Abstract
Objective
Assessing the level of eHealth literacy in a population is essential to designing appropriate public health interventions. This study aimed to assess eHealth literacy among adult internet users in Lebanon, recruited through social media and printed materials. The study examined the relationship between internet use, perceived eHealth literacy, and sociodemographic characteristics.
Methods
A cross-sectional study based on a web-based questionnaire was conducted between January and May 2020. The survey assessed internet use and eHealth literacy using the homonymous scale (eHEALS) in English and Arabic. Cronbach's alpha and factor analyses were used to evaluate eHEALS’ psychometric properties. A generalized linear model was used to identify factors predicting the eHEALS.
Results
A total of 2715 respondents were recruited mostly through Facebook (78%) and printed materials (17%). Most respondents completed the survey in English (82%), were aged 30 ± 11 years, female (60%), Lebanese (84%), unmarried (62%), employed (54%), and with a graduate-level education (53%). Those who completed the eHEALS questionnaire (n = 2336) had a moderate eHealth literacy (M = 28.7, SD = 5.5). eHEALS was significantly higher among older females with a high education level, recruited from Facebook, Instagram, or ResearchGate, and perceived the Internet as a useful and important source of information.
Conclusions
Future internet-delivered public health campaigns in Lebanon should account for moderate-to-low levels of eHealth literacy and find ways to engage older males with low education levels representing neglected segments (e.g. Syrians). To be more inclusive, campaigns should reach neglected population segments through non-digital, community-based outreach activities.
Keywords: Health literacy, internet, information seeking behavior, consumer health information, Lebanon
Introduction
Internet as a source of health information
The active internet population is growing worldwide, rising from 4.6 billion in January 2021 1 to 5 billion in April 2022, reaching a 63% penetration rate. 2 However, internet penetration rates range widely, from 98% in Northern Europe to 25% in central Africa 3 ; the highest rates were recorded in Denmark, the United Arab Emirates (UAE), and Ireland (99%), followed by South Korea, the United Kingdom, Switzerland, and Saudi Arabia (98%). 4 In the Middle East, the average penetration rate in 2021 was 75%, with the lowest rate recorded in Yemen (26%). 5 These figures demonstrate that internet access is yet to be universal, and the “digital divide” 6 affects both developing and developed countries. 7 This discrepancy exacerbates existing health, and social inequalities, particularly that rich and highly educated individuals can benefit from internet resources.8–10 The internet is a common source of health-related information globally11,12 and in the Arab world.13–15 Research evidence consistently confirms that individuals with access to online information are more likely to have better health literacy,16,17 which translates into better health outcomes.18–20 Examining the approaches people adopt to access health information online is fundamental to expanding the reach and impact of internet-delivered public health campaigns.10,21–25
eHealth literacy
Digital health interventions and campaigns assume that users possess the ability to “seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem,” 26 a complex skillset that Norman and Skinner 26 called “eHealth literacy.” In 2006, Norman and Skinner 26 proposed a conceptual model of eHealth literacy, metaphorically represented as a lily flower with six petals representing as many types of skills, three analytical (functional, media, and information literacies), and three context-specific (scientific, health, and computer literacies). The analytical skills can apply to any information-seeking context, whereas the context-specific abilities cannot be easily transferred to different domains. 26 For example, when searching for information online, one must know how to read and write or type (functional literacy), learn how to use the device to search (e.g. computer literacy), know how to search and which databases to consult (information literacy). Finally, one must appraise the information, its quality, and sources (media literacy) and discern amongst scientific data related to a specific health topic (scientific and health literacies). The eHealth literacy model is mainly conceptual as the outlined six skills are not easily acquired.21,27,28 Some research demonstrated a close link between health literacy and eHealth literacy,21,27 with the latter being associated with improved health outcomes in various digital health interventions.8,10 A recent scoping review looking at the application of the eHealth literacy model in digital interventions noted that eHealth literacy and health literacy were the two most frequently assessed domains of the Lily model. 22 Understanding the level of eHealth literacy is essential in developing public health campaigns that are inclusive by design, practical, and effective. For instance, knowing the level of eHealth literacy allows campaign designers to adapt the content and decide the best channel to deliver it.
Assessing eHealth literacy
The first tool designed to assess eHealth literacy is the homonymous scale (“eHEALS”), created by Norman and Skinner. 29 Designed as a self-reported instrument, it is intended to assess an individual's perception of their skills and knowledge about finding, appraising, and using information online. 29 The eHEALS consists of eight questions (see Table 4), chosen through an iterative scale development process, 29 to assess the perceived ability to seek, find, understand, and appraise information online, closely representing the Lily model. 30 The eHEALS demonstrated good reliability, showing good internal consistency (Cronbach's alpha = 0.88), 29 which was consistently confirmed in many eHEALS studies done in different languages.31–36 However, the eHEALS was developed in 2006 when there were no social media sites, and the internet looked much more static than it is today. In 2011, Norman 37 admitted that the instrument needed some improvements and updates. The items referred to the internet in generic terms, not acknowledging that individuals might find information through social networking sites. Between 2009 and 2014, several other eHealth literacy assessments were developed to overcome some eHEALS conceptual and methodological limitations, according to existing systematic reviews.30,38 The most recent study, by Lee et al., 30 identified six additional instruments: the “eHealth literacy scale–extended” (eHEALS-E), 39 the “electronic health literacy scale” (e-HLS), 40 the “digital health literacy instrument” (DHLI), 41 the “eHealth literacy assessment toolkit” (eHLA), 42 the “eHealth literacy questionnaire,” (eHLQ) 43 and the “transactional eHealth literacy instrument” (TeHLI). 44 While some instruments were based on the original eHEALS, many proposed several new items that diverged from the original eHealth literacy model. All new eHealth literacy assessment tools provided evidence supporting their psychometric properties, but this was limited to the respective validation study. 30
Table 4.
Model fit indices of EFAs and CFAs completed (n = 2336).
| Model | χ² (df) | CFI | TLI | SRMR | RMSEA (90% CI) | AIC | BIC |
|---|---|---|---|---|---|---|---|
| 1. EFA single factor | 1039.56** (20) | 0.854 | 0.148 (0.140–0.155) | 884.43 | |||
| 2. EFA three factor | 54.54**(7) | 0.981 | 0.054 (0.041–0.068) | 0.24 | |||
| 3. CFA single factor | 1067.84** (20) | 0.895 | 0.853 | 0.051 | 0.148 (0.141–0.156) | 44927.91 | 45066.50 |
| 4. CFA three factors as identified in Model 2 | 298.56** (17) | 0.972 | 0.953 | 0.027 | 0.083 (0.075–0.092) | 40419.52 | 40575.43 |
| 5. CFA three factors with modifications | 141.28** (15) | 0.988 | 0.986 | 0.019 | 0.047 (0.039–0.054) | 40266.25 | 40433.71 |
| 6. CFA three factors from the literature | 628.50** (17) | 0.939 | 0.899 | 0.040 | 0.123 (0.115–0.131) | 40749.46 | 40905.37 |
Note: CFI: comparative fit index; TLI: Tucker-Lewis index; SRMR: standardized root mean square residual; RMSEA: root mean square error of approximation; AIC: Akaike information criterion. BIC: Bayesian Information Criterion.
* p < 0.05, **p < 0.001.
