Abstract
Aim:
Time outdoors and contact with nature are positively associated with a broad range of children’s health outcomes. Pediatricians are uniquely positioned to promote active play in nature (APN) but may face challenges to do so during well child visits. The objective of this study was to understand barriers to children’s APN, before and during the COVID-19 pandemic, and how health care providers could promote APN.
Methods:
Focus groups were conducted with 14 pediatric providers and interviews with 14 parents (7 in English, 7 in Spanish) of children ages 3 to 10 on public insurance. Dedoose was used for coding and content analysis. We contextualized this work within the WHO’s Commission on Social Determinants of Health conceptual framework.
Results:
Parents mentioned a range of material circumstances (time, finances, family circumstances, access to safe outdoor play spaces and age-appropriate activities) and behavioral/psychosocial factors (previous experiences in nature, safety, and weather concerns), many of which were exacerbated by the pandemic, that serve as barriers to children’s APN. Providers said they were motivated to talk to families about children’s APN but mentioned barriers to this conversation such as time, other pressing priorities for the visit, and lack of resources to give families.
Conclusions:
Many pre-pandemic barriers to APN were exacerbated by the COVID-19 pandemic. Well-child visits may be an effective setting to discuss the benefits of APN during and beyond the pandemic, and there is a need for contextually appropriate resources for pediatric providers and families.
Keywords: pediatrics, well child care, outdoor play, nature contact, qualitative methods
Introduction
Daily outdoor play and physical activity are recommended by the American Academy of Pediatrics and other experts to promote child health and well-being.1 -3 Current literature also demonstrates a positive relationship between nature contact and a broad range of children’s health outcomes. A recent systematic review found strong evidence that exposure to nature is positively associated with children’s physical activity and mental health, both public health priorities. 4 Before the COVID-19 pandemic only 24% of US children aged 6 to 17 years met recommendations for 60 min per day of physical activity; and being outdoors has been found to be a consistent correlate of physical activity for children.5,6 These health priorities became even more salient during the pandemic as studies found that children were less active and played outside less compared to before the pandemic.7 -9 Furthermore, park access was associated with better mental health among children and parents during the pandemic.1,9,10 Critically, park access is not equitable 11 ; 1 in 3 children in the U.S. do not live within a 10-min walk to a park. 12 Parks in communities with more families of color tend to be smaller 13 and neighborhood income is positively associated with condition of park amenities. 14 Given the evidence on the health benefits of contact with nature, multilevel strategies that target environmental and behavioral factors are needed to promote equitable access to and play in nature-rich environments. 15
Pediatric health care providers are trusted sources of information regarding children’s health and are uniquely positioned to encourage families to engage in active play outdoors, and well-child visits create an ideal setting for communication with families. Prior studies have called for family doctors to provide information, guidance, and even physical “prescriptions” to encourage time in nature, and raised the importance of studying whether these programs are effective.15 -17 While numerous such programs now exist, the evidence evaluating these interventions is limited. Critically, very few studies focus on implementation challenges, by providers 17 incorporating guidance about nature contact into well visits, and by families experiencing structural barriers to active play in nature (APN) that may not easily be addressed during clinical encounters. Understanding barriers and facilitators to children’s APN would help determine the appropriateness of intervention in the healthcare setting and inform potential strategies that health care providers and others could adopt in supporting this health promoting behavior.
The overall goals of this project were to understand the potential role pediatric health care providers could play in supporting children’s APN. To that end, we sought to: (1) identifying barriers to APN for children ages 3 to 10 with low resources and (2) identifying barriers pediatric providers face in promoting APN with families. Since this study occurred during the midst of the COVID-19 pandemic, we were able to explore the aims above within the context of the pandemic and asked participants to reflect on circumstances pre-pandemic.
Methods
Study Design and Research Personnel
We conducted a qualitative study in the Seattle, Washington area from 2020 to 2021. This report conforms to the Standards for Reporting Qualitative Research. 18
The Institutional Review Board approved the study. The research team included a pediatrician (PT), a public health researcher (EK), a medical anthropologist (KS), a research scientist (AA), a pediatric sports medicine physician (MB), a pediatric sports medicine fellow (MP), and 3 research coordinators (KG, KH, YG). Data were collected by KH, AA, MB, and MP, and analyzed by KH and YG.
