Abstract
Background
The analysis of acute malnutrition in 2018 for the Integrated Phase Classification of Food Security in Yemen shows that high malnutrition rates are present in Abyan governorate (23%) and Lahj governorate (21%). This analysis was community based addressed all children and mostly due to problems related to food intake. The role of diseases was not yet addressed in Yemen. The aim of this study is to assess acute and chronic malnutrition among hospitalized children at 12–59 months of age in Lahj and Abyan governorates in Yemen.
Methodology
A cross-sectional, multi-center study is designed. The assessment of the nutritional status was measured by standardized anthropometry of 951 sick children at 12–59 months of age.
Results
The prevalence of Global acute malnutrition (GAM) among the sick children seeking care in health facilities in Lahj and Abyan is 21%. More specifically; the prevalence of moderate acute malnutrition (MAM) is 15.1% while the prevalence of severe acute malnutrition (SAM) is 6.2%. The prevalence of acute malnutrition (wasting) among the studied sick children in lahj is 23.4% while in Abyan is 19.3%. The prevalence of MAM in Lahj is 17.7% and the prevalence of SAM is 5.7%. The prevalence of acute malnutrition (wasting) in Abyan is 12.6% while the prevalence of SAM in Abyan is 6.7%. The prevalence of acute malnutrition among male children (25.2%) is significantly higher than among female children (17.5%). The prevalence of the chronic malnutrition (Stunting) in the studied sick children is 41.3%; the prevalence of stunting in Lahj is 41% while in Abyan is 41.7%.
Conclusions
High acute and chronic malnutrition rates were identified among sick children seeking care in health facilities in lahj and Abyan, and higher than the SPHERE indicators of malnutrition. Boys are more exposed than girls to acute and chronic malnutrition.
Keywords: Malnutrition, Sick children, Stunting, Wasting
Introduction
Malnutrition in children is of high concern in developing countries like Yemen. However, malnutrition is multifactorial. Malnutrition in low-income countries is often, but not solely, be attributable to limited access to food and/or medical care, it is often triggered by disease [1]. In one study among 3101 hospitalized children in nine countries in sub-Saharan Africa in 2019; it was found that 24.6% of the hospitalized children had moderate wasting, and 39·3% had severe wasting with death rate of 11·3% [2].
Most of the local and international reports described the situation in Yemen is the worst humanitarian crises in the world. Malnutrition among Yemeni children is one of the painful crises. In 2015, UNICEF's report concludes that a striking ten of Yemen's 22 governorates are on the edge of famine, as defined by the five-point Integrated Food Security Phase Classification (IPC) scale [3]. In 2017; a study published in the lancet indicated that according to organizations working to end hunger, about 370 000 of Yemen's children are suffering from severe malnutrition. Additionally, one million children younger than five years old are at risk of acute malnutrition [4].
The rate of child malnutrition in Yemen is one of the highest in the world and the nutrition situation continues to deteriorate. World food program (WFP) reported that about one third of families have gaps in their diets, and hardly ever consume foods like pulses, vegetables, fruit, dairy products or meat. Malnutrition rates among children in Yemen remain among the highest in the world, with 2.3 million children under five years requiring treatment for acute malnutrition [5].
Another study among children under five years of age identified that the high malnutrition level (the prevalence of stunting was 47%, wasting was 16%, and underweight was 39%) [6].
Recent study in 2022 reported that more than 2.3 million children under the age of five in Yemen suffer from acute malnutrition. Approximately 450,000 are expected to suffer from severe acute malnutrition and may die if they do not receive urgent treatment [7].
Cases of acute malnutrition among children under five have risen to the highest levels recorded in parts of Yemen. More than half a million cases recorded in the southern districts. Analysis of acute malnutrition in 2018 in Yemen for the Integrated Phase Classification of Food Security issued by the Organization Food and Agriculture of the United Nations (FAO), the United Nations Children's Fund (UNICEF), the World Food Program and their partner identified high rate of malnutrition. The most affected areas included in this analysis are Abyan governorate (23%), Lahj governorate (21%) [8], in another two studies the global acute malnutrition in Abyan was 10% [9]. And in lahj was 27.3% [10].
Malnourished children are more vulnerable to illnesses, including diarrhea, respiratory infections, and malaria, which are a major concern in Yemen [11] Disease-related malnutrition in children is the consequence of different factors. For example, food intake due to anorexia, feeding difficulties or the effects of medications or due to the hyper metabolic state caused by the underlying disease [12–14].
Identification of malnutrition among hospitalized children is important because most pediatricians have no concern on the impact of malnutrition on the clinical outcome of the sick child. Mostly, they neglect the malnutrition as a determinant of the disease prognosis. This study aimed is to assess the malnutrition among sick children in two governorates in the southern Yemen of high malnutrition prevalence. The specific objective is to assess the prevalence of acute and chronic malnutrition among children aged 12 to 59 months seeking outpatient care and their association with governorate, health facility, gender, residency, family income, availability to drinking water.
Methodology
A cross-sectional, multi-center study was designed in to determine the prevalence of malnutrition and related morbidity among hospitalized children 12–59 months of age in Abyan and Lahj governorates.
In Yemen, there are 22 governorates; since The Civil War in 2015; twelve governorates in the south are under the control of International recognized government (IRG) including lahj and Abyan governorates. The total population of Yemen in 2021 is 31,153,000 people. The total population of Lahj in 2021 is 1,070,000 people including 115,685 children at 12–59 months while population of Abyan is 609,000 people including 55,547 children at age of 12–59 months [15]. In each governorate there is one government hospital and, in each district, there is one district hospitals. In each district there is a main city and a group of villages, in a big village there is one primary health care (PHC) center. Figure 1
Fig. 1.
Map of Yemen the coloured areas are Lahj (left) and Abyan (Right) governorates. Source: https://en.wikipedia.org/wiki/Lahij_Governorate & https://en.wikipedia.org/wiki/Abyan_Governorate
The assessment of the nutritional status was measured by standardized anthropometry at attendance in outpatient clinic. Wasting measured by Weight for height/length or MUAC and stunting measured by Hight/length for age (SDS, WHO reference) are the primary outcome variables. Gender, Family residency, family income, availability of drinking water in the house are the independent variables.