Most of the criticisms of the eHEALS revolve around its factor structure. In the original eHEALS study, 29 Norman and Skinner 29 used principal component analysis (PCA) based on eigenvalues above 1. While the authors did not report model fit indices, they identified a single factor explaining 56% of the variance in the data, with factor loadings ranging from 0.60 to 0.84 across the eight items. However, several studies questioned the validity of a single-factor solution (e.g.33,35,45–48). For example, Sudbury-Riley et al. 45 and Brørs et al., 35 who tested the eHEALS using confirmatory factor analyses (CFAs), reported that a single-factor was not fitting the data as well as a three-factor solution. The authors of these studies argued that items 1–3 were assessing a latent factor, “awareness of what health sources are available,” that items 3–5 were expressing the latent factor “skills and behaviors needed to access health resources,” and the items 5–8 indicated a factor labeled “evaluation of health resources once accessed.”35,45 Similar findings were reported in eHEALS studies employing exploratory factor analyses (EFA),49,50 arguably deemed appropriate when testing translated instruments and new populations (see eHEALS translations in Hungarian, 51 Polish, 52 Serbian, 36 Spanish, 50 Korean, 53 Chinese, 49 and Arabic 54 ). These studies supported the superiority of a multi-factor over a single-factor solution. Yet, despite its criticisms and limitations, the eHEALS remains the most frequently used instrument to assess eHealth literacy, according to systematic reviews on the topic.30,38 A systematic review of eHealth literacy interventions among older adults found that the eHEALS was used in 16 of the 27 selected studies (59%). 55 Additionally, the eHEALS has been translated into 18 languages and validated across 26 countries, 30 making it an ideal instrument for cross-cultural comparisons.
eHealth literacy assessment in the Middle East and Arab World
The eHealth literacy research in the Middle East and the Arab world is limited to affluent countries of the Gulf-Cooperating Council (GCC), 56 including Kuwait 57 and Saudi Arabia,58–60 and Jordan. 61 Most of these studies used the eHEALS to assess eHealth literacy among internet users, 57 nursing students,60,61 and patients living with diabetes 58 and breast cancer, 59 demonstrating the instrument's flexibility and convergent validity. Recently, the eHEALS was validated in Arabic among a sample of native speakers living in Sweden. 54 However, to our knowledge, no studies assessed eHealth literacy in Lebanon, a country in the Eastern Mediterranean region with a high internet penetration rate comparable to those of the neighboring Jordan and GCC countries. As of January 2022, there were more than 6 million internet users (89% penetration rate) and 5.1 million active social media users. 62 In the last decade, the Lebanese Ministries of Public Health and Telecommunications have invested in digital transformation, establishing an eHealth unit, and fostering some programs and campaigns. Some preliminary evidence shows that digital technologies could be used to facilitate access to a heavily privatized public health infrastructure.63–65 Lebanon has recently become constrained by multiple economic, financial, sociopolitical, and health crises hindering livelihoods 66 and making it difficult to manage the COVID-19 outbreak that started in February 2020. 67 In this context, heavily characterized by high levels of COVID-19-related misinformation on social media,68–70 factors such as education, literacy, and social norms play a crucial role in respecting COVID-19 guidelines. 71 Understanding the level of eHealth literacy in the Lebanese population is essential to developing an adequate and efficient response to the pandemic and other public health issues.
This study aimed to (1) examine what health-related information internet users residing in Lebanon seek and why; (2) assess the level of eHealth literacy; and (3) determine which demographic characteristics and Internet usage patterns were associated with eHealth literacy. The results will allow us to make recommendations for governmental and non-governmental policy makers and designers of public health campaigns in the country.
Materials and methods
Study design
A cross-sectional study was conducted using an anonymous, web-based questionnaire. The study received ethical approval from the Institutional Review Board (IRB) of the American University of Beirut (AUB) (ref. number: SBS-2019–0503; 27/12/2019).
Population and sample size
Participants were eligible if they were adults residing in Lebanon and provided informed consent. Considering the existing 5 million internet users, of which four were social media users,62,72 assuming a confidence level of 95% and a 5% margin of error, the estimated minimum sample size was 385.
Recruitment strategy
Participants were recruited between January 27 and 5 May 2020, using digital and printed communication materials distributed at two large university campuses, local community-based health organizations, schools, and religious centers in Beirut. Printed materials included a QR code linking to the web-based questionnaire. The study was also advertised on Facebook with four paid posts in February and April. One post included a screenshot representing a Google search for “Coronavirus in Lebanon,” which attracted much traffic. The link to the questionnaire was diffused on the institution's official Twitter, Facebook, and Instagram profiles, and on our personal profiles on Twitter, Facebook, Instagram, ResearchGate, and Linkedin. Participation was entirely voluntary, and no incentives were provided. Participants could skip any questions or quit the survey at any time.
Questionnaire
The questionnaire was created using LimeSurvey 73 and was available in English and Arabic. It collected data on participants’ demographics (age, gender, nationality, marital status, employment, education); internet use (i.e. number of hours spent online per day); the types of information sought, and reasons for seeking information (multiple-choice questions) 57 ; perceived usefulness and perceived importance of the internet as a source of health information (5-point scales: not useful/beneficial; not important/very important)57,61; the eHEALS, 29 entailing a battery of eight 5-point Likert-type items (1, strongly disagrees and 5, strongly agree), showing excellent internal consistency (Cronbach's alpha = 0.88). 29 Since the eHEALS was not yet translated into Arabic in late 2019 when this study was designed, the version used in the Kuwaiti study 57 was adapted to the Lebanese Arabic variety and piloted to test comprehension and language appropriateness.
Data analyses
Data collected from LimeSurvey was exported into Excel, cleaned, and prepared for the analyses completed in JASP. 74 Descriptive statistics summarized demographic characteristics, types, and reasons for seeking health information online, perceived internet usefulness and importance, and the eHEALS items. Once the psychometric properties were verified, a total eHEALS score was computed by summing all eight items (range: 8–40), the median point of 26 being the threshold for high literacy as reported in various eHEALS studies,57,61,75 including the recent Arabic validation. 54
As web-based surveys inevitably generate missing outcome data, missing value analyses were conducted on the eHEALS items and scale. We created a binary variable to distinguish between those respondents who answered all eight items of the eHEALS and those who completed less than that eight items. Sensitivity analyses were conducted to compare those who completed all eHEALS items to those who did not. Bivariate associations were explored using Chi-square, t-tests, ANOVAs, and Pearson's r.
As this was the first study to employ eHEALS in Lebanon, its psychometric properties were tested by examining its internal consistency and factor structure. Internal consistency was examined using Cronbach's alpha, 76 whereas its factor structure was examined through exploratory (EFA) and CFAs,77,78 following other similar eHEALS studies.49,50 While CFA is generally performed with established instruments, EFA is deemed appropriate when testing tools with new populations. Furthermore, EFA allows testing the adequacy of the sample using the Kaiser-Meyer-Olkin index (> 0.80) and of the data structure (i.e. significant Bartlett's test of sphericity). 77 Using a varimax rotation, EFA was used to establish the optimal factor structure based on eigenvalues above 1. 36 The goodness of fit of EFA models was based on the Chi-square test (p < 0.001), the Tucker-Lewis index (TLI > 0.95), and the root mean square error of approximation (RMSEA < 0.07, p < 0.05). The Bayesian information criterion (BIC) was performed to define model performance. The goodness of fit of CFA models was based on the Chi-square test, TLI, RMSEA, the comparative fit Index (CFI > 0.95), and the standardized root mean square residual (SRMR < 0.05).79,80 Models were compared according to the Akaike Information Criterion (AIC) and BIC (the smaller values, the better).35,81 Modification indices were inspected to identify sources of poor fit.
A generalized linear model employing a Gaussian distribution and an identity link function with robust standard errors82,83 was used to estimate eHEALS based on all sociodemographic variables, internet use, and perceived usefulness, importance, and the number of reasons for seeking health information.
Results
Sample characteristics
A total of 3904 internet users accessed the survey during the recruitment window. Of these, 191 were ineligible, 35 did not consent, and 963 consented but failed to complete the survey. The remaining 2715 provided informed consent and completed the questionnaire. Table 1 summarizes the sociodemographic profile and internet usage characteristics of the sample.
Table 1.
Characteristics of the total sample and eHEALS completers and non-completers.
