Abstract
Objectives
This study considered whether experiencing the death of a child is associated with subsequent psychological distress in older populations, as well as variation in both exposure and vulnerability to the death of a child among Black, Hispanic, and White older parents.
Methods
We used multilevel models to link the death of a child with subsequent distress for 9,763 non-Hispanic White, 2,496 non-Hispanic Black, 1,014 foreign-born Hispanic, and 712 U.S.-born Hispanic parents from the Health and Retirement Study, 2006–2016.
Results
The death of a child is associated with increased psychological distress in mid to later life for Black, White, and Hispanic parents, with greater vulnerability for foreign-born Hispanic parents. Notably, Black and U.S.-born Hispanic parents are disadvantaged because of the additive effects of their greater exposure to bereavement and their higher distress levels regardless of bereavement status. These effects persist net of additional stressors associated with race/ethnicity.
Discussion
The death of a child is a traumatic life course event associated with lasting psychological distress for aging parents. Black and U.S.-born Hispanic parents are disadvantaged in that they are more likely than White parents to experience the death of a child, and foreign-born Hispanic parents may be disadvantaged by greater vulnerability to distress following child death.
Keywords: Bereavement, Cumulative advantage/disadvantage, Mental health, Minority aging, Race/ethnicity
A child’s death is a transformative event for parents, with lifelong implications for their health and well-being (Hendrickson, 2009; Song et al., 2019; Stroebe et al., 2007). Hundreds of studies have documented the adverse psychological consequences of experiencing the death of a child; however, these studies are based primarily on White populations. Thus, we know very little about racial/ethnic variation in life course experiences involving the death of a child, despite evidence that Black parents are more likely than White parents to experience a child’s death in the United States (Umberson et al., 2017). Although Hispanics exhibit lower mortality rates than non-Hispanic Whites (e.g., Hummer & Hayward, 2015; Rogers et al., 2019), mortality rates are higher for some Hispanic subgroups, particularly young adults and U.S.-born Hispanics (Borrell & Lancet, 2012; Rogers et al., 2019). These patterns suggest that some groups of Hispanic parents may be at greater risk of experiencing a child’s death compared to White parents; however, this risk has not been documented in prior research. These gaps in knowledge are striking in the American context of systemic racism and recent public attention to grief associated with premature mortality in racial and ethnic minority communities (Cooper & Williams, 2020; Jones-Eversley & Rice, 2020).
In this study, we analyze Health and Retirement Study (HRS) data to consider whether experiencing a child’s death is associated with parents’ subsequent psychological distress in mid to later life. We first document variation in life course exposure to the death of a child for Black, White, U.S.-born Hispanic, and foreign-born Hispanic parents. Second, in recognition of systemic racism that contributes to racial/ethnic disparities in mortality and bereavement, we focus on racial and ethnic disadvantage in exposure to child death as a traumatic life course event that may add to racial/ethnic disadvantage in psychological distress, net of other race-related stressors. Third, in light of greater stress and discrimination experienced by Black and Hispanic populations, we ask if the death of a child has stronger effects on psychological distress (i.e., more vulnerability) for Black and Hispanic parents than for White parents.
This study is critical in documenting racial/ethnic inequality in exposure to a child’s death, with attention to lifelong psychological consequences. Psychological distress is an important dimension of overall quality of life that predicts subsequent health and mortality risk (Domingue et al., 2020). The life course events that contribute to racial/ethnic disadvantage in psychological well-being need to be better understood so that future research can incorporate these findings as potential mechanisms linking bereavement events to inequality in other life outcomes for aging populations such as dementia (Umberson et al., 2020) and mortality risk (Donnelly et al., 2020).
Background
Black Americans face greater mortality risk than White Americans from birth through about age 85 (Lariscy, 2017; Rogers et al., 2019). Recent research suggests that this higher mortality risk translates into a greater risk of repeated bereavement events for Black Americans throughout the life course. By age 20, Black parents are about 2.5 times more likely than White parents to experience the death of a child, and this disparity increases as parents grow older, with Black parents in their 70s about four times more likely to have experienced a child’s death (Umberson et al., 2017). Prior research, however, does not document the risk of experiencing a child’s death among Hispanic populations, and the prevalence of child death among Hispanic parents is likely to vary by nativity status. While most foreign-born Hispanic populations tend to have favorable mortality rates relative to non-Hispanic Whites, this mortality advantage is not as apparent for U.S.-born Hispanics (Hummer & Hayward, 2015; Rogers et al., 2019). U.S.-born Hispanics experience a slight mortality disadvantage that begins in infancy (Hummer et al., 2007); however, this disadvantage is not as significant as the mortality disparities experienced by Black Americans. Taken together, these mortality patterns likely translate into a higher risk of child death for U.S.-born Hispanic parents, but not foreign-born Hispanic parents, compared to non-Hispanic White parents. Therefore, we test the following hypothesis:
H1: The risk of U.S.-born Hispanic parents experiencing a child’s death will be greater than that of White parents. The risk of child death will be similar for foreign-born Hispanic parents compared to White parents. We will confirm that Black parents are more likely than White parents to experience a child’s death (as documented in prior research).
Death of a Child and Psychological Distress
The death of a significant other is a highly stressful life event, and the death of a child is often considered the most devastating type of bereavement (Hendrickson, 2009; Stroebe et al., 2007). Although the experience of bereavement may differ depending on a child’s age, parents expect to predecease their children regardless of age (Rubin & Malkinson, 2001), and a child’s death at any age is associated with significant adverse effects on parents’ health, well-being, and mortality risk (Espinosa & Evans, 2013; Rostila et al., 2012; Song et al., 2019). Carstensen’s work on socioemotional selectivity—fewer negative emotions with advancing age—suggests the possibility that a child’s death might be less strongly associated with distress for parents in later life compared to midlife. However, few studies on bereavement following the death of a child consider the impact on parents in later life. Research on the persistence of bereavement effects on parents is somewhat inconsistent but, overall, suggests lasting effects (Floyd et al., 2013; Stroebe et al., 2007). Yet, these findings are based primarily on White populations in the United States and Europe and tell us little about long-term effects on the psychological well-being of racial and ethnic minority populations in the United States.
