Abstract
Background and Objectives
The transition from home to a nursing home is a stressful event for both older persons and informal caregivers. Currently, this transition process is often fragmented, which can create a vicious cycle of health care-related events. Knowledge of existing care interventions can prevent or break this cycle. This project aims to summarize existing interventions for improving transitional care, identifying their effectiveness and key components.
Research Design and Methods
A scoping review was performed within the European TRANS-SENIOR consortium. The databases PubMed, EMBASE (Excerpta Medica Database), PsycINFO, Medline, and CINAHL (Cumulated Index to Nursing and Allied Health Literature) were searched. Studies were included if they described interventions designed to improve the transition from home to a nursing home.
Results
17 studies were identified, describing 13 interventions. The majority of these interventions focused on nursing home adjustment with 1 study including the entire transition pathway. The study identified 8 multicomponent and 5 single-component interventions. From the multicomponent interventions, 7 main components were identified: education, relationships/communication, improving emotional well-being, personalized care, continuity of care, support provision, and ad hoc counseling. The study outcomes were heterogeneous, making them difficult to compare. The study outcomes varied, with studies often reporting nonsignificant changes for the main outcome measures.
Discussion and Implications
There is a mismatch between the theory on optimal transitional care and current transitional care interventions, as they often lack a comprehensive approach. This research is the first step toward a uniform definition of optimal transitional care and a tool to improve/develop (future) transitional care initiatives on the pathway from home to a nursing home.
Keywords: Innovations, Long-term care, Transitional care
A transition can be defined as “the move between different healthcare settings or between different levels of care within the same setting” (Coleman, 2003). A common transition experienced by older persons and informal caregivers is the transition from home to a nursing home. Generally, this transition pathway can be defined as having three transition phases: the pre-, mid-, and posttransition phases. Despite the differences in delineation in the existing definitions of each transition phase, a suitable definition is provided for all phases. The pretransition phase begins when a nursing home admission is first discussed and it ends when a nursing home is chosen (Afram et al., 2015; Lord et al., 2015; Sussman & Dupuis, 2012, 2014). In the midtransition phase, the older person prepares for the move while on a nursing home waiting list. It ends when the physical move has taken place (Hainstock et al., 2017; Sussman & Dupuis, 2012, 2014). Finally, the posttransition phase commences the day after placement and focuses on the adjustment to, and acceptance of, the new living situation (Afram et al., 2015; Hainstock et al., 2017; Sussman & Dupuis, 2012, 2014). The transition from home to a nursing home can be experienced as a stressful and emotionally challenging event for both older persons and informal caregivers (Eika et al., 2014; Ellis, 2010; Melrose, 2004).
For older persons, this care transition often entails a sudden change in identity associated with changes in autonomy, daily routine, social status, and contacts (Križaj et al., 2016; Riedl et al., 2013; Wada et al., 2020). Informal caregivers can be confronted with feelings of grief and loneliness when relinquishing care to the nursing home (Graneheim et al., 2014; Paun et al., 2015). These negative experiences can be intensified when transitional care is poorly coordinated and therefore fragmented (Boling, 2009; Wagner et al., 2011). Poor transitional care can lead to adverse outcomes for both the older person (e.g., mortality, medication-associated events, delirium, and falling incidents) and their informal caregivers (e.g., feelings of guilt, sadness, and failure; Cheek & Ballantyne, 2001; Coleman, 2003; Coleman & Boult, 2003; Graneheim et al., 2014; Nolan & Dellasega, 2000; Schön et al., 2016). Furthermore, it leads to an increased cost for the health care setting due to the duplication of services, which is associated with work overload and burnout in health care professionals (Greenglass et al., 2001; Mansukhani et al., 2015; Nantsupawat et al., 2016; National Transitions of Care Coalition, 2008; Pauly et al., 2018).
To avoid these negative outcomes, transitional care can be improved by developing comprehensive, multicomponent transitional care interventions (World Health Organization [WHO], 2016). These interventions can focus on the different challenges throughout all transition phases. More specifically, in the pretransition phase, challenges include, but are not limited to, a first-time transitional care discussion or choosing an appropriate nursing home. In the midtransition, this can entail the transfer of medical information to the nursing home and organizing a warm welcome. Posttransition interventions can focus on making the resident and informal caregiver feel at home. Moreover, these interventions ideally provide a continuous pathway throughout the three phases of transitional care (Coleman, 2003; Groenvynck et al., 2020). Preferably, the interventions are tailored to the needs of older persons, informal caregivers, and health care professionals, also referred to as the “triad of care” (Afram et al., 2015; Coleman & Boult, 2003; WHO, 2016). A recent literature review by Groenvynck et al. (2020) led to the development of the TRANSCIT model. The model identified the need for communication, information, support, time, and a partnership with health care professionals throughout the whole transition process. This extensive list of identified needs highlights the importance of integrating multiple intervention components throughout the transition from home to a nursing home. A multicomponent intervention is, moreover, encouraged by the WHO when aiming to improve transitional care (WHO, 2016).
Given this knowledge, the literature on the care pathway from home to a nursing home is relatively scarce as most transitional care research focuses on the transition from and to a hospital (Rojas Smith et al., 2014). As far as we are aware, only one systematic review has focused on interventions in the transition from home to a nursing home. However, this review focused on comparing the effectiveness of existing transitional care interventions. Moreover, the systematic review only included interventions offering support (Müller et al., 2017). Currently, a comprehensive overview of existing interventions and their intervention components is missing. Additionally, it is unclear how these interventions can contribute to the defragmentation of care while taking the care triad of older persons, informal caregivers, and health care professionals into account. Therefore, this scoping review aims to summarize the existing interventions designed to improve the transition from home to a nursing home by identifying their key components and intervention effectiveness.
Method
A scoping review was conducted following the steps of Arksey and O’Malley (2005) and adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR; Arksey & O’Malley, 2005; Tricco et al., 2018). This review type was chosen to identify the intervention components, the scope, and gaps in the literature regarding care transitions (Heyn et al., 2019). The PRISMA checklist for scoping reviews was used (Supplementary Table 1; Tricco et al., 2018). The five steps described by Arksey and O’Malley (2005) were followed. These steps were followed as they provide a framework for systematically conducting this scoping review to enhance reliability and replicability (Arksey & O’Malley, 2005).
Data Sources and Search Strategy
Stage 1: Identifying the research question
Based on the identified gap in the literature, a research question was formulated: “Which interventions, aiming at the improvement of transitions from home to a nursing home, are described in the peer-reviewed literature?” This research question was used to build the search string for which four key terms were identified: “older persons,” “transitional care,” “home care,” and “nursing home.” For each of the key terms, synonyms and related terms were searched. A librarian reviewed and finalized the search string for every electronic database employed. The search string for PubMed can be found in Supplementary Table 2.
Stage 2: Identifying relevant studies
Five electronic databases were searched for potential studies: PubMed, Medline, PsycINFO, CINAHL (Cumulated Index to Nursing and Allied Health Literature), and EMBASE (Excerpta Medica Database). The final search was performed on May 11, 2020. Additionally, relevant studies were identified using the reference lists of the included studies and the reference lists of reviews relevant to the research question.
Study Selection
Stage 3: Study selection
The studies were included if they were published in Dutch or English and published between January 2000 and May 11, 2020. There were no restrictions regarding the study design. Studies were included if (a) they described an intervention aiming to improve transitional care; (b) the target populations, meaning the person(s) for whom the intervention was developed, were older persons (65 and older), informal caregivers, and/or health care professionals (in)directly involved in the transition process; and (c) the study focused on the transition from home to permanently residing in a nursing home. In this article, the term nursing home is used to define a long-term care facility where room and board and 24-h assistance are provided to older persons who have complex care needs due to physical and cognitive impairment (Sanford et al., 2015). Studies were also included when the older person had a short hospital stay before a first-time nursing home admission. Moreover, studies focusing on a first-time nursing home admission, with the origin of the move not specifically stated, were also included. Studies were excluded if they did not describe an intervention or if the transition pathway or future care facility was not clearly defined.
