Abstract
Background:
The prevalence of substance use disorders (SUDs) among adults ages 65 and older has been increasing at a notably high rate in recent years, yet little information exists on hospitalizations for SUDs among this age group. In this study we examined trends in hospitalizations for alcohol use disorders (AUDs) and opioid use disorders (OUDs) among adults 65 and older in the United States, including differences by gender and race/ethnicity.
Methods:
We used Medicare claims data for years 2007-2014 from beneficiaries ages 65 and older. We abstracted hospitalization records with an ICD-9 diagnostic code for an AUD or OUD. Hospitalization rates were calculated using population estimates from the United States Census. We examined trends in quarterly hospitalization rates for hospitalizations with AUD/OUD as primary diagnoses, and separately for those with these disorders as secondary diagnoses. We also examined comorbidities for those with a primary diagnosis of AUD/OUD. Analyses were conducted for all hospitalizations with AUD/OUD diagnoses, and separately by gender and race/ethnicity.
Results:
Between the last quarter of 2007 and the third quarter of 2014, AUD hospitalization rates increased from 485 to 579 per million (19%), and OUD hospitalization rates from 46 to 101 per million (120%) and varied by gender (for AUD) and race/ethnicity (for both AUD and OUD). Hospitalization rates were particularly high for Black older adults, as was the increase in hospitalization rates. The increase in hospitalization rates was substantially higher for hospitalizations with AUD (84%) and OUD (269%) as secondary diagnoses.
Conclusions:
Hospitalizations for AUDs and OUDs among older adults increased at an alarming rate during the observation period, and disparities existed in hospitalization rates for these conditions. Interventions focusing on the needs of older adults with AUD and/or OUD are needed, particularly to address the needs of a growing racially/ethnically diverse older adult population.
Keywords: Alcohol use disorders, opioid use disorders, older adults, hospitalizations
Introduction
Alcohol use, drug use, and the prevalence of substance use disorders have grown substantially among adults in recent years, particularly among older adults (those 65 and older). Alcohol use among this age group is notably higher than in previous generations,1 -5 and rates of excessive alcohol use among adults 65 and older increased by 65% between 2001-2002 and 2012-2013. 6 Although the prevalence of alcohol use disorders (AUDs) among older adults (estimated at about 3%) is low compared to other age groups, the prevalence is growing rapidly with an estimated increase of over 100% in that same time period. 6
There is less data available on opioid misuse and opioid use disorders (OUDs) among older adults, yet the sharp increase in prescriptions of opioid pain relievers in the last 2 decades7,8 has likely led to increases in OUDs among this age group given their higher rate of chronic pain. There is already some evidence of these changes. Rates of misuse of pain relievers among adults 50 and older has already increased9,10 and emergency department visits for adults over the age of 65 suffering from opioid misuse increased by over 200% between 2006 and 2014. 11
Alcohol and opioid misuse rates vary by gender. Rates of alcohol misuse and AUDs are generally higher for men compared to women, but the gender gap in heavy drinking, AUDs, and alcohol-related mortality has been shrinking.12 -16 Among older adults specifically, past-month binge drinking and past-year AUD has increased more for women than men.17,18 Opioid overdose death rates among adults 65 to 74 are higher for men 19 but women account for a higher proportion of emergency department visits for opioid misuse. 11 Thus, examining gender differences in health care utilization for these conditions among older adults is imperative.
It is also critical that changes in health care utilization for AUDs and OUDs in older adults be examined separately by race/ethnicity so that racial/ethnic inequities can be identified and addressed. To the best of our knowledge, prevalence data of problem drinking, AUDs, opioid misuse, and OUDs in older adults by race/ethnicity is not available. Among adults in general, however, rates of AUDs tend to be substantially higher for Native Americans than all other racial/ethnic groups. 20 Although the rates for AUDs among Black and Latino adults are lower than among White adults, 20 the health consequences of alcohol misuse such as cirrhosis of the liver, and alcohol-related mortality, tend to be worse for Latino and Black individuals compared to their White counterparts, though there is variation between groups by gender.21 -23 In terms of opioids, opioid-involved overdose death rates have generally been higher among White older adults. 24 However, overdose rates in metropolitan areas have been increasing much more rapidly among Black older adults 24 and nationally, the growth in overdose death rates is now higher for Blacks individuals than for White individuals.25,26
These increases in prevalence of substance misuse among older adults are occurring at the same time that the population of older adults in the U.S is growing at a faster rate than the general population. 27 In 2019, adults 65 and older made up 16% of the population, a total of 54.1 million individuals. 28 It is projected that by 2060 1 of 4 U.S. residents will be an adult 65 years old or older, almost 100 million. 29 Moreover, the population of older adults is becoming substantially more diverse with estimates that by 2050, 39% of those 65 and older will be racial/ethnic minorities. 30
As older adults are making up a larger proportion of the overall population, the impact of these changes in demographic and substance misuse prevalence will have an enormous impact on the U.S. health care system. Yet little information exists on AUD- and OUD-related hospitalizations among this age group, existing comorbidities, and variations by demographic subgroups.
Using Medicare hospitalization records, the most comprehensive source of hospitalization data for US adults 65 and older, 31 we describe trends in hospitalizations for alcohol and opioid use disorders among adults ages 65 and over between 2007 and 2014. We examine trends by gender and race/ethnicity within this age group to identify groups that may be at particular risk. We also examine comorbidities among patients hospitalized with an AUD or OUD. The findings from this study are necessary to address the impact of AUDs and OUDs among older adults, and to address any inequities in the impact of these conditions.
Methods
Data source and data abstraction
Hospitalization records of Medicare beneficiaries were obtained from the Centers for Medicare and Medicaid (CMS). Medicare provides health coverage for most adults 65 and over (estimated at 98%) in the US. 31 We used Medicare Provider Analysis and Review (MedPAR) datasets from fiscal years 2008 to 2014 (October 1, 2007-September 30, 2014). These datasets include 100% of Medicare beneficiaries who use hospital inpatient services. We abstracted hospitalization records of anyone who was 65 and older at the time of hospital admission, and who had an AUD or OUD diagnosis in any diagnostic field. We used ICD-9 CM codes related to alcohol/opioid withdrawal, abuse, dependence, and alcohol or opioid induced mental disorders, as well as alcohol or opioid-related poisonings. Finally, we included ICD-9 codes for other conditions associated with a substance (eg, alcohol cirrhosis of the liver disease). See Supplemental Appendix Table 1 for a list of ICD-9 CM codes used.