The study population are children at 12–59 months of age who attend the health facility to seek care for certain health problem. Mothers were interviewed while a trained nurse measured the weight and height and mid upper arm circumference (MUAC) of the sick child.
From each governorate; five health facilities were selected. These facilities were: the main governorate hospital, two district hospitals and two health centers from two different villages in two different districts. There is only one governorate hospital in every governorate. The other four health facilities were selected based on the selection of the districts. From every governorate; two districts were selected by simple random sampling out of 12 districts in every governorate. From each district we select the district hospital (it is only one district hospital in each district) and two villages out of 8–12 villages in each district. From each village we select the village PHC center (it is one center in every village).
Data was collected through a group of enumerators and two field supervisors. Training of two days were conducted in Lahj (Al-Hottah city) in 28th of February, 2022 and in Abyan (Zunjibar city) in 3rd of March, 2022 where enumerators were trained about the questionnaire and the selection of the targeted children (sick children seeking care in the selected health facility within 12–59 months of age). IT personal trained the enumerators about applying the KOBO toolbox and upload the digital questionnaire to their mobiles. This method is most effective method to make the research team monitors in daily basis the process of data collection.
Sample size calculation
The formula that is used to calculate the sample size is Danieal formula of cross-sectional study in infinite population [16].
The following simple formula (Daniel, 1999) can be used:
where = sample size, = z statistic for a level of confidence (1.96), = expected prevalence or proportion, here is 10% based on the prevalence of malnutrition in Abyan[9], and = precision ( = 2). Accordingly; the sample size will be:
We add 10% to avoid non response, so the final sample size was 864 + 86 = 950.
The samples size was distributed equally for Lahj and Abyan (475 from each) then was distributed proportional to health facility category and based on the follow of the sick children to health facilities (37% in hospitals, 21% in district hospitals and 42% in health centers). So; the sample was distributed as 175 children from each governorate hospital, 100 children from each district hospital and 50 children from each health center.)
Anthropometric measurements [17]
Weight: Children were weighed standing on the weight scale to the nearest 0.1 kg. For the children who could not stand, weight was measured in infant weight scale.
Height/Length: Height and length of children were measured using height scale and recorded to the nearest 0.1 cm. Children equal or less than 87.0 cm were measured lying down, and children greater than or equal to 87.0 cm were measured in standing position.
MUAC: Mid-upper arm circumference measurements were made using a flexible and non-stretch tape. MUAC measurements was taken on the mid-point of the left upper arm. All the selected sick children in the aged 12–59 months were measured to the nearest 0.1 cm. The MUAC is interpreted as both for graduated and color labeled. Red color [MUAC > 115 mm], and < 125 mm] were considered a moderately malnourished. While the green color [MUAC ≥ 125 mm] were categorized as normal according to WHO classification.
Operational definition of the Outcome indicators [18]
Wasting: Weight‐for‐height (wasting) provides the clearest picture of acute malnutrition.
Moderate Acute Malnutrition (MAM) is identified by moderate wasting WFH ≤ -2 z score and ≥ -3 z‐score for children 0‐59 months (or for children 6‐59 months, MUAC < 115 mm and ≥ 125 mm). Table 1.
Table 1.
Anthropometric measurements and indicators
| Measurement | Indicator | Nutritional status |
|---|---|---|
| Weight-for-height index (W/H) | ≥ -2 z-score | Normal nutrition status |
| (< -3 z-score and/or oedema and/or < 115 mm (MUAC) | Acute severe malnutrition (SAM) | |
| WHZ ≥ -3 and < -2 | Acute moderate malnutrition (MAM) | |
| MUAC | > or = 125 | Normal nutrition status |
| < 125 and > or = 115 | Acute moderate malnutrition (MAM) | |
| < 115 | Acute severe malnutrition (SAM) | |
| Stunting (Height for Age -HAZ) | ≥ -2 z-score | Normal nutrition status |
| 3 z-score ≤ H/A < -2 z-score | Stunting (moderate) | |
| < -3 z-score | Stunting (Severe) |
Severe Acute Malnutrition (SAM) is identified by severe wasting < -3 z‐score for children 12‐59 months (or for children 12‐59 months, MUAC < 115 mm) or the presence of bilateral pitting edema.
Global Acute Malnutrition (GAM) is the presence of both MAM and SAM in a population. A GAM value of more than 10 percent indicates an emergency. If GAM is exceeding 15% it is considered critical while at 11–14% is severe GAM and if GAM at level of > 5% and less than 10% is considered poor indicator.
Chronic malnutrition (Stunting) (Height-for-age Z score (HAZ)) The HAZ measure indicates if a child of a given age is chronically malnourished (stunted). The height-for-age index of a child from the studied population is expressed in Z-score (HAZ).
The indicators
-
proportion of wasting (MAM, SAM and GAM) among the hospitalized children in Lahj and Abyan
= Number of hospitalized children have MAM/ all hospitalized children under study.
= Number of hospitalized children have SAM/ all hospitalized children under study.
Proportion of stunting (Chronic malnutrition) among the hospitalized children in Lahj and Abyan
= Number of hospitalized children have stunting/ all hospitalized children under study.
Statistical analysis
Data were transforming from the KOBO application data set to excel file, then to the statistical package for social sciences (SPSS) version 24. Descriptive statistics uses are mean, standard deviations, to describe the quantitative variables while frequency and percentages to describe the qualitative variables. Chi square test is used as a tool of inferential statistics to assess the significance of association between malnutrition and the independent variables of gender, residency, family income, availability of drinking water in the house. A cut of point of 0.05 was used for significant level. Fischer exact test is used alternatively to chi square test if the expected dells are less than 5.