| eHEALS
completers n = 2336 |
eHEALS
non-completers n = 379 |
Total
sample n = 2715 |
p-valuea | |
|---|---|---|---|---|
| Recruitment channel, n (%) | 0.097 | |||
| Printed | 418 (17.9) | 49 (12.9) | 467 (17.2) | |
| 1809 (77.4) | 315 (83.1) | 2124 (78.2) | ||
| 28 (1.2) | 2 (0.5) | 30 (1.1) | ||
| 55 (2.4) | 8 (2.1) | 63 (2.3) | ||
| 4 (0.2) | 0 (0.0) | 4 (0.15) | ||
| 6 (0.3) | 0 (0.0) | 6 (0.2) | ||
| ResearchGate | 16 (0.7) | 5 (1.3) | 21 (0.8) | |
| Language of survey, n (%) | 0.051 | |||
| Arabic | 436 (18.7) | 55 (14.5) | 491 (18.1) | |
| English | 1900 (81.3) | 324 (85.5) | 2224 (81.9) | |
| Age, M (SD) [18–83] | 30.42 (10.51) | 28.21 (10.35) | 30.11 (10.51) | <0.001 |
| Gender, n (%) | 0.008 | |||
| Male | 881 (37.7) | 171 (45.1) | 1052 (38.7) | |
| Female | 1424 (60.9) | 200 (52.8) | 1624 (59.8) | |
| Not specified/no answer | 31 (1.3) | 8 (2.1) | 39 (1.4) | |
| Nationality, n (%) | 0.071 | |||
| Lebanese | 1948 (83.4) | 324 (85.5) | 2272 (83.7) | |
| Syrian | 187 (8.0) | 19 (5.0) | 206 (7.6) | |
| Palestinian/other | 191 (8.2) | 32 (8.4) | 223 (8.2) | |
| Not specified/no answer | 10 (0.4) | 4 (1.1) | 14 (0.5) | |
| Marital status, n (%) | 0.003 | |||
| Single | 1431 (61.3) | 263 (69.4) | 1694 (62.4) | |
| Married/divorced/widowed | 893 (38.2) | 110 (29.0) | 1003 (36.9) | |
| Not specified/no answer | 12 (0.5) | 6 (1.6) | 18 (0.7) | |
| Employment status, n (%) | <0.001 | |||
| Unemployed | 1016 (43.5) | 204 (53.8) | 1220 (44.9) | |
| Employed | 1308 (56.0) | 171 (45.1) | 1479 (54.5) | |
| Not specified/no answer | 12 (0.5) | 4 (1.1) | 16 (0.6) | |
| Education, n (%) | <0.001 | |||
| High school or less | 380 (16.3) | 74 (19.5) | 454 (16.7) | |
| Undergraduate level | 689 (29.5) | 122 (32.2) | 811 (29.9) | |
| Graduate level or PhD | 1258 (53.9) | 176 (46.4) | 1434 (52.9) | |
| Not specified/no answer | 9 (0.4) | 7 (1.8) | 16 (0.6) | |
| Internet use, n (%) | 0.198 | |||
| Less than 1 h/day | 51 (2.2) | 3 (0.8) | 54 (2.0) | |
| 1–3 h/day | 571 (24.4) | 57 (15.0) | 628 (23.1) | |
| 3–5 h/day | 778 (33.3) | 61 (16.1) | 839 (30.9) | |
| More than 5 h/day | 924 (39.6) | 62 (16.4) | 986 (36.3) | |
| Not specified/no answer | 12 (0.5) | 196 (51.7) | 208 (7.7) | |
| Perceived internet usefulness, M (SD) [1–5 = very useful] |
3.79 (0.79) | 3.54 (0.92) | 3.77 (0.80) | <0.001 |
| Perceived internet importance, M (SD) [1–5 = very important] |
4.13 (0.78) | 3.86 (0.84) | 4.11 (0.78) | <0.001 |
| No. of reasons for seeking information online, M (SD) [0–10] | 3.41 (2.13) | 2.41 (1.91) | 3.34 (2.13) | <0.001 |
Note: ap-value for an independent sample t-test or Chi-square test comparing completers with non-completers.
Most participants were recruited through Facebook (78%) and printed materials (17%), scanning the QR code or typing the shortened links. Most participants chose to complete the survey in English (82%). Respondents were aged 30 ± 11 years, primarily female (60%), Lebanese (84%), unmarried (62%), employed (54%), and with a graduate education level (53%). Most respondents used the Internet for more than 3 h/day (67%). The perceived usefulness and the perceived importance of the internet were high (average four out of five points), and participants reported 3 ± 2 reasons (range 0–10) for using the internet to seek health information.
Chi-square tests, t-tests, and ANOVA tests showed bivariate associations among sociodemographic factors. For instance, respondents recruited through Facebook (n = 2124) were more likely to complete the survey in Arabic (p < 0.001), be males (p = 0.047), Syrian (p < 0.001), married (p < 0.001), and use the internet for more than 5 h/day (p = 0.004). Participants who completed the survey in Arabic (n = 491) were significantly older (p = 0.019) and more likely to be males (p < 0.001), Syrian (p < 0.001), married (p < 0.001), unemployed (p = 0.016), with an undergraduate or high-school level of education (p < 0.001), and perceived the internet as a less important source of health information (p < 0.001) compared to those who completed the survey in English.
Compared to their female counterparts, male respondents were more likely to be Syrian (p < 0.001), unmarried (p = 0.007), have the lowest education level (p < 0.001); they were more likely to use the internet for more than 5 h/day (p = 0.039), finding it less useful (p = 0.016), and less important (p < 0.001), and reporting fewer reasons for seeking health information (p < 0.001).
Syrian respondents, compared to the other nationalities, were more likely to be younger (p = 0.025), married (p = 0.001), unemployed (p < 0.001), and with the lowest levels of education (p < 0.001); they also perceived the internet as less useful (p = 0.011) and important and reported fewer reasons for using it to seek health information (both p < 0.001).
Married individuals, compared to unmarried, were more likely to be employed and have the highest level of education (both p < 0.001); they used the internet fewer hours per day (p < 0.001) and provided fewer reasons to use it for health information (p = 0.008) despite finding it more useful (p < 0.001).
Employed respondents were more likely to be older (p < 0.001), have the highest level of education (p < 0.001), use the internet for fewer hours per day (p < 0.001), but perceive it more useful (p = 0.003) and important (p < 0.001) than unemployed counterparts.
Respondents with the highest level of education (graduate) were significantly older (p < 0.001) and more likely to use the internet for fewer hours per day (p < 0.001), despite finding it more useful (p = 0.011) and an important source of information (p < 0001) and providing a higher number of reasons for seeking health information (p < 0.001) compared to respondents with undergraduate or high-school levels of education.
Respondents who used the internet for more than 5 h/day were significantly younger than the other categories, perceived it more important than those who used it for less time, and reported more reasons for using it (all p < 0.001).
Finally, age was positively related to perceived internet importance (r = 0.08, p < 0.001) and negatively related to the number of reasons (r = −0.04, p = 0.043). Perceived internet usefulness was positively related to importance (r = 0.433, p < 0.001) and to the number of reasons (r = 0.21, p < 0.001). Perceived importance was also positively associated with the number of reasons (r = 0.27, p < 0.001).
Online health information seeking
Table 2 summarizes the reasons for seeking health information and the type of information sought among those who responded to the related questions. The table represents the number of selections as this was a multiple-choice question. Respondents indicated 3 ± 2 reasons for 10 possible options. Most of the sample wanted to gain more knowledge (63%) or were curious (48%) about a health topic, including a disease (78%), a treatment (60%), or a medication (53%).
Table 2.
Reasons for seeking information online and type of information sought (n = 2515).
| n (%)a,b | % of cases (n = 2515) | |
|---|---|---|
| Reasons for seeking health information online | ||
| To gain more knowledge | 1702 (20.3) | 62.6 |
| Out of interest and curiosity | 1289 (15.4) | 47.5 |
| To find more information | 1162 (13.8) | 42.8 |
| To manage my health more effectively | 1012 (12.1) | 37.2 |
| To clarify the information provided by a health professional | 923 (11.0) | 34.0 |
| To look for alternative or additional treatment options | 717 (8.5) | 26.4 |
| To verify the information discussed with a health professional after the visit | 642 (7.7) | 23.6 |
| Insufficient information from a health professional during the consultation | 376 (4.5) | 13.8 |
| Limited time with a health professional during the consultation | 325 (3.9) | 12.0 |
| Disagree with a health professional's advice | 244 (2.9) | 9.0 |
| Types of health-related information sought | ||
| A disease or a health problem | 2109 (25.6) | 77.7 |
| A treatment or a medical procedure | 1641 (20.0) | 60.4 |
| Drugs/medication | 1443 (17.5) | 53.1 |
| Nutrition, diet, or nutritional supplements | 1314 (16.0) | 48.3 |
| Sports, aerobics, and physical exercise | 1008 (12.3) | 37.1 |
| A specific doctor or a hospital | 512 (6.2) | 18.9 |
| Online support groups | 197 (2.4) | 7.3 |
Note: aPercentages are based on the number of answers, not cases, as this was a multiple-choice question.
bp-value for an independent sample t-test or Chi-square test comparing completers with non-completers.
eHealth literacy assessment
Of the 2715 respondents, 2336 (86%) completed all eight items of the eHEALS (further referred to as “eHEALS completers”), 32 respondents answered 7/8 items (1%), 11 answered between six and one items (0.4%), and 366 (12%) did not complete any item (“eHEALS non-completers”). Due to the small proportion of those that provided incomplete eHEALS data, we grouped them under “non-completers.” As Table 1 shows, eHealth completers were significantly older (p < 0.001), more likely to be female (p = 0.008), married (p = 0.003), employed (p < 0.001), and with a graduate education level (p < 0.001) than non-completers. Additionally, completers perceived the internet as more useful and important, reporting more reasons for using it than non-completers (p < 0.001).
