Abstract
Introduction
Greater tuberosity (GT) fractures associated with anterior gleno-humeral (GH) dislocations are unstable, with inadequate treatment leading to displacement, malunion, stiffness and functional disability. We explored its morphological characteristics to ultimately optimize their management.
Methods
We retrospectively reviewed all shoulder radiographs with GT fractures associated with anterior GH dislocations in a university hospital between December 1, 2009 and December 31, 2019. Special considerations were given to fracture morphology, presence and site of comminution, degree of displacement and need for surgical intervention.
Results
133 patients were identified. Most of the fracture-dislocations were multi-fragmentary (86.5%) and located antero- or postero-superiorly (68.7%). Superiorly comminuted GT fractures were twice as likely to displace compared to other sites of comminution (43% vs. 21%, p = 0.03), and require surgery (p = 0.03). Undisplaced comminuted GT fragments, particularly superior patterns, could undergo secondary migration if conservatively treated (p = 0.01). GT fractures fixed with interfragmentary screw suffered more secondary migration but those treated with double-row suture anchors (DRSA) did not on follow-up x-rays at two months.
Conclusion
GT fractures with anterior GH dislocations are frequently comminuted. Those with superiorly situated comminution should have a low threshold for surgical fixation, particularly with DRSA which can prevent secondary fragment migration.
Keywords: Greater tuberosity, Glenohumeral dislocation, Fracture morphology, Displacement, Radiological outcome
1. Introduction
Isolated greater tuberosity (GT) fractures account for 20% of proximal humeral fractures.1 It is widely accepted that at least a 5 mm displacement in any plane is an indication for surgical fixation,1, 2, 3 with as little as 3 mm in a cohort of subjects routinely performing overhead activities.4, 5, 6 Such displacement often leads to a loss of shoulder abduction.7, 8, 9 This is mainly due to alterations in the rotator cuff biomechanics or a direct mechanical block.10, 11, 12, 13 Furthermore painful impingement can result, particularly in those GT fragments displaced superiorly or posteriorly.3,4,14, 15, 16 Therefore, the goals of surgical fixation are anatomical restoration of the displaced GT, preservation of the rotator cuff integrity and early range of motion (ROM).17 Despite extensive literature to ascertain optimal surgical management for isolated GT fractures,12,13,18, 19, 20 there is a scarcity in the literature regarding fracture morphology and treatment of GT fractures associated with anterior glenohumeral (GH) dislocations. 10–30% of dislocations involve a GT fracture, usually due to an impaction against the glenoid or acromion.3,21,22 Compared to isolated GT fractures, these fracture-dislocations are likely to be more unstable,23 have a higher proportion of GT comminution, secondary migration, and acromial impingement.24, 25, 26 Therefore, appropriate management in preventing such pathological sequelae is important. Management can be guided by analysing the fracture pattern morphology of the GT fracture-dislocations. This was our primary aim of the study. In exploring this, it may help to identify those more likely to displace ≥ 5 mm and those where secondary (delayed) migration is common after a period of conservative treatment. Both circumstances are strong indications for surgery,1, 2, 3 and thus one can identify the fracture patterns predisposing to this. The secondary aim was to analyse the success of fixation techniques for these fracture-dislocation morphologies, particularly on preventing further fracture migration in the post-operative period.
2. Materials and methods
A retrospective review of all shoulder radiographs at a single University teaching hospital was performed using the picture archiving and communication system (PACS) that was instituted on December 1, 2009. The review was carried out until December 31, 2019.
Inclusion criteria were GT fractures associated with anterior gleno-humeral (GH) joint dislocation, skeletal maturity and good-quality radiographs of the acute fracture (at minimum an anteroposterior (AP) and lateral view.)
Patients with isolated GT fractures, open fractures, prior bone injuries to the shoulder girdle, and other concurrent fractures of the proximal humerus were excluded.