For purpose of bivariate and logistic regression; the dependent variables were ree-classified into two categories: the acute malnutrition is reclassified into acute malnutrition and normal, where acute malnutrition included MAM and SAM children. The chronic malnutrition (Stunting) variable is a dependent variable is re-classified int o two categories: Chronic malnutrition (Stunting) and normal, where chronic malnutrition included moderate stunting and sever stunting. the socioeconomic variables of more than two categories are reclassified. The independent variables are re-classified in to two categories: For example, residency is re-classified to be (Resident and non-resident. The non-resident group includes IDPs, refugees and marginalized people. The availability of water of in the house is re-classified to available or not available. The availability of water includes the available and regular supply and availability with irregular supply. The outcome variables; acute and chronic malnutrition, each variable is classified into two categories. In all bivariate and logistic regression, the significant level is 0.05, Odds Ratio (OR) and 95% confidence interval (95%CI) are used to assess the strength of the association.
Results
Socio-demographic characteristics of the studied children
The total number of sick children seeking care in the selected 10 health facilities in Lahj and Abyan during the study period (1–13, March 2022) are 951 children at the age of 12–59 months. The mean age is 29.5 years old (± 14 years). The range from 12 to 59 months. A total of 491 female children (51.6%) while male children are 460 children (48.4%). There are 474 children form Lahj governorate (49.8%) and 477 children from Abyan governorate (50.2%). Most of the children's mothers are either illiterate (37.4%) or has primary /essential education (36/1%) while most of the fathers had primary or essential education (39.2%). About 64% of children's fathers are employed, but about 35% is unemployed; most of the mothers reported that their family monthly income is not enough (88.1%). About 75% of the children are of resident families and 23.7% of internal displaced people (IDPs). Most of the households of the children (62%) has irregular drinking water supply Table 2.
Table 2.
Socio-demographic characteristics of the sick children involved in the study (N = 951)
| Socio-demographic characteristics | Number of the studied sick children (N = 951) | % | |
|---|---|---|---|
| Sex | Male | 460 | 48.4% |
| Female | 491 | 51.6% | |
| Governorate | Lahj | 474 | 49.8% |
| Abyan | 477 | 50.2% | |
| Mother educational level | Illiterate | 356 | 37.4% |
| Primary/elementary/preparatory | 343 | 36.1% | |
| Secondary/diploma | 186 | 19.6% | |
| University + | 66 | 6.9% | |
| Father educational level | Illiterate | 161 | 16.9% |
| Primary/elementary/preparatory | 373 | 39.2% | |
| Secondary/diploma | 283 | 29.8% | |
| University + | 134 | 14.1% | |
| Father job | Unemployed | 332 | 34.9% |
| Employed | 617 | 64.9% | |
| Student | 2 | 0.2% | |
| Family monthly income | Enough | 112 | 11.9% |
| Not enough | 838 | 88.1% | |
| Residency | resident | 713 | 75% |
| IDPs | 225 | 23.7% | |
| Refugees | 8 | 0.8% | |
| Muhamsheen | 5 | 0.5% | |
| Drinking water supply in the house | Available and Regular | 262 | 27.5% |
| Available but not regular | 647 | 68% | |
| Not available | 42 | 4.5% | |
Prevalence of acute malnutrition among sick children
The prevalence of Global acute malnutrition (GAM) among the sick children seeking care in health facilities in Lahj and Abyan is 21% (203/951) Fig. 2. More specifically; the prevalence of moderate acute malnutrition (MAM is 15.1% (144/951) while the prevalence of severe acute malnutrition (SAM) is 6.2%. (59/951) Fig. 3
Fig. 2.
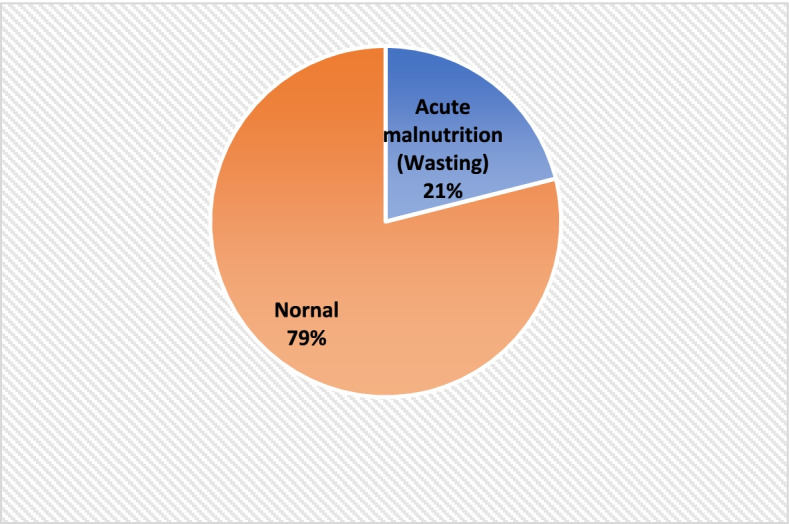
Prevalence of acute malnutrion (Wasting) among 951 sick children seeking care in health facilities in Lahj and Abyan, March 2022
Fig. 3.
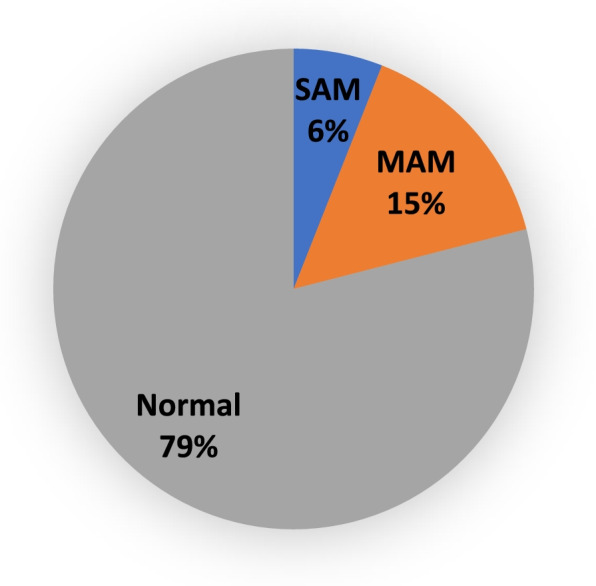
Prevalence of MAM and SAM among sick children seeking care in health facilities in Lahj and Abyan, March 2022
The prevalence of global acute malnutrition (wasting) among the studied sick children in lahj is 23.4% while in Abyan is 19.3%. The prevalence of MAM in Lahj is 17.7% and the prevalence of SAM is 5.7%. The prevalence of MAM among the studied sick children in Abyan is 12.6% while the prevalence of SAM in Abyan is 6.7% but these differences are not significant (P-value 0.113).