The search results were uploaded to EndNote from which the screening process commenced. The first author screened the titles and subsequently the abstracts of the identified studies. A fellow researcher independently screened 10% of the studies. For both screenings, the first author made an easy-to-follow chart containing the inclusion and exclusion criteria of each screening phase. If the researchers did not reach a consensus of 90%, the second researcher screened an additional 10% of the records. Both authors screened the full-text articles. Disagreements were resolved by reevaluating the inclusion and exclusion criteria with the second screener and via discussions with the entire research team.
Data Extraction and Analysis
Stage 4: Charting the data
A data-charting form was made, using the MS Office program Excel, to extract data from the included studies. The data-charting form included the aim of the intervention, the target population, and a description of the intervention characteristics. The interventions were described per component and linked to one of the transition phases (pre-, mid-, or posttransition; Groenvynck et al., 2020). Furthermore, study characteristics such as the goal, study design, participants’ characteristics, and data collection methods were also charted.
Stage 5: Collating, summarizing, and reporting the results
Data analysis was performed for the study characteristics, intervention components, and effectiveness of the intervention. First, the study characteristics were analyzed descriptively. Second, a thematic analysis was performed, identifying the different intervention components used to improve the transition from home to a nursing home. Third, the included interventions were compared to the earlier described TRANSCIT model. More specifically, all interventions were categorized according to the three transition phases (the pretransition, midtransition, and posttransition phases) and compared the overall key components: partnership, communication, information, support, and time (Groenvynck et al., 2020). Finally, a summary was conceived, describing the process and outcome evaluations of the included studies.
Results
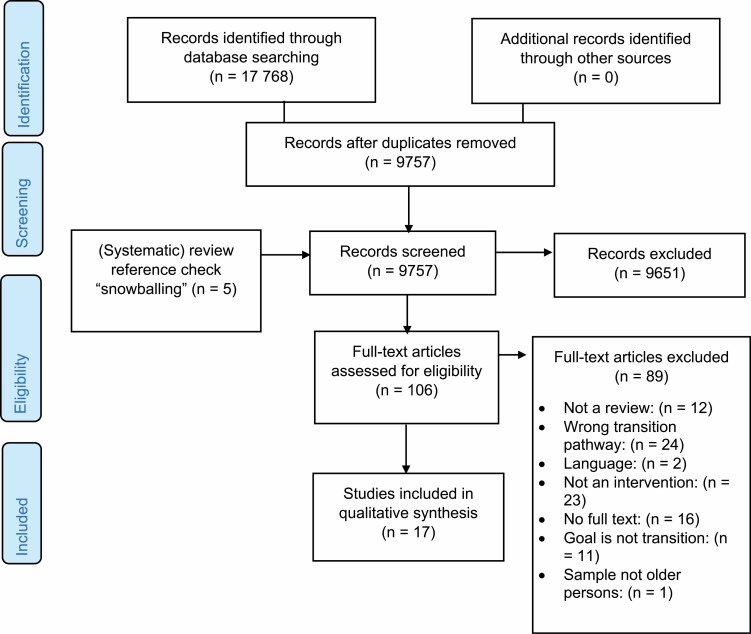
The database search identified 9,757 studies after duplicates had been removed (see flowchart, Figure 1). Following the screening of titles and abstracts, 106 studies qualified for full-text screening. A total of 12 out of these 106 were included in the scoping review. The snowball method led to the inclusion of an additional five studies. Finally, a total of 17 studies were considered relevant to the research question. The 17 studies described 13 distinct interventions.
Figure 1.
PRISMA flowchart: data selection process. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study Characteristics
An overview of the study characteristics is given in Table 1. The studies were conducted in the United States (n = 11), Australia (n = 2), the Netherlands (n = 2), and the United Kingdom (n = 2). The study designs used by the researchers were randomized control trials (n = 6; Crotty et al., 2004; Davis et al., 2011; Gaugler et al., 2008, 2011; Mukamel et al., 2016; Schulz et al., 2014), quasi-experimental study designs (n = 2; Paun & Farran, 2011; Paun et al., 2015), mixed-method studies (n = 3; Gaugler et al., 2015; Saint-Bryant et al., 2020), observational studies (n = 3; Lichtenberg, 2007; Meiland et al., 2002; Ward et al., 2008), two study protocols (n = 2; Davison et al., 2020; Gaugler et al., 2020), and a qualitative explorative study (n = 1; Van Mierlo et al., 2015).
Table 1.
Characteristics of the Studies
| Study; country | Goal of study | Design | Sample and agea | Measures | Outcomes |
|---|---|---|---|---|---|
| Crotty et al., 2004; Australia | To investigate whether the quality of first-time transfer of older persons from a hospital to an NH would be improved by having a pharmacist coordinate the transition | Randomized controlled trial | Older person (n = 110); age: 82 mean (6.4 SD) | Older persons’ medication charts; case note | Intervention outcomes: (a) the quality of prescribing; (b) hospital usage, falls, worsening mobility, increased confusion, worsening behaviors, and pain; and (c) adverse drug events and some medication-related problems at admission |
| Davis et al., 2011; United States of America | FITT-NH—intervention: To report on the preliminary findings of the intervention for informal caregivers who had recently placed a family member with dementia into an NH for long-term care | Randomized control trial | Informal caregivers (n = 53); age: 57.25 mean (10.67 SD) | Face-to-face assessments, self-report measures; audiotape intervention sessions; assessment telephone calls | Intervention outcomes: (a) informal caregiver guilt, depression, burden; (b) hassles with staff; (c) satisfaction with the NH; and (d) return to daily activities |
| Intervention outcomes: (a) satisfaction with the program and (b) adherence to the intervention | |||||
| Davison et al., 2020; Australia | PEARL—intervention: To address the high rates of depression in NH by using an individually tailored care approach addressing the psychological needs of newly admitted older persons | Study protocol | Not applicable | Audiotaped sessions; interviews | Intervention outcomes: depressive disorder/symptoms |
| Secondary outcomes: (a) treatment fidelity, (b) stress, (c) anxiety, (d) quality of life, (e) adjustment to an NH, (f) functional dependency, (g) meaningful activity in residential care, and (h) resident perception of NH allocation | |||||
| Gaugler et al., 2008; United States of America | NYUCI—intervention: To determine whether the availability of long-term counseling and support reduces the burden and depressive symptoms throughout the transition | Randomized controlled trial | Informal caregiver (n = 385); age: 71.55 mean (8.71 SD) for the intervention group | Interviews, intervention records, and ad hoc telephone contact records | Intervention outcomes: (a) informal caregiver burden and (b) informal caregivers’ mood and psychological well-being |
| Gaugler et al., 2011; United States of America | NYUCI—intervention: To estimate the effects of comprehensive psychosocial support intervention and NH admission for a person with Alzheimer’s disease on husband and wife caregivers’ well-being | Randomized controlled trial | Informal caregivers (n = 406); age: 71.6 mean (8.7 SD) for the intervention group; 71.0 mean (9.5 SD) for the control group | Interviews, intervention records, and ad hoc telephone contact records | Intervention outcomes: (a) informal caregiver burden and (b) informal caregivers’ mood and psychological well-being |
| Gaugler et al., 2015; United States of America | RCTM—intervention: Whether and how a psychosocial family intervention reduced negative experiences associated with the admittance of cognitively impaired older persons in an NH | Mixed-method study | Informal caregivers (n = 36); age: 62.9 mean (10.9 SD) for the intervention group; 62.5 mean (14.4 SD) for the control group | Interviews, checklist and counselor notes, and focus groups | Intervention outcomes: (a) the transition placement and how the intervention helped informal caregivers and enhanced engagement with older persons or NH staff, (b) dementia severity, (c) stress, (d) depressive symptoms, and (e) informal caregiver adaptation to placement |
| Gaugler et al., 2020; United States of America | RCTM—intervention: To describe the protocol the intervention will employ to determine whether and how the intervention can help families better navigate NH transitions of cognitively impaired older persons | Study protocol | Not applicable | Surveys, contact log, counselor notes, intervention review checklist, semistructured interviews | Intervention outcomes: (a) the older persons ADL and IADL, (b) socioemotional support and informal caregiver self-efficacy/competence, (c) primary subjective stress during NH placement, (d) NH stress, and (e) informal caregivers’ depressive symptoms |
| Hayward et al., 2018; United Kingdom | To develop and validate the feasibility and intervention focused on promoting healthy adjustment in the initial stage of residency, for older persons with dementia following placement into an NH | Mixed-method study | Older persons (n = 13); age: 87.9 mean (7.2 SD) | Copies of the workbook, recorded field reports, semistructured interviews | Process outcomes: (a) delivery of the intervention, (b) feasibility and barriers of implementation when implementation took place, (c) feasibility and barriers when implementation did not take place, (d) staff benefits yet resident outcome reports were contradictory, and (e) improvements to SettleIN, and (f) validation of qualitative results |