Data Tools
Interview and focus group guides were developed according to study goals and adjusted as necessary per standard qualitative methodology.19,20 The parent interview guide was pilot tested with parents analogous to the sample. Focus groups with pediatric healthcare providers addressed: personal experience with, value of, and clinic resources for APN discussions. Individual interviews with parents focused on family barriers to outdoor play before and during the pandemic and conversations about APN with their pediatrician. Supplemental Appendix A is a consolidated list of all focus group and interview questions. All participants completed demographic questionnaires.
Theoretic Framework
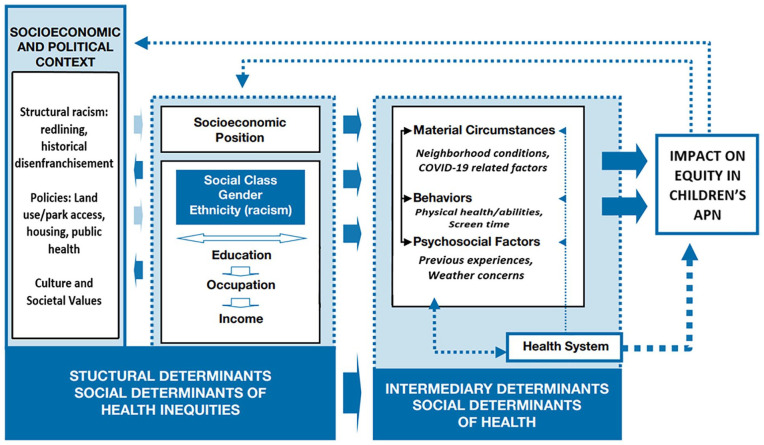
Data collection and analyses were broadly guided by a social ecological perspective, in that we viewed children and families as nested in contexts at multiple levels of influence. 21 Consistent with this lens, analyses were more specifically guided by the more nuanced- and equity-focused World Health Organization’s (WHO) Commission on Social Determinants of Health (CSDH) Conceptual Framework. 22 This framework situates the health outcome of interest (in this case children’s APN) in intermediary social determinants of health (eg, family’s material and psychosocial circumstances), which are in turn influenced by structural determinants of health inequalities, including the family’s socioeconomic position, and more distal social and political contextual factors. Within this framework, the health system is conceptualized as a modifiable intermediary social determinant of health that is shaped by broader structural determinants of health, and that can help modify the association between family-level intermediary determinants and child outcomes.
Sampling Frame and Data Analysis
A purposeful sample of providers was recruited via word of mouth and a message in the Washington Chapter of the American Academy of Pediatrics newsletter. Parents were recruited via flyers distributed at pediatric clinics in the Seattle area that serve a high proportion of patients with public insurance.
Fourteen pediatric providers participated in 6 focus groups via Zoom. Fourteen parents (7 interviewed in English, 7 interviewed in Spanish) of children who have public health insurance were interviewed individually by phone or Zoom. The initial sample estimates achieved data sufficiency, and thus the sample size did not change after an early review of transcripts. 23
Interviews and focus groups were digitally recorded, professionally transcribed, and spot checked by interviewers to ensure data integrity.24 -26 In the results, quotes are identified by participant number, parent versus provider (PA = Parent, PR = provider), and language (ENG = English, SP = Spanish).
Data were uploaded into Dedoose Version 7.0.23 (Sociocultural Research Consultants, Los Angeles, California) for coding and analysis24 -26 following procedures outlined by Braun and Clarke. 27 Steps to codebook development were: initial codes were derived from study goals; codes were augmented by a reading of 2 transcripts; codes were tested on 3 additional transcripts by both coders; the codebook was edited until an exhaustive but manageable code list was reached. We used a multi-step approach to developing the codebook which allowed for both deductive codes (eg, Barriers to physical activity during COVID) extracted from study goals, instruments, frameworks, and inductive codes (eg, Active outdoor play pre-COVID) emerging from review of transcripts.
Transcripts were open coded, and coders were blind to each other’s coding and differences were resolved by discussion until 100% agreement was reached. During synthesis, coded excerpts were systematically summarized into themes and subthemes with associated quotes.
Results
Participants included 14 parents and 14 pediatric providers (12 pediatricians, 1 sports medicine pediatrician, and 1 pediatric physical therapist) and their demographics are displayed in Tables 1 and 2.
Table 1.