Trends in AUD and OUD hospitalization counts and rates
We tabulated total quarterly admissions for the total population, as well as quarterly admissions separately by gender and race/ethnicity. To calculate hospitalization rates, we obtained annual population estimates for the total U.S. population aged 65 and over, as well as population estimates by race/ethnicity, and age from the U.S. Census Office of Population Estimates for years 2007 to 2014. Quarterly hospitalization rates were calculated by dividing quarterly stratum-specific hospitalization counts by stratum-specific population counts for each calendar year of data and multiplying by 4. Because hospitalizations for AUDs and OUDs are relatively rare events in the general population, we calculated hospitalization rates based on the number of hospitalizations per 1 000 000. We calculated the absolute and the percent change in number of hospitalizations and hospitalization rates overall and by gender and race/ethnicity subgroups. We also calculated the mean quarterly hospitalization rates (N = 28 for number of quarters) and used t-tests to test for gender differences and Welch tests to test for racial/ethnic differences given unequal variances. We set the significance level at P < .05 and used a Bonferroni correction for multiple comparisons.
We tested for trends overtime for AUD and OUD hospitalization rates overall by estimating linear (OLS) models using the following equation: Y = β0 + β1Quarter + ε where Y represents the predicted AUD or OUD hospitalization rate, Quarter represents each consecutive quarter in the study period starting with 0 = Quarter 4 in 2007, and β1 is the estimated change in quarterly hospitalization rates. To determine whether trends were significantly different by gender and race/ethnicity respectively, we used t-tests comparing the estimated coefficient for each subgroup. We set the significance level at P < .05.
Examination of comorbidities
Among hospitalizations with an AUD or OUD as the principal diagnosis, we examined the frequency of other diagnoses in all other diagnostic fields (excluding other AUD or OUD diagnoses in those fields if that was the principal diagnosis). Other substance use disorders (eg, cocaine use disorder, methamphetamine use disorder) were considered separately from mental health. Calculations for comorbidities were conducted aggregated for the entire observation period. As with other analyses, we did this across all hospitalizations, as well as separately by demographic group. We tested whether the prevalence of the most common comorbidities varied by gender and by race/ethnicity using Chi-squared tests, followed by pair-wise comparisons (for race/ethnicity). We set the significance level at P < .05, with a Bonferroni correction for multiple comparisons (for race/ethnicity).
Because most older patients have more than one chronic condition, 32 AUD or OUD may not be listed as the principal diagnosis but it still impacts the care patients must receive. Therefore, we also examined the principal diagnosis for hospitalizations that had an AUD or OUD diagnoses in a diagnosis field that was not the principal diagnosis.
Results
Total hospitalizations
Over the study period, there were a total of 160 901 hospitalizations with AUD as the primary diagnosis and 24 048 hospitalizations with OUD as the primary diagnosis among Medicare beneficiaries 65 and older. Table 1 shows the total number of hospitalizations with an AUD or OUD diagnosis as primary or secondary diagnosis by age, race/ethnicity, and gender during the study period. The total number of hospitalizations with AUD as primary and secondary diagnoses were substantially higher for men compared to women. However, for hospitalizations with OUD as primary or secondary diagnoses, the difference by gender was not as high. Most hospitalizations for AUD or OUD as primary or secondary diagnoses were from White older adults.
Table 1.
Number of hospitalizations with alcohol use disorder and opioid use disorder diagnoses in U.S. older adults, 2007 quarter 4 to 2014 quarter 3.
| Alcohol use disorders | Opioid use disorders | |||||
|---|---|---|---|---|---|---|
| Total | Men | Women | Total | Men | Women | |
| AUD/OUD AS PRIMARY DIAGNOSES | ||||||
| Total | 160 901 | 117 168 | 43 733 | 24 048 | 9839 | 14 209 |
| Age | ||||||
| 65-69 | 80 028 (49.7%) | 60 000 (51.2%) | 20 028 (45.8%) | 11 384 (47.3%) | 5271 (53.6%) | 6113 (43.0%) |
| 70-74 | 44 094 (27.4%) | 31 863 (27.2%) | 12 231 (28.0%) | 6213 (25.8%) | 2434 (24.7%) | 3779 (26.6%) |
| 75-79 | 21 753 (13.5%) | 15 196 (13.0%) | 6557 (15.0%) | 3218 (13.4%) | 1130 (11.5%) | 2088 (14.7%) |
| 80-84 | 10 358 (6.4%) | 7 072 (6.0%) | 3286 (7.5%) | 1830 (7.6%) | 615 (6.3%) | 1215 (8.5%) |
| 85+ | 4668 (2.9%) | 3037 (2.6%) | 1631 (3.7%) | 1403 (5.8%) | 389 (4.0%) | 1014 (7.1%) |
| Race/ethnicity | ||||||
| White | 134 067 (83.3%) | 95 462 (81.5%) | 38 605 (88.3%) | 20 069 (83.5%) | 7 611 (77.4%) | 12 458 (87.7%) |
| Black | 19 167 (11.9%) | 15 279 (13.1%) | 3888 (8.9%) | 3069 (12.8%) | 1781 (18.1%) | 1288 (9.1%) |
