Abstract
The assessment of muscle health is of paramount importance, as the loss of muscle mass and strength can affect performance. Two non-invasive tools that have been found to be useful in this are the MyotonPRO and rehabilitative ultrasound imaging, both have shown to be reliable in previous studies many of which conducted by the research team. This study aims to determine the reliability of previously unassessed local body structures and to determine their minimal detectable changes (MDC) to support both researchers and clinicians. Twenty healthy participants were recruited to determine the reliability of seven skin positions out of a previously established protocol. Reliability was determined between three independent raters, and day to day reliability was assessed with one rater a week apart. Intraclass Correlation Coefficients (ICC) between raters and between days for tissue stiffness, tone and elasticity range from moderate to excellent (ICC 0.52–0.97), with most good or excellent. ICCs for subcutaneous thickness between days was good or excellent (ICC 0.86–0.91) and moderate to excellent between raters (ICC 0.72–0.96), in muscles it was moderate to excellent between raters and days (ICC 0.71–0.95). The protocol in this study is repeatable with overall good reliability, it also provides established MDC values for several measurement points.
Subject terms: Physiology, Medical research, Medical imaging
Introduction
The assessment of muscle health is of paramount importance, as the loss of muscle mass and strength can affect physical function1, quality of life2, and even mortality3. Assessment is relevant to a variety of situations and settings, many of which are out in the field where ease of access, handling and cost are critical factors. These situations include assessing changes in muscle over time in people: who are frail due to ageing4; after injury5; post-surgery6; during a period of inactivity (e.g. on intensive care7; neurodegenerative diseases i.e. Parkinson’s disease, stroke8 etc.; or during/after exposure to microgravity9). Accurate and reliable assessment requires robust protocols using valid and reliable tools. Assessment of abnormality for an individual can be made by comparison with normative values in the literature or between groups of people10. Where individuals are assessed over time, the precision of error in measurements needs to be known, so that real change can be identified, hence the minimal detectable change (MDC) for a measurement is needed10–12. The present paper describes a protocol for a study of astronauts (Myotones project; European Space Agency) on 6-month missions on the International Space Station (ISS), to examine whether there are any effects of microgravity on muscles/tendons/fascial biomechanical and viscoelastic tissue properties. The structures under investigation in the present reliability study were selected by anatomical criteria for their superficial location, ease of recognition of anatomical landmarks on the body for locating measurement points (MPs), and ease of reference for operators without a medical background. The study focuses on sites not previously evaluated for reliability and provides MDC values for each site, to enable individuals to be assessed and monitored over time.
Two portable technologies that have been shown to be valid and reliable and being used in the Myotones project are rehabilitative Ultrasound Imaging (RUSI) for measuring muscle thickness13,14 and non-invasive Myoton technology for assessing biomechanical and viscoelastic properties15,16. There is evidence of good reliability for both RUSI17–19 and the MyotonPRO device8,11 for particular muscles and tendons, but for new sites used in the Myotones project, their reliability (both interrater and intrarater) needs to be established.
The RUSI technique provides a safe, portable and relatively inexpensive means to evaluate muscle health status and observe changes in clinical and research environments13,14. Muscle strength is correlated to cross-sectional area (CSA)20 and CSA is strongly correlated with muscle thickness21,22. Muscle thickness therefore provides an indirect measure of muscle strength without the need for complex equipment and in people not otherwise able to perform strength tests, e.g., due to pain or cognitive impairments.
The MyotonPRO device does not require such high levels of expertise as RUSI and can be used effectively by novices16, as long as the correct measurement positions can be found. The MyotonPRO detects the damped natural oscillations of the superficial tissue in the form of an acceleration signal allowing resting tone (Hz), dynamic stiffness (N/m) and elasticity (logarithmic decrement; log), to be measured16.
The present study examined the reliability of the MyotonPRO and RUSI measurements at specific sites for various structures (muscle, tendon, fascia) of the lower and upper limbs and the trunk as previously reported in principle from a recent study on 24 healthy male bedrest participants23, to produce MDC values for monitoring changes over time in individuals. These sites are based on the structures being assessed in the Myotones project on the ISS, which aims to evaluate a means of rapid, efficient, accurate inflight monitoring of the health status of an astronaut’s muscles and related soft tissues24. Assessing these structures reliably is also intended to be of use to clinicians and researchers.
Aim
To describe the protocol for examining several muscles potentially affected by prolonged inactivity affected by inactivity using two technologies (MyotonPRO and ultrasound imaging) and to establish reliability of measurements and produce MDC values.
Objectives
Define the methodology and protocol used to measure the mechanical properties of superficial structures using the MyotonPRO and muscle and subcutaneous tissue thickness using ultrasound imaging.
To examine interrater reliability of Myoton and ultrasound measurements between three independent researchers at seven measurement sites on the same day.
To examine intrarater reliability of measurements taken on different days one week apart.
To establish MDC values for measurements of the various structures, repeated on different days to provide reference values for assessment of change in individuals over time.
Methods
Participants
Published recommendations of sample size requirements for reliability studies vary, but 15–20 participants has been suggested as sufficient25, and previous studies with Myoton have used 20 or fewer participants26–28. Twenty healthy participants were recruited (n = 10 males, n = 10 females) from staff and students at the University of Southampton (age 28.95 ± 2.77 BMI 24.28 ± 1.47) took part in the study. Ethics approval was obtained from the Faculty of Environmental and Life Sciences Ethics Committee (no. 40307), University of Southampton. All methods were performed in accordance with the relevant guidelines and regulations. Posters were circulated throughout the faculty advertising the study. Informed consent was obtained from all subjects prior to testing. Participants were asked to attend two sessions, the first lasting approximately two hours, and the second a week later lasting one hour held in the afternoons29. The room was set to an ambient temperature 22–24 °C, warm clothes worn during measurements, to avoid temp induced tonus changes.
Inclusion criteria
Over the age of 18 up to the age of 40; able to understand English.