Radiographs were obtained in the standard anteroposterior and lateral views (before and after reduction). Two of the authors (A.S. and G.P.) independently evaluated the radiographs in a standardized manner. All measurements on x-rays were appropriately calibrated and standardized on the digital templating TraumaCad software. To ensure appropriate evaluation of each radiograph, any discrepancies were highlighted and resolved by consultant shoulder surgeons (A.M. and H·S.). Each of the observers evaluated the radiographs with special considerations given to fracture morphology, site of comminution when present, fracture migration and those requiring surgical intervention. The standardized morphological description distinguished between single, two and multiple (comminuted) fragments (Fig. 1a, b and 1c respectively).27 Relative to its anatomical landmark, direction and site of comminution of the GT fragment (superior, inferior and widespread) in the anteroposterior (AP) view and lateral view were evaluated in mm (Fig. 1, Fig. 2). Fragment migration was also measured in mm. A fracture was defined as ‘displaced’ when any fragment was shifted ≥5 mm or more in any plane. Surgical intervention was defined as early (within three weeks of initial injury) or delayed (those where a trial of conservative treatment was undertaken for more than three weeks).28 Those that underwent surgery had their latest follow-up x-ray analysed to assess for subsequent migration.
Fig. 1.
Morphological description of the GT fragment. A. Single fragment (AP view of right shoulder, November 2011). B. Two fragments (AP view of left shoulder, December 2016) C. Multi-fragmentary, widespread pattern (AP view of right shoulder, February 2012).
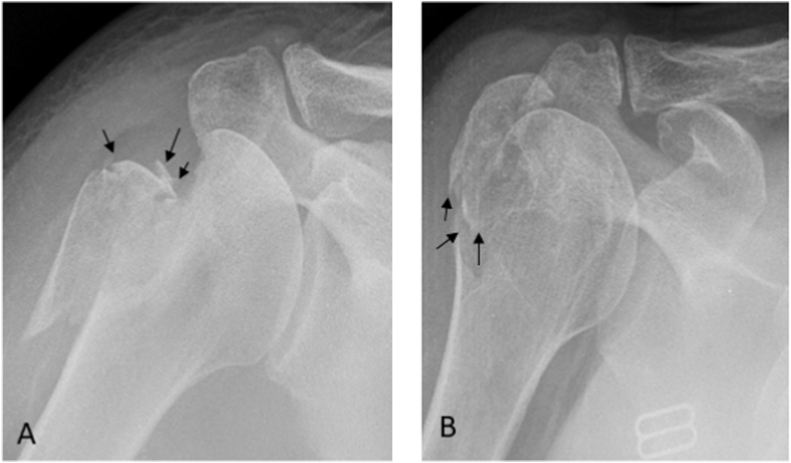
Fig. 2.
A. Superiorly situated comminution of the GT fracture (AP view of right shoulder, November 2012). B. Inferiorly situated comminution of the GT fracture (AP view of right shoulder, November 2014).
Basic demographic variables including age, gender, side and mechanism of injury were recorded for the entire cohort.
2.1. Statistical analysis
Mann-Whitney U test was used for continuous data, and ANOVA and Chi-Squared tests, where appropriate, for categorical data. The latter were performed, where appropriate, to compare age, sex, fracture characteristics, GT displacement and migration. A P value < 0.05 was considered statistically significant. All data analysis was performed with SPSS Version 23.0 (IBM).
3. Results
3.1. Baseline characteristics
A total of 1860 cases GH dislocations were identified over the ten-year period. From this, 133 cases had a GT fracture associated with an anterior GH dislocation (7.2%). The average age was 63 years (range, 18–96 years) with a mean follow-up of 2 months (range, 1–4 months). Both gender and side were evenly distributed over all morphological fracture types. Forty-two patients underwent surgical fixation (either early or delayed). (Table 1).
Table 1.
