Abstract
Lower third molar extraction is the most common surgical treatment among routine dental and oral surgical procedures. while the surgical procedures for lower third molar extraction are well established, the difficulty of tooth extraction and the frequency of postoperative complications differ depending on the patient’s background. To establish a management protocol for the lower third molars, the prevalence of and risk factors for postoperative complications after lower third molar extraction were investigated in a large number of Japanese patients in a multicenter prospective study. During 6 consecutive months in 2020, 1826 lower third molar extractions were performed at the 20 participating institutions. The medical records of the patients were reviewed, and relevant data were extracted. The prevalence of and risk factors for postoperative complications were analyzed. The prevalence of postoperative complications after lower third molar extraction was 10.0%. Multivariate analysis indicated that age (≤32 vs >32, odds ratio [OR]: 1.428, 95% confidence interval [95% CI]: 1.040–1.962, P < .05), the radiographic anatomical relationship between the tooth roots and mandibular canal (overlapping of the roots and canal vs no close anatomical relationship between the roots and the superior border of the canal, OR: 2.078, 95% CI: 1.333–3.238, P < .01; overlapping of the roots and canal vs roots impinging on the superior border of the canal, OR: 1.599, 95% CI: 1.050–2.435, P < .05), and impaction depth according to the Pell and Gregory classification (position C vs position A, OR: 3.7622, 95% CI: 2.079–6.310, P < .001; position C vs position B, OR: 2.574, 95% CI: 1.574–4.210, P < .001) are significant independent risk factors for postoperative complications after lower third molar extraction. These results suggested that higher age and a deeply impacted tooth might be significant independent risk factors for postoperative complications after lower third molar extraction.
Keywords: extraction, lower third molar, Pell and Gregory classification, postoperative complication, risk factor
1. Introduction
Lower third molar extraction is the most common surgical treatment among routine dental and oral surgical procedures. The age and comorbidities of patients that undergo lower third molar extraction vary markedly, and while the surgical procedures for lower third molar extraction are well established, the difficulty of tooth extraction and the frequency of postoperative complications differ depending on the patient’s background. The surgical extraction of an impacted lower third molar that does not exhibit symptoms or pathological findings as a preventative measure remains controversial among clinicians.[1,2] According to a White Paper produced by the American Association of Oral and Maxillofacial Surgeons (AAOMS), third molars associated with disease or a higher risk of disease progression are recommended for extraction.[3] In addition, the AAOMS suggested that surgical intervention or the removal of third molars prior to the development of pathology should be considered in patients who have insufficient physiological space for eruption, and maintenance should be performed once optimal postsurgical healing has been achieved and the risk of complications is low.[4] Postoperative complications make patients uncomfortable, and patients fear complications that result in additional dental visits and treatment.[5] Therefore, before the extraction of lower third molars patients must be provided with full information, including regarding the advantages and disadvantages of the surgical procedure and any potential intraoperative or postoperative complications.
The common postoperative complications of lower third molar extraction include swelling; pain; temporomandibular joint symptoms, such as trismus; hemorrhaging; a dry socket; infection; and sensory alterations relating to the inferior alveolar or lingual nerve.[6,7] The postoperative complications rate following lower third molar extraction has been reported to range from 4.6% to 30.9%.[8–11] In a recent nationwide population-based cohort study conducted in Taiwan, the incidence rates of dry sockets, surgical site infections, and temporomandibular joint symptoms were reported to be 3.6%, 0.17%, and 0.41%, respectively.[7] The prevalence of inferior alveolar nerve injuries was reported to range from 1.2% to 13.0%,[12–14] and the prevalence of lingual nerve injuries was reported to range from 0.02% to 4%.[15,16] Postoperative complications after lower third molar extraction have been found to be associated with various factors, including age, medical history, the patient’s health conditions, the depth of the impacted tooth, the surgeon’s experience, smoking habits, the use of contraceptive medication, the patient’s oral hygiene level, and the surgical procedure.[10,17] However, there have been few large prospective studies of the postoperative complications that can occur after lower third molar extraction.[13,16] Therefore, to establish a management protocol for lower third molars, the prevalence of and risk factors for postoperative complications after lower third molar extraction were investigated in Japanese patients in a multicenter prospective study involving a large number of cases.
2. Patients and Methods
The study protocol was approved by the Committee on Medical Research of Shinshu University (#4489). We obtained informed consent from all study participants.
This was a nonrandomized, multicenter prospective observational study, which included pooled data for individual patients from 20 institutions. During 6 consecutive months in 2020, 1826 lower third molar extractions were performed at the 20 institutions. The medical records of these patients were reviewed, and relevant data were extracted.
