Abstract
Ketogenic diets (KD) are dietary strategies low in carbohydrates, normal in protein, and high, normal, or reduced in fat with or without (Very Low-Calories Ketogenic Diet, VLCKD) a reduced caloric intake. KDs have been shown to be useful in the treatment of obesity, metabolic diseases and related disorders, neurological diseases, and various pathological conditions such as cancer, nonalcoholic liver disease, and chronic pain. Several studies have investigated the intracellular metabolic pathways that contribute to the beneficial effects of these diets. Although epigenetic changes are among the most important determinants of an organism’s ability to adapt to environmental changes, data on the epigenetic changes associated with these dietary pathways are still limited. This review provides an overview of the major epigenetic changes associated with KDs.
Keywords: ketogenic diet, Very Low-Calories Ketogenic Diet, DNA methylation, histone modifications, miRNAs
1. Introduction
Ketogenic diets (KD) are a group of diets characterized by low carbohydrate, normal protein, and high fat content. This combination of macronutrients aims to force the body to break down fat instead of glucose to synthesize adenosine triphosphate, inducing ketosis [1] and mimicking the metabolic state of starvation or fasting. In general, urinary ketone levels can be used as an indicator of dietary adherence [2]. Several variations of the KD have been proposed [3]. The best studied is a KD with a 4:1 or 3:1 ratio of dietary fat to combined dietary protein and carbohydrate, sometimes referred to as a “classic” KD [3].
The earliest evidence showing the role of a ketogenic diet dates back to the 1920s, when it was discovered that by eliminating carbohydrates from the diet, the metabolic effects of fasting could be mimicked. KD results in a marked increase in circulating concentrations of β-hydroxybutyrate (β-HB) [4]. β-HB is the main representative of ketone bodies in animal cells, and its baseline concentrations in serum are in the micromolar range in humans. During fasting or after carbohydrate-free KD, serum concentrations of β-HB can rise well above 2 mM [5].
This dietary approach was first used in pediatrics to treat drug-resistant epilepsies [6]. Later, the studies of Cahill and his group were critical in clarifying the physiology of starvation and the protein-sparing effects of ketosis [7,8]. The authors demonstrated that ketones reduce muscle protein breakdown during starvation by providing alternative fuel to the brain, thereby reducing the need for gluconeogenesis. In addition, the decrease in insulin levels caused by caloric deprivation and carbohydrate restriction allows the production of glucose through glycogenolysis and gluconeogenesis to fuel the brain. In addition, free fatty acids are released from adipose tissue and used as a substrate for the liver production of ketone bodies (acetoacetate, beta-hydroxybutyrate, and acetone). These molecules gradually become an alternative source of energy for the body and brain [8,9]. Finally, the metabolic changes induced by fasting, due to the anorexic properties of ketone bodies, allow a reduction in the sensation of hunger and reduce protein breakdown in the body, allowing the organism to survive [10]. This model has been defined as “Protein Sparing Modified Fast” (PSMF) and consists of a highly hypocaloric diet, based mainly on an adequate intake of proteins and essential fatty acids, which allows rapid weight loss while maintaining muscle mass [11]. This type of treatment may even be therapeutic in certain pathological conditions [12].
The Very Low-Calorie Ketogenic Diet (VLCKD) is a nutritional intervention characterized by a very low carbohydrate content (equivalent to 5–10% of the total daily caloric intake or 30–50 g of carbohydrate per day [13,14]), a low fat content, and a high-biological-value protein content of 0.8 to 1.2 g/kg of ideal body weight [15]. VLCKD promotes metabolic changes and optimizes energy metabolism by simulating the effects of fasting, with a drastic restriction of the daily carbohydrate intake and a relative proportional increase of fats and proteins for a total caloric intake of about 800 kcal/day [16,17].
In the past century, the use of diets with very severe caloric restriction was not uncommon. In some cases, the treatment consisted in the administration of water-only diets and total fasting (with or without vitamin supplements, depending on the duration of the diet) [10]. The first report on the effects of prolonged fasting was published by Benedict in 1915 [18], followed by Keys in 1940 [19]. Both authors found that fasting resulted in weight loss in normal-weight individuals, mainly at the expense of lean mass [18,19]. In subsequent years, treatment of obesity by complete fasting was introduced [20,21]. In obese individuals, the weight loss induced by fasting was less relevant in terms of fat-free mass consumption due to increased fat reserves. Consequently, in these individuals, the duration of fasting could be extended from two months (in lean individuals) [22] to almost one year [23]. Complete [23,24] or intermittent [25,26] fasting was then more commonly used to treat obesity. Although fasting diets were generally well tolerated, they were associated with several adverse effects, including malnutrition, rapid weight loss, heart disease, hypotension, and hypoglycemia [10,27,28].
Nowadays, KD and VLCKD are considered valid therapeutic options in various clinical situations, including severe obesity, obesity in the presence of concomitant diseases, hepatic steatosis, polycystic ovary syndrome, drug-resistant epilepsy, migraine, and in the preoperative management of bariatric surgery [16,29]. In recent years, increasing scientific evidence has favored the rediscovery of KD and VLCKD, and these approaches have been proposed as attractive nutritional strategies for the treatment of obesity in individuals who have already tried unsuccessfully to lose weight with more balanced diets [16]. In addition, KD and VLCKD have been shown to have beneficial effects on body composition, the metabolic profile, and the expression of genes related to inflammation and oxidative stress [16,29,30,31].
Although KD and VLCKD are now widely used to prevent and treat various clinical conditions [1], the molecular mechanisms underlying the beneficial effects of these diets are still largely unknown. This is a very critical issue, as the characterization of these mechanisms could enable the development of potential long-term therapeutic options to extend the benefits of carbohydrate restriction after diet discontinuation [32].
The epigenome is a link between an individual’s genetic background and the environment, and it determines an organism’s ability to respond and adapt to changes in the environment [33]. Diet is among the most important epigenetic modulators [34,35], and increasing evidence suggests that epigenetic changes are associated with nutritional deficiency or supplementation [36,37] and with ketogenic diets [38,39,40,41,42].
The term epigenetics refers to heritable changes in gene expression without changes in DNA sequence. Major epigenetic mechanisms include DNA methylation, histone modifications, microRNA, and chromatin remodeling. All of these mechanisms can bidirectionally affect the state of chromatin by changing it from “closed”, which restricts the access of transcription proteins, to “open”, which allows the access of transcription factors [43] and the initiation of transcription.
In the next pages, we will examine the epigenetic changes induced by KD and VLCKD, as these may be among the mechanisms by which KD and VLKD achieve their beneficial effects.