Demographics, displacement and outcome of GT fractures with anterior GH dislocations. Consideration by number of fragments (single, two and multi-fragmentary). All p-values shown are the results of analysis for all three groups using Chi-Square or ANOVA tests where appropriate. Significant relationships (p < 0.05) are in bold.
| All types | Single (1) fragment | Two (2) fragments | Multi-fragmentary (>2) | Significance | |
|---|---|---|---|---|---|
| Number of cases (%) | 133 (100) | 9 (6.8) | 9 (6.8) | 115 (86.4) | |
| Age (IQR) in years | 63 (50–76) | 35 (32–38) | 58 (56–64) | 65 (53–77) | p = 0.00017 |
| Gender - Male (%) | 66 M (49) | 8M (89) | 5 M (56) | 53 M (46) | p = 0.04 |
| Side - Right (%) | 60 R (45) | 4 R (44) | 3 R (33) | 53 R (46) | p = 0.76 |
| Displaced ≥5 mm post-reduction (n (%)) | 48 (38) | 5 (55) | 1 (11) | 42 (37) | p = 0.14 |
| Surgical Treatment | 42 (32) | 5 (56) | 5 (56) | 32 (28) | p = 0.06 |
3.2. Fracture characteristics: overall population (Table 1)
One-hundred and fifteen patients had a multi-fragmentary (comminution) fracture pattern, with the elderly found to present more with this fracture pattern (65 years, mean age). The younger population presented more frequently with a single fragment fracture (35 years, mean age) (p = 0.00017).
Displacement of the GT fragment and the need for surgical fixation were similar between all fragment groups (p = 0.14 and 0.06 respectively).
Amongst the multi-fragmentary (comminuted) subgroup, the predominant site of comminution was antero- or posterosuperior (68.7%), followed by a widespread pattern (29.6%). Due to insufficient sample size, the inferior site was excluded from further analysis.
Comparison of single, two and superior and widespread multi-fragmentary pattern. In total, forty-eight cases (38%) displaced ≥ 5 mm, and these were found to be more common in the single fragment and superiorly situated multi-fragmentary pattern (p = 0.03).
Comparison of superior and widespread multi-fragmentary pattern. Patients with superior comminution had twice as more displacement of the GT fragments than that of the widespread pattern (43% vs 21% respectively, p = 0.03). All other demographic outcomes were similar.
3.3. Displacement
As earlier described, surgical fixation is indicated for at least a 5 mm GT fragment displacement.1, 2, 3 There were forty-eight cases within this cohort (Table 1). However only twenty-seven patients underwent surgery. The remaining twenty-one were treated conservatively due to several factors, including increasing age (77 years, mean age vs. 65 years, mean age), frailty, complex cardiac, respiratory or neurological co-morbidities, reduced baseline function or had declined surgical intervention.
3.4. Early surgery
Thirty-two patients (22.5%) underwent early surgery. Twenty-four patients had ≥ 5 mm of GT displacement with thirteen within the cohort having a superior comminution pattern. Eight patients had < 5 mm displacement, in which the majority were in the superior comminuted pattern (6/8, 75%). Surgery occurred in this cohort due to concerns of further fracture migration. In total, over half of these patients had a superiorly situated multi-fragmentary pattern (19/32, 59%). They were generally treated with interfragmentary screw compression (eleven cases) or tension band sutures (TBS) (five cases). Three cases were treated with double row suture anchor repair (DRSA). (Table 3).
Table 3.
Methods of fixation and radiological outcome for those with early surgery. Consideration by number of fragments and pattern of comminution. TBS – Tension Band Suture.
| Single fragment | Two fragments | Multi-fragmentary: Pattern of comminution |
||||
|---|---|---|---|---|---|---|
| Superior | Inferior | Widespread | ||||
| Early surgery (n = 32) | 4 | 4 | 19 | 1 | 4 | |
| TBS | 0 | 0 | 5 | 1 | 2 | |
| Interfragmentary screw | 3 | 3 | 11 | 0 | 1 | |
| Double Row Anchor | 0 | 0 | 3 | 0 | 0 | |
| Interfragmentary screw and TBS | 1 | 1 | 0 | 0 | 0 | |
| Locking Plate |
0 |
0 |
0 |
0 |
1 |
|
| Radiological outcome | ||||||
| Delayed migration (n = 16) | 3 | 2 | 10 | 0 | 1 | p = 0.6 |
Radiological outcome. Mean follow up was two months (range one to four months). Fifty percent had radiological evidence of secondary migration despite fixation. This was generally observed for the GT fragments with superiorly situated comminution (10/16, 62.5%), and all had been treated with either interfragmentary screws (seven cases) or TBS (three cases) (Fig. 3, Fig. 4 respectively). There was no secondary migration in those treated with DRSA repair (Fig. 5).