The prevalence of the chronic malnutrition (Stunting)
The prevalence of the chronic malnutrition (Stunting) in the studied sick children is 41.3%; the prevalence of stunting in Lahj is 41% while in Abyan is 41.7%. The prevalence of moderate stunting in all the studied sick children is 24.3% and the prevalence of severe stunting is 17.2%. Prevalence of moderate stunting is higher in Abyan 26.4% while the prevalence of severe stunting is higher in Lahj (19.2%) but these differences are not significant (P-vale 0.117). Table 3. A 65 out of 951 children was found have concurrent form of malnutrition (wasting and stunting), giving the prevalence of concurrent forms of malnutrition to 6.8%
Table 3.
Prevalence of acute malnutrition among the sick children seeking care in health facilities by governorate, March 2022
| Governorate | Category of Acute malnutrition | χ2 | P-value | |||||
|---|---|---|---|---|---|---|---|---|
| MAM | % | SAM | % | GAM | % | |||
| Lahj (n = 474) | 84 | 17.7% | 27 | 5.7% | 111 | 23.4% | 0.24 | 0.113 |
| Abyan (n = 477) | 60 | 12.6% | 32 | 6.7% | 92 | 19.3% | ||
| Category of chronic malnutrition (stunting) | χ2 | P-value | ||||||
| Governorate | Moderate stunting | % | Severe stunting | % | Overall stunting | % | ||
| Lahj (n = 474) | 103 | 21.7% | 91 | 19.2% | 194 | 41% | 0.42 | 0.117 |
| Abyan (n = 477) | 126 | 26.4% | 73 | 15.3% | 199 | 41.7% | ||
Variations in prevalence of malnutrition by gender
The prevalence of acute malnutrition among male children (25.2%) is significantly higher than prevalence of acute malnutrition among female children (17.5%). Moreover, Prevalence of MAM and SAM among males (17.6% & 7.6% respectively) are significantly higher than females (12.8% & 4.9% respectively) (P-value 0.004). The prevalence of stunting in males (45.3%) is significantly higher than females (37.7%). Moreover, Prevalence of moderate stunting and severe stunting among males (25.5% & 19.8% respectively) are significantly higher than females (22.6% & 15.1% respectively) (P-value 0.05). Table 4.
Table 4.
Gender and malnutrition
| Sex | Category of Acute malnutrition | χ2 | P-value | |||||
|---|---|---|---|---|---|---|---|---|
| MAM | % | SAM | % | GAM | % | |||
| Male (n = 460) | 81 | 17.6% | 35 | 7.6% | 116 | 25.2% | 8.42 | 0.004* |
| Female (n = 491) | 63 | 12.8% | 24 | 4.9% | 86 | 17.5% | ||
| Category of chronic malnutrition (stunting) | χ2 | P-value | ||||||
| Sex | Moderate stunting | % | Severe stunting | % | Overall stunting | % | ||
| Male (n = 460) | 118 | 25.5% | 90 | 19.8% | 208 | 45.3% | 5.99 | 0.005* |
| Female (n = 491) | 111 | 22.6% | 74 | 15.1% | 185 | 37.7% | ||
*Statistically significant at 0.05 significant level
The socio-economic characteristics and malnutrition
For purpose of bivariate analysis; the socioeconomic variables are re-classified to be dichotomous variables for example; Residency and availability of water (see the statistical analysis section). In Table 5, the bivariate analysis is presented between the socio-economic factors (independent variables) and acute malnutrition (dependent variable). In bivariate analysis; only sex and type of health facility have significant association with acute malnutrition. Table 5 shows that high prevalence of acute malnutrition among the males (25.2%) is significantly higher than females (17.5%) (P-value 0.004). The prevalence of acute malnutrition in sick children seeking care in hospital clinics (24.8%) is significantly higher than prevalence of acute malnutrition in sick children seeking care in PHC centers (16.3%) (p-value 0.002). In Table 6, the bivariate analysis is presented between the socio-economic factors (independent variables) and chronic malnutrition (dependent variable). In bivariate analysis, sex, type of health facility and residency are significantly associated with chronic malnutrition (Stunting). Table 6 shows that the prevalence of stunting is higher in males (45.2%) than females (37.7%) (p-value 0.021). The prevalence of stunting in sick children seeking care in hospital clinics (47.8%) is significantly higher than prevalence of stunting in sick children seeking care in PHC centers (32.3%) (p-value 0.000). The prevalence of stunting in non-residents (IDPS, Refuges and marginalized groups) is significant higher (51.7%) than the prevalence of stunting in residents (37.9%) (P-value 0.000). Table 6.
Table 5.
Bivariate analysis of association of acute malnutrition and socio-economic characteristics
| Item | Acute malnutrition | Well nourished | Total | Prevalence of acute malnutrition | X2 | P-value | |
|---|---|---|---|---|---|---|---|
| Governorate |
Lahj Abyan |
111 91 |
363 386 |
474 477 |
23.4% 19.1% |
0.27 | 0.113† |
| Sex |
Male Female |
116 86 |
344 405 |
460 491 |
25.2% 17.5% |
8.42 | 0.004†* |
| Type of the Health facility |
Hospital PHC centers |
137 65 |
415 334 |
552 399 |
24.8% 16.3% |
10 | 0.002†* |
| Residency | Resident | 150 | 563 | 713 | 21% | 0.07* | 0.784 |
| Non-resident | 52 | 186 | 238 | 21.8% | |||
| Monthly family income | Enough | 26 | 87 | 113 | 23% | 0.24 | 0.625 |
| Not enough | 176 | 662 | 838 | 21% | |||
| Availability of drinking water in the house | available | 193 | 716 | 909 | 21.2% | 1* | 0.551 |
| Not available | 9 | 33 | 42 | 21.4% | |||
†Fischer exact test
*Significant, P-value < 0.05
Table 6.