Internal consistency
The eHEALS descriptive statistics are presented in Table 3. Cronbach's alpha was 0.892 (95% CI: 0.885–0.899), and the average inter-item correlation was 0.516 (95% CI: 0.496–0.536), suggesting excellent internal consistency.
Table 3.
eHealth literacy scale (eHEALS) – n = 2336.
| eHEALS items | Mean (SD) | Cronbach's alpha if item dropped |
|---|---|---|
| 1. I know what health resources are available on the Internet | 3.43 (0.89) | 0.879 |
| 2. I know where to find helpful health resources on the Internet | 3.56 (0.93) | 0.872 |
| 3. I know how to find helpful health resources on the Internet | 3.69 (0.88) | 0.869 |
| 4. I know how to use the Internet to answer my questions about health | 3.88 (0.80) | 0.878 |
| 5. I know how to use the health information I find on the Internet to help me | 3.82 (0.79) | 0.878 |
| 6. I have the skills I need to evaluate the health resources I find on the Internet | 3.59 (0.97) | 0.880 |
| 7. I can tell high-quality health resources from low-quality health resources on the Internet | 3.67 (0.99) | 0.885 |
| 8. I feel confident in using information from the Internet to make health decisions | 3.16 (1.01) | 0.888 |
| Total score (sum score) | 28.79 (5.51) | |
| Mean score | 3.60 (0.69) |
Exploratory factor analyses
Bartlett's test of sphericity was significant, and the KMO was 0.894, supporting the sampling and data structure adequacy. The fit indices of the tested models are reported in Table 4. A single factor (Model 1) produced factor loadings above 0.4, explaining about 52% of the variance in the data. However, the model did not fit the data well, with TLI and RMSEA suggesting a poor fit. A parallel EFA showed that a three-factor solution (Model 2) fitted the data better and explained 62% of the total variance. Overall, the factor loadings (see Table 5) suggested good correlations between the items and their respective latent factors. The first three items identified a latent factor that could be defined as “Awareness skills” about what, where, and how to find information; items 4 and 5 would indicate “Applied knowledge skills,” which would put the information to use; items 6–8 would mean “Evaluation skills,” needed to appraise the information and make decisions. Notably, item 3 (“I know how to find helpful health resources on the Internet”) displayed a coefficient above 0.43 cross-loading on latent factors 1 and 3. This is plausible in the context of EFA and could be interpreted as a linkage between “Awareness” and “Applied knowledge” skills that pertain to eHealth literacy.
Table 5.
Factor loadings were obtained through EFA and CFA models (n = 2336).
| EFA | CFA | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 5 | |||||||
| eHEALS items | F1 | F1 | F2 | F3 | F1 | F2 | F3 | ||
| 1. I know what health resources are available on the Internet | 0.73 | 0.62 | 0.31 | 0.28 | 0.72 | ||||
| 2. I know where to find helpful health resources on the Internet | 0.83 | 0.87 | 0.27 | 0.25 | 0.79 | ||||
| 3. I know how to find helpful health resources on the Internet | 0.86 | 0.68 | 0.30 | 0.43 a | 0.81 | ||||
| 4. I know how to use the Internet to answer my questions about health | 0.73 | 0.36 | 0.28 | 0.67 | 0.65 | ||||
| 5. I know how to use the health information I find on the Internet to help me | 0.70 | 0.28 | 0.36 | 0.66 | 0.63 | ||||
| 6. I have the skills I need to evaluate the health resources I find on the Internet | 0.65 | 0.23 | 0.74 | 0.31 | 0.71 | ||||
| 7. I can tell high-quality health resources from low-quality health resources on the Internet | 0.63 | 0.33 | 0.58 | 0.23 | 0.65 | ||||
| 8. I feel confident in using information from the Internet to make health decisions | 0.59 | 0.25 | 0.43 | 0.38 | 0.67 | ||||
| Explained variance % (cumulative) | 51.8 | 25.4 | 45.7 | 62.3 | 56.2 | 65.0 | 60.1 | ||
Note: aCross-loading.
Confirmatory factor analyses
Similarly, a single factor CFA model showed a moderate fit (Table 4, Model 3), explaining about 42% of the variance in the data. Inspecting the modification indices showed potential covariances among items 1–3, signifying a possible separate factor. A CFA based on the three factors identified in Model 2 showed an improved fit (Model 4). Nevertheless, modification indices indicated cross-loadings of item 3 on factors 1 and 2 and other intra-item covariances. Since cross-loadings are not permitted in a strict CFA framework, plausible covariances between items explaining the same latent factor were added (items 1–3 and 6–7). The modified Model 5 showed a good fit, with factor loadings above 0.63 and explaining about 60% of the variance in the data. The model had one latent factor with items 1–3, a second factor with items 4 and 5, and a third latent factor comprising items 6–8. An alternative 3-factor model derived from the literature35,45,81 was tested. This model had items 1 and 2 representing “Awareness,” items 3–5 “Applied Knowledge,” and items 6–8 “Evaluation” (Model 6). However, all fit indices indicated that this model fitted the data worse than Model 4, which was based on a well-fitting EFA Model 2, and worse than Model 5 (CFI and TLI were smaller than our model; SRMR, RMSEA, AIC, and BIC were larger than our model).
Factors associated with eHealth literacy
Once the psychometric properties of eHEALS were ascertained, the mean total score across the sample was 28.8 (SD = 5.5), corresponding to a 3.6 (SD = 0.69) on a 5-point scale, suggesting a moderate level of perceived eHealth literacy. Based on the median cut-off point, 1752 participants were classified as having a high level of eHealth literacy (1752/2336, 75%).
Bivariate analyses showed that eHEALS was significantly lower among participants who responded to printed materials compared to Facebook (p = 0.013) and ResearchGate (p < 0.001); respondents recruited through ResearchGate had significantly higher eHEALS than those recruited from Facebook (p = 0.007). eHEALS was higher among those who completed the survey in English (p < 0.001), female, Lebanese, highly educated, employed, who perceived the internet as useful and important, and reported a high number of reasons for seeking information online (all p < 0.001).
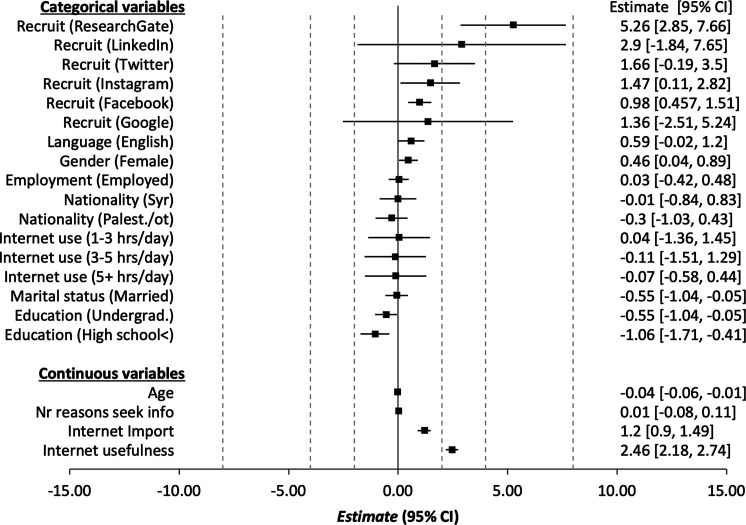
A multivariable generalized linear model predicting eHEALS showed a good fit with the data (−2LL = 52298.57, df = 2277, p < 0.001). The estimated effects on eHEALS are represented in the forest plot in Figure 1. The data showed that eHEALS was higher among participants recruited through Facebook and ResearchGate (p < 0.001), and Instagram (p = 0.034). The eHEALS was higher among young (p = 0.005), females (p = 0.033), with a graduate-level of education, compared to undergraduate level (p = 0.030) or high school or less (p = 0.001); eHEALS was also higher among those who rated the internet as a useful (p < 0.001) and important source of information (p < 0.001). For example, holding constant recruitment channel, age, gender, and education level, a one-unit increase in the perceived internet usefulness or importance scales would translate into an increase of 2.5 points or 1.2 points in eHEALS, respectively. Considering the estimated marginal means (EMM), averaged across nationality, marital status, employment, and internet use, a female respondent with a graduate level of education who was recruited through ResearchGate scored 7.4 points higher on the eHEALS (EMM = 33.5; 95% CI: 31.0–35.9) than a male with a high school level of education, recruited through printed materials, who completed the survey in Arabic (EMM = 27.2; 95% CI: 26.5–27.9).