Exclusion criteria
Musculoskeletal injury or surgery in the last five years which led to immobility for more than one week; uncontrolled diabetes or blood pressure; a known neurological disorder; arthritis restricting ability to perform everyday activities; receiving treatment for cancer; taking medication which affects muscle function. No scars on MP sites, no obvious inflammation/reddening of the skin, no underlying disease leading to spasms/paralysis (Parkinson’s disease, Huntington’s disease, stroke, nerve damage, etc.), no tonus reducing or enhancing agents were taken 12 h previous to the measurement (muscle relaxants, coffee more than 1 cup, alcohol, drugs, etc.), Participants were asked not to undertake any strenuous exercise within 12 h before the data collection session, including their mode of transport to the session (e.g. to take public transport or drive, as opposed to walking or cycling).
Measurement points
The MP for this study were based on those for the Myotones project currently ongoing on the ISS24, where both technologies are tested at 11 sites (seven of which are assessed in this study). All MPs (all on right side) can be seen below (Fig. 1).
Figure 1.
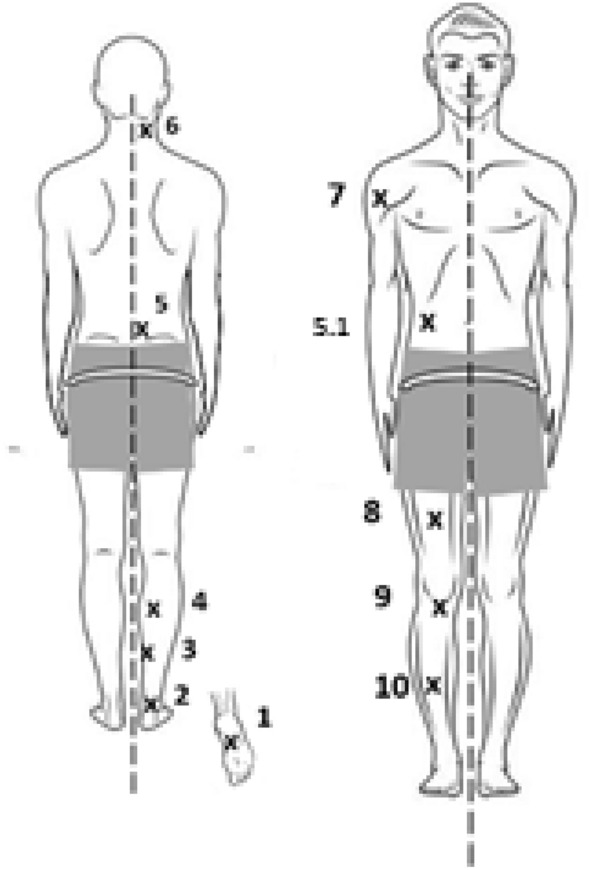
Dorsal (left) and Ventral (right) measurement points (right side only) are shown in body chart.
As some of the MPs listed below included in the Myotones study already have well established reliability, only seven measurement points were examined in the present study: MP1, MP2, MP3, MP6, MP7, MP9, and MP10.
Participant in prone lying: with roller under the ankle
Plantar fascia (MP1)—palpate the fascia (tight band) from the middle arch of the foot up towards the heel until the feel of the band is lost. MP1 is 1 cm down from the base of the heel (confirmed with ultrasound)—ultrasound image taken longitudinally.
Achilles tendon (MP2)—thinnest part of the tendon (palpatable using thumb and index finger as “forceps” or “tweezer grip”)—ultrasound image taken longitudinally.
Soleus (MP3)—Measure the distance between MP2 and middle of the popliteal crease at the back of the knee. MP3 is located 33% up the back of the calf from MP2, then 3 cm medially—ultrasound image taken longitudinally.
Gastrocnemius (MP4)—from MP2, measure 66% up the back of the calf, then 3 cm medially—ultrasound image taken longitudinally.
Multifidus lumbar L4 (MP5)—draw the line (tape measure) between the top of hips (Iliac crests of pelvis) to find level on the backbone. From the mid-point on the spine, measure x = 1 cm to the right—ultrasound image taken transversely.
Transversus abdominis (TrA; 5.1)—find the Umbilicus (belly button), move laterally until the three lateral abdominal muscles (external oblique, internal oblique, TrA) are seen as parallel (ultrasound only).- ultrasound image taken transversely.
Participant in sitting
-
7.
Splenius capitis (MP6)—tape measure between the base of the external occipital protuberance (bump at back of the skull base) and the Acromion (bump on top of shoulder) and mark the centre of the line. Tape measure between C7 and angle of the jaw (mandible) just below the ear and mark where the lines cross. From this intersection, move 3 cm forward from this cross (confirmed with ultrasound).—ultrasound image taken transversely.
Participant in supine lying: with roller under the knee
-
8.
Deltoid anterior (MP7)—place a tape measure from the Acromion down to the crease on front of elbow. Put your finger on the tape at the same height as the crease of the armpit and move your finger up 2 cm. To confirm the point, ask the participant to raise their arm, and the muscle should contract under your finger—ultrasound image taken transversely.
-
9.
Rectus femoris (MP8)—tape measure in a line formed between the superior border of the patella and the iliac spine (bump on front of right side of pelvis). From the patella, measure 33% up of the total distance between the above two points—ultrasound image taken transversely.
-
10.
Infrapatellar tendon (MP9)—Locate the inferior edge of the patella in the middle and the tibial tuberosity (bump on top of the tibia or shin bone). Measure 50% of distance between the two points—ultrasound image taken longitudinally.
-
11.
Anterior tibialis (MP10)—measure the distance from the lower edge of the patella to the middle of the ankle joint between the medial and lateral malleoli. Measure 50% of the distance between these two points. Then move 2 cm to the outside of the leg over the muscle belly (Tibialis Anterior)—ultrasound image taken transversely.
MyotonPRO device
A smartphone-sized, non-invasive digital palpation device (MyotonPRO) was used to assess biomechanical properties of muscles (Myoton AS, Estonia). The MyotonPRO device applies mechanical impulses to the skin (duration 15 ms, force 0.4 N) under a pre-compression force of (0.18 N) on the tissue layer of interest to minimize signal bias from soft tissue overlying muscle and tendon. The device is held perpendicular to the skin ± 5° (checked by MyotonPRO device). The impulses cause damped oscillations of the underlying tissues, which are recorded as parameters for tone (represented by frequency, Hz), stiffness (N/m), and elasticity (Logarithmic Decrement). There is a small mark on the probe to show how far to push down on the skin and once the pre-compression load is met, an indicator light changes from orange to green and the preset impulses are applied automatically. The MyotonPRO device records the coefficient of variation (CV) between the sets of at least five different mechanical impulses per measurement and displays this as a percentage next to each parameter. In the present study a threshold of 3% CV was set, if any parameters were over this threshold the measurement was repeated.