| Lichtenberg, 2007; United States of America | Mentoring model: To test an intervention that aims to assist family caregivers who were beginning the transition to having their loved one in an NH | Longitudinal observational study | Informal caregivers (n = 20); age: 60.1 mean (13.4 SD) | Assessment tools, mentor logs | Process outcomes: satisfaction with the mentor |
| Meiland et al., 2002; The Netherlands | Urgency coding intervention: To study an intervention’s fair selection of older persons waiting for admission to a psychogeriatric NH | Longitudinal observational study | Dyad (n = 93); age: 83.2 mean (range 51–96) for older person with dementia; 57.3 mean (range 24–89) for informal caregivers | Structured questionnaire in the face-to-face interview, self-reported questionnaires, interview, older persons’ files | Intervention outcomes: (a) the dynamics in the urgency code, (b) reasons for a higher urgency coding, (c) urgency codes related to waiting time, (d) urgency codes concerning the preference for a particular NH, and (e) transfer to the preferred NH |
| Process outcomes: perceived waiting time | |||||
| Mukamel et al., 2016; United States of America | To test whether the use of a personalized report card embedded in a reengineered discharge process can lead to better outcomes in the transition from hospital to an NH | Randomized controlled trial | Older persons (n = 225); age: 75.6 mean (10.5 SD) for the control group; 74.9 mean (9.9 SD) for the intervention group | Log information of data entered in the iPad, survey, medical records | Intervention outcomes: (a) iPad use, (b) confidence and satisfaction with the decision, (c) hospital ranking and distance, and (d) length of hospital stay |
| Process outcomes: (a) usability of the NHCPlus app, (b) confidence with the NH decision, and (c) satisfaction with the decision | |||||
| Paun & Farran, 2011; United States of America | CGMI—intervention: To present a study description focusing on the development and implementation of the intervention | Quasi-experimental design | Informal caregivers (n = 34); age: 60.7 mean (10.65 SD) | A questionnaire | Process outcomes: (a) feasibility of the intervention, (b) experience with the intervention, and (c) satisfaction with the intervention |
| Paun et al., 2015; United States of America | CGMI—intervention: To determine the feasibility and the preliminary effects of the intervention on informal caregivers’ outcomes | Quasi-experimental design | Informal caregivers (n = 83); age: 60.7 mean (10.65 SD) | Population survey, three direct questions | Intervention outcomes: (a) informal caregivers’ conflict management skills, (b) exacerbators of grief in an NH environment, and (c) informal caregiver knowledge, chronic grief, depression |
| Process outcomes: (a) feasibility and (b) satisfaction with the program | |||||
| Saint-Bryant et al., 2020; United Kingdom | To examine the feasibility and effectiveness of the enhanced version of the SettleIN intervention | Mixed-method study | Older persons (n = 19); age: 87.9 mean (7.20 SD) | Residents’ care plan at the NH, semistructured interviews | Intervention outcomes: (a) current adjustment support, (b) residents’ psychological well-being, (c) residents’ quality of life, and (d) residents’ overall adjustment |
| Implementation outcomes: (a) recruitment and retention, (b) implementation, (c) program factors acting as barriers, (d) individual resident factors, (e) acceptability of SettleIN, and (f) overcoming challenges | |||||
| Schulz et al., 2014; United States of America | To test the efficacy of an informal caregiver intervention for family members who recently placed their relative in an NH | Randomized control trial | Dyad (n = 217); age: 61.8 mean (10.78 SD) for informal caregiver; 82.8 mean (9.23 SD) for older persons | Assessment tools | Intervention outcomes: (a) depression, (b) anxiety, (c) caregiver burden, (d) complicated grief, (e) perceived quality of care in the NH, (f) satisfaction with the care provided, (g) problems with the NH, (h) functional status, (i) perceived quality of life of the older person, and (j) advanced care planning |
| Van Mierlo et al., 2015; The Netherlands | To conduct a process evaluation and evaluate a mental health care transfer intervention after an older person with dementia moves to an NH | Qualitative explorative study design | Older persons (n = 24) and informal caregivers (n = 20); age: 82 mean (7.5 SD) for older persons; 57.7 mean (16.5 SD) for informal caregivers | File research, structured interviews, semistructured questionnaire, clinical assessment | Intervention outcomes: (a) outcomes of barriers and facilitators of the implementation, (b) face-to-face evaluation by caregivers, and (c) evaluation of the face-to-face follow-up by an NH staff/conductor of the intervention |
| Ward et al., 2008; United States of America | To develop an intervention that expedites the delivery of medication orders during the transfer of older persons from the hospital to an NH | Observational study | Older persons (n = 20); age: 83.0 mean (9.22 SD) | NH medical records, medication administration records | Intervention outcomes: (a) implementation of the intervention protocol, (b) arrival time at the NH, (c) discrepancies in medication orders, (d) delay or omission of medication doses, and (e) severity of omitted medication |
Note: NH = nursing home; FITT-NH = Family Intervention: Telephone Tracking-Nursing Home; NYUCI = New York University Caregiver Intervention; PEARL = Program to Enhance Adjustment to Residential Living; RCTM = The Residential Care Transition Module; CGMI = Chronic Grief Management Intervention; ADL = activities of daily living; IADL = instrumental activities of daily living.
aAge in years.
The Interventions
Supplementary Tables 3 and 4 present the characteristics of the 13 interventions. None of the described interventions directly targeted or focused their intervention on the entire triad of care, meaning the older person, informal caregiver, and health care professionals. Only the study of Van Mierlo et al. (2015) directly targeted health care professionals/informal caregivers and indirectly targeted the older person. Six interventions solely targeted informal caregivers. Five interventions mainly targeted older persons, and of those, two interventions included older persons with dementia (Davison et al., 2020; Hayward et al., 2018; Saint-Bryant et al., 2020). Finally, the study of Meiland et al. (2002) targeted the health care system by developing a better waiting list system. The most common interventionists were clinicians trained to conduct the intervention (Crotty et al., 2004; Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Mukamel et al., 2016; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014; Van Mierlo et al., 2015). Three interventions were delivered by health care professionals responsible for the daily care of an older person (e.g., nursing staff and hospital physicians; Hayward et al., 2018; Meiland et al., 2002; Saint-Bryant et al., 2020; Ward et al., 2008). Finally, Lichtenberg et al. (2007) trained peer, informal caregivers at the nursing home to deliver the intervention.
The 13 interventions are divided into two groups. The first group includes multicomponent interventions. These are interventions conducted over multiple weeks/months, implementing multiple intervention elements. The second group describes single-component interventions. These interventions were shorter, denser, and focused on one specific element of the transition.
Multicomponent Interventions
Eight of the 13 interventions described a multicomponent intervention (Supplementary Table 3). The interventions were composed of multiple sessions, defined as meetings organized to exchange knowledge, educate, and/or offer support. The number of sessions varied between six and 21. Most sessions were one-on-one. However, they were often extended by inviting family and staff to participate (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Hayward et al., 2018; Lichtenberg, 2007; Saint-Bryant et al., 2020; Schulz et al., 2014). Paun et al. (2011, 2015) provided the only group-based program.