| Latino/Hispanic | 2917 (1.8%) | 2638 (2.3%) | 279 (0.6%) | 322 (1.3%) | 172 (1.8%) | 150 (1.1%) |
| Asian | 595 (0.4%) | 517 (0.4%) | 78 (0.2%) | 115 (0.5%) | 44 (0.5%) | 71 (0.5%) |
| Native American | 1328 (0.8%) | 954 (0.8%) | 374 (0.9%) | 173 (0.7%) | 51 (0.5%) | 122 (0.9%) |
| Other race/ethnicity | 1807 (1.1%) | 1500 (1.3%) | 307 (0.7%) | 227 (0.9%) | 136 (1.4%) | 91 (0.6%) |
| Unknown | 1020 (0.6%) | 818 (0.7%) | 202 (0.5%) | 73 (0.3%) | 44 (0.4%) | 29 (0.2%) |
| AUD/OUD AS SECONDARY DIAGNOSES | ||||||
| Total | 1 304 233 | 961 024 | 343 209 | 173 139 | 75 610 | 97 529 |
| Age | ||||||
| 65-69 | 492 842 (37.8%) | 375 565 (39.1%) | 117 277 (34.2%) | 78 056 (45.1%) | 40 029 (52.9%) | 38 027 (39.0%) |
| 70-74 | 353 302 (27.1%) | 264 535 (27.5%) | 88 767 (25.9%) | 43 628 (25.2%) | 19 024 (25.2%) | 24 604 (25.2%) |
| 75-79 | 229 047 (17.6%) | 165 605 (17.2%) | 63 442 (18.5%) | 24 803 (14.3%) | 9131 (12.1%) | 15 672 (16.1%) |
| 80-84 | 141 078 (10.8%) | 98 162 (10.2%) | 42 916 (12.5%) | 14 660 (8.5%) | 4511 (6.0%) | 10 149 (10.4%) |
| 85+ | 87 964 (6.7%) | 57 157 (6.0%) | 30 807 (9.0%) | 11 992 (6.9%) | 2915 (3.9%) | 9077 (9.3%) |
| Race/ethnicity | ||||||
| White | 1 069 439 (82.0%) | 773 377 (80.5%) | 296 062 (86.3%) | 141 642 (81.8%) | 55 558 (73.5%) | 86 084 (88.3%) |
| Black | 174 876 (13.4%) | 137 497 (14.3%) | 37 379 (10.9%) | 24 660 (14.2%) | 16 126 (21.3%) | 8534 (8.8%) |
| Latino/Hispanic | 22 324 (1.7%) | 19 755 (2.1%) | 2569 (0.8%) | 2825 (1.6%) | 1893 (2.5%) | 932 (1.0%) |
| Asian | 6458 (0.5%) | 5583 (0.6%) | 875 (0.3%) | 789 (0.5%) | 393 (0.5%) | 396 (0.4%) |
| Native American | 10 818 (0.8%) | 7 649 (0.8%) | 3169 (0.9%) | 1185 (0.7%) | 394 (0.5%) | 791 (0.8%) |
| Other race/ethnicity | 14 217 (1.1%) | 12 103 (1.3%) | 2114 (0.6%) | 1563 (0.9%) | 963 (1.3%) | 600 (0.6%) |
| Unknown | 6101 (0.5%) | 5060 (0.5%) | 1041 (0.3%) | 475 (0.3%) | 283 (0.4%) | 192 (0.2%) |
Abbreviations: AUD = Alcohol use disorders; OUD = Opioid use disorders.
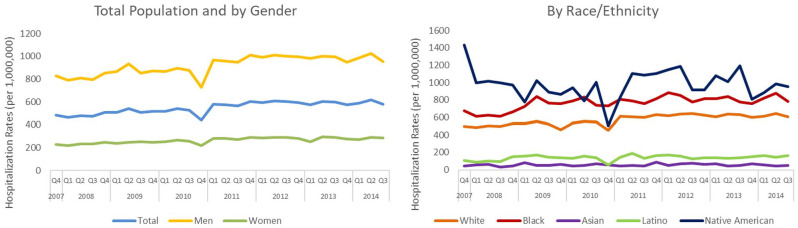
AUD hospitalizations and hospitalization rates
Supplemental Appendix Table 2 shows the number of hospitalizations and the hospitalization rates at the beginning and end of the study period for hospitalizations which had AUD as the primary diagnosis, the mean hospitalization rates across all quarters in the study period, and the percent change in quarterly hospitalization rates between the first and last quarter of observation. Figure 1 shows a graphical representation of quarterly AUD hospitalization rates for AUD for the entire population, as well as by gender and race/ethnicity. The number of quarterly hospitalizations with an AUD as the primary diagnosis increased by 46%, from 4584 hospitalizations in the first quarter to 6689 hospitalizations in the last quarter of the study period.
Figure 1.
Quarterly alcohol use disorder hospitalization rates; U.S. older adults, 2007 quarter 4 to 2014 quarter 3.
The mean quarterly AUD hospitalization rate during the study period was 592 hospitalizations per million (standard deviation (SD) = 337), and the quarterly AUD hospitalization rate increased by 19%, from 485 hospitalizations per million in the first quarter of the study to 579 hospitalizations per million in the last quarter. The mean quarterly AUD hospitalization rate for men (M = 920, SD = 82) was over 3 times higher than the mean quarterly AUD hospitalization rate for women (M = 263, SD = 24, P < .001).
Mean AUD hospitalization rates were highest for Native American older adults (M = 978, SD = 170) followed by Black (M = 770, SD = 75), White (M = 572, SD = 59), and Latino older adults (M = 139, SD = 28) and lowest for Asian older adults (M = 56, SD = 14) (all pair-wise comparisons significant, at P < .05 using Bonferroni correction for multiple comparisons). It is important to note, however, that the number of AUD hospitalizations per quarter were less than 100 for Latino older adults in several quarters, and even lower for Native American(<60/quarter) and Asian older adults (<30/quarter). At the same time, records with “Unknown” and “Other” race/ethnicity make up a substantial number of AUD (and OUD) hospitalizations each year, particularly relative to the number of hospitalizations of Latino, Asian, and Native American older adults (See Supplemental Appendix Figure 1).
The results of the regression analyses showed that trends were positive and statistically significant for AUD hospitalization rates (Coeff = 5.14, 95% CI = 3.74-6.54, P < .01). Trends were also significant for all gender, and racial/ethnic groups, except for Asian and Native American older adults. Furthermore, quarterly AUD hospitalization rates increased faster for men compared to women, and for White and Black older adults compared to Latino and Asian older adults (See Table 2).
Table 2.
Results of trends analyses for quarterly change in hospitalization rates where alcohol use disorder or opioid use disorder are primary and secondary diagnoses; U.S. Older Adults, 2007 quarter 4 to 2014 quarter 3.