When considering the link between the death of a child and parents’ psychological distress, we must consider overall patterns of distress across racial/ethnic groups. A consistent epidemiologic finding is that Black and U.S.-born Hispanic Americans experience more psychological distress than White Americans (Miranda et al., 2008; Sternthal et al., 2011; Williams, 2018). This is likely because measures of psychological distress tap into depressive symptoms that fluctuate in relation to stress, and Black and Hispanic Americans face higher levels of stress than do White Americans throughout life (Williams, 2018). Moreover, depressive symptoms are more prevalent for U.S.-born than foreign-born Hispanic adults in the United States (Alegría et al., 2007; Sternthal et al., 2011), highlighting the importance of considering nativity status in Hispanic populations.
Therefore, in addition to being more likely to experience a child’s death, Black and Hispanic parents are more likely to experience disadvantage in psychological distress regardless of exposure to a child’s death. Both the greater risk of bereavement and disadvantage in psychological distress result from systemic racism in the United States. Compared to non-Hispanic White parents, Black and Hispanic parents experience lower socioeconomic status, higher overall levels of stress, more discrimination and prejudice, and more family member deaths over the life course (Brown et al., 2020; Forrester et al., 2019; Miranda et al., 2008; Sternthal et al., 2011; Umberson et al., 2017; Williams, 2018). In light of structural disadvantages associated with systemic racism, minoritized parents might then also be more psychologically vulnerable to the death of a child. Thus, when assessing racial/ethnic variation in bereavement experiences, both differential exposure and differential vulnerability should be tested.
The effects of a child’s death on parents’ distress should be considered net of constellations of stress that are associated with race and ethnicity as a result of systemic racism. In addition to child death, Black Americans are more likely than White Americans to experience the deaths of other family members prior to midlife such as a parent, sibling, or spouse (Umberson et al., 2017). Moreover, as a result of structural disadvantages, Black and Hispanic adults are more likely to experience a greater overall stress burden (Forrester et al., 2019; Williams, 2018) and lower levels of personal control (Shaw & Krause, 2001; Zahodne et al., 2017). Overall stress burden includes chronic stressors across various domains such as finances, work, housing, and caregiving (Thoits, 2010). Personal control, a sense that one can control future events and life circumstances, helps people to cope with and alleviate stress (Ross & Mirowsky, 2013). Because bereavement, chronic stressors, and lower levels of personal control have lasting consequences for psychological distress (Mirowsky & Ross, 2003; Pearlin et al., 2005; Stroebe et al., 2007; Thoits, 2010), we consider whether the death of a child undermines older adults’ mental health, net of these stress-related covariates. Therefore, in this study, we test the following hypotheses:
H2a. Parents who have experienced the death of a child will report higher levels of psychological distress in mid to later life than parents who have not experienced a child’s death, potentially adding to racial/ethnic disadvantage in psychological distress (exposure hypothesis).
H2b. The estimated effect of child death on parents’ distress in Hypothesis 2a (exposure) will persist, even after accounting for other race-related stressors.
H3a. The death of a child will have stronger effects on psychological distress for Black and Hispanic (foreign-born and U.S.-born) parents than for White parents (vulnerability hypothesis).
H3b. Differential vulnerability to child death by parents’ race/ethnicity (Hypothesis 3a) will persist, even after accounting for other race-related stressors.
Method
Data
We analyzed data from the HRS, a nationally representative sample of the United States population over age 50. The biannual HRS began in 1992 with a sample of adults aged 51–61 years and continues to add a new cohort of adults aged 51–56 years every 6 years. The HRS also surveys the spouses of focal respondents, some of whom are younger than 51 or older than 56 when they entered the study. Cohorts in the present study include the original HRS cohort (born 1931–1941; entered in 1992), the War Babies cohort (born 1942–1947; entered in 1998), the Early Baby Boomers (born 1948–1953; entered in 2004), and the Mid Baby Boomers (born 1954–1959; entered in 2010). We excluded the Late Baby Boomer cohort (entered in 2016) because respondents were not asked about the death of a child.
Since 2006, the HRS has administered a leave-behind questionnaire that provides additional information about life circumstances, including personal control, chronic stress, and the death of a child. Respondents completed this questionnaire every other HRS wave. Psychological distress and sociodemographic measures are from the core biannual HRS interview. Thus, the present study relied on the 2006–2016 data and excluded respondents who exited the study by 2006. We excluded respondents with missing data on psychological distress or child death; missing data on the covariates were imputed. We restricted the analytic sample to parents (respondents who reported ever having a child) for a final sample of 9,763 non-Hispanic White parents, 2,496 non-Hispanic Black parents, 712 U.S.-born Hispanic parents, and 1,014 foreign-born Hispanic parents (n = 13,985).
Measures
Psychological distress
Psychological distress was measured with the eight-item Center for Epidemiological Studies Depression scale. Respondents reported whether they felt depressed, everything was an effort, their sleep was restless, they could not get going, lonely, enjoyed life, sad, or happy much of the time during the past week. Positive items were reverse coded, and all items were summed so that higher values indicate higher levels of distress (range 0–8; α = 0.82; Steffick, 2000). Psychological distress is measured in every wave of the HRS, and we assessed distress as a time-varying measure.
Death of a child
Respondents were asked whether they had ever experienced a child’s death (1 = yes). We assessed exposure to child death based on an affirmative response to this question in the leave-behind questionnaire. Because of the complex design of the HRS, parents answered this question in different waves from 2006 to 2014 (this question was not included in the 2016 questionnaire). Parents were also asked in what year their child died or the most recent year of a child’s death if parents experienced multiple deaths. In sensitivity analyses, we included a measure of duration since the child’s death (in years) to account for recency of bereavement by subtracting the year the child died from the year of survey completion.
