Abstract
Resources to prepare Allergy and Immunology trainees and providers to recognize and address health disparities are lacking. We designed a curriculum using interactive sessions incorporating disease-specific, evidence-based content, and a panel-based workshop with facilitated discussion to prepare Allergy and Immunology trainees to identify structural racism and health disparities. Pre-session surveys revealed that a high portion of trainees reported feeling comfortable recognizing bias and discussing health equity (n = 16, mean = 3.6/5 on a Likert scale), but felt less confident in their ability to address disparities in practice or to identify resources to care for historically disadvantaged communities (n = 16, mean = 2.9/5 on a Likert scale). The curriculum improved respondents’ confidence in their ability to address these issues, with a panel-based workshop increasing attendees’ scores an average of 0.65 points (n = 17, mean: pre-survey 3.31 vs post-survey 3.95). After the sessions, a toolkit was created to optimize delivery of medical education to address health disparities and define core concepts for this subject. Resources to implement these concepts in research design and recruitment efforts were included. With inadequate guidance for the incorporation of disparities-focused medical education curricula, our educational series, resources, and interactive toolkit add to existing literature to improve disparities competencies in teaching, clinical practices, and research design.
Keywords: Health disparities, Asthma, Food allergy, Atopic dermatitis, Equity, Medical education, Curriculum, Structural racism
Health disparities are a particular type of health difference that a patient experiences that is closely linked with social, economic, and/or environmental disadvantage(s).1 Health equity is the focused effort to eliminate health disparities by addressing the structural and social inequalities and injustices that result in the unfair and avoidable differences in health across individuals and groups.1 Patients from marginalized backgrounds not only experience adversity related to disparities in health, but they are also more likely to experience systematically or institutionally derived social adversities such as food insecurity, educational inequity, violence, economic instability, childhood maltreatment, racism, and discrimination.2–4 There has been a focused effort to address the institutional, systemic structures and processes that contribute to disparities in the field of medicine in order to achieve health equity for all persons who seek care.
In 2017, the Accreditation Council for Graduate Medical Education (ACGME) implemented a mandate that required all US residency programs to include health disparity training within their residency curricula.5 This requirement extended to fellowship programs.6 However, despite this core requirement, the onus has been on individual programs to create, design, and implement impactful and useful curricula to train fellows in this regard without specific guidance from the ACGME. The Allergy-Immunology Milestones v2.0 for achieving competency in Allergy-Immunology does incorporate the need for competence in systems-based practice in community and population health.7 In the Milestones v2.0 supplementary guide, achieving a high level of competence (levels 4 and 5) in this area suggests that a trainee “participates in changing and adapting practice to provide for the needs of specific populations or communities” and “leads innovations to advocate for specific populations or communities with health care inequities.” Unfortunately, despite these aims, neither specific resources for achieving these goals nor resources for health disparities education are mapped to this competency in the supplementary guide. Neither the ACGME nor professional organizations have clearly defined the role of clinician-educators in reducing disparities for their unique patient populations; rather the responsibility in gaining competency lies on the individual fellow.8 Recently, a workgroup of the American Academy of Allergy, Asthma, and Immunology (AAAAI) published guidance for practitioners on addressing health disparities using a multilevel approach.9 The report outlines the current state of disparities in allergic and immunologic disorders and details best practices to address disparities in several ways including advocacy efforts, community partnerships, and approaches to recruitment, which is very much needed. This toolkit addresses the need for further structured education for trainees and builds on the content outlined in the Workgroup Report.
To address the current deficiencies in appropriately preparing Allergy and Immunology fellowship trainees and faculty to recognize and address health disparities in their local context, an effort to define the knowledge, skills, and disparity competencies in both research and clinical practice is required. We developed and implemented a 3-session teaching resource at our institution in the form of 2 lecture series and a workshop to address this gap in education and training and to promote structural humility (the practice of provider self-reflection and growth that leads to recognizing one’s role in addressing health disparities as an ally who engages in processes, partnerships, and training to better understand structural barriers related to patient care). During curriculum implementation, we identified unique specialty-specific competencies that could be incorporated and adapted for curricula to train health care providers in addressing and reducing health disparities.
To approach this effort, the first hurdle we encountered was the lack of available resources or standard curricula beyond single didactic lectures or podcasts describing health disparities. We set out to create a curriculum that would highlight areas that would benefit from direct teaching, and subsequently designed a toolkit to assist programs to adapt resources for their own local context. Here we provide a framework to guide the development of a platform to share and exchange evidence-based content for adaptation by other institutions and providers to assess whether or not institutional expertise on disparities exists among the faculty. This toolkit serves as a foundation for identifying how to operationalize, optimize, and implement health disparities education and approaches at the individual and institutional level.
METHODS
This educational series was designed by a faculty member and clinical fellow (PK and CU) using evidence-based approaches and adult learning theory. The main goal was to design a curriculum at our institution to meaningfully discuss and develop critical consciousness for trainees and faculty on the topics of social determinants of health (SDoH), health disparities, and health equity in the field of Allergy and Immunology. A secondary goal was to assess the effectiveness of the intervention and to provide the design of the curriculum as a resource for graduate medical education (GME) planning purposes at other institutions. The series included 3 sessions for learners at all levels to introduce and develop understanding of health disparities broadly and to recognize the impact of health inequities on the experience of Allergy and Immunology patients.
Planning
The series was designed to address key learning objectives in a safe space while considering time, resource, and format constraints.10 Curriculum design involved, as a first step, acquisition of foundational knowledge and skills by the facilitators after a comprehensive literature review. This literature review also served as a guide for identifying high-yield, evidence-based information formatted into engaging activities for prospective participants that included clinical fellows, academic allergists, and clinician-scientists in the field of Allergy and Immunology. We then designed 3 sessions, 2 lectures with learning activities and 1 workshop, using adult learning theory with an interactive breakout room format to engage participants in discussions and to disseminate information related to health disparities in Allergy and Immunology. Because of the COVID-19 pandemic, all sessions were conducted using a virtual conference platform.
Delivery
The series was planned for a goal audience of trainees and faculty at varied levels of training and patient care responsibilities. The series were divided into sessions to be attended sequentially with an overall goal of directly addressing knowledge gaps related to disparities and health equity for patients from historically disadvantaged backgrounds. The first session, consisting of lectures and case presentations, was geared toward clinical fellows, with a second session provided for both faculty and clinical fellows. The third session, an interactive workshop, was designed for all prior participants and was facilitated by an expert panel, including 2 of the authors (AJ and JS) as well as an epidemiologist focused on disparities and environmental health from National Institutes of Health and a public health official from the Center for Disease Control’s Office of Minority Health and Health Equity.
Table I describes each session’s objectives, learning activities, reflection exercises, and resources used to facilitate the session. Detailed design elements are available in this article’s Online Repository at www.jaci-inpractice.org.
TABLE I.
