Dear Editor,
There has been a growing interest in the actual spreadability of the injected drugs through novel and diverse modalities, such as the erector spinae plane block, quadratus lumborum block, and serratus plane block, etc. used for pain relief. For evaluation of the actual spread of the injectant, imaging techniques such as X-ray, computed tomography, and magnetic resonance imaging with contrast agents have been utilized traditionally.
Recently, the ultrasound has been recognized as more reliable than other devices for precisely guiding the needle tip to the targeted structure for injection or nerve blockade. Thus, it has been applied to a number of cadaveric studies for estimating the spreadability of the injection using solutions blended with dyes. In these studies, the stabbing feeling associated with the needle, injection speed, and absorption of drugs, etc. may show variable results in different conditions between cadavers and living patients. In addition, the viscosity of the injected solution may also affect their final results. Therefore, the results are different from the actual clinical practice.
In the previous cadaveric studies, diverse solutions have been utilized for the injection: a solution mixed with 0.9% normal saline, methylene blue, and gadopentetate dimeglumine,1 a mixture with distilled water, latex, and green colored dye,2 a mixture with 0.5% methylene blue, latex, and black colored ink,3 and a mixture with 0.5% methylcellulose and India ink.4 However, these solutions have some limitations, such as leakage and stickiness associated with the dissection, and some of these materials are likely to be expensive. For overcoming these limitations, some previous studies recommended gelatin as an option.5 Gelatin is a derived protein obtained from collagen, a natural protein, characterized by dissolving above a certain temperature (37 °C) and re-coagulating when cooled. The shape of gelatin can be maintained after its spread, which is the reason why gelatin is suitable for estimating the distribution and volume of the injected solution. However, the detailed description about formulating the solution using gelatin or the process of injecting is lacking in the previous studies. Thus, we would like to introduce the actual processes of manufacturing and injecting the solution used in our laboratory, which are as follows.
Preparation:
Gelatin (available regardless of any brand) / Tap water / Blue colored ink (any brand) / 80-mm × 20G echogenic Tuohy needle (any brand) / Syringe (adequate volume for study) / Beaker / Water bath / Hot plate with temperature control / Hot towel / Ice bag / Ultrasound device (any brand).
Processes of manufacturing the solution (Figure 1) and confirming the status:
-
1)
Blend the gelatin with the tap water in 1:1 volume ratio in a small beaker.
-
2)
Fill a water bath and place it a hot plate.
-
3)
Place the beaker having the mixture and thermometer in the water bath.
-
4)
Check the complete dissolution of the mixture with temperature held constant between 40 °C and 45 °C (boiling gelatin mixture can destroy tissue structures during injection).
-
5)
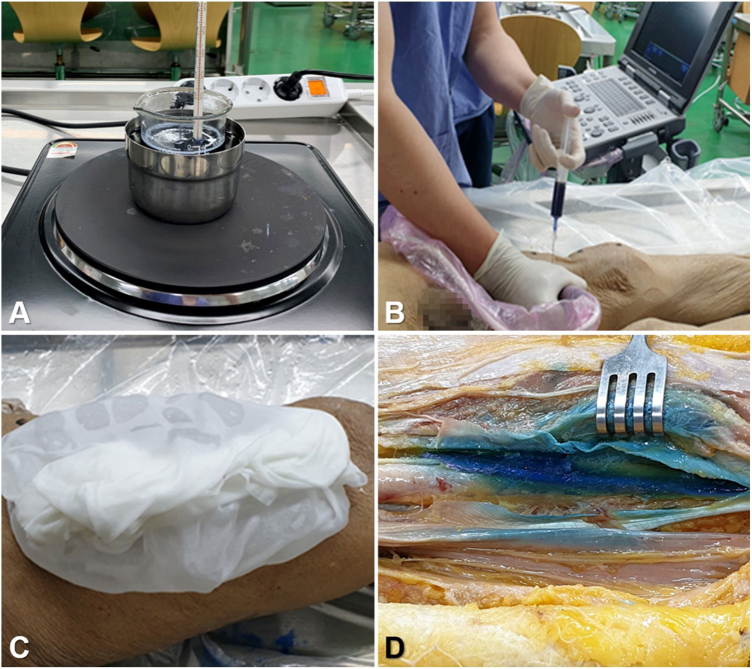
Blend the melted mixture with moderate amount of blue colored ink (Figure 2A) and place a drop or two on ice for checking its coagulability and the depth of shade.
-
6)
Apply a hot towel to the target area of cadaver before the US-guided injection for 5 minutes, for preventing unexpected coagulation of gelatin.
-
7)
Inject the gelatin solution slowly using Tuohy needle, monitoring the US image to determine whether the solution is working as expected (Figure 2B).
-
8)
Wait for 1–2 min after injection and apply the prepared ice bag to the target area of cadaver for the complete coagulation of gelatin (Figure 2C).
-
9)
Confirm the volume and area of spread of the injectant through fine dissection by the anatomy expert (Figure 2D).
Figure 1.
A diagram for showing processes of manufacturing the gelatin solution.
Figure 2.
Pictures for showing each step for real practice using gelatin. (A) Applying heat to the gelatin mixture, (B) US-guided injection of gelatin solution by pain physician, (C) Freezing with ice on injected area, (D) Fine dissection and confirmation by the anatomy expert.
In conclusion, we anticipate that this protocol would encourage pain physicians to develop a new injection technique and to reveal the associated anatomical relationship.
Conflicts of interest
The authors declare no conflicts of interest.
Contributor Information
Yeon-Dong Kim, Email: kydpain@hanmail.net.
Hyung-Sun Won, Email: hswon01@wku.ac.kr.
References
- 1.Adhikary S.D., Bernard S., Lopez H., Chin K.J. Erector spinae plane block versus retrolaminar block: A magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43:756–762. doi: 10.1097/AAP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 2.Yang H.M., Choi Y.J., Kwon H.J., O J, Cho T.H., Kim S.H. Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia. 2018;73:1244–1250. doi: 10.1111/anae.14408. [DOI] [PubMed] [Google Scholar]
- 3.Mayes J., Davison E., Panahi P., et al. An anatomical evaluation of the serratus anterior plane block. Anaesthesia. 2016;71:1064–1069. doi: 10.1111/anae.13549. [DOI] [PubMed] [Google Scholar]
- 4.Elsharkawy H., Maniker R., Bolash R., Kalasbail P., Drake R.L., Elkassabany N. Rhomboid intercostal and subserratus plane block: A cadaveric and clinical evaluation. Reg Anesth Pain Med. 2018;43:745–751. doi: 10.1097/AAP.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 5.Pepper A.M., North T.W., Sunderland A.M., Davis J. Intraoperative adductor canal block for augmentation of periarticular injection in total knee arthroplasty: a cadaveric study. J Arthroplasty. 2016;31:2072–2076. doi: 10.1016/j.arth.2016.02.030. [DOI] [PubMed] [Google Scholar]