2. DNA Methylation
DNA methylation is the most studied epigenetic modification. It consists in the transfer of a methyl group from the main methyl-donor, S-adenosylmethionine (SAM), to the C5 position of cytosine within CpG dinucleotides and the formation of 5-methylcytosine [44]. This process is mediated by the action of enzymes belonging to the family of DNA methyltransferases (DNMTs) [45].
Most of the available information on the effects of KD on DNA methylation comes from a rat model suffering from chronic epilepsy or from the adjuvant treatment in drug-resistant epilepsy [46]. Administration of a ketogenic, high-fat, low-carbohydrate diet to these animals attenuated seizure progression and reduced the global DNA methylation status [47]. These effects are likely related to the KD-induced increase in adenosine in the hippocampus [48,49]: increased adenosine promotes the formation of S-adenosylhomocysteine (SAH) [50], which in turn blocks DNA methyltransferase [51], reducing global DNA methylation [50,52]. Global DNA hypermethylation has been found in patients with temporal lobe epilepsy [53], and increased concentrations of adenosine in the brain observed after KD have been proposed as the main mechanisms by which this diet improves the clinical picture in patients with drug-resistant epilepsy [52,54,55].
Complex changes in DNA methylation patterns have also been found during aging [56,57] and have been associated with various age-related diseases [39]. It has been suggested that KD or exogenous ketogenic supplements [58] may promote anti-aging effects [58,59,60,61]. It is likely that these effects occur via the modulation of the DNA methylation of the same genes that respond to changes in brain adenosine levels [50,57], including KLF14, ELOVL2, FHL2, OTUD7A, SLC12A5, ZYG11A, and CCDC102B genes [57].
Recently, an interesting study was published examining the effects of VLCKD for the treatment of obesity on DNA methylation patterns [62]. In the study, 850,000 CpG sites were compared, using a dedicated array-based platform, between twenty-one patients with obesity after six months of VLCKD and twelve normal-weight volunteers. After weight reduction by VLCKD, differences were found in 988 CpG sites (786 unique genes) whose methylation patterns resembled those of normal-weight volunteers, suggesting the downregulation of DNMT1, DNMT3a, and DNMT3b gene expression [62]. Several of the genes whose methylation status changed were involved in metabolic processes, protein metabolism, and the development of muscles, organs, and skeletal system development, confirming the hypothesis of epigenetic dysregulation in the adipose tissue of subjects with obesity [63,64]. In addition, changes in the methylation status were also detected in some novel genes, including ZNF331, FGFRL1, CBFA2T3, C3orf38, JSRP1, and LRFN4, whose methylation status was specifically associated with VLCKD-induced weight loss and/or ketosis [62].
It is well known that a specific methylation profile is associated not only with obesity in various tissues [65,66,67,68,69,70,71], but also with complications of obesity such as insulin resistance [63] and cancer [72,73]. Therefore, it is possible to hypothesize that one of the mechanisms by which VLCKD contributes to the maintenance of weight loss in the treatment of obesity is related to the changes in DNA methylation that this diet may induce [31,74].
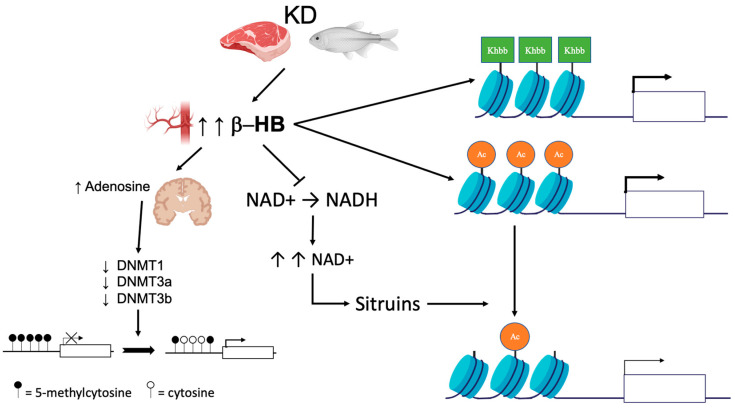
The described effects of KD/VLCKD on DNA methylation are shown in Figure 1. Data in the literature suggest that the effects on DNA methylation caused by KD or VLCKD may be various and more complex than those reported so far; therefore, additional studies are needed to clarify these interplays.
Figure 1.
Epigenetic changes induced by KD. KD leads to an increase in circulating ketone bodies (β-hydroxybutyrate [β-HB]). In the brain, higher concentrations of β-HB have inhibitory effects on DNA methyltransferases (DNMT) via an increase in adenosine, which in turn leads to global DNA hypomethylation. Ketone bodies also act as epigenetic modifiers that determine covalent modifications at key histones such as lysine acetylation (Ac), methylation, and β-hydroxybutyrylation (Kbhb). Finally, β-HB is less efficient than glucose as a substrate for NADH production. The increase in the NAD + level promotes histone demethylation via the modulation of sirtuin activity.
3. Histone Modifications
The genetic information in the nucleus of eukaryotic cells is organized in a highly conserved structural polymer called chromatin [75]. The basic unit of chromatin is the nucleosome. The nucleosome consists of 147 bp of DNA wrapped around an octamer of histones composed of two H3/H4 dimers and two H2A/H2B dimers [33]. The dynamic and reversible modifications of histone proteins influence all DNA-based processes, including DNA packaging and chromatin compaction, nucleosome dynamics, and transcription [76,77]. This process is regulated by several post-translational modifications, most of which occur within the amino terminal in histone tails [78].
Recently, ketone bodies have been shown to act as epigenetic modifiers that determine covalent modifications at key histones [4,40,79]. These include lysine acetylation, methylation, and a novel epigenetic modification, lysine β-hydroxybutyrylation (Kbhb) [80]. Since Kbhb sites overlap with lysine residues, this novel histone modification integrates the classic histone lysine acetylation, methylation, and histone phosphorylation and ubiquitination, producing changes in the chromatin status (Figure 1). Generally, a genome-wide analysis (ChIP-swq) associated with transcriptional profiling revealed that the β-hydroxybutyrylation of histones is associated with active gene transcription. In liver from mice undergoing long-term fasting or streptozotocin-induced diabetic ketoacidosis, histone lysines susceptible to beta-hydroxybutyrylation were identified, including H1K168, H2AK5/K125, H2BK20, H3K4/K9/K14/K23, and H4K8/K12 [4]. In their study, the authors demonstrate that upregulated genes bearing the H3K9ac and H3K4me3 marks are different from those carrying the H3K9bhb mark, suggesting that histone Kbhb has different transcriptional-promoting functions than histone acetylation and methylation [80,81].