Key planning elements for each session
| Session(s) | Learning objectives | Learning activities | Resources used |
|---|---|---|---|
| 1 and 2 |
|
For fellow-focused session:
|
1–2 presenters Clinical case of <disease> related to health disparity/inequity Poll everywhere for generating word cloud |
| 3 |
|
|
1–2 presenters/main facilitators 3–4 panelists 1 discussion facilitator per small group Technical facilitation of virtual breakout rooms GoogleDrive (or similar document sharing platform) for sharing and documenting ideas in breakout rooms |
Sessions 1 and 2: health disparities in Allergy and Immunology: a discussion of race and bias in medicine
For session 1, 2 facilitators led a 90-minute interactive, discussion-based lecture for clinical fellows at our institution. These facilitators were not formally trained in disparities education or research but were versed in the general literature and evidence-based practices in health disparities. This session was focused on providing a framework and introduction to the topics of disparities and health equity in both a broad health care context and specifically in the field of Allergy and Immunology. Session 2 was an abbreviated 60-minute format, similar to session 1, for faculty and fellows at our institution to build on prior instructions using spaced learning and to facilitate more in-depth exploration of the topics. There was no preparation required for these sessions. Fellows who attended the prior session were permitted, but not required, to attend this additional session.
We started the session by providing the historical context of race, systemic racism, and disparities in health care within the United States, and presenting epidemiologic data for disparate health outcomes of common Allergy and Immunology disorders such as asthma, food allergy, and atopic dermatitis based on race and SDoH. We specifically focused on the impact of racism on disparate health outcomes and the influence of race and ethnicity on patient experiences in health care. Important examples were highlighted, including the legacy of redlining in the United States, upstream and downstream effects of disparities, impacts of SDoH on care experience, and how race (as a social construct) is a poor surrogate for genetic differences between individuals. The session also addressed effective strategies for becoming an ally. Complementary self- and group-reflection exercises were used to assist participants with awareness of the influence that unconscious bias (ie, implicit bias) and stereotypes have on their personal and professional lives, as well as how these biases and stereotypes directly impact patient care, patient attitudes, and how patients interact with the health care system. Throughout the session, facilitators encouraged participants to share personal and professional examples and insight related to their experience with race, racism, health disparities, and health equity. Resources for further reading and learning were provided to all participants after the sessions were completed. Feedback obtained from this introductory session directly informed the development of session 3, which was focused on how to apply this knowledge in both clinical and research settings.
Session 3: taking action—disparities in Allergy and Immunology research and practice: an interactive panel-based discussion
The third session, an experiential learning workshop, was designed with diverse voices and subject matter experts on disparities in Allergy and Immunology. We aimed to define and share competencies, approaches, and tools for both clinical training purposes and identification of unmet needs for incorporation of health disparities into research design efforts. The 90-minute session was designed for physicians from our institution, but other local institutions and associated programs were invited to attend to attain as diverse of voices and backgrounds, and experience as possible. Attendees were primarily clinical fellows, academic allergists, and clinician-scientists.
This workshop consisted of a panel-based large-group discussion, followed by facilitated small-group breakout-room discussions and then a large-group debriefing session to share reflections at the end. We selected and invited 4 panelists with experience in health disparities clinical practice, research, and public health policy. The large-group discussion was transitioned into 6 virtual breakout rooms with mixed level participants, a panelist, and a facilitator/record keeper. Each small group addressed a particular domain or key question related to patient care or research design involving historically excluded patients and participants (see this article’s Online Repository at www.jaci-inpractice.org). The groups were then transitioned back into a large group where further discussions occurred. The facilitators directed questions to the panelists who provided expert opinion as well as summaries of the small-group discussions and further resources that could be integral to addressing disparities in clinical practice or research.
After the session, information and resources compiled from the workshop were shared with participants and informed the framework for the toolkit.
Evaluations and feedback
We distributed anonymous, electronic pre- and post-participation surveys for sessions required as a part of the fellowship didactic curriculum, which included sessions 1 and 3. Session 2 participants were not surveyed, as this was an accessory session performed for an audience that volunteered to attend based on their interest in the subject matter, which included both faculty and fellows. We collected information on participant role, training year, and affiliation. The evaluations also assessed participants’ prior training experience on the topic, as well as interest in future plans to advance these skills, and comments on the curriculum.
Survey results
All results were collected using an online, anonymized survey administration tool. Results are presented as means unless otherwise specified. Survey responses were graded on a Likert scale from 1 to 5, where a score of 1 indicates that the respondent “strongly disagrees” with the survey prompt, whereas a score of 5 indicates that the respondent “strongly agrees” with the prompt, with a score of 3 representing “undecided/neutral.” These surveys were used to identify areas of weakness and confidence in relation to the concepts, goals, and aims of the curriculum session.
RESULTS
Sessions 1 and 2
The introductory session 1 was attended by 6 clinical fellows at our institution. All participants completed a pre-participation survey, and 83% of participants completed a post-participation survey. The pre-survey evaluations found that 67% of participants had prior educational experience or had completed formal training in bias and disparities in health care. All participants who completed the pre-survey, however, responded with an average score of 2.7 out of 5 in response to the prompt: “I feel confident in my ability to reference the current literature and guidelines regarding caring for underserved and disadvantaged populations.”
The second introductory session, session 2, designed for faculty and fellows at our institution, had 15 participants in attendance (8 faculty members and 7 clinical fellows). Feedback evaluations were not collected because of the similar content presented as the first session and the intent of the session (non-mandatory, supplementary session for faculty and fellows).
Session 3
The experiential learning workshop, session 3, was attended by 33 participants, including 20 faculty members and 13 GME fellows across 4 different regional academic institutions. Most participants in this session had also attended sessions 1 and/or 2. Among the faculty members, 13 identified as clinician-scientists and 7 identified as predominantly clinician-educators in academia. Eighty-eight percent of participants completed the preparticipation survey. Of the respondents, 78.6% reported prior educational experience or completed formal training in bias and disparities in health care, and 100% of participating fellows reported prior training. The pre-survey for this session found that of the 28 respondents, only 8 (28.6%) scored an average of 4 or more on the Likert scale in response to their ability to address the objectives of the session (which is consistent with “agreeing” with the survey prompt). The response scores are detailed in Table II.
TABLE II.
