar]
- 5.Asa S. The Current Histologic Classification of Thyroid Cancer. Endocrinol. Metab. Clin. N. Am. 2019;48:1–22. doi: 10.1016/j.ecl.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Cramer J.D., Fu P., Harth K.C., Margevicius S., Wilhelm S.M. Analysis of the rising incidence of thyroid cancer using the Surveillance, Epidemiology and End Results national cancer data registry. Surgery. 2010;148:1147–1153. doi: 10.1016/j.surg.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 7.Simard E.P., Ward E.M., Siegel R., Jemal A. Cancers with increasing incidence trends in the United States: 1999 through 2008. CA Cancer J. Clin. 2012;62:118–128. doi: 10.3322/caac.20141. [DOI] [PubMed] [Google Scholar]
- 8.Udelsman R., Zhang Y. The Epidemic of Thyroid Cancer in the United States: The Role of Endocrinologists and Ultrasounds. Thyroid. 2014;24:472–479. doi: 10.1089/thy.2013.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brito J.P., Morris J.C., Montori V.M. Thyroid cancer: Zealous imaging has increased detection and treatment of low risk tumours. BMJ. 2013;347:f4706. doi: 10.1136/bmj.f4706. [DOI] [PubMed] [Google Scholar]
- 10.Mehanna H., Al-Maqbili T., Carter B., Martin E., Campain N., Watkinson J., McCabe C., Boelaert K., Franklyn J.A. Differences in the Recurrence and Mortality Outcomes Rates of Incidental and Nonincidental Papillary Thyroid Microcarcinoma: A Systematic Review and Meta-Analysis of 21 329 Person-Years of Follow-up. J. Clin. Endocrinol. Metab. 2014;99:2834–2843. doi: 10.1210/jc.2013-2118. [DOI] [PubMed] [Google Scholar]
- 11.Zheng W., Wang X., Rui Z., Wang Y., Meng Z., Wang R. Clinical features and therapeutic outcomes of patients with papillary thyroid microcarcinomas and larger tumors. Nucl. Med. Commun. 2019;40:477–483. doi: 10.1097/MNM.0000000000000991. [DOI] [PubMed] [Google Scholar]
- 12.Baldini E., Tuccilli C., Prinzi N., Sorrenti S., Falvo L., DE Vito C., Catania A., Tartaglia F., Mocini R., Coccaro C., et al. Deregulated Expression of Aurora Kinases Is Not a Prognostic Biomarker in Papillary Thyroid Cancer Patients. PLoS ONE. 2015;10:e0121514. doi: 10.1371/journal.pone.0121514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caliskan M., Park J.H., Jeong J.S., Lee C.-R., Park S.K., Kang S.-W., Jeong J.J., Chung W.Y., Park C.S. Role of prophylactic ipsilateral central compartment lymph node dissection in papillary thyroid microcarcinoma. Endocr. J. 2012;59:305–311. doi: 10.1507/endocrj.EJ11-0366. [DOI] [PubMed] [Google Scholar]
- 14.Gui C.Y., Qiu S.L., Peng Z.H., Wang M. Clinical and pathologic predictors of central lymph node metastasis in papillary thyroid microcarcinoma: A retrospective cohort study. J. Endocrinol. Investig. 2017;41:403–409. doi: 10.1007/s40618-017-0759-y. [DOI] [PubMed] [Google Scholar]
- 15.Yin Y., Xu X., Shen L., Zhao W., Diao H., Li C. Influencing Factors and Cumulative Risk Analysis of Cervical Lymph Node Metastasis of Papillary Thyroid Microcarcinoma. Front. Oncol. 2021;11:644645. doi: 10.3389/fonc.2021.644645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao J., Zhao Y., Ling Y., Kang H. Risk Factors of Central Lymph Node Metastasis in Papillary Thyroid Microcarcinoma and the Value of Sentinel Lymph Node Biopsy. Front. Surg. 2021;8:680493. doi: 10.3389/fsurg.2021.680493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiangqian Z., Chen P., Ming G., Jingtai Z., Xiukun H., Jingzhu Z., Xi W., Jiadong C., Dapeng L., Biyun Q. Risk factors for cervical lymph node metastasis in papillary thyroid microcarcinoma: A study of 1587 patients. Cancer Biol. Med. 2019;16:121–130. doi: 10.20892/j.issn.2095-3941.2018.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y., Guan Q., Xiang J. Nomogram for predicting central lymph node metastasis in papillary thyroid microcarcinoma: A retrospective cohort study of 8668 patients. Int. J. Surg. 2018;55:98–102. doi: 10.1016/j.ijsu.2018.05.023. [DOI] [PubMed] [Google Scholar]