The effects of D-3-hydroxybutyric acid (BHB), one of the most abundant ketone bodies, on the establishment of histone tails’ posttranslational modifications are very controversial. Initially, BHB was considered an endogenous inhibitor of class I and class II histone deacetylases (HDACs); indeed, it has been shown that BHB treatment, in HEK293 cells or high levels of BHB produced by a subcutaneous pump delivery in C57BL6/J mice maintained on caloric restriction [82,83], produced a dose-dependent histone hyperacetylation, especially on lysine 9 and 14 of histone 3 (H3K9/K14). Other studies suggest that BHB only induces very marginal changes in the acetylation patterns, i.e., experiments conducted in various cell lines such as HEK293 cells, myotubes (L6), and endothelial cells (HMEC-1) showed that BHB administration had no effect on histone acetylation and did not inhibit histone deacetylase catalytic activity [84].
Understanding the effect of BHB on chromatin acetylation patterns is complicated by the NAD+/NADH ratio, which depends significantly on the presence of BHB or glucose.
BHB can substitute glucose as fuel; however, while glucose is able to produce four moles of NADH from NAD+, BHB is able to reduce only two moles of NAD+. The excess of the NAD+ resulting from the ketogenic diet modulates the activity of NAD+-dependent enzymes such as the Sirtuin proteins (SIRT1-7), which are involved in the deacetylation process [85] (Figure 1).
Mice fed a ketogenic, low-carbohydrate diet showed a global increase in protein acetylation. These changes were accompanied by modifications in the regulation of rapamycin complex 1 (mTORC1), and in older animals, motor function and memory were preserved and tumor incidence was lower [60]. Similarly, obesity, higher mortality, and age-related memory loss were prevented in mice fed a cyclic (every two weeks) ketogenic diet [83]. These effects have been linked to the downregulation of genes involved in fatty acid metabolism and the upregulation of Peroxisome Proliferator-Activated Receptor alpha (PPAR-) target genes [83], mechanisms that have been shown to be closely linked to epigenetic changes, at least in adipose tissue [64,86].
Further evidence for the role of epigenetic regulation by KD has been obtained in several mouse models. In mice exposed to hypobaric hypoxia, KD increased histone acetylation and rescued spatial memory impairment [87]. Moreover, in Kmt2d(+/betaGeo), a mouse model with Kabuki syndrome, KD had the same effect as the administration of AR-42, a histone deacetylase inhibitor that promotes chromatin opening and rescues both the neurogenesis defect and hippocampal memory impairment. These effects are mediated via an increase in βOHB, which in turn modulates H3 acetylase and H3K4me3 [88].
4. MicroRNAs
MicroRNAs (miRNAs) are small non-coding RNAs consisting of about 20–22 nucleotides [89]. miRNAs are formed during the processing of longer RNA transcripts [90] and regulate gene expression by binding to target mRNAs to modulate their stability, adjust their intracellular concentrations, and control their translation into proteins [89,91]. It is estimated that only a few hundred miRNAs regulate between 30 and 80% of the genes encoded in the human genome [92]. Numerous miRNAs have been identified in human adipose tissue, and recent data suggest that there are several circulating miRNAs that are differentially expressed and can be detected in the serum of people with obesity compared with lean people. These can be used to predict the risk of obesity-related complications and to monitor the outcomes of weight loss interventions [93]. In addition, miRNAs have emerged as attractive therapeutic agents for various diseases in recent years, and miRNA-based therapeutic tools have been tested in preclinical studies and clinical trials [93]. Finally, recent preliminary findings by Caradonna and coworkers suggest that circulating miRNA levels may be modulated by specific dietary interventions [94]. Many of them, like the Mediterranean Diet, have been demonstrated to protect from chronic degenerative diseases and have also been proposed as an additional therapeutic option in several clinical conditions, suggesting possible links between miRNA, diet, and aging or age-related inflammation [94,95].
In animal models, caloric restriction has been shown to modulate circulating microRNAs. A very recent study examined miRNA levels in the serum and tissues of mice fed 40% CR for 28 days [96]. The results showed that miR-16-5p, miR-196b-5p, and miR-218-5p were increased in serum and that miR-16-5p was also increased in the spleen, thymus, colon, and stomach of CR animals. Of note, miR-16-5p is able to downregulate the expression of inflammatory cytokines, suggesting that CR can indirectly modulate inflammation [96].
To date, few human studies have investigated the effects of KD or VLCKD on miRNA. In 2019, Cannataro and coworkers examined the miRNA profile of 36 subjects with obesity who underwent six weeks of biphasic KD. The authors examined 799 circulating miRNAs and found that changes in only three of them (hsa-let-7b-5p, hsa-miR-143-3p, and hsa-miR-504-5p) were associated with KD in a sex-independent manner. The targets of these miRNAs were involved in cytokine signaling pathways, nutrient metabolism, oxidative phosphorylation, functional regulation of PPARs, and insulin signaling [97]. The same authors have also shown that miRNAs associated with antioxidant and anti-inflammatory signaling pathways are altered in individuals with obesity but return to levels comparable to those of lean individuals after KD [98].
Considering the multiple potential targets of these miRNAs, it is possible to use KD and VLCKD as an adjuvant therapeutic option in various diseases, including neurological disorders and cancer [97].
5. Conclusions
The data presented here suggest that KD and VLCKD achieve some of their beneficial effects via the modulation of the epigenome, resulting in changes in DNA methylation, histone modifications, and miRNA levels (Table 1). Although the data presented here are still preliminary and limited to a few reports, the relationship between ketosis and epigenetic changes is very interesting, and this area clearly needs further investigation.
Table 1.