Panelist session participant survey responses based on professional title
| Survey prompt | Averaged pre-survey Likert scale score (max of 5: 1—strongly disagree; 5—strongly agree) |
Averaged post-survey Likert scale score (max of 5: 1—strongly disagree; 5—strongly agree) |
||||
|---|---|---|---|---|---|---|
| All (28 respondents) |
Faculty (n, %) (18, 64.3%) |
Fellow (n, %) (10, 35.7%) |
All (17 respondents) |
Faculty (n, %) (8, 47.0%) |
Fellow (n, %) (9, 52.9%) |
|
| “I feel confident in my ability to identify, review, and apply current literature regarding health disparities in Allergy and Immunology and to identify barriers to care in clinical practice and research.” | 3.3 | 3.4 | 3.1 | 3.9 | 3.9 | 3.9 |
| “I can readily identify approaches, including resources and research efforts, to mitigate the impact of race, bias, and structural inequities in order to improve health outcomes.” | 3.1 | 3.3 | 2.7 | 3.9 | 3.9 | 3.9 |
| “I can readily identify evidence-based methods for caring for underserved and minoritized populations.” | 3.3 | 3.3 | 3.1 | 3.8 | 3.8 | 3.9 |
| “I can readily identify evidence-based methods for caring for underserved and minoritized populations.” | 3.8 | 3.9 | 3.6 | 4.1 | 4.1 | 4.1 |
| “I recognize the multiple aspects of inequalities in care experienced by minority patients in the field of Allergy and Immunology.” | 3.6 | 3.8 | 3.3 | 4.1 | 4.1 | 4.0 |
In addition, the average overall and individual Likert scale score for pre-survey prompts in fellows was lower than the average score for faculty members, with greatest score discrepancies related to confidence identifying resources to mitigate inequities and confidence caring for patients from disparate backgrounds. Faculty self-scored 3.4 compared with fellows’ 3.1 in response to the prompt: “I feel confident in my ability to identify, review, and apply current literature regarding health disparities in Allergy and Immunology and to identify barriers to care in clinical practice and research.” Faculty self-scored 3.3 compared with fellows’ 2.7 in response to the prompt: “I can readily identify approaches, including resources and research efforts, to mitigate the impact of race, bias, and structural inequities in order to improve health outcomes.” Faculty self-scored 3.3 compared with fellows’ 3.1 in response to the prompt: “I can readily identify evidence-based methods for caring for underserved and minoritized populations.” Faculty self-scored 3.9 compared with fellows’ 3.6 in response to the prompt: “I can readily identify evidence-based methods for caring for underserved and minoritized populations.” Faculty self-scored 3.8 compared with fellows’ 3.3 in response to the prompt: “I recognize the multiple aspects of inequalities in care experienced by minority patients in the field of Allergy and Immunology.”
The post-participation survey had a 51.5% response rate (17 of 33). Of the 17 respondents, 10 (58.8%) scored an average of 4 or more on the Likert scale in response to their ability to address all of the objectives of the session. Compared with the pre-survey, all respondents had a higher Likert score on the post-survey in the overall and individual prompt scores, with no discrepancy in scoring between faculty and fellows. Both faculty and fellows who completed the post-survey had an averaged self-score of 3.9 in response to the prompt: “I feel confident in my ability to identify, review, and apply current literature regarding health disparities in Allergy and Immunology and to identify barriers to care in clinical practice and research.” Faculty and fellows also self-scored 3.9 in response to the prompt: “I can readily identify approaches, including resources and research efforts, to mitigate the impact of race, bias, and structural inequities in order to improve health outcomes.” Both faculty and fellows self-scored 3.8 in response to the prompt: “I can readily identify evidence-based methods for caring for underserved and minoritized populations.” Faculty and fellows self-scored 4.1 in response to the prompt: “I can readily identify evidence-based methods for caring for underserved and minoritized populations.” Faculty self-scored 4.1 compared with fellows’ 4.0 in response to the prompt: “I recognize the multiple aspects of inequalities in care experienced by minority patients in the field of Allergy and Immunology.”
In addition, the session was well received with 88.2% of respondents reported that they would be interested in participating in another or similar session in health disparities and bias in Allergy and Immunology addressing more advanced concepts and topics.
Our interactive, multi-institutional series identified several areas of improvement in the training of Allergy and Immunology clinicians on health equity and health disparities. The areas of interest and unmet need discussed during the program are detailed in Table III and helped to shape the guiding principles for suggesting core competencies for disparities training of Allergy and Immunology trainees outlined in Figure 1.
TABLE III.
Summarized barriers and action items identified by session 3 with associated structural competencies addressed
| Domain | Barrier | Action | Structural competency addressed12,13 |
|---|---|---|---|
| Food allergy | Financial barriers in care of patients with food allergy
|
Multidisciplinary approach incorporating social workers, dieticians, and community health workers Implement screeners to assess barriers to care Partner with community members to provide needed resources (eg, food pantries, support groups, food vouchers with local grocery stores/farmer’s markets, drug assistance programs, food policy council) Engage with primary care providers to educate and provide resources on food allergy |
Recognize the influence of structures on patient health Recognize and respond to influences of structures on the clinical encounter Engage in structural humility |
| Atopic dermatitis | Lack of training of disease recognition in different skin types and pigmentation Cultural sensitivity for impact of pigmentation with medication initiation and disease severity Financial or time-consuming barriers to treatment (eg, access to bathtubs, financial/time burden of twice daily baths, or costs of emollients or wraps) Access to subspecialists and participation in research studies |
Include images of affected individuals with diverse backgrounds and skin pigmentation in educational and training resources or materials Model discussing issues related to skin pigmentation during clinical interactions Coordinate efforts to connect with and engage communities of color affected by atopic dermatitis Improve efforts to recruit patients from diverse backgrounds to participate in clinical trials for atopic dermatitis |
Demonstrate skills necessary to assess, diagnose, and manage atopic dermatitis in patients of diverse ethnic and cultural backgrounds Recognize and use extra-clinical resources to enhance patient care and outcomes in multicultural clinical settings Recognize the role of public health resources and agencies to enhance patient care and outcomes in multicultural settings Exhibit empathy and discuss alternate care options for patients in low-economic or -resource settings Engage in structural humility |
| Asthma | Access to subspecialist care Underestimation or unacknowledged assessment of barriers to health care Distrust of providers due to patient biases stemming from structural racism Lack of resources to attend visits or engage with health care system |
Incorporate home or telemedicine visits into assessment of patients with poor clinical improvement or difficulty attending appointments Coordinate with social services to assist with building trust and bridging care gaps (eg, use of case managers or community health workers to perform home visits, adherence to medications, and health assessments) Improve assessment of social determinants of health (eg, assess presence of allergens/irritants in home, insurance status, access to medications, transportation) Improve recruitment practices and protocol design in clinical trials by recruiting clinical staff from diverse backgrounds Improve efforts to build trust in communities that experienced systemic oppression |
Recognize and use extra-clinical resources to enhance patient care and outcomes in diverse cultural and socioeconomic settings Recognize and/or use the specialty specific role of interdisciplinary teams in addressing health equity Assess or design quality improvement interventions to improve diverse patient’s experience of health care Identify, evaluate, and incorporate clinical practices that promote health equity in clinical practice and/or medical research |
| Research design and recruitment | Mistrust between marginalized communities and centers for research Reduced number of pre-established relationships between marginalized communities and the health institutions that serve them Lack of cultural and ethnic diversity in study staff and leadership Improve efforts to appropriately identify and assess risks and socioeconomic status that impact patient outcomes while enrolled in a research study |
Establish partnerships and relationships with community organizations and providers that care for marginalized communities Improve access by establishing and increasing community-based referrals to research studies Increase efforts to include vulnerable and marginalized populations in research studies Incentivize, track, and monitor diversity of participants recruited to a study Create a funded structure for accountability and addressing bias through feedback and monitoring of study participant demographics Assess diverse elements related to SDoH during the recruitment and enrollment of study participants |
Identify strengths, deficiencies, and limits in one’s ability to address implicit bias and health equity in research Recognize how structural forces impact clinical and research outcomes Incorporate evidence-based practices to assess the impact of cultural barriers (social, infrastructural, economic factors) on research practices and outcomes Appraise and assess the quality of care provided to patients from diverse ethnic and socioeconomic backgrounds Appraise and assess the quality of research endeavors to accurately involve and serve diverse patient populations Use evidence-based models to identify strengths and weaknesses in care and research in patients from marginalized backgrounds |
SDoH, Social determinants of health.
FIGURE 1.