Fig. 3.
A. Superiorly situated comminution prior to inter-fragmentary screw compression (AP view of left shoulder, May 2012). B. Intra-fragmentary screw compression failure with GT fragment migration postero-superiorly (Axillary view of left shoulder, January 2013).
Fig. 4.
Two months following tension band suture fixation of superior comminution, the GT fragment has migrated postero-superiorly (AP view of left shoulder, December 2016).
Fig. 5.
A. Intra-operative DRSA repair of a superiorly situated GT comminution (AP of right shoulder, October 2016). B. At three-month follow-up, radiological union was achieved with no secondary migration (AP of right shoulder, January 2017).
3.5. Late surgery
Ten patients underwent a trial of conservative treatment before surgical intervention. Three had a GT fragment displacement of more than 5 mm (one single fragment, one double fragment and one widespread comminution). All but one of the remaining seven were superiorly situated GT fragments and were initially undisplaced. However, they underwent surgery due to progressive fracture fragment migration on follow up. Furthermore, they all underwent fixation with DRSA and there was no secondary migration on follow up at two months (range one to four months).
3.6. Conservative treatment
Of the ninety-one cases treated conservatively, sixty-five were available for follow up (71.4%) (Table 4).
Table 4.
Comparison of demographics and fracture pattern in those treated conservatively and its effect on GT migration. MF – multi-fragmentary.
| No migration (n = 32) | Secondary migration (n = 33) | Significance | |
|---|---|---|---|
| Age | 50 (37–63) | 73 (72–80) | <0.00001 |
| Gender | 13 | 19 | 0.22 |
|
Displaced 5 mm+ (n (%)) |
4 | 11 | 0.08 |
| Single fragment | 4 | 0 | – |
| Two fragments | 2 | 0 | – |
| Multi-fragmentary | 26 | 33 | 0.01 |
| MF: Superior | 15 | 23 | 0.08 |
| MF: Inferior | 0 | 0 | – |
| MF: Widespread | 11 | 10 | 1 |
| Median follow up (months) | 1.5 (1–3.5) | 1.75 (0.75–5) | 0.86 |
Radiological outcomes for secondary GT fragment migration were assessed (Table 4).
Fracture fragment migration were more common in the elderly population (73 vs. 50 years, p < 0.001) and those with a multi-fragmentary pattern regardless of type (p = 0.01). Reasons for non-operative treatment despite fracture migration included increasing age, frailty, complex cardiac, respiratory or neurological co-morbidities, reduced baseline function or had declined surgical intervention.
4. Discussion
Greater tuberosity fractures associated with traumatic anterior GH dislocation have been shown to result in stiffness, functional disability and high rates of malunion/displacement.15,26 Although isolated GT fracture morphology are well described to ascertain optimal treatment algorithms,18,20 there is a paucity in the literature in its characteristics when associated with anterior GH dislocation. As a result, we carried out the largest study to date exploring such fracture-dislocation morphology and characteristics in hopes to ultimately optimize their management.
Many GT fragment fracture-dislocations in this cohort were multi-fragmentary (86.5%), occurred in the elderly (≥65 years), and were located antero- or postero-superiorly (68.7%).
