Abstract
Background and objectives
With the intensive study of lung protective ventilation strategies, people begin to advocate the individualized application of positive end-expiratory pressure (PEEP). This study investigated the optimal PEEP in patients during one-lung ventilation (OLV) and its effects on pulmonary mechanics and oxygenation.
Methods
Fifty-eight patients who underwent elective thoracoscopic lobectomy were randomly divided into two groups. Both groups received an alveolar recruitment maneuver (ARM) after OLV. Patients in Group A received optimal PEEP followed by PEEP decremental titration, while Group B received standard 5 cmH2O PEEP until the end of OLV. Relevant indexes of respiratory mechanics, pulmonary oxygenation and hemodynamics were recorded after entering the operating room (T0), 10 minutes after intubation (T1), pre-ARM (T2), 20 minutes after the application of optimal PEEP (T3), at the end of OLV (T4) and at the end of surgery (T5). Postoperative outcomes were also assessed.
Results
The optimal PEEP obtained in Group A was 8.8 ± 2.4 cmH2O, which positively correlated with BMI and forced vital capacity (FVC). Group A had a higher CPAT than Group B at T3, T4, T5 (p < 0.05) and a smaller ΔP than Group B at T3, T4 (p < 0.01). At T4, PaO2 was significantly higher in Group A (p < 0.01). At T3, stroke volume variation was higher in Group A (p < 0.01). Postoperative outcomes did not differ between the two groups.
Conclusions
Our findings suggest that the individualized PEEP can increase lung compliance, reduce driving pressure, and improve pulmonary oxygenation in patients undergoing thoracoscopic lobectomy, with little effect on hemodynamics.
Keywords: Positive end-expiratory pressure, Respiratory mechanics, Oxygenation, Video assisted thoracoscopic surgery
Introduction
One-lung ventilation (OLV) is often required in thoracic surgery to achieve pulmonary isolation. This non-physiological ventilation can affect pulmonary oxygenation and cause changes in respiratory mechanics. During one-lung ventilation, a lung protective ventilation strategy that involves an alveolar recruitment maneuver (ARM) and small tidal volume plus apositive end-expiratory pressure (PEEP) is recommended, which may avoid the overexpansion of the alveoli and its cyclic collapse and reaeration. This strategy allows individualized management according to the patient's specific situation and surgical process.1 For different patients, different responses to the same level of PEEP are generated due to lung heterogeneity, and a recent expert consensus recommendation on lung protective ventilation in surgical patients suggests individualized PEEP strategies can optimize respiratory mechanics and reduce postoperative pulmonary complications.2
Thoracoscopic lobectomy is the most common operation in thoracic surgery, so our study aimed to explore the effect of individualized PEEP on intraoperative respiratory mechanics and pulmonary oxygenation in patients undergoing such surgery, in order to provide a reference for the individualized application of PEEP during surgery in the future.
Methods
This was a prospective, randomized, controlled clinical trial, approved by the medical ethics committee of our hospital (2019PS613K). The research was conducted in accordance with the Helsinki Declaration of 1975 (revised 2000) and all patients signed an informed consent form. The trial was registered at Chinese Clinical Trial Registry (ChiCTR1900027148).
Study population
Patients who underwent elective thoracoscopic lobectomy, with an age above 18 years and an American Society of Anesthesiologists (ASA) physical status I–III were selected. Exclusion criteria included: (1) New York Heart Association (NYHA) classification of cardiac function III–IV; (2) Preoperative hemoglobin <100 g.L-1; (3) presence of pulmonary bullae; (4) a change to wedge resection or thoracotomy during surgery; and (5) operation time less than 30 minutes.
Study protocol
The patients were divided into two groups by computer-generated random sequence after entering the operating room. Electrocardiography and peripheral oxygen saturation (SpO2) were routinely monitored. A radial artery puncture catheter was inserted to monitor invasive arterial pressure and connected to the FloTrac/Vigileo monitor (Edwards Lifesciences Company, Irvine, CA, USA) to continuously observe cardiac output (CO) and stroke volume variation (SVV). A bispectral index (BIS) (Aspect Company, Newton, MA, USA) was also used for keeping a suitable depth of sedation.