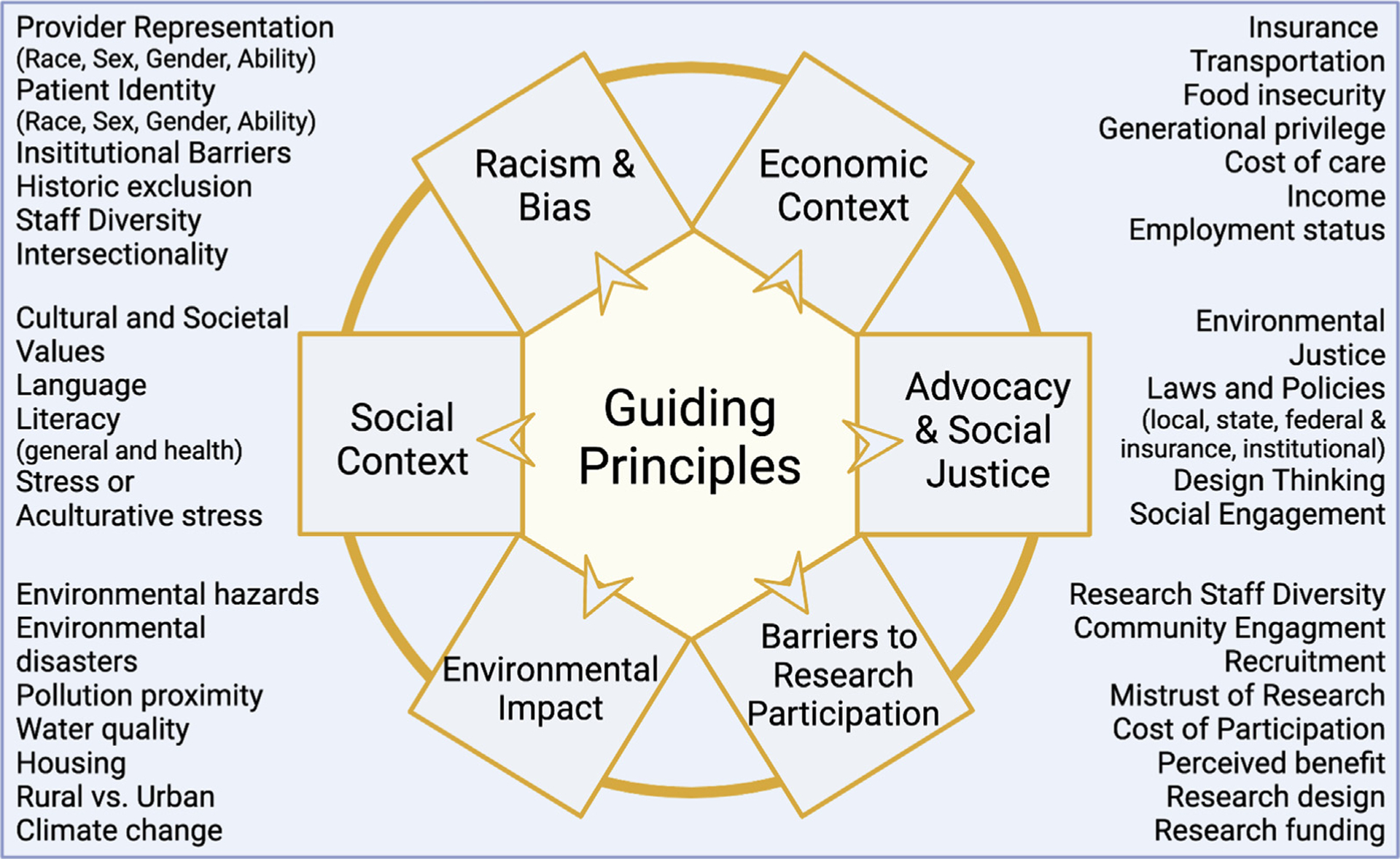
Guiding principles for developing a framework of core competencies for disparities training in Allergy and Immunology, including: (1) racism and bias; (2) economic context; (3) barriers to research participation; (4) advocacy and social justice; (5) social context; and (6) environmental impact.
DISCUSSION
Although health disparities are well described in Allergy and Immunology patient populations, integration of health disparities recognition, mitigation efforts, and curricula into Allergy and Immunology medical education is nascent. The primary goal of our educational series was to address the need for allergy-specific disparities education.
As a 3-session series, sessions 1 and 2 introduced health disparities and structural racism broadly and within Allergy and Immunology. Session 3 was developed with the goal of operationalizing the knowledge gained to provide a framework for future health disparities education in Allergy and Immunology. Although most participants were familiar with health disparities concepts and had received some form of prior bias or disparities training, we found that most participants did not feel competent in their skills to adequately approach or address specialty-specific health disparities in their practice. This finding suggests that there are both educational and performance gaps. Formal curricula to recognize disparities and dissemination of context-specific tools and resources to address health disparities in individual programs are needed.
In addition, we found that before our program implementation, clinical fellows had an even greater need for guidance in disparities education. Clinical fellows, when compared with faculty, scored themselves lower in their ability to recognize disparities-related barriers and apply resources to the care of underserved and marginalized patients (Table II). On completion of the program, all participants’ scores improved in their ability to address the session objectives, with clinical fellows having the largest improvement. Unfortunately, because of the small sample size, low post-survey response rate, and survey collection technique, it is difficult to make inferences regarding the magnitude of the effect of the curriculum on practice improvements, but the series was well received, and most participants were interested in future sessions on health disparities and bias in Allergy and Immunology. Future designs of educational initiatives will require better focus on the ability to appropriately assess and capture changes in participants’ understanding of SDoH concepts in the curricula.
The session 3 workshop provided large- and small-group discussions focused on 4 allergy-specific domains (food allergy, atopic dermatitis, asthma, research design and recruitment) and health disparities related to each domain. Group discussions focused on barriers within each area and brainstorming of actionable areas to address disparities were gathered with expert facilitators in each room (Table III). In each domain, issues unique to Allergy and Immunology and applicable to disparities more broadly were elucidated. The workshop also led to discussions of structural competency, a medical education approach that teaches clinicians how to identify and respond to the impact of upstream structural determinants of health on patient care.14 In the food allergy group, food insecurity was highlighted as a significant barrier. Incorporation of social workers and dieticians into food allergy practice, and community partnerships to provide access to resources such as food pantries, vouchers, and other support were identified as action areas. The atopic dermatitis group importantly focused on the lack of diversity and cultural sensitivity in the training of skin disease recognition across differing skin types and tones (eg, diagnosing atopic dermatitis or recognizing rashes or erythema in skin of color). Integration of diverse racial and ethnic patients for educational and training purposes, and improving efforts to recruit patients from multiple racial and ethnic backgrounds into atopic dermatitis clinical trials were identified as action areas. The group discussing asthma identified access to subspecialists and consideration of economic or social factors (eg, insurance, access to medications, environmental factors) as critically important. Improving the quality and type of clinical assessments, such as social needs intake forms, and coordination with social services to provide multidisciplinary care were identified as action areas.
