Abstract
This cross-sectional study of US second-year medical students examines the proportion of accommodation requests made across disability categories.
Access to accommodations is critical for medical students with disabilities and may explain differences in performance,1 program persistence,1,2 and graduation.2 Lack of accommodations has also been associated with greater risk of increased depressive symptoms and self-reported medical errors among training physicians.3 Despite the potential consequences of nonaccommodations, and a growing number of medical students reporting disabilities,4 to our knowledge, no study has investigated differences in the proportion of accommodation requests across disability categories. Variation in request by disability category may reveal barriers and vulnerabilities within subpopulations of students with disabilities. This study aimed to identify the proportion of accommodation requests across disability categories.
Methods
We analyzed data from 2 cohorts (2019 and 2020) of the Association of American Medical Colleges Year Two Questionnaires, a national online survey of second-year MD students. Data included demographic characteristics (sex, age group, sexual orientation, race and ethnicity; Table) and disability-related questions, including self-reported disability, disability type, whether the “medical school provided accommodations for your disability,” and why no accommodations were made (eMethods in the Supplement). In keeping with previous studies,1 we assigned self-reported disability into 3 categories: chronic health disabilities, cognitive disabilities, and motor/sensory disabilities. Because our goal was to assess differences in the proportion of accommodation requests by disability category, only students who provided responses to both the disability category and accommodation questions and who reported 1 or more disabilities belonging to a single disability category were included.
Table. Demographic and Disability-Related Characteristics of Participants.
| Characteristic | Students with chronic health disabilities (n = 336) | Students with cognitive disabilities (n = 1655) | Students with motor/sensory disabilities (n = 149) | Total (n = 2140) |
|---|---|---|---|---|
| Demographic characteristics, No. (%) | ||||
| Sex | ||||
| Male | 121 (36.0) | 700 (42.3) | 81 (51.4) | 902 (42.2) |
| Female | 215 (64.0) | 954 (57.7) | 48 (45.6) | 1237 (57.8) |
| Age, y | ||||
| ≤26 | 268 (79.8) | 1212 (73.2) | 123 (82.6) | 1603 (54.9) |
| ≥27 | 68 (20.2) | 443 (26.8) | 26 (17.4) | 537 (25.1) |
| Sexual orientation | ||||
| Heterosexual or straight | 278 (83.2) | 1283 (79.6) | 125 (86.8) | 1686 (80.7) |
| Lesbian, gay, or bisexual | 56 (16.8) | 329 (20.4) | 19 (13.2) | 404 (19.3) |
| Race and ethnicity | ||||
| Underrepresented in medicinea | 62 (18.8) | 401 (24.6) | 24 (16.2) | 487 (23.1) |
| Nonunderrepresented in medicine | 268 (81.2) | 1232 (75.4) | 124 (83.8) | 1627 (73.9) |
| Disability-related characteristics, No. (%) [95% CI] | ||||
| Types of disability within categoriesb | ||||
| Chronic health category | ||||
| Chronic health disability | 296 (88.1) [84.1-91.4] | 296 (13.8) [12.4-15.4] | ||
| Other (open-text responses)c | 40 (11.9) [8.6-15.9] | 40 (1.9) [1.3-2.5] | ||
| Cognitive category | ||||
| ADHD | 1247 (75.3) [73.2-77.4] | 1247 (58.3) [56.2-60.4] | ||
| Learning disability | 173 (10.5) [9.0-12.0] | 173 (8.1) [7.0-9.3] | ||
| Psychological disability | 435 (26.3) [24.2-28.5] | 435 (20.3) [18.6-22.1] | ||
| Other (open-text responses)c | 56 (3.4) [2.6-4.4] | 56 (2.6) [2.0-3.4] | ||
| Motor/sensory category | ||||
| Deaf or hard of hearing | 56 (37.6) [29.8-45.9] | 56 (2.6) [2.0-3.4] | ||
| Mobility disability | 31 (20.8) [14.6-28.2] | 31 (1.4) [1.0-2.0] | ||
| Visual disability | 61 (40.9) [33.0-49.3] | 61 (2.9) [2.2-3.6] | ||
| Other (open-text responses)c | 4 (2.7) [0.7-6.7] | 4 (0.2) [0.1-0.5] | ||
| Need for accommodations: nod (n = 772) | ||||
| Did not request accommodation because does not need accommodation | 80 (23.8) [19.4-28.7] | 646 (39.0) [36.7-41.4] | 46 (30.9) [23.6-38.9] | 772 (36.1) [34.0-38.2] |
| Need for accommodation: yes (n = 1368) | ||||
| Did not request accommodations for any reason other than not needing accommodations | 37 (11.0) [7.9-14.9] | 214 (12.9) [11.4-14.6] | 9 (6.0) [2.8-11.2] | 260 (12.1) [10.8-13.6] |
| Requested accommodations: accommodation was provided by medical school | 210 (62.5) [57.1-67.7] | 772 (46.6) [44.2-49.1] | 92 (61.7) [53.4-69.6] | 1074 (50.2) [48.1-52.3] |
| Requested accommodations: request was denied by medical school | 7 (2.1) [0.8-4.2] | 14 (0.8) [0.5-1.4] | 1 (0.7) [0.0-3.7] | 22 (1.0) [0.7-1.6] |
| Requested accommodations: request is under review by medical school | 2 (0.6) [0.1-2.1] | 9 (0.5) [0.3-1.0] | 1 (0.7) [0.0-3.7] | 12 (0.6) [0.3-1.0] |
Race and ethnicity were categorized as “underrepresented in medicine” and “nonunderrepresented in medicine” in the raw data set received from the Association of American Medical Colleges (AAMC). The group underrepresented in medicine includes any US citizen or permanent resident who self-identified as 1 or more of the following: American Indian or Alaska Native; Black or African American; Hispanic, Latino, or of Spanish Origin; or Native Hawaiian or Other Pacific Islander.