Seven intervention components were identified from these eight interventions: education, relationships/communication, improving emotional well-being, personalized care, continuity of care, support provision, and ad hoc counseling.
Education
Education entailed the provision of information and the acquisition of skills to facilitate transitional care for both older persons and informal caregivers. The education component could focus on all different challenges of transitional care, regardless of the transition phase. For instance, the education component of one intervention focused on multiple elements of the transition process (Gaugler et al., 2008, 2011), whereas the education of another intervention focused on the adaptation of the informal caregiver to the new living situation (Davis et al., 2011; Gaugler et al., 2015, 2020; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014). Hence, there was a diversity in transitional care challenges for which education was provided.
Seven of the eight interventions provided older persons and informal caregivers with the necessary education aiming to aid adjustment to the nursing home. The informative education was usually provided to informal caregivers, mainly addressing four topics: (a) dementia, (b) problem solving, (c) nursing home policy and practice, and (d) caregiving (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Hayward et al., 2018; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Saint-Bryant et al., 2020; Schulz et al., 2014). Six of the eight interventions included educating informal caregivers on dementia (Davis et al., 2011; Gaugler et al., 2008, 2011, 2015, 2020; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014). Four interventions provided education to older persons and informal caregivers on the organizational structure and procedures of a nursing home (Davison et al., 2020; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014). Finally, three interventions provided education to informal caregivers themselves on the importance of self-care. Knowledge concerning the psychological and physical effects of caregiving and the importance of “care for the caregiver” was taught (Davis et al., 2011; Lichtenberg, 2007). Additionally, information on advanced care planning (e.g., living will and power of attorney), residents’ rights, and problem reporting at the nursing home was imparted to informal caregivers (Schulz et al., 2014).
Furthermore, five of those interventions mentioned teaching problem-solving techniques and conflict resolution for informal caregivers. The study of Davison et al. (2020) also mentioned teaching problem-solving techniques and conflict resolution to older persons. More specifically, three interventions offered training to their participants on the skills required to resolve problems or address barriers to adjustment. Two interventions aided problem solving (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015).
Relationships/communication
This intervention component focused on the importance of efficient collaboration and communication between the care triad of health care professionals, informal caregivers, and older persons. More specifically, six interventions aimed to improve communication, facilitate cooperation, and mend relationships between residents, staff, or other family members to help with nursing home adjustment (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015). This was done by improving autonomy and by providing techniques and strategies to facilitate communication (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014).
Improving emotional well-being
Six interventions used different strategies to improve emotional well-being throughout the transition from home to a nursing home. The strategies used were improving the coping process, helping to adjust, facilitating role acceptance, and encouraging positivity and well-being (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014).
Three out of six interventions specifically addressed strategies to improve coping. Davis et al. (2011) and Lichtenberg et al. (2007) taught informal caregivers different coping styles, and how to handle general problems throughout transitional care. Two interventions aimed to improve adjustment to the new living situation for informal caregivers. Davis et al. (2011) targeted emotional adjustment by addressing feelings of guilt and loss while Paun et al. (2011, 2015) let informal caregivers discuss hindering and facilitating elements of the adjustment/acceptance that the older person is no longer home. Moreover, the intervention supported the relinquishment of old attachments. The same interventions also offered support in adapting to changes in the caregiver role (Davis et al., 2011; Paun & Farran, 2011; Paun et al., 2015). Finally, five interventions used strategies to improve older persons and informal caregivers well-being and offer positivity (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014). Three interventions achieved this by reinforcing positive thoughts, successes, and achievements (Davis et al., 2011; Davison et al., 2020; Paun & Farran, 2011; Paun et al., 2015). Two interventions used relaxation techniques and exercises (Gaugler et al., 2015, 2020; Schulz et al., 2014).
Personalized care
Several interventions described personalized care as a patient-centered care approach in which the preferences and needs of the target population are an integral part of the care intervention. Six of the eight interventions tailored their intervention to the needs, preferences, and life stories of both older persons and informal caregivers (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Hayward et al., 2018; Saint-Bryant et al., 2020; Schulz et al., 2014). Gaugler et al. (2008, 2011) used individualized sessions to address the unmet needs of informal caregivers. However, they failed to provide information on how they tailored their intervention. Four studies conducted some form of assessment to achieve tailored care (Davis et al., 2011; Davison et al., 2020; Hayward et al., 2018; Saint-Bryant et al., 2020; Schulz et al., 2014). Schulz et al. (2014) assessed the knowledge/skill levels of the informal caregivers’ before every session, while Hayward et al. (2018), Saint-Bryant et al. (2020), Gaugler et al. (2015, 2020), and Davis et al. (2011) assessed their participants at the beginning of the intervention. Davison et al. (2020) used a structured tool to develop a personalized plan for creating meaningful activities and increasing autonomy for the older person. Hayward et al. (2018) and Saint-Bryant et al. (2020) were the only ones who offered a completely individualized intervention for older persons based on a needs assessment at the start of the intervention.
Continuity of care
Continuity of care referred to the follow-up of a transitional care intervention. This included transferring the responsibility for a successful intervention implementation from the interventionists to care professionals in the field. This entailed informing care professionals how to continue the intervention as well as gathering the necessary information to plan future care (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Hayward et al., 2018, 2020; Mukamel et al., 2016; Saint-Bryant et al., 2020; Van Mierlo et al., 2015). After terminating the intervention, in five of the included studies, the researchers transferred the necessary knowledge and information to health care professionals responsible for further care of the older person (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Mukamel et al., 2016; Van Mierlo et al., 2015). The studies of Davison et al. (2020), Hayward et al. (2018), and Saint-Bryant et al. (2020) specifically focused on further implementation of their interventions. Davison et al. (2020) taught key staff members how to use their intervention and they selected individual actions to implement in future care. Hayward et al. (2018) and Saint-Bryant et al. (2020) summarized the older person’s perspective and used it to plan future care. Furthermore, four interventions kept written records of the intervention outcomes and goals to further optimize care (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Hayward et al., 2018; Saint-Bryant et al., 2020).
Support provision
Four interventions offered emotional and social support to improve transitional care for informal caregivers (Davis et al., 2011; Gaugler et al., 2008, 2011, 2015, 2020; Schulz et al., 2014). Emotional support was offered by Schulz et al. (2014) and Davis et al. (2011), who used psychological strategies (e.g., validation or venting) and offered a listening ear. Social support was found in three interventions. Davis et al. (2011) and Gaugler et al. (2015, 2020) encouraged participants to build a social network, providing support beyond the intervention—either as part of the intervention or within a family network. Finally, Gaugler et al. (2008, 2011) let participants join an Alzheimer’s support group as part of the intervention.
Ad hoc counseling
In the three interventions, care on demand was offered by providing ad hoc support/counseling as part of the intervention (Gaugler et al., 2008, 2011, 2015, 2020; Hayward et al., 2018; Saint-Bryant et al., 2020). The two interventions of Gaugler et al. (2008, 2011, 2015, 2020) left informal caregivers free to contact the study counselor whenever a problem or change occurred. In the interventions of Hayward et al. (2018) and Saint-Bryant et al. (2020), the lead researcher provided weekly support to health care professionals conducting the intervention.
Single-Component Interventions
The second group included five single-component interventions (Supplementary Table 4; Crotty et al., 2004; Meiland et al., 2002; Mukamel et al., 2016; Van Mierlo et al., 2015; Ward et al., 2008). Three of the interventions focused on a specific element of the pre- and/or midtransition phase. More specifically, one intervention was an urgency coding system aiming for a more efficient nursing home waiting list system (Meiland et al., 2002). As part of one intervention, health professionals at the nursing home were informed about challenging behaviors in newly admitted older persons and they supported the informal caregiver in their coping process (Van Mierlo et al., 2015). In the third intervention, an app was developed to create a personalized nursing home list based on the preferences and needs of older persons (Mukamel et al., 2016). The two remaining interventions were medication reconciliation interventions from the hospital to a nursing home, in persons who initially lived at home (Crotty et al., 2004; Ward et al., 2008).