The group addressing research design and recruitment highlighted multiple barriers such as mistrust of research among historically marginalized communities, poor relationships between communities and research institutions, and the lack of cultural, racial, or ethnic diversity of research staff and principal investigators. Several action areas were proposed including establishing partnerships with communities to improve relationships and research access. In addition, recognition of social determinants of research participants was felt to be important. Importantly, historical and present-day structural forces and biases leading to persistent lack of research diversity were felt to be especially important to address during early stages of research design. Key examples included considering the number of study visits, accessibility of study sites, transportation needs, and compensation during clinical study or trial development.
The workshop identified the key areas of interest and unmet need in health disparities and equity education. We organized these areas into guiding principles for developing a framework of core competencies for disparities training in Allergy and Immunology, namely: (1) racism and bias; (2) economic context; (3) barriers to research participation; (4) advocacy and social justice; (5) social context; and (6) environmental impact (Figure 1). This framework is aligned with other conceptual frameworks of disparities scholarship but includes Allergy and Immunology specific examples.15,16 The workshop identified the need for tangible resources to reference evidence-based education on health disparities, SDoH, and health equity, and these resources were incorporated into a toolkit (Table IV). In addition, the group developed some example question prompts for use by fellows or practitioners during patient encounters (Table V). Although these examples are not intended to be comprehensive, they serve the purpose of fostering additional thought and facilitating comfort with the language that can be employed when addressing health disparities in key competency domains. In addition, we recognize that although some providers may not feel comfortable responding to issues that arise when employing these prompts, it is important to facilitate these conversations with our patients in the proper clinical context. Further, these prompts should be used when the provider is able to address identified issues and/or refer patients to local and institutional resources to aid in addressing them. Another use of the toolkit (Table IV) could be to identify areas where gaps exist in local clinical or academic settings to address disparities and to start to advocate for and assemble local or regional resources.
TABLE IV.
Toolkit: identify and address health disparities competency domains
| Area | Opportunities and mechanisms to address health disparities for trainees and providers | Resources | |
|---|---|---|---|
| General concepts for health disparities focused care of patients with allergic and immunologic diseases | Educational course for trainees and providers | AAAAI Slide Deck17 on Disparities within Allergy and Immunology by the Committee on the Underserved (AAAAI membership required) Health and Human Services has created an educational program18 for physicians (and other providers) directed at addressing the National CLAS Standards, which are a set of 15 action steps intended to advance health equity, improve quality, and help eliminate health care disparities AAP Course: Fighting Racism to Advance Child Health Equity (AAP membership required)19 |
|
| Engage in structural humility by identifying bias and structural barriers in local context | Hire and support diverse staff representative of the community—American Hospital Association Diversity Assessment Tool20 Ensure that systems are in place to provide culturally competent, shared decision-making in counseling and education regarding disease—Cultural Competency Self-Assessment Tool21 by the NCCC |
||
| Incorporate and assess community needs or social determinants of health assessments in clinical practice and management decisions | Adaptable resources | American Academy of Family Practice 10-Question Screening Tool22 (Everyone Project) iScreen Social Screening Questionnaire—46 Question Survey Tool23 CDC Community Health Improvement Navigator24 NACHC Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE)25 Rural Health Information Hub’s Tools26 to assess and measure social determinants of health |
|
| Care of patients with food allergy | Engage in structural humility by identifying bias and structural barriers to care/health outcomes | Educational course for trainees and providers | Recorded episode of the AAAAI podcast series, Conversations from the World of Allergy—Carla Davis, MD, FAAAAI, discusses disparities related to food allergy27 |
| Administrative interventions | Best practice checks to ensure that Food Allergy Plans, EAI, and Food Insecurity screenings are provided/performed for all patients | ||
| Create multidisciplinary approaches to address complex care needs (eg, social work, dietician, nutrition, pharmacists, etc) | Examples of programs | Children’s Mercy Food Allergy Center of Excellence28 Industry Sponsored EpiPen for Schools Program29 |
|
| Design peer-based educational sessions with partnered referral providers and communities | Examples of programs | Code Ana30—Guides schools through the development and implementation of medical emergency response plan | |
| Identify and partner with local and national advocacy groups | National advocacy and patient-centered groups | Food Allergy Research and Education31 The FPIES Foundation32 Food Equality Initiative33 |
|
| Care of patients with atopic dermatitis | Engage in structural humility by identifying bias and structural barriers to care/health outcomes | Educational course for trainees and providers | Dermatologist, Amy McMichael, MD, Chair of the LiVDerm Deep Dive Racial Disparities in Dermatology programs, shares highlights in a youtube video34 on the current health disparities in dermatologic care for patients with skin of color The Impact of Skin Color and Ethnicity on Clinical Diagnosis and Research, Virtual Series35 by Skin of Color Society, NEJM Group, and VisualDx |
| Identify and partner with local and national advocacy groups | National Eczema Association36 International Eczema Council37 National Eczema Society38 Skin of Color Society39 |
||
| Identify alternative resources to train providers in recognizing AD in patients of all skin types | ACAAI and AAN partnered teaching resource Project impact40 | ||
| Care of patients with asthma | Engage in structural humility by identifying bias and structural barriers to care/health outcomes | Educational course for trainees and providers | Recorded episode of the AAAAI podcast series41, Conversations from the World of Allergy featuring interview with Tamara Perry, MD, FAAAAI, on socioeconomic and racial/ethnic disparities of asthma |
| Administrative interventions | Best practices check to ensure that appropriate clinical assessments and medication use are evaluated during visits Increase funding to provide care to underinsured and publicly insured patients Assess opportunities to implement prescription monitoring programs to assess costs and adherence in addition to best prescribing practices are used during care visits |
||
| Incorporate social determinants of health assessments in community clinics or multidisciplinary academic clinics | Example program | Impact DC Program42 sponsored by Children’s National Medical Center | |
| Identify and partner with local and national advocacy groups | National and patient advocacy groups | Asthma and Allergy Foundation of America43 Allergy and Asthma Network44 |
|
| School-based programs | AAAAI - School-based Asthma Management Program45 | ||
| Understand and incorporate the impact environment on health outcome | Environmental Protection Agency (EPA)—EJScreen | An environmental justice mapping and screening tool called EJScreen46 Combines environmental and demographic indicators in maps and reports | |
| Racism, bias, or discrimination in recruiting practices and protocol design for research studies | Engage in structural humility by incorporating bias and disparities training related to research into fellowship curricula | AAAAI educational lectures47 | |
| QI projects | Encourage the assessment and implementation of DEI-focused quality improvement projects and efforts for the clinical practice, institutional policies, and research protocols at the practicing institution | ||
| COLA Conference Lecture by Dr Bridgette Jones | Dr Jones’ COLA lecture48 on bias and racism (presented on August 14, 2020) | ||
| Assess understanding of the impact of structural racism on health outcomes and research design | Integrating equity into QI and PS (Institute for Health Care Improvement-IHI) | Free IHI resources49 available to help guide and support health care entities and providers interested in developing sustainable ways to advance health outcomes within their community, health system, and beyond | |
| PROMIS (Patient-Reported Outcomes Measurement Information System) | A set of person-centered measures50 that evaluates and monitors physical, mental, and social health in adults and children. It can be used with the general population and with individuals living with chronic conditions | ||
| Agency for Healthcare Research and Quality | A comprehensive source of data on health care delivery and patient outcomes over time, and at the national, regional, state, and community levels. In addition, the National Healthcare Quality and Disparities Report presents trends for measures related to access to care, affordable care, care coordination, effective treatment, healthy living, patient safety, and person-centered care Healthcare Cost and Utilization Database51 National Healthcare Quality and Disparities Reports52 |
||