Data regarding patient characteristics, including age; sex; and the presence/absence of comorbidities, such as diabetes mellitus, hypertension, immunosuppressive factors, diarrhea, and cerebral infarctions, were extracted from the patients’ medical records. The preoperative use of antibiotics or nonsteroidal antiinflammatory drugs and the number of cases of postoperative complications were also investigated. As lower third molar-related factors, the depth of the impacted lower third molar (impaction depth) and the anatomical relationship between the mandibular ramus and the lower third molar were investigated based on the Pell and Gregory classification.[18] The radiographic findings of the lower third molars, such as disappearance of the periodontal ligament space and the anatomical relationship between the tooth roots and the mandibular canal, were also investigated with panoramic radiography. Bone removal, tooth sectioning, primary wound closure, the surgeon’s experience, and the operation time were investigated as surgical factors. During the initial tooth extraction, the use of a hemostat (oxidized cellulose), suturing, or a surgical splint were investigated as procedure-related factors. The use of a hemostat (oxidized cellulose, Surgicel; Ethicon, Somerville, NJ), sutures (5-0 silk), surgical splints, and antibiotic or antiinflammatory drugs was based on the surgeon’s discretion.
The optimal age cutoff value for predicting postoperative complications after lower third molar extraction was determined based on receiver operating characteristic (ROC) curve analysis. Univariate analyses of the risk factors for postoperative complications after lower third molar extraction were performed using Fisher exact test, Wilcoxon test, or Pearson chi-square test, and multivariate analysis was performed with multivariate logistic regression analysis. All of the variables that were found to be associated with postoperative complications in the univariate analyses were included in the multivariate logistic regression analysis. Multivariate odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for the factors that exhibited significance. Decision-tree analysis was also performed as an alternative way of investigating the factors related to postoperative complications after lower third molar extraction. All statistical analyses were conducted using JMP ver.13 (SAS Institute Inc., NC). P values of < 0.05 were considered to be significant.
3. Results
One thousand, eight hundred twenty-six patients underwent lower third molar extraction during the study period and were included in the study population. The patients’ characteristics are shown in Table 1. Among the 1826 patients, 756 (41.4%) were male, and 1070 (58.6%) were female. The median age at extraction was 31.4 ± 12.4 years (range: 13–88 years). The surgeons had a mean of 9.0 ± 8.6 years’ experience. The mean operation time was 26.5 ± 17.5 minutes. The prevalence of postoperative complications after lower third molar extraction was 10.0% (183/1826 patients). Among the postoperative complications seen after lower third molar extraction, a dry socket was the most common (59 patients; prevalence rate: 3.2%), followed by inferior alveolar nerve injuries (31 patients; 1.7%) and postoperative pain (30 patients; 1.6%) (Table 2). The prevalence of postoperative hemorrhaging was 0.3% (6/1826 patients). All postoperative complications were resolved within 6 months.
Table 1.
The characteristics of the patients (n = 1826).
| Variables | Number (%) | Variables | Number (%) |
|---|---|---|---|
| Gender | Disappearance of periodontal ligament space | ||
| Male | 756 (41.4) | No | 1492 (81.7) |
| Female | 1070 (58.6) | Yes | 334 (18.3) |
| Age (average ± SD) | 31.4 ± 12.4 | Radiographical association between root and inferior alveolar canal | |
| Diabetes mellitus | No association between root structure and the superior border of the canal | 820 (44.9) | |
| No | 1803 (98.7) | Root structure impinging the superior border of canal | 760 (41.6) |
| Yes | 23 (1.3) | Overlapping root structure and canal | 246 (13.5) |
| Immunosuppressor factor | Pell and Gregory classification | ||
| No | 1799 (98.5) | Class I | 475 (26.0) |
| Yes | 27 (1.5) | Class II | 1084 (59.4) |
| Hypertension | Class III | 267 (14.6) | |
| No | 1761 (96.4) | Position A | 772 (42.3) |
| Yes | 65 (3.6) | Position B | 902 (49.4) |
| Cerebral infarction | Position C | 152 (8.3) | |
| No | 1813 (99.3) | Bone removal | |
| Yes | 13 (0.7) | No | 172 (9.4) |
| Drinking habit | Yes | 1654 (90.6) | |
| No | 1484 (81.3) | Tooth sectioning | |
| Yes | 342 (18.7) | No | 173 (9.5) |
| Diarrhea | Yes | 1653 (90.5) | |
| No | 1813 (99.3) | Primary wound closure | |
| Yes | 13 (0.7) | No | 275 (15.1) |
| Comorbidities | Yes | 1551 (84.9) | |
| No | 1473 (80.7) | Postoperative complication | |
| Yes | 353 (19.3) | No | 1643 (90.0) |
| Preoperative use of antibiotic | Yes | 183 (10.0) | |
| No | 1349 (73.9) | Operation time (min ± SD) | 26.5 ± 17.5 |
| Yes | 477 (26.1) | Surgeon’s experience (y ± SD) | 9.0 ± 8.6 |
| Preoperative use of painkiller | |||
| No | 1790 (98.0) | ||
| Yes | 36 (2.0) |
Table 2.