Bivariate analysis of association of Chronic malnutrition and socio-economic characteristics
| Item | Stunting | Normal | Total | Prevalence of Stunting | X2 | P-value | |
|---|---|---|---|---|---|---|---|
| Governorate |
Lahj Abyan |
194 199 |
280 278 |
474 477 |
40.9% 41.7% |
0.06 | 0.834 |
| Sex |
Male Female |
208 185 |
252 306 |
460 491 |
45.2% 37.7% |
5.56 | 0.021†* |
| Type of the Health facility |
Hospital PHC centers |
264 129 |
288 270 |
552 399 |
47.8% 32.3% |
22.3 | 0.000* |
| Residency | Resident | 270 | 443 | 713 | 37.9% | 14 | 0.000†* |
| Non-resident | 123 | 115 | 238 | 51.7% | |||
| Monthly family income | Enough | 38 | 75 | 113 | 33.6% | 3.13 | 0.084 |
| Not enough | 355 | 483 | 838 | 42.4% | |||
| Availability of drinking water in the house | available | 370 | 539 | 909 | 40.7% | 3.27 | 0.079† |
| Not available | 23 | 19 | 42 | 54.8% | |||
†Fischer exact test
*Significant, P-value < 0.05
In logistic regression, gender (male) and type of health facility (Hospital) are significantly associated with acute malnutrition (wasting). The odds of a male child have acute malnutrition is 60% higher than that of the female child (adjusted OR 1.6, 95% CI (0.161–0.797), p = 0.003) when other variables are held constant. Also, the odds of a child admitted into hospital having acute malnutrition is 0.45 lower than the child from the PHC facility child (adjusted OR 0.55, 95% CI (-0952–0.239), p = 0.001) when other variables are held constant. Regarding chronic malnutrition (Stunting); gender, type of health facility (Hospital) and residency are significantly associated with chronic malnutrition (stunting). The odds of a male child have chronic malnutrition is 40% higher than that of the female child (adjusted OR 1.4, 95% CI (0.082–0.625) when other variables are held constant, P-value 0.010. The odds of a child admitted into hospital having chronic malnutrition is 80% more than the child from the PHC facility (adjusted OR 1.8, 95% CI (0.345–0.947), P-value 0.000 when other variables are held constant. The odds of child of non-resident family having acute malnutrition are 39% more than the child from resident family (adjusted OR 1.39, 955 CI 0.009- 0.652. P-value 0.040) when other variables are held constant. Table 7
Table 7.
Association of acute/chronic malnutrition and socio-economic characteristics as a result of logistic regression
| Association of acute malnutrition (Wasting) and socio-economic characteristics | |||||
|---|---|---|---|---|---|
| 95%CI | |||||
| socio-economic characteristics | B | Exp(B) | Lower limit | Upper limit | P-value |
| Governorate (Lah) | 0.328 | 0.720 | -0.687 | 0.002 | 0.054 |
| Sex (Male) | 0.470 | 1.600 | 0.161 | 0.797 | 0.003* |
| Type pf health facility (Hospital) | 0.589 | 0.555 | -0.952 | 0.239 | 0.001* |
| Monthly family income | 0.198 | 0.821 | -0.677 | 0.343 | 0.444 |
| Residency (Non -resident) | 0.109 | 0.897 | -0.510 | 0.290 | 0.581 |
| Availability of drinking water | 0.284 | 1.328 | -0.600 | 1.095 | 0.446 |
| Association of chronic malnutrition (Stunting) and socio-economic characteristics | |||||
| Governorate (Lahj) | 0.080 | 1.084 | -0.196 | 0.380 | 0.565 |
| Sex (Male) | 0.347 | 1.414 | 0.082 | 0.625 | 0.010 |
| Type pf health facility (Hospital) | 0.632 | 1.882 | 0.345 | 0.947 | 0.000 |
| Monthly family income | 0.349 | 1.418 | -0.090- | 0.828 | 0.123 |
| Residency (Non -resident) | 0.333- | 1.395 | 0.009- | 0.652 | 0.040 |
| Availability of drinking water | 0.780 | 2.181 | 0.067 | 1.591 | 0.018 |
*Significant at 0.05 significant level
Discussion
This health facility-based study was conducted in two southern governorates in Yemen (Lahj and Abyan) where facing armed conflicts since 2015 affecting negatively upon the provision of the health services and exacerbate the existing malnutrition problem among children under five years. Out of the scope of the routine measurements of malnutrition in the community; this study focused on sick children seeking care in the health facilities for other health problems rather than malnutrition.
In this study; results revealed high prevalence of acute and chronic malnutrition (21.3% & 41.3% respectively) among studied sick children at 12–59 months of age in Lahj and Abyan governorates. This study focused on sick children observed in the outpatient clinics in both primary health care centers and hospitals. The reported rates of malnutrition in this study are higher than what, were reported in other developed or developing countries. Studies in developed countries reported significant proportion of malnutrition among hospitalized patients, Groleau V (2014) in their study in Canada reported that the prevalence of acute and chronic malnutrition among hospitalized children was 13.3% [19]. In another study in Canada in 2014; it was found that prevalence of acute malnutrition among children admitted to pediatric department was 6.9% while prevalence of chronic malnutrition was 13.4% [20]. Hulst J et al., (2004) concluded in their study in Netherlands that among critically ill patients it was found that the prevalence of malnutrition among children admitted to intensive care units (ICU) was 24% [21]. In developing countries, one study in Malaysia reported that the prevalence of acute and chronic under-nutrition among hospitalized children were 11% and 14% respectively [22]. In Pakistan the prevalence of stunting among children attending out-patient clinics was 21% [23]. In one controversial result from Tanzania; the prevalence of stunting and wasting was 8.37% & 1.41% respectively among children attending hospitals and primary care centers with predominance of boys' malnutrition over females [24]. This controversial results of low prevalence are due to methodological issue; investigators targeted all children attend to the health facilities either for seeking care or to attending to well child clinic for vaccination.