Figure 1.
Forest plot of the multivariate model investigating the association with eHealth literacy using the homonymous scale (eHEALS) (n = 2299).
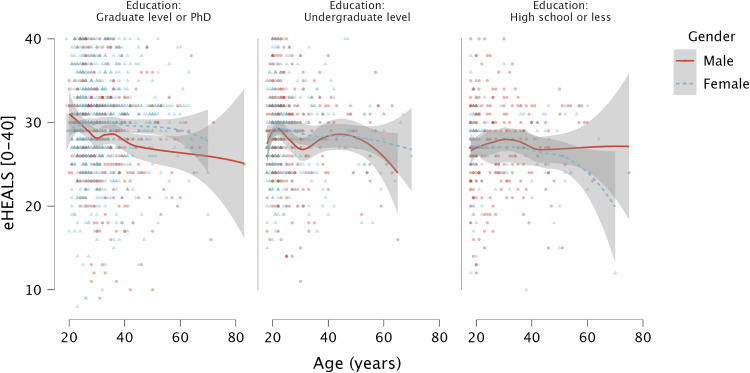
The data portray a complex inter-relationship between eHEALS, sociodemographic variables, perceived internet usefulness, and recruitment channels. Since the last three variables were related to the level of education, we can assume that eHEALS is mainly determined by three sociodemographic factors: age, education, and gender. Figure 2 visually represents the relationship between eHEALS and age by gender and education level. Among respondents with the highest level of education, eHEALS was high among young females and appeared constant over time, while it declined among males. This diverging trend between males and females was more emphasized among those with an undergraduate level of education. Finally, among participants with the lowest level of education, eHEALS remained constant across age but declined more among female individuals.
Figure 2.
Scatterplot of the relationship between eHealth literacy using the homonymous scale (eHEALS) and age by education and gender.
Discussion
Online information seeking
To the best of our knowledge, this is the first cross-sectional study that assessed health information-seeking, eHealth literacy, and its associated factors among a large sample (n = 2715) of internet users in Lebanon. Compared to the estimated population aged 15 and above (4.3 million), 84 the average age of the recruited sample (30.1 years) was slightly lower than the estimated country average of 33.7 years (33.1 for males, 34.4 for females). 84 The male–female ratio in the sample (0.65) was lower than the estimated one for the country (1.00). 84 The sample included a proportion of females (60%) higher than the country's population (50%) 84 and the active internet population (44%). 62 Nevertheless, the proportion of females is comparable to other eHEALS studies conducted among similar populations in the Middle East57,58 and Europe.50,52
Our findings showed that most respondents use the internet to learn more about a disease or a treatment, similar to what was reported in the Kuwaiti study. 57 This evidence reaffirms that the internet is a preferred source of health-related information globally and in the Middle East.11,13–15 Even though the questionnaire did not explicitly ask about what specific disease-related information users sought, the concurrent COVID-19 outbreak in Lebanon might have increased the number of users reporting seeking disease and treatment-related information. Moreover, the multiple reasons for searching online were significantly higher among users who completed the eHEALS, suggesting that eHEALS completers were avid health information seekers. Furthermore, most respondents perceived the Internet as a beneficial and essential source of health information, consistent with the global eHealth literacy literature.26,37 While these results are encouraging, considering the proliferation of COVID-19-related misinformation and disinformation on social media,68,69 future studies should investigate the role of COVID-19 literacy, a context-specific competence, according to the Lily model, 26 whose level and adequacy have been questioned even among experts. 85
eHealth literacy assessment
In our study, the eHEALS demonstrated good psychometric properties showing an excellent internal consistency, in line with the original eHEALS study, 29 the Kuwaiti, 57 the recent Arabic validation study, 54 and other eHEALS translation studies.31–36 These findings support the usefulness of the eHEALS for cross-cultural comparisons. The instrument can be adopted and easily deployed by organizations in the Middle East or other parts of the world to conduct formative or summative research in digital health interventions. The eHEALS is a short instrument providing a quick yet reliable way to assess perceived eHealth literacy. Assessing eHealth literacy should be a prerequisite for developing digital health interventions, whether these are aimed to enhance eHealth literacy or to influence other types of literacies. 22 Future studies could investigate potential differences between countries that share similar cultural traits, but this was beyond the scope of this study.
Even though the eHEALS is a reliable instrument, the validity of the original single-factor solution remains questionable. Our study proved that a three-factor solution fitted the data better than a single-factor one. This is consistent with numerous studies evaluating the eHEALS through CFAs33,35,45–48,57 and EFAs36,4.9,50,52,53 A three-factor solution fitted the data well also in the Kuwaiti study, which recruited a very similar sample of internet users and used CFAs to test the eHEALS but did not report the tested factorial structure configuration. 57 In our study, we identified three latent factors that we called “Awareness,” “Applied knowledge,” and “Evaluation” in agreement with the labels used in similar studies (i.e. “Awareness,” “Skills,” and “Evaluation”).35,45,81 We believe “Applied knowledge” provides a better definition of the latent factor than skills, as the items are supposed to measure the perceived skills needed to seek, understand, and appraise information online, which matches the original definition of eHealth literacy. 26
Similar to Sudbury-Riley et al. 45 and Brørs et al., 35 we found some cross-loadings or correlations between item 3 (“I know how to find helpful health resources on the Internet”), which was loading on “Awareness” and “Skills,” and item 5 (“I know how to use the health information I find on the Internet to help me”), which loaded on both “Skills” and “Evaluation.”35,45 Since cross-loadings are not accepted in a strict CFA framework,77,78 Sudbury-Riley et al., 45 and Brørs et al. 35 provided a model with items 1 and 2 loading on “Awareness,” items 3–5 loading on “Skills,” and items 6–8 loading on “Evaluation.”35,45,81 This same configuration proposed by the literature was tested (see Model 6), but the model did not fit the data well compared to the one emerging from the EFA (Model 2), with items 1–3 loading on “Awareness,” items 4 and 5 loading on “Applied Knowledge,” and items 6–8 loading on “Evaluation.” These nuances may be due to the different sample sizes and characteristics of the populations recruited (i.e. 1695 Norwegian patients with cardiovascular problems, 35 484 Korean registered nurses, 81 and 996 baby boomers 45 ). Future studies should investigate different latent factor configurations among larger samples, perhaps by pooling the data together from multiple studies, as done in other contexts (e.g. psychometric evaluation of the Mobile App Rating Scale 86 ). This would allow generalizing the eHEALS and clarifying whether a multiple-factor solution is appropriate across different countries, cultural contexts, and sociodemographic groups.
The level of perceived eHealth literacy reported in our study was moderate (mean eHEALS = 28.8, SD = 5.5, range: 8–40), but if we consider the median cutoff point in the eHEALS as reported in the literature,57,61,75 three-quarters of our sample demonstrated a high level of perceived eHealth literacy. This figure is similar to those reported in other eHEALS studies, comprising the Kuwaiti study targeting adult internet users (28.9), 57 the Hungarian eHEALS (29.2), 51 involving a majority of educated female users recruited from an online panel, and Jordanian nursing students (28.6).57,61 These findings corroborate the validity of the eHEALS as a tool to compare perceived eHealth literacy across different countries, even outside the Middle East. 29 These results are encouraging as eHealth literacy might reduce the impact of COVID-19-related misinformation on the various social media channels,68–70 which characterizes the ongoing pandemic. However, these results need to be interpreted with caution, as they cannot be generalizable to the entire population living in the country where these surveys were conducted, but only to those with similar characteristics, as discussed in the following paragraph.