Stress-related covariates
We considered additional bereavement events, personal control, and chronic stress as life course features that are associated with race/ethnicity and contribute to psychological distress. We accounted for other family member deaths prior to midlife to address the higher rates of family bereavement for Black parents compared to White parents. Respondents in the HRS reported whether their parents were alive and, if not, they reported the year of death. Respondents also reported the end date of every marriage, including marriages that ended in widowhood. We used this information to create a summed count of whether respondents experienced the death of a mother, father, or spouse (range 0–3) by the parent’s baseline wave (average age at baseline: 54 years).
Respondents completed five questions to measure personal control. They indicated agreement with the following statements: I often feel helpless in dealing with the problems of life, other people determine most of what I can and cannot do, what happens in my life is often beyond my control, I have little control over the things that happen to me, and there is no way I can solve the problems I have. Response options ranged from (1) strongly disagree to (6) strongly agree. We reverse-coded responses and averaged scores across items, excluding respondents with more than three missing items (Lachman & Weaver, 1998; Pearlin & Schooler, 1978). Higher values indicate higher levels of personal control (range 1–6; α = 0.86).
To measure chronic stress, respondents reported whether eight events were ongoing problems that lasted 12 months or longer (Troxel et al., 2003): health problems (self), physical or emotional problems in a spouse or child, problems with alcohol or drug use in a family member, difficulties at work, financial strain, housing problems, problems in a close relationship, and helping at least one sick or limited family member or friend on a regular basis. Response options ranged from (1) No, did not happen to (4) Yes, very upsetting. Responses were summed such that higher values indicate more chronic stress (range 1–32; α = 0.72). Measures of additional family member deaths, personal control, and chronic stress are time-invariant and measured at the baseline wave.
Race/Ethnicity
Respondents were asked whether they consider themselves to be Hispanic or Latino (Yes, No) and what race they consider themselves (White, Black or African American, American Indian, Alaska Native, Asian, Native Hawaiian, Pacific Islander, or something else). Respondents also report nativity, which allows us to identify respondents born outside the United States. We used these three questions to indicate non-Hispanic Black, U.S.-born Hispanic, foreign-born Hispanic, and non-Hispanic White parents.
Other Covariates
All analyses accounted for sociodemographic covariates potentially associated with both child death and psychological distress. These covariates include age (in years) and age-squared, gender (1 = female), whether respondents were born in the South or elsewhere (1 = South), the number of children a parent has given birth to or fathered (range 1–9), and educational attainment (less than high school (reference), high school graduate, some college, college degree or more).
Analytic Strategy
Because of the multilevel structure of the data, with repeated observations (Level 1) nested within respondents (Level 2), we used multilevel regression models to examine whether a child’s death was associated with psychological distress among parents. To ensure appropriate time order such that exposure to child death occurred before the assessment of psychological distress, we excluded any observations (i.e., waves) that occurred prior to the death of a child. For example, if a parent experienced the death of a child in 2009, we excluded their waves of data from 2006 and 2008, but we retained observations from 2010 onward. Less than 0.5% of observations were excluded with this approach. Respondents contributed an average of 4.8 waves of data to the analyses.
We first tested whether child death was related to psychological distress, net of sociodemographic covariates. Then, we tested whether the association between child death and psychological distress was robust to exposure to other racially distributed stressors including family deaths that occurred before baseline, chronic stress, and personal control. We then examined variation in the association between child death and distress by parents’ race/ethnicity by adding an interaction of child death with race/ethnicity. We also tested whether these findings persisted net of other racially distributed stressors. We illustrated key findings graphically by presenting predicted scores for psychological distress by child death and race/ethnicity.
Analyses accounted for the complex survey design of the HRS and we applied respondent-level weights to the descriptive results in Table 1. Regression analyses did not include weights because the models included covariates related to sample selection; this approach produces unbiased coefficients without weights (Heeringa et al., 2017).
Table 1.
Weighted Descriptive Data for the Analytic Sample, by Race/Ethnicity (HRS, 2006–2016)
| Overall (% or Mean) | Non-Hispanic Black | U.S.-born Hispanic | Foreign-born Hispanic | Non-Hispanic White | |
|---|---|---|---|---|---|
| Psychological distress | 1.33 (1.96) | 1.69c,d (1.71) | 1.85d (1.92) | 2.02a,d (2.03) | 1.22a,b,c (1.85) |
| Experienced child death | 14.02 | 21.41c,d | 20.31d | 15.31a | 12.65a,b |
| Duration since child death | 21.49 (16.49) | 20.81 (15.47) | 20.48 (15.36) | 21.66 (14.82) | 21.71 (17.13) |
| Age at first observation | 60.88 (8.12) | 60.26d (7.76) | 59.77 (7.48) | 60.19 (8.00) | 61.06a (8.12) |
| Female | 52.06 | 58.45b,d | 53.23a | 55.15 | 50.97a |
| Born in the South | 31.14 | 66.21b,c,d | 49.82a,c,d | 0.00a,b,d | 27.53a,b,c |
| Less than high school diploma | 14.15 | 24.33b,c,d | 30.92a,c,d | 58.71a,b,d | 9.18a,b,c |
| High school diploma | 34.55 | 32.01c,d | 35.64c | 18.69a,b,d | 35.80a,c |
| Some college | 26.26 | 28.56b,c | 21.97a,c,d | 14.15a,b,d | 26.94b,c |
| College degree or more | 25.04 | 15.10c,d | 11.47d | 8.45a,d | 28.07a,b,c |
| Number of children | 2.75 | 3.22c,d | 3.35d | 3.61a,d | 2.60a,b,c |
| (1.55) | (1.92) | (1.73) | (2.00) | (1.32) | |
| Number of family deaths before baseline | 1.19 (0.78) | 1.25b,c,d (0.78) | 1.13a,d (0.79) | 1.12a (0.80) | 1.19a,b (0.78) |
| Personal control at baseline | 4.85 (1.16) | 4.80b,c,d (1.18) | 4.64a,c,d (1.18) | 4.45a,b,d (1.37) | 4.90a,b,c (1.12) |
| Chronic stress at baseline | 12.43 (3.88) | 12.95c,d (4.20) | 12.90d (4.14) | 12.38a (4.24) | 12.34a,b (3.72) |
| Non-Hispanic Black | 10.47 | ||||
| U.S.-born Hispanic | 4.21 | ||||
| Foreign-born Hispanic | 4.99 | ||||
| Non-Hispanic White | 80.33 | ||||
| Unweighted N | 13,985 | 2,496 | 712 | 1,014 | 9,763 |
Notes: HRS = Health and Retirement Study. Standard deviations in parentheses.