Results Concerning the TRANSCIT Model
It was notable that only the intervention of Gaugler et al. (2008, 2011) looked at transitional care as a continuum, including all three transition phases in the intervention. However, Gaugler et al. (2008, 2011) only focused their intervention on informal caregivers. The other interventions all focused on one or two transition phases. More specifically, Mukamel et al. (2016) focused on the pretransition phase, while the interventions of Meiland et al. (2002) and Ward et al. (2008) focused on the midtransition phase. Eight interventions focused on the posttransition phase. To be precise, they developed interventions to aid the adjustment process after older persons relocated to a nursing home (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Hayward et al., 2018; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Saint-Bryant et al., 2020; Schulz et al., 2014; Van Mierlo et al., 2015). The remaining study of Crotty et al. (2004) focused on both the mid- and posttransition phases.
As the majority of studies only focused on one specific transition phase, the continued partnership between older persons, informal caregivers, and health care professionals could not be offered. The intervention of Gaugler et al. (2008, 2011), which included all the transition phases, inadvertently addressed this partnership by offering ad hoc care whenever the informal caregiver needed it. The key component information, as identified by the TRANSCIT model, was found in all but one intervention of Meiland et al. (2002) and it was delivered in different forms (e.g., psychoeducation and skill development). Moreover, the majority of interventions used communication to transfer care to other health care professionals (Crotty et al., 2004; Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Hayward et al., 2018; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Saint-Bryant et al., 2020; Ward et al., 2008). Nine interventions offered support. However, it was noticeable that support was mostly offered in interventions targeting informal caregivers (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2008, 2011, 2015, 2020; Hayward et al., 2018; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Saint-Bryant et al., 2020; Schulz et al., 2014; Van Mierlo et al., 2015). Finally, only three interventions focused on guaranteeing sufficient time (Meiland et al., 2002; Mukamel et al., 2016; Ward et al., 2008). To conclude, it was noticeable that although different key components of the TRANSCIT model were identified throughout each of the interventions, none of the interventions took into account all key components combined (communication, information, support, and time).
Process and Outcome Evaluation
The majority of studies (n = 15) reported on the process and/or effectiveness of the studied interventions. In general, the study outcomes were heterogeneous, making them difficult to compare. This was exacerbated by the broad intervention aims described in some studies. More specifically, the aims of the single-component interventions (e.g., medication reconciliation) were more strongly related to the outcomes measured (e.g., medication omittance). This can be explained by the specific focus of single-component interventions, allowing for concrete outcome measures. This focus was not present in the studies describing the multicomponent interventions, as they often had a broader aim (e.g., facilitating nursing home adjustment or skills and knowledge acquisition). More specifically, this meant that the aim of these multicomponent interventions (e.g., facilitating adjustment) could not directly be related to the outcome measured (e.g., burden). Therefore, it was difficult to compare the studies, focusing on the same goals, as they measured different outcomes.
Process outcomes such as satisfaction and feasibility were reported in 12 studies (Davis et al., 2011; Gaugler et al., 2008, 2011; Hayward et al., 2018; Lichtenberg, 2007; Meiland et al., 2002; Mukamel et al., 2016; Paun & Farran, 2011; Paun et al., 2015; Saint-Bryant et al., 2020; Van Mierlo et al., 2015; Ward et al., 2008). Studies reporting on satisfaction were positive overall. Despite the occasional suggestion for improvement, the participants were satisfied with the interventions developed (Davis et al., 2011; Hayward et al., 2018; Lichtenberg, 2007; Meiland et al., 2002; Mukamel et al., 2016; Paun & Farran, 2011; Van Mierlo et al., 2015). The studies of Van Mierlo et al. (2015) and Ward et al. (2008) looked at the fidelity of their intervention. Ward et al. (2008) had good fidelity with the intervention being followed as intended, except for the timely handover of medication orders. This is in contrast to Van Mierlo et al. (2015), whose intervention was not able to advise health care professionals on behavioral problems in admitted residents, as prescribed in the intervention protocol. The two interventions measuring feasibility indicated positive results (Hayward et al., 2018; Paun & Farran, 2011; Saint-Bryant et al., 2020).
The intervention effectiveness was measured by 13 studies, six interventions in the multicomponent group, and four interventions in the single-component group (Crotty et al., 2004; Davis et al., 2011; Gaugler et al., 2008, 2011, 2015; Hayward et al., 2018; Meiland et al., 2002; Mukamel et al., 2016; Paun & Farran, 2011; Paun et al., 2015; Saint-Bryant et al., 2020; Schulz et al., 2014; Ward et al., 2008). In the multicomponent group, most studies indicated the importance of the evaluation of psychological well-being in informal caregivers after nursing home admission. These studies were generally unable to show significant effects. More specifically, five studies investigated depression and/or depressive symptoms in the posttransition phase among informal caregivers. No significant changes were found (Davis et al., 2011; Gaugler et al., 2015; Paun & Farran, 2011; Paun et al., 2015; Schulz et al., 2014). Notably, the two studies testing the effect of the intervention, which included the entire transition pathway from home to a nursing home (pre-, mid-, and posttransition), did find a positive effect on informal caregiver depression (Gaugler et al., 2008, 2011). Other outcomes measured in the studies on the multicomponent interventions were caregiver guilt, caregiver burden, and caregiver stress. The effectiveness of these studies was mixed (Davis et al., 2011; Gaugler et al., 2008, 2011, 2015). An example of these mixed results is the caregiver burden. The intervention performed by Davis et al. (2011) did not reduce caregiver burden, while the intervention of Gaugler et al. (2011) was able to reduce burden, but only in women. Moreover, interventions indicating these positive results were not able to indicate positive results at all the time points they measured (Gaugler et al., 2008, 2011, 2015; Paun et al., 2015; Schulz et al., 2014).
All single-component interventions, except for Van Mierlo et al. (2015), reported on effectiveness. The intervention of Meiland et al. (2002) significantly reduced the waiting time for persons with a higher or the highest urgency code, when compared with the “normal” urgency group. The study of Mukamel et al. (2016) reported that older persons choose significantly better-quality nursing homes. The quality of those nursing homes was determined based on the quality report cards. Finally, Crotty et al. (2004) and Ward et al. (2008) studied a medication reconciliation intervention. Crotty et al. (2004) showed a significant reduction in the medication appropriateness index. This is in contrast to Ward et al. (2008), whose intervention did not reduce the delay or omittance of medication doses.
Discussion
This scoping review examined the existing interventions designed to improve the transition from home to a nursing home by identifying their key components and intervention effectiveness. A comprehensive intervention, including the care triad of the older person, informal caregivers, and health care professionals, taking into account all phases in the transition process, is missing. All 13 included interventions focused on either a specific phase or target population throughout the transition process. None of the interventions included the care triad (older people, family caregivers, and health care professionals), and only one intervention focused on all phases of the transition process. Eight interventions were multicomponent interventions, in which seven intervention components were identified: education, relationships/communication, improving emotional well-being, personalized care, continuity of care, support provision, and ad hoc counseling. These intervention components mostly addressed informal caregivers, thus dealing with the consequences of, and adjustments to a new life situation after the older person moved into a nursing home. The five remaining interventions were single-component interventions on a variety of topics. These were shorter, denser, and focused on one specific element of the transition. Overall, studies reported high levels of satisfaction with the interventions, although insight into the effectiveness was mixed, mainly due to the high heterogeneity of the outcome measures used.