The contents and prevalence of the postoperative complications after the lower third molar extraction (n = 183).
| Postoperative complication | Number (%) |
|---|---|
| Inferior alveolar nerve paralysis | 31 (1.7) |
| Lingual nerve paralysis | 4 (0.2) |
| Wound infection | 26 (1.4) |
| Prolonged wound healing | 15 (0.8) |
| Dry socket | 59 (3.2) |
| Postoperative pain | 30 (1.6) |
| Postoperative hemorrhage | 6 (0.3) |
| Tooth residue | 6 (0.3) |
| Allergy due to postoperative use of antibiotic | 6 (0.3) |
The univariate analyses indicated that the occurrence of postoperative complications after lower third molar extraction was associated with age (OR: 1.539, P < .01), the preoperative use of antibiotics (OR: 1.646, P < .01), the radiographic anatomical relationship between the tooth roots and mandibular canal (P < .001), the Pell and Gregory classification (class and position, P < .001), bone removal (OR: 2.426, P < .05), and tooth sectioning (OR: 2.144, P < .05) (Table 3). Although there was no significant association, the perioperative use of painkillers tended to be associated with postoperative complications (P = .083). No associations were observed between the occurrence of postoperative complications after lower third molar extraction and sex, comorbidities, the radiographic disappearance of the periodontal ligament space, or primary wound closure. There were no significant associations between the occurrence of postoperative complications after lower third molar extraction and the surgeon’s experience or the operation time (Wilcoxon test, data not shown).
Table 3.
The univariate analysis of the postoperative complications after the lower third molar extraction.
| No. of Postoperative complications (%) | No. of Postoperative complications (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | No | Yes | OR | P value | Variables | No | Yes | OR | P value |
| Gender | Disappearance of periodontal ligament space | ||||||||
| Male | 686 (37.6) | 70 (3.8) | 1.157 | NS | No | 1345 (73.7) | 147 (8.1) | 1.105 | NS |
| Female | 957 (52.4) | 113 (6.2) | .385 | Yes | 298 (16.3) | 36 (2.0) | .615 | ||
| Age, y | Radiographical association between root and inferior alveolar canal | ||||||||
| <32 | 1034 (56.6) | 96 (5.3) | 1.539 | <.01 | No association between root structure and the superior border of the canal | 759 (41.6) | 61 (3.) | – | <.001* |
| ≧32 | 609 (33.4) | 87 (4.6) | Root structure impinging the superior border of canal | 680 (37.2) | 80 (4.4) | ||||
| Diabetes mellitus | Overlapping root structure and canal | 204 (11.2) | 42 (2.3) | ||||||
| No | 1622 (88.8) | 181 (9.9) | 0.853 | NS | Pell and Gregory classification | ||||
| Yes | 21 (1.2) | 2 (0.1) | 1.000 | Class I | 446 (24.4) | 29 (1.6) | – | <.001* | |
| Immunosuppressor factor | Class II | 968 (53.0) | 116 (6.4) | ||||||
| No | 1619 (88.7) | 180 (9.9) | 1.124 | NS | Class III | 229 (12.5) | 38 (2.1) | ||
| Yes | 24 (1.3) | 3 (0.2) | .747 | Position A | 722 (42.3) | 50 (2.7) | – | .001* | |
| Hypertension | Position B | 806 (44.1) | 96 (5.3) | ||||||
| No | 1585 (86.8) | 176 (9.6) | 1.087 | NS | Position C | 115 (6.3) | 37 (2.0) | ||
| Yes | 58 (3.2) | 7 (0.4) | .833 | Bone removal | |||||
| Cerebral infarction | No | 164 (9.0) | 8 (0.4) | 2.426 | .05 | ||||
| No | 1630 (89.3) | 183 (10.0) | 0 | NS | Yes | 1479 (81.0) | 175 (9.6) | ||
| Yes | 13 (0.7) | 0 (0) | .632 | Tooth sectioning | |||||
| Drinking habit | No | 164 (9.0) | 9 (0.5) | 2.144 | <.05 | ||||
| No | 1335 (73.1) | 149 (8.2) | 0.989 | NS | Yes | 1479 (81.0) | 174 (9.5) | ||
| Yes | 308 (16.9) | 34 (1.9) | 1.000 | Primary wound closure | |||||
| Diarrhea | No | 250 (13.7) | 25 (1.4) | 1.134 | NS | ||||
| No | 1631 (89.3) | 182 (10.0) | 0.747 | NS | Yes | 1393 (76.3) | 158 (8.7) | .633 | |
| Yes | 12 (0.7) | 1 (0.1) | 1.000 | ||||||
| Comorbidities | |||||||||
| No | 1333 (73.0) | 140 (7.7) | 1.321 | NS | |||||
| Yes | 310 (17.0) | 43 (2.4) | |||||||
| Preoperative use of antibiotic | |||||||||
| No | 1231 (67.4) | 118 (6.5) | 1.646 | <.01 | |||||
| Yes | 412 (22.6) | 65 (3.6) | |||||||
| Preoperative use of painkiller | |||||||||
| No | 1614 (88.4) | 179 (9.8) | 2.214 | NS | |||||
| Yes | 29 (1.6) | 7 (0.4) | .083 | ||||||
Multivariate analysis indicated that age (≤32 vs ˃32, OR: 1.428, 95% CI: 1.040–1.962, P < .05), the radiographic anatomical relationship between the tooth roots and mandibular canal (overlapping of the roots and canal vs no close anatomical relationship between the roots and the superior border of the canal, OR: 2.078, 95% CI: 1.333–3.238, P < .01; overlapping of the roots and canal vs roots impinging on the superior border of the canal, OR: 1.599, 95% CI: 1.050–2.435, P < .05), and impaction depth according to the Pell and Gregory classification[18] (position C vs position A, OR: 3.7622, 95% CI: 2.079–6.310, P < .001; position C vs position B, OR: 2.574, 95% CI: 1.574–4.210, P < .001) are significant independent risk factors for postoperative complications after lower third molar extraction (Table 4). The frequency of postoperative complications after lower third molar extraction differed significantly between Pell and Gregory classification class II and class I (OR: 1.565, 95% CI: 1.006–2.435, P < .05). These results suggested that higher age and a deeply impacted tooth are significant independent risk factors for postoperative complications after lower third molar extraction.