Factors associated with eHealth literacy
Despite the small sample size for some recruitment channels, there was an apparent pattern that recruitment channels beyond Facebook had higher levels of eHealth literacy. Participants recruited through ResearchGate had significantly higher eHEALS than those recruited through printed materials and Facebook; this is an expected finding given that ResearchGate is a niche scholarly collaboration platform. 87 A similar trend was observed for other channels (Twitter, Instagram, and LinkedIn). Nonetheless, Facebook was the principal recruitment channel, and the sample distribution across age and gender resembled the distribution of the active user population in Lebanon at the time of the study. Facebook recruited participants were more likely to be male, older, and less educated than their female counterparts. Also, participants recruited from this channel tended to have higher eHEALS than those recruited from printed materials. Similar findings were reported in a recent cross-sectional study assessing cancer prevention practices in Lebanon, recruiting participants through Facebook ads and community outreach through inpatient clinics. 88 The authors reported that knowledge about cancer-preventive behaviors (a proxy of health literacy) was much higher among the internet sample compared to the community one and among young and educated individuals. 88 These findings suggest that recruiting research participants through Facebook may produce large samples due to its broad reach. While these samples may represent the active internet population, some implicit selection bias toward young generations (e.g. 16–24 and 25–34) cannot be excluded. 89 However, health-related research projects seem to attract older women with high socioeconomic status (i.e. higher levels of education in employment). Researchers should oversample younger segments of the active internet population, finding creative strategies or using financial incentives to attract and retain males of lower socioeconomic status.
In this study, younger males, unmarried, unemployed, with a low education level, who perceived the internet as less useful and important, were less likely to complete the eHEALS items (we called them “non-completers”), which means they dropped out of the survey. This is not surprising as females’ participation in web-based surveys is considered a well-established sociological phenomenon.90–92 We cannot know what level of eHEALS the non-completers might have. Still, we can safely assume that it is likely low due to gender, age, and education differences detected in the analyzed sample.
This study showed higher levels of eHEALS among younger females with a high level of education than their male counterparts. Other eHEALS studies reported significant associations between eHealth literacy and age,34,51,59,93 gender,57,94 and education.8,41,59,61 Age, gender, and education are consistently reported as major social determinants of the health and health literacy. 9 Gender was an essential discriminant factor of eHealth literacy in the Kuwaiti study 57 and studies outside the Middle East, such as Serbia, 36 Korea, 95 and Japan. 96 In Figure 2, we attempted to visually represent the complex relationship between eHEALS age, gender, and education; future studies should examine the potential interactions between these factors. Most importantly, longitudinal studies must examine whether perceived eHealth literacy changes over the life course.
In our study, we did not observe a direct relationship between eHEALS and internet use (expressed in terms of hours spent online per week) as reported in some literature. 97 This finding might be explained by the fact that we recruited a relatively homogeneous sample of individuals who used the internet for many hours a day. However, we observed a positive bivariate association between using the internet for more than 5 h/day and the perceived importance of the internet, which was in turn related to its perceived usefulness. Additionally, perceived internet usefulness and importance were both significantly associated with eHEALS. This finding is consistent with those reported in the studies conducted in Kuwait and Jordan,57,61 Australia,27,75 and China, 98 which all identified a positive association between eHEALS and the perceived internet usefulness. Suppose eHEALS is high among those who perceive the internet as a valuable and essential source of information. In that case, one can argue that these users will likely utilize the platform more than others, but perhaps not in terms of hours spent online. It might be because of their elevated information-seeking skills that these users use the internet more efficiently. Future studies should investigate the mediating and moderating role of internet use and perceived usefulness and importance as cognitive predictors of eHEALS.
Strengths and Limitations
This is the first study comprehensively assessing eHealth literacy among internet users in Lebanon. A unique strength of this study is the large sample size obtained through an efficient recruitment strategy, which leveraged Facebook advertising features during the first COVID-19 lockdown in Lebanon. We recruited more than 2700 respondents, which is a much larger sample compared to the other similar regional studies (Jordan: 541 nursing students, recruited through two universities 61 ; Kuwait: 386 adults recruited through web advertisements 57 ; Saudi Arabia: 120 diabetic patients from outpatient clinics of two large hospitals 58 ), and compared to all other eHEALS studies in general. The sample size allowed us to use advanced statistical methods that enhance the value of our findings that can be generalized among internet users who are active on social media in Lebanon.
Despite the large sample size and data quality, we must acknowledge some limitations common to web-based surveys based on convenience sampling. Limitations include self-selection and response biases. While participation was open to any adult living in Lebanon, the sample had most Facebook-recruited, English-speaking, young, female respondents who also had high levels of education. As age, gender, and education were related to the primary study outcome, eHEALS, we could thus expect lower eHealth literacy in a more representative sample and more differences in gender and subgroups with low socioeconomic status and limited Internet resources. Future studies should aim to recruit participants using different strategies to include hard-to-reach population segments.
Another limitation pertains to the eHEALS, which provides a measure of perceived rather than actual eHealth literacy. Future studies should compare the eHEALS to instruments assessing fundamental eHealth literacy skills through observed knowledge or performance tests as proposed by van der Vaart et al. 99 Furthermore, the instrument measures “internet skills” without distinguishing among different sources of information such as blogs, official websites, or social networking sites. This limitation is not new, 37 and several instruments have tried to overcome it; however, their applicability remains limited. 30 Future studies should investigate whether the sources of information might play a moderating role in eHealth literacy.
Conclusions
Higher levels of eHealth literacy were recorded among young, highly educated female Internet users in Lebanon. Organizations responsible for publishing health-related content and undertaking public health campaigns and digital interventions may assume that many individuals reached through social media might understand the scope and find helpful information to prevent or self-manage a disease or a chronic condition. As a moderate to high literacy level can be assumed, most users might not find it difficult to process the information currently available.
However, the observed differences in eHEALS based on recruitment channel, age, gender, education, and perceived internet usefulness and importance suggest that public health campaigns should be designed to segment the population according to these dimensions.
Government and healthcare organizations should develop tailored and targeted health information that accounts for low eHealth literacy. Alternative communication channels should be used concurrently to reach younger males with limited eHealth literacy as they lack confidence on the Internet as a valuable source of information. Campaigns should strive to find different ways to get relevant yet neglected segments of the population that lack internet access through non-digital, community-based outreach activities.
Acknowledgements
We thank all study participants.
Footnotes
Conflicting interests: The authors declare no competing interests.
Contributorship: MB and AK designed and conducted the study. AK performed preliminary analyses and drafted an initial version of the manuscript. MB performed final analyses and drafted the final version of the manuscript. MEB: Provided intellectual input to the study, helped with the analyses of missing data, revised the manuscript, and approved the final version. SA: Provided intellectual input to the design and execution of the study and the manuscript, provided feedback on the final version, and approved the final version. All authors reviewed and edited the manuscript and approved the final version.
Ethical approval: The Institutional Review Board (IRB) of the American University of Beirut (AUB) approved this study (ref. number: SBS-2019-0503; 27/12/2019).
Funding: This study was partially supported by the Master Card Foundation Scholarship program at the American University of Beirut through a scholarship awarded to the second author.
Guarantor: MB
ORCID iD: Marco Bardus https://orcid.org/0000-0002-0707-7196
References
- 1.Johnson J. Global digital population as of January 2021. Statista, https://www.statista.com/statistics/617136/digital-population-worldwide/ (2021, accessed 27 October 2021).
- 2.Kemp S. Digital 2022: April Global Statshot Report. DataReportal – Global Digital Insights, https://datareportal.com/reports/digital-2022-april-global-statshot (2022, accessed 6 June 2022).
- 3.Statista. Global internet penetration rate as of April 2022, by region. Statista, https://www.statista.com/statistics/269329/penetration-rate-of-the-internet-by-region/ (2022, accessed 15 June 2022).
- 4.Statista. Countries with the highest internet penetration rate as of April 2022. Statista, https://www.statista.com/statistics/227082/countries-with-the-highest-internet-penetration-rate/ (2022, accessed 15 June 2022).
- 5.Internet World Stats. Middle East Internet Statistics, Population, Facebook and Telecommunications Reports, https://www.internetworldstats.com/stats5.htm (2022, accessed 7 June 2022).
- 6.Cruz-Jesus F, Oliveira T, Bacao F. The global digital divide: evidence and drivers. J Glob Inf Manag JGIM 2018; 26: 1–26. [Google Scholar]
- 7.Makri A. Bridging the digital divide in health care. Lancet Digit Health 2019; 1: e204–e205. [Google Scholar]
- 8.Neter E, Brainin E. Ehealth literacy: extending the digital divide to the realm of health information. J Med Internet Res 2012; 14: e1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schillinger D. The intersections between social determinants of health, health literacy, and health disparities. Stud Health Technol Inform 2020; 269: 22–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chesser A, Burke A, Reyes J, et al. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care 2016; 41: 1–19. [DOI] [PubMed] [Google Scholar]
- 11.Liu F. How Information-Seeking Behavior Has Changed in 22 Years. Nielsen Norman Group, https://www.nngroup.com/articles/information-seeking-behavior-changes/ (2020, accessed 26 October 2021).