- 19.Huang K., Gao N., Bian D., Zhai Q., Yang P., Zhang Y. Associations of BRAF V600E, clinical pathology and imaging factors with the recurrence rate of papillary thyroid microcarcinoma. Exp. Ther. Med. 2020;20:243. doi: 10.3892/etm.2020.9373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ulisse S., Baldini E., Lauro A., Pironi D., Tripodi D., Lori E., Ferent I.C., Amabile M.I., Catania A., Di Matteo F.M., et al. Papillary Thyroid Cancer Prognosis: An Evolving Field. Cancers. 2021;13:5567. doi: 10.3390/cancers13215567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Medas F., Canu G.L., Cappellacci F., Boi F., Lai M.L., Erdas E., Calò P.G. Predictive Factors of Lymph Node Metastasis in Patients with Papillary Microcarcinoma of the Thyroid: Retrospective Analysis on 293 Cases. Front. Endocrinol. 2020;11:551. doi: 10.3389/fendo.2020.00551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gu J.-H., Zhao Y.-N., Xie R.-L., Xu W.-J., You D.-L., Zhao Z.-F., Wang F., Fei J. Analysis of risk factors for cervical lymph node metastasis of papillary thyroid microcarcinoma: A study of 268 patients. BMC Endocr. Disord. 2019;19:124. doi: 10.1186/s12902-019-0450-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheng F., Chen Y., Zhu L., Zhou B., Xu Y., Chen Y., Wen L., Chen S. Risk Factors for Cervical Lymph Node Metastasis of Papillary Thyroid Microcarcinoma: A Single-Center Retrospective Study. Int. J. Endocrinol. 2019;2019:8579828. doi: 10.1155/2019/8579828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chow S.-M., Law S.C.K., Chan J.K.C., Au S.-K., Yau S., Lau W.-H. Papillary microcarcinoma of the thyroid? Prognostic significance of lymph node metastasis and multifocality. Cancer. 2003;98:31–40. doi: 10.1002/cncr.11442. [DOI] [PubMed] [Google Scholar]
- 25.Kaliszewski K., Diakowska D., Rzeszutko M., Nowak Ł., Aporowicz M., Wojtczak B., Sutkowski K., Rudnicki J. Risk factors of papillary thyroid microcarcinoma that predispose patients to local recurrence. PLoS ONE. 2020;15:e0244930. doi: 10.1371/journal.pone.0244930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim T.Y., Hong S.J., Kim J.M., Kim W.G., Gong G., Ryu J.S., Kim W.B., Yun S.-C., Shong Y.K. Prognostic parameters for recurrence of papillary thyroid microcarcinoma. BMC Cancer. 2008;8:296. doi: 10.1186/1471-2407-8-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Siraj A.K., Parvathareddy S.K., Qadri Z., Siddiqui K., Al-Sobhi S.S., Al-Dayel F., Al-Kuraya K.S. Annual Hazard Rate of Recurrence in Middle Eastern Papillary Thyroid Cancer over a Long-Term Follow-Up. Cancers. 2020;12:3624. doi: 10.3390/cancers12123624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parvathareddy S.K., Siraj A.K., Qadri Z., Ahmed S.O., DeVera F., Al-Sobhi S., Al-Dayel F., Al-Kuraya K.S. Lymph node ratio is superior to AJCC N stage for predicting recurrence in papillary thyroid carcinoma. Endocr. Connect. 2022;11:e210518. doi: 10.1530/EC-21-0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parvathareddy S.K., Siraj A.K., Iqbal K., Qadri Z., Ahmed S.O., Al-Rasheed M., AlQatie A.A., Al-Sobhi S.S., Al-Dayel F., Al-Kuraya K.S. TERT Promoter Mutations Are an Independent Predictor of Distant Metastasis in Middle Eastern Papillary Thyroid Microcarcinoma. Front. Endocrinol. 2022;13:808298. doi: 10.3389/fendo.2022.808298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Zaher N., Al-Salam S., El Teraifi H. Thyroid carcinoma in the United Arab Emirates: Perspectives and experience of a tertiary care hospital. Hematol. Oncol. Stem Cell Ther. 2008;1:14–21. doi: 10.1016/S1658-3876(08)50055-0. [DOI] [PubMed] [Google Scholar]