Table 4.
The multivariate analysis of the postoperative complications after the lower third molar extraction.
| Variables | OR | 95% CI | P value |
|---|---|---|---|
| Age (≧32/>32) | 1.428 | 1.040–1.962 | <.05 |
| Use of preoperative antibiotic (yes/no) | 1.214 | 0.857–1.720 | NS (.276) |
| Use of preoperative painkiller (yes/no) | 1.661 | 0.668–4.132 | NS (.275) |
| Radiographical association between root and inferior alveolar canal (root structure impinging the superior border of canal/No association between root structure and the superior border of the canal)) | 1.300 | 0.908–1.860 | NS (=.152) |
| (Overlapping root structure and canal/no association between root structure and the superior border of the canal) | 2.078 | 1.333–3.238 | <.01 |
| (Overlapping root structure and canal/root structure impinging the superior border of canal) | 1.599 | 1.050–2.435 | <.05 |
| Pell and Gregory classification (class II/class I) | 1.565 | 1.006–2.435 | <.05 |
| (Class III/class I) | 1.148 | 0.637–2.066 | NS (.646) |
| (Class III/class II) | 0.733 | 0.461–1.167 | NS (.191) |
| (Position B/position A) | 1.407 | 0.971–2.041 | NS (.072) |
| (Position C/position A) | 3.622 | 2.079–6.310 | <.0001 |
| (Position C/position B) | 2.574 | 1.574–4.210 | <.001 |
| Bone removal (yes/no) | 1.558 | 0.657–3.696 | NS (.314) |
| Tooth sectioning (yes/no) | 1.171 | 0.516–2.660 | NS (.706) |
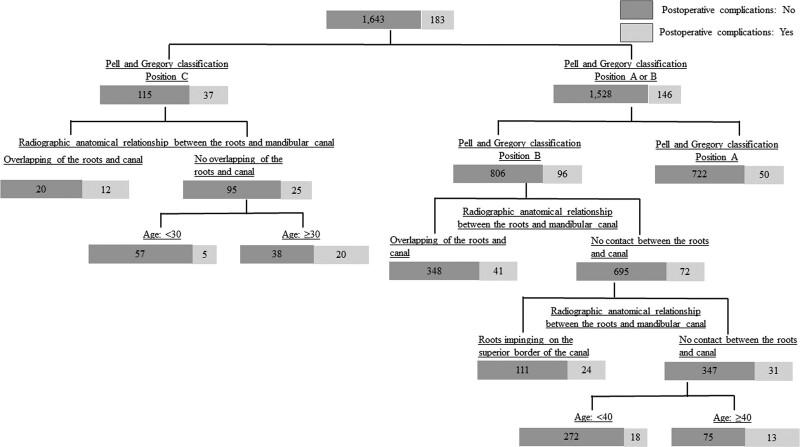
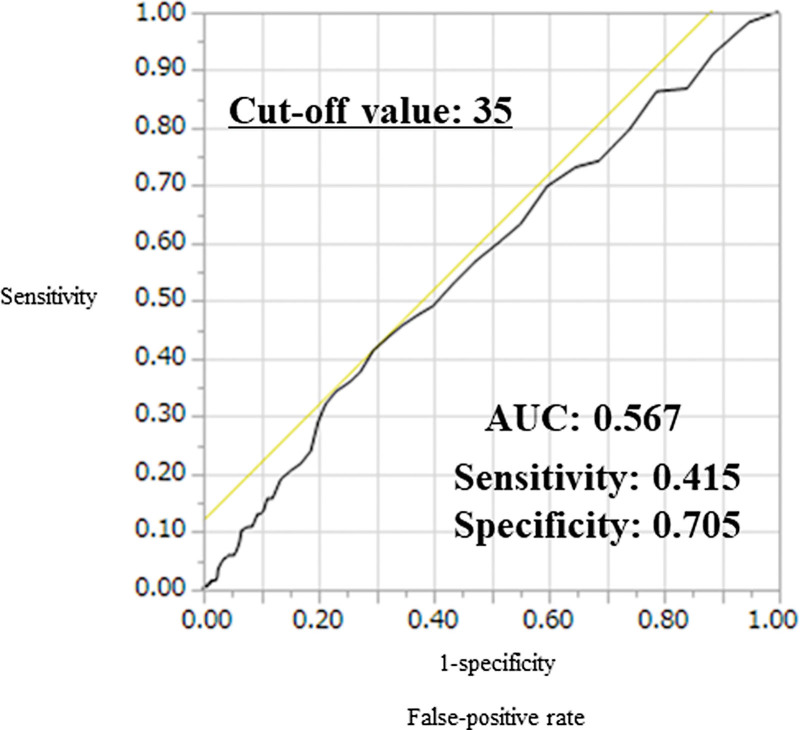
An additional investigation of the factors related to postoperative complications after lower third molar extraction was performed with decision-tree analysis (Fig. 1). The findings of the latter analysis were consistent with those of the multivariate analysis. The decision-tree analysis revealed significant associations between postoperative complications after lower third molar extraction and higher age, a deeply impacted tooth, or a close radiographic anatomical relationship between the tooth roots and mandibular canal. The optimal age cutoff value for predicting postoperative complications after lower third molar extraction was 35 years (area under the ROC curve [AUC]: 0.567, sensitivity: 0.415, specificity: 0.705) according to the ROC analysis (Fig. 2).