Epigenetic changes determined by KD.
| Epigenetic Modifications | Effect of Ketosis | Possible Mechanisms | Subject of Investigation |
Refs |
|---|---|---|---|---|
| DNA methylation |
Global DNA hypomethylation | Increased brain adenosine | Rats | [47] |
| Human | [52,54,55] | |||
| Modulation of genes regulating DNA methylation |
Rats | [50] | ||
| Human | [57] | |||
| Downregulation of DNMT1, DNMT3a, and DNMT3b | Human (subjects with obesity) | [62] | ||
| Histone modifications |
Covalent modifications to key histones | Lysine acetylation, methylation, and β-hydroxybutyrylation |
Cell lines | [79] |
| HEK293 cell, mice | [4,40,80] | |||
| βOHB inhibits class I histone deacetylases | Cell lines | [40] | ||
| βOHB increases histone acetylation | HEK293 cell line | [2,82] | ||
| Sirtuins-mediated histone deacetylation | Cell lines | [40] | ||
| Global increase in protein acetylation | Mice | [60] | ||
| Increased the levels of histone acetylation | Rats | [87] | ||
| miRNAs | Elevation of miR-16-5p, miR-196b-5p, and miR-218-5p |
Unknown. Changes in these miRNAs are determined by caloric restriction. |
Mice | [96] |
| Modifications in hsa-let-7b-5p, hsa-miR-143-3p, and hsa-miR-504-5p |
Unknown. The target genes of the miRNAs are associated with obesity and metabolism-related pathways. | Human | [97] |
A better understanding of the relationship between diet, obesity, and epigenetic changes induced by KD or VLCKD could have important consequences for elucidating the effects of ketosis, not only in terms of weight loss but also for the possible use of KD or VLCKD as supportive treatment for various diseases, as well as to reduce the side effects associated with these diets. Indeed, several reports have indicated that KD or VLCKD are associated with some adverse effects. Constipation, headache, bad breath, muscle cramps, diarrhea, vomiting, and general weakness have been reported during the first few weeks of the diet. These symptoms, termed “keto flu,” are among the factors that may limit adherence to these diets [99,100]. In addition, some important potential cardiovascular side effects of KD have also been reported [100]. These include an increase in triglycerides and low-density lipoprotein (LDL) cholesterol [101], a transient increase in endothelial dysfunction [102], an increase in cardiac insulin resistance [103], and various others side effects [99,100]. There are no data in the literature examining the molecular mechanisms by which KD and VLCKD contribute to these adverse effects, and it cannot be ruled out that these mechanisms are also mediated by the modulation of the epigenome.
It is possible that additional strategies to stabilize the epigenetic changes induced by ketosis may contribute to the long-term success of KD. Among other things, it cannot be ruled out that combining KD/VLCKD with other nutrients whose consumption has been shown to have epigenetic effects may help to enhance and/or stabilize epigenetic changes and thus support the success of nutritional programs. This could enhance and prolong the global chromatin changes induced by ketosis, thus promoting the beneficial effects associated with these diets. In conclusion, this is a new field of research that will open up interesting possibilities for the treatment and prevention of obesity, metabolic disorders, and various chronic diseases in the near future.
Author Contributions
Conceptualization, P.U., A.C. and P.E.M.; PubMed search, P.U., I.C.N., F.F. and G.P.; writing—draft preparation, P.U., I.C.N., F.F. and P.E.M.; writing—review and editing, P.U., G.M. and P.E.M.; supervision and critical revision, P.U. and P.E.M.; funding acquisition, P.E.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was partially funded by the project entitled “Nanofotonica per nuovi approcci diagnostici e terapEutici in Oncologia e Neurologia (NeON)” and by the project PRIN2017 Protocollo# 20173CRP3H_002, entitled “nanoPhotonIc plaTforms for ultraSensiTive Liquid BiOPsy (PIT STOP)”, both from the Ministero dell’Istruzione, Università e Ricerca to P.E.M.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Crosby L., Davis B., Joshi S., Jardine M., Paul J., Neola M., Barnard N.D. Ketogenic Diets and Chronic Disease: Weighing the Benefits against the Risks. Front. Nutr. 2021;8:702802. doi: 10.3389/fnut.2021.702802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Newman J.C., Verdin E. beta-Hydroxybutyrate: A Signaling Metabolite. Annu. Rev. Nutr. 2017;37:51–76. doi: 10.1146/annurev-nutr-071816-064916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roehl K., Sewak S.L. Practice Paper of the Academy of Nutrition and Dietetics: Classic and Modified Ketogenic Diets for Treatment of Epilepsy. J. Acad. Nutr. Diet. 2017;117:1279–1292. doi: 10.1016/j.jand.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Dabek A., Wojtala M., Pirola L., Balcerczyk A. Modulation of Cellular Biochemistry, Epigenetics and Metabolomics by Ketone Bodies. Implications of the Ketogenic Diet in the Physiology of the Organism and Pathological States. Nutrients. 2020;12:788. doi: 10.3390/nu12030788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mierziak J., Burgberger M., Wojtasik W. 3-Hydroxybutyrate as a Metabolite and a Signal Molecule Regulating Processes of Living Organisms. Biomolecules. 2021;11:402. doi: 10.3390/biom11030402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilder R.M. The effects of ketonemia on the course of epilepsy. Mayo. Clin. Bull. 1921;2:307–308. [Google Scholar]
- 7.Cahill G.F., Jr. Starvation in man. N. Engl. J. Med. 1970;282:668–675. doi: 10.1016/S0300-595X(76)80028-X. [DOI] [PubMed] [Google Scholar]
- 8.Cahill G.F., Jr. Fuel metabolism in starvation. Annu. Rev. Nutr. 2006;26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258. [DOI] [PubMed] [Google Scholar]