After preoxygenation for 5 minutes, the patient received anesthesia induction with sufentanil 0.2 μg.kg-1, etomidate 0.2 mg.kg-1 and cisatracurium 0.15 mg.kg-1. An appropriate type of double lumen was chosen according to the height of the patient and operation requirements. After intubation, we used the fiber bronchoscope to confirm that the double lumen was in the right position. Anesthesia was maintained with inhalation of 1–2% sevoflurane, continuous intravenous infusion of propofol of 4–12 mg.kg-1.h-1 and remifentanil of 0.1–0.2 μg.kg-1.min-1, aiming for a BIS between 40–60. The muscle relaxant, cisatracurium, was used in time according to the need during surgery. The infusion rate of crystalloid solution was 3 mL.kg-1.h-1. Before the end of surgery, analgesia and anti-nausea drugs were routinely administered.
The ventilation settings and related intervention points are as follows. Volume controlled ventilation was adopted. Tidal volume during two-lung ventilation was set to 6–8 mL.kg-1 of predicted body weight with a fractional inspired oxygen concentration (FiO2) of 100%. The inspiration and expiration ratio (I/E) was 1:2 and the respiratory rate was 12–20 times per minute to maintain end-tidal carbon dioxide (EtCO2) between 35–45 mmHg (1 mmHg = 0.133 kPa). After moving the patient to a lateral position, the double lumen was confirmed with the fiber bronchoscope again. The two cuffs were inflated with proper air, and one-lung ventilation began. The tidal volume was changed to 5–7 mL.kg-1 of predicted body weight, with the remaining parameters the same as before. Then, an ARM was performed on the healthy lung under adequate volume status and stable hemodynamics. The method was as follows.3 The initial tidal volume was set to 6 mL.kg-1 of predicted body weight, the I/E was changed to 1:1, and the tidal volume was increased successively by 2 mL.kg-1. Each tidal volume level was maintained for six respiratory cycles until the plateau pressure (PPLAT) exceeded 30 cmH2O (1 cmH2O = 0.098 kPa). Group A was treated with 15 cmH2O PEEP, while Group B was treated with 5 cmH2O PEEP. The respiratory parameters were changed back to the beginning of one-lung ventilation in both groups. Next, group A was titrated using a PEEP decremental trial by starting PEEP at 15 cmH2O. And then the PEEP level was decreased every 2 cmH2O with intervals of 2 minutes until the maximum pulmonary compliance (CPAT) was obtained at the optimum PEEP level.4 Then the PEEP application level of Group A was changed to the optimal PEEP, while Group B remained unchanged. During the above process, if the blood pressure dropped more than 20% of its basic level, ephedrine was promptly administered for intervention. If SpO2 less than 90%, the research process would be suspended. PEEP was discontinued at the end of one-lung ventilation in both groups, and manual pulmonary recruitment was applied to the non-ventilated lung at the beginning of two-lung ventilation.
Outcomes
The following six time points were established: after entering the operating room (T0), 10 minutes after intubation (T1), before ARM (T2), 20 minutes after the application of optimal PEEP (T3), at the end of one-lung ventilation (T4), and at the end of surgery (T5). The relevant respiratory mechanics indexes, including PPLAT, peak pressure (PPEAK), CPAT and driving pressure (ΔP) were recorded at T1–T5. Pulmonary oxygenation indexes including pH, arterial partial oxygen pressure (PaO2) and arterial partial carbon dioxide pressure (PaCO2) at T0, T3 and T4 were recorded. In addition, we recorded the hemodynamic parameters of T0–T5 including mean arterial pressure (MAP), heart rate (HR), CO and SVV. The incidence of postoperative pulmonary complications (including pulmonary infection, atelectasis, hypoxemia) within 3 days and the length of hospital stay after surgery were also assessed.