Figure 1.
Decision-tree analysis of the factors affecting the risk of postoperative complications after lower third molar extraction (n = 1826). The decision-tree analysis revealed significant associations between postoperative complications after lower third molar extraction and age, impaction depth, and a close radiographic anatomical relationship between the tooth roots and mandibular canal.
Figure 2.
The optimal age cutoff value for predicting postoperative complications after lower third molar extraction. The optimal age cutoff value for predicting postoperative complications after lower third molar extraction was 35 years old (AUC: 0.567) according to ROC analysis. AUC = area under the ROC curve, ROC = receiver operating characteristic.
4. Discussion
The postoperative complications that occur after lower third molar extraction can have serious implications for both patients and clinicians. When obtaining informed consent from patients for lower third molar extraction, the prevalence of postoperative complications and the risk factors for such complications represent important information. Therefore, in this multicenter prospective observational study we aimed to investigate the prevalence of postoperative complications after lower third molar extraction and the risk factors for such complications in Japan. As a result, it was suggested that age and impaction depth are significant independent risk factors for postoperative complications after lower third molar extraction.
The postoperative complications rate after lower third molar extraction was 10.0% in this study. Among the observed postoperative complications, the most common were a dry socket (3.2%), inferior alveolar nerve injuries (1.7%), wound infections (1.4%), and lingual nerve injuries (0.2%). These prevalence rates were consistent with the findings of previous studies.[7–16,19,20] The onset of postoperative complications is influenced by various factors. The risk factors for a dry socket were reported to include the difficulty of extraction, age, female sex, smoking, oral hygiene, the complexity of odontectomy, and a history of gingivitis or pericoronitis.[7,8,21–25] Inferior alveolar nerve injuries were reported to be significantly associated with deviation of the mandibular canal; a greater impaction depth; intraoperative hemorrhaging within the socket/nerve exposure; a longer operation time; surgical difficulty; radiographic signs, such as loss of the white lines of the roots and diversion of the mandibular canal; and the presence of a multirooted third molar.[12–14,19] Lingual nerve injuries were reported to be associated with female sex, being aged ≥ 26 years, lingual flap retraction, an impaction depth of ≥ 10 mm, an operation time of ≥30 min, and distoangular impaction.[16,26] Although it was reported that there were no significant risk factors for surgical site infections after lower third molar extraction, delayed-onset infections were reported to be associated with younger age and long surgical procedures.[20] As described above, age, impaction depth, and radiographic risk factors have been reported to influence postoperative complications after lower third molar extraction. These findings were consistent with the results of our multicenter prospective observational study. Since the administrations of nonsteroidal antiinflammatory drugs and antibiotics has been reported to increase the risk of the postoperative bleeding, especially in patients with anticoagulants,[27–31] the effects of these drugs on the postoperative complications in this study. However, these factors were not significant independent risk factor for the postoperative complications after the lower third molar extractions.
Although it was reported that surgical morbidity did not increase with age,[32] age has been reported to affect the mandible and the lower third molars, for example, a higher age is associated with increased bone density, a reduction in bone elasticity, hypercementosis, complete root formation, and a reduced capacity for healing.[11,33] A rise in age of 1 year increased the OR of developing nerve damage by 6.9%.[32] In addition, more deeply impacted lower third molars are located closer to the mandibular canal, which increases the risk of an inferior alveolar nerve injury. Deeper impaction of a lower third molar reduces surgical accessibility and visibility, which can also contribute to postoperative morbidity.[33] The difficulty of extraction was reported to increase 3 times with every 1-mm increase in the impaction depth.[34] Hasegawa et al[19] reported that although there was no significant association between the Pell and Gregory classification and inferior alveolar nerve hypoesthesia, the surgical removal of a deeply impacted tooth may require more extensive manipulation and bone removal close to the inferior alveolar nerve, which may increase the risk of postoperative inflammation and both direct and indirect nerve injuries. Since there is a close anatomical relationship between the roots of the lower third molars and the mandibular canal, the distance between the roots and the mandibular canal was also identified as a major predictor of postoperative complications.[19] However, it is impossible to evaluate the anatomical relationship between the roots of lower third molars and the mandibular canal using the Pell and Gregory classification. In a study investigating the anatomical differences among lower third molars according to panoramic radiographs and cone-beam computed tomography, it was found that if a panoramic radiograph indicated that the roots of a lower third molar overlapped with more than one-third of the mandibular canal (position B or C), there was a close anatomical relationship between the lower third molar and the mandibular canal. In addition, a good correlation was observed between the proximity of the lower third molar roots to the mandibular canal and complications after lower third molar removal.[35] Thus, our findings indicate that age, impaction depth, and the radiographic anatomical relationship between the lower third molar roots and the mandibular canal might be very useful predictors of postoperative complications after lower third molar extraction.
