Abstract
Both the rate of mobile phone addiction and suicidality among adolescents have increased during the pandemic lockdown. However, the relationship between mobile phone addiction and suicide risk and the underlying psychological mechanisms remains unknown. This study examined the associations between mobile phone addiction in adolescents during the first month of lockdown and the suicide risk in the subsequent five months. A two-wave short-term longitudinal web-based survey was conducted on 1609 senior high school students (mean age = 16.53 years, SD = 0.97 years; 63.5% female). At Time 1 (T1), the severity of mobile phone addiction and basic demographic information was collected from Feb 24 to 28, 2020 in Sichuan Province, China (at the pandemic’s peak). Five months later, between July 11 and July 23 (Time 2, T2), mobile phone addiction, daytime sleepiness, depression, and suicidality were measured within the past five months. The regression analysis revealed that mobile phone addiction during quarantine directly predicted suicidality within the next five months, even after controlling for the effect of depression and daytime sleepiness. Meanwhile, mobile phone addiction at T1 also indirectly predicted suicidality at T2, with depression and daytime sleepiness mediating this association. Programs targeting improvement of daytime sleepiness and depressive symptoms may be particularly effective in reducing suicide risk among adolescents with mobile phone addiction.
Keywords: COVID-19, Suicidality, Depression, Daytime sleepiness, Mobile phone addiction
Introduction
COVID-19 emerged in late 2019 and forced many countries to implement quarantine measures, such as lockdowns, home confinement, self-isolation, and social distancing [1], which raise public health concerns [2, 3]. Because school-aged children had to take online classes from home during the pandemic, there was a significant increase in their use of mobile phones [4, 5], which led to the rise in mobile phone addiction [6–8]. It has also been found that pandemic lockdown measures resulted in a rise in negative emotions in adolescents, which manifested as sleep problems [9], anxiety, depression, and suicidality [10–14]. Indeed, youth suicide risk has become a significant global health concern during the pandemic [15, 16]. However, neither the connection between mobile phone addiction and the increased suicide risk during the pandemic, nor the associated psychosocial mechanisms, have been adequately explored [17, 18]. Therefore, to fully understand the underlying mechanisms in the relationship between adolescent mobile phone addiction and suicidality during the COVID-19 pandemic, there has been a call for more profound investigative research [19–22].
COVID-19 and suicidality
Many studies have investigated suicidality during the COVID-19 pandemic. For example, Every-Palmer et al. (2020) surveyed 2010 New Zealand adults in April 2020 and found that 6% had suicidal ideation and 2% had attempted suicide [23]. Iob et al. (2020) reported that 18% (n = 7984) of 44,775 adults in the UK had experienced thoughts of suicide or self-harm, and 5% (n = 2174) had harmed themselves at least once in the first month of the COVID-19 lockdown. Czeisler et al. (2020) surveyed 5412 United States adults and found that 10.7% had seriously considered suicide in the 30 days before completing the survey [24]. Wang et al. (2020) reported that 18.04% of 2031 undergraduate and graduate students in the United States had experienced suicidal ideation during the COVID-19 pandemic, and Sun et al. (2021) found that 19.56% of Chinese university students had had suicidal ideation during the COVID-19 quarantine. However, a study in Spain did not find any significant change in the overall suicidal ideation prevalence before and after the COVID-19 outbreak [25],. Similarly, Isumi et al. (2020) found that the suicide rates in children and adolescents under 20 during the school closures from March to May 2020 in Japan did not change significantly compared with the same period in 2018 and 2019.
Although many studies have investigated the rate of suicidal ideation or behaviors during the COVID-19 crisis, several research gaps need to be addressed: 1) the majority of the studies have only reported the rate of suicidal ideation, attempts, or behaviors, but few studies have investigated the underlying suicidality mechanisms; 2) most previous studies have been cross-sectional rather than longitudinal; however, as the pandemic psychological sequelae may persist for months and years to come and peak later than the actual pandemic [26], longitudinal or follow up studies are needed; 3) most studies on pandemic related suicidality have been conducted on adults, yet adolescents are vulnerable to negative emotions and may be particularly disposed to suicidality [27, 28], therefore, longitudinal studies on suicidality and the related mechanisms in adolescents are needed.
Mobile phone addiction and suicidality
Mobile phone addiction is defined as the inability to regulate personal mobile phone use, which can eventually lead to symptoms similar to substance abuse disorders, such as compulsive use, withdrawal, cravings, loss of control, and mood dysregulation [29]. A significant increase in mobile phone use and addiction has been found in many COVID-19 studies. For example, Zhang et al. (2021) found an elevated risk of problematic mobile phone use in Chinese adults during the COVID-19 pandemic, with the prevalence being as high as 43.3%. Saadeh et al. (2021) reported a 62.4% mobile phone addiction prevalence in 6154 Jordanian undergraduates during the COVID-19 quarantine, and Caponnetto et al. (2021) and Serra et al. (2021) both found a growth in pathological cell phone use during the Italian COVID-19 lockdown.
Several studies have also found that mobile phone addiction could result in several physical and mental health issues, such as dry eyes, migraine headaches, sleep disorders, intellectual impairment, depression, and anxiety [30–32]. However, only a few studies have investigated the associations between mobile phone addiction and suicidality. For example, Chen et al. (2020) found that high mobile phone use intensity directly predicted suicide-related behaviors in Chinese adolescents and that depression mediated this relationship [33]. Ismail et al.(2020) found that smartphone addiction was positively associated with suicidality in Malaysian college students; however, no predictive effects were identified in this association [34].
Pathways from mobile phone addiction to suicidality
It has been found that mobile phone addiction can lead to adverse psychological sequelae, with depression and sleep disturbance being the most commonly reported [35–37]. For example, Lemola et al. (2015) found excessive mobile phone use at night to cause sleep difficulties, depression, and stress in adolescents [38]. Demirci et al. (2015) reported positive correlations between mobile phone addiction scale scores, depression levels, and sleep quality scores [39]. Thomee et al.’s (2011) longitudinal study revealed an association between high-frequency mobile phone use, sleep disturbances, and depression at a one-year follow-up on 4156 young adults [40]. Elhai et al.(2017) conducted a literature review and found that nine of 10 included studies reported at least medium effect size associations between problematic smartphone use and the depression severity [41]. Other cross-sectional studies revealed correlations between high levels of mobile phone addiction severity and poor sleep quality [42–44].
In addition to the association with mobile phone addiction, depression and sleep disorders have also been associated with suicidality [45–47]. For example, Bernert et al.’s (2015) systematic review concluded preliminary, converging evidence that sleep disturbances were an empirical risk factor for suicidal behaviors. Liu et al. (2004) found that sleeping less than eight hours and frequent nightmares were significantly associated with an increased risk of suicide attempts in adolescents. Wang et al. (2021) found that sleep disturbances could prospectively predict the development and persistence of suicidal ideation. Daytime sleepiness, defined as an inability to maintain wakefulness and alertness during the day [48], is one of the most common sleep disturbance sequelae [49], which is most directly associated with daytime dysfunction. Notably, studies have proposed that daytime sleepiness may mediate the association between mobile phone addiction and PTSD in adolescents during COVID-19 (Hu, Wang, et al., 2021). It is also possible for daytime sleepiness to play a mediating role between mobile phone addiction and suicidality [50, 51].