Ultrasound imaging
Images were taken using a real-time B-mode ultrasound scanner (ORCHEO lite, SONOSCANNER, Paris, France; designed by CNES, CSA and ESA, referred to as the ECHO device) with a 3.5–16.7 MHz linear transducer. The transducer was placed transversely or longitudinally on the skin, depending upon the MP being imaged (see specific sites above), with minimal pressure to avoid compression of the underlying tissues. Ultrasound images were taken in accordance with the directions stated above, with one image taken at each point.
All images were measured later off-line by one investigator (PM), using a Matlab algorithm (written by MW). Ultrasound imaging of musculoskeletal soft tissues is known to be reliable30,31 and valid32,33 against the gold standard of magnetic resonance imaging (MRI). As with the Myoton technique, standardization of factors influencing recording of images is important14.
Operator experience
The number of years of experience for the three researchers collecting data was: Researcher 1: Ultrasound Imaging 5 years, Myoton technology 5 years; Researcher 2: Ultrasound 13 years, Myoton technology 9 years; Researcher 3: Ultrasound over 30 years, Myoton technology 9 years.
Experimental procedure
During the first session one operator initially located the anatomical measurement points (MPs) and marked them on the participant lying on a gurney at full relaxation. The measurements were recorded in a logbook for each participant ahead of the next session. Three independent operators blind to the other recordings then undertook the MyotonPRO and ultrasound measurements. Raters were not required to re-mark the participants within the same sessions, so reliability of the data acquisition was evaluated and not the whole Myoton or ultrasound procedure.
For the MyotonPRO recordings, two sets of five impulses were applied as described above. Coefficient of variation measurements for each variable on the device were inspected and if any were higher than 3% the measurement was retaken. All points were recorded twice and a mean of the 10 pulses was taken and used in the analysis. Ultrasound images were taken in accordance with the directions stated above, with one image taken at each point.
For the between days intrarater reliability, participants were invited back a minimum of a week later for the second session (in the afternoons), where only measured by one operator repeated both ultrasound and MyotonPRO measurements, after relocating the same MPs as in the previous session.
Data analysis
Interrater reliability was assessed using a two-way mixed, single score intraclass correlation coefficient (ICC) (3,1)34.
Intrarater reliability between days was assessed two-way mixed, single score intraclass correlation coefficient (ICC) (3,1)34.
Intrarater reliability within sessions was assessed using a two-way mixed, average score intraclass correlation coefficient (ICC) (3,2) to compare between the two sets of five impulses.
All statistical tests were performed using SPSS (v 26, Armonk, NY: IBM Corp), with the alpha value set at 0.05.
The guidelines for interpretation of ICC results were taken from Koo and Li30 with below 0.5 = poor, between 0.5–0.75: moderate, between 0.75 and 0.90 = good, and above 0.90 excellent.
Matlab programme for measuring scans
Ultrasound scans were measured with a custom written graphical user interface (GUI) created in Matlab (Mathworks, USA) using bespoke functions (MW). The GUI allowed the investigator to import the bitmap images obtained from the ultrasound scanner. The GUI calibrated the images by determining a scaling factor between the number of pixels and a 1 cm distance obtained from the scale displayed on the side of the ultrasound image. The GUI then allowed measurements to be made on the ultrasound image by the investigator through identifying and clicking on various landmarks. Specific landmarks and measurements are detailed below for each muscle and tendon. Distances were then calculated as the Euclidean distance between landmarks, then converting to centimetres using the scaling factor and then exported to an Excel file.
Scans were calibrated against the scale on the side of the ultrasound scan, marking a measurement of 1 cm with a cursor.
Passive muscle thickness was measured on cross-section planes of ultrasound scans between the muscle’s borders from the bottom of their superior fascia to the top of the inferior fascia.
Tendon/fascia thickness was measured by creating a 1 cm wide box, then creating a line on the top of the structure and a line at bottom. The distance between the two lines was then automatically measured 100 times and the mean thickness measurement was taken.
Subcutaneous tissue thickness was measured from the top of the skin to the superior border of the muscle fascia (that is regular peripheral body fascia structure with compartment fascia and epimysial layers considered as one structural layer (i.e., muscle fascia) of regional variance however all these structural layers are however below USI image resolution). A second measurement was taken from the superior border of the muscle fascia to its inferior border. The thickness of the fascia was included with fat thickness in the subcutaneous tissue measurement (Fig. 2). The deep foot extensors (MP10 deep foot extensors)- only measured with ultrasound using the same subcutaneous tissue thickness as MP10, but with the muscles measured as one complex all the way to the tibia.
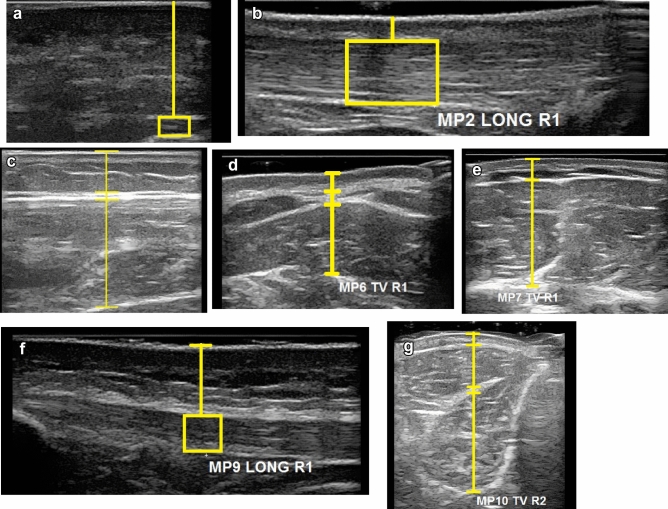
Figure 2.