Sample size
The sample size was calculated based on the primary outcome “the CPAT at T4”. In our preliminary experiments, we included 16 patients. The CPAT at T4 was 33.6 ± 6.1 mL.cm-1 H2O in the experimental group, while in the control group was 27.2 ± 4.7 mL.cm-1 H2O. And on the basis of that, we calculated the sample size and at least 22 patients for each group were required, assuming a two-tailed type I error (α) of 0.01 and a power of 90%. Considering potential data loss, a total of 70 patients were enrolled in this study.
Statistical analysis
The Kolmogorov-Smirnov test was used to evaluate whether continuous variables conform to normal distribution. When it is, continuous variables were represented as mean ± standard deviation and two independent samples t-test was used for comparison between groups, otherwise the Mann-Whitney U test was used. A Pearson correlation test was used to analyze the correlation between two variables. Categorical variables were expressed in the form of the number of cases, and the chi-square test was used for inter-group comparisons. A p-value less than 0.05 was considered statistically significant. SPSS 23.0 software (IBM Corporation, Armonk, NY, USA) was used for data processing.
Results
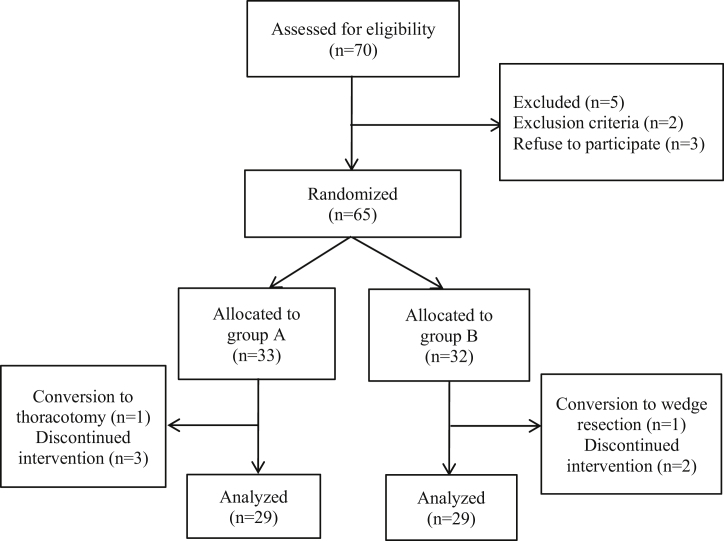
A total of 58 patients, 29 patients in Group A and 29 patients in Group B, were finally included in the analysis (Fig. 1). There were no significant differences in age, sex, ASA physical status, height, weight, body mass index (BMI), surgical site, duration of surgery, duration of OLV, and preoperative pulmonary function between the two groups (Table 1).
Figure 1.
Flow diagram of the study.
Table 1.
Patient demographic data.
| Group A (n = 29) | Group B (n = 29) | p-value | |
|---|---|---|---|
| Age (years) | 59 ± 8 | 60 ± 6 | 0.414 |
| Sex (male/female) | 12/17 | 11/18 | 0.788 |
| ASA (Ⅰ/Ⅱ/Ⅲ) | 1/26/2 | 1/25/3 | 0.896 |
| Height (cm) | 165.9 ± 6.7 | 164.1 ± 7.7 | 0.289 |
| Weight (kg) | 65.7 ± 10.7 | 66.6 ± 9.3 | 0.734 |
| BMI (kg.m-2) | 23.8 ± 3.0 | 24.7 ± 3.0 | 0.246 |
| Surgical site (left/right) | 12/17 | 13/16 | 0.791 |
| Duration of surgery (min) | 130 ± 15 | 129 ± 17 | 0.865 |
| Duration of OLV (min) | 104 ± 13 | 102 ± 16 | 0.575 |
| FEV1 (L) | 2.6 ± 0.6 | 2.4 ± 0.7 | 0.378 |
| FVC (L) | 3.2 ± 0.6 | 3.1 ± 0.8 | 0.561 |
| FEV1/FVC (%) | 80.8 ± 9.1 | 78.6 ± 9.5 | 0.239 |
Values are expressed as mean ± SD for continuous variables and two independent samples t-test is used for inter-group comparisons; Values are expressed as the number of patients for categorical variables and the Chi-Square test is used for inter-group comparisons.