In this study, ROC analysis indicated that the optimal age cutoff value for predicting postoperative complications after lower third molar extraction was 35 years old. In previous studies, the optimal age cutoff values for predicting such complications were reported to be 25 to 26 years.[14,16,36] However, the AUC, sensitivity, and specificity values associated with these cutoff values were relatively low. It has been reported that age (25 years old) and various widely used panoramic radiography indicators can be employed as criteria for defining risk groups,[14] which suggests that other factors, such as impaction depth and radiographic findings, should be considered as potential predictors of postoperative complications.
Since age, impaction depth, and the radiographic anatomical relationship between the lower third molar roots and the mandibular canal might be very useful predictors of postoperative complications after lower third molar extraction in this study, the extraction of impacted lower third molar, which have a deep impacted depth and its apex of the tooth is close to the mandibular canal, requires caution with aging. However, the establishment of a management protocol for the lower third molars has been controversial. In the pilot study investigating the unpredictable lower third molar migration, the unpredictable migrations were reported the relation to any type of lesion.[37] Considering the unpredictable behavior of the lower third molar, impacted lower third molar recommends to evaluate periodically and radiographically, even if surgical extraction is not indicated.[37] The establishment of the management protocol would be needed for the lower third molar.
Although, due to the SARS-CoV-2 pandemic, medical and dental treatments were restricted in Japan during the study period, and the accumulation of cases did not progress as expected, the main strengths of the present study were that it was the first to investigate the prevalence of and risk factors for postoperative complications after lower third molar extraction based on a relatively large number of cases and that it was a multicenter prospective study. In order to prevent the infection of the SARA-CoV-2, although the extraoral vacuum aspirator had used for the decreasing the dust during the lower third molar extractions, this infection prevention method had no effects on the results of this study. The main limitation of this study was that the results may have been affected by the surgeon’s experience. However, no significant association was detected between the surgeon’s experience or the operation time and postoperative complications after lower third molar extraction. Regarding the reason for this, we speculate that it may have been due to “real-world” case selection based on the patient’s age and the expected difficulty of tooth removal; that is, that more experienced clinicians or specialists were selected as surgeons for cases involving deeply impacted teeth or older or systemically compromised patients.[7]
In conclusion, the present study provides information about the prevalence of and risk factors for postoperative complications after lower third molar extraction in Japan. The prevalence of such complications was 10.0%. Multivariate analysis revealed that increased age, deeper impaction of the third molar, and radiographic overlapping between the roots and mandibular canal may be significant independent risk factors for postoperative complications after lower third molar extraction. Although various other factors may have affected our results, it was found that the optimal cutoff age for predicting postoperative complications after lower third molar extraction is 35 years.
Acknowledgments
We wish to thank Medical English Service (https://www.med-english.com/) for their help with the English proofreading. We also wish to thank Drs Morishita K, Sakurai S, Kita R, Yamada K, Imai R, Tachibana A, Imamachi K, and Karasawa I for their help with the data collection.
Author contributions
Conception and design of the study: Y.S. and K.H.; Analysis and interpretation of data: Y.S.; Collection and assembly of data: Y.S., H.T., Y.N., H.Y., N.T., S.N., M.H., Y.H., U.N., Y.Y., O.H., T.A., N.Y., I.E., A.D., I.R., S.S., K.K., K.S., H.H., K.Y., M.Y., N.H., A.M., K.T., S.Y., and U.M.; Drafting of the article: Y.S.; Critical revision of the article for important intellectual content: Y.S.; Final approval of the article: K.H.
Abbreviations:
- AAOMS =
- American Association of Oral and Maxillofacial Surgeons
- AUC =
- area under the ROC curve
- CI =
- confidence interval
- OR =
- odds ratio
- ROC =
- receiver operating characteristic
How to cite this article: Yamada S-I, Hasegawa T, Yoshimura N, Hakoyama Y, Nitta T, Hirahara N, Miyamoto H, Yoshimura H, Ueda N, Yamamura Y, Okuyama H, Takizawa A, Nakanishi Y, Iwata E, Akita D, Itoh R, Kubo K, Kondo S, Hata H, Koyama Y, Miyamoto Y, Nakahara H, Akashi M, Kirita T, Shibuya Y, Umeda M, Kurita H, Prevalence of and risk factors for postoperative complications after lower third molar extraction: A multicenter prospective observational study in Japan. Medicine 2022;101:32(e29989).
The authors have no funding and conflicts of interest to disclose.