Example of ultrasound, and measurement points for data analysis. (a) Plantar Fascia, (b) Achilles tendon, (c) Soleus, (d) Splenius capitis, (e) Anterior Deltoid, (f) Patellar tendon, (g) Anterior tibialis.
Minimal detectable change (MDC)
The MDC gives a meaningful and practical assessment of measurement error, providing a single value for each variable in the unit of relevant measure35, which is the smallest change in score that occurs due to error and not likely related to chance variation in measurement36. The MDC based on the SEM was calculated using the following formula outlined in Haley and Fragala-Pinkham36: MDC = 1.96 (z scorelevel of confidence) × √2 × SEM). The formula to calculate SEM was SEM = SD × (√(1 − ICC)) as outlined in Wilken, Rodriguez35.
Bland and Altman
To complement the ICC reliability data, the Bland and Altman test with limits of agreement was used and graphed (Supplementary Table 1)36. This test was conducted between each researcher (R1–R2, R2–R3, R1–R3), and for the between day testing.
Results
The results of the MyotonPRO and Ultrasound are presented below, they range from moderate to excellent, with the vast majority being good or excellent.
MyotonPRO results
The same day intrarater reliability within session for the MyotonPRO comparing the two sets of five pulses was excellent for all parameters in all sites tested (ranging from 0.96–0.99, Supplementary Table 2) and are not presented in further detail below.
Stiffness (N/m)
Interrater reliability within session was excellent or good at all measurement points with the exception of Splenius capitis (MP6 = 0.733) which is moderate (Table 1). Between days intrarater reliability is also excellent or good for all but two measurement points, Splenius capitis (MP6) and Soleus (MP3), which are moderate.
Table 1.
MyotonPRO stiffness results for intrarater (between days) and interrater reliability, mean stiffness of first session and minimal detectable change (within and between raters).
| Measurement point | Interrater reliability | Intrarater reliability | Mean stiffness (N/m) of first session (standard deviation) | Minimal detectable change (N/m) (between days rater 1) | Minimal detectable change (N/m) (interrater) |
|---|---|---|---|---|---|
| MP1 | 0.97 | 0.96 | 476 (83) | 47.4 | 40.9 |
| MP2 | 0.86 | 0.90 | 796 (67) | 58.8 | 69.0 |
| MP3 | 0.95 | 0.66 | 368 (88) | 140.6 | 52.0 |
| MP6 | 0.73 | 0.57 | 212 (33) | 59.1 | 47.2 |
| MP7 | 0.89 | 0.92 | 214 (53.3) | 40.5 | 47.7 |
| MP9 | 0.85 | 0.98 | 383 (124.5) | 50.9 | 127.9 |
| MP10 | 0.93 | 0.85 | 573 (81.9) | 88.5 | 61.7 |
MP1 Plantar Fascia, MP2 Achilles tendon, MP3 Soleus, MP6 Splenius capitis, MP7 Anterior Deltoid, MP9 Patellar tendon, MP10 Anterior tibialis.
Tone (frequency)
Most measurement points showed good to excellent interrater reliability with the exception of Achilles tendon (MP2) and Splenius capitis (MP6), both of which have moderate reliability (Table 2). Between day reliability is excellent for plantar fascia (MP1), Soleus (MP3), Tibialis anterior (MP10), good for anterior deltoid (MP7) and Patellar tendon (MP9), and moderate for the Achilles tendon (MP2) and Splenius capitis (MP6). The MDC for each measurement point has also been calculated.
Table 2.
Myoton frequency results for intrarater (between-days) and interrater reliability, mean frequency of first session and minimal detectable change.
| Measurement point | Interrater reliability | Intrarater reliability | Mean frequency (Hz) of first session (standard deviation) | Minimal detectable change (Hz) (between days) | Minimal detectable change (Hz) (interrater) |
|---|---|---|---|---|---|
| MP1 | 0.92 | 0.85 | 23.5 (2.6) | 3.0 | 2.0 |
| MP2 | 0.52 | 0.52 | 29.9 (2.4) | 4.6 | 5.0 |
| MP3 | 0.95 | 0.90 | 17.5 (3.6) | 3.2 | 2.1 |
| MP6 | 0.70 | 0.51 | 13.2 (1.0) | 2.4 | 1.6 |
| MP7 | 0.80 | 0.75 | 13.9 (1.8) | 2.6 | 2.3 |
| MP9 | 0.88 | 0.77 | 17.5 (2.6) | 3.5 | 2.5 |
| MP10 | 0.91 | 0.80 | 24.7 (2.8) | 3.7 | 2.5 |
MP1 Plantar Fascia, MP2 Achilles tendon, MP3 Soleus, MP6 Splenius capitis, MP7 Anterior Deltoid, MP9 Patellar tendon, MP10 Anterior tibialis.
Elasticity (decrement)
Interrater reliability was excellent or good at all measurement points with the exception of Solues (MP3; 0.65), which had moderate reliability (Table 3). Between days intrarater reliability was excellent for Splenius capitis (MP6), Anterior Deltoid (MP7), and Anterior tibialis (MP10), and moderate for Plantar Fascia (MP1), Achilles tendon (MP2), Soleus (MP3), and Patellar tendon (MP9).
Table 3.
Myoton elasticity results for intrarater (between-days) and interrater reliability, mean elasticity of first session and minimal detectable change.
| Measurement point | Interrater reliability | Intrarater reliability | Mean elasticity (log decrement) of first session (standard deviation) | Minimal detectable change (log decrement) (between days) | Minimal detectable change (log decrement) (interrater) |
|---|---|---|---|---|---|
| MP1 | 0.90 | 0.55 | 1.15 (0.12) | 0.23 | 0.12 |
| MP2 | 0.77 | 0.63 | 0.84 (0.21) | 0.33 | 0.25 |
| MP3 | 0.65 | 0.71 | 1.18 (0.17) | 0.27 | 0.26 |
| MP6 | 0.92 | 0.91 | 1.15 (0.20) | 0.17 | 0.15 |
| MP7 | 0.77 | 0.94 | 0.91 (0.19) | 0.13 | 0.25 |
| MP9 | 0.85 | 0.68 | 0.99 (0.13) | 0.21 | 0.14 |
| MP10 | 0.87 | 0.95 | 0.82 (0.16) | 0.09 | 0.16 |
MP1 Plantar Fascia, MP2 Achilles tendon, MP3 Soleus, MP6 Splenius capitis, MP7 Anterior Deltoid, MP9 Patellar tendon, MP10 Anterior tibialis.