The results of the scoping review indicated that almost all interventions from home to a nursing home focused on one phase of the transitional care process, with the majority focusing on the posttransition phase (Davis et al., 2011; Davison et al., 2020; Gaugler et al., 2015, 2020; Hayward et al., 2018; Lichtenberg, 2007; Paun & Farran, 2011; Paun et al., 2015; Saint-Bryant et al., 2020; Schulz et al., 2014). This is in contrast to recommendations in the literature expressing the importance of including the entire transition process (Afram, 2015; Davies, 2005; Groenvynck et al., 2020). Moreover, evidence suggests that the experience of the pretransition phase can significantly affect the outcomes of the posttransition phase, which indicates the importance of starting a transitional care intervention before admission (Brownie et al., 2014; Eika et al., 2014; Graneheim et al., 2014). However, the seven intervention components were derived from interventions that mostly focused on nursing home adjustment (the posttransition phase). This makes generalizing the identified intervention components as standard throughout the whole transition process difficult. Only one intervention by Gaugler et al. (2008, 2011) did comprise the entire transition process from pretransition to posttransition. The intervention showed promising outcomes on effectiveness (e.g., depressive symptoms; Gaugler et al., 2008).
The results of this scoping review showed that a comprehensive intervention that includes the care triad of the older person, informal caregivers, and health care professionals is lacking. All interventions targeted a specific target population. Most studies focused their intervention on either the older person or the informal caregiver, with only two studies focusing on the role of the health care professional or the health care system. This might be explained by the fact that older studies, aiming to improve care for informal caregivers and older persons with dementia, did not target the latter due to their cognitive status (Davis et al., 2011; Gaugler et al., 2008, 2011; Mukamel et al., 2016). Literature, however, emphasizes the importance of recognizing the older person (regardless of a dementia diagnosis), the informal caregiver, and the health care professional as an inseparable care triad throughout the transition process. More specifically, the health care professional should have the necessary skills to coordinate the care process in collaboration with the older person and the informal caregiver by integrating the perspectives of all involved (Afram, 2015; Hirschman et al., 2015; Pauly et al., 2018; Toscan et al., 2012; WHO, 2016). The importance of this care triad was also demonstrated in a recent review of needs during the transition period, as expressed by older persons and informal caregivers. Here, older persons and informal caregivers expressed the need to form a partnership with health care professionals throughout the transition process from home to a nursing home (Groenvynck et al., 2020).
Limitations
A few limitations need to be addressed. First, the search string built for this review might not have identified all transitional care interventions available from the literature due to the heterogeneity of terminology for transitional care and related interventions. The researchers consulted a librarian who specialized in building search strings. However, the researchers acknowledge that some degree of uncertainty remains about retrieving all relevant studies. Furthermore, some interventions might only be found in gray literature, which was not considered in this study. Additionally, language restrictions were imposed, including only Dutch and English language papers.
Second, data extraction and analysis were challenging for reasons of incomplete or vague intervention descriptions in some studies. Vague descriptions of interventions complicated the thematic analysis of the intervention components as it was often unclear just how the interventions were conducted. Moreover, these incomplete descriptions made us unable to identify the exact transition pathway of the study. This may have led to the exclusion of relevant studies. Finally, a quality appraisal of the included studies was not performed, as this review primarily aimed to provide an overview of existing interventions focusing on improving the transition from home to a nursing home. However, for the additional aim of considering the effects of such interventions, omitting such a quality assessment is a limitation.
Practice and/or Policy Implications
Transitional care is defined as a set of actions designed to guarantee continuity of care (Coleman, 2003). This scoping review identified a clear mismatch between optimal transitional care as defined in the literature and transitional care initiatives evaluated in scientific studies. More specifically, this review has shown that a comprehensive intervention, starting when transitional care is first considered (pretransition) and ending when the older person/informal caregiver adjusted to the new living situation (posttransition), and in which the older person, informal caregiver, and health care professionals are considered an inseparable care triad, is missing in the literature. Perhaps it might not be feasible for an intervention, concerning budget and time constriction, to include all transitional care phases. However, interventionists should appraise the previous and proceeding phases following a certain transition event (e.g., choosing a nursing home). Yet, this kind of appraisal was not found in current intervention studies. It probably indicates that transitional care is still insufficient, and often too narrowly focused, possibly leading to fragmented care (National Transitions of Care Coalition, 2010). Moreover, it suggests that health care organizations are often considered as individual entities, rather than links in a continuous chain.
Interventions aiming to create continuity and ensure coordination between care settings are highly warranted. Researchers, policymakers, (in)formal caregivers, and older persons should work together to define optimal transitional care and uniform outcome measures (Coleman, 2003; WHO, 2016). This standardization can aid in the comparison of alternative transitional care interventions, thus enabling the identification of the most effective transitional care interventions and their components. Moreover, a partnership between these policymakers, (in)formal caregivers, and older persons should be established, starting in the pretransition phase and continuing into the posttransition phase (Coleman & Boult, 2003; Groenvynck et al., 2020; Wagner et al., 2011).
This scoping review offers the first step toward the identification of common elements in designing an intervention facilitating the transition from home toward a nursing home. The seven potentially relevant intervention components could be used to develop a transitional care plan based on the needs of older people and their families (Coleman, 2003; WHO, 2016). Combining components in a multifaceted intervention is supported by the WHO, indicating the importance of combining different intervention components to optimize the transition process (WHO, 2016). As most of these intervention components were created from interventions designed for the posttransition phase, future research should focus on determining the effectiveness of these components throughout the transition process and identify any missing intervention components. Moreover, these intervention components, once evaluated, can be used as a first step in composing a tool or guideline aiming at the improvement of current transitional care initiatives and the development of overarching transitional care initiatives.
Conclusions
This review identified a mismatch between optimal transitional care and the focus/content of existing, transitional care interventions designed to improve the transition from home to a nursing home. The majority of interventions either focused on a specific transition phase rather than the overall transition continuum or focused on specific stakeholders rather than all stakeholders involved. This limits a continuous partnership in which the needs of the older person and informal caregiver are paramount. However, common intervention components have been identified: education, relationships/communication, improving emotional well-being, personalized care, continuity of care, support provision, and ad hoc counseling. These components can be considered in building a comprehensive transitional care intervention that optimizes and defragmentizes the transitional care pathway from home to a nursing home.
Funding
This work was supported by the TRANS-SENIOR project. This project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement number 812656.
Conflict of Interest
None declared.
Supplementary Material
Acknowledgments
This article acknowledges the contribution of the librarians of the KU Leuven Libraries—2Bergen for their advice in the completion of the search strings used in this scoping review.
Contributor Information
Lindsay Groenvynck, Department of Health Services Research, CAPHRI Care and Public Health Research Institute, Faculty of Health Medicine and Life Sciences, Maastricht University, The Netherlands; Department of Public Health and Primary Care, Academic Center for Nursing and Midwifery, KU Leuven, Belgium.
Amal Fakha, Department of Health Services Research, CAPHRI Care and Public Health Research Institute, Faculty of Health Medicine and Life Sciences, Maastricht University, The Netherlands; Department of Public Health and Primary Care, Academic Center for Nursing and Midwifery, KU Leuven, Belgium.
Bram de Boer, Department of Health Services Research, CAPHRI Care and Public Health Research Institute, Faculty of Health Medicine and Life Sciences, Maastricht University, The Netherlands; Living Lab in Ageing and Long-Term Care, Maastricht, The Netherlands.
Jan P H Hamers, Department of Health Services Research, CAPHRI Care and Public Health Research Institute, Faculty of Health Medicine and Life Sciences, Maastricht University, The Netherlands; Living Lab in Ageing and Long-Term Care, Maastricht, The Netherlands.
Theo van Achterberg, Department of Public Health and Primary Care, Academic Center for Nursing and Midwifery, KU Leuven, Belgium.
Erik van Rossum, Living Lab in Ageing and Long-Term Care, Maastricht, The Netherlands; Academy of Nursing, Research Center on Community Care, Zuyd University of Applied Sciences, Heerlen, The Netherlands.
Hilde Verbeek, Department of Health Services Research, CAPHRI Care and Public Health Research Institute, Faculty of Health Medicine and Life Sciences, Maastricht University, The Netherlands; Living Lab in Ageing and Long-Term Care, Maastricht, The Netherlands.