The study protocol was approved by the ethics committee of Shinshu University School of Medicine (No. 4489).
We obtained full informed consent from all study participants.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
NS = not significant, OR = odd ratio.
Pearson chi-square test; Fischer exact test.
CI = confidence interval, NS = not significant, OR = odd ratio.
Contributor Information
Takumi Hasegawa, Email: hasetaku@med.kobe-u.ac.jp.
Nobuhiko Yoshimura, Email: yoshimurahitoshi9@gmail.com.
Yusuke Hakoyama, Email: haccotin@hotmail.com.
Tetsuya Nitta, Email: nitta-t50@kch.kagoshima.jp.
Narihiro Hirahara, Email: hirahara-n46@kch.kagoshima.jp.
Hironori Miyamoto, Email: miyamoto@tokushima-u.ac.jp.
Hitoshi Yoshimura, Email: yoshimurahitoshi9@gmail.com.
Nobuhiro Ueda, Email: n-ueda@naramed-u.ac.jp.
Yoshiko Yamamura, Email: yamamura.yoshiko@tokushima-u.ac.jp.
Hideki Okuyama, Email: hikky_os03@ybb.ne.jp.
Atsushi Takizawa, Email: takiatsu1127@gmail.com.
Yoshitaka Nakanishi, Email: nakanisi@shinshu-u.ac.jp.
Eiji Iwata, Email: eiwata@med.kobe-u.ac.jp.
Daisuke Akita, Email: d.akita0404@gmail.com.
Ryuichi Itoh, Email: ryuichi.itoh@gmail.com.
Kiriko Kubo, Email: kiriko@shinshu-u.ac.jp.
Seiji Kondo, Email: kondo@fukuoka-u.ac.jp.
Hironobu Hata, Email: hatabooh@gmail.com.
Yoshito Koyama, Email: kyoshito@shinshu-u.ac.jp.
Youji Miyamoto, Email: miyamoto@tokushima-u.ac.jp.
Hirokazu Nakahara, Email: nakahara.hirokazu@med.osaka-cu.ac.jp.
Masaya Akashi, Email: akashim@med.kobe-u.ac.jp.
Tadaaki Kirita, Email: tkirita@naramed-u.ac.jp.
Yasuyuki Shibuya, Email: shibuya@med.nagoya-cu.ac.jp.
Masahiro Umeda, Email: mumeda@nagasaki-u.ac.jp.
Hiroshi Kurita, Email: hkurita@shinshu-u.ac.jp.
References
- [1].Mettes TD, Ghaeminia H, Nienhuijs ME, et al. Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth. Cochrane Database Syst Rev. 2012;6:CD003879. [DOI] [PubMed] [Google Scholar]
- [2].Ghaeminia H, Nienhuijs ME, Toedtling V, et al. Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth. Cochrane Database Syst Rev. 2020;5:CD003879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].American Association of Oral and Maxillofacial Surgeons. White paper on the management of third molar teeth. 2017. Available at: https://www.aaoms.org/docs/govt_affairs/advocacy_white_papers/ management_third_molar_white_paper.pdf. [Access date June 2, 2021].
- [4].American Association of Oral and Maxillofacial Surgeons. Supporting information to the management of patients with third molar teeth. 2017. Available at: https://www.aaoms.org/images/uploads/pdfs/management_third_molar_supporting_information.pdf [access date June 2, 2021].
- [5].Lee CT, Zhang S, Leung YY, et al. Patients’ satisfaction and prevalence of complications on surgical extraction of third molar. Patient Prefer Adherence. 2015;9:257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sayed N, Bakathir A, Pasha M, et al. Complications of Third Molar Extraction: a retrospective study from a tertiary healthcare centre in Oman. Sultan Qaboos Univ Med J. 2019;19:230e230–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen YW, Chi LY, Lee OK. Revisit incidence of complications after impacted mandibular third molar extraction: a nationwide population-based cohort study. PLoS One. 2021;16:e0246625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bouloux GF, Steed MB, Perciaccante VJ. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am. 2007;19:117–28, vii. [DOI] [PubMed] [Google Scholar]
- [9].Osborn TP, Frederickson G, Jr, Small IA, et al. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg. 1985;43:767–9. [DOI] [PubMed] [Google Scholar]
- [10].Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003;61:1379–89. [DOI] [PubMed] [Google Scholar]
- [11].Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc. 2007;73:325. [PubMed] [Google Scholar]
- [12].Pippi R, Santoro M. A multivariate statistical analysis on variables affecting inferior alveolar nerve damage during third molar surgery. Br Dent J. 2015;219:E3. [DOI] [PubMed] [Google Scholar]
- [13].Jain N, Thomas S, Prabhu S, et al. Influence of tooth sectioning technique and various risk factors in reducing the IAN injury following surgical removal of an impacted mandibular third molar. Oral Maxillofac Surg. 2016;20:149–56. [DOI] [PubMed] [Google Scholar]
- [14].Barone R, Clauser C, Testori T. Del Fabbro M. Self-assessed neurological disturbances after surgical removal of impacted lower third molar: a pragmatic prospective study on 423 surgical extractions in 247 consecutive patients. Clin Oral Investig. 2019;23:3257–65. [DOI] [PubMed] [Google Scholar]