Therefore, as mobile phone addiction can result in depression, sleep disturbances, and daytime sleepiness, which in turn may increase suicidality, it is reasonable to assume that depression and daytime sleepiness could mediate between mobile phone addiction and suicidality. However, the above evidence illustrates that only a few studies have explored the underlying mediating mechanisms between mobile phone addiction and suicidality in a longitudinal design. For instance, a Chinese study has shown that depression mediates the relationship between mobile phone addiction and suicidal behavior in adolescents in a cross-sectional study [52]. Another study found that insomnia and depression mediated the relationship between internet gaming addiction and suicidal ideation [53]. As prior studies have been primarily cross-sectional, there is a need to conduct longitudinal studies investigating these associations, and the underlying mechanisms, in adolescents during the COVID-19pandemic.
The present study
Research into the complex interactions and associations between mobile phone addiction, suicidality, depression, and daytime sleepiness could provide a more comprehensive understanding of the potential suicidality mechanisms. Therefore, this study was a two-wave longitudinal study aimed at investigating: (a) the severity of mobile phone addiction in Chinese adolescent students during the COVID-19 quarantine (Time 1, T1), and (b) the suicide risk five months later (Time 2, T2) when the pandemic was in remission in China. Specifically, we tested the following hypotheses: (1) That mobile phone addiction (T1) would be positively correlated with suicidality (T2); (2) That mobile phone addiction (T1) would predict suicidality (T2); (3) That depression and daytime sleepiness would mediate the link between mobile phone addiction (T1) and suicidality (T2). These findings may advance the understanding of how and when mobile phone addiction causes suicidality and how to protect adolescents from the unfavorable impacts of excessive mobile phone use.
Methods
Participants and procedures
Students from two senior high schools (12 ~ 18 years old, those over 18 are excluded) in Sichuan province, China, were invited to participate in an online survey for basic demographic information on mobile phone addiction from February 24 to 28, 2020 (T1, about one month after the national lockdown in China that began on January 21, 2020). Five months later, between July 11 and July 23 (Time 2, T2), mobile phone addiction, daytime sleepiness, depression, and suicidality in the past five months were measured. In Sichuan Province, the state lockdown was lifted at the end of March 2020, and students returned to school in early April. Therefore, the COVID-19 pandemic was considered in remission at Time 2.
This study was approved by the Ethics Committee of the Sichuan Psychological Society (NO. 2020_12). Informed consent was given online by participants and their statutory guardians. This survey was part of the Surveys on the Behavior and Psychological Health Project affected by COVID-19.
Measures
Measures included demographic variables, pandemic exposure questionnaires, and four psychopathological conditions, including mobile phone addiction, depressive symptoms, daytime sleepiness, and suicidal ideation or attempts. At T1, we measured mainly what happened in the past month, within the first month during the lockdown. At T2, we measured mainly what occurred in the past five months, that is, within the five months between T1 and T2.
Demographic variables and COVID-19 related exposure
Demographic information on age, gender, and grade level was collected. COVID-19 exposure was evaluated with three yes/no questions derived from previous traumatic studies [54, 55], whether a friend or relative had been infected with COVID-19; whether the participants lived in a community in which someone was infected; whether the participants had a friend or relative who had died of COVID-19.
Mobile Phone Addiction Index (MPAI)
Mobile phone addiction at T1 was assessed using the Chinese version of the Mobile phone Addiction Index (MPAI) [56], which was a self-report questionnaire with 17 items under four subscales: losing control and receiving complaints; anxiety, and cravings; withdrawal/escape; and productivity loss. At T1, MPAI was measured within the first month of the lockdown. The participants were required to rate each item on a five-point Likert scale ranging from 1 = never to 5 = very often. The total MPAI score ranged from 17 to 85, with higher scores indicating a higher intensity of mobile phone use and 51 or above showing mobile phone addiction [57]. In the present study, the Cronbach’s a is 0.92 at T1 and 0.94 for the T2.
Daytime sleepiness
The participants’ daytime sleepiness at T2 was evaluated using the Chinese Adolescent Daytime Sleepiness Scale (CADSS) [58] for the past five months between T1 and T2. The CADSS comprised seven items; each scored on a five-point Likert scale. Higher scores indicate more severe daytime sleepiness (Range = 7–35), and a score greater than 16 indicates excessive daytime sleepiness. In the current study, Cronbach’s α was 0.89.
Depression
Depression at T2 was assessed using the abbreviated Kutcher Adolescent Depression Scale (KADS) in the past five months, with six items and a self-report scale to diagnose adolescent depression and its severity [59]. This scale has been used on Chinese children and adolescents and has shown good internal and test–retest reliability [60]. The total KADS score ranged from 0 to 18, with scores ≥ 6 indicating possible depression. The Cronbach’s α in the current study was 0.91.
Suicidality
At T2, suicidality in the past five months between T1 and T2 was measured using the modified Chinese version of the Suicidal Behaviors Questionnaire-Revised (SBQ-R) [61], which is a brief suicidality self-reported scale that has four questions, such as “Have you ever thought about or attempted to kill yourself in the past five months?” marked on a Likert scale on the frequency of suicidal ideation or attempts, with the total score ranging from 3 to 18 and scores ≥ 7 indicating a non-clinically significant risk of suicide. This questionnaire's good psychometric properties have been reported in previous studies on Chinese adolescents and young adults [62]. In the present study, Cronbach’s α was 0.76.
Data analysis
Pearson’s correlation analysis was used to examine the clinical variable associations; To identify whether and how much variance mobile phone addiction at T1 were independent predictors of subsequent suicidal risk, stepwise and enter regression analyses were carried out while controlling for demographic and COVID-19 exposure factors, daytime sleepiness, and depressive symptoms step by step. The mediation analysis adopts PROCESS model 6 [63], which allows four variables to exist in a chain effect to examine the mediating effects of daytime sleepiness/depression on the associations between mobile phone addiction and suicidality. The indirect effects and 95% bootstrap confidence intervals (CI) were calculated on 5000 bootstrapped samples as conducting the bootstrap resampling method requires at least 2000 replications [64] and more bootstrapped samples improve estimation [65]. The statistical analyses were conducted using SPSS version 22.0.
Results
Demographic information and COVID-19 exposure
Two thousand three hundred ninety-nine participants were initially surveyed from the two senior high schools; 1609 (73.6%) completed the T1 and T2 surveys. The mean age for these 1609 adolescents (range 12 ~ 18 years old) was 16.53 (SD = 0.97) years, 1021 (63.5%) of whom were female. Three hundred and twenty-two (20.0%) students reported suicidal ideation or suicide attempts at T2, 207(64.3%) females. The detailed sample characteristics are presented in Table 1. Suicidality stratified by demographic and exposure variables were displayed in Table 2.
Table 1.
Demographic and exposure variables in a sample of Chinese adolescents (N = 1609)
| Variables | N | % |
|---|---|---|
| Total | 1609 | 100 |
| Gender | ||
| Male | 588 | 36.5 |
| Female | 1021 | 63.5 |
| Age(yr) | ||
| ≤ 15 | 243 | 15.1 |
| 16 | 526 | 32.7 |
| 17 | 552 | 34.3 |
| 18 | 288 | 17.9 |
| Grade | ||
| 10 | 485 | 30.1 |
| 11 | 692 | 43.0 |
| 12 | 432 | 26.9 |
| Only-child status | ||
| Yes | 397 | 24.7 |
| No | 1212 | 75.3 |
| Someone in the community is infected | ||
| Yes | 92 | 5.7 |
| No | 1517 | 94.3 |
| A relative or friend is infected | ||
| Yes | 13 | 0.8 |
| No | 1596 | 99.2 |
| A relative or friend died from the infection | ||
| Yes | 3 | 0.2 |
| No | 1606 | 99.8 |
| Smoker | ||
| Yes | 31 | 19.3 |
| No | 1578 | 80.7 |
| Drinker | ||
| Yes | 93 | 5.8 |
| No | 1516 | 94.2 |
Table 2.