Group A is the experimental group; Group B is the control group.
ASA, American Society of Anesthesiologists physical status; BMI, Body Mass Index; OLV, One-Lung Ventilation; FEV1, Forced Expiratory Volume in the first second; FVC, Forced Vital Capacity.
Optimal PEEP
The optimal PEEP obtained using PEEP decremental titration based on pulmonary compliance in Group A was 8.8 ± 2.4 cmH2O, which was significantly different compared to the fixed 5 cmH2O in Group B (t = 8.47, p < 0.01, 95% CI of the difference was 2.9 to 4.7 cmH2O). In addition, the correlation between the optimal PEEP and patient characteristics was further analyzed. It was found that there was a significant correlation between the optimal PEEP and BMI (r = 0.756, p < 0.01). There was also a correlation between the optimal PEEP and FVC (r = 0.406, p < 0.05).
Respiratory mechanics
There was no significant difference in PPLAT and PPEAK between the two groups at all time points (p > 0.05). Compared with group B, the CPAT of group A at T3, T4 and T5 were higher (p < 0.05). And the ΔP at T3 and T4 in group A were lower (p < 0.01) (Table 2).
Table 2.
Intergroup differences in respiratory mechanics.
| Group | T1 | T2 | T3 | T4 | T5 | |
|---|---|---|---|---|---|---|
| PPLAT (cmH2O) | A | 11.8 ± 2.0 | 18.4 ± 2.3 | 21.9 ± 2.5 | 20.5 ± 2.5 | 11.6 ± 2.3 |
| B | 11.8 ± 2.7 | 18.6 ± 2.6 | 21.4 ± 2.7 | 19.8 ± 2.4 | 12.5 ± 2.8 | |
| PPEAK (cmH2O) | A | 14.1 ± 2.3 | 22.6 ± 2.5 | 26.9 ± 3.1 | 24.5 ± 3.3 | 14.3 ± 2.4 |
| B | 14.8 ± 2.4 | 24.0 ± 3.5 | 26.2 ± 3.8 | 24.6 ± 3.2 | 15.6 ± 2.7 | |
| CPAT (mL.cm-1 H2O) | A | 41.7 ± 6.0 | 23.3 ± 4.8 | 28.9 ± 4.9a | 32.0 ± 5.1b | 41.8 ± 6.3a |
| B | 39.3 ± 6.5 | 21.0 ± 4.5 | 26.3 ± 4.4 | 28.1 ± 4.3 | 37.6 ± 6.6 | |
| ΔP (cmH2O) | A | 11.8 ± 2.0 | 18.4 ± 2.3 | 13.1 ± 3.2b | 11.7 ± 3.3b | 11.6 ± 2.3 |
| B | 11.8 ± 2.7 | 18.6 ± 2.6 | 16.4 ± 2.7 | 14.8 ± 2.4 | 12.5 ± 2.8 |
Values are expressed as mean ± SD for continuous variables and two independent samples t-test is used for inter-group comparisons.
Group A is the experimental group; Group B is the control group.
Two independent samples t-test ap < 0.05, Group A vs. Group B.
Two independent samples t-test bp < 0.01, Group A vs. Group B.
PPLAT, Plateau Pressure; PPEAK, Peak Pressure; CPAT, Pulmonary Compliance; ΔP, Driving Pressure; T1, 10 min after intubation; T2, before ARM; T3, 20 min after the application of optimal PEEP; T4, at the end of one-lung ventilation; T5, at the end of surgery.
Pulmonary oxygenation
There was no statistically significant difference in basic PaO2 between the two groups after entering the operating room without preoxygenation (p > 0.05). PaO2 in Group A was significantly higher than that in Group B at T4 (p < 0.01). There was no significant difference in PaCO2 and pH between the two groups (p > 0.05, Table 3).