References
- Afram, B. (2015). From home towards the nursing home in dementia: Informal caregivers’ perspectives on why admission happens and what they need. Maastricht University. https://cris.maastrichtuniversity.nl/en/publications/2e3becf0-1c20-4a95-b178-fb82ee803f7c [Google Scholar]
- Afram, B., Verbeek, H., Bleijlevens, M. H., & Hamers, J. P. (2015). Needs of informal caregivers during transition from home towards institutional care in dementia: A systematic review of qualitative studies. International Psychogeriatrics, 27(6), 891–902. doi: 10.1017/S1041610214002154 [DOI] [PubMed] [Google Scholar]
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Boling, P. A. (2009). Care transitions and home health care. Clinics in Geriatric Medicine, 25(1), 135–148, viii. doi: 10.1016/j.cger.2008.11.005 [DOI] [PubMed] [Google Scholar]
- Brownie, S., Horstmanshof, L., & Garbutt, R. (2014). Factors that impact residents’ transition and psychological adjustment to long-term aged care: A systematic literature review. International Journal of Nursing Studies, 51(12), 1654–1666. 10.1016/j.ijnurstu.2014.04.011 [DOI] [PubMed] [Google Scholar]
- Cheek, J., & Ballantyne, A. (2001). Moving them on and in: The process of searching for and selecting an aged care facility. Qualitative Health Research, 11(2), 221–237. doi: 10.1177/104973201129119064 [DOI] [PubMed] [Google Scholar]
- Coleman, E.A., & Boult, C. (2003). Improving the quality of transitional care for persons with complex care needs. Journal of the American Geriatrics Society, 51(4), 556–557. doi: 10.1046/j.1532-5415.2003.51186 [DOI] [PubMed] [Google Scholar]
- Coleman, E. A. (2003). Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. Journal of the American Geriatrics Society, 51(4), 549–555. doi: 10.1046/j.1532-5415.2003.51185.x [DOI] [PubMed] [Google Scholar]
- Crotty, M., Rowett, D., Spurling, L., Giles, L. C., & Phillips, P. A. (2004). Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized, controlled trial. The American Journal of Geriatric Pharmacotherapy, 2(4), 257–264. doi: 10.1016/j.amjopharm.2005.01.001 [DOI] [PubMed] [Google Scholar]
- Davies, S. (2005). Meleis’s theory of nursing transitions and relatives’ experiences of nursing home entry. Journal of Advanced Nursing, 52(6), 658–671. doi: 10.1111/j.1365-2648.2005.03637.x [DOI] [PubMed] [Google Scholar]
- Davis, J. D., Tremont, G., Bishop, D. S., & Fortinsky, R. H. (2011). A telephone-delivered psychosocial intervention improves dementia caregiver adjustment following nursing home placement. International Journal of Geriatric Psychiatry, 26(4), 380–387. doi: 10.1002/gps.2537 [DOI] [PubMed] [Google Scholar]
- Davison, T. E., McCabe, M. P., Busija, L., O’Connor, D. W., Costa, V. C., & Byers, J. (2020). A cluster-randomized trial of the Program to Enhance Adjustment to Residential Living (PEARL): A novel psychological intervention to reduce depression in newly admitted aged care residents. Geriatrics, 20(1), 98. doi: 10.1186/s12877-020-1492-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eika, M., Espnes, G. A., Söderhamn, O., & Hvalvik, S. (2014). Experiences faced by next of kin during their older family members’ transition into long-term care in a Norwegian nursing home. Journal of Clinical Nursing, 23(15–16), 2186–2195. doi: 10.1111/jocn.12491 [DOI] [PubMed] [Google Scholar]
- Ellis, J. M. (2010). Psychological transition into a residential care facility: Older people’s experiences. Journal of Advanced Nursing, 66(5), 1159–1168. doi: 10.1111/j.1365-2648.2010.05280.x [DOI] [PubMed] [Google Scholar]
- Gaugler, J. E., Reese, M., & Sauld, J. (2015). A pilot evaluation of psychosocial support for family caregivers of relatives with dementia in long-term care: The residential care transition module. Research in Gerontological Nursing, 8(4), 161–172. doi: 10.3928/19404921-20150304-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler, J. E., Roth, D. L., Haley, W. E., & Mittelman, M. S. (2008). Can counseling and support reduce burden and depressive symptoms in caregivers of people with Alzheimer’s disease during the transition to institutionalization? Results from the New York University caregiver intervention study. Journal of the American Geriatrics Society, 56(3), 421–428. doi: 10.1111/j.1532-5415.2007.01593.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler, J. E., Roth, D. L., Haley, W. E., & Mittelman, M. S. (2011). Modeling trajectories and transitions: Results from the New York University caregiver intervention. Nursing Research, 60(3 Suppl), S28–S37. doi: 10.1097/NNR.0b013e318216007d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler, J. E., Statz, T. L., Birkeland, R. W., Louwagie, K. W., Peterson, C. M., Zmora, R., Emery, A., McCarron, H. R., Hepburn, K., Whitlatch, C. J., Mittelman, M. S., & Roth, D. L. (2020). The residential care transition module: A single-blinded randomized controlled evaluation of a telehealth support intervention for family caregivers of persons with dementia living in residential long-term care. BMC Geriatrics, 20(1), 133. doi: 10.1186/s12877-020-01542-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim, U. H., Johansson, A., & Lindgren, B. M. (2014). Family caregivers’ experiences of relinquishing the care of a person with dementia to a nursing home: Insights from a meta-ethnographic study. Scandinavian Journal of Caring Sciences, 28(2), 215–224. doi: 10.1111/scs.12046 [DOI] [PubMed] [Google Scholar]
- Greenglass, E. R., Burke, R. J., & Fiksenbaum, L. (2001). Workload and burnout in nurses. Journal of Community & Applied Social Psychology, 11(3), 211–215. doi: 10.1002/casp.614 [DOI] [Google Scholar]
- Groenvynck, L., de Boer, B., Hamers, J., van Achterberg, T., van Rossum, E. H. J. L., & Verbeek, H. (2020). Towards a partnership in the transition from home to a nursing home: The TRANSCIT model. Maastricht University. doi: 10.1016/j.jamda.2020.09.041 [DOI] [PubMed] [Google Scholar]
- Hainstock, T., Cloutier, D., & Penning, M. (2017). From home to ‘home’: Mapping the caregiver journey in the transition from home care into residential care. Journal of Aging Studies, 43, 32–39. doi: 10.1016/j.jaging.2017.09.003 [DOI] [PubMed] [Google Scholar]
- Hayward, J. K., Nunez, K. M., Ballard, C., & Spector, A. (2018). Healthy adjustment for new residents with dementia using SettleIN: A feasibility study in UK care homes. Dementia (London), 1471301218806082. doi: 10.1177/1471301218806082 [DOI] [PubMed] [Google Scholar]
- Heyn, P. C., Meeks, S., & Pruchno, R. (2019). Methodological guidance for a quality review article. The Gerontologist, 59(2), 197–201. doi: 10.1093/geront/gny123 [DOI] [PubMed] [Google Scholar]
- Hirschman, K. B., Shaid, E., McCauley, K., Pauly, M. V., & Naylor, M. D. (2015). Continuity of care: The transitional care model. Online Journal of Issues in Nursing, 20(3), 1. [PubMed] [Google Scholar]
- Križaj, T., Warren, A., & Slade, A. (2016). “Holding on to what I do”: Experiences of older Slovenians moving into a care home. The Gerontologist, 58, 512–520. doi: 10.1093/geront/gnw150 [DOI] [PubMed] [Google Scholar]
- Lichtenberg, P. A. (2007). Assisting urban caregivers after nursing home placement. Clinical Gerontologist, 30(2), 65–77. doi: 10.1300/J018v30n02_06 [DOI] [Google Scholar]
- Lord, K., Livingston, G., & Cooper, C. (2015). A systematic review of barriers and facilitators to and interventions for proxy decision-making by family carers of people with dementia. International Psychogeriatrics, 27(8), 1301–1312. doi: 10.1017/S1041610215000411 [DOI] [PubMed] [Google Scholar]