- 9.Longo V.D., Mattson M.P. Fasting: Molecular mechanisms and clinical applications. Cell Metab. 2014;19:181–192. doi: 10.1016/j.cmet.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casanueva F.F., Castellana M., Bellido D., Trimboli P., Castro A.I., Sajoux I., Rodriguez-Carnero G., Gomez-Arbelaez D., Crujeiras A.B., Martinez-Olmos M.A. Ketogenic diets as treatment of obesity and type 2 diabetes mellitus. Rev. Endocr. Metab. Disord. 2020;21:381–397. doi: 10.1007/s11154-020-09580-7. [DOI] [PubMed] [Google Scholar]
- 11.Bistrian B.R., Blackburn G.L., Flatt J.P., Sizer J., Scrimshaw N.S., Sherman M. Nitrogen metabolism and insulin requirements in obese diabetic adults on a protein-sparing modified fast. Diabetes. 1976;25:494–504. doi: 10.2337/diab.25.6.494. [DOI] [PubMed] [Google Scholar]
- 12.Cahill G.F., Jr., Herrera M.G., Morgan A.P., Soeldner J.S., Steinke J., Levy P.L., Reichard G.A., Jr., Kipnis D.M. Hormone-fuel interrelationships during fasting. J. Clin. Investig. 1966;45:1751–1769. doi: 10.1172/JCI105481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phinney S.D., Bistrian B.R., Wolfe R.R., Blackburn G.L. The human metabolic response to chronic ketosis without caloric restriction: Physical and biochemical adaptation. Metabolism. 1983;32:757–768. doi: 10.1016/0026-0495(83)90105-1. [DOI] [PubMed] [Google Scholar]
- 14.Yancy W.S., Jr., Olsen M.K., Guyton J.R., Bakst R.P., Westman E.C. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: A randomized, controlled trial. Ann. Intern. Med. 2004;140:769–777. doi: 10.7326/0003-4819-140-10-200405180-00006. [DOI] [PubMed] [Google Scholar]
- 15.Napoleao A., Fernandes L., Miranda C., Marum A.P. Effects of Calorie Restriction on Health Span and Insulin Resistance: Classic Calorie Restriction Diet vs. Ketosis-Inducing Diet. Nutrients. 2021;13:1302. doi: 10.3390/nu13041302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muscogiuri G., Barrea L., Laudisio D., Pugliese G., Salzano C., Savastano S., Colao A. The management of very low-calorie ketogenic diet in obesity outpatient clinic: A practical guide. J. Transl. Med. 2019;17:356. doi: 10.1186/s12967-019-2104-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caprio M., Infante M., Moriconi E., Armani A., Fabbri A., Mantovani G., Mariani S., Lubrano C., Poggiogalle E., Migliaccio S., et al. Very-low-calorie ketogenic diet (VLCKD) in the management of metabolic diseases: Systematic review and consensus statement from the Italian Society of Endocrinology (SIE) J. Endocrinol. Investig. 2019;42:1365–1386. doi: 10.1007/s40618-019-01061-2. [DOI] [PubMed] [Google Scholar]
- 18.Benedict F.G., Goodall H.W., Ash J.E., Langfeld H.S., Kendall A.I., Higgins H.L. A Study of Prolonged Fasting. Carnegie Institution of Washington; Washington, DC, USA: 1915. p. 416. [Google Scholar]
- 19.Keys A.B., Brozek J., Henschel A. The Biology of Human Starvation. University of Minnesota Press; Minneapolis, MN, USA: 1950. p. 2v. (1385p). [Google Scholar]
- 20.Bloom W.L. Fasting as an introduction to the treatment of obesity. Metabolism. 1959;8:214–220. [PubMed] [Google Scholar]
- 21.Drenick E.J., Swendseid M.E., Blahd W.H., Tuttle S.G. Prolonged Starvation as Treatment for Severe Obesity. JAMA. 1964;187:100–105. doi: 10.1001/jama.1964.03060150024006. [DOI] [PubMed] [Google Scholar]
- 22.Leiter L.A., Marliss E.B. Survival during fasting may depend on fat as well as protein stores. JAMA. 1982;248:2306–2307. doi: 10.1001/jama.1982.03330180066037. [DOI] [PubMed] [Google Scholar]
- 23.Stewart W.K., Fleming L.W. Features of a successful therapeutic fast of 382 days’ duration. Postgrad. Med. J. 1973;49:203–209. doi: 10.1136/pgmj.49.569.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomson T.J., Runcie J., Miller V. Treatment of obesity by total fasting for up to 249 days. Lancet. 1966;2:992–996. doi: 10.1016/S0140-6736(66)92925-4. [DOI] [PubMed] [Google Scholar]
- 25.Duncan G.G., Jenson W.K., Fraser R.I., Cristofori F.C. Correction and control of intractable obesity. Practicable application of intermittent periods of total fasting. JAMA. 1962;181:309–312. doi: 10.1001/jama.1962.03050300029006. [DOI] [PubMed] [Google Scholar]
- 26.Gilliland I.C. Total fasting in the treatment of obesity. Postgrad. Med. J. 1968;44:58–61. doi: 10.1136/pgmj.44.507.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomas D.D., Istfan N.W., Bistrian B.R., Apovian C.M. Protein sparing therapies in acute illness and obesity: A review of George Blackburn’s contributions to nutrition science. Metabolism. 2018;79:83–96. doi: 10.1016/j.metabol.2017.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Longo V.D., Di Tano M., Mattson M.P., Guidi N. Intermittent and periodic fasting, longevity and disease. Nat. Aging. 2021;1:47–59. doi: 10.1038/s43587-020-00013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castellana M., Biacchi E., Procino F., Casanueva F.F., Trimboli P. Very-low-calorie ketogenic diet for the management of obesity, overweight and related disorders. Minerva Endocrinol. 2021;46:161–167. doi: 10.23736/S2724-6507.20.03356-8. [DOI] [PubMed] [Google Scholar]
- 30.Merra G., Gratteri S., De Lorenzo A., Barrucco S., Perrone M.A., Avolio E., Bernardini S., Marchetti M., Di Renzo L. Effects of very-low-calorie diet on body composition, metabolic state, and genes expression: A randomized double-blind placebo-controlled trial. Eur. Rev. Med. Pharm. Sci. 2017;21:329–345. [PubMed] [Google Scholar]
- 31.Castellana M., Conte E., Cignarelli A., Perrini S., Giustina A., Giovanella L., Giorgino F., Trimboli P. Efficacy and safety of very low calorie ketogenic diet (VLCKD) in patients with overweight and obesity: A systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 2020;21:5–16. doi: 10.1007/s11154-019-09514-y. [DOI] [PubMed] [Google Scholar]
- 32.Boison D. New insights into the mechanisms of the ketogenic diet. Curr. Opin. Neurol. 2017;30:187–192. doi: 10.1097/WCO.0000000000000432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Russo G.L., Vastolo V., Ciccarelli M., Albano L., Macchia P.E., Ungaro P. Dietary polyphenols and chromatin remodeling. Crit. Rev. Food Sci. Nutr. 2017;57:2589–2599. doi: 10.1080/10408398.2015.1062353. [DOI] [PubMed] [Google Scholar]