Suicidality stratified by demographic and exposure variables (N = 1609)
| Variables | Suicidality (n) | Prevalence(%) | χ2 |
|---|---|---|---|
| Total | n = 322 | 20.0 | |
| Gender | 0.12 | ||
| Male | 115 | 19.6 | |
| Female | 207 | 20.3 | |
| Age(yr) | 3.44 | ||
| ≤ 15 | 38 | 15.6 | |
| 16 | 110 | 20.9 | |
| 17 | 115 | 20.8 | |
| 18 | 59 | 20.5 | |
| Grade | 2.68 | ||
| 10 | 85 | 17.5 | |
| 11 | 146 | 21.1 | |
| 12 | 91 | 21.1 | |
| Only-child status | 0.05 | ||
| Yes | 81 | 20.4 | |
| No | 241 | 19.9 | |
| Someone in the community is infected | 0.48 | ||
| Yes | 21 | 22.8 | |
| No | 301 | 19.8 | |
| A relative or friend is infected | 1.24 | ||
| Yes | 1 | 7.7 | |
| No | 321 | 20.1 | |
| A relative or friend died from the infection | 0.75 | ||
| Yes | 0 | 0 | |
| No | 322 | 20.0 | |
| Smoker | 2.96** | ||
| Yes | 10 | 32.3 | |
| No | 312 | 19.8 | |
| Drinker | 0.41 | ||
| Yes | 21 | 22.6 | |
| No | 301 | 19.9 |
**p < 0.01
Correlations between the main variables
Mobile phone addiction at T1 was significantly correlated with daytime sleepiness (r = 0.316), depression (r = 0.312), and suicidality (r = 0.289) at T2. Meanwhile, suicidality at T2 was significantly correlated with depression at T2 (r = 0.469) and daytime sleepiness at T2 was also significantly correlated with suicidality at T2 (r = 0.311). Details are present in Table 3. The correlations between these four variables indicated that subsequent regression was needed.
Table 3.
Correlations of main study variables (N = 1609)
| Variable | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. MPA_T1 | 41.60 | 12.59 | 1 | |||
| 2. DS_T2 | 13.45 | 5.80 | 0.316** | 1 | ||
| 3. Depression_T2 | 4.22 | 3.73 | 0.312** | 0.364** | 1 | |
| 4. Suicidality_T2 | 4.68 | 2.88 | 0.289** | 0.311** | 0.469** | 1 |
**p < 0.01
MPA_T1 Time 1 smartphone addiction score, DS_T2 Time 2 daytime sleepiness score, Depression_T2 Time 2 depression score, Suicidality_T2 Time 2 suicidality score
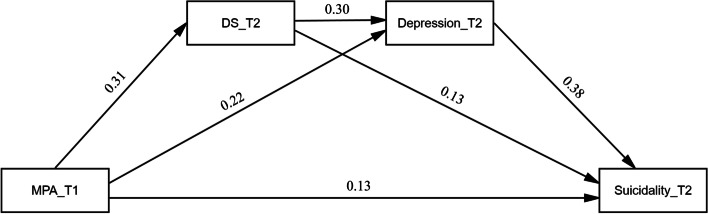
The chain mediation model
The pathways between the main variables are shown in Table 4 and Fig. 1. The total standardized effect of the three variables on the outcome variable of suicidality was 0.29 (95% CI [0.24, 0.34], F = 146.12, p < 0.001). Mobile phone addiction at T1 was significantly directly related to suicidality at T2 (β = 0.13; 95%CI: 0.08–0.17; p < 0.001). Additionally, Mobile phone addiction had indirect effects on suicidality at T2 through daytime sleepiness (β = 0.04, SE = 0.01, 95%CI = 0.02–0.06), and depression (β = 0.08, SE = 0.01, 95%CI = 0.06–0.11) respectively. Furthermore, mediation paths of mobile phone addiction → daytime sleepiness → depression → suicidality (β = 0.04, SE = 0.01, 95%CI = 0.03–0.05) was also identified by the mediation analyses.
Table 4.
Results of the Chain Mediating Effect with daytime sleepiness and depression as mediators between mobile phone addiction and suicidality
| Path | Effect | SE | p | 95% CI |
|---|---|---|---|---|
| MPA_T1(X) → DS_T2(M1) → Depression_T2(M2) → Suicidality_T2(Y) | ||||
| Total effect of X on Y | 0.289 | 0.024 | < 0.001 | 0.242–0.336 |
| Direct effect of X on Y | 0.129 | 0.023 | < 0.001 | 0.083–0.174 |
| Indirect effect of X on Y(Total) | 0.160 | 0.014 | - | 0.133–0.189 |
| Indirect effect of X on Y(Via M1) | 0.042 | 0.010 | - | 0.023–0.062 |
| Indirect effect of X on Y(Via M2) | 0.083 | 0.012 | - | 0.059–0.110 |
| Indirect effect of X on Y(Via M1 → M2) | 0.036 | 0.006 | - | 0.026–0.047 |
| X → M1 | 0.316 | 0.026 | < 0.001 | 0.265–0.367 |
| M1 → Y | 0.131 | 0.030 | < 0.001 | 0.073–0.189 |
| X → M2 | 0.218 | 0.027 | < 0.001 | 0.162–0.271 |
| M2 → Y | 0.381 | 0.035 | < 0.001 | 0.316–0.451 |
| M1 → M2 | 0.295 | 0.029 | < 0.001 | 0.238–0.353 |
Note. MPA Mobile phone addiction, DS Daytime sleepiness
Fig. 1.
The standardized path coefficients in chain mediation model. MPA_T1: Time 1 smartphone addiction score; DS_T2: Time 2 daytime sleepiness score; Depression_T2: Time 2 depression score; Suicidality_T2: Time 2 suicidality score
Stepwise linear regression analysis results
In our data, earlier mobile phone addiction could directly predict subsequent suicidal risk when controlling for age, gender, exposures, depressive symptoms and daytime sleepiness (β = 0.13, t = 5.60, ΔR2 = 0.015, p < 0.001) (see Table 5). Depression_T2 and daytime sleepiness_T2 were also significant risk factors for suicidality_T2 in the regression model, with depression showing the most statistical significance.
Table 5.