| Alcohol use disorder | Opioid use disorder | |||
|---|---|---|---|---|
| Quarterly change in hospitalization
rate (95% CI) |
Differences by subgroup 1 | Quarterly change in hospitalization
rate (95% CI) |
Differences by subgroup 1 | |
| AUD/OUD AS PRIMARY DIAGNOSES | ||||
| All hospitalizations | 5.14 (3.74-6.54)*** | 2.14 (1.86-2.43)*** | ||
| Sex | ||||
| Men | 7.93 (5.45-10.40)*** | Men > Women | 2.12 (1.82-2.41)*** | n.s. |
| Women | 2.40 (1.71-3.08)*** | 2.21 (1.86-2.55)*** | ||
| Race/ethnicity | ||||
| White | 5.83 (4.14-7.52)*** |
W > L,
A
B > L, A |
2.09 (1.68-2.49)*** |
B > W,
L, A
W > L, A |
| Black | 6.24 (3.57-8.91)*** | 4.05 (3.19-4.91)*** | ||
| Latino/Hispanic | 1.30 (0.02-2.58)* | 0.30 (0.09-0.50)** | ||
| Asian | 0.18 (−0.48-0.84) | 0.20 (−0.02-0.43) | ||
| Native American | −0.89 (−9.21-7.44) | 2.23 (−0.49-4.94) | ||
| AUD/OUD AS SECONDARY DIAGNOSES | ||||
| All hospitalizations | 139.80 (110.44 –169.15)*** | 29.30 (26.43-32.17)*** | ||
| Sex | ||||
| Men | 231.74 (181.03-282.45)*** | Men > Women | 29.09 (26.19-31.99)*** | n.s. |
| Women | 64.58 (51.46-77.70)*** | 29.46 (26.58-32.34)*** | ||
| Race/ethnicity | ||||
| White | 148.68 (117.88-179.47)*** | B, W, N > L, A | 31.52 (28.43-34.62)*** |
B > W, L,
A N > L, A W > L, A |
| Black | 203.40 (160.36-246.44)*** | 41.64 (37.73-45.55)*** | ||
| Latino/Hispanic | 26.81 (18.65-34.97)*** | 4.65 (3.75-5.55)*** | ||
| Asian | 19.16 (14.21-24.10)*** | 3.01 (2.14-3.89)*** | ||
| Native American | 158.36 (90.13-226.58)*** | 40.87 (31.59-50.15)*** | ||
Abbreviations: AUD = alcohol use disorder; OUD = opioid use disorder.
1Indicates that the estimated quarterly change in hospitalization rates is significantly different for those groups (W = White, B = Black, L = Latino, A = Asian, N = Native American) at the P < .05 level with Bonferroni correction for multiple comparisons.
P < .05, **P < .01, ***P < .001.
OUD hospitalizations and hospitalization rates
The number of OUD hospitalizations, hospitalization rates, and mean quarterly hospitalization rates during the observation period can be found in Supplemental Appendix Table 2, and a graphical representation of quarterly OUD hospitalization rates overall and by demographic group are shown in Figure 2. The number of quarterly hospitalizations with an OUD as the primary diagnosis increased from 433 hospitalizations in the first quarter of the study to 1163 hospitalizations in the last quarter of the study period, an increase of 169%.
Figure 2.
Quarterly opioid use disorder hospitalization rates; U.S. older adults, 2007 quarter 4 to 2014 quarter 3.
The mean quarterly OUD hospitalization rate during the study period was 81 per million (SD = 19). Unlike AUD hospitalization rates, the mean quarterly OUD hospitalization rate for men (M = 76, SD = 18) was not significantly different than the rate for women (M = 85, SD = 19, P = .08). Across race/ethnicity, mean quarterly hospitalization rates were highest for Native American (M = 126, SD = 58) and Black (M = 119, SD = 38) older adults, followed by White (M = 86, SD = 19), Latino (M = 15, SD = 5), and Asian (M = 11, SD = 5) older adults (all pairwise comparisons significant at P < .05 with a Bonferroni correction, with the exception of the difference between Native American and Black older adults which was not significant). The number of quarterly OUD hospitalizations was small for Latino, Asian, and Native American older adults (<25/quarter), and the number of OUD hospitalization records with “Unknown” and “Other” for race/ethnicity is in some cases similar or larger than the number of hospitalizations with Latino, Asian, and Native American race/ethnicity (See Supplemental Appendix Figure 1).
The results of the regression analyses showed that the overall trend was positive and statistically significant for OUD quarterly hospitalization rates (Coeff = 2.14 (95% CI = 1.86-2.43), P < .001). Trends were positive and statistically significant at the P < .05 level for all gender and racial/ethnic groups, except for Asian and Native American older adults (see Table 2). The quarterly change in OUD hospitalization rates was not significantly different for men compared to women. However, quarterly hospitalization rates increased significantly faster for Black older adults compared to all other racial/ethnic groups, followed by that of White older adults.
Comorbidities among individuals with an AUD or OUD as primary diagnoses
Figures 3 and 4 show the frequencies of the most common comorbidities for hospitalizations with AUD and OUD as primary diagnosis, as well as results of statistical comparisons in prevalence of those comorbidities by subgroup. For both AUD and OUD hospitalizations, the 3 most common comorbidities were, in order of frequency: circulatory system, endocrine/metabolic/immunological, and mental health conditions (excluding SUDs). As can be seen in the graphs, some differences in frequencies of comorbidities exist by subgroup. For example, circulatory conditions were significantly more common in hospitalizations in men (78%) compared to women (72%); and in Black older adults (81%) relative to older adults of other racial/ethnic groups (71%-76%). On the other hand, mental health comorbidities were significantly more common for White older adults (58%) and significantly less common for Latino (37%) and Asian (38%) older adults hospitalized for an AUD compared to other racial/ethnic groups (48%-58%).
Figure 3.
Most common comorbidities for alcohol use disorder hospitalizations; U.S. older adults, 2007 quarter 4 to 2014 quarter 3.
Note: 1“W” in graph indicates that the prevalence rate of that comorbidity for men is significantly different from that of women, P < .0001. 2Letters within graph indicate that the comorbidity prevalence rate for that racial/ethnic group is significantly different than other racial ethnic group (W = White, B = Black, L = Latino, A = Asian, N = Native American) at the P < .05 level with Bonferroni correction for multiple comparisons. 3Mental disorders do not include alcohol use disorders, opioid use disorders, or any other substance use disorders.
Figure 4.
Most common comorbidities for opioid use disorder hospitalizations; U.S. older adults, 2007 quarter 4 to 2014 quarter 3.
Note: 1 “W” in graph indicates that the prevalence rate of that comorbidity for men is significantly different from that of women, P < .0001. 2Letters within graph indicate that the comorbidity prevalence rate for that racial/ethnic group is significantly different than other racial ethnic group (W = White, B = Black, L = Latino, A = Asian, N = Native American) at the P < .05 level with Bonferroni correction for multiple comparisons. 3Mental disorders do not include alcohol use disorders, opioid use disorders, or any other substance use disorders.