Demographics of Pediatric Healthcare Providers (n = 14).
| n (%) | |
|---|---|
| Gender | |
| Female | 12 (85.7) |
| Male | 2 (14.3) |
| Age | |
| 30-39 years | 4 (28.6) |
| 40-49 years | 6 (42.8) |
| 50-59 years | 2 (14.3) |
| 60-69 years | 2 (14.3) |
| Hispanic or of Mexican or Latin American descent | |
| 1 (7.1%) | |
| Race | |
| African-American or Black | 0 (0.0) |
| American Indian or Alaskan Native | 0 (0.0) |
| Asian-American | 2 (14.3) |
| White | 7 (50.0) |
| Two or more | 5 (35.7) |
| Years practicing pediatrics | |
| 5-9 years | 3 (21.4) |
| 10-14 years | 3 (21.4) |
| 15-19 years | 4 (28.6) |
| 20+ years | 4 (28.6) |
Table 2.
Demographics of Parents (n = 14).
| n (%) | |
|---|---|
| Gender | |
| Female | 13 (92.9) |
| Male | 1 (7.1) |
| Age | |
| 20-29 years | 1 (7.1) |
| 30-39 years | 7 (50.0) |
| 40-49 years | 5 (35.7) |
| 50+ years | 1 (7.1) |
| Child age (n = 17) | |
| 3-5 years | 5 (29.4) |
| 6-8 years | 7 (41.1) |
| 9-10 years | 5 (29.4) |
| Hispanic or of Mexican or Latin American descent | |
| 8 (57.1) | |
| Race | |
| African-American or Black | 0 (0.0) |
| American Indian or Alaskan Native | 0 (0.0) |
| Asian-American | 2 (14.3) |
| White | 4 (28.6) |
| Other | 6 (42.9) |
| Unknown | 2 (14.3) |
| Primary language in home | |
| English | 5 (35.7) |
| Russian | 1 (7.1) |
| Spanish | 8 (57.1) |
Figure 1 illustrates an adapted version of the WHO CSDH Framework with themes from the current study primarily related to intermediary determinants of health—material circumstances, psychosocial factors, behaviors of the family, and attributes of the health system. 28 Below, key themes within intermediary determinants are presented, recognizing that they are situated within a broader structural context (eg, policies, structural racism) that gives rise to health inequities.
Figure 1.
Considerations regarding equity in children’s active play in nature mapped to the WHO Commission on Social Determinants of Health Conceptual Framework. Items in italics are contributions from this study.
Material Circumstances
Resources
Parents stated that work responsibilities limited time and energy available for facilitating children’s APN. This barrier was heightened for single parents, especially when supporting children’s online and hybrid learning during the pandemic.
“I have to make sure I get him to school on time and then get my work done and then pick him up at 10:45 and get him home and then we do school all afternoon and you’re just going, going, going, and then everything’s done. And oh, now I have to cook dinner and I have to do laundry. It’s like the never ending, there’s not enough time.” [15_PN_ENG]
Children of parents working shift work, low wage work, and/or multiple jobs, had caregivers that were often older (eg, grandparents) and unable to help facilitate APN due to mobility issues or discomfort supervising multiple children outdoors. Family resources impacted children’s APN when families were unable to pay for organized sports, transportation, or equipment. Overall, parents felt that their children wanted to play outside, but were reliant on others to supervise and/or transport them.
One parent stated,
“the park is quite far – I’ll have to drive there. So, I guess that’s one thing that gets in between his activities. It’s dependent on my schedule.” [00_PA_ENG]
Additionally, nature spaces could be far or on unmaintained roads, making transportation challenging. Sometimes families did not know where to access nature and needed to search online; this required access to technology and culturally and linguistically appropriate resources.
“The truth is that we have not visited many places like the mountains, and it is not us who do not enjoy nature, but one because we do not know much and sometimes the places are very far away.” [17_PA_SP]
Neighborhood conditions and pandemic-related concerns
Families living in apartments or without yard space had less access to safe play areas. The pandemic had shifted priorities for parents, who had become increasing focused on protecting children from infection even at the cost of limiting active play time.
A parent described a bleak situation early in the pandemic:
“The first six months, there was nothing. Looking back, I can’t believe that happened. But it was complete isolation, where he couldn’t play any games with kids, he can’t do any games that had touch, physical closeness. . . And even now, it’s still hard to play something like that, where you’re all wearing masks and it’s like, can I actually play with you or not really?” [14_PA_ENG]
Many parents mentioned pandemic-related barriers to their children’s physical activity such as cancellations and closures of sports, playgrounds, and schools. Concerns about social distancing on public transportation and in crowded parks, public bathroom closures, all limited or prohibited APN. Low-resource families were already struggling with having enough time and money before the pandemic. Parents and providers reported that these issues had been exacerbated by the fact that many of these families were working in industries especially hard hit by the pandemic. This trickled down to issues with childcare, time for children, and funds to support children’s activities.