Severe acute malnutrition (SAM) has a significant contribution to child death if untreated, and may be exceeded the minimum Sphere standard (< 10%) especially in developing countries like Yemen and Ethiopia [25, 26].
In this study; the prevalence of SAM and MAM in sick children were 6.2% and 12.8% respectively, these figures are higher than the same indicators from community-based survey in Yemen (SAM 4.9%, MAM 8.4%) [27] and Ethiopia (SAM 3.6%, MAM 10.6%) prevalence of SAM in children under 5byears in Ethiopia [28].
Male children are more exposed to both acute and chronic malnutrition than females [29, 30]. In one study in Pakistan authors reported that significant higher prevalence of stunting in males than female children [23].
Concurrent wasting and stunting are an important problem among children under five years and it is considered risk factor to child mortality [31]. in this study; the prevalence of concurrent wasting and stunting was 6.85%, it is similar to prevalence in other developing countries like in Senegal it was 6.2% [31], 5.8% in Ethiopia [32] and 5% in Uganda [33].
Poverty is a critical determinant of malnutrition [34–36]. Yemen is a poor country, with poverty rates in Yemen increasing in recent years. For example, in 2018; the country ranked 178th out of 188 countries in the global Human Development Index ranking. Since 2015; Yemen was facing dramatic situation due to war and multi-epidemics and poverty [37]. Poverty can be both a cause and a consequence of malnutrition [38]. In this study; significant high prevalence chronic malnutrition among non-residents groups (IDPs, refugees and marginalized groups (so-called in Yemen Al-Mahmasheen).
The implication of this study is to give more attention for screening malnutrition among sick children as a routine examination. Studies reported that this routine screening is ignored in the routine medical care of sick children in many developing countries. In one study in Burundi (2019) it was found that only 3% of health workers screened children (6–59 months) for malnutrition [39].
There are certain limitations of this study. The study was limited to a selected health facilities in two governorates in southern Yemen due to logistics and accessibility issues. The study limited to patients attending health facilities in outpatient clinics, so critically ill-children were not included in the study.
Conclusions
High acute and chronic malnutrition rates were identified among sick children seeking care in health facilities in lahj and Abyan governorates in Yemen. These higher malnutrion rates exceeded the SPHERE indicators of malnutrition. Boys are more exposed than girls to acute and chronic malnutrition. Gender (male) and type of health facility (Hospital) are predictors to acute malnutrition (wasting) while gender, type of health facility (Hospital) and residency (Non-resident) are predictors to chronic malnutrition (stunting). Authors advised that early detection of malnutrition in children at outpatient clinics should not be neglected. To avoid this ignorance to treat appropriately and to reduce mortality, authors recommended every sick child observed in outpatient or in-patents pediatric departments should be screening for malnutrition.
Acknowledgements
This study is implemented in Lahj and Abyan governorates in Yemen and aimed to investigate the malnutrition among children at the age of 1-4 years and seeking care in the health facilities. This work can't accomplish without cooperation and coordination with different actors from funding to implementation to finalize of this report. Here, the investigators appreciated the support of The International War and Disaster Victims Protection Association (IRVD) who grant this study, the investigators thank a lot this funding agency for their great support.
The investigators thank Mr. Ahmed Qiad for his great work during the preparation the digital questionnaire, using the KOBO application. Mr Ahmed trained the enumerators in Lahj and Abyan about the electronic monitoring system which developed that makes our daily follow-up easy and more flexible quick. Regarding the fieldwork at the governorate level; Investigators appreciated the great role of Mr. Fahd Abdu (lahj supervisor) and Mr. Kamal Jubran (Abyan supervisor) for their close supervision of the fieldwork. Our thanks extended to the enumerators who did a hard duty in data collection. They collected data from mothers and take the anthropometric measurements of the sick children who attended the selected health facilities in Abyan and Lahj governorates. Finally, the investigators thank mothers who participated in this study by giving valuable data about their children and hope their children receiving a good care and being cured.
Abbreviations
- GAM
Global Acute Malnutrition
- H/A
Height for Age
- HAZ
Height for Age Z score
- HUCOM
Hadhramout University College of Medicine
- FAO
Food and Agriculture Organization
- IDPs
Internally Displaced people
- IPC
Integrated Phase Classification of Food Security
- IRG
International Recognized Government
- IRVD
The International War and Disaster Victims Protection Association
- MAM
Moderate Acute Malnutrition
- MUAC
Mid-upper arm circumference
- OR
Odds Ratio
- 95%CI
95% Confidence Interval
- PHC
Primary Health Care
- SAM
Severe Acute Malnutrition
- SPSS
Statistical Package for Social Sciences
- UNICEF
United Nations Children's Fund
- WFP
World Food Program
- W/H
Weight for Height
- WHO
World health Organization
Author contributions
AL-Waleedi AA and Bin-Ghouth AS participated in proposal development. Bin-Ghouth design the questionnaire and participated in training of data collectors. Al-Waleedi reviewed the questionnaire, organized and supervised the fieldwork. Both authors participated in data analysis, writing the first draft of the final report and reviewed and approved the manuscript.
Funding
The research team obtained fund from The International War and Disaster Victims Protection Association (IRVD).
Availability of data and materials
All data sets are available and can be shared by requesting it from the corresponding author by email.
Declarations
Ethics approval and consent to participate
The research proposal was approved by Research ethics committee of Hadramout University College of Medicine (HUCOM). The objectives of the study were clarified for the participant. We ensured that the information of those who agreed to participate in this study was kept in the strictest confidence and used for the benefit of the community. Writing informed consent was obtained from mothers of studied children. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
Authors declared that there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ali Ahmed Al-Waleedi, Email: Ali_Alwaleedi@hotmial.com.
Abdulla Salem Bin-Ghouth, Email: abinghouth2007@yahoo.com.