The reasons could include greater degree of osteoporosis,29 predominant involvement of the supra and infraspinatus facet along with its related rotator cuff (RC),30 and the glenoid impaction on the posterior GT during anterior dislocation.31 The latter subsequently causes a spasmic contraction of the RC, pulling it superiorly.15,32 Although we found such pathology occurring more often in the elderly, the population cohort followed a bimodal distribution (range, 18–90 years), and thus was in support of previous studies.33
The impaction during dislocation is likely to create a greater mismatch between the GT fragment size and fracture bed for both the single and superiorly situated GT comminuted fragment compared to the other fragment characteristics with a larger surface area (two and widespread comminuted fragments).25 Consequently, this results in both a reduced bony contact and intrinsic instability of the fracture fragments. This may explain why single and superiorly situated GT fragments displaced more often compared to the others (Table 2), and why they were offered surgery, particularly in the early phase (Table 3). However, age may have also influenced surgery, underlined by the fact that over half of the two-fragment pattern cohort group (5/9, 55.6%) were surgically treated despite only one patient having ≥ 5 mm displacement (Table 2).
Table 2.
Demographics, displacement and outcome of GT fractures with anterior GH dislocations. Consideration by pattern of comminution (superior, inferior and widespread). All p-values shown are the results of analysis for all three groups using Chi-Square or ANOVA tests where appropriate. Significant relationships (p < 0.05) are in bold. * - Inferior pattern was excluded from analysis due to insufficient sample size.
| Single (1) fragment | Two (2) fragments | Multi-fragmentary: Comminution Pattern |
Significance |
||||
|---|---|---|---|---|---|---|---|
| Superior | Inferior* | Widespread | All fragments | Multi-fragmentary | |||
| Number of cases (%) | 9 (6.8) | 9 (6.8) | 79 (59.4) | 2 (1.5) | 34 (25.6) | ||
| Age (IQR) in years | 35 (32–38) | 58 (56–64) | 63 (19–90) | 59 (49–68) | 72 (25–96) | p = 0.00015 | p = 0.07 |
| Gender – Male (%) | 8 M (89) | 5 M (56) | 36 M (46) | 1 M (50) | 16 M (47) | p = 0.10 | p = 1.0 |
| Side – Right (%) | 4 R (44) | 3 R (33) | 37 R (47) | 1 R (50) | 15 R (44) | p = 0.89 | p = 0.84 |
| Displaced 5 mm+ (n (%)) | 5 (56) | 1 (11) | 34 (43) | 1 (50) | 7 (21) | p = 0.03 | p = 0.03 |
| Surgical Treatment | 5 (56) | 5 (56) | 25 (32) | 1 (50) | 6 (18) | p = 0.054 | p = 0.17 |
Interestingly, we found the majority of cases requiring late surgery were the superior comminution pattern as all had undergone secondary migration. Furthermore, from our conservatively treated cohort, secondary migration was more likely with GT fragment comminution (p = 0.01, Table 4) and despite statistical insignificance this was again with the superior fragment patterns (p = 0.08, Table 4). Such findings have been supported in earlier studies with or without anterior GH dislocations,16,25,26 with the likelihood of progressive scarring of the supra and infraspinatus causing chronic GT retraction, with those comminuted superiorly predominantly affected. The statistical insignificance may have been confounded by those without migration to be of a younger age and thus strictly more compliant to rehabilitation than the secondary migration group who were much older (50 vs 73 years, p < 0.00001).
Nevertheless, such patterns identified has played a role in influencing our practice in the later years. This is particularly the case in fixing superiorly comminuted fragments much earlier than expected, underlined by the majority of those undergoing early surgery despite < 5 mm displacement coming from this cohort (6/8, 75%). Previous studies have reported that it is not known to what extent displacement of comminuted fragment warrant surgical intervention.32 However, in view of our findings, we suggest the fracture morphology in the fracture-dislocation cohort should play an equally important role in determining surgical fixation. Whilst we suspect this needs further clarification in clinical and biomechanical studies, we suggest close follow-up with serial radiographs for the first several weeks in patients with minimally displaced comminuted fractures (<5 mm) that are managed conservatively.