Behavioral Factors
Pre-pandemic participation in APN
Prior to the pandemic, some children spent time in nature-rich activities such as: hiking; going to the beach; gardening; camping; and collecting leaves and flowers. While most parents reported their children had spent time in nature, a few reported that their children had never done so. Parents defined being in nature as places with mountains, rivers, lakes, beaches, forest, animals, and clean, fresh air. Some parents believed that nature is accessed when you get far away from the city and crowds; “Getting out of the city. Being completely surrounded by the woods and nature.” [00_PA_ENG]
Other family challenges with APN
Parents mentioned challenges such as children being tired after school, other extracurriculars, screen time, and difficulty finding enjoyable APN activities for children with autism and ADHD.
Psychosocial Factors
Getting out in cold, wet weather
Weather was the most frequently mentioned barrier to APN, specifically heavy rain, cold temperatures, and limited daylight during the winter that are all typical of the Pacific Northwest. Some parents described their belief that playing outdoors in “bad weather” would make children sick. Providers perceived the conversation about APN as even more important in winter months, especially for families where the parents had been raised in warmer climates, but acknowledged that appropriate outdoor gear could be prohibitively expensive for some. One provider stated, “There’s a big belief – hot and cold theories of disease. . . the cold air is going to make you sick. So, you do not go outside. So, I usually say, “You live in Seattle. This is our weather. This is what happens. So, please, just go outside even if it’s cold, even if it’s raining.” [113_114_PR]
Health System Factors
Motivation to discuss APN during appointments
Providers reported being motivated to talk with families about APN during their well child appointments. For 3 to 5 year olds, they attempted to educate and inspire parents about the importance of APN. Conversations were focused on the child’s daily activities, and how APN could influence screen time, sleep or behavioral issues. Providers felt APN was even more important to discuss during 6 to 10-year-old visits because older children typically engage in more screen time, and suffer from more obesity, and behavioral and mental health issues. Providers mentioned that for this age group, it is important to bring up the topic of APN because children were learning to be independent and resilient, and it was important for them to find activities they enjoyed. As a provider explained, “I try to incorporate it into the conversation about building self-esteem, self-confidence, learning new skills, feeling good about something in their lives.” [105_106_107_PR]
Providers had found it especially important to promote APN during the pandemic, especially as they saw an increased need to address mental and behavioral health; “I’ve seen a lot of kids in this age group for anxiety and sleep troubles in the last couple months, so this is part of why I talk about physical activity with them, as sort of a way to help buffer some of those more challenging emotional things that are coming up.” [105_106_107_PR]
Some providers acknowledged that APN was important to them but not always a priority for families because many believed their child was sufficiently active. Parents reported that they believed APN was important and some recalled having brief conversations about physical activity during well-child visits but not specifically about APN. A few parents did not recall any conversation with a provider about physical activity or APN.
Despite providers’ best intentions to avoid blaming the families, some parents said they felt guilty after talking with their child’s provider about APN. Parents preferred when providers were mindful of the family situation and approached the conversation in a non-judgmental way rather than lecturing the family. Providers recognized that this conversation could be uncomfortable for some families and were committed to sustaining trusting relationships.
Provider resources
Providers noted the topic of APN was not raised in every visit although all providers asserted that APN is a priority for them as a provider and that they would ideally like to discuss it with all patients. For providers, short patient visits strictly limited time allocated to APN and other anticipatory guidance topics. Irrespective of provider priorities, “If the family has a very pressing concern about development, or about behavior, or about an illness, then sometimes I can’t address [APN] in depth. I can say something in passing about how important it is to have physical activity, and preferably outdoor activity, but that’s as far as it can go.” [105_106_107_PR]. Access to developmentally, culturally, and linguistically appropriate materials could also be a limiting factor. Some providers stated that there are no easy-to-use and up-to-date APN resources for patients which prompted some to create their own; [For] preschoolers – I’ve created what to do during the holidays with a combination of outdoor and indoor activities. I feel like, based on kids’ interests. . .we come up together with a list of ideas that could work for them. [108_109_110_PR]
After-visit, hard-copy summaries usually included physical activity recommendations—though not necessarily resources for how and where to do APN, nor was it available for non-English readers. Some referred patients to organizations like the YMCA and local sports clubs. Providers generally had a sense of local parks but no formal way to share with families, and sometimes they lacked locally relevant materials for some patients depending on address. Generally, there was a consensus that resources were limited and became even less helpful during the pandemic.