| AAAAI Committee on the Underserved | Committee focused on defining, addressing, and mitigating health disparities within allergy/immunology in racial and ethnic underserved populations9 | ||
| Engage with private and public entities with vested interest in identifying, prioritizing, and addressing disparities in clinical practice and research involving patients from minoritized backgrounds | Patient-Centered Outcomes Research Institute (PCORI) | PCORI53 funds research that offers patients and caregivers the information they need to make important health care decisions. The Evaluation and Analysis program provides evaluation expertise, whereas the Engagement program gives patients, caregivers, clinicians, and other health care stakeholders opportunities for meaningful involvement in all their activities | |
| National Institute of Minority Health Disparities (NIMHD)—HD Pulse | A repository of data54 and resources for addressing health disparities including a data portal for analyzing health disparities and intervention portal (still in development) for identifying evidence-based interventions for addressing health disparities | ||
| NIMHD Publication (Textbook)—The Science of Health Disparities Research | A textbook55 authored by experts in health disparities research that provides information on conducting clinical and translational health disparities studies | ||
| NIMHD—Health Disparities Research Institute | The National Institute on Minority Health and Health Disparities (NIMHD) annually hosts the Health Disparities Research Institute (HDRI)56, which aims to support the research career development of promising early-career minority health/health disparities research scientists and stimulate research in the disciplines supported by health disparities science | ||
| The Office of Minority Health of the HHS | The Office57 provides quantitative information related to health, including sourcing and maintaining a body of expert knowledge on health status initiatives, and demographic statistics and analyses on disadvantaged populations, compiled by the National Center for Health Statistics, the Census Bureau, private foundations, clinical practitioners, private data sources, and public agencies | ||
| CDC CORE Health Equity Science and Intervention Strategy | CDC’s CORE Health Equity58 Science and Intervention Strategy is designed to work in collaboration to challenge CDC centers to incorporate health equity and efforts to address health disparities as a foundational element across all our work—from science and research to programs, and from partnerships to workforce | ||
| National Minority Quality Forum | The NMQF59 is a research and educational organization dedicated to ensuring that high-risk racial and ethnic populations and communities receive optimal health care | ||
| PRIDE—RISE Program | UCSF Research in Implementation Science for Equity (RISE)60 Program are to train and sustain scholars underrepresented in biomedical sciences for long-term success in academic careers pursuing innovative research of interest to the NHLBI | ||
| HOPE Initiative | Interactive data tool61 designed to track social determinants of health and health outcomes by race, ethnicity, and socioeconomic status on state and national level | ||
| PhenX Toolkit | Catalog of validated resources62 for measurement of social and structural impacts on health for incorporation in research | ||
| Improve gaps and disparities in recruitment practices and protocol design | MRCT Center of Diversity, Inclusion, and Equity in Clinical Research | A collaborative resource created by a diversity representative workgroup; their website63 features resources, tools, case studies, and documents designed to help improve diversity in clinical research | |
TABLE V.
Sample prompts and questions for clinical practice to address and assess disease-based clinical competency: a nonexhaustive, noncomprehensive list of sample prompts and questions that can be used in a clinical setting with patients
| Racism/bias | (Opening statement) I would like to ask you some questions that will help me to get a sense of your life outside of the hospital/clinic.64 How often, if ever, have you ever experienced discrimination, been prevented from doing something, or made to feel inferior while receiving care because of your race, ethnicity, or skin color? In terms of race and ethnicity, how do you identify? How often, if ever, have you felt that you were treated unfairly or received substandard care because of your race, gender, sexual orientation, or disability? |
| Economic context | Since your last visit, have you been unable to take or start medications because you were unable to afford the cost? Have you had issues finding and affording allergen-free products (eg, food, formula)? Do you ever have difficulty making ends meet at the end of the month? In the last year, has there been any time where you were without medical insurance? |
| Social context | Sometimes, words in English that we use in the medical field are difficult to understand even for native English speakers. Would you mind if I use a translator to ensure we prevent anything from being lost in translation? You seem hesitant about our plan for your treatment, what concerns do you have about what we have discussed so far? I know that sometimes it can be confusing and/or overwhelming to come to the doctor’s office. We’ve gone over a lot of information, is there anything that I can help explain or communicate more clearly before we finish our visit today? Can you tell me, in your own words, what you think was the most important information you learned from this visit today? I recognize that it can be difficult or expensive for some patients to come to my clinic. I’ve noticed that you arrived late the past few visits. Are there any barriers that make it difficult for you to get here (like cost of transportation or arranging for childcare)? (Follow-Up Question) Is there anything that I can do to help make it easier for you to connect with our medical team? How confident are you in filling out medical forms by yourself?65,66 |
| Environmental impact | It’s important for me to know about your home environment and how it might impact your health. Have you noticed any regular and/or recurring issues with mice, visible mold, cockroaches, or other infestations in the place where you live, work, or spend the majority of your time? Do you feel safe where you live? Is the area where you work, live, or spend a lot of time close to buildings and structures where you (or your child) might be exposed to pollutants (eg, an interstate/highway, power plant, industrial plant, or other similar places)? In the last few months, have you had significant worries or concerns about having a safe and stable place where you own, rent, or stay? (Follow-Up Question) Do you know what housing resources are available to you if you feel unsafe? |
The development of this program has several limitations. First, participation was limited to a small number of institutional faculty and trainees and may not reflect the experience of faculty or clinical fellows at other institutions. Second, although other intersectional domains of health, such as gender and sexual orientation, are known to impact health disparities, the focus of our educational workshops was primarily related to race and ethnicity due to time limitations. Third, the paucity of specific educational materials and guidance through ACGME or other organizations for Allergy and Immunology fellowship disparities education prompted an effort to collate this information using a scoping review of the existing literature. This process was not as rigorous as a systematic review, and there may be additional resources or concepts that are not covered. The influence of race and ethnicity on disparities is well described and closely linked to SDoH. Given the large impact that race and ethnicity have on disparate health outcomes, and the lack of purposeful training to address them, we focused our framework in this space. Future curricula might build on this work to adequately address other domains of health disparities.
Lastly, resources to operationalize disparities competencies will differ by locale and institution, including the ability to address specific barriers identified during the program and attain facilitators who can intelligibly speak on the topic. For example, in atopic dermatitis, local demographics may limit access to diverse patient populations for education, training, and research purposes, and identifying a provider well versed in dermatologic issues, competency in SDoH, and experience in clinical or research related to patients from minoritized backgrounds may be difficult. Given this limitation, it is important for subspecialty organizations to provide guidance and resources or identify speakers in specific areas. In addition, in this digital age, program leadership and individuals interested in implementing curricula focused on expanding trainees’ and providers’ understandings of health disparities within our field must look to leveraging resources that can be shared between institutions, including employing this toolkit, using virtual meeting spaces, and/or engaging with other locally designed educational programs. Entities such as Center for Disease Control’s Office of Minority Health and Health Equity, National Institute of Minority Health Disparities, and the AAAAI Committee on the Underserved have member experts who can serve as important partners for identifying facilitators and additional educational resources important for implementing a similar curriculum. In addition, many programs with a university affiliation have centers or departments of health disparities or schools of public health that could be contacted for creation of programs. More work is currently being done to formalize a resource list, and a concerted effort by the specialty organizations to support and lead this effort will be paramount for advancing this goal.