Stepwise regression of suicidal risk with age, gender, COVID-19 related exposure, daytime sleepiness, depressive symptoms, and MPAI in adolescents (N=1609)
| Independent variable | Step 1: Adjusted R2=0.001 |
Step 2: Adjusted R2= 0.003 |
Step 3: Adjusted R2= 0.244 |
Step 4: Adjusted R2= 0.259 |
|---|---|---|---|---|
| Beta | Beta | Beta | Beta | |
| Age | 0.019 | 0.019 | 0.021 | 0.021 |
| Gender | 0.026 | 0.025 | 0.006 | 0.004 |
| Someone in the community is infected | 0.010 | 0.008 | 0.011 | |
| A relative or friend is infected | -0.037 | -0.030 | -0.035 | |
| A relative or friend died from the infection | -0.025 | -0.018 | -0.019 | |
| Daytime sleepiness_T2 | 0.410*** | 0.381*** | ||
| Depression_T2 | 0.160*** | 0.130*** | ||
| MPAI_T1 | 0.130*** |
Abbreviations: MPA_T1 Time1 mobile phone addiction score, Daytime sleepiness _T2 Time 2 daytime sleepiness score, Depression_T2 Time 2 depression score
***p < 0.001
Discussion
This study is one of the few longitudinal studies that have examined the associations between mobile phone addiction and suicidality in adolescents during COVID-19. It was found that mobile phone addiction during the COVID-19 quarantine period could directly predict suicidality in the subsequent five months even after controlling for the effect of depression and daytime sleepiness. In addition, mediation analysis showed that mobile phone addiction during the COVID-19 quarantine period could indirectly predict suicidality in the following five months, with depression and daytime sleepiness mediating in this association.
Mobile phone addiction predicts suicidality regardless of mental health problems and other covariables
The regression analysis revealed that mobile phone addiction during the COVID-19 quarantine period could directly predict suicidality independent of covariables such as mental health and psychosocial factors in the subsequent five months. Several previous correlation studies supported this result. For example, Steinbüchel reported that 48.3% of the patients with Internet addiction (with and without comorbidity) exhibited significantly more often suicidal symptoms as compared to healthy controls (3.5%) [66]. Two nationally representative surveys of U.S. adolescents (N = 506,820) reported that among those who used electronic devices five or more hours a day, 48% had at least one suicide-related outcome [67]. Furthermore, the meta-analysis also found an increased risk of suicidal behavior in adolescents with internet addiction [68].
Our results confirmed and extended a previous cross-sectional study that internet overuse by children and adolescents in the context of COVID-19 could elevate their risks for self-injured behavior [69]. Actually, both the rate of phone addiction [70] and the risk of suicide [71, 72] among teenagers have risen dramatically during the pandemic although few studies, especially longitudinal design, confirmed the relationship between mobile phone overuse and subsequent suicide risk. Therefore, our study has important implications for considering the important role of mobile phone addiction when enacting suicide prevention programs for adolescents.
Mobile phone addiction has been related to various negative psychosocial consequences, which may contribute to subsequent suicidality. Schutten et al. reported that heavy media addiction was at risk for problematic behaviors such as substance abuse, overeating, problematic gambling, and poor financial management [73]. These unhealthy lifestyles would result in poor life performance, daily life function, social relationships, and academic or occupational achievements [74–76]. Furthermore, heavy screen-addicted adolescents were also found to have less social support and attachment with family and peers[77–79]. Poor social support would increase the risk of further isolation and loneliness, leading to suicidality [80–82].
In addition to the negative psychosocial consequences, mobile phones and internet addiction has been also associated to structural and functional abnormalities in brain areas related to cognitive control and emotional regulation. For example, Cheng and Liu found that internet addiction subjects had decreased negative functional connectivity (FC) between the dorsolateral prefrontal cortex (DLPFC) and amygdala [83], which is responsible for emotion-cognition interactions [84]. Turel et al. showed that Facebook users with addiction-like symptoms have a hyperactive amygdala-striatal system [85]. He et al. found that social network site addiction is associated with a more impulsive brain system, manifested through reduced gray matter volumes in the amygdala bilaterally [86]. Similarly, Dong et al. found that males with Internet addiction showed significantly greater ‘Stroop effect’-related activity in the anterior and posterior cingulate cortices than healthy males, indicating diminished efficiency of response-inhibition processes [87].
Depression was a mediator between mobile phone addiction and suicidality
The mediation analysis identified a pathway from mobile phone addiction to depression to suicidality, which confirmed the mediating role of depression in the association between mobile phone addiction and suicidality. This result was consistent with a previous cross-sectional study reporting that depression mediated the relationship between high-intensity mobile phone use and suicide-related behaviors in Chinese adolescents [33]. Depression has been one of the most commonly reported adverse psychological sequelae associated with mobile phone addiction, which is characterized by depressive moods, such as adolescent feelings of irritability or emptiness, diminished interest, loss of pleasure, feelings of hopelessness and worthlessness, changes in appetite or sleep, and reduced energy or fatigue.
Several reasons have been proposed for the pathogenesis of addiction-related depression. First, mobile phone addiction can lead to work or school performance impairments [88], which could induce criticism, blame, or arguments from teachers and family members, which could, in turn, lead to impaired social relationships, low self-esteem, and negative emotions, such as depression [29]. This may result in a more compulsive mobile phone use to escape these real-world problems and alleviate any negative emotions [30, 89]. Therefore, there seems to be a vicious cycle between mobile phone addiction and depression and subsequent suicidality risk [41]. As depression has long been recognized as one of the most critical risk factors for suicide prediction [45, 47], more attention needs to be paid to its presence when screening people with mobile phone addiction and the intervening suicidality. As it may be challenging to evaluate the severity of the negative influence of mobile phone addiction and when and how to implement an intervention, the presence of depression could be a valuable warning sign; that is, greater attention should be focused on adolescent mobile phone addicts who also have depressive symptoms.
Daytime sleepiness was a mediator between mobile phone addiction and suicidality
The mediation analysis indicated that mobile phone addiction was associated with suicidality, and daytime sleepiness mediated this association. Daytime sleepiness, defined as the inability to maintain wakefulness and alertness during the day [48], is one of the most common sleep disturbance sequelae [49]. Adolescents with mobile phone addiction tend to spend more time on their mobile phones at night, which often leads to decreased sleep duration and circadian rhythm disturbances from the mobile phone’s light and electromagnetic fields that can negatively influence serum melatonin and cerebral blood flow [90–92]. Extensive mobile phone use can also result in frequent headaches, tension, fatigue, and vertigo [93], resulting in sleep disturbances.
Sleep disturbance has also been identified as a risk factor for suicidality [94]. For example, a recent two-year follow-up study found that shorter sleep duration at the baseline was associated with an increased suicidality risk in school-aged boys [95], and another longitudinal analysis found that short sleep durations predicted the onset or persistence of suicidal ideation [96]. One possible mechanism for this association may be that sleep deprivation and circadian disturbances compromise frontal lobe/executive functions, diminish problem-solving abilities, and increase impulsive behavior, increasing the likelihood of suicide [97]. Insufficient sleep can also lead to mood regulation impairments and improve suicide ideation [98] and has been associated with hypothalamus/hypothalamic–pituitary–adrenal (HPA) axis dysregulation, which has been linked to depression and suicidality risk [99–101].
Daytime sleepiness has been strongly associated with sleep disturbance, which is more directly associated with daytime dysfunction compared to sleep disturbance. This study identified the mediating role of daytime sleepiness on the association between mobile phone addiction and suicidality. Although these are only preliminary results, they highlight that it is essential to monitor daytime sleepiness carefully, especially in adolescents with mobile phone addiction.
Daytime sleepiness and depression as chain mediation between mobile phone addiction and suicidality
Our study adds to previous research showing that mobile phone addiction could affect daytime sleepiness which contributes to depressive symptoms, and subsequently increases the risk of suicide. This chain mediating effects highlights daytime sleepiness may be a precursor to depressive symptoms, especially among teenagers who are heavily exposed to mobile phone use. Our results were partly consistent with a previous Korean study indicating that insufficient sleep time and feeling sleepy during the day in adolescence was significantly associated with depression [102]. Therefore, monitoring sleep duration in adolescents and reducing daytime dozing may effectively reducing depressive symptoms, which in turn may lower the risk of suicide. The mechanism between daytime sleepiness and depressive symptoms may require more research to explore, such as longitudinal studies and a combination of biological and neuroscience research methods.