aStatistically different from non-Hispanic Black at p < .05.
bStatistically different from U.S.-born Hispanic at p < .05.
cStatistically different from foreign-born Hispanic at p < .05.
dStatistically different from non-Hispanic White at p < .05.
Results
Descriptive Results
Table 1 presents descriptive results for the analytic sample. Two-tailed t-tests compare descriptive results by race/ethnicity of parents. Non-Hispanic White parents reported the lowest levels of psychological distress, followed by non-Hispanic Black parents, U.S.-born Hispanic parents, and foreign-born Hispanic parents. Non-Hispanic White parents reported the highest levels of personal control, whereas foreign-born Hispanic parents reported the lowest levels of personal control. Non-Hispanic Black and U.S.-born Hispanic parents reported higher levels of chronic stress compared to Non-Hispanic White and foreign-born Hispanic parents.
Table 1 shows that Non-Hispanic White parents (13%) were less likely than non-Hispanic Black (21%) and U.S.-born Hispanic (20%) parents to experience a child’s death; the likelihood of child death was similar for non-Hispanic White parents and foreign-born Hispanic parents (15%). Non-Hispanic Black parents were also more likely than other parents to experience multiple family member deaths prior to baseline. These results support Hypothesis 1.
Exposure to The Death of a Child and Subsequent Psychological Distress
Model 1 of Table 2 shows that net of sociodemographic covariates, having experienced the death of a child was associated with more psychological distress for parents (b = 0.25, p < .001) in mid to later life. The results in Model 1 also show racial/ethnic disparities in distress. Non-Hispanic Black parents (b = 0.24, p < .001), U.S.-born Hispanic parents (b = 0.45, p < .001), and foreign-born Hispanic parents (b = 0.39, p < .001) reported more distress than non-Hispanic White parents, net of sociodemographic covariates. Notably, race/ethnicity and child death had independent and additive associations with psychological distress. Results in Table 2 then support Hypothesis 2a, indicating robust associations of child death with psychological distress in mid to later life that may add to racial/ethnic disadvantage in distress.
Table 2.
Multilevel Models Regressing Psychological Distress on the Death of a Child (HRS, 2006–2016; n = 13,985)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Experienced child death | 0.25*** (0.04) | 0.15*** (0.03) | 0.25*** (0.05) | 0.16*** (0.04) |
| Age (centered at 65) | −0.01*** (0.00) | −0.01*** (0.00) | −0.01*** (0.00) | −0.01*** (0.00) |
| Age-squared | 0.00*** (0.00) | 0.00*** (0.00) | 0.00*** (0.00) | 0.00*** (0.00) |
| Non-Hispanic Black (ref: Non-Hispanic White) | 0.24*** (0.04) | 0.19*** (0.03) | 0.25*** (0.05) | 0.21*** (0.04) |
| U.S.-born Hispanic (ref: Non-Hispanic White) | 0.45*** (0.10) | 0.35*** (0.08) | 0.48*** (0.12) | 0.39*** (0.10) |
| Foreign-born Hispanic (ref: Non-Hispanic White) | 0.39*** (0.08) | 0.31*** (0.07) | 0.33*** (0.09) | 0.26** (0.08) |
| Female | 0.30*** (0.03) | 0.23*** (0.02) | 0.30*** (0.03) | 0.23*** (0.02) |
| Born in the South | 0.14*** (0.03) | 0.11*** (0.02) | 0.14*** (0.02) | 0.11*** (0.02) |
| High school diploma (ref: Less than high school) | −0.55*** (0.05) | −0.38*** (0.05) | −0.55*** (0.05) | −0.39*** (0.05) |
| Some college (ref: Less than high school) | −0.77*** (0.05) | −0.58*** (0.05) | −0.77*** (0.05) | −0.58*** (0.05) |
| College degree or more (ref: Less than high school) | −1.09*** (0.06) | −0.75*** (0.05) | −1.09*** (0.06) | −0.76*** (0.05) |
| Number of children | −0.00 (0.01) | −0.00 (0.01) | −0.00 (0.01) | −0.00 (0.01) |
| Total family deaths before baseline | 0.03* (0.01) | 0.03* (0.01) | ||
| Personal control at baseline | −0.40*** (0.01) | −0.40*** (0.01) | ||
| Chronic stress at baseline | 0.12*** (0.00) | 0.12*** (0.00) | ||
| Experienced child death × Non-Hispanic Black | −0.06 (0.10) | −0.07 (0.09) | ||
| Experienced child death × U.S.-born Hispanic | −0.16 (0.14) | −0.19 (0.14) | ||
| Experienced child death × Foreign-born Hispanic | 0.40* (0.18) | 0.33+ (0.19) | ||
| Intercept variance | 1.97*** (0.04) | 1.41*** (0.03) | 1.97*** (0.04) | 1.41*** (0.03) |
| Residual variance | 1.71*** (0.03) | 1.71*** (0.03) | 1.71*** (0.03) | 1.71*** (0.03) |
| Constant | 1.61*** (0.06) | 1.92*** (0.11) | 1.61*** (0.06) | 1.92*** (0.10) |
Notes: HRS = Health and Retirement Study. Standard errors in parentheses; ***p < .001, **p < .01, *p < .05, +p < .10.