Hospitalizations with AUD and OUD as secondary diagnoses
We also examined hospitalizations and hospitalization rates when AUD and OUD diagnoses were in secondary diagnosis fields. The increase in hospitalization rates was substantially higher when the condition was in the secondary diagnostic fields compared to the increase in hospitalization rates for these conditions as the primary diagnosis (Supplemental Appendix Table 2). Hospitalization rates with an AUD in a secondary diagnosis field increased by 84%, and for OUD in a secondary diagnosis field by 269%. The trends were significant, with an estimated quarterly change in hospitalization rates of 140 hospitalizations per million for AUD (95% CI = 110-169, P < .001) and 29 per million for OUD (95% CI = 26.43-32.17, P < .001). We found that the quarterly increase in hospitalization rates with secondary AUD and OUD diagnoses varied somewhat by subgroup, with men and Black, White, and Native American older adults having some of the largest quarterly increases in hospitalization rates for AUD in secondary diagnoses; and Black older adults having the largest increase in hospitalizations for OUD in secondary diagnoses (See Table 2). Figures 5 and 6 shows quarterly hospitalization rates for AUD and OUD diagnosis in secondary diagnosis fields. As can be seen in these figures, there was a sharp increase in hospitalization rates in Quarter 4 of 2010. This increase is most likely due to the change in Medicare policy where the number of ICD diagnosis code fields on a claim increased from 9 to 25 in fiscal year 2011 (beginning October 2010). 33
Figure 5.
Quarterly hospitalization rates for hospitalization with alcohol use disorder as secondary diagnosis; U.S. older adults, 2007 quarter 4 to 2014 quarter 3.
Figure 6.
Quarterly hospitalization rates for hospitalizations with opioid use disorder as secondary diagnosis in U.S. older adults, 2007 quarter 4 to 2014 quarter 3.
The most common primary diagnoses in hospitalizations when AUD or OUD diagnosis were in a secondary diagnosis field were circulatory system disorders, mental health disorders, digestive disorders, respiratory diseases, and injury and poisoning, although the order of prevalence varied for AUD compared to OUD (See Supplemental Appendix Tables 3–6). For example, for those with an AUD in a secondary diagnosis field, circulatory system diseases were the most prevalent primary diagnoses; but for those with an OUD in a secondary diagnosis field, mental disorders were the most prevalent primary diagnoses. Differences also existed by subgroup. For those with an AUD diagnosis, circulatory systems diseases were the most common primary diagnoses among men, and among White, Black, and Asian older adults. However, among women, mental disorders were the most common primary diagnosis; and among Latinos and Native Americans, digestive diseases were the most common primary diagnosis. Differences also existed across subgroups among hospitalizations for secondary OUD diagnoses. In some subgroups (i.e., Native Americans, and Asians) infections/parasitic conditions were among the top 5 diagnoses for hospitalizations with an OUD in a secondary field, but not for any other group.
Discussion
We examined trends in AUD and OUD hospitalizations and related comorbidities among older adults between 2007 and 2014 and assessed differences by gender and race/ethnicity. We found substantial increases in the number and rates of hospitalizations for AUDs and OUDs between 2007 and 2014 among adults 65 and older, and wide variation in hospitalization rates and in changes in hospitalization rates by gender and race/ethnicity. The increase in AUD hospitalizations among older adults is consistent with reports of higher prevalence of risky drinking, alcohol misuse, and AUDs in the baby boomer cohort (those born in 1946-1964) as well as with AUD hospitalizations rising among those 45 and older using data from earlier time periods.12,14 -16,34 AUD hospitalization rates are substantially higher among men consistent with the documented higher prevalence of unhealthy alcohol drinking among this group 20 and with prior findings focusing on hospitalizations through 2010. 34 The higher increase in hospitalization rates among men is inconsistent with the documented reduction in the gender gap for heavy drinking, AUD prevalence, and alcohol-related mortality, due to larger increases in alcohol use and AUDs among women.12 -18 Because studies that found increases in alcohol outcomes among women have focused on samples younger than 65, it is possible that their impact on hospitalizations among older adults will be observed later, as those cohorts age.
AUD hospitalization rates also varied by race/ethnicity with Black and Native American older adults having higher rates of hospitalizations for these conditions. To the best of our knowledge, prevalence data of alcohol misuse or AUDs in older adults by race/ethnicity is not available, making a comparison between prevalence and hospitalization not possible. But these results highlight the need to pay particular attention to inequities on the impact of AUDs in these racial/ethnic groups.
Hospitalization rates for OUDs increased at a rapid pace among older adults during this short period. A recent analysis using data from the National Inpatient Samples (NIS) also found a steep increase in OUD-related hospitalizations among this age group. 35 Few studies have examined OUDs among older adults, even though there is concern that older adults might have been affected as other age groups have from the increase in prescribing of opioid pain medications in the late 1990s and early 2000s,8,36 and perhaps especially due to high rates of chronic pain experienced by this age group. 37
We found that hospitalization rates for OUDs were similar for men and women, although nationally, opioid overdose death rates among adults 65 to 74 are higher for men 19 and women account for a higher proportion of emergency department visits for opioid misuse. 11 We did find that OUD hospitalization rates were particularly high among Black older adults during this time frame and that the increase in hospitalization rates was highest among this group as well. These findings are in contrast with opioid-involved overdose death rates, which have been generally higher among White older adults, at least in the years following the present study’s years of observations (2015-2017). 24 More recently, the growth in rates of opioid overdose death rates have been higher for Black individuals than for White individuals,25,38 and although drug overdose deaths increased for all racial/ethnic groups between 2019 and 2020 during the first year of the COVID-19 pandemic, Black Americans experienced the highest increase (44%). 39 In our study, the mean quarterly hospitalization rates were highest for Native Americans despite the small number hospitalization records for Native Americans and the likely undercount of hospitalizations for this racial/ethnic group. More attention should be paid to addressing opioid use disorders among older adults in this population, which in 2018 had the second highest rate of opioid related overdose rates. 40
It is worth noting that a substantial number of the hospitalization records we examined had missing information on race/ethnicity. The large amount of missing and misclassified race/ethnicity data can be traced back to the way that Social Security Administration (SSA), the source of race/ethnicity data for Medicare, collected race/ethnicity data. Until 1980, the SSA used only 3 racial/ethnic categories in their applications: White, Black, and Other. There have been efforts to improve Medicare race/ethnicity data and reduce the number of “unknown” or “other” race/ethnicity using surveys and algorithms, as well as working with Indian Health Services for beneficiaries covered by both agencies.41,42 However, our analyses show that gaps in the data remain, likely creating a large undercount of substance use hospitalization rates for Latino, Asian, and Native American older adults. Improving quality of race/ethnicity data in Medicare is imperative for identifying and addressing racial/ethnic disparities in health and health care among older adults.