Ultrasound imaging results
Subcutaneous thickness
Interrater reliability for subcutaneous thickness ranges from excellent Soleus (MP3), Patellar tendon (MP9), and Anterior tibialis (MP10) to moderate Plantar Fascia (MP1), with the majority showing good reliability (Table 4). Intrarater reliability was good or excellent.
Table 4.
Ultrasound imaging subcutaneous thickness results for interrater and intrarater (between-days) reliability, mean subcutaneous thickness, and minimal detectable change.
| Measurement points | Subcutaneous thickness interrater reliability | Subcutaneous thickness Intrarater reliability (between-days) | Mean subcutaneous thickness (mm) of first session (standard deviation) | Subcutaneous thickness MDC between-days (mm) |
|---|---|---|---|---|
| MP1 | 0.72 | 0.88 | 14.3 (2.2) | 2.1 |
| MP2 | 0.86 | 0.91 | 3.4 (1.1) | 0.9 |
| MP3 | 0.96 | 0.91 | 11.3 (4.3) | 3.8 |
| MP6 | 0.85 | 0.90 | 6.5 (1.8) | 1.6 |
| MP7 | 0.87 | 0.9 | 6.3 (4.1) | 4.9 |
| MP9 | 0.90 | 0.90 | 6.1 (1.4) | 1.3 |
| MP10 | 0.93 | 0.86 | 3.7 (2.0) | 2.2 |
MP1 Plantar Fascia, MP2 Achilles tendon, MP3 Soleus, MP6 Splenius capitis, MP7 Anterior Deltoid, MP9 Patellar tendon, MP10 Anterior tibialis.
Muscle/tendon/plantar fascia
Intrarater reliability for muscle/tendon/plantar fascia thickness ranged from excellent Plantar Fascia (MP1), Patellar tendon (MP9), and Anterior tibialis deep muscle group (MP10) to moderate Achilles tendon (MP2). Interrater reliability ranged from excellent Splenius capitis (MP6), Anterior deltoid (MP7), Patellar tendon (MP9), and Anterior tibialis deep muscle group (MP10) to moderate Achilles tendon (MP2), with the majority showing good reliability (Table 5).
Table 5.
Ultrasound imaging Muscle/tendon/fascia thickness results for interrater and intrarater (between-days) reliability, mean Muscle/tendon/fascia thickness, and minimal detectable change.
| Measurement points | Muscle/tendon/fascia thickness interrater reliability | Muscle/tendon/fascia thickness intrarater reliability | Average of first session muscle/tendon/fascia thickness (mm) | Muscle/tendon/fascia MDC between days (mm) |
|---|---|---|---|---|
| MP1 | 0.80 | 0.91 | 1.85 | 0.36 |
| MP2 | 0.74 | 0.71 | 4.44 | 0.83 |
| MP3 | 0.88 | 0.82 | 14.84 | 3.2 |
| MP6 | 0.92 | 0.85 | 6.9 | 2.08 |
| MP7 | 0.90 | 0.93 | 19.83 | 4.17 |
| MP9 | 0.92 | 0.90 | 3.73 | 0.53 |
| MP10 | 0.94 | 0.95 | 7.06 | 1.51 |
| MP10 (deep foot extensors) | 0.82 | 0.87 | 29.38 | 3.61 |
MP1 Plantar Fascia, MP2 Achilles tendon, MP3 Soleus, MP6 Splenius capitis, MP7 Anterior Deltoid, MP9 Patellar tendon, MP10 Anterior tibialis.
Discussion
The purposes of this study have been achieved, which were to: describe the protocol for examining several muscles affected by inactivity using two technologies (MyotonPRO and ultrasound imaging); establish the interrater and intrarater reliability of the measurement techniques; and provide reference values for MDC for use in studies monitoring change over time in people undergoing or recovering from the effects of inactivity. Examples of this include, astronauts during and after microgravity; people in intensive care or inactive with an illness or injury and during rehabilitation; or people living with long-term conditions affecting muscle mass. Reliability for some of the measurement points in the protocol of 11 sites have already been established in the literature in healthy cohorts, so the present study focussed on sites requiring reliability data, including MDC, and for completion in the context of the entire protocol, results from all sites are included in the discussion below. Overall, the majority of measurement points had good or excellent reliability with both the MyotonPRO and ultrasound device, with several found to be moderate, and none poor. It is important to note when interpreting the interrater reliability results that the raters did not re-mark measurement points so only the reliability of the data acquisition was evaluated.
Reliability of measurements from the MyotonPRO
Same session intrarater reliability was excellent at all points and for all Myoton parameters (ICC 0.96–0.99), which is well established in the literature8,15,20,37. This high level of reliability is enabled when, as in the present study, a threshold CV of 3% is used, and any measurements with higher values are discarded and recordings re-taken. Even in Dellalana et al.11 where the CV value for the gastrocnemius medialis measurements were 5.5% for stiffness the ICC was 0.96, showing the robustness of the device and the importance of taking a mean of the measurements. It should, however, be noted that a different probe was used in the above study11, which focussed on skin stiffness, while the present study focussed on muscle stiffness.
The intrarater reliability between-days was examined by Rater 1 and was excellent to good for all three Myoton parameters at most of the measurement points, with several being moderately reliable. None of the measurement points were fair or poor, which is consistent with the literature on other measurement points16,30,36,38,39. The MDCs between sessions are also low (Tables 1, 2, 3).