Model 2 tested whether the effect of child death persisted, even after accounting for other stressors that disproportionately burden Black and Hispanic adults. Model 2 shows that additional family member deaths prior to midlife (b = 0.03, p < .05) and more chronic stress at baseline (b = 0.12, p < .001) were associated with more psychological distress among parents in mid to later life, and higher levels of personal control at baseline were associated with less distress in mid to later life (b = −0.40, p < .001). Although the coefficient for exposure to the death of a child was reduced by 40%, child death remained a significant predictor of distress among parents (Model 2; b = 0.15, p < .001) even after accounting for other stress-related covariates, supporting Hypothesis 2b.
Differential Vulnerability to Child Death by Race/Ethnicity
To test the differential vulnerability hypothesis, we examined whether the association between child death and subsequent psychological distress varied by parents’ race/ethnicity. In Model 3 (Table 2), the nonsignificant interaction terms for non-Hispanic Black and U.S.-born Hispanic parents indicate that, net of sociodemographic covariates, experiencing the death of a child was associated with psychological distress in similar ways for non-Hispanic White, non-Hispanic Black, and U.S.-born Hispanic parents. The interaction of child death with foreign-born Hispanic parents is significant and positive (b = 0.40, p < .05), suggesting that exposure to the death of a child was associated with more psychological distress for foreign-born Hispanic parents compared to non-Hispanic White parents. Overall, results in Model 3 provide partial support for Hypothesis 3a; only foreign-born Hispanic parents exhibited differential vulnerability to child death.
We also tested Hypothesis 3b that differential vulnerability to child death, particularly among foreign-born Hispanic parents, would persist despite the higher levels of stress and lower levels of personal control experienced by Black and Hispanic parents. Results in Model 4 show that the addition of other stress-related covariates reduced the interaction term for foreign-born Hispanic parents and child death to marginal statistical significance, although the magnitude of the coefficient remained large (b = 0.33, p < .10). When including stress-related covariates in the model, the interaction term for foreign-born Hispanic parents was only reduced by about 18% (b = 0.40 in Model 3, b = 0.33 in Model 4). Moreover, a Z test for equality of coefficients revealed that the interaction terms for foreign-born Hispanic parents were statistically indistinguishable between Model 3 and Model 4. These results generally support Hypothesis 3b.
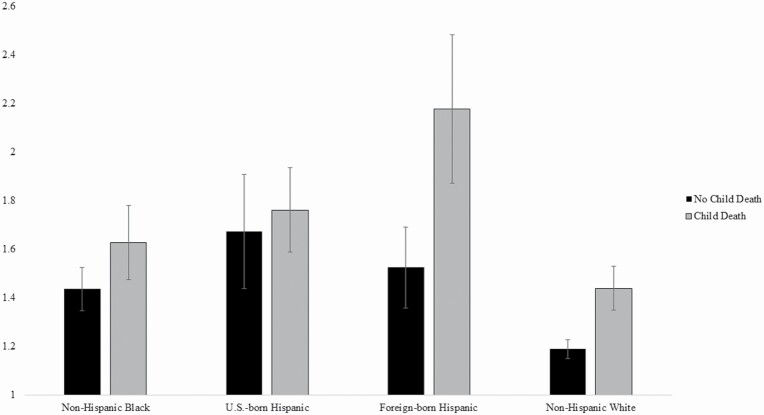
We illustrate two key findings in Figure 1, which shows predicted scores for psychological distress by bereavement status and parents’ race/ethnicity. First, Figure 1 shows that parents who experienced a child’s death reported more distress than parents who did not experience the death of a child. Second, non-White parents reported more distress than non-Hispanic White parents regardless of bereavement status. Thus, Figure 1 shows the additive effects of child death and race/ethnicity, with Black and Hispanic bereaved parents experiencing the highest levels of distress. Figure 1 also shows the unique vulnerability of bereaved foreign-born Hispanic parents.
Figure 1.
Predicted levels of psychological distress by child death and parents’ race/ethnicity (Health and Retirement Study, 2006–2016).
Sensitivity analysis
We explored the possibility that the impact of child death on psychological distress might vary depending on the parent’s current age. When examining heterogeneity by the age of the parent, we accounted for duration since the death of a child using the internal moderator approach (Mirowsky, 2013). Supplement A shows that the interaction of child death with parental age was significant and negative (b = −0.01, p < .05), suggesting that the adverse consequences of child death for psychological distress were slightly smaller for older compared to younger respondents. However, the size of the coefficient indicates a substantively modest difference. Analyses accounted for duration (in years) since the death of a child to account for the recency of bereavement. Supplementary Material shows that the interaction term of child death with parent age remains significant after accounting for other stressors.
Discussion
Despite growing attention to the disproportionate risk of child death experienced by Black Americans in the United States (Umberson et al., 2017), most studies on bereavement following the death of a child are based on White populations in the United States and Europe. Moreover, prior research does not document the extent of child death among Hispanic parents in the United States. In this study, we argue that inequality in exposure and vulnerability to the death of a child may add to disadvantage in psychological distress for Black and Hispanic parents in mid to later life. Thus, we assess the extent to which child death differently impacts the mental health of Black, Hispanic, and White midlife and older adults and the extent to which these patterns persist net of other race-related stressors. Overall, we find that bereaved parents, compared to nonbereaved parents, experience lasting effects on their distress levels in mid to later life. Although child death is associated with higher levels of distress for all parents, there is group-specific racial/ethnic disadvantage in terms of increased exposure and vulnerability to the death of a child. These effects persist net of other significant race-related life course stressors. Below, we discuss the findings on racial/ethnic variation in exposure and vulnerability to bereavement.