Percentages within categories may not sum to 100% because students with multiple types of disabilities were included if all reported disabilities belonged to the same category. Chronic health disabilities include cancer, diabetes, lupus, rheumatoid arthritis, etc. Cognitive disabilities include attention-deficit/hyperactivity disorder (ADHD), learning disabilities, psychological disabilities, and mental health/neuropsychiatric disorders. Motor/sensory disabilities include all mobility disabilities, deaf and hard of hearing disabilities, and visual disabilities.
Open-text responses from students who replied “other” to the question on the type of disability were categorized into 1 of 3 groups (chronic health disabilities, cognitive disabilities, and motor/sensory disabilities). Examples of open-text responses categorized as chronic health disabilities include cancer, diabetes, epilepsy, HIV, lupus, rheumatoid arthritis, and ulcerative colitis. Examples of open-text responses categorized as cognitive disabilities include depressive disorder, generalized anxiety disorder, obsessive-compulsive disorder, posttraumatic stress disorder, and test anxiety. Examples of open-text responses categorized as motor/sensory disabilities include amputee, hand splint, and spinal cord injury.
Includes students who replied “I did not request accommodations because I feel I do not need accommodations” to the question “Which of the following best describes why your medical school did not or has not provided accommodations.”
We calculated descriptive summary statistics for the overall sample, stratified by disability category. Differences in accommodation requests across different disability categories were assessed using χ2 tests. A 2-sided P < .05 was considered statistically significant. Analyses were conducted using SPSS-21 (IBM Corp). The study was deemed exempt by the University of Colorado Medical School Institutional Review Board.
Results
Overall, 27 009 students (61.3%) replied to the survey and 2438 (9.0% [95% CI, 8.7%-9.4%]) self-reported a disability. Of those, 2353 (96.5%) provided responses about disability type and accommodations and 2140 (90.9%) reported disabilities within a single disability category (336 [15.7%] chronic health, 1655 [77.3%] cognitive, and 149 [7.0%] motor/sensory) and were included in our analysis (Table).
Of these 2140 students, 1108 (51.8% [95% CI, 49.6%-53.9%]) reported requesting accommodations (chronic health: 219/336 [65.2%]; cognitive: 795/1655 [48.0%]; motor/sensory: 94/149 [63.1%]), 772 (36.1% [95% CI, 34.0%-38.1%]) reported not needing accommodations (chronic health: 80/336 [23.8%]; cognitive: 646/1655 [39.0%]; motor/sensory: 46/149 [30.9%]), and 260 (12.1% [95% CI, 10.8%-13.6%]) reported not requesting accommodations for any reason other than not needing them (chronic health: 37/336 [11.0%]; cognitive: 214/1655 [12.9%]; motor/sensory: 9/149 [6.0%]). Of 1108 accommodation requests, 22 (2.0%) were denied.