The lower reliability observed between days compared to measurements during the same session was expected and could be explained by several factors, such as: ability of the operator to find the same testing site on a different day, which was not required for recordings repeated within the same session; subtle changes in the muscle length and tension due to slightly different positioning; different activity prior to testing, or change in temperature etc.40. Differences in recordings are unlikely to be due to the device used, which is calibrated by the manufacturer remains consistent when tested on phantom materials. Between-day reliability is necessary to enable monitoring of changes over time to examine the effects of disuse/disease/injury and in response to an intervention. Reliability between days seems to be higher on larger structures that are easier to relocate such as soleus (MP3), gastrocnemius medialis (MP4), multifidus (MP5), and rectus femoris (MP8).
Subcutaneous tissue overlying the tissue of interest (muscle/tendon/fascia) may vary in structure and composition (dermis collagens vs adipose) but also water/fluid content between participants and between different body locations (limbs and trunk). Due to the MyotonPRO device presettings and algorithm, however, short moderate pre-compression of the probe (targeted to soft tissue compression), followed by several stronger compression impulses (targeted to more dense muscle tissue with oscillation signal reflows), does not completely mitigate but minimizes oscillation signal bias from overlying subcutaneous tissue composition41.
Interrater reliability was excellent or good for all measurement points, in both the present study and previous studies (Supplementary Table 3). This indicates that the Myoton technique is robust, giving confidence in situations where it is not always possible to have the same operator for each session. Such as in the Schoenrock, Zander23 study which was required to used two independent operators due to scheduling. Most studies have involved experienced operators, but reliability has also been examined in novice operators, and has been found to be good16,37. Demonstration of reliability in novices was important for using the present protocol in the Myotones project, in which astronauts conduct Myoton recordings (as relative novices) on one another during their 6-month inflight period on the International Space Station24.
Not all reliability studies have reported MDCs for all three parameters reported in the present paper, as indicated in Supplementary Table 3.
Reliability of ultrasound imaging of muscle and related tissues
The present study demonstrated excellent or good intrarater reliability between days (Table 4) for all MPs apart from the thickness of the Achilles tendon, which was still moderate (ICC 0.71). These findings were similar to those of previous studies that also found excellent or good intrarater reliability (Supplementary Table 4). The only other study found to assess intrarater reliability of subcutaneous tissue thickness found excellent results30, further supporting the present results.
Interrater reliability was also excellent to good, with the exception of two points (plantar fascia subcutaneous thickness and Achilles thickness, which were still moderate (ICC 0.72 and 0.71 respectively), potentially due to the small measurements involved. This is similar to the results of previous studies assessing ultrasound interrater reliability (Supplementary Table 3)17,42–45.
It is common for ultrasound studies to take more than one scan and using the mean value in the analysis (similar to MyotonPRO)46,47. Excellent intrarater results within the same session from previous studies48 have demonstrated that it is not always necessary to take more than one scan at each measurement point. This fact is very helpful for situations where time restraints make only one measurement feasible, such as astronaut protocols in spaceflight and research projects with high level athletes.
Relevance of the MPs studied
It is hypothesized that during human body unloading in spaceflight muscle stiffness will decrease particularly in those muscles which are most important for postural support and movement (running, walking) on the ground (e.g. Soleus, Multifidus, vastus lateralis, paraspinal muscles of neck and back), whilst other phasic muscles (such as Gastrocnemius, Rectus abdominis, or shoulder and arm muscles) which are only slightly active if at all during microgravity-induced unloading in spaceflight will be relatively unaffected thus serving as internal control.
Limitations of the study
A limitation of this study is that the reliability of finding the measurement points of interest has not been established amongst novice users or those who are not familiar with anatomical positions. Between day reliability was also only assessed by one researcher, so other variations could have been present if all the researchers were required to take measurements again. All ultrasound scans were measured by one investigator, so interreliabilty examined the ultrasound acquisition technique of the raters but not the whole technique of obtaining and measuring scans. Furthermore, as same day measurements did not require re-marking of measurement points between raters, the interrater reliability evaluates data acquisition, rather than the full protocol. However, this study design enabled reliability of the actual imaging technique to be examined, which is of value to determine. Whilst effort was made to keep the time of day consistent, this was not always possible, this could have accounted for some of the change in muscle tone, as Basti, Yalçin29 states that resting muscle tone can be naturally change across the time of day.
Conclusions
A protocol for testing muscle biomechanical properties such as tone, stiffness and elasticity (using the MyotonPRO device) and subcutaneous and muscle thickness (using ultrasound imaging) has been described for measuring several sites of the healthy body (female and male) relevant for assessing the effects of inactivity and recovery in relatively young and healthy study participants. Reliability of both technologies was high. Intrarater reliability (same session) for the MyotonPRO was consistently excellent (all ICCs > 0.96) at all measurement points and for each of the three parameters, indicating that only one set of five mechanical impulses (5 × 0.4 N force) are necessary per measurement point.
Overall, interrater reliability of MyotonPRO measurements was excellent to good, with a small number of values moderate. This indicates that any Myoton operators within future protocols in many research laboratories and clinical settings will be able to collect reliable data.
The excellent to moderate intra-rater reliability (between-days) results indicate that the Myoton results for the operator studied (Rater 1) were repeatable.
The ultrasound scans from this study have been shown to be good to excellent except for three points which remained moderate: Intrarater reliability between days thickness of the Achilles tendon (ICC 0.71), Interrater reliability plantar fascia subcutaneous thickness and Achilles tendon thickness, (ICC 0.72 and 0.71 respectively).
Minimal detectable change (MDC) values have been documented for measurement points over particular muscles, tendons and the plantar fascia, for both Myoton and ultrasound measurements, providing a reference source for studies monitoring change over time. Values for MDC available in the literature from measurement points in the Myotones protocol but not included in the present study are also given in the present paper to provide a more complete reference for the protocol.
Supplementary Information
Author contributions
All authors read and approved the final manuscript and met the four primary I.C.M.J.E. criteria for authorship. In addition, all authors have been actively involved in the study in different capacities: P.E.M drafted the paper with contributions and approval from all authors. P.E.M, M.B.W, M.S, M.H, D.M, R.M, B.S and D.B were involved in the concept and design of the study. P.E.M, T.CJ, M.B.W, M.S and R.M were involved in the acquisition and analysis of the data.
Funding
Funding was provided by UK Space Agency & Science and Technology Facilities Council (Grant No. ST/R005680/1).
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-17507-2.