Although prior research has established that Black parents are more likely than White parents to be exposed to the death of a child (Umberson et al., 2017), our study goes further to show that U.S.-born Hispanic parents are almost twice as likely as non-Hispanic White parents to be exposed to the death of a child, with rates similar to those of non-Hispanic Black parents. These findings fit with prior studies suggesting a mortality disadvantage for some U.S.-born Hispanic populations (Hummer & Hayward, 2015; Rogers et al., 2019). Our findings also suggest possible differences in bereavement by nativity, with foreign-born parents more similar to non-Hispanic White parents in risk of child death. This may occur because, as prior research indicates, immigrants are a selectively healthier population and foreign-born Hispanics may have a shorter duration of exposure to the high levels of stress and discrimination experienced by U.S.-born Hispanics in the United States (e.g., Hummer & Hayward, 2015; Sternthal et al., 2011). Experiencing a child’s death is significantly more likely to occur for U.S.-born Hispanic and Black parents, and future research on bereavement should include Hispanic populations, with attention to nativity.
Our overarching finding is the death of a child has lasting effects on the psychological distress of Black, White, and Hispanic parents. However, racial/ethnic variation in exposure to the death of a child potentially adds to racial/ethnic disadvantage in distress in that, compared to White parents, Black and U.S.-born Hispanic parents experience more psychological distress regardless of bereavement status and are significantly more likely to experience the death of a child during their lifetime. Overall, our findings suggest independent and additive effects of exposure to child death and race/ethnicity in predicting parents’ mid to later-life psychological distress. Differential exposure to stress is central to the production of health disparities (Ward et al., 2019), and we suggest that exposure to the death of a child is a uniquely stressful life event with lasting consequences that add to racial/ethnic disparities in the psychological distress of mid to later life adults.
We also hypothesized that Black and Hispanic parents, compared to White parents, would be more vulnerable to distress following the death of a child because this traumatic life event occurs in the context of lifelong exposure to wide-ranging stressors associated with systemic racism (Brown et al., 2020; Forrester et al., 2019; Miranda et al., 2008; Umberson et al., 2017; Williams, 2018). We found mixed evidence for this hypothesis. The death of a child had similar effects on psychological distress for Black, White, and U.S.-born Hispanic parents, which aligns with previous research on similar responses to stressful experiences for Black and White adults (e.g., Sternthal et al., 2011; Umberson et al., 2020). However, our results suggest that foreign-born Hispanic parents may be uniquely vulnerable to the consequences of child death for psychological distress. This might occur because foreign-born Hispanic women and men are less likely to have access to formal and informal support systems due to language and immigration status barriers, or because they have fewer family members in the United States to rely on for support (e.g., Hummer & Hayward, 2015; Philbin et al., 2018). The unique vulnerability of foreign-born Hispanic parents emerges despite some advantages—lower levels of chronic stress and less exposure to additional family member deaths—and suggests that future research should consider the array of risks and resources apparent in this population. We caution that older foreign-born parents in the HRS are a small, heterogenous population, and future research should seek to explain why bereaved foreign-born parents may be particularly vulnerable and explore differences in vulnerability to child death by country of origin and length of time in the United States. Taken together, our findings suggest that differential exposure to child death undermines the mental health of Black and U.S.-born Hispanic parents, and differential vulnerability to child death may be a unique risk factor for the mental health of foreign-born Hispanic parents.
The death of a child, as well as higher levels of psychological distress, among Black and Hispanic adults result from life course experiences shaped by systemic racism. This raises the possibility that exposure to other life course stressors might account for some of the impact of child death on distress (exposure effect), and greater vulnerability following bereavement (vulnerability effect). While Black and Hispanic parents reported more chronic stress, lower levels of personal control, and exposure to more family member deaths prior to midlife, the effect of child death on distress, including vulnerability to child death, was reduced but persisted net of these race-related stressors. That the effects of bereavement persist beyond the effects of other major stressors underscore the profound and lasting impact of a child’s death.
Given the prevalence and consequences of child death in the United States (e.g., Hendrickson, 2009; Umberson et al., 2017), greater attention should be directed toward screening and intervention in older populations. New approaches should also consider the potentially unique effects on midlife parents. Prior research suggests that negative emotions may be stronger in midlife than later life (Carstensen et al., 2003), and midlife parents may have more work/family responsibilities than later life parents (Pearlin et al., 2005) that add to their distress. Although the effect size is modest, we found somewhat stronger effects of child death on distress for midlife compared to later-life parents. Yet this age effect may also be explained if older adults are a more robust group that survived to later life. It is also important for future studies to identify possible life course pathways through which bereavement affects psychological distress because it is by disrupting these pathways that future policy and practice efforts may help to reduce the long-term adverse effects of bereavement on distress across diverse populations.
Several study limitations should be noted. First, the HRS sample primarily includes adults over age 50, excluding adults who died before age 50 or were unable to participate in the study due to their health. Because child death is associated with worse health and greater mortality risk (Donnelly et al., 2020; Hendrickson, 2009; Song et al., 2019), selective survival in the analytic sample may lead to an underestimation of the consequences of child death for psychological outcomes. Second, the HRS does not include information about the child’s age at the time of their death, the child’s gender, or the cause of death. These factors shape bereavement experiences (Hendrickson, 2009); thus, we may be missing variation in psychological distress based on these factors. Third, our findings concerning foreign-born Hispanics should be viewed as suggestive and preliminary in that this is a small and heterogeneous group in the HRS. Finally, although we can establish time order between a child’s death and parents’ psychological distress, we relied on retrospective reports of child death and could not observe bereavement and distress prospectively.