We developed and implemented an interactive educational program that provides a framework for current education in disparities for Allergy and Immunology trainees and clinicians. Our 3-part series sought to develop methods of involving clinicians to move beyond identifying disparities to brainstorming mechanisms to address disparities for individual patients and to incorporate these concepts in research recruitment efforts. Further, we developed guiding principles to serve as potential benchmarks to measure Allergy and Immunology trainee competencies in disparities using a toolkit to supplement existing literature in Allergy and Immunology clinical practice and research. In this effort, we advocate that disparities education be considered an integral part of Allergy and Immunology training as much as training in immune disease pathogenesis.
Our pilot program provides a needed model for health disparitiese–focused medical education that can be adopted by individual Allergy and Immunology fellowship programs and used as a framework for future curricula with the goal of providing equitable and high-quality care for all patients. The next step should include obtaining real-world feedback on the application and usability of this resource in various regional, research, and care settings. In addition, further work should be done to add to the available body of works, resources, and guiding principles aimed toward enhancing our ability to not only train providers in addressing disparities, but to transform and innovate our approaches to addressing and ameliorating health disparities.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Alicia Simmons, Jaime Cheman, Dr Anna Napoles, Edwin Mayah, Dr Ana Penman-Aguilar, Dr Stephanie London, Katelyn Andersen, Karin Peterson, Nakita McKever, Erin Stinson, and Biorender for their contribution to this curricula, toolkit, and manuscript.
This work was funded in part by the Division of Intramural Research, National Institutes of Allergic and Infectious Diseases, National Institutes of Health.
Abbreviations used
- AAAAI
American Academy of Allergy, Asthma, and Immunology
- ACGME
Accreditation Council for Graduate Medical Education
- GME
Graduate medical education
- SDoH
Social determinants of health
Footnotes
Conflicts of interest: The authors declare that they have no relevant conflicts of interest.
REFERENCES
- 1.Penman-Aguilar A, Talih M, Huang D, Moonesinghe R, Bouye K, Beckles G. Measurement of health disparities, health inequities, and social determinants of health to support the advancement of health equity. J Public Health Manag Pract 2016;22(Suppl 1):S33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, et al. Racial disparities in child adversity in the U.S.: interactions with family immigration history and income. Am J Prev Med 2016;50:47–56. [DOI] [PubMed] [Google Scholar]
- 3.Suglia SF, Campo RA, Brown AGM, Stoney C, Boyce CA, Appleton AA, et al. Social determinants of cardiovascular health: early life adversity as a contributor to disparities in cardiovascular diseases. J Pediatr 2020;219:267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tackett KJ, Jenkins F, Morrell DS, McShane DB, Burkhart CN. Structural racism and its influence on the severity of atopic dermatitis in African American children. Pediatr Dermatol 2020;37:142–6. [DOI] [PubMed] [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education. Common program requirements (residency). Chicago, IL: ACGME; 2022. https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/CPRResidency_2022_TCC.pdf. Accessed February 22, 2022. [Google Scholar]
- 6.Accreditation Council for Graduate Medical Education. Common program requirements (fellowship). Chicago, IL: ACGME; 2019. https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/CPRFellowship2019.pdf. Accessed February 22, 2022. [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education. Allergy and immunology milestone. Chicago, IL: ACGME; 2019. https://www.acgme.org/globalassets/PDFs/Milestones/AllergyandImmunologyMilestones.pdf. Accessed February 22, 2022. [Google Scholar]
- 8.Wagner R, Koh N, Bagian JP, Weiss KB, for the CLER Program. CLER 2016 National Report of Findings. Issue Brief #4: Health Care Disparities. Chicago, IL: ACGME; 2017. https://www.acgme.org/globalassets/pdfs/cler/cler_health_care_disparities_issue_brief.pdf. Accessed February 22, 2022. [Google Scholar]
- 9.Davis CM, Apter AJ, Casillas A, Foggs MB, Louisias M, Morris EC, et al. Health disparities in allergic and immunologic conditions in racial and ethnic underserved populations: a work group report of the AAAAI Committee on the Underserved. J Allergy Clin Immunol 2021;147:1579–93. [DOI] [PubMed] [Google Scholar]
- 10.Belay HT, Ó Ruairc B, Guérandel A. Workshops: an important element in medical education. BJPsych Adv 2019;25:7–13. [Google Scholar]
- 11.DeGannes C, Coke KW, Henderson TB, Sanders-Phillips K. A small-group reflection exercise for increasing the awareness of cultural stereotypes: a facilitator’s guide. MedEdPORTAL 2009;5:668. [Google Scholar]
- 12.Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med 2014;103:126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neff J, Holmes SM, Knight KR, Strong S, Thompson-Lastad A, McGuinness C, et al. Structural competency: curriculum for medical students, residents, and interprofessional teams on the structural factors that produce health disparities. MedEdPORTAL 2020;16:10888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carraccio C, Englander R, Van Melle E, Ten Cate O, Lockyer J, Chan MK, et al. Advancing competency-based medical education: a charter for clinician-educators. Acad Med 2016;91:645–6499. [DOI] [PubMed] [Google Scholar]
- 15.Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice) [Internet]; 2010. Available at: https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf. Accessed November 13, 2021. [Google Scholar]
- 16.NIMHD Research Framework [Internet]. National Institute on Minority Health and Health Disparities c2017. Available at: https://nimhd.nih.gov/researchFramework. Accessed November 13, 2021.
- 17.AAAAI. Allergic and Immunologic Conditions in the Underserved: Awareness, Recognition, and Resources among Populations at Risk for Health Disparities Teaching. Available at: https://www.aaaai.org/Aaaai/media/MembersMedia/Member%20Secure%20Files/Teaching%20Slides/Allergic-and-Immunologic-Conditions-in-the-Underserved.pptx. Accessed February 22, 2022.
- 18.U.S. Department of Health and Human Services. Think Cultural Health. Available at: https://thinkculturalhealth.hhs.gov/education/physicians. Accessed February 22, 2022.
- 19.American Academy of Pediatrics. Fighting Racism to Advance Child Health Equity. Available at: https://shop.aap.org/fighting-racism-to-advance-child-health-equity/. Accessed February 22, 2022.
- 20.American Hospital Association. Does Your Hospital Reflect the Community it Serves. Available at: https://www.aha.org/toolkitsmethodology/2018-02-08-does-your-hospital-reflect-community-it-serves. Accessed February 22, 2022.
- 21.National Center for Cultural Competence. Tools and Processes for Self Assessment. Available at: https://nccc.georgetown.edu/foundations/assessment.php. Accessed February 22, 2022.
- 22.American Academy of Family Physicians. Social Needs Screening Tool. Available at: https://www.aafp.org/dam/AAFP/documents/patient_care/everyone_project/patient-short-print.pdf. Accessed February 22, 2022.