In the early period, many of our GT fragment fracture comminutions were treated with either tension band wiring or interfragmentary screw compression as previously described.31 In most cases there was secondary migration on follow-up (Fig. 1, Fig. 2). We suspect such failure was due to the poor rotational stability and cut through propensity in osteoporotic bone by the Tenson band sutures. Regarding the inter-fragmentary screw use in isolation, it increases the likelihood of GT fragmentation with subsequent fracture displacement and RC deficiency. This may also underline the reasons for failure.
Instead, over the last few years we have now treated all our superiorly situated GT comminutions similarly to full-thickness rotator cuff tears. A DRSA was performed in all cases (3, early surgery and 6, late surgery) to ensure secure fixation through the RC tendon to prevent escape of the fracture fragments. All united with no evidence of secondary migration at two months. Despite these favourable results and support from earlier studies,18,31 future studies with larger sample sizes, patient reported outcomes, and longer follow-up are required.
There are several limitations in this study. First, this is a retrospective review with prospective data collection. Although we attempted to ensure uniform data collection, inherent variability was likely. Secondly, in the early period, each surgeon dictated treatment in case-by-case fashion. Only in the last few years were protocols set up to guide initial management and treatment. Furthermore, we acknowledge that the high multi-fragmentary pattern in our study may be reflected by the large elderly population (mean age 65). However, we have studied a large sample size with support from previous studies of such pathology occurring in this age cohort.33 More interestingly however is the bulk of our population being in their early 50s (IQR: 53–77), suggesting no age category is without risk.
The study gives important insight on the behaviour of these fractures. Although the largest study on GT fracture-dislocation morphology to date with an incidence (7.2%) lower than that reported in previous studies (10–30%),3,21,34, 35, 36 the small surgical intervention sizes in the single, two and widespread fragments meant little to no substantive conclusions can be made for pattern of fixation failure. Although clinical outcomes were not reported, particular GT fracture morphology and its pathological sequelae identified in these fracture-dislocations are likely to have negative implications in function based on its alteration in the rotator cuff biomechanics.10,11,37
5. Conclusion
GT fractures with anterior GH dislocations are frequently comminuted. Those with superiorly situated comminution tend to displace ≥ 5 mm and if undisplaced may undergo secondary migration after a period of conservative treatment. Furthermore, when fixed with screws of tension band sutures they can potentially suffer secondary migration due to further comminution. Future studies with longer follow ups should be undertaken however to explore this further.
Ethical review committee statement
Our institutional review board approved of this study.
Funding/scholarship
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Contributorship
K. Boksh: Collection of Data, Data Analysis and Interpretation, Writing of Manuscript, final approval of manuscript, A. Srinivasan: Collection of Data, Data Analysis and Interpretation, G. Perianayagam: Conception, Design, Final Approval of Manuscript, H. Singh: Writing of Manuscript, Final Approval of Manuscript, A. Modi: Conception, Design, Final Approval of Manuscript.
Conflict of interest
None of the authors have any conflicts of interest to disclose.
Funding
Nil.
Ethical approval
N/A.
Data sharing statement
All relevant data are included in the article.
Declaration of competing interest
None.
Acknowledgement
None.
Contributor Information
Khalis Boksh, Email: khalis_boksh@hotmail.co.uk.
Ananth Srinivasan, Email: ananthsrinivasan92@gmail.com.
Ganapathy Perianayagam, Email: ganaps77@doctors.org.uk.
Harvinder Singh, Email: hps9@leicester.ac.uk.
Amit Modi, Email: amit.modi@uhl-tr.nhs.uk.