The literature on bereavement is voluminous, but scholars have only recently begun to highlight population inequality in bereavement (Cooper & Williams, 2020; Jones-Eversley & Rice, 2020; Kidman et al., 2021; Umberson et al., 2017). The Black Lives Matter movement and the coronavirus pandemic have drawn greater attention to racial/ethnic disparities in the death of family members (Cooper & Williams, 2020; Garcia et al., 2020; Verdery et al., 2020). Our findings show that U.S.-born Hispanic and Black parents are more likely to experience a child’s death than their non-Hispanic White counterparts, with long-term psychological consequences. These findings highlight the need for future research to document population patterns of bereavement and its consequences across diverse groups. Practitioners should screen for bereavement events, and policymakers should address the significant health consequences of bereavement that remain largely invisible and untreated in diverse older populations.
Supplementary Material
Contributor Information
Debra Umberson, Population Research Center, The University of Texas at Austin, Austin, Texas, USA.
Rachel Donnelly, Department of Sociology, Vanderbilt University, Nashville, Tennessee, USA.
Funding
This work was supported by the National Institute on Aging (R01AG054624 and P30 AG066614) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2C HD042849).
Author Contributions
D. Umberson planned the study and wrote the article. R. Donnelly performed statistical analyses and assisted with writing and revising the article.
Conflict of Interest
None declared.
References
- Alegría, M., Mulvaney-Day, N., Torres, M., Polo, A., Cao, Z., & Canino, G. (2007). Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health, 97(1), 68–75. doi: 10.2105/AJPH.2006.087205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell, L. N., & Lancet, E. A. (2012). Race/ethnicity and all-cause mortality in US adults: Revisiting the Hispanic paradox. American Journal of Public Health, 102(5), 836–843. doi: 10.2105/AJPH.2011.300345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, L. L., Mitchell, U. A., & Ailshire, J. A. (2020). Disentangling the stress process: Race/ethnic differences in the exposure and appraisal of chronic stressors among older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(3), 650–660. doi: 10.1093/geronb/gby072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen, L. L., Fung, H. H., & Charles, S. T. (2003). Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation and Emotion, 27(2), 103–123. doi: 10.1023/A:1024569803230 [DOI] [Google Scholar]
- Cooper, L. A., & Williams, D. R. (2020). Excess deaths from COVID-19, community bereavement, and restorative justice for communities of color. JAMA, 324(15), 1491–1492. doi: 10.1001/jama.2020.19567 [DOI] [PubMed] [Google Scholar]
- Domingue, B. W., Duncan, L., Harrati, A., & Belsky, D. W. (2020). Short-term mental health sequelae of bereavement predict long-term physical health decline in older adults: US Health and Retirement Study analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(6), 1231–1240. doi: 10.1093/geronb/gbaa044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly, R., Umberson, D., Hummer, R. A., & Garcia, M. A. (2020). Race, death of a child, and mortality risk among aging parents in the United States. Social Science & Medicine (1982), 249, 112853. doi: 10.1016/j.socscimed.2020.112853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinosa, J., & Evans, W. N. (2013). Maternal bereavement: The heightened mortality of mothers after the death of a child. Economics and Human Biology, 11(3), 371–381. doi: 10.1016/j.ehb.2012.06.002 [DOI] [PubMed] [Google Scholar]
- Floyd, F. J., Mailick Seltzer, M., Greenberg, J. S., & Song, J. (2013). Parental bereavement during mid-to-later life: Pre- to postbereavement functioning and intrapersonal resources for coping. Psychology and Aging, 28(2), 402–413. doi: 10.1037/a0029986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester, S. N., Gallo, J. J., Whitfield, K. E., & Thorpe, R. J. (2019). A framework of minority stress: From physiological manifestations to cognitive outcomes. The Gerontologist, 59(6), 1017–1023. doi: 10.1093/geront/gny104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, M. A., Homan, P. A., García, C., & Brown, T. H. (2020). The color of COVID-19: Structural racism and the disproportionate impact of the pandemic on older Black and Latinx adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(3), e75–e80. doi: 10.1093/geronb/gbaa114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa, S. G., West, B. T., Berglund, P. A., West, B. T., & Berglund, P. A. (2017). Applied survey data analysis (2nd ed.). Chapman and Hall/CRC. doi: 10.1201/9781315153278 [DOI] [Google Scholar]
- Hendrickson, K. C. (2009). Morbidity, mortality, and parental grief: A review of the literature on the relationship between the death of a child and the subsequent health of parents. Palliative & Supportive Care, 7(1), 109–119. doi: 10.1017/S1478951509000133 [DOI] [PubMed] [Google Scholar]
- Hummer, R. A., & Hayward, M. D. (2015). Hispanic older adult health & longevity in the United States: Current patterns & concerns for the future. Daedalus, 144(2), 20–30. doi: 10.1162/DAED_a_00327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer, R. A., Powers, D. A., Pullum, S. G., Gossman, G. L., & Frisbie, W. P. (2007). Paradox found (again): Infant mortality among the Mexican-origin population in the United States. Demography, 44(3), 441–457. doi: 10.1353/dem.2007.0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones-Eversley, S. D., & Rice, J. (2020). A call for epidemiology and thanatology to address the dying, death, and grief pipeline among Blacks in the United States. Death Studies, 51(3), 251–272. doi: 10.1080/07481187.2020.1721618 [DOI] [PubMed] [Google Scholar]
- Kidman, R., Margolis, R., Smith-Greenaway, E., & Verdery, A. M. (2021). Estimates and projections of COVID-19 and parental death in the US. JAMA Pediatrics, 175(7), 745–746. doi: 10.1001/jamapediatrics.2021.0161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman, M. E., & Weaver, S. L. (1998). The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology, 74(3), 763–773. doi: 10.1037//0022-3514.74.3.763 [DOI] [PubMed] [Google Scholar]