Conflict: Pressing social and health issues
Providers stated that the importance of having the APN conversation was dependent on family needs: some patients were dealing with food insecurity, not meeting developmental milestones, or other concerns. In those cases, the topic was often sidelined or only mentioned briefly. Sometimes providers notice that parents were stressed, unable to support their children’s APN, living in unsafe neighborhoods, unable to pay for organized sports or experiencing large systematic barriers. In these cases, the provider did not feel like it was appropriate to bring up APN. Expressing their own frustration, a provider said: “I don’t have a ton of solutions for a lot of the challenges that they bring up. We always try to talk through and think of creative solutions to get outside. . . but it’s not like I have some magic solution like, aha, here, now I can make it easy for you and you can do this.” [108_108_110_PR]
As one provider explained, “There’s so many structural problems with our society that for me to say, “Go outside and play!” is so naïve.” [101_102_PR]. It was perceived as defeating for both patient and provider to quickly talk about APN when more time and resources would be needed to adequately address this topic. Providers also mentioned that their own burnout could impact their choice of whether to initiate an APN discussion.
Discussion
This qualitative study explored parent and health care provider perspectives on outdoor play and nature contact for children ages 3 to 10, during and before the COVID-19 pandemic, and how this topic is covered during pediatric well child visits. We aligned our findings with the WHO’s social determinants of health framework to highlight how the intermediary determinants of equitable engagement by children in active play in nature emergent from this study are in part a consequence of structural conditions and family socioeconomic position. Parents reported a range of barriers relating to supporting their children in active play in nature, and many pre-pandemic barriers were exacerbated by the COVID-19 pandemic. While pediatric health care providers generally considered the discussion of physical activity and outdoor play important for children, especially during the pandemic, they often needed to focus on other priorities. Providers reported few or no resources to support them in adequately discussing APN with their patients and families. These findings lay the foundation for future efforts to decrease disparities to children’s APN, develop materials that are beneficial for providers when discussing APN with their patients, and prioritize strategies that recognize and address potential barriers families may face in engaging in APN.
Parents and providers highlighted material barriers to physical activity and nature contact for families including not having nearby access to parks, not knowing where to go, or having the means to get there. Determinants of such inequities may reflect historical context and policies rooted in structural discrimination. For example, “redlining,” a government-sanctioned practice of denying mortgages to people of color has led to disinvested neighborhoods which continue to have fewer built environment features that promote health. 29 These challenges are compounded by the family’s socioeconomic position wherein work demands and available childcare options add additional barriers for children’s APN. Previous research has shown that preschoolers from non-White families or those with mothers that work outside the home had lower odds of playing outside daily with a parent. 30 Overcoming these barriers will require political will and investment in community assets that promote healthy behaviors and health equity. Additionally, multilevel, multi-sector interventions based on ecological models that target practices, environments, and policies will be needed to promote active living and outdoor time across age groups.31,32
We also heard about how these structural barriers connected to intermediary behavioral determinants of children engaging in APN. Notably, many families did not think of nature as something that existed in their neighborhoods and a few even felt that their child had never spent time in nature. A recent paper that reviewed a range of nature exposure types found the strongest evidence for nature contact close to children’s homes and schools. 4 In addition to advocacy for increasing access to larger public greenspaces, there may be opportunities for less resource intensive strategies such as addition of gardens in childcare, school and community spaces, for which there is moderate evidence in that review paper. Furthermore, families may need information about nearby nature that does exist, how to access it, and how to support their children’s play safely in those spaces and under different weather conditions. Particular attention needs to be given to making sure this information is available in ways that are linguistically and culturally appropriate for all families.