References
- 1.Gruson K.I., Ruchelsman D.E., Tejwani N.C. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39:284–298. doi: 10.1016/j.injury.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 2.Williams G.R., Jr., Wong K.L. Two-part and three-part fractures: open reduction and internal fixation versus closed reduction and percutaneous pinning. Orthop Clin N Am. 2000;31(1):1–21. doi: 10.1016/s0030-5898(05)70124-3. [DOI] [PubMed] [Google Scholar]
- 3.George M.S. Fractures of the greater tuberosity of the humerus. J Am Acad Orthop Surg. 2007;15(10):607–613. doi: 10.5435/00124635-200710000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Park T.S., Choi I.Y., Kim Y.H., et al. A new suggestion for the treatment of minimally displaced fractures of the greater tuberosity of the proximal humerus. Bull Hosp Jt Dis. 1997;56:171–176. [PubMed] [Google Scholar]
- 5.Kim S.H., Ha K.I. Arthroscopic treatment of symptomatic shoulders with minimally displaced greater tuberosity fracture. Arthroscopy. 2000;16:695–700. doi: 10.1053/jars.2000.9237. [DOI] [PubMed] [Google Scholar]
- 6.Platzer P., Thalhammer F., Oberleitner G., et al. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma. 2008;65:843–848. doi: 10.1097/01.ta.0000233710.42698.3f. [DOI] [PubMed] [Google Scholar]
- 7.Iannotti J., Sidor M. Complex and Revision Problems in Shoulder Surgery. Lippincott-Raven; Philadelphia: 1997. Malunions of the proximal humerus; pp. 245–264. [Google Scholar]
- 8.Craig E. In: Master Techniques in Orthopaedic Surgery: The Shoulder. Craig E., editor. Raven, Press; New York: 1995. Open reduction and internal fixation of greater tuberosity fractures, malunions and nonunions; pp. 289–307. [Google Scholar]
- 9.DePalma A., Cautill R. Fractures of the upper end of the humerus. Clin Orthop. 1961;20:73–93. [PubMed] [Google Scholar]
- 10.Stevens J. The action of the short rotator on the normal abduction of the arm, with a consideration of their action in some cases of subacromial bursitis and allied conditions. Am J Med Sci. 1909;138:870–884. [Google Scholar]
- 11.Bono C.M., Renard R., Levine R.G., et al. Effect of displacement of fractures of the greater tuberosity on the mechanics of the shoulder. J Bone Joint Surg [Br] 2001;83-B:1056–1062. doi: 10.1302/0301-620x.83b7.10516. [DOI] [PubMed] [Google Scholar]
- 12.Neer C.S. Displaced proximal humeral fractures. I Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 13.Neer C.S. Displaced proximal humeral fractures. II Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52(6):1090–1103. [PubMed] [Google Scholar]
- 14.Conner P., Flatow E. In: Instructional Course Lectures. Springfield D., editor. American Academy of Orthopaedic Surgeons; Rosemont: 1997. Complications of internal fixation of proximal humeral fractures; pp. 25–37. [PubMed] [Google Scholar]
- 15.Green A., Izzi J., Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003;12:641–649. doi: 10.1016/s1058-2746(02)86811-2. [DOI] [PubMed] [Google Scholar]
- 16.Platzer P., Kutscha-Lissberg F., Lehr S., et al. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Injury. 2005;36:1185–1189. doi: 10.1016/j.injury.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 17.DeBottis D., Anavian J., Green A. Surgical management of isolated greater tuberosity fractures of the proximal humerus. Orthop Clin N Am. 2014;45(2):207–218. doi: 10.1016/j.ocl.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Mutch J., Laflamme G.Y., Hagemeister N., et al. A new morphologic classification for greater tuberosity fractures of the proximal humerus: validation and clinical implications. Bone Joint Lett J. 2014;96-B(5):646–651. doi: 10.1302/0301-620X.96B5.32362. [DOI] [PubMed] [Google Scholar]
- 19.Jakob R.P., Ganz R. Proximal humerus fractures. Helv Chir Acta. 1982;48:595–610. [PubMed] [Google Scholar]