References
- 1.Fukagawa NK, et al. The relationship of strength to function in the older adult. J. Gerontol. A. 1995;50:55–59. doi: 10.1093/gerona/50A.Special_Issue.55. [DOI] [PubMed] [Google Scholar]
- 2.Silva Neto LS, et al. Association between sarcopenia, sarcopenic obesity, muscle strength and quality of life variables in elderly women. Braz. J. Phys. Ther. 2012;16(5):360–367. doi: 10.1590/S1413-35552012005000044. [DOI] [PubMed] [Google Scholar]
- 3.Rantanen T, et al. Muscle strength and body mass index as long-term predictors of mortality in initially healthy men. J. Gerontol. A Biol. Sci. Med. Sci. 2000;55(3):M168–M173. doi: 10.1093/gerona/55.3.M168. [DOI] [PubMed] [Google Scholar]
- 4.Cuellar W, et al. The assessment of abdominal and multifidus muscles and their role in physical function in older adults: A systematic review. Physiotherapy. 2017;103(1):21–39. doi: 10.1016/j.physio.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Hodges P, et al. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine. 2006;31(25):2926–2933. doi: 10.1097/01.brs.0000248453.51165.0b. [DOI] [PubMed] [Google Scholar]
- 6.Hebert JJ, et al. A systematic review of the reliability of rehabilitative ultrasound imaging for the quantitative assessment of the abdominal and lumbar trunk muscles. Spine. 2009;34(23):E848–E856. doi: 10.1097/BRS.0b013e3181ae625c. [DOI] [PubMed] [Google Scholar]
- 7.Berg HE, et al. Hip, thigh and calf muscle atrophy and bone loss after 5-week bedrest inactivity. Eur. J. Appl. Physiol. 2007;99(3):283–289. doi: 10.1007/s00421-006-0346-y. [DOI] [PubMed] [Google Scholar]
- 8.Chuang LL, Wu CY, Lin KC. Reliability, validity, and responsiveness of myotonoinetric measurement of muscle tone, elasticity, and stiffness in patients with stroke. Arch. Phys. Med. Rehabil. 2012;93(3):532–540. doi: 10.1016/j.apmr.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Hides JA, et al. Changes in multifidus and abdominal muscle size in response to microgravity: Possible implications for low back pain research. Eur. Spine J. 2016;25(1):175–182. doi: 10.1007/s00586-015-4311-5. [DOI] [PubMed] [Google Scholar]
- 10.Jansen J, et al. Resting thickness of transversus abdominis is decreased in athletes with longstanding adduction-related groin pain. Man. Ther. 2010;15(2):200–205. doi: 10.1016/j.math.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Dellalana LE, et al. Reproducibility of the durometer and myoton devices for skin stiffness measurement in healthy subjects. Skin Res. Technol. 2018;1:1–10. doi: 10.1111/srt.12646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filippo M, et al. Inter-rater and intra-rater reliability of ultrasound imaging for measuring quadriceps muscle and non-contractile tissue thickness of the anterior thigh. Biomed. Phys. Eng. Express. 2019;5(3):037002. doi: 10.1088/2057-1976/ab102f. [DOI] [Google Scholar]
- 13.Whittaker JL, et al. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br. J. Sports Med. 2019;53(23):1447–1453. doi: 10.1136/bjsports-2018-100193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whittaker JL, et al. Rehabilitative ultrasound imaging: Understanding the technology and its applications. J. Orthop. Sports Phys. Ther. 2007;37(8):434–449. doi: 10.2519/jospt.2007.2350. [DOI] [PubMed] [Google Scholar]
- 15.Agyapong-Badu S, et al. Measurement of ageing effects on muscle tone and mechanical properties of rectus femoris and biceps brachii in healthy males and females using a novel hand-held myometric device. Arch. Gerontol. Geriatr. 2016;62:59–67. doi: 10.1016/j.archger.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Aird L, Samuel D, Stokes M. Quadriceps muscle tone, elasticity and stiffness in older males: Reliability and symmetry using the MyotonPRO. Arch. Gerontol. Geriatr. 2012;55(2):e31–e39. doi: 10.1016/j.archger.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Cho KH, Lee HJ, Lee WH. Reliability of rehabilitative ultrasound imaging for the medial gastrocnemius muscle in poststroke patients. Clin. Physiol. Funct. Imaging. 2014;34(1):26–31. doi: 10.1111/cpf.12060. [DOI] [PubMed] [Google Scholar]
- 18.English C, Fisher L, Thoirs K. Reliability of real-time ultrasound for measuring skeletal muscle size in human limbs in vivo: A systematic review. Clin. Rehabil. 2012;26(10):934–944. doi: 10.1177/0269215511434994. [DOI] [PubMed] [Google Scholar]
- 19.Norasteh A, et al. Reliability of B-mode ultrasonography for abdominal muscles in asymptomatic and patients with acute low back pain. J. Bodyw. Mov. Ther. 2007;11(1):17–20. doi: 10.1016/j.jbmt.2005.11.002. [DOI] [Google Scholar]
- 20.Lohr C, et al. Reliability of tensiomyography and myotonometry in detecting mechanical and contractile characteristics of the lumbar erector spinae in healthy volunteers. Eur. J. Appl. Physiol. 2018;2018:1–11. doi: 10.1007/s00421-018-3867-2. [DOI] [PubMed] [Google Scholar]
- 21.Young A, Stokes M, Crowe M. Size and strength of the quadriceps muscles of old and young women. Eur. J. Clin. Invest. 1984;14(4):282–287. doi: 10.1111/j.1365-2362.1984.tb01182.x. [DOI] [PubMed] [Google Scholar]
- 22.Young A, Stokes M, Crowe M. The size and strength of the quadriceps muscles of old and young men. Clin. Physiol. 1985;5(2):145–154. doi: 10.1111/j.1475-097X.1985.tb00590.x. [DOI] [PubMed] [Google Scholar]
- 23.Schoenrock B, et al. Bed rest, exercise countermeasure and reconditioning effects on the human resting muscle tone system. Front. Physiol. 2018;9:810. doi: 10.3389/fphys.2018.00810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blottner, D., Muckelt, P., Albracht, K., Schoenrock, B., Salanova, M., Warner, M., Gunga, C., Stokes, M. MYOTONES|Inflight Muscle Health Status Monitoring During Long-Duration Space Missions Onboard the International Space Station (2019).