The COVID-19 pandemic both worsened and highlighted barriers and disparities to children’s APN as typical opportunities were restricted, families worried about keeping their children free of infection, and children spent more time at home and sedentary.33,34 Studies using national data found that park proximity and physical activity were each associated with better mental for school age children.7,10 While providers recognized the increased salience of addressing active play and nature contact during this challenging time, particularly given trends of increasing weight gain and mental and behavioral health concerns for children,35,36 they continued to struggle with the need to prioritize how to spend their limited time during well child visits. Providers were also mindful about bringing up this topic in a non-judgmental manner, so as to prevent families from feeling burdened or guilty if they felt unable to easily incorporate APN into their lives. Furthermore, they reported few or no existing resources to support them in this discussion besides ones they had created on their own or briefly added to after visit summaries. Despite all the providers in this study strongly endorsing the importance of this topic in promoting child health, parents rarely reported discussing outdoor play or nature contact during their child’s well visits.
Limitations of our study include having a small sample of demographically-limited participants from one geographic area. While generalizability was not the goal, demography and geography were significant contexts for participants’ lived experiences, and could not help but influence what we were told during data collection. Thus, we do not suggest that our findings are representative across other contexts. All of our data collection occurred during the COVID-19 pandemic which created unprecedented stressors for families and health care providers, and although we asked participants to reflect on pre-pandemic circumstances, their responses need to be reviewed with that context in mind.
These findings suggest opportunities for the health system and pediatric health care providers to play a larger role in endorsing and encouraging APN to promote children’s health and development, and health equity. At the same time, these findings caution about the various barriers families face in engaging in APN, and the structural origins of these challenges that make them potentially difficult to modify through intervention in the healthcare setting. An approach that has gained some attention is providers using nature prescriptions during their clinical visits to “prescribe” time in nature. Some programs include resources such as information about local parks, park passes, and pedometers37 -39 in addition to a written prescription for time outdoors. Other programs include more structured components such as invitations to park outings and referrals to park-based programs.38,40 Such programs have come up across the country 41 although the evidence for them is sparse and mixed. 17 Most studies included in a recent review of nature prescription programs used convenience samples, evaluated patient adherence (rather than health outcomes), did not include control groups, and rarely included provider perspectives.
Given our findings, additional research is needed on how clinical approaches can address both the material and psychosocial circumstances that contribute to family APN inequities and give healthcare providers both materials and guidance on how to approach this topic with their patients. In addition to the necessary societal efforts to promote environmental justice and eliminate structural barriers to nature access, this study contributes patient and provider perspectives to the emerging movement to include health systems in strategies to increase equitable opportunities for children to access and play in nature.
Supplemental Material
Supplemental material, sj-docx-1-jpc-10.1177_21501319221114842 for A Framework for Pediatric Health Care Providers to Promote Active Play in Nature for Children by Pooja S. Tandon, Kiana Hafferty, Emily Kroshus, Antionette Angulo, Monique Burton, Michael Peyton and Kirsten Senturia in Journal of Primary Care & Community Health
Acknowledgments
We are grateful to Kim Garrett and Yesenia Garcia for their contributions to data collection. We acknowledge Dr. Danette Glassy and Edna Maddalena from Beststart WA for their thoughtful review of the study design.
Footnotes
Author’ Contributions: Dr. Tandon conceptualized and designed the study, participated in data analysis, drafting the initial manuscript, and reviewed and revised the manuscript. Ms. Hafferty participated in data collection, data analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Dr. Kroshus participated in data analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Dr. Angulo participated in data collection and reviewed and revised the manuscript. Dr. Burton participated in data collection and reviewed and revised the manuscript. Dr. Peyton participated in data collection and reviewed and revised the manuscript. Dr. Senturia participated in data analysis, drafting the initial manuscript, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: All phases of this study were supported by a grant from the Seattle Children’s Research Institute, Research Integration Hub.
Ethics Approval: This study was approved by the Seattle Children’s Institutional Review Board.
Consent to Participate: All participants provided verbal consent to participate in this study. No identifiers are used in this manuscript.
ORCID iD: Kiana Hafferty  https://orcid.org/0000-0001-6114-9480
https://orcid.org/0000-0001-6114-9480
Supplemental Material: Supplemental material for this article is available online.
Availability of Data and Material: Available upon request.
Code Availability: Available upon request.