- 31.Keinan-Boker L., Silverman B.G. Trends of thyroid cancer in Israel: 1980–2012. Rambam Maimonides Med. J. 2016;7:e0001. doi: 10.5041/RMMJ.10228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doubi A., Al-Qannass A., Al-Angari S., Al-Qahtani K.H., Alessa M., Al-Dhahri S. Trends in thyroid carcinoma among thyroidectomy patients: A 12-year multicenter study. Ann. Saudi Med. 2019;39:345–349. doi: 10.5144/0256-4947.2019.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Samargandy S., Qari R., Aljadani A., Assaqaf D., Etaiwi A., Alghamdi D., Marzouki H., Alhozali A., Merdad M., Al-Hajeili M., et al. Clinicopathological Characteristics of Thyroid Cancer in a Saudi Academic Hospital. Cureus. 2020;12:e8044. doi: 10.7759/cureus.8044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim H., Devesa S.S., Sosa J.A., Check D., Kitahara C.M. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974–2013. JAMA. 2017;317:1338–1348. doi: 10.1001/jama.2017.2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haugen B.R., Alexander E.K., Bible K.C., Doherty G.M., Mandel S.J., Nikiforov Y.E., Pacini F., Randolph G.W., Sawka A.M., Schlumberger M., et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siraj A.K., Parvathareddy S.K., Pratheeshkumar P., Divya S.P., Al-Sobhi S.S., Al-Dayel F., Al-Kuraya K.S. PD-L1 Is an Independent Prognostic Marker in Middle Eastern PTC and Its Expression is Upregulated by BRAFV600E Mutation. Cancers. 2021;13:555. doi: 10.3390/cancers13030555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bu R., Siraj A.K., Divya S.P., Kong Y., Parvathareddy S.K., Al-Rasheed M., Al Obaisi K.A.S., Victoria I.G., Al-Sobhi S.S., Al-Dawish M., et al. Telomerase reverse transcriptase mutations are independent predictor of disease-free survival in Middle Eastern papillary thyroid cancer. Int. J. Cancer. 2018;142:2028–2039. doi: 10.1002/ijc.31225. [DOI] [PubMed] [Google Scholar]
- 38.Kim K.-E., Kim E.-K., Yoon J.H., Han K., Moon H.J., Kwak J.Y. Preoperative Prediction of Central Lymph Node Metastasis in Thyroid Papillary Microcarcinoma Using Clinicopathologic and Sonographic Features. World J. Surg. 2012;37:385–391. doi: 10.1007/s00268-012-1826-3. [DOI] [PubMed] [Google Scholar]
- 39.Huang Y., Yin Y., Zhou W. Risk Factors for Central and Lateral Lymph Node Metastases in Patients with Papillary Thyroid Micro-Carcinoma: Retrospective Analysis on 484 Cases. Front. Endocrinol. 2021;12:640565. doi: 10.3389/fendo.2021.640565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim S.K., Park I., Woo J.-W., Lee J.H., Choe J.-H., Kim J.-H., Kim J.S. Predictive Factors for Lymph Node Metastasis in Papillary Thyroid Microcarcinoma. Ann. Surg. Oncol. 2016;23:2866–2873. doi: 10.1245/s10434-016-5225-0. [DOI] [PubMed] [Google Scholar]
- 41.Zhang X., Zhang L., Xue S., Wang P., Chen G. Predictive factors of lateral lymph node metastasis in solitary papillary thyroid microcarcinoma without gross extrathyroidal extension. Asian J. Surg. 2018;42:563–570. doi: 10.1016/j.asjsur.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 42.Mercante G., Frasoldati A., Pedroni C., Formisano D., Renna L., Piana S., Gardini G., Valcavi R., Barbieri V. Prognostic Factors Affecting Neck Lymph Node Recurrence and Distant Metastasis in Papillary Microcarcinoma of the Thyroid: Results of a Study in 445 Patients. Thyroid. 2009;19:707–716. doi: 10.1089/thy.2008.0270. [DOI] [PubMed] [Google Scholar]