- 23.Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A randomized trial on screening for social determinants of health: the iScreen study. Pediatrics 2014; 134:e1611–8. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Assess Needs and Resources. Available at: https://www.cdc.gov/chinav/tools/assess.html. Accessed February 22, 2022. [Google Scholar]
- 25.National Association of Community Health Centers, Inc., Association of Asian Pacific Community Health Organizations, Oregon Primary Care Association. PREPARE: Protocol for Responding and Assessing Patient Assets, Risks, Experiences. Available at: https://www.nachc.org/wp-content/uploads/2018/05/PRAPARE_One_Pager_Sept_2016.pdf. Accessed February 22, 2022.
- 26.Rural Health Information Hub. Tools to Assess and Measure Social Determinants of Health. Available at: https://www.ruralhealthinfo.org/toolkits/sdoh/4/assessment-tools. Accessed February 22, 2022.
- 27.American Academy of Allergy, Asthma & Immunology. Episode 37: Impact of Disparities on Food Allergy. Available at: https://education.aaaai.org/podcasts/podcast_FAdisparities. Accessed February 22, 2022.
- 28.Dinakar C, Warady B. Food Allergy Care: It Takes a Team. Mo Med 2016;113: 314–9. [PMC free article] [PubMed] [Google Scholar]
- 29.EpiPen. Epinephrine in Schools. EpiPen4Schools. Available at: https://www.epipen.com/en/hcp/for-health-care-partners/for-school-nurses. Accessed February 22, 2022.
- 30.CodeAna. Available at: https://codeana.org. Accessed February 22, 2022.
- 31.Food Allergy Research & Education. Available at: https://www.foodallergy.org. Accessed February 22, 2022.
- 32.The FPIES Foundation. Available at: https://fpiesfoundation.org. Accessed February 22, 2022.
- 33.Food Equality Initiative. Available at: https://foodequalityinitiative.org/. Accessed February 22, 2022.
- 34.Digital Highlights Hub (McMichael) - YouTube, https://www.youtube.com/watch?v=qN56w76_GNQ. Accessed February 22, 2022.
- 35.New England Journal of Medicine. The Impact of Skin Color and Ethnicity on Clinical Diagnosis and Research. Available at: https://specialevents.nejm.org/impact-of-skin-color-and-ethnicity-on-clinical-diagnosis-and-research/. Accessed February 22, 2022.
- 36.National Eczema Association. Available at: www.nationaleczema.org. Accessed February 22, 2022.
- 37.International Eczema Society. Available at: www.eczemacouncil.org. Accessed February 22, 2022.
- 38.National Eczema Society. Available at: www.eczema.org. Accessed February 22, 2022.
- 39.Skin of Color Society. Available at: https://skinofcolorsociety.org/. Accessed February 22, 2022.
- 40.VisualDx. #ProjectIMPACT. Available at: https://www.visualdx.com/projectimpact/. Accessed February 22, 2022.
- 41.American Academy of Allergy, Asthma & Immunology. Episode 38: Asthma Disparities. Available at: https://education.aaaai.org/podcasts/podcast_AsthmaDisparities. Accessed February 22, 2022.
- 42.Children’s National. IMPACT DC. Available at: https://childrensnational.org/departments/impact-dc-asthma-clinic. Accessed February 22, 2022.
- 43.Asthma and Allergy Foundation of America. Available at: https://www.aafa.org. Accessed February 22, 2022.
- 44.Allergy and Asthma Network. Available at: https://allergyasthmanetwork.org. Accessed February 22, 2022.
- 45.American Academy of Allergy, Asthma & Immunology. AAAAI - The School-Based Allergy, Asthma and Anaphylaxis Management Program: Comprehensive Asthma Educational Resources. Available at: https://www.aaaai.org/Tools-for-the-Public/School-Tools/SAMPRO. Accessed February 22, 2022.
- 46.U.S. Environmental Protection Agency. EJScreen: Environmental Justice Screening and Mapping Tool. Available at: https://www.epa.gov/ejscreen. Accessed February 22, 2022.
- 47.American Academy of Allergy, Asthma & Immunology. AAAAI Education Center. Available at: https://education.aaaai.org. Accessed February 22, 2022.
- 48.Bias and Racism (Jones) - YouTube. Available at: https://www.youtube.com/watch?v=2YqxTp5VKo0. Accessed February 22, 2022.
- 49.Institute for Healthcare Improvement. Free Resources. Available at: http://www.ihi.org/resources/Pages/default.aspx. Accessed February 22, 2022.
- 50.Health Measures. PROMIS. Available at: https://www.healthmeasures.net/explore-measurement-systems/promis. Accessed February 22, 2022.
- 51.Agency for Healthcare Research and Quality. Health Cost and Utiloization Project. Available at: https://www.ahrq.gov/data/hcup/index.html. Accessed February 22, 2022.
- 52.Agency for Healthcare Research and Quality. National Healthcare Quality and Disparities Reports. Available at: https://www.ahrq.gov/research/findings/nhqrdr/index.html. Accessed February 22, 2022.
- 53.Patient-Centered Outcomes Research Institute. Homepage ǀ PCORI. Available at: https://www.pcori.org/. Accessed February 22, 2022.
- 54.National Institute on Minority Health and Health Disparities. HDPulse - Health Disparities Resources. Available at: https://hdpulse.nimhd.nih.gov/. Accessed February 22, 2022.
- 55.National Institute on Minority Health and Health Disparities. The Science of Health Disparties. Available at: https://www.nimhd.nih.gov/about/publications/the-science-of-health-disparities-research.html. Accessed February 22, 2022.
- 56.National Institute on Minority Health and Health Disparities. Health. Disparities Research Institute. Available at: https://www.nimhd.nih.gov/programs/edu-training/hdri/. Accessed February 22, 2022.
- 57.U.S. Department of Health and Human Services. Policy and Data. Available at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=1&lvlid=4. Accessed February 22, 2022.
- 58.Centers for Disease Control and Prevention. Core Health Equity Science and Intervention Strategy. Available at: https://www.cdc.gov/healthequity/core/index.html. Accessed February 22, 2022.
- 59.National Minority Quality Form. Available at: https://www.nmqf.org/. Accessed February 22, 2022.
- 60.Programs to Increase Diversity Among Individuals Engaged in Health Related Research (PRIDE). Research in Implementation Science for Equity (RISE). Available at: https://pridecc.wustl.edu/programs/research-in-implementation-science-for-equity. Accessed February 22, 2022.
- 61.HOPE Initiative. Home. Available at: https://www.hopeinitiative.org. Accessed February 22, 2022.
- 62.PhenX Toolkit. Available at: https://www.phenxtoolkit.org. Accessed February 22, 2022.
- 63.MRCT Center Diversity Project. Improve Diversity in Clinical Research. Available at: https://mrctcenter.org/diversity-in-clinical-research/. Accessed February 22, 2022.
- 64.Soklaridis S, Hunter JJ, Ravitz P. Twelve tips for asking and responding to difficult questions during a challenging clinical encounter. Med Teach 2014;36: 769–74. [DOI] [PubMed] [Google Scholar]
- 65.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008;23:561–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nutbeam D, McGill B, Premkumar P. Improving health literacy in community populations: a review of progress. Health Promot Int 2018;33: 901–11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