References
- 1. Piercy KL, Troiano RP. Physical activity guidelines for Americans from the US Department of Health and Human Services: cardiovascular benefits and recommendations. Circ Cardiovasc Qual Outcomes. 2018;11(11):e005263. doi: 10.1161/CIRCOUTCOMES.118.005263 [DOI] [PubMed] [Google Scholar]
- 2. Tremblay MS, Gray C, Babcock S, et al. Position statement on active outdoor play. Int J Environ Res Public Health. 2015;12(6):6475-6505. doi: 10.3390/ijerph120606475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yogman M, Garner A, Hutchinson J, Hirsh-Pasek K, Golinkoff RM. The power of play: a pediatric role in enhancing development in young children. Pediatrics. 2018;142(3):e20182058. doi: 10.1542/peds.2018-2058 [DOI] [PubMed] [Google Scholar]
- 4. Fyfe-Johnson AL, Hazlehurst MF, Perrins SP, et al. Nature and children’s health: a systematic review. Pediatrics. 2021;148(4):e2020049155. doi: 10.1542/peds.2020-049155 [DOI] [PubMed] [Google Scholar]
- 5. Gray C, Gibbons R, Larouche R, et al. What is the relationship between outdoor time and physical activity, sedentary behaviour, and physical fitness in children? A systematic review. Int J Environ Res Public Health. 2015;12(6):6455-6474. doi: 10.3390/ijerph120606455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Larouche R, Mire EF, Belanger K, et al. Relationships between outdoor time, physical activity, sedentary time, and Body Mass Index in children: a 12-country study. Pediatr Exerc Sci. 2019;31(1):118-129. doi: 10.1123/pes.2018-0055 [DOI] [PubMed] [Google Scholar]
- 7. Tandon PS, Zhou C, Johnson AM, Gonzalez ES, Kroshus E. Association of children’s physical activity and screen time with mental health during the COVID-19 pandemic. JAMA Netw Open. 2021;4(10):e2127892. doi: 10.1001/jamanetworkopen.2021.27892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rossi L, Behme N, Breuer C. Physical Activity of children and adolescents during the COVID-19 pandemic - a scoping review. Int J Environ Res Public Health. 2021;18(21):11440. doi: 10.3390/ijerph182111440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17(1):85. doi: 10.1186/s12966-020-00987-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hazlehurst MF, Muqueeth S, Wolf KL, Simmons C, Kroshus E, Tandon PS. Park access and mental health among parents and children during the COVID-19 pandemic. BMC Public Health. 2022;22:800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dai D. Racial/ethnic and socioeconomic disparities in urban green space accessibility: Where to intervene? Landsc Urban Plan. 2011;102(4):234-244. doi: 10.1016/j.landurbplan.2011.05.002 [DOI] [Google Scholar]
- 12. Trust for Public Land. Parks and an equitable recovery. Published May 27, 2021. Accessed December 16, 2021. https://www.tpl.org/parks-and-an-equitable-recovery-parkscore-report
- 13. Trust for Public Land. The heat is on. Published 2020. Accessed May 25, 2021. https://www.tpl.org/sites/default/files/files_upload/The-Heat-is-on_A-Trust-for-Public-Land_special-report_r1_2.pdf
- 14. McKenzie TL, Moody JS, Carlson JA, Lopez NV, Elder JP. Neighborhood income matters: disparities in community recreation facilities, amenities, and programs. J Park Recreat Adm. 2013;31(4):12-22. [PMC free article] [PubMed] [Google Scholar]
- 15. Calogiuri G, Chroni S. The impact of the natural environment on the promotion of active living: an integrative systematic review. BMC Public Health. 2014;14(1):873. doi: 10.1186/1471-2458-14-873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Frumkin H, Bratman GN, Breslow SJ, et al. Nature contact and human health: a research agenda. Environ Health Perspect. 2017;125(7):075001. doi: 10.1289/EHP1663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kondo MC, Oyekanmi KO, Gibson A, South EC, Bocarro J, Hipp JA. Nature prescriptions for health: a review of evidence and research opportunities. Int J Environ Res Public Health. 2020;17(12):4213. doi: 10.3390/ijerph17124213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245-1251. doi: 10.1097/ACM.0000000000000388 [DOI] [PubMed] [Google Scholar]
- 19. Patton MQ. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. SAGE Publications; 2014. [Google Scholar]
- 20. Bernard HR. (Harvey R 1940-. Research Methods in Anthropology : Qualitative and Quantitative Approaches, 3rd ed. AltaMira Press; 2002. https://search.library.wisc.edu/catalog/999926279902121 [Google Scholar]
- 21. Bronfenbrenner U, Husen T, Postlethwaite TN. International encyclopedia of education. Ecol Models Hum Dev. 1994;3:37-43. [Google Scholar]