- 12.Jia X, Pang Y, Liu LS. Online health information seeking behavior: a systematic review. Healthcare 2021; 9: 1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aldabbagh D, Alsharif K, Househ MS. Health information in the Arab World. Stud Health Technol Inform 2013; 190: 297–299. [PubMed] [Google Scholar]
- 14.Bahkali S, Almaiman R, El-Awad M, et al. Exploring the impact of information seeking behaviors of online health consumers in the Arab World. Stud Health Technol Inform 2016; 226: 279–282. [PubMed] [Google Scholar]
- 15.Ghweeba M, Lindenmeyer A, Shishi S, et al. What predicts online health information-seeking behavior among Egyptian adults? A cross-sectional study. J Med Internet Res 2017; 19: e6855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nutbeam D, Levin-Zamir D, Rowlands G. Health literacy in context. Int J Environ Res Public Health 2018; 15: 2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nutbeam D. The evolving concept of health literacy. Soc Sci Med 2008; 67: 2072–2078. [DOI] [PubMed] [Google Scholar]
- 18.Fedele DA, Cushing CC, Fritz A, et al. Mobile health interventions for improving health outcomes in youth: a meta-analysis. JAMA Pediatr 2017; 171: 461–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hou S-I, Charlery S-AR, Roberson K. Systematic literature review of internet interventions across health behaviors. Health Psychol Behav Med 2014; 2: 455–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oosterveen E, Tzelepis F, Ashton L, et al. A systematic review of eHealth behavioral interventions targeting smoking, nutrition, alcohol, physical activity and/or obesity for young adults. Prev Med 2017; 99: 197–206. [DOI] [PubMed] [Google Scholar]
- 21.Watkins I, Xie B. Ehealth literacy interventions for older adults: a systematic review of the literature. J Med Internet Res 2014; 16: e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Benny ME, Kabakian-Khasholian T, El-Jardali F, et al. Application of the eHealth literacy model in digital health interventions: scoping review. J Med Internet Res 2021; 23: e23473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han H-R, Hong H, Starbird LE, et al. Ehealth literacy in people living with HIV: systematic review. JMIR Public Health Surveill 2018; 4: e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobs RJ, Lou JQ, Ownby RL, et al. A systematic review of eHealth interventions to improve health literacy. Health Informatics J 2016; 22: 81–98. [DOI] [PubMed] [Google Scholar]
- 25.Ghaddar SF, Valerio MA, Garcia CM, et al. Adolescent health literacy: the importance of credible sources for online health information. J Sch Health 2012; 82: 28–36. [DOI] [PubMed] [Google Scholar]
- 26.Norman CD, Skinner HA. Ehealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006; 8: e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richtering SS, Morris R, Soh S-E, et al. Examination of an eHealth literacy scale and a health literacy scale in a population with moderate to high cardiovascular risk: Rasch analyses. PloS One 2017; 12: e0175372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bo A, Friis K, Osborne RH, et al. National indicators of health literacy: ability to understand health information and to engage actively with healthcare providers – a population-based survey among Danish adults. BMC Public Health 2014; 14: 1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res 2006; 8: e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee J, Lee E-H, Chae D. Ehealth literacy instruments: systematic review of measurement properties. J Med Internet Res 2021; 23: e30644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Neter E, Brainin E, Baron-Epel O. The dimensionality of health literacy and eHealth literacy. Eur Health Psychol 2015; 17: 275–280. [Google Scholar]
- 32.van der Vaart R, van Deursen AJ, Drossaert CH, et al. Does the eHealth literacy scale (eHEALS) measure what it intends to measure? Validation of a Dutch version of the eHEALS in two adult populations. J Med Internet Res 2011; 13: e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Soellner R, Huber S, Reder M. The concept of eHealth literacy and its measurement. J Media Psychol 2014; 26: 29–38. [Google Scholar]
- 34.Diviani N, Dima AL, Schulz PJ. A psychometric analysis of the Italian version of the eHealth literacy scale using item response and classical test theory methods. J Med Internet Res 2017; 19: e114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brørs G, Wentzel-Larsen T, Dalen H, et al. Psychometric properties of the Norwegian version of the electronic health literacy scale (eHEALS) among patients after percutaneous coronary intervention: cross-sectional validation study. J Med Internet Res 2020; 22: e17312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gazibara T, Cakic J, Cakic M, et al. Ehealth and adolescents in Serbia: psychometric properties of eHEALS questionnaire and contributing factors to better online health literacy. Health Promot Int 2019; 34: 770–778. [DOI] [PubMed] [Google Scholar]
- 37.Norman C. Ehealth literacy 2.0: problems and opportunities with an evolving concept. J Med Internet Res 2011; 13: e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karnoe A, Kayser L. How is eHealth literacy measured and what do the measurements tell us? A systematic review. Knowl Manag E-Learn Int J 2015; 7: 576–600. [Google Scholar]
- 39.Petrič G, Atanasova S, Kamin T. Ill literates or illiterates? Investigating the eHealth literacy of users of online health communities. J Med Internet Res 2017; 19: e7372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seçkin G, Yeatts D, Hughes S, et al. Being an informed consumer of health information and assessment of electronic health literacy in a national sample of internet users: validity and reliability of the e-HLS instrument. J Med Internet Res 2016; 18: e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van der Vaart R, Drossaert C. Development of the digital health literacy instrument: measuring a broad spectrum of health 1.0 and health 2.0 skills. J Med Internet Res 2017; 19: e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Karnoe A, Furstrand D, Christensen KB, et al. Assessing competencies needed to engage with digital health services: development of the eHealth literacy assessment toolkit. J Med Internet Res 2018; 20: e8347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kayser L, Karnoe A, Furstrand D, et al. A multidimensional tool based on the eHealth literacy framework: development and initial validity testing of the eHealth literacy questionnaire (eHLQ). J Med Internet Res 2018; 20: e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paige SR, Stellefson M, Krieger JL, et al. Transactional eHealth literacy: developing and testing a multi-dimensional instrument. J Health Commun 2019; 24: 737–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sudbury-Riley L, FitzPatrick M, Schulz PJ. Exploring the measurement properties of the eHealth literacy scale (eHEALS) among baby boomers: a multinational test of measurement invariance. J Med Internet Res 2017; 19: e5998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paige SR, Miller MD, Krieger JL, et al. Electronic health literacy across the lifespan: measurement invariance study. J Med Internet Res 2018; 20: e10434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hyde LL, Boyes AW, Evans T-J, et al. Three-Factor structure of the eHealth literacy scale among magnetic resonance imaging and computed tomography outpatients: a confirmatory factor analysis. JMIR Hum Factors 2018; 5: e9039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stellefson M, Paige SR, Tennant B, et al. Reliability and validity of the telephone-based eHealth literacy scale among older adults: cross-sectional survey. J Med Internet Res 2017; 19: e8481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ma Z, Wu M. The psychometric properties of the Chinese eHealth literacy scale (C-eHEALS) in a Chinese rural population: cross-sectional validation study. J Med Internet Res 2019; 21: e15720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pérez G P, Almagro BJ, Hernando Gómez Á, et al. Validación de la escala eHealth Literacy (eHEALS) en población universitaria española. Rev Esp Salud Pública 2015; 89: 329–338. [DOI] [PubMed] [Google Scholar]
- 51.Zrubka Z, Hajdu O, Rencz F, et al. Psychometric properties of the Hungarian version of the eHealth literacy scale. Eur J Health Econ 2019; 20: 57–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Burzyńska J, Rękas M, Januszewicz P. Evaluating the psychometric properties of the eHealth literacy scale (eHEALS) among polish social Media users. Int J Environ Res Public Health 2022; 19: 4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chung S, Park BK, Nahm E-S. The Korean eHealth literacy scale (K-eHEALS): reliability and validity testing in younger adults recruited online. J Med Internet Res 2018; 20: e138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wångdahl J, Dahlberg K, Jaensson M, et al. Arabic version of the electronic health literacy scale in Arabic-speaking individuals in Sweden: prospective psychometric evaluation study. J Med Internet Res 2021; 23: e24466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oh SS, Kim K-A, Kim M, et al. Measurement of digital literacy among older adults: systematic review. J Med Internet Res 2021; 23: e26145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weber AS, Turjoman R, Shaheen Y, et al. Systematic thematic review of e-health research in the Gulf Cooperation Council (Arabian Gulf): Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and the United Arab Emirates. J Telemed Telecare 2017; 23: 452–459. [DOI] [PubMed] [Google Scholar]
- 57.Alhuwail D, Abdulsalam Y. Assessing electronic health literacy in the state of Kuwait: survey of internet users from an Arab state. J Med Internet Res 2019; 21: e11174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.AlOthman R, Zakaria N, AlBarrak A. Saudi diabetic patients’ attitudes towards patient portal use and their perceived E-health literacy. Stud Health Technol Inform 2017; 245: 1211. [PubMed] [Google Scholar]
- 59.Almoajel A, Alshamrani S, Alyabsi M. The relationship between e-health literacy and breast cancer literacy among Saudi women. Front Public Health 2022; 10: 841102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Balay-odao EM, Alquwez N, Alsolami F, et al. COVID-19 crisis: influence of eHealth literacy on mental health promotion among Saudi nursing students. J Taibah Univ Med Sci 2021; 16: 906–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tubaishat A, Habiballah L. Ehealth literacy among undergraduate nursing students. Nurse Educ Today 2016; 42: 47–52. [DOI] [PubMed] [Google Scholar]
- 62.Kemp S. Digital 2022: Lebanon. DataReportal – Global Digital Insights, https://datareportal.com/reports/digital-2022-lebanon (2022, accessed 27 October 2021).