- 43.Liu Z., Lei J., Liu Y., Fan Y., Wang X., Lu X. Preoperative predictors of lateral neck lymph node metastasis in papillary thyroid microcarcinoma. Medicine. 2017;96:e6240. doi: 10.1097/MD.0000000000006240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou C., Li J., Wang Y., Xue S., Zhang Y. Association of BRAF gene and TSHR with cervical lymph node metastasis of papillary thyroid microcarcinoma. Oncol. Lett. 2018;17:183–194. doi: 10.3892/ol.2018.9572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vorasubin N., Nguyen C., Wang M. Risk factors for cervical lymph node metastasis in papillary thyroid microcarcinoma: A meta-analysis. Ear Nose Throat J. 2016;95:73–77. [PubMed] [Google Scholar]
- 46.Jeon M.J., Chung M.S., Kwon H., Kim M., Park S., Baek J.H., Song D.E., Sung T.-Y., Shong Y.K., Kim T.Y., et al. Features of papillary thyroid microcarcinoma associated with lateral cervical lymph node metastasis. Clin. Endocrinol. 2017;86:845–851. doi: 10.1111/cen.13322. [DOI] [PubMed] [Google Scholar]
- 47.Back K., Kim J.S., Kim J.-H., Choe J.-H. Superior located papillary thyroid microcarcinoma is a risk factor for lateral lymph node metastasis. Ann. Surg. Oncol. 2019;26:3992–4001. doi: 10.1245/s10434-019-07587-2. [DOI] [PubMed] [Google Scholar]
- 48.Qu N., Zhang L., Ji Q.-H., Chen J.-Y., Zhu Y.-X., Cao Y.-M., Shen Q. Risk Factors for Central Compartment Lymph Node Metastasis in Papillary Thyroid Microcarcinoma: A Meta-Analysis. World J. Surg. 2015;39:2459–2470. doi: 10.1007/s00268-015-3108-3. [DOI] [PubMed] [Google Scholar]
- 49.Al-Qurayshi Z., Nilubol N., Tufano R.P., Kandil E. Wolf in Sheep’s Clothing: Papillary Thyroid Microcarcinoma in the US. J. Am. Coll. Surg. 2020;230:484–491. doi: 10.1016/j.jamcollsurg.2019.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Giordano D., Gradoni P., Oretti G., Molina E., Ferri T. Treatment and prognostic factors of papillary thyroid microcarcinoma. Clin. Otolaryngol. 2010;35:118–124. doi: 10.1111/j.1749-4486.2010.02085.x. [DOI] [PubMed] [Google Scholar]
- 51.Wu M.-H., Shen W.T., Gosnell J., Duh Q.-Y. Prognostic significance of extranodal extension of regional lymph node metastasis in papillary thyroid cancer. Head Neck. 2014;37:1336–1343. doi: 10.1002/hed.23747. [DOI] [PubMed] [Google Scholar]
- 52.Park Y.M., Wang S.-G., Lee J.-C., Shin N.H., Kim I.-J., Son S.-M., Mun M., Lee B.-J. Metastatic lymph node status in the central compartment of papillary thyroid carcinoma: A prognostic factor of locoregional recurrence. Head Neck. 2015;38:E1172–E1176. doi: 10.1002/hed.24186. [DOI] [PubMed] [Google Scholar]
- 53.Randolph G., Duh Q.-Y., Heller K.S., LiVolsi V.A., Mandel S.J., Steward D., Tufano R.P., Tuttle R.M. The Prognostic Significance of Nodal Metastases from Papillary Thyroid Carcinoma can be Stratified Based on the Size and Number of Metastatic Lymph Nodes, as Well as the Presence of Extranodal Extension ATA Surgical Affairs Committee’s Taskforce on Thyroid Cancer Nodal Surgery. Thyroid. 2012;22:1144–1152. doi: 10.1089/thy.2012-0043. [DOI] [PubMed] [Google Scholar]
- 54.Lee J., Song Y., Soh E.Y. Prognostic Significance of the Number of Metastatic Lymph Nodes to Stratify the Risk of Recurrence. World J. Surg. 2013;38:858–862. doi: 10.1007/s00268-013-2345-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available in the article.