References
- 1.McCarthy A, Delvin E, Marcil V, et al. Prevalence of Malnutrition in Pediatric Hospitals in Developed and In-Transition Countries: The Impact of Hospital Practices. Nutrients. 2019;11(2):236. Published 2019 Jan 22. doi:10.3390/nu11020236 Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6412458/ [DOI] [PMC free article] [PubMed]
- 2.The Childhood Acute Illness and Nutrition (CHAIN) Network. Childhood mortality during and after acute illness in Africa and south Asia: a prospective cohort study. Lancet Glob Health 2022; 10: e673–84. Available at: https://www.thelancet.com/action/showPdf?pii=S2214-109X%2822%2900118-8 Accessed 4/5/2022 [DOI] [PMC free article] [PubMed]
- 3.UNICEF. Yemen Humanitarian Situation Report. http://www.unicef.org/mena/UNICEF_Yemen_Crisis_SitRep_-_8_July_to_21_July_2015.pdf. (accessed Feb 28, 2022).
- 4.Abdulaziz M Eshaq, Ahmed M Fothan, Elyse C Jensen, Tehreem A Khan, Abdulhadi A AlAmodi. Malnutrition in Yemen: an invisible crisis. The Lancet. 2017. (389): 10064:31–32. DOI: 10.1016/S0140-6736(16)32592-2 Available at: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)32592-2/fulltext Accessed Feb 11, 2022 [DOI] [PubMed]
- 5.WFP. Yemen emergency. Available at: https://www.wfp.org/emergencies/yemen-emergency Accessed Feb 11,2022
- 6.Al-Zangabila K, Poudel Adhikari S, Wang Q, Sunil TS, Rozelle S, Zhou H. Alarmingly high malnutrition in childhood and its associated factors: A study among children under 5 in Yemen. Medicine (Baltimore) 2021;100(5):e24419. doi: 10.1097/MD.0000000000024419.PMID:33592890;PMCID:PMC7870187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nélio Barreto Vieira, Sionara Melo Figueiredo de Carvalho, Modesto Leite Rolim Neto, Hildson Leandro de Menezes. The silence of the lambs: Child morbidity and mortality from malnutrition in Yemen. Journal of pediatric nyrsing. January 05, 2022. DOI:10.1016/j.pedn.2021.12.006 (Article in Press). Available at: https://www.pediatricnursing.org/article/S0882-5963(21)00374-2/pdf Accessed Feb 11, 2022 [DOI] [PubMed]
- 8.UNICEF. Increasing the cases of malnutrition in young children in Yemen within the deteriorated situation. Available at: https://www.unicef.org/yemen/ar/ Accessed 11/2/2022 (in Arabic)
- 9.UNICEF & Action contra la faim. NUTRITION AND RETROSPECTIVE MORTALITY SURVEY HIGHLANDS AND LOWLANDS LIVELIHOOD ZONES OF ABYAN GOVERNORATE. Final survey report. 2018. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/smart_survey_abyan_jan_2018.pdf Accessed Feb 12, 2022.
- 10.OCHA. NUTRITION AND RETROSPECTIVE MORTALITY SURVEY HIGHLANDS AND LOWLANDS LIVELIHOOD ZONES OF LAHJ GOVERNORATE. Final survey report. 2018. Available at: https://www.humanitarianresponse.info/en/operations/yemen/document/smart-survey-lahj-jul-2017 Accessed Feb 21,2022
- 11.Alves RNP, de Vasconcelos CAC, Vieira NB, Pereira YTG, Feitosa PWG, Maia MAG, de Carvalho SMF, Neto MLR, de Menezes HL. The silence of the lambs: Child morbidity and mortality from malnutrition in Yemen. J Pediatr Nurs. 2022 Jan 5:S0882–5963(21)00374–2. doi: 10.1016/j.pedn.2021.12.006. Epub ahead of print. PMID: 34998655. Available at: https://pubmed.ncbi.nlm.nih.gov/34998655/ Accessed April 16, 2022 [DOI] [PubMed]
- 12.Hecht C, Weber M, Grote V, Daskalou E, Dell’Era L, Flynn D, Gerasimidis K, Gottrand F, Hartman C, Hulst J, et al. Disease associated malnutrition correlates with length of hospital stay in children. Clin Nutr. 2015;34:53–59. doi: 10.1016/j.clnu.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Pawellek I, Dokoupil K, Koletzko B. Prevalence of malnutrition in paediatric hospital patients. Clin Nutr. 2008;27:72–76. doi: 10.1016/j.clnu.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Marino LV, Thomas PC, Beattie RM. Screening tools for paediatric malnutrition: Are we there yet? Curr Opin Clin Nutr Metab Care. 2018;21:184–194. doi: 10.1097/MCO.0000000000000464. [DOI] [PubMed] [Google Scholar]
- 15.Central Statistics Organization, Yemen. Population projection. Available at: http://www.cso-yemen.com/content.php?lng=arabic&id=553 Accessed 1/5/2022).