Comorbidities
For both AUD and OUD hospitalizations, the 3 most common comorbidities were circulatory system diseases; endocrine, nutritional, metabolic, and immunological diseases; and mental health conditions. Circulatory system diseases are the most common primary diagnoses for hospitalizations for older adults in general. 43 Endocrine, nutritional, metabolic, immunological diseases are more common in our samples than in the general older adult population, perhaps reflecting the impact that long-term alcohol and opioid use have on the endocrine system.43 -45 Mental health conditions are also more common in our sample than in the general adult population, 43 consistent with the well-documented co-occurrence of mental health and substance use disorders, although research on co-occurring disorders among older adults is limited.46,47 Our study suggests older adults suffering from substance use disorders should be assessed and treated for mental health conditions and vice-versa. Substance use disorders on their own are now considered a risk factor for getting severely ill from COVID-19, as are having a mental health condition and cardiovascular diseases. As the risk of severe illness from COVID-19 increases with the number of conditions an individual has and for those older than 65, older adults with substance use disorders and mental health conditions seem particularly high risk of severe illness from COVID-19. 48
We found some differences by gender and race/ethnicity in comorbidities. This may reflect differences in the prevalence of diseases, such as Black older adults generally having higher rates of circulatory conditions than other racial/ethnic groups. Some differences worth noting are those related to mental health comorbidities. Among those hospitalized for an AUD or OUD, women had higher rates of mental health comorbidities than men and racial/ethnic minority older adults hospitalized for an AUD and OUD had lower rates of mental health comorbidities than White older adults. Racial/ethnic differences could be due to lower prevalence of mental health conditions in general among older adults in these racial/ethnic groups. But these differences could also be due to disparities in access to mental health care, 49 leading to lower rates of diagnoses.
Hospitalizations with AUD and OUD as secondary diagnoses
For the most part, we found similar patterns of primary diagnoses for those hospitalizations that had AUD or OUD in a secondary diagnostic field, and by gender and race/ethnicity. Circulatory diseases, digestive diseases, injury and poisoning, respiratory diseases, and mental health conditions (excluding SUDs) were the most common primary diagnoses, though the order of commonality varied. For example, the most common primary diagnoses for hospitalizations when AUD was not in the primary field were circulatory systems diseases followed by digestive diseases, but for OUD the 2 most common primary diagnoses were for mental health disorders followed by respiratory diseases. More research is needed to understand this variation.
Strengths and limitations
Our study has several strengths. We used a dataset that includes 100% of hospitalizations records of Medicare beneficiaries. Medicare covers hospitalizations for almost the entire population of adults 65 and older in the United States, allowing us to analyze trends in AUD and OUD hospitalizations and related comorbidities with the highest degree of accuracy possible. Our study adds to the scant literature on AUD and OUD among this age group, and even more limited literature on health care utilization for these conditions in this population, even though there have been calls for more research in these areas for some time. 50 Additionally, to the best of our knowledge, this is the first study examining comorbidities in older adults hospitalized for an AUD or OUD. Finally, our examination of differences by gender and race/ethnicity is also an important contribution, particularly as our findings highlighted striking disparities in hospitalizations for these conditions.
Several limitations should be noted. Our study was restricted through 2014. However, there are no other studies with more recent data available, particularly ones that include analyses of differences by subgroups or comorbidities. Future studies should examine trends using more recent data and findings from this study provides baseline information that could be used to compare with more recent trends.
It is important to note the jump in hospitalization rates seen in 2011 for hospitalizations with a secondary AUD/OUD diagnosis. This is likely due to a change in Medicare billing where the number of diagnostic codes allowed increased from 9 to 25. 51 Research is needed to understand whether having more diagnostic fields helps reflect a more accurate picture of hospitalizations of patients with AUD and OUD.
Implications and future research
Our findings highlight the need to pay increased attention to AUD and OUD among adults 65 and older. This is particularly important given that the U.S. population is aging, with older adults making up a larger proportion of the population. Our findings suggest that if trends continued at the same rate, the projected AUD hospitalization rate among older adults would have increased by 61% from the end of 2007 to the end of 2021, and the OUD hospitalization rate by 234%, a concerning increase in a relative short time period.
These projections could be used for examining the impact of COVID-19 on older adults’ use of alcohol and other substances. The number of drug overdose deaths has increased substantially for most age groups during the pandemic, including older adults, 52 as did drinking in older adults with depression and anxiety,53,54 and it would be important to assess the impact of these changes on the health care system using more recent data. In particular, more attention is needed to address the relatively high rate of AUD and OUD hospitalizations in Black older adults and the faster increase in AUD- and OUD-related hospitalizations among this population indicating that disparities are widening. The population of older adults is becoming substantially more racially/ethnically diverse, with estimates that by 2050, 39% of individuals 65 and older will be racial/ethnic minorities. 30 Investment in research for prevention and intervention to address the specific needs of people of color with AUDs and OUDs is imperative. At the same time, the quality and completeness of race/ethnicity data for Medicare data, the main source of payment for medical care among older adults, should be improved. These data are critical to measure, understand, and address racial/ethnic disparities in heath and health care of older adults, and ultimately make progress toward health equity in the aging population in the United States.
Additionally, the pandemic has highlighted structural racial/ethnic inequalities in the United States.55 -58 SUDs and racial/ethnic inequalities can intersect and could make some racial/ethnic minority groups particularly vulnerable to the impact of COVID-19. In fact, a recent study found that among patients with a recent diagnosis of a SUD, Black Americans were at greater risk of being infected with COVID-19 and had worse COVID-19 outcomes (including hospitalizations and death) compared to White Americans. 59 Comparing more recent data on hospitalizations for AUD and OUD among older adults by race/ethnicity with projections using our study findings could provide a more complete picture of the impact of the pandemic for different groups.
The U.S. Preventive Services Task Force recommends screening for unhealthy alcohol use for adults, 60 but in general, screening is not widely implemented and there is little recent information on the prevalence and impact of screening for unhealthy alcohol use among older adults. Additionally, interventions to specifically help with unhealthy substance use among older adults are needed. The proportion of substance use treatment admissions that are made up of older adults is already increasing. 61 Our findings add to the urgent call to prepare the health care workforce to care for older adults who have substance use conditions. 50 In addition to health care, substance use specialty treatment facilities might want to include special programing for older adults. Currently, only 25% of substance use treatment facilities report special programs for older adults. 62
Conclusion
Our study findings provide an important snapshot some years before the pandemic of the growing impact of substance use disorders on this vulnerable population, which have likely been exacerbated by the COVID-19 pandemic. Research using more recent data is needed to determine the current extent of AUD and OUD hospitalizations among older adults, the current trajectory of these hospitalizations, as well as the impact of COVID-19 on older adults with substance use disorders. As hospitalization is an important step to avoid mortality, and alcohol- and opioid-related deaths have surged during the pandemic, our findings point to the urgency of addressing the impact of these disorders among older adults.