- 34.Vastolo V., Nettore I.C., Ciccarelli M., Albano L., Raciti G.A., Longo M., Beguinot F., Ungaro P. High-fat diet unveils an enhancer element at the Ped/Pea-15 gene responsible for epigenetic memory in skeletal muscle. Metabolism. 2018;87:70–79. doi: 10.1016/j.metabol.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 35.Nettore I.C., Rocca C., Mancino G., Albano L., Amelio D., Grande F., Puoci F., Pasqua T., Desiderio S., Mazza R., et al. Quercetin and its derivative Q2 modulate chromatin dynamics in adipogenesis and Q2 prevents obesity and metabolic disorders in rats. J. Nutr. Biochem. 2019;69:151–162. doi: 10.1016/j.jnutbio.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 36.Ideraabdullah F.Y., Zeisel S.H. Dietary Modulation of the Epigenome. Physiol. Rev. 2018;98:667–695. doi: 10.1152/physrev.00010.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ciccarelli M., Vastolo V., Albano L., Lecce M., Cabaro S., Liotti A., Longo M., Oriente F., Russo G.L., Macchia P.E., et al. Glucose-induced expression of the homeotic transcription factor Prep1 is associated with histone post-translational modifications in skeletal muscle. Diabetologia. 2016;59:176–186. doi: 10.1007/s00125-015-3774-6. [DOI] [PubMed] [Google Scholar]
- 38.Jaworski D.M., Namboodiri A.M., Moffett J.R. Acetate as a Metabolic and Epigenetic Modifier of Cancer Therapy. J. Cell Biochem. 2016;117:574–588. doi: 10.1002/jcb.25305. [DOI] [PubMed] [Google Scholar]
- 39.Moreno C.L., Mobbs C.V. Epigenetic mechanisms underlying lifespan and age-related effects of dietary restriction and the ketogenic diet. Mol. Cell Endocrinol. 2017;455:33–40. doi: 10.1016/j.mce.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 40.Ruan H.B., Crawford P.A. Ketone bodies as epigenetic modifiers. Curr. Opin. Clin. Nutr. Metab. Care. 2018;21:260–266. doi: 10.1097/MCO.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 41.Bandera-Merchan B., Boughanem H., Crujeiras A.B., Macias-Gonzalez M., Tinahones F.J. Ketotherapy as an epigenetic modifier in cancer. Rev. Endocr. Metab. Disord. 2020;21:509–519. doi: 10.1007/s11154-020-09567-4. [DOI] [PubMed] [Google Scholar]
- 42.Lorenzo P.M., Crujeiras A.B. Potential effects of nutrition-based weight loss therapies in reversing obesity-related breast cancer epigenetic marks. Food Funct. 2021;12:1402–1414. doi: 10.1039/D0FO01984D. [DOI] [PubMed] [Google Scholar]
- 43.Han J.M., Yoon Y.S. Epigenetic landscape of pluripotent stem cells. Antioxid. Redox Signal. 2002;17:205–223. doi: 10.1089/ars.2011.4375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moore L.D., Le T., Fan G. DNA methylation and its basic function. Neuropsychopharmacology. 2013;38:23–38. doi: 10.1038/npp.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lyko F. The DNA methyltransferase family: A versatile toolkit for epigenetic regulation. Nat. Rev. Genet. 2018;19:81–92. doi: 10.1038/nrg.2017.80. [DOI] [PubMed] [Google Scholar]
- 46.Gough S.M., Casella A., Ortega K.J., Hackam A.S. Neuroprotection by the Ketogenic Diet: Evidence and Controversies. Front. Nutr. 2021;8:782657. doi: 10.3389/fnut.2021.782657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kobow K., Kaspi A., Harikrishnan K.N., Kiese K., Ziemann M., Khurana I., Fritzsche I., Hauke J., Hahnen E., Coras R., et al. Deep sequencing reveals increased DNA methylation in chronic rat epilepsy. Acta Neuropathol. 2013;126:741–756. doi: 10.1007/s00401-013-1168-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lusardi T.A., Akula K.K., Coffman S.Q., Ruskin D.N., Masino S.A., Boison D. Ketogenic diet prevents epileptogenesis and disease progression in adult mice and rats. Neuropharmacology. 2015;99:500–509. doi: 10.1016/j.neuropharm.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Masino S.A., Li T., Theofilas P., Sandau U.S., Ruskin D.N., Fredholm B.B., Geiger J.D., Aronica E., Boison D. A ketogenic diet suppresses seizures in mice through adenosine A(1) receptors. J. Clin. Investig. 2011;121:2679–2683. doi: 10.1172/JCI57813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams-Karnesky R.L., Sandau U.S., Lusardi T.A., Lytle N.K., Farrell J.M., Pritchard E.M., Kaplan D.L., Boison D. Epigenetic changes induced by adenosine augmentation therapy prevent epileptogenesis. J. Clin. Investig. 2013;123:3552–3563. doi: 10.1172/JCI65636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.James S.J., Melnyk S., Pogribna M., Pogribny I.P., Caudill M.A. Elevation in S-adenosylhomocysteine and DNA hypomethylation: Potential epigenetic mechanism for homocysteine-related pathology. J. Nutr. 2002;132:2361S–2366S. doi: 10.1093/jn/132.8.2361S. [DOI] [PubMed] [Google Scholar]
- 52.Chen F., He X., Luan G., Li T. Role of DNA Methylation and Adenosine in Ketogenic Diet for Pharmacoresistant Epilepsy: Focus on Epileptogenesis and Associated Comorbidities. Front. Neurol. 2019;10:119. doi: 10.3389/fneur.2019.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kobow K., Blumcke I. The emerging role of DNA methylation in epileptogenesis. Epilepsia. 2012;53((Suppl. 9)):11–20. doi: 10.1111/epi.12031. [DOI] [PubMed] [Google Scholar]
- 54.Schoeler N.E., Cross J.H. Ketogenic dietary therapies in adults with epilepsy: A practical guide. Pract. Neurol. 2016;16:208–214. doi: 10.1136/practneurol-2015-001288. [DOI] [PubMed] [Google Scholar]
- 55.Martin K., Jackson C.F., Levy R.G., Cooper P.N. Ketogenic diet and other dietary treatments for epilepsy. Cochrane Database Syst. Rev. 2016;2:CD001903. doi: 10.1002/14651858.CD001903.pub3. [DOI] [PubMed] [Google Scholar]
- 56.Romanov G.A., Vanyushin B.F. Methylation of reiterated sequences in mammalian DNAs. Effects of the tissue type, age, malignancy and hormonal induction. Biochim. Biophys. Acta. 1981;653:204–218. doi: 10.1016/0005-2787(81)90156-8. [DOI] [PubMed] [Google Scholar]