Limitations, strengths, and future directions
One of our strengths is the use of follow-up design to explore how mobile phone addiction predicts later suicide risk in a representative adolescent sample. The current study added further and reliable evidence for the relationship between adolescent behavior addiction and suicide risk, and provided evidence and reference for further intervention. There were several limitations in the present study. First, the study sample was recruited in areas classified as moderate risk COVID-19 prevalence areas, which means that the results are not necessarily applicable to adolescents in other areas. Second, the psychological variables investigated in the present study were limited; therefore, future studies could include more variables such as sleep disorders, anxiety, interpersonal relationships, and acute stress. Third, as no participant information was gathered before the pandemic, the pre-COVID mobile phone use, daytime sleepiness, depression, and suicidality were unknown. Fourth, since this study uses a self-assessment questionnaire, the subjective deviation is inevitable. More reliable tools such as face-to-face interviews or objective indicators are needed in future research. Fifth, because depression is positively correlated with daytime sleepiness, it is difficult to explore the causal relationship between the two because it is cross-sectional data, and future studies need to explore the causal connection in a longitudinal design. Finally, as the period between the two waves was relatively short, longitudinal studies over more extended periods and different survey waves would provide a more transparent, long-term picture.
Conclusion and implications
This study was one of the few studies that have examined the prospective associations between mobile phone addiction and suicidality in a short-term longitudinal study during COVID-19 in a large cohort of adolescents. The key findings were that mobile phone addiction during the COVID-19 quarantine period could, directly and indirectly, predict suicidality five months later when the pandemic was in remission. Depression and daytime sleepiness plays a mediating role in linking mobile phone addiction and suicidality. These findings confirmed the importance of long-term regular monitoring of suicide risk, depression, and daytime sleepiness in adolescents with mobile phone addiction. Long-term psychosocial care or support is needed for vulnerable adolescents with depression, and daytime sleepiness, as these could be warning signs for suicide risk detection, prevention, and intervention.
Acknowledgements
The authors wish to thank all study participants and all research collaborators.
Authors’ contributions
Wanjie Tang designed the study; Gangqin Li, Changjian Qiu, and Wanjie Tang wrote the main manuscript text, and Aldo Conti prepared Fig. 1 and Tables. All authors reviewed the manuscript.
Funding
This research was supported by grants from the China Postdoctoral Science Foundation (2018M643488) and the National Natural Science Foundation of China (81901928).
Availability of data and materials
Data could be obtained from the corresponding authors upon reasonable request.
Declarations
Ethics approval and consent to participate
The authors assert that all procedures contributing to this work comply with the ethical standards of the Ethics Committee of Sichuan Psychological Society (NO. 2020_12) on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The informed consent was obtained from all the participants and their caregivers prior to the study.
Competing interests
All authors have no conflict of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Changjian Qiu, Email: qiuchangjian@wchscu.cn.
Wanjie Tang, Email: wanjie.tang@kcl.ac.uk.
References
- 1.Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, Lane HC, Memish Z, Oh Md, Sall AA, et al. COVID-19: towards controlling of a pandemic. The Lancet. 2020;395(10229):1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang N, Yang S, Jia P. Cultivating resilience during the COVID-19 pandemic: A socioecological perspective. Annual Review of Psychology. 2022;73:575–598. doi: 10.1146/annurev-psych-030221-031857. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Mendez R, Díaz M. Volunteers’ compassion fatigue, compassion satisfaction, and post-traumatic growth during the SARS-CoV-2 lockdown in Spain: Self-compassion and self-determination as predictors. PLoS ONE. 2021;16(9):e0256854. doi: 10.1371/journal.pone.0256854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J, Zhan D, Zhou Y, Gao X. Loneliness and problematic mobile phone use among adolescents during the COVID-19 pandemic: The roles of escape motivation and self-control. Addict Behav. 2021;118:106857. doi: 10.1016/j.addbeh.2021.106857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masaeli N, Farhadi H. Prevalence of Internet-based addictive behaviors during COVID-19 pandemic: A systematic review. J Addict Dis. 2021;39(4):468–488. doi: 10.1080/10550887.2021.1895962. [DOI] [PubMed] [Google Scholar]
- 6.Duan L, He J, Li M, Dai J, Zhou Y, Lai F, Zhu G. Based on a Decision Tree Model for Exploring the Risk Factors of Smartphone Addiction Among Children and Adolescents in China During the COVID-19 Pandemic. Front Psych. 2021;12:897. doi: 10.3389/fpsyt.2021.652356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chauhan N, Patra S, Bhargava R, Srivastava C, Gujar KV, Gupta N, Seshadri S. Exposure to smartphone and screen media in children and adolescents and COVID-19 pandemic. Journal of Indian Association for Child and Adolescent Mental Health-ISSN 0973–1342. 2021;7(2):219–229. doi: 10.1177/0973134220210215. [DOI] [Google Scholar]
- 8.Fernandes B, Uzun B, Aydin C, Tan-Mansukhani R, Vallejo A, Saldaña-Gutierrez A, Biswas UN, Essau CA. Internet use during COVID-19 lockdown among young people in low-and middle-income countries: Role of psychological wellbeing. Addictive Behaviors Reports. 2021;14:100379. doi: 10.1016/j.abrep.2021.100379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, McKyer ELJ, Ahmed HU, Ma P. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 11.Li S, Wang Y, Xue J, Zhao N, Zhu T. The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: A Study on Active Weibo Users. Int J Environ Res Public Health. 2020;17(6):2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Twenge JM, Joiner TE. US Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. 2020;37(10):954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. doi: 10.1016/j.sleep.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fitzpatrick KM, Harris C, Drawve G. How bad is it? Suicidality in the middle of the COVID-19 pandemic. Suicide and Life-Threatening Behavior. 2020;50(6):1241–1249. doi: 10.1111/sltb.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoekstra PJ. Suicidality in children and adolescents: lessons to be learned from the COVID-19 crisis. Eur Child Adolesc Psychiatry. 2020;29:737–738. doi: 10.1007/s00787-020-01570-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fountoulakis KN, Apostolidou MK, Atsiova MB, Filippidou AK, Florou AK, Gousiou DS, Katsara AR, Mantzari SN, Padouva-Markoulaki M, Papatriantafyllou EI. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J Affect Disord. 2021;279:624–629. doi: 10.1016/j.jad.2020.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allan NP, Volarov M, Koscinski B, Pizzonia KL, Potter K, Accorso C, Saulnier KG, Ashrafioun L, Stecker T, Suhr J. Lonely, anxious, and uncertain: critical risk factors for suicidal desire during the COVID-19 pandemic. Psychiatry Res. 2021;304:114144. doi: 10.1016/j.psychres.2021.114144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.John A, Pirkis J, Gunnell D, Appleby L, Morrissey J. Trends in suicide during the covid-19 pandemic. BMJ. 2020;371:m4352. doi: 10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]