Supplemental Material
Supplemental material, sj-docx-1-sat-10.1177_11782218221116733 for Hospitalizations for Alcohol and Opioid Use Disorders in Older Adults: Trends, Comorbidities, and Differences by Gender, Race, and Ethnicity by Andrea Acevedo, Ivette Rodriguez Borja, Tania M Alarcon Falconi, Nicole Carzo and Elena Naumova in Substance Abuse: Research and Treatment
Acknowledgments
Not Applicable.
Footnotes
List of Abbreviations: AUD = Alcohol use disorders
OUD = Opioid use disorders
U. S. = United States
Authors’ Contributions: All authors contributed to the conceptualization of the study and study design. E.N.N facilitated data acquisition. T.A.F., I.R.B., and N.C. assisted with data preparation. A.A. conducted the analyses and drafted the manuscript with important contributions from E.N.N. and I.R.B. All authors edited the manuscript and read and approved the final manuscript.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was partially supported by the FRAC Summer Faculty Fellowship at Tufts University. The Tufts University Faculty Research Awards Committee covered open access publication fees.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: This study was determined to be exempt by the Tufts Medical Center/Tufts University Health Sciences Institutional Review Board (IRB protocol #: 13332).
Consent for Publication: Not Applicable
Availability of Data and Materials: The datasets analyzed during the current study are available from the Centers for Medicare and Medicaid Services. Restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Johnson RA, Gerstein DR. Initiation of use of alcohol, cigarettes, marijuana, cocaine, and other substances in US birth cohorts since 1919. Am J Public Health. 1998;88:27-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kuerbis A, Sacco P, Blazer DG, Moore AA. Substance abuse among older adults. Clin Geriatr Med. 2014;30:629-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wu LT, Blazer DG. Substance use disorders and psychiatric comorbidity in mid and later life: a review. Int J Epidemiol. 2014;43:304-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Salas-Wright CP, Vaughn MG, Cummings-Vaughn LA, et al. Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002-2014. Drug Alcohol Depend. 2017;171:97-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Han B, Gfroerer JC, Colliver JD, Penne MA. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104:88-96. [DOI] [PubMed] [Google Scholar]
- 6. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on alcohol and Related Conditions. JAMA Psychiatr. 2017;74:911-923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paulozzi L, Jones C, Mack K, Rudd R. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. JAMA. 2011;306:2444-2446. [PubMed] [Google Scholar]
- 8. Guy GP, Jr, Zhang K, Bohm MK, et al. Vital Signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66:697-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Substance Abuse and Mental Health Administration. Opioid misuse increases among older adults. 2017. https://www.samhsa.gov/data/sites/default/files/report_3186/Spotlight-3186.html. Accessed September 4, 2017.
- 10. Schepis TS, McCabe SE. Trends in older adult nonmedical prescription drug use prevalence: results from the 2002-2003 and 2012-2013 National Survey on Drug Use and health. Addict Behav. 2016;60:219-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carter MW, Yang BK, Davenport M, Kabel A. Increasing rates of opioid misuse among older adults visiting emergency departments. Innov Aging. 2019;3:igz002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Stud Alcohol. 1997;58:464-473. [DOI] [PubMed] [Google Scholar]
- 13. Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend. 2008;93:21-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Holdcraft LC, Iacono WG. Cohort effects on gender differences in alcohol dependence. Addiction. 2002;97:1025-1036. [DOI] [PubMed] [Google Scholar]
- 15. Rice JP, Neuman RJ, Saccone NL, et al. Age and birth cohort effects on rates of alcohol dependence. Alcohol Clin Exp Res. 2003;27:93-99. [DOI] [PubMed] [Google Scholar]
- 16. Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: a review and Synthesis. Alcohol Clin Exp Res. 2011;35:2101-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Han BH, Moore AA, Sherman S, Keyes KM, Palamar JJ. Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005-2014. Drug Alcohol Depend. 2017;170:198-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Breslow RA, Castle IJ, Chen CM, Graubard BI. Trends in alcohol consumption among older Americans: National Health Interview Surveys, 1997–2014. Alcohol Clin Exp Res. 2017;41:976-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Centers for Disease Control. Drug overdoses: Data for the U.S. https://www.cdc.gov/nchs/fastats/drug-overdoses.htm. 2020. Accessed September 18, 2020.
- 20. Substance Abuse and Mental Health Services Administration. 2019 NSDUH Detailed Tables. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 21. Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Netw Open. 2020;3:e1921451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Keyes KM, Liu XC, Cerda M. The role of race/ethnicity in alcohol-attributable injury in the United States. Epidemiol Rev. 2012;34:89-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yoon Y-H, Chen CM. Liver Cirrhosis Mortality in the United States: National, State, and Regional Trends, 2000–2013 [Surveillance Report #105]. Arlington, VA: National Institute on Alcohol Abuse and Alcoholism; 2016. [Google Scholar]
- 24. Lippold KM, Jones CM, Olsen EO, Giroir BP. Racial/ethnic and age group differences in opioid and synthetic opioid–involved overdose deaths among adults aged ⩾18 years in metropolitan areas — United States, 2015–2017. MMWR Morb Mortal Wkly Rep. 2019;68:967-973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Furr-Holden D, Milam AJ, Wang L, Sadler R. African Americans now Outpace Whites in opioid-involved overdose deaths: a comparison of temporal trends from 1999 to 2018. Addiction. 2021;116:677-683. [DOI] [PubMed] [Google Scholar]
- 26. Larochelle MR, Slavova S, Root ED, et al. Disparities in opioid overdose death trends by race/ethnicity, 2018–2019, from the HEALing Communities Study. Am J Public Health. 2021;111:1851-1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Census Bureau. 2010. Census Shows 65 and Older Population Growing Faster Than Total U.S. Population. https://www.census.gov/newsroom/releases/archives/2010_census/cb11-cn192.html. 2011. Accessed September 10, 2017.