- 57.Florath I., Butterbach K., Muller H., Bewerunge-Hudler M., Brenner H. Cross-sectional and longitudinal changes in DNA methylation with age: An epigenome-wide analysis revealing over 60 novel age-associated CpG sites. Hum. Mol. Genet. 2014;23:1186–1201. doi: 10.1093/hmg/ddt531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kovacs Z., Brunner B., Ari C. Beneficial Effects of Exogenous Ketogenic Supplements on Aging Processes and Age-Related Neurodegenerative Diseases. Nutrients. 2021;13:2197. doi: 10.3390/nu13072197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Han Y.M., Ramprasath T., Zou M.H. beta-hydroxybutyrate and its metabolic effects on age-associated pathology. Exp. Mol. Med. 2020;52:548–555. doi: 10.1038/s12276-020-0415-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roberts M.N., Wallace M.A., Tomilov A.A., Zhou Z., Marcotte G.R., Tran D., Perez G., Gutierrez-Casado E., Koike S., Knotts T.A., et al. A Ketogenic Diet Extends Longevity and Healthspan in Adult Mice. Cell Metab. 2018;27:1156. doi: 10.1016/j.cmet.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Veech R.L., Bradshaw P.C., Clarke K., Curtis W., Pawlosky R., King M.T. Ketone bodies mimic the life span extending properties of caloric restriction. IUBMB Life. 2017;69:305–314. doi: 10.1002/iub.1627. [DOI] [PubMed] [Google Scholar]
- 62.Crujeiras A.B., Izquierdo A.G., Primo D., Milagro F.I., Sajoux I., Jacome A., Fernandez-Quintela A., Portillo M.P., Martinez J.A., Martinez-Olmos M.A., et al. Epigenetic landscape in blood leukocytes following ketosis and weight loss induced by a very low calorie ketogenic diet (VLCKD) in patients with obesity. Clin. Nutr. 2021;40:3959–3972. doi: 10.1016/j.clnu.2021.05.010. [DOI] [PubMed] [Google Scholar]
- 63.Crujeiras A.B., Diaz-Lagares A., Moreno-Navarrete J.M., Sandoval J., Hervas D., Gomez A., Ricart W., Casanueva F.F., Esteller M., Fernandez-Real J.M. Genome-wide DNA methylation pattern in visceral adipose tissue differentiates insulin-resistant from insulin-sensitive obese subjects. Transl. Res. 2016;178:13–24.e5. doi: 10.1016/j.trsl.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 64.Macchia P.E., Nettore I.C., Franchini F., Santana-Viera L., Ungaro P. Epigenetic regulation of adipogenesis by histone-modifying enzymes. Epigenomics. 2021;13:235–251. doi: 10.2217/epi-2020-0304. [DOI] [PubMed] [Google Scholar]
- 65.Crujeiras A.B., Diaz-Lagares A., Sandoval J., Milagro F.I., Navas-Carretero S., Carreira M.C., Gomez A., Hervas D., Monteiro M.P., Casanueva F.F., et al. DNA methylation map in circulating leukocytes mirrors subcutaneous adipose tissue methylation pattern: A genome-wide analysis from non-obese and obese patients. Sci. Rep. 2017;7:41903. doi: 10.1038/srep41903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wahl S., Drong A., Lehne B., Loh M., Scott W.R., Kunze S., Tsai P.C., Ried J.S., Zhang W., Yang Y., et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature. 2017;541:81–86. doi: 10.1038/nature20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.van Dijk S.J., Molloy P.L., Varinli H., Morrison J.L., Muhlhausler B.S., Members of Epi S. Epigenetics and human obesity. Int. J. Obes. 2015;39:85–97. doi: 10.1038/ijo.2014.34. [DOI] [PubMed] [Google Scholar]
- 68.Liu L., Chen Y., Chen J., Lu M., Guo R., Han J., Zhang Y., Pei X., Ping Z. The relationship between PRDM16 promoter methylation in abdominal subcutaneous and omental adipose tissue and obesity. Clin. Nutr. 2021;40:2278–2284. doi: 10.1016/j.clnu.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 69.Ding X., Zheng D., Fan C., Liu Z., Dong H., Lu Y., Qi K. Genome-wide screen of DNA methylation identifies novel markers in childhood obesity. Gene. 2015;566:74–83. doi: 10.1016/j.gene.2015.04.032. [DOI] [PubMed] [Google Scholar]
- 70.Goni L., Milagro F.I., Cuervo M., Martinez J.A. Single-nucleotide polymorphisms and DNA methylation markers associated with central obesity and regulation of body weight. Nutr. Rev. 2014;72:673–690. doi: 10.1111/nure.12143. [DOI] [PubMed] [Google Scholar]
- 71.Almen M.S., Nilsson E.K., Jacobsson J.A., Kalnina I., Klovins J., Fredriksson R., Schioth H.B. Genome-wide analysis reveals DNA methylation markers that vary with both age and obesity. Gene. 2014;548:61–67. doi: 10.1016/j.gene.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 72.Crujeiras A.B., Diaz-Lagares A., Stefansson O.A., Macias-Gonzalez M., Sandoval J., Cueva J., Lopez-Lopez R., Moran S., Jonasson J.G., Tryggvadottir L., et al. Obesity and menopause modify the epigenomic profile of breast cancer. Endocr. Relat. Cancer. 2017;24:351–363. doi: 10.1530/ERC-16-0565. [DOI] [PubMed] [Google Scholar]
- 73.Crujeiras A.B., Morcillo S., Diaz-Lagares A., Sandoval J., Castellano-Castillo D., Torres E., Hervas D., Moran S., Esteller M., Macias-Gonzalez M., et al. Identification of an episignature of human colorectal cancer associated with obesity by genome-wide DNA methylation analysis. Int. J. Obes. 2019;43:176–188. doi: 10.1038/s41366-018-0065-6. [DOI] [PubMed] [Google Scholar]
- 74.Gibson A.A., Sainsbury A. Strategies to Improve Adherence to Dietary Weight Loss Interventions in Research and Real-World Settings. Behav. Sci. 2017;7:44. doi: 10.3390/bs7030044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Laskowski R.A., Thornton J.M. Understanding the molecular machinery of genetics through 3D structures. Nat. Rev. Genet. 2008;9:141–151. doi: 10.1038/nrg2273. [DOI] [PubMed] [Google Scholar]
- 76.Strahl B.D., Allis C.D. The language of covalent histone modifications. Nature. 2000;403:41–45. doi: 10.1038/47412. [DOI] [PubMed] [Google Scholar]
- 77.Yu G., Su Q., Chen Y., Wu L., Wu S., Li H. Epigenetics in neurodegenerative disorders induced by pesticides. Genes Environ. 2021;43:55. doi: 10.1186/s41021-021-00224-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kimura H. Histone modifications for human epigenome analysis. J. Hum. Genet. 2013;58:439–445. doi: 10.1038/jhg.2013.66. [DOI] [PubMed] [Google Scholar]
- 79.Gao X., Lin S.H., Ren F., Li J.T., Chen J.J., Yao C.B., Yang H.B., Jiang S.X., Yan G.Q., Wang D., et al. Acetate functions as an epigenetic metabolite to promote lipid synthesis under hypoxia. Nat. Commun. 2016;7:11960. doi: 10.1038/ncomms11960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xie Z., Zhang D., Chung D., Tang Z., Huang H., Dai L., Qi S., Li J., Colak G., Chen Y., et al. Metabolic Regulation of Gene Expression by Histone Lysine beta-Hydroxybutyrylation. Mol. Cell. 2016;62:194–206. doi: 10.1016/j.molcel.2016.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chen L., Miao Z., Xu X. beta-hydroxybutyrate alleviates depressive behaviors in mice possibly by increasing the histone3-lysine9-beta-hydroxybutyrylation. Biochem. Biophys. Res. Commun. 2017;490:117–122. doi: 10.1016/j.bbrc.2017.05.184. [DOI] [PubMed] [Google Scholar]