- 16.L. Naing, T. Winn, B.N. Rusli. Practical Issues in Calculating the Sample Size for Prevalence Studies. Archives of Orofacial Sciences 2006; 1: 9–14. Available at: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.504.2129&rep=rep1&type=pdf Accessed Feb 12, 2022
- 17.MOPH&P. GUIDELINES FOR THE MANAGEMENT OF THE SEVERELY MALNOURISHED IN YEMEN. 1st version. 2008
- 18.WHO. Understanding the Difference Among MAM, SAM, and GAM and their Importance on a Population Basis in: WHO. 2000. The Management of Nutrition in Major Emergencies. Available at: https://www.globalhealthlearning.org/sites/default/files/page-files/MAM%2C%20SAM%2C%20and%20GAM.pdf Accessed Feb 13, 2022
- 19.Groleau V, Thibault M, Doyon M, Brochu EE, Roy CC, Babakissa C. Malnutrition in hospitalized children: prevalence, impact, and management. Can J Diet Pract Res. 2014 Spring;75(1):29–34. doi: 10.3148/75.1.2014.29. PMID: 24606957. [DOI] [PubMed]
- 20.Baxter JA, Al-Madhaki FI, Zlotkin SH. Prevalence of malnutrition at the time of admission among patients admitted to a Canadian tertiary-care pediatric hospital. Pediatric Child Health. 2014;19(8):413–417. doi: 10.1093/pch/19.8.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hulst J et al. Malnutrition in critically ill children from admission to 6 months after discharge. Clinical nutrition. 2004. 23:223–232. Available at: https://d1wqtxts1xzle7.cloudfront.net/44323778/Malnutrition_20critically Accessed 13/4/2022. [DOI] [PubMed]
- 22.Lee WS, Ahmad Z. The prevalence of undernutrition upon hospitalization in children in developing country: a single hospital study from Malaysia. Pediatric and neonatology. 2017. 58; 5: 415–420 DOI: 10.1016/j.pedneo.2016.08.010 available at: https://www.pediatr-neonatol.com/article/S1875-9572(17)30101-8/fulltext Accessed 13/4/2022. [DOI] [PubMed]
- 23.Fatima, Sehrish et al. “Stunting and associated factors in children of less than five years: A hospital-based study.” Pakistan journal of medical sciences vol. 36,3 (2020): 581–585. doi:10.12669/pjms.36.3.1370 [DOI] [PMC free article] [PubMed]
- 24.Juma OA, Enumah ZO, Wheatley H, et al. Prevalence and assessment of malnutrition among children attending the Reproductive and Child Health clinic at Bagamoyo District Hospital. Tanzania BMC Public Health. 2016;16:1094. doi: 10.1186/s12889-016-3751-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bitew ZW, Ayele EG, Worku T, et al. Determinants of mortality among under-five children admitted with severe acute malnutrition in Addis Ababa. Ethiopia Nutr J. 2021;20:94. doi: 10.1186/s12937-021-00750-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Organization WH. Pocket book of hospital care for children: guidelines for the management of common childhood illnesses: World Health Organization; 2013. https://apps.who.int/iris/handle/10665/81170. [PubMed]
- 27.Dureab F, Al-Falahi E, Ismail O, et al. An Overview on Acute Malnutrition and Food Insecurity among Children during the Conflict in Yemen. Children (Basel). 2019;6(6):77. Published 2019 Jun 5. doi:10.3390/children6060077 [DOI] [PMC free article] [PubMed]
- 28.Yeshaneh A, Mulu T, Gasheneit A, Adane D. Prevalence of wasting and associated factors among children aged 6–59 months in Wolkite town of the Gurage zone, Southern Ethiopia, 2020. A cross-sectional study PLoS ONE. 2022;17(1):e0259722. doi: 10.1371/journal.pone.0259722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dukhi N. Global Prevalence of Malnutrition: Evidence from Literature. OPEN ACCESS PEER-REVIEWED CHAPTER. AVAIABLE AT: HTTPS://WWW.INTECHOPEN.COM/CHAPTERS/71665 DOI: 10.5772/intechopen.92006.
- 30.Sand A, Kumar R, Shaikh BT, Somrongthong R, Hafeez A, Rai D. Determinants of severe acute malnutrition among children under five years in a rural remote setting: A hospital-based study from district Tharparkar-Sindh. Pakistan Pak J Med Sci. 2018;34(2):260–265. doi: 10.12669/pjms.342.14977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garenne M, Myatt M, Khara T, Dolan C, Briend A. Concurrent wasting and stunting among under-five children in Niakhar, Senegal. Matern Child Nutr. 2019 Apr;15(2):e12736. doi: 10.1111/mcn.12736. Epub 2018 Nov 25. PMID: 30367556; PMCID: PMC6587969. Accessed 4/5/2022 [DOI] [PMC free article] [PubMed]
- 32.Roba AA, Assefa N, Dessie Y, Tolera A, Teji K, Elena H, Bliznashka L, Fawzi W. Prevalence and determinants of concurrent wasting and stunting and other indicators of malnutrition among children 6–59 months old in Kersa, Ethiopia. Matern Child Nutr. 2021 Jul;17(3):e13172. doi: 10.1111/mcn.13172. Epub 2021 Mar 16. PMID: 33728748; PMCID: PMC8189198. Accessed 4/5/2022 [DOI] [PMC free article] [PubMed]
- 33.Iversen PO, Ngari M, Westerberg AC, Muhoozi G, Atukunda P. Child stunting concurrent with wasting or being overweight: A 6-y follow up of a randomized maternal education trial in Uganda. Nutrition. 2021 Sep;89:111281. doi: 10.1016/j.nut.2021.111281. Epub 2021 Apr 16. PMID: 34090214. Accessed 4/5/2022 [DOI] [PMC free article] [PubMed]
- 34.Siddiqui F, Salam RA, Lassi ZS, Das JK. The Intertwined Relationship Between Malnutrition and Poverty. Front Public Health. 2020;28(8):453. doi: 10.3389/fpubh.2020.00453.PMID:32984245;PMCID:PMC7485412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Panda BK, Mohanty SK, Nayak I, et al. Malnutrition and poverty in India: does the use of public distribution system matter? BMC Nutr. 2020;6:41. doi: 10.1186/s40795-020-00369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rahman MA, Halder HR, Rahman MS, Parvez M. Poverty and childhood malnutrition: Evidence-based on a nationally representative survey of Bangladesh. PLoS ONE. 2021;16(12):e0261420. doi: 10.1371/journal.pone.0261420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ghouth ASB. The Multi-Epidemics in Yemen: the Ugly Face of the War. Ann Infect Dis Epidemiol. 2018; 3(2): 1033. Available at: http://www.remedypublications.com/open-access/the-multi-epidemics-in-yemen-the-ugly-face-of-the-war-1171.pdf
- 38.YEMEN MULTISECTORAL NUTRITION ACTION PLAN 2020–2023. Official report. 2020. Available at: https://mqsunplus.path.org/wp-content/uploads/2020/08/Yemen-MSNAP-FINAL_29April2020.pdf accessed 14/4/2022.
- 39.Nimpagaritse M, Korachais C, Nsengiyumva G, et al. Addressing malnutrition among children in routine care: how is the Integrated Management of Childhood Illnesses strategy implemented at health centre level in Burundi? BMC Nutr. 2019;5:22. doi: 10.1186/s40795-019-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data sets are available and can be shared by requesting it from the corresponding author by email.