- [15].Renton T, McGurk M. Evaluation of factors predictive of lingual nerve injury in third molar surgery. Br J Oral Maxillofac Surg. 2001;39:423–8. [DOI] [PubMed] [Google Scholar]
- [16].Charan Babu HS, Reddy PB, Pattathan RK, et al. Factors influencing lingual nerve paraesthesia following third molar surgery: a prospective clinical study. J Maxillofac Oral Surg. 2013;12:168–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Contar CM, de Oliveira P, Kanegusuku K, et al. Complications in third molar removal: a retrospective study of 588 patients. Med Oral Patol Oral Cir Bucal. 2010;15:e74–8. [DOI] [PubMed] [Google Scholar]
- [18].Pell GJ, Gregory BT. Impacted mandibular third molars: classification and modified techniques for removal. Dent Digest. 1933;39:330–8. [Google Scholar]
- [19].Hasegawa T, Ri S, Umeda M, et al. Multivariate relationships among risk factors and hypoesthesia of the lower lip after extraction of the mandibular third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:e1–7. [DOI] [PubMed] [Google Scholar]
- [20].Brunello G, De Biagi M, Crepaldi G, et al. An observational cohort study on delayed-onset infections after mandibular third-molar extractions. Int J Dent. 2017;2017:1435348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Sweet JB, Butler DP. Effect of smoking on the incidence of localized osteitis following mandibular third molar surgery. Quintessence Int Dent Dig. 1978;9:9–10. [PubMed] [Google Scholar]
- [22].Sweet JB, Butler DP. The relationship of smoking to localized osteitis. J Oral Surg. 1979;37:732–5. [PubMed] [Google Scholar]
- [23].Field EA, Speechley JA, Rotter E, et al. Dry socket incidence compared after a 12 year interval. Br J Oral Maxillofac Surg. 1985;23:419–27. [DOI] [PubMed] [Google Scholar]
- [24].Benediktsdottir IS, Wenzel A, Petersen JK, et al. Mandibular third molar removal: risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:438–46. [DOI] [PubMed] [Google Scholar]
- [25].Cardoso CL, Rodrigues MT, Ferreira Junior O, et al. de Carvalho PS. Clinical concepts of dry socket. J Oral Maxillofac Surg. 2010;68:1922–32. [DOI] [PubMed] [Google Scholar]
- [26].Tojyo I, Nakanishi T, Shintani Y, et al. Risk of lingual nerve injuries in removal of mandibular third molars: a retrospective case-control study. Maxillofac Plast Reconstr Surg. 2019;41:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Shorr RI, Ray WA, Daugherty JR, et al. Concurrent use of nonsteroidal anti-inflammatory drugs and oral anticoagulants places elderly persons at high risk for hemorrhagic peptic ulcer disease. Arch Intern Med. 1993;153:1665–70. [PubMed] [Google Scholar]
- [28].Silverstein FE, Faich G, Goldstein JL, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA. 2000;284:1247–55. [DOI] [PubMed] [Google Scholar]
- [29].Perry DJ, Noakes TJ, Helliwell PS; British Dental Society. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. Br Dent J. 2007;203:389–93. [DOI] [PubMed] [Google Scholar]
- [30].Aframian DJ, Lalla RV, Peterson DE. Management of dental patients taking common hemostasis-altering medications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:S45.e1–11. [DOI] [PubMed] [Google Scholar]
- [31].Yamada SI, Hasegawa T, Soutome S, et al. Prevalence of and risk factors for postoperative hemorrhage after lower third molar extraction on warfarin therapy: a multicenter retrospective study in Japan. Odontology. 2020;108:462–9. [DOI] [PubMed] [Google Scholar]
- [32].Adeyemo WL, Ogunlewe MO, Ladeinde AL, et al. Prevalence and surgical morbidity of impacted mandibular third molar removal in the aging population: a retrospective study at the Lagos University Teaching Hospital. Afr J Med Med Sci. 2006;35:479–83. [PubMed] [Google Scholar]
- [33].Leung YY, Cheung LK. Risk factors of neurosensory deficits in lower third molar surgery: an literature review of prospective studies. Int J Oral Maxillofac Surg. 2011;40:1–10. [DOI] [PubMed] [Google Scholar]
- [34].Howe GL. Minor oral surgery. Mumbai: Varghese Publishing House, 1996, pp 109–143. [Google Scholar]
- [35].Jun SH, Kim CH, Ahn JS, et al. Anatomical differences in lower third molars visualized by 2D and 3D X-ray imaging: clinical outcomes after extraction. Int J Oral Maxillofac Surg. 2013;42:489–96. [DOI] [PubMed] [Google Scholar]
- [36].Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28:20–5. [DOI] [PubMed] [Google Scholar]
- [37].Chamorro-Petronacci CM, Pérez-Sayáns M, Gay-Escoda C, et al. Analysis of the unpredictable migration of impacted mandibular third molars: a pilot study. J Clin Exp Dent. 2020;12:e1145–9. [DOI] [PMC free article] [PubMed] [Google Scholar]