- 22. WHO. Commission on social determinants of health. Published 2008. Accessed May 4, 2022. https://www.who.int/teams/social-determinants-of-health/equity-and-health/commission-on-social-determinants-of-health
- 23. Hennink MM, Kaiser BN, Weber MB. What influences saturation? Estimating sample sizes in Focus Group Research. Qual Health Res. 2019;29(10):1483-1496. doi: 10.1177/1049732318821692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bazeley P. Qualitative data analysis: practical strategies.2013. Accessed December 20, 2021. https://researchdirect.westernsydney.edu.au/islandora/object/uws%3A48650/
- 25. Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114-116. doi: 10.1136/bmj.320.7227.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hennink M, Hutter I, Bailey A. Qualitative Research Methods. SAGE Publications Ltd; 2021: Accessed December 20, 2021 https://uk.sagepub.com/en-gb/eur/qualitative-research-methods/book242878 [Google Scholar]
- 27. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 28. WHO. A conceptual framework for action on the social determinants of health. 2010. Accessed December 27, 2021. https://www.who.int/publications-detail-redirect/9789241500852
- 29. Locke DH, Hall B, Grove JM, et al. Residential housing segregation and urban tree canopy in 37 US cities. npj Urban Sustain. 2021;1(1):15. doi: 10.1038/s42949-021-00022-0 [DOI] [Google Scholar]
- 30. Tandon PS, Zhou C, Christakis DA. Frequency of parent-supervised outdoor play of US preschool-aged children. Arch Pediatr Adolesc Med. 2012;166(8):707-712. doi: 10.1001/archpediatrics.2011.1835 [DOI] [PubMed] [Google Scholar]
- 31. Outdoor Play Canada. Outdoor play in Canada: 2021 State of the sector report. July 2021. Accessed May 4, 2022. https://www.outdoorplaycanada.ca/wp-content/uploads/2021/09/OPC_SSR_english_FINAL.pdf
- 32. Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297-322. https://www.annualreviews.org/doi/10.1146/annurev.publhealth.27.021405.102100?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed#_i18 Accessed May 4, 2022. [DOI] [PubMed] [Google Scholar]
- 33. Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351. doi: 10.1186/s12889-020-09429-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wilke J, Mohr L, Tenforde AS, et al. A pandemic within the pandemic? Physical activity levels substantially decreased in countries affected by COVID-19. Int J Environ Res Public Health. 2021;18(5):2235. doi: 10.3390/ijerph18052235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lange SJ, Kompaniyets L, Freedman DS, et al. Longitudinal trends in Body Mass Index before and during the COVID-19 pandemic among persons aged 2-19 years - United States, 2018-2020. MMWR Morb Mortal Wkly Rep. 2021;70:1278-1283. doi: 10.15585/mmwr.mm7037a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;17(22):8479. doi: 10.3390/ijerph17228479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Coffey JS, Gauderer L. When pediatric primary care providers prescribe nature engagement at a State Park, do children “fill” the prescription? Ecopsychology. 2016;8(4):207-214. doi: 10.1089/eco.2016.0019 [DOI] [Google Scholar]
- 38. Razani N, Kohn MA, Wells NM, Thompson D, Hamilton Flores H, Rutherford GW. Design and evaluation of a park prescription program for stress reduction and health promotion in low-income families: the Stay Healthy in Nature Everyday (SHINE) study protocol. Contemp Clin Trials. 2016;51:8-14. doi: 10.1016/j.cct.2016.09.007 [DOI] [PubMed] [Google Scholar]
- 39. Zarr R, Cottrell L, Merrill C. Park Prescription (DC Park Rx): a new strategy to combat chronic disease in children. J Phys Act Health. 2017;14(1):1-2. doi: 10.1123/jpah.2017-0021 [DOI] [PubMed] [Google Scholar]
- 40. Razani N, Meade K, Schudel C, Johnson C, Long D. Healing through nature: a park-based health intervention for young people in Oakland, California. Child Youth Environ. 2015;25(1):147-159. doi: 10.7721/chilyoutenvi.25.1.0147 [DOI] [Google Scholar]
- 41. Parkrx. Directory of programs. Published October 1, 2018. Accessed December 20, 2021. https://www.parkrx.org/content/directory-programs
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpc-10.1177_21501319221114842 for A Framework for Pediatric Health Care Providers to Promote Active Play in Nature for Children by Pooja S. Tandon, Kiana Hafferty, Emily Kroshus, Antionette Angulo, Monique Burton, Michael Peyton and Kirsten Senturia in Journal of Primary Care & Community Health