- 20.Rouleau D.M., Laflamme G.Y., Mutch J. Fractures of the greater tuberosity of the humerus: a study of associated rotator cuff injury and atrophy. Shoulder Elbow. 2016;8(4):242–249. doi: 10.1177/1758573216647896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robinson C.M., Shur N., Sharpe T., et al. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am. 2012;94(1):18–26. doi: 10.2106/JBJS.J.01795. [DOI] [PubMed] [Google Scholar]
- 22.Atoun E., Narvani A., Even T., et al. Management of first-time dislocations of the shoulder in patients older than 40 years: the prevalence of iatrogenic fracture. J Orthop Trauma. 2013;27:190–193. doi: 10.1097/BOT.0b013e31826576f8. [DOI] [PubMed] [Google Scholar]
- 23.Harding T.M., Dolan R., Hannah S., et al. Isolated greater tuberosity fracture stability and association with dislocation. J Bone Joint Surg Br. 2018;95-B Sup. 31. [Google Scholar]
- 24.Bahrs C., Lingenfelter E., Fischer F., et al. Mechanism of injury and morphology of the greater tuberosity fracture. J Shoulder Elbow Surg. 2006;15:140–147. doi: 10.1016/j.jse.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Hebert-Davies J., Mutch J., Rouleau D., et al. Delayed migration of greater tuberosity fractures associated with anterior shoulder dislocation. J Orthop Trauma. 2015;29(10):396–400. doi: 10.1097/BOT.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 26.Dimakopoulos P., Panagopoulos A., Kasimatis G., et al. Anterior traumatic shoulder dislocation associated with displaced greater tuberosity fracture: the necessity of operative treatment. J Orthop Trauma. 2007;21:104–112. doi: 10.1097/BOT.0b013e3180316cda. [DOI] [PubMed] [Google Scholar]
- 27.Johnson A. How fractures are described: by the number of fracture fragments. Essential Radiology Review. 2019:409–412. [Google Scholar]
- 28.Das A., Rollins K.E., Elliott K., et al. Early versus delayed operative intervention in displaced clavicle fractures. J Orthop Trauma. 2014;28:119–123. doi: 10.1097/BOT.0b013e3182a2968e. [DOI] [PubMed] [Google Scholar]
- 29.Clavert P., Bouchaib J., Sommaire C., et al. Does bone density of the greater tuberosity change in patients over 70? Orthop Traumatol Surg Res. 2014;100(1):109–111. doi: 10.1016/j.otsr.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Ogawa K., Yoshida A., Ikegami H. Isolated fractures of the greater tuberosity of the humerus: solutions to recognizing a frequently overlooked fracture. J Trauma. 2003;54(4):713–717. doi: 10.1097/01.TA.0000057230.30979.49. [DOI] [PubMed] [Google Scholar]
- 31.Rouleau D.M., Mutch J., Laflamme G.-Y. Surgical treatment of displaced greater tuberosity fractures of the humerus. J Am Acad Orthop Surg. 2016;24(1):46–56. doi: 10.5435/JAAOS-D-14-00289. [DOI] [PubMed] [Google Scholar]
- 32.Resch H., Thöni H. Dislocation fractures of the shoulder: special status and therapeutic concepts. Orthopä. 1992;21(2):131–139. [PubMed] [Google Scholar]
- 33.Rees J.L., Shah A., Edwards K. Treatment of first-time traumatic anterior shoulder dislocation: the UK TASH-D cohort study. Health Technol Assess. 2019;23(18) doi: 10.3310/hta23180. 1-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hovelius L. Anterior dislocation of the shoulder in teen-agers and young adults. Five-year prognosis. J Bone Joint Surg Am. 1987;69:393–399. [PubMed] [Google Scholar]
- 35.Rowe C.R. Prognosis in dislocation of the shoulder. J Bone Joint Surg Am. 1956;38:957–977. [PubMed] [Google Scholar]
- 36.Runkel M., Kreitner K.F., Wenda K., et al. Nuclear magnetic tomography in shoulder dislocation. Unfallchirurg. 1993;96:124–128. [PubMed] [Google Scholar]
- 37.Matti Z., Unnithan A., Hong T. Isolated greater tuberosity fractures: comparison of outcomes. J Bone Joint Surg Br. 2012;94-B:9. [Google Scholar]