- Lariscy, J. T. (2017). Black–White disparities in adult mortality: Implications of differential record linkage for understanding the mortality crossover. Population Research and Policy Review, 36(1), 137–156. doi: 10.1007/s11113-016-9415-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda, J., McGuire, T. G., Williams, D. R., & Wang, P. (2008). Mental health in the context of health disparities. The American Journal of Psychiatry, 165(9), 1102–1108. doi: 10.1176/appi.ajp.2008.08030333 [DOI] [PubMed] [Google Scholar]
- Mirowsky, J. (2013). Analyzing associations between mental health and social circumstances. In Aneshensel C. S., Phelan J. C., & Bierman A. (Eds.), Handbook of the sociology of mental health (pp. 143–165). Springer. doi: 10.1007/978-94-007-4276-5_8 [DOI] [Google Scholar]
- Mirowsky, J., & Ross, C. E. (2003). Social causes of psychological distress. Aldine de Gruyter. [Google Scholar]
- Pearlin, L. I., & Schooler, C. (1978). The structure of coping. Journal of Health and Social Behavior, 19(1), 2–21. doi: 10.2307/2136319 [DOI] [PubMed] [Google Scholar]
- Pearlin, L. I., Schieman, S., Fazio, E. M., & Meersman, S. C. (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46(2), 205–219. doi: 10.1177/002214650504600206 [DOI] [PubMed] [Google Scholar]
- Philbin, M. M., Flake, M., Hatzenbuehler, M. L., & Hirsch, J. S. (2018). State-level immigration and immigrant-focused policies as drivers of Latino health disparities in the United States. Social Science & Medicine (1982), 199, 29–38. doi: 10.1016/j.socscimed.2017.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers, R. G., Hummer, R. A., Krueger, P. M., & Vinneau, J. M. (2019). Adult mortality. In D. L. Poston & M. Micklin (Eds.), Handbook of population (pp. 355–381). Springer. [Google Scholar]
- Rostila, M., Saarela, J., & Kawachi, I. (2012). Mortality in parents following the death of a child: A nationwide follow-up study from Sweden. Journal of Epidemiology and Community Health, 66(10), 927–933. doi: 10.1136/jech-2011-200339 [DOI] [PubMed] [Google Scholar]
- Ross, C. E., & Mirowsky, J. (2013). The sense of personal control: Social structural causes and emotional consequences. In Aneshensel C. S., Phelan J. C., & Bierman A. (Eds.), Handbook of the sociology of mental health (pp. 379–402). Springer. [Google Scholar]
- Rubin, S. S., & Malkinson, R. (2001). Parental response to child loss across the life cycle: Clinical and research perspectives. In M.S. Stroebe, R.O. Hansson, W. Stroebe, & H. Schut (Eds.), Handbook of bereavement research: Consequences, coping, and care (pp. 219–240). American Psychological Association. [Google Scholar]
- Shaw, B. A., & Krause, N. (2001). Exploring race variations in aging and personal control. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56(2), S119–S124. doi: 10.1093/geronb/56.2.s119 [DOI] [PubMed] [Google Scholar]
- Song, J., Mailick, M. R., Greenberg, J. S., & Floyd, F. J. (2019). Mortality in parents after the death of a child. Social Science & Medicine (1982), 239, 112522. doi: 10.1016/j.socscimed.2019.112522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffick, D. E. (2000). Documentation of affective functioning measures in the Health and Retirement Study. Institute for Social Research, University of Michigan. [Google Scholar]
- Sternthal, M. J., Slopen, N., & Williams, D. R. (2011). Racial disparities in health: How much does stress really matter? Du Bois Review: Social Science Research on Race, 8(1), 95–113. doi: 10.1017/S1742058X11000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe, M., Schut, H., & Stroebe, W. (2007). Health outcomes of bereavement. Lancet (London, England), 370(9603), 1960–1973. doi: 10.1016/S0140-6736(07)61816-9 [DOI] [PubMed] [Google Scholar]
- Thoits, P. A. (2010). Stress and health: Major findings and policy implications. Journal of Health and Social Behavior, 51 Suppl, S41–S53. doi: 10.1177/0022146510383499 [DOI] [PubMed] [Google Scholar]
- Troxel, W. M., Matthews, K. A., Bromberger, J. T., & Sutton-Tyrrell, K. (2003). Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology, 22(3), 300–309. doi: 10.1037/0278-6133.22.3.300 [DOI] [PubMed] [Google Scholar]
- Umberson, D., Donnelly, R., Xu, M., Farina, M., & Garcia, M. A. (2020). Death of a child prior to midlife, dementia risk, and racial disparities. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(9), 1983–1995. doi: 10.1093/geronb/gbz154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Olson, J. S., Crosnoe, R., Liu, H., Pudrovska, T., & Donnelly, R. (2017). Death of family members as an overlooked source of racial disadvantage in the United States. Proceedings of the National Academy of Sciences of the United States of America, 114(5), 915–920. doi: 10.1073/pnas.1605599114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdery, A. M., Smith-Greenaway, E., Margolis, R., & Daw, J. (2020). Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proceedings of the National Academy of Sciences of the United States of America, 117(30), 17695–17701. doi: 10.1073/pnas.2007476117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, J. B., Gartner, D. R., Keyes, K. M., Fliss, M. D., McClure, E. S., & Robinson, W. R. (2019). How do we assess a racial disparity in health? Distribution, interaction, and interpretation in epidemiological studies. Annals of Epidemiology, 29, 1–7. doi: 10.1016/j.annepidem.2018.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, D. R. (2018). Stress and the mental health of populations of color: Advancing our understanding of race-related stressors. Journal of Health and Social Behavior, 59(4), 466–485. doi: 10.1177/0022146518814251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne, L. B., Manly, J. J., Smith, J., Seeman, T., & Lachman, M. E. (2017). Socioeconomic, health, and psychosocial mediators of racial disparities in cognition in early, middle, and late adulthood. Psychology and Aging, 32(2), 118–130. doi: 10.1037/pag0000154 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.