- 28. Administration on Aging. 2020. Profile of Older Americans. https://acl.gov/aging-and-disability-in-america/data-and-research/profile-older-americans. 2021. Accessed January 7, 2022.
- 29. Census Bureau. Facts for Features: Older Americans Month. https://www.census.gov/newsroom/facts-for-features/2017/cb17-ff08.html. 2017. Accessed September 10, 2017.
- 30. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States. Vol P25-1140. U.S. Census Bureau; 2014. [Google Scholar]
- 31. (ResDAC) RDAC. Strengths and Limitations of CMS Administrative Data in Research. https://www.resdac.org/articles/strengths-and-limitations-cms-administrative-data-research. 2020. Accessed June 15, 2020.
- 32. Boersma P, Black LI, Ward BW. Prevalence of multiple chronic conditions among US adults, 2018. Prev Chronic Dis. 2020;17:E106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mues KE, Liede A, Liu J, et al. Use of the Medicare database in epidemiologic and health services research: a valuable source of real-world evidence on the older and disabled populations in the US. Clin Epidemiol. 2017;9:267-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sacco P, Unick GJ, Kuerbis A, Koru AG, Moore AA. Alcohol-related diagnoses in hospital admissions for all causes among middle-aged and older adults: trends and cohort differences from 1993 to 2010. J Aging Health. 2015;27:1358-1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Weiss AJ, Heslin KC, Barrett ML, Izar R, Bierman A. Opioid-Related Inpatient Stays and Emergency Department Visits Among Patients Aged 65 Years and Older, 2010 and 2015. HCUP Statistical Brief #244. Agency for Healthcare Research and Quality; 2018. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb244-Opioid-Inpatient-Stays-ED-Visits-Older-Adults.pdf [PubMed] [Google Scholar]
- 36. Boudreau D, Von Korff M, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009;18:1166-1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67:1001-1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kline D, Pan Y, Hepler SA. Spatiotemporal trends in opioid overdose deaths by race for counties in Ohio. Epidemiology. 2021;32:295-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hedegaard H, Miniño AM, Spencer MR, Warner M. Drug overdose deaths in the United States, 1999-2020. NCHS Data Brief. 2021;1-8. [PubMed] [Google Scholar]
- 40. Wilson N, Kariisa M, Seth P, Smith H, 4TH, Davis NL. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69:290-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zaslavsky AM, Ayanian JZ, Zaborski LB. The validity of race and ethnicity in enrollment data for Medicare beneficiaries. Health Serv Res. 2012;47:1300-1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Filice CE, Joynt KE. Examining Race and ethnicity information in Medicare administrative data. Med Care. 2017;55:e170-e176. [DOI] [PubMed] [Google Scholar]
- 43. Agency for Healthcare Research and Quality. Data Query Tools. Healthcare Cost and Utilization Project (HCUP). https://www.hcup-us.ahrq.gov/dataquerytools.jsp. 2021. Accessed January 5, 2022. [PubMed]
- 44. Katz N, Mazer NA. The impact of opioids on the endocrine system. Clin J Pain. 2009;25:170-175. [DOI] [PubMed] [Google Scholar]
- 45. Rachdaoui N, Sarkar DK. Pathophysiology of the effects of alcohol abuse on the endocrine system. Alcohol Res. 2017;38:255-276. [PMC free article] [PubMed] [Google Scholar]
- 46. Bartels SJ, Blow FC, Van Citters AD, Brockmann LM. Dual diagnosis among older adults: co-occurring substance abuse and psychiatric illness. J Dual Diagn. 2006;2:9-30. [Google Scholar]
- 47. Searby A, Maude P, McGrath I. Dual diagnosis in older adults: a review. Issues Ment Health Nurs. 2015;36:104-111. [DOI] [PubMed] [Google Scholar]
- 48. Centers for Disease Control and Prevention. COVID-19: People with Certain Medical Conditions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. 2021. Accessed November 30, 2021. [PubMed]
- 49. Cook BL, Trinh N-H, Li Z, Hou SS, Progovac AM. Trends in racial-ethnic disparities in access to mental health care, 2004-2012. Psychiatr Serv. 2017;68:9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. IOM (Institute of Medicine). The Mental Health and Substance Use Workforce for Older Adults: In Whose Hands? The National Academies Press; 2012. [PubMed] [Google Scholar]
- 51. Centers for Medicare and Medicaid Services. CMS manual system: Pub 100-04 Medicare claims processing. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R2028CP.pdf. 2010. Accessed October 6, 2021.
- 52. Centers for Disease Control and Prevention. Provisional Drug Overdose Deaths by Quarter and Demographic Characteristics 2019 to 2020. https://www.cdc.gov/nchs/data/health_policy/Provisional-Drug-Overdose-Deaths-by-Quarter-and-Demographic-Characteristics-2019-to-2020.pdf. 2021. Accessed October 6, 2021.
- 53. Capasso A, Jones AM, Ali SH, Foreman J, Tozan Y, DiClemente RJ. Increased alcohol use during the COVID-19 pandemic: the effect of mental health and age in a cross-sectional sample of social media users in the U.S. Prev Med. 2021;145:106422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Eastman MR, Finlay JM, Kobayashi LC. Alcohol use and mental health among older American adults during the early months of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:4222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol consumption during the COVID-19 pandemic: a cross-sectional survey of US adults. Int J Environ Res Public Health. 2020;17:9189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pollard MS, Tucker JS, Green HD., Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3:e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. McKnight-Eily LR, Okoro CA, Strine TW, et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic - United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2021;70:162-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Roberts A, Rogers J, Mason R, et al. Alcohol and other substance use during the COVID-19 pandemic: a systematic review. Drug Alcohol Depend. 2021;229:109150-109150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2021;26:30-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Curry SJ, Krist AH, Owens DK, et al. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320:1899-1909. [DOI] [PubMed] [Google Scholar]
- 61. Chhatre S, Cook R, Mallik E, Jayadevappa R. Trends in substance use admissions among older adults. BMC Health Serv Res. 2017;17:584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS): Data on Substance Abuse Treatment Facilities. Substance Abuse and Mental Health Services Administration; 2020:2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sat-10.1177_11782218221116733 for Hospitalizations for Alcohol and Opioid Use Disorders in Older Adults: Trends, Comorbidities, and Differences by Gender, Race, and Ethnicity by Andrea Acevedo, Ivette Rodriguez Borja, Tania M Alarcon Falconi, Nicole Carzo and Elena Naumova in Substance Abuse: Research and Treatment