- 20.Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, Khan M, O'Connor RC, Pirkis J, Appleby L, et al. Suicide risk and prevention during the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(6):468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sher L. Suicide research and prevention during and after the COVID-19 pandemic. Acta Psychiatr Scand. 2020;142(5):353–354. doi: 10.1111/acps.13248. [DOI] [PubMed] [Google Scholar]
- 22.Que J, Yuan K, Gong Y, Meng S, Bao Y, Lu L. Raising awareness of suicide prevention during the COVID-19 pandemic. Neuropsychopharmacol Rep. 2020;40(4):392–395. doi: 10.1002/npr2.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Every-Palmer S, Jenkins M, Gendall P, Hoek J, Beaglehole B, Bell C, Williman J, Rapsey C, Stanley J. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: A cross-sectional study. PLoS ONE. 2020;15(11):e0241658. doi: 10.1371/journal.pone.0241658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Czeisler ME, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24–30, 2020. Mmwr-Morbidity and Mortality Weekly Report. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ayuso-Mateos JL, Morillo D, Haro JM, Olaya B, Lara E, Miret M. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol Psychiatr Sci. 2021;30:e49. doi: 10.1017/S2045796021000408. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26.Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawton K, Saunders KEA, O'Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379(9834):2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- 28.Picazo-Zappino J. Suicide among children and adolescents: a review. Actas Espanolas De Psiquiatria. 2014;42(3):125–132. [PubMed] [Google Scholar]
- 29.Billieux J, Maurage P, Lopez-Fernandez O, Kuss DJ, Griffiths MD. Can Disordered Mobile Phone Use Be Considered a Behavioral Addiction? An Update on Current Evidence and a Comprehensive Model for Future Research. Curr Addict Rep. 2015;2(2):156–162. doi: 10.1007/s40429-015-0054-y. [DOI] [Google Scholar]
- 30.Elhai JD, Levine JC, Dvorak RD, Hall BJ. Non-social features of smartphone use are most related to depression, anxiety and problematic smartphone use. Comput Hum Behav. 2017;69:75–82. doi: 10.1016/j.chb.2016.12.023. [DOI] [Google Scholar]
- 31.El-Sayed Desouky D, Abu-Zaid H. Mobile phone use pattern and addiction in relation to depression and anxiety. East Mediterr Health J. 2020;26(6):692–699. doi: 10.26719/emhj.20.043. [DOI] [PubMed] [Google Scholar]
- 32.Billieux J. Problematic Use of the Mobile Phone: A Literature Review and a Pathways Model. Current Psychiatry Reviews. 2012;8(4):299–307. doi: 10.2174/157340012803520522. [DOI] [Google Scholar]
- 33.Chen RS, Liu JB, Cao XL, Duan SQ, Wen SY, Zhang SM, Xu JC, Lin L, Xue ZP, Lu JP. The relationship between mobile phone use and suicide -related behaviors among adolescents: The mediating role of depression and interpersonal problems. J Affect Disorders. 2020;269:101–107. doi: 10.1016/j.jad.2020.01.128. [DOI] [PubMed] [Google Scholar]
- 34.Ismail WSW, Sim ST, Tan KA, Bahar N, Ibrahim N, Mahadevan R, Jaafar NRN, Baharudin A, Aziz MA. The relations of internet and smartphone addictions to depression, anxiety, stress, and suicidality among public university students in Klang Valley. Malaysia Perspectives in Psychiatric Care. 2020;56(4):949–955. doi: 10.1111/ppc.12517. [DOI] [PubMed] [Google Scholar]
- 35.Mahamid FA, Berte DZ, Bdier D. Problematic internet use and its association with sleep disturbance and life satisfaction among Palestinians during the COVID-19 pandemic. Curr Psychol. 2021:1–8. 10.1007/s12144-021-02124-5. [DOI] [PMC free article] [PubMed]
- 36.Song Y, Sznajder K, Cui C, Yang Y, Li Y, Yang X. Anxiety and its relationship with sleep disturbance and problematic smartphone use among Chinese medical students during COVID-19 home confinement—A structural equation model analysis. J Affect Disord. 2022;296:315–321. doi: 10.1016/j.jad.2021.09.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oliveira T, Costa D, Alvim-Soares A, de Paula J, Kestelman I, Silva A, Malloy-Diniz L, Miranda D. Children's behavioral problems, screen time, and sleep problems' association with negative and positive parenting strategies during the COVID-19 outbreak in Brazil. Child Abuse Negl. 2022;130:105345. doi: 10.1016/j.chiabu.2021.105345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents' Electronic Media Use at Night, Sleep Disturbance, and Depressive Symptoms in the Smartphone Age. J Youth Adolesc. 2015;44(2):405–418. doi: 10.1007/s10964-014-0176-x. [DOI] [PubMed] [Google Scholar]
- 39.Demirci K, Akgonul M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict. 2015;4(2):85–92. doi: 10.1556/2006.4.2015.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thomee S, Harenstam A, Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults - a prospective cohort study. Bmc Public Health. 2011;11:66. doi: 10.1186/1471-2458-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elhai JD, Dvorak RD, Levine JC, Hall BJ. Problematic smartphone use: A conceptual overview and systematic review of relations with anxiety and depression psychopathology. J Affect Disorders. 2017;207:251–259. doi: 10.1016/j.jad.2016.08.030. [DOI] [PubMed] [Google Scholar]
- 42.Ibrahim NK, Baharoon BS, Banjar WF, Jar AA, Ashor RM, Aman AA, Al-Ahmadi JR. Mobile Phone Addiction and Its Relationship to Sleep Quality and Academic Achievement of Medical Students at King Abdulaziz University, Jeddah, Saudi Arabia. J Res Health Sci. 2018;18(3):e00420. [PMC free article] [PubMed] [Google Scholar]
- 43.Liu QQ, Zhou ZK, Yang XJ, Kong FC, Niu GF, Fan CY. Mobile phone addiction and sleep quality among Chinese adolescents: A moderated mediation model. Comput Hum Behav. 2017;72:108–114. doi: 10.1016/j.chb.2017.02.042. [DOI] [Google Scholar]
- 44.Sahin S, Ozdemir K, Unsal A, Temiz N. Evaluation of mobile phone addiction level and sleep quality in university students. Pakistan Journal of Medical Sciences. 2013;29(4):913–918. doi: 10.12669/pjms.294.3686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Omary A. National Prevalence Rates of Suicidal Ideation and Suicide Attempts Among Adults With and Without Depression. Journal of Nervous and Mental Disease. 2021;209(5):378–385. doi: 10.1097/NMD.0000000000001309. [DOI] [PubMed] [Google Scholar]