- Mansukhani, R. P., Bridgeman, M. B., Candelario, D., & Eckert, L. J. (2015). Exploring transitional care: Evidence-based strategies for improving provider communication and reducing readmissions. P & T, 40(10), 690–694. [PMC free article] [PubMed] [Google Scholar]
- Meiland, F. J., Danse, J. A., Wendte, J. F., Gunning-Schepers, L. J., & Klazinga, N. S. (2002). Urgency coding as a dynamic tool in management of waiting lists for psychogeriatric nursing home care in The Netherlands. Health Policy (Amsterdam, Netherlands), 60(2), 171–184. doi: 10.1016/s0168-8510(01)00209-3 [DOI] [PubMed] [Google Scholar]
- Melrose, S. (2004). Reducing relocation stress syndrome in long-term care facilities. The Journal of Practical Nursing, 54(4), 15–17. [PubMed] [Google Scholar]
- Mukamel, D. B., Amin, A., Weimer, D. L., Ladd, H., Sharit, J., Schwarzkopf, R., & Sorkin, D. H. (2016). Personalizing nursing home compare and the discharge from hospitals to nursing homes. Health Services Research, 51(6), 2076–2094. doi: 10.1111/1475-6773.12588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller, C., Lautenschläger, S., Meyer, G., & Stephan, A. (2017). Interventions to support people with dementia and their caregivers during the transition from home care to nursing home care: A systematic review. International Journal of Nursing Studies, 71, 139–152. doi: 10.1016/j.ijnurstu.2017.03.013 [DOI] [PubMed] [Google Scholar]
- Nantsupawat, A., Nantsupawat, R., Kunaviktikul, W., Turale, S., & Poghosyan, L. (2016). Nurse burnout, nurse-reported quality of care, and patient outcomes in Thai hospitals. Journal of Nursing Scholarship, 48(1), 83–90. doi: 10.1111/jnu.12187 [DOI] [PubMed] [Google Scholar]
- National Transitions of Care Coalition . (2008). Improving transitions of care. The vision of the national transitions of care coalition. Washington DC: National Transitions of Care Coalition. [Google Scholar]
- Nolan, M., & Dellasega, C. (2000). ‘I really feel I’ve let him down’: Supporting family carers during long-term care placement for elders. Journal of Advanced Nursing, 31(4), 759–767. doi: 10.1046/j.1365-2648.2000.01346.x [DOI] [PubMed] [Google Scholar]
- Pauly, M. V., Hirschman, K. B., Hanlon, A. L., Huang, L., Bowles, K. H., Bradway, C., McCauley, K., & Naylor, M. D. (2018). Cost impact of the transitional care model for hospitalized cognitively impaired older adults. Journal of Comparative Effectiveness Research, 7(9), 913–922. doi: 10.2217/cer-2018-0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paun, O., & Farran, C. J. (2011). Chronic grief management for dementia caregivers in transition: Intervention development and implementation. Journal of Gerontological Nursing, 37(12), 28–35. doi: 10.3928/00989134-20111103-04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paun, O., Farran, C. J., Fogg, L., Loukissa, D., Thomas, P. E., & Hoyem, R. (2015). A chronic grief intervention for dementia family caregivers in long-term care. Western Journal of Nursing Research, 37(1), 6–27. doi: 10.1177/0193945914521040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedl, M., Mantovan, F., & Them, C. (2013). Being a nursing home resident: A challenge to one’s identity. Nursing Research and Practice, 2013, 932381. doi: 10.1155/2013/932381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas Smith, L., Ashok, M., Morss Dy, S., Wines, R. C., & Teixeira-Poit, S. (2014). AHRQ methods for effective health care. Contextual frameworks for research on the implementation of complex system interventions. Agency for Healthcare Research and Quality (US). [PubMed] [Google Scholar]
- Saint-Bryant, C. A., Murrill, J., Hayward, J. K., Nunez, K. M., & Spector, A. (2020). SettleIN: Using a manualised intervention to facilitate the adjustment of older adults with dementia following placement into residential care. International Journal of Environmental Research and Public Health, 17(7), 1–18. doi: 10.3390/ijerph17072606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanford, A. M., Orrell, M., Tolson, D., Abbatecola, A. M., Arai, H., Bauer J. M., Cruz-Jentoft, A. J., Dong, B., Ga, H., Goel, A., Hajjar, R., Holmerova, I., Katz, P. R., Koopmans, R. T., Rolland, Y., Visvanathan, R., Woo, J., Morley, J. E., & Vellas, B. (2015). An international definition for “nursing home”. Journal of the American Medical Directors Association, 16(3), 181–184. doi: 10.1016/j.jamda.2014.12.013 [DOI] [PubMed] [Google Scholar]
- Schön, P., Lagergren, M., & Kåreholt, I. (2016). Rapid decrease in length of stay in institutional care for older people in Sweden between 2006 and 2012: Results from a population-based study. Health & Social Care in the Community, 24(5), 631–638. doi: 10.1111/hsc.12237 [DOI] [PubMed] [Google Scholar]
- Schulz, R., Rosen, J., Klinger, J., Musa, D., Castle, N. G., Kane, A., & Lustig, A. (2014). Effects of a psychosocial intervention on caregivers of recently placed nursing home residents: A randomized controlled trial. Clinical Gerontologist, 37(4), 347–367. doi: 10.1080/07317115.2014.907594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman, T., & Dupuis, S. (2012). Supporting a relative’s move into long-term care: Starting point shapes family members’ experiences. Canadian Journal on Aging, 31(4), 395–410. doi: 10.1017/S0714980812000384 [DOI] [PubMed] [Google Scholar]
- Sussman, T., & Dupuis, S. (2014). Supporting residents moving into long-term care: Multiple layers shape residents’ experiences. Journal of Gerontological Social Work, 57(5), 438–459. doi: 10.1080/01634372.2013.875971 [DOI] [PubMed] [Google Scholar]
- Toscan, J., Mairs, K., Hinton, S., & Stolee, P.; InfoRehab Research Team . (2012). Integrated transitional care: Patient, informal caregiver and health care provider perspectives on care transitions for older persons with hip fracture. International Journal of Integrated Care, 12, e13. doi: 10.5334/ijic.797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Van Mierlo, L. D., Bootsma-Van der Wiel, A., Meiland, F. J., Van Hout, H. P., Stek, M. L., & Dröes, R. M. (2015). Tailored mental health care after nursing home admission: Improving transfers of people with dementia with behavioral problems. An explorative study. Aging & Mental Health, 19(10), 902–911. doi: 10.1080/13607863.2014.977774 [DOI] [PubMed] [Google Scholar]
- Wada, M., Canham, S. L., Battersby, L., Sixsmith, J., Woolrych, R., Fang, M. L., & Sixsmith, A. (2020). Perceptions of home in long-term care settings: Before and after institutional relocation. Aging and Society, 40(6), 1267–1290. doi: 10.1017/S0144686X18001721 [DOI] [Google Scholar]
- Wagner, E., Schaefer, J., Horner, K., Cutsogeorge, D., & Perraul, R. (2011). Reducing care fragmentation: A toolkit for coordinating care.http://www.improvingchroniccare.org/downloads/reducing_care_fragmentation.pdf
- Ward, K. T., Bates-Jensen, B., Eslami, M. S., Whiteman, E., Dattoma, L., Friedman, J. L., DeCastro Mariano, J., & Moore, A. A. (2008). Addressing delays in medication administration for patients transferred from the hospital to the nursing home: A pilot quality improvement project. The American Journal of Geriatric Pharmacotherapy, 6(4), 205–211. doi: 10.1016/j.amjopharm.2008.10.001 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2016). Transitions of care: Technical series on safer primary care. https://www.who.int/patientsafety/topics/primary-care/technical_series/en/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.