- 63.Saleh S, Khodor R, Alameddine M, et al. Readiness of healthcare providers for eHealth: the case from primary healthcare centers in Lebanon. BMC Health Serv Res 2016; 16: 644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saleh S, Alameddine M, Farah A, et al. Ehealth as a facilitator of equitable access to primary healthcare: the case of caring for non-communicable diseases in rural and refugee settings in Lebanon. Int J Public Health 2018; 63: 577–588. [DOI] [PubMed] [Google Scholar]
- 65.Saleh S, Farah A, Dimassi H, et al. Using mobile health to enhance outcomes of noncommunicable diseases care in rural settings and refugee camps: randomized controlled trial. JMIR MHealth UHealth 2018; 6: e137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Badr N, Chami E, Asmar M. e-Health implementation in Lebanese teaching hospitals: what can we learn from their successes and imminent challenges: In: Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies. Online Streaming, – Select a Country –: SCITEPRESS – Science and Technology Publications, pp. 304–311.
- 67.Koweyes J, Salloum T, Haidar S, et al. COVID-19 Pandemic in Lebanon: one year later, what have we learnt? mSystems 2021; 6: e00351–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Siddiqui MYA, Mushtaq K, Mohamed MFH, et al. “Social media Misinformation”—an epidemic within the COVID-19 pandemic. Am J Trop Med Hyg 2020; 103: 920–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kouzy R, Abi Jaoude J, Kraitem A, et al. Coronavirus goes viral: quantifying the COVID-19 misinformation epidemic on Twitter. Cureus 2020; 12: e7255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Makhoul J, Kabakian-Khasholian T, Chaiban L. Analyzing the social context of health information and misinformation during the COVID-19 pandemic: a case of emerging inequities in Lebanon. Glob Health Promot 2021; 28: 1757975920984178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kabakian-Khasholian T, Makhoul J, Bardus M. To wear or not to wear a mask in the COVID-19 era? The broken bridge between recommendations and implementation in Lebanon. J Glob Health 2020; 10: 020322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kemp S. Digital in Lebanon: All the Statistics You Need in 2021. DataReportal – Global Digital Insights, https://datareportal.com/reports/digital-2022-lebanon (2021, accessed 27 October 2021).
- 73.LimeSurvey. Home page – LimeSurvey – Easy online survey tool, https://limesurvey.org/ (accessed 20 March 2021).
- 74.JASP Team. JASP (Version 0.10.0)[Computer software], https://jasp-stats.org/ (2018).
- 75.Richtering SS, Hyun K, Neubeck L, et al. Ehealth literacy: predictors in a population with moderate-to-high cardiovascular risk. JMIR Hum Factors 2017; 4: e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.DeVellis RF. Scale development: theory and applications. 4 edition. Los Angeles: Sage Publications, Inc, 2016. [Google Scholar]
- 77.Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval 2005; 10: 131–146. [Google Scholar]
- 78.Brown TA. Confirmatory factor analysis for applied research. 1st ed. New York, London: The Guilford Press, 2006. [Google Scholar]
- 79.Tabachnick BG, Fidell LS. Using multivariate statistics. 5th revised International ed. Upper Saddle River, NJ: Pearson Education, 2007. [Google Scholar]
- 80.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J 1999; 6: 1–55. [Google Scholar]
- 81.Gartrell K, Han K, Trinkoff A, et al. Three-factor structure of the eHealth Literacy Scale and its relationship with nurses’ health-promoting behaviours and performance quality. J Adv Nurs 2020; 76: 2522–2530. [DOI] [PubMed] [Google Scholar]
- 82.Garson GD. Generalized linear models & generalized estimating equations. Asheboro, NC: Statistical Associates Publishing, 2012. [Google Scholar]
- 83.Rasch D, Verdooren R, Pilz J. Generalised linear models. In: Applied statistics. Oxford: John Wiley & Sons, Ltd, pp. 393–428. [Google Scholar]
- 84.CIA, Central Intelligence Agency. Lebanon. The World Factbook, https://www.cia.gov/the-world-factbook/countries/lebanon/#people-and-society (2022, accessed 2 July 2022).
- 85.Paakkari L, Okan O. COVID-19: health literacy is an underestimated problem. Lancet Public Health 2020; 5: e249–e250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Terhorst Y, Philippi P, Sander LB, et al. Validation of the mobile application rating scale (MARS). PLOS ONE 2020; 15: e0241480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.O’Brien K. Researchgate. J Med Libr Assoc JMLA 2019; 107: 284–285. [Google Scholar]
- 88.Telvizian T, Al Ghadban Y, Alawa J, et al. Knowledge, beliefs, and practices related to cancer screening and prevention in Lebanon: community and social media users’ perspectives. Eur J Cancer Prev 2021; 30: 341–349. [DOI] [PubMed] [Google Scholar]
- 89.Whitaker C, Stevelink S, Fear N. The use of Facebook in recruiting participants for health research purposes: a systematic review. J Med Internet Res 2017; 19: e7071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Smith G. Does gender influence online survey participation?: A record-linkage analysis of university faculty online survey response behavior. ERIC Doc Reprod Serv 2008; 22. [Google Scholar]
- 91.Slauson-Blevins K, Johnson KM. Doing gender, doing surveys? Women’s gatekeeping and men’s non-participation in multi-actor reproductive surveys. Sociol Inq 2016; 86: 427–449. [Google Scholar]
- 92.Becker R. Gender and survey participation: an event history analysis of the gender effects of survey participation in a probability-based multi-wave panel study with a sequential mixed-mode design. Methods Data Anal 2022; 16: 30. [Google Scholar]
- 93.Chang A, Schulz PJ. The measurements and an elaborated understanding of Chinese eHealth literacy (C-eHEALS) in chronic patients in China. Int J Environ Res Public Health 2018; 15: 1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mitsutake S, Shibata A, Ishii K, et al. [Developing Japanese version of the eHealth literacy scale (eHEALS)]. Nihon Koshu Eisei Zasshi Jpn J Public Health 2011; 58: 361–371. [PubMed] [Google Scholar]
- 95.Kim S-H, Son Y-J. Relationships between eHealth literacy and health behaviors in Korean adults. Comput Inform Nurs CIN 2017; 35: 84–90. [DOI] [PubMed] [Google Scholar]
- 96.Mitsutake S, Shibata A, Ishii K, et al. Association of eHealth literacy with colorectal cancer knowledge and screening practice among internet users in Japan. J Med Internet Res 2012; 14: e153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mitsutake S, Shibata A, Ishii K, et al. Associations of eHealth literacy with health behavior among adult internet users. J Med Internet Res 2016; 18: e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lwin MO, Panchapakesan C, Sheldenkar A, et al. Determinants of eHealth literacy among adults in China. J Health Commun 2020; 25: 385–393. [DOI] [PubMed] [Google Scholar]
- 99.van der Vaart R, Drossaert CH, Heus Md, et al. Measuring actual eHealth literacy among patients with rheumatic diseases: a qualitative analysis of problems encountered using health 1.0 and health 2.0 applications. J Med Internet Res 2013; 15: e2428. [DOI] [PMC free article] [PubMed] [Google Scholar]