- 25.Atkinson G, Nevill AM. Selected issues in the design and analysis of sport performance research. J. Sports Sci. 2001;19(10):811–827. doi: 10.1080/026404101317015447. [DOI] [PubMed] [Google Scholar]
- 26.Bizzini M, Mannion AF. Reliability of a new, hand-held device for assessing skeletal muscle stiffness. Clin. Biomech. 2003;18(5):459–461. doi: 10.1016/S0268-0033(03)00042-1. [DOI] [PubMed] [Google Scholar]
- 27.Janecki D, et al. Muscle passive stiffness increases less after the second bout of eccentric exercise compared to the first bout. J. Sci. Med. Sport. 2011;14(4):338–343. doi: 10.1016/j.jsams.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Viir R, et al. Repeatability of trapezius muscle tone assessment by a myometric method. J. Mech. Med. Biol. 2006;6(02):215–228. doi: 10.1142/S0219519406001856. [DOI] [Google Scholar]
- 29.Basti A, et al. Diurnal variations in the expression of core-clock genes correlate with resting muscle properties and predict fluctuations in exercise performance across the day. BMJ Open Sport Exerc. Med. 2021;7(1):e000876. doi: 10.1136/bmjsem-2020-000876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agyapong-Badu S, et al. Anterior thigh composition measured using ultrasound imaging to quantify relative thickness of muscle and non-contractile tissue: A potential biomarker for musculoskeletal health. Physiol. Meas. 2014;35(10):2165. doi: 10.1088/0967-3334/35/10/2165. [DOI] [PubMed] [Google Scholar]
- 31.Hebert JJ, et al. Early multimodal rehabilitation following lumbar disc surgery: A randomised clinical trial comparing the effects of two exercise programmes on clinical outcome and lumbar multifidus muscle function. Br. J. Sports Med. 2015;49(2):100–106. doi: 10.1136/bjsports-2013-092402. [DOI] [PubMed] [Google Scholar]
- 32.Mendis MD, et al. Validity of real-time ultrasound imaging to measure anterior hip muscle size: A comparison with magnetic resonance imaging. J. Orthop. Sports Phys. Ther. 2010;40(9):577–581. doi: 10.2519/jospt.2010.3286. [DOI] [PubMed] [Google Scholar]
- 33.Worsley PR, et al. Validity of measuring distal vastus medialis muscle using rehabilitative ultrasound imaging versus magnetic resonance imaging. Man. Ther. 2014;19(3):259–263. doi: 10.1016/j.math.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 34.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilken JM, et al. Reliability and minimal detectible change values for gait kinematics and kinetics in healthy adults. Gait Posture. 2012;35(2):301–307. doi: 10.1016/j.gaitpost.2011.09.105. [DOI] [PubMed] [Google Scholar]
- 36.Bland JM, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. The Lancet. 1986;327(8476):307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 37.Mullix J, Warner M, Stokes M. Testing muscle tone and mechanical properties of rectus femoris and biceps femoris using a novel hand held MyotonPRO device: relative ratios and reliability. Work. Pap. Health Sci. 2012;1(1):1–8. [Google Scholar]
- 38.Hu X, et al. Quantifying paraspinal muscle tone and stiffness in young adults with chronic low back pain: A reliability study. Sci. Rep. 2018;8(1):1–10. doi: 10.1038/s41598-018-33214-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kelly JP, et al. Characterization of tissue stiffness of the infraspinatus, erector spinae, and gastrocnemius muscle using ultrasound shear wave elastography and superficial mechanical deformation. J. Electromyogr. Kinesiol. 2018;38:73–80. doi: 10.1016/j.jelekin.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 40.Agyapong-Badu SWM, Samuel D, Stokes M. Practical considerations for standardised recording of muscle mechanical properties using a myometric device: Recording site, muscle length, state of contraction and prior activity. J Musculoskel Res. 2018;2018:21. [Google Scholar]
- 41.Technology—Myoton. (2022). https://www.myoton.com/technology/. Accessed 1 Jun 2022
- 42.Bemben MG. Use of diagnostic ultrasound for assessing muscle size. J. Strength Cond. Res. 2002;16(1):103–108. [PubMed] [Google Scholar]
- 43.Raj IS, Bird SR, Shield AJ. Reliability of ultrasonographic measurement of the architecture of the vastus lateralis and gastrocnemius medialis muscles in older adults. Clin. Physiol. Funct. Imaging. 2012;32(1):65–70. doi: 10.1111/j.1475-097X.2011.01056.x. [DOI] [PubMed] [Google Scholar]
- 44.Thoirs K, English C. Ultrasound measures of muscle thickness: Intra-examiner reliability and influence of body position. Clin. Physiol. Funct. Imaging. 2009;29(6):440–446. doi: 10.1111/j.1475-097X.2009.00897.x. [DOI] [PubMed] [Google Scholar]
- 45.Wilson A, et al. Measuring ultrasound images of abdominal and lumbar multifidus muscles in older adults: A reliability study. Man. Ther. 2016;23:114–119. doi: 10.1016/j.math.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 46.Koppenhaver SL, et al. The effect of averaging multiple trials on measurement error during ultrasound imaging of transversus abdominis and lumbar multifidus muscles in individuals with low back pain. J. Orthop. Sports Phys. Ther. 2009;39(8):604–611. doi: 10.2519/jospt.2009.3088. [DOI] [PubMed] [Google Scholar]
- 47.Sions JM, et al. Ultrasound imaging: Intraexaminer and interexaminer reliability for multifidus muscle thickness assessment in adults aged 60 to 85 years versus younger adults. J. Orthop. Sports Phys. Ther. 2014;44(6):425–434. doi: 10.2519/jospt.2014.4584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Birtles D, et al. Effect of eccentric exercise on patients with chronic exertional compartment syndrome. Eur. J. Appl. Physiol. 2003;88(6):565–571. doi: 10.1007/s00421-002-0740-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on request.