- 46.Hardy P. Severe depression : morbidity-mortality and suicide. Encephale-Revue De Psychiatrie Clinique Biologique Et Therapeutique. 2009;35(7):S269–S271. doi: 10.1016/S0013-7006(09)73484-0. [DOI] [PubMed] [Google Scholar]
- 47.Ribeiro JD, Huang XY, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Brit J Psychiat. 2018;212(5):279–286. doi: 10.1192/bjp.2018.27. [DOI] [PubMed] [Google Scholar]
- 48.Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–1394. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 49.Cerniglia L, Zoratto F, Cimino S, Laviola G, Ammaniti M, Adriani W. Internet Addiction in adolescence: Neurobiological, psychosocial and clinical issues. Neurosci Biobehav Rev. 2017;76(Pt A):174–184. doi: 10.1016/j.neubiorev.2016.12.024. [DOI] [PubMed] [Google Scholar]
- 50.Guo W, Tao Y, Li X, Lin X, Meng Y, Yang X, Wang H, Zhang Y, Tang W, Wang Q. Associations of internet addiction severity with psychopathology, serious mental illness, and suicidality: large-sample cross-sectional study. J Med Internet Res. 2020;22(8):e17560. doi: 10.2196/17560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jasso-Medrano JL, Lopez-Rosales F. Measuring the relationship between social media use and addictive behavior and depression and suicide ideation among university students. Comput Hum Behav. 2018;87:183–191. doi: 10.1016/j.chb.2018.05.003. [DOI] [Google Scholar]
- 52.Chen R, Liu J, Cao X, Duan S, Wen S, Zhang S, Xu J, Lin L, Xue Z, Lu J. The relationship between mobile phone use and suicide-related behaviors among adolescents: the mediating role of depression and interpersonal problems. J Affect Disord. 2020;269:101–107. doi: 10.1016/j.jad.2020.01.128. [DOI] [PubMed] [Google Scholar]
- 53.Yu Y, Yang X, Wang S, Wang H, Chang R, Tsamlag L, Zhang S, Xu C, Yu X, Cai Y. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai. China BMC psychiatry. 2020;20(1):1–9. doi: 10.1186/s12888-019-2374-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roussos A, Goenjian AK, Steinberg AM, Sotiropoulou C, Kakaki M, Kabakos C, Karagianni S, Manouras V. Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia. Greece American Journal of Psychiatry. 2005;162(3):530–537. doi: 10.1176/appi.ajp.162.3.530. [DOI] [PubMed] [Google Scholar]
- 55.Tang WJ, Zhao JD, Lu Y, Zha YL, Liu H, Sun Y, Zhang J, Yang YC, Xu JP. Suicidality, posttraumatic stress, and depressive reactions after earthquake and maltreatment: A cross-sectional survey of a random sample of 6132 chinese children and adolescents. J Affect Disorders. 2018;232:363–369. doi: 10.1016/j.jad.2018.02.081. [DOI] [PubMed] [Google Scholar]
- 56.Huang H, Niu L, Zhou C, Wu H. Reliability and validity of mobile phone addiction index for Chinese college students. Chin J Clin Psychol. 2014;22(5):835–838. [Google Scholar]
- 57.Bianchi A, Phillips JG. Psychological predictors of problem mobile phone use. Cyberpsychol Behav. 2005;8(1):39–51. doi: 10.1089/cpb.2005.8.39. [DOI] [PubMed] [Google Scholar]
- 58.Liu X, Yang Y, Liu Z, Chen H, Fan F, Jia C. Psychometric assessment of the Chinese adolescent daytime sleepiness scale (CADSS) Sleep Biol Rhythms. 2017;15(3):207–216. doi: 10.1007/s41105-017-0106-x. [DOI] [Google Scholar]
- 59.LeBlanc JC, Almudevar A, Brooks SJ, Kutcher S. Screening for adolescent depression: comparison of the Kutcher Adolescent Depression Scale with the Beck depression inventory. J Child Adolesc Psychopharmacol. 2002;12(2):113–126. doi: 10.1089/104454602760219153. [DOI] [PubMed] [Google Scholar]
- 60.Shun CM, Jane CH, Jung SW, Nan LC, Cheng KC, Che HW, Sheue CY, Ping CH, Pesus C. A rapid screening test for depression in junior high school children. J Chin Med Assoc. 2011;74(8):363–368. doi: 10.1016/j.jcma.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 61.Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8(4):443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- 62.Fang Q, Freedenthal S, Osman A. Validation of the Suicide Resilience Inventory-25 with American and Chinese College Students. Suicide Life Threat Behav. 2015;45(1):51–64. doi: 10.1111/sltb.12108. [DOI] [PubMed] [Google Scholar]
- 63.Hayes AF, Montoya AK, Rockwood NJ. The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Australas Mark J. 2017;25(1):76–81. doi: 10.1016/j.ausmj.2017.02.001. [DOI] [Google Scholar]
- 64.DiCiccio TJ, Efron B. Bootstrap confidence intervals. Stat Sci. 1996;11(3):189–228. doi: 10.1214/ss/1032280214. [DOI] [Google Scholar]
- 65.Martin MA, Roberts S. An evaluation of bootstrap methods for outlier detection in least squares regression. J Appl Stat. 2006;33(7):703–720. doi: 10.1080/02664760600708863. [DOI] [Google Scholar]
- 66.Steinbuchel TA, Herpertz S, Dieris-Hirche J, Kehyayan A, Kulpmann I, Diers M, Te Wildt BT. Internet Addiction and Suicidality - A Comparison of Internet-Dependent and Non-Dependent Patients with Healthy Controls. Psychother Psychosom Med Psychol. 2020;70(11):457–466. doi: 10.1055/a-1129-7246. [DOI] [PubMed] [Google Scholar]
- 67.Twenge JM, Joiner TE, Rogers ML, Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science. 2017;6(1):3–17. doi: 10.1177/2167702617723376. [DOI] [Google Scholar]
- 68.Wang J, Hao Q-H, Tu Y, Peng W, Wang Y, Li H, Zhu T-M. Assessing the Association Between Internet Addiction Disorder and Health Risk Behaviors Among Adolescents and Young Adults: A Systematic Review and Meta-Analysis. Front Public Health. 2022;10:809232. doi: 10.3389/fpubh.2022.809232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Deslandes SF, Coutinho T. The intensive use of the internet by children and adolescents in the context of COVID-19 and the risks for self-inflicted violence. Ciencia & saude coletiva. 2020;25:2479–2486. doi: 10.1590/1413-81232020256.1.11472020. [DOI] [PubMed] [Google Scholar]
- 70.Marengo D, Fabris MA, Longobardi C, Settanni M. Smartphone and social media use contributed to individual tendencies towards social media addiction in Italian adolescents during the COVID-19 pandemic. Addict Behav. 2022;126:107204. doi: 10.1016/j.addbeh.2021.107204. [DOI] [PubMed] [Google Scholar]
- 71.Fortgang RG, Wang SB, Millner AJ, Reid-Russell A, Beukenhorst AL, Kleiman EM, Bentley KH, Zuromski KL, Al-Suwaidi M, Bird SA. Increase in suicidal thinking during COVID-19. Clinical Psychological Science. 2021;9(3):482–488. doi: 10.1177/2167702621993857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Plener PL. COVID-19 and nonsuicidal self-injury: the pandemic's influence on an adolescent epidemic. Am J Public Health. 2021;111(2):195–196. doi: 10.2105/AJPH.2020.306037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schutten D, Stokes KA, Arnell KM. I want to media multitask and I want to do it now: Individual differences in media multitasking predict delay of gratification and system-1 thinking. Cogn Res. 2017;2(1):8. doi: 10.1186/s41235-016-0048-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Leung L, Lee PSN. Impact of Internet Literacy, Internet Addiction Symptoms, and Internet Activities on Academic Performance. Soc Sci Comput Rev. 2012;30(4):403–418. doi: 10.1177/0894439311435217. [DOI] [Google Scholar]