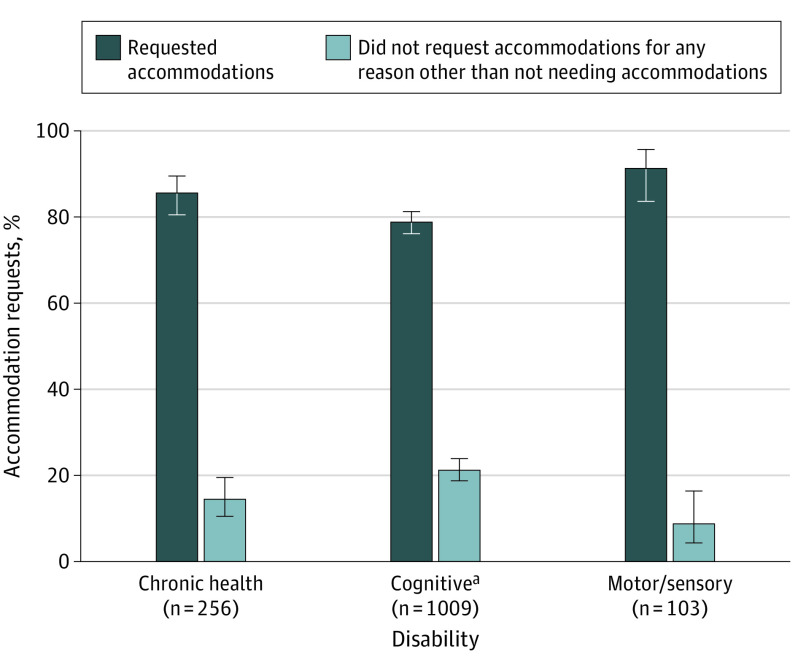
Among the 1368 students (63.9%) who reported needing accommodations, 260 (19.0% [95% CI, 17.0%-21.2%]) reported not requesting accommodation for reasons other than not needing them, with a significantly lower proportion of students with cognitive disabilities reporting requesting accommodations (795 [78.8%]) compared with students with chronic health (219 [85.5%]) or motor/sensory disabilities (94 [91.3%]), P = .001 (Figure).
Figure. Proportion of Accommodation Request by Disability Category Among Medical Students Who Reported Needing Accommodations (n = 1368).
Excludes participants who reported not needing accommodations (ie, those who replied “I did not request accommodations because I feel I do not need accommodations” to the survey question “Which of the following best describes why your medical school did not or has not provided accommodations?”).
aStatistically significantly lower proportion of students who requested accommodations than the other groups (χ22 = 13.7; P = .001).
Discussion
This study found that approximately half of second-year students who self-reported disability requested accommodations, which was lower among students with cognitive disabilities. Among those needing accommodations, nearly 1 in 5 did not request them; for those who did request accommodations, few were denied.
Previous studies suggest that students with cognitive disabilities, including those with attention-deficit/hyperactivity disorder, learning disabilities, and psychological disabilities, encounter stigma and misinformation about their ability to successfully navigate medical school.5 Although not assessed by the present study, the nonapparent nature of many cognitive disabilities,1 fear of stigma,5 and the possible downstream consequences of disability disclosure6 may contribute to the lower frequency of requests within this disability category.
Limitations include the self-reported nature of the survey and lack of detailed information regarding type and quality of accommodation.
Given the risks associated with lack of disability accommodations when needed,1,2,3 schools should highlight the availability of accommodations and increase efforts to encourage accommodation requests, especially among students with cognitive disabilities. Future studies should investigate possible factors serving as drivers of nonrequests.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Senior Editor.
eMethods. 2019 and 2020 Association of American Medical Colleges Year-Two Questionnaire survey questions used in the present study
References:
- 1.Meeks LM, Plegue M, Swenor BK, et al. The performance and trajectory of medical students with disabilities: results from a multisite, multicohort study. Acad Med. 2022;97(3):389-397. doi: 10.1097/ACM.0000000000004510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen KH, Jain NR, Case B, Jain S, Meeks LM. Impact of USMLE Step-1 accommodation denial on US medical schools: A national survey. PLoS One. 2022;17(4):e0266685. doi: 10.1371/journal.pone.0266685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meeks LM, Pereira-Lima K, Frank E, Stergiopoulos E, Ross KET, Sen S. Program Access, Depressive Symptoms, and Medical Errors Among Resident Physicians With Disability. JAMA Netw Open. 2021;4(12):e2141511. doi: 10.1001/jamanetworkopen.2021.41511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meeks LM, Case B, Herzer K, Plegue M, Swenor BK. Change in Prevalence of Disabilities and Accommodation Practices Among US Medical Schools, 2016 vs 2019. JAMA. 2019;322(20):2022-2024. doi: 10.1001/jama.2019.15372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meeks LM, Jain NR. Accessibility, inclusion, and action in medical education: lived experiences of learners and physicians with disabilities. Association of American Medical Colleges; March 13, 2018; Washington, DC.
- 6.Saddawi-Konefka D, Brown A, Eisenhart I, Hicks K, Barrett E, Gold JA. Consistency Between State Medical License Applications and Recommendations Regarding Physician Mental Health. JAMA. 2021;325(19):2017-2018. doi: 10.1001/jama.2021.2275 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. 2019 and 2020 Association of American Medical Colleges Year-Two Questionnaire survey questions used in the present study