- 82.Shimazu T., Hirschey M.D., Newman J., He W., Shirakawa K., Le Moan N., Grueter C.A., Lim H., Saunders L.R., Stevens R.D., et al. Suppression of oxidative stress by beta-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 2013;339:211–214. doi: 10.1126/science.1227166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Newman J.C., Covarrubias A.J., Zhao M., Yu X., Gut P., Ng C.P., Huang Y., Haldar S., Verdin E. Ketogenic Diet Reduces Midlife Mortality and Improves Memory in Aging Mice. Cell Metab. 2017;26:547–557.e8. doi: 10.1016/j.cmet.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chriett S., Dabek A., Wojtala M., Vidal H., Balcerczyk A., Pirola L. Prominent action of butyrate over beta-hydroxybutyrate as histone deacetylase inhibitor, transcriptional modulator and anti-inflammatory molecule. Sci. Rep. 2019;9:742. doi: 10.1038/s41598-018-36941-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cambronne X.A., Stewart M.L., Kim D., Jones-Brunette A.M., Morgan R.K., Farrens D.L., Cohen M.S., Goodman R.H. Biosensor reveals multiple sources for mitochondrial NAD(+) Science. 2016;352:1474–1477. doi: 10.1126/science.aad5168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nettore I.C., Franchini F., Palatucci G., Macchia P.E., Ungaro P. Epigenetic Mechanisms of Endocrine-Disrupting Chemicals in Obesity. Biomedicines. 2021;9:1716. doi: 10.3390/biomedicines9111716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhao M., Huang X., Cheng X., Lin X., Zhao T., Wu L., Yu X., Wu K., Fan M., Zhu L. Ketogenic diet improves the spatial memory impairment caused by exposure to hypobaric hypoxia through increased acetylation of histones in rats. PLoS ONE. 2017;12:e0174477. doi: 10.1371/journal.pone.0174477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Benjamin J.S., Pilarowski G.O., Carosso G.A., Zhang L., Huso D.L., Goff L.A., Vernon H.J., Hansen K.D., Bjornsson H.T. A ketogenic diet rescues hippocampal memory defects in a mouse model of Kabuki syndrome. Proc. Natl. Acad. Sci. USA. 2017;114:125–130. doi: 10.1073/pnas.1611431114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ranganathan K., Sivasankar V. MicroRNAs—Biology and clinical applications. J. Oral. Maxillofac. Pathol. 2014;18:229–234. doi: 10.4103/0973-029X.140762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bartel D.P. Metazoan MicroRNAs. Cell. 2018;173:20–51. doi: 10.1016/j.cell.2018.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Arner P., Kulyte A. MicroRNA regulatory networks in human adipose tissue and obesity. Nat. Rev. Endocrinol. 2015;11:276–288. doi: 10.1038/nrendo.2015.25. [DOI] [PubMed] [Google Scholar]
- 92.Lu J., Clark A.G. Impact of microRNA regulation on variation in human gene expression. Genome Res. 2012;22:1243–1254. doi: 10.1101/gr.132514.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ji C., Guo X. The clinical potential of circulating microRNAs in obesity. Nat. Rev. Endocrinol. 2019;15:731–743. doi: 10.1038/s41574-019-0260-0. [DOI] [PubMed] [Google Scholar]
- 94.Caradonna F., Consiglio O., Luparello C., Gentile C. Science and Healthy Meals in the World: Nutritional Epigenomics and Nutrigenetics of the Mediterranean Diet. Nutrients. 2020;12:1748. doi: 10.3390/nu12061748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Olivieri F., Capri M., Bonafe M., Morsiani C., Jung H.J., Spazzafumo L., Vina J., Suh Y. Circulating miRNAs and miRNA shuttles as biomarkers: Perspective trajectories of healthy and unhealthy aging. Mech. Ageing Dev. 2017;165:162–170. doi: 10.1016/j.mad.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yamada K., Takizawa S., Ohgaku Y., Asami T., Furuya K., Yamamoto K., Takahashi F., Hamajima C., Inaba C., Endo K., et al. MicroRNA 16-5p is upregulated in calorie-restricted mice and modulates inflammatory cytokines of macrophages. Gene. 2020;725:144191. doi: 10.1016/j.gene.2019.144191. [DOI] [PubMed] [Google Scholar]
- 97.Cannataro R., Perri M., Gallelli L., Caroleo M.C., De Sarro G., Cione E. Ketogenic Diet Acts on Body Remodeling and MicroRNAs Expression Profile. Microrna. 2019;8:116–126. doi: 10.2174/2211536608666181126093903. [DOI] [PubMed] [Google Scholar]
- 98.Cannataro R., Caroleo M.C., Fazio A., La Torre C., Plastina P., Gallelli L., Lauria G., Cione E. Ketogenic Diet and microRNAs Linked to Antioxidant Biochemical Homeostasis. Antioxidants. 2019;8:269. doi: 10.3390/antiox8080269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.O’Neill B., Raggi P. The ketogenic diet: Pros and cons. Atherosclerosis. 2020;292:119–126. doi: 10.1016/j.atherosclerosis.2019.11.021. [DOI] [PubMed] [Google Scholar]
- 100.Luong T.V., Abild C.B., Bangshaab M., Gormsen L.C., Sondergaard E. Ketogenic Diet and Cardiac Substrate Metabolism. Nutrients. 2022;14:1322. doi: 10.3390/nu14071322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Foster G.D., Wyatt H.R., Hill J.O., Makris A.P., Rosenbaum D.L., Brill C., Stein R.I., Mohammed B.S., Miller B., Rader D.J., et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: A randomized trial. Ann. Intern. Med. 2010;153:147–157. doi: 10.7326/0003-4819-153-3-201008030-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Buscemi S., Verga S., Tranchina M.R., Cottone S., Cerasola G. Effects of hypocaloric very-low-carbohydrate diet vs. Mediterranean diet on endothelial function in obese women. Eur. J. Clin. Investig. 2009;39:339–347. doi: 10.1111/j.1365-2362.2009.02091.x. [DOI] [PubMed] [Google Scholar]
- 103.Karwi Q.G., Biswas D., Pulinilkunnil T., Lopaschuk G.D. Myocardial Ketones Metabolism in Heart Failure. J. Card Fail. 2020;26:998–1005. doi: 10.1016/j.cardfail.2020.04.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.