- 75.Saraei F, Ebrahimi ME, Paydar MRZ. Relationship between Internet Addiction, Mental Health, and Academic Performance among Adolescents 15 to 18 Years Referred to Cafe-Net in Hamedan-Iran. Life Sci J. 2013;10(1):1260–1267. [Google Scholar]
- 76.Nalwa K, Anand AP. Internet addiction in students: a cause of concern. Cyberpsychol Behav. 2003;6(6):653–656. doi: 10.1089/109493103322725441. [DOI] [PubMed] [Google Scholar]
- 77.Wu XS, Zhang ZH, Zhao F, Wang WJ, Li YF, Bi LD, Qian ZZ, Lu SS, Feng F, Hu CY, et al. Prevalence of Internet addiction and its association with social support and other related factors among adolescents in China. J Adolescence. 2016;52:103–111. doi: 10.1016/j.adolescence.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 78.Pea R, Nass C, Meheula L, Rance M, Kumar A, Bamford H, Nass M, Simha A, Stillerman B, Yang S, et al. Media Use, Face-to-Face Communication, Media Multitasking, and Social Well-Being Among 8- to 12-Year-Old Girls. Dev Psychol. 2012;48(2):327–336. doi: 10.1037/a0027030. [DOI] [PubMed] [Google Scholar]
- 79.Richards R, McGee R, Williams SM, Welch D, Hancox RJ. Adolescent Screen Time and Attachment to Parents and Peers. Arch Pediat Adol Med. 2010;164(3):258–262. doi: 10.1001/archpediatrics.2009.280. [DOI] [PubMed] [Google Scholar]
- 80.Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, Pallesen S. The Relationship Between Addictive Use of Social Media and Video Games and Symptoms of Psychiatric Disorders: A Large-Scale Cross-Sectional Study. Psychol Addict Behav. 2016;30(2):252–262. doi: 10.1037/adb0000160. [DOI] [PubMed] [Google Scholar]
- 81.Boniel-Nissim M, Tabak I, Mazur J, Borraccino A, Brooks F, Gommans R, van der Sluijs W, Zsiros E, Craig W, Harel-Fisch Y, et al. Supportive communication with parents moderates the negative effects of electronic media use on life satisfaction during adolescence. Int J Public Health. 2015;60(2):189–198. doi: 10.1007/s00038-014-0636-9. [DOI] [PubMed] [Google Scholar]
- 82.Mentzoni RA, Brunborg GS, Molde H, Myrseth H, Skouveroe KJM, Hetland J, Pallesen S. Problematic Video Game Use: Estimated Prevalence and Associations with Mental and Physical Health. Cyberpsych Beh Soc N. 2011;14(10):591–596. doi: 10.1089/cyber.2010.0260. [DOI] [PubMed] [Google Scholar]
- 83.Cheng HW, Liu J. Alterations in Amygdala Connectivity in Internet Addiction Disorder. Sci Rep-Uk. 2020;10(1):2370. doi: 10.1038/s41598-020-59195-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pessoa L. On the relationship between emotion and cognition. Nat Rev Neurosci. 2008;9(2):148–158. doi: 10.1038/nrn2317. [DOI] [PubMed] [Google Scholar]
- 85.Turel O, He Q, Xue G, Xiao L, Bechara A. Examination of neural systems sub-serving facebook "addiction". Psychol Rep. 2014;115(3):675–695. doi: 10.2466/18.PR0.115c31z8. [DOI] [PubMed] [Google Scholar]
- 86.He QH, Turel O, Brevers D, Bechara A. Excess social media use in normal populations is associated with amygdala-striatal but not with prefrontal morphology. Psychiat Res-Neuroim. 2017;269:31–35. doi: 10.1016/j.pscychresns.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 87.Dong G, Devito EE, Du X, Cui Z. Impaired inhibitory control in 'internet addiction disorder': a functional magnetic resonance imaging study. Psychiatry Res. 2012;203(2–3):153–158. doi: 10.1016/j.pscychresns.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vahedi Z, Saiphoo A. The association between smartphone use, stress, and anxiety: A meta-analytic review. Stress Health. 2018;34(3):347–358. doi: 10.1002/smi.2805. [DOI] [PubMed] [Google Scholar]
- 89.Kardefelt-Winther D. A conceptual and methodological critique of internet addiction research: Towards a model of compensatory internet use. Comput Hum Behav. 2014;31:351–354. doi: 10.1016/j.chb.2013.10.059. [DOI] [Google Scholar]
- 90.Shrivastava A, Saxena Y. Effect of mobile usage on serum melatonin levels among medical students. Indian J Physiol Pharmacol. 2014;58(4):395–399. [PubMed] [Google Scholar]
- 91.Loughran SP, Wood AW, Barton JM, Croft RJ, Thompson B, Stough C. The effect of electromagnetic fields emitted by mobile phones on human sleep. NeuroReport. 2005;16(17):1973–1976. doi: 10.1097/01.wnr.0000186593.79705.3c. [DOI] [PubMed] [Google Scholar]
- 92.Aalto S, Haarala C, Bruck A, Sipila H, Hamalainen H, Rinne JO. Mobile phone affects cerebral blood flow in humans. J Cereb Blood Flow Metab. 2006;26(7):885–890. doi: 10.1038/sj.jcbfm.9600279. [DOI] [PubMed] [Google Scholar]
- 93.Al-Khlaiwi T, Meo SA. Association of mobile phone radiation with fatigue, headache, dizziness, tension and sleep disturbance in Saudi population. Saudi Med J. 2004;25(6):732–736. [PubMed] [Google Scholar]
- 94.Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep Disturbances as an Evidence-Based Suicide Risk Factor. Curr Psychiatry Rep. 2015;17(3):554. doi: 10.1007/s11920-015-0554-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gong QH, Li SX, Wang SJ, Li H, Han LY. Sleep and suicidality in school-aged adolescents: A prospective study with 2-year follow-up. Psychiatry Res. 2020;287:112918. doi: 10.1016/j.psychres.2020.112918. [DOI] [PubMed] [Google Scholar]
- 96.Wang D, Ross B, Zhou X, Meng D, Zhu Z, Zhao J, Fan F, Liu X. Sleep disturbance predicts suicidal ideation during COVID-19 pandemic: A two-wave longitudinal survey. J Psychiatr Res. 2021;143:350–356. doi: 10.1016/j.jpsychires.2021.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Perlisa ML, Grandnerd MA, Chakravorty S, Bernertf RA, Browng GK, Thaseh ME. Suicide and sleep: Is it a bad thing to be awake when reason sleeps? Sleep Med Rev. 2016;29:101–107. doi: 10.1016/j.smrv.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sarchiapone M, Mandelli L, Carli V, Iosue M, Wasserman C, Hadlaczky G, Hoven CW, Apter A, Balazs J, Bobes J, et al. Hours of sleep in adolescents and its association with anxiety, emotional concerns, and suicidal ideation. Sleep Med. 2014;15(2):248–254. doi: 10.1016/j.sleep.2013.11.780. [DOI] [PubMed] [Google Scholar]
- 99.Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. Journal of Endocrinology and Metabolism. 2005;90(5):3106–3114. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- 100.Bao AM, Meynen G, Swaab DF. The stress system in depression and neurodegeneration: focus on the human hypothalamus. Brain Res Rev. 2008;57(2):531–553. doi: 10.1016/j.brainresrev.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 101.Kirkcaldy BD, Eysenck MW, Siefen GR. Psychological and social predictors of suicidal ideation among young adolescents. Sch Psychol Int. 2004;25(3):301–316. doi: 10.1177/0143034304046903. [DOI] [Google Scholar]
- 102.Yang B, Choe K, Park Y, Kang Y. Associations among daytime sleepiness, depression and suicidal ideation in Korean adolescents. Int J Adolesc Med Health. 2019;31(2). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data could be obtained from the corresponding authors upon reasonable request.