Table 3.
Intergroup differences in pulmonary oxygenation.
| Group | T0 | T3 | T4 | |
|---|---|---|---|---|
| PaO2 (mmHg) | A | 79.8 ± 8.6 | 334.2 ± 53.1 | 310.6 ± 43.6b |
| B | 79.1 ± 10.6 | 316.0 ± 45.2 | 237.8 ± 40.4 | |
| PaCO2 (mmHg) | A | 40.7 ± 3.5 | 40.3 ± 2.1 | 41.7 ± 3.2 |
| B | 41.5 ± 2.8 | 40.9 ± 3.0 | 40.8 ± 3.0 | |
| pH | A | 7.41 ± 0.03 | 7.40 ± 0.03 | 7.39 ± 0.03 |
| B | 7.41 ± 0.02 | 7.40 ± 0.03 | 7.39 ± 0.05 |
Values are expressed as mean ± SD for continuous variables and two independent samples t-test is used for inter-group comparisons.
Group A is the experimental group; Group B is the control group.
Two independent samples t-test bp < 0.01, Group A vs. Group B.
PaO2, Arterial Partial Oxygen Pressure; PaCO2, Arterial Partial Carbon Dioxide Pressure; T0, after entering the operating room; T3, 20 min after the application of optimal PEEP; T4, at the end of one-lung ventilation.
Hemodynamics
There was no significant difference in MAP, HR or CO between the two groups at all time points (p > 0.05). Compared with group B, SVV in group A was higher at T3 (p < 0.01), and there were no other statistically significant differences in SVV between the two groups at any other time points (p > 0.05) (Table 4).
Table 4.
Intergroup differences in hemodynamics.
| Group | T0 | T1 | T2 | T3 | T4 | T5 | |
|---|---|---|---|---|---|---|---|
| MAP (mmHg) | A | 103 ± 10 | 85 ± 8 | 86 ± 9 | 82 ± 8 | 86 ± 9 | 94 ± 10 |
| B | 101 ± 10 | 84 ± 8 | 84 ± 8 | 79 ± 5 | 84 ± 7 | 97 ± 9 | |
| HR (beats.min-1) | A | 72 ± 7 | 69 ± 8 | 67 ± 7 | 67 ± 8 | 71 ± 8 | 75 ± 8 |
| B | 70 ± 7 | 66 ± 7 | 69 ± 9 | 67 ± 7 | 69 ± 7 | 75 ± 8 | |
| CO (L.min-1) | A | 5.5 ± 0.4 | 3.9 ± 0.5 | 4.5 ± 0.4 | 4.4 ± 0.4 | 4.7 ± 0.4 | 5.0 ± 0.4 |
| B | 5.4 ± 0.5 | 3.6 ± 0.6 | 4.3 ± 0.4 | 4.2 ± 0.5 | 4.6 ± 0.5 | 4.8 ± 0.5 | |
| SVV (%) | A | 10.8 ± 1.0 | 12.6 ± 1.0 | 11.0 ± 1.1 | 10.0 ± 0.9b | 9.4 ± 0.9 | 9.2 ± 1.0 |
| B | 10.5 ± 0.9 | 12.1 ± 1.4 | 10.4 ± 1.0 | 9.3 ± 0.9 | 9.0 ± 1.0 | 9.2 ± 1.1 |
Values are expressed as mean ± SD for continuous variables and two independent samples t-test is used for inter-group comparisons.
Group A is the experimental group; Group B is the control group.
Two independent samples t-test bp < 0.01, Group A vs. Group B.
MAP, Mean Arterial Pressure; HR, Heart Rate; CO, Cardiac Output; SVV, Stroke Volume Variation; T0, after entering the operating room; T1, 10-min after intubation; T2, before ARM; T3, 20-min after the application of optimal PEEP; T4, at the end of one-lung ventilation; T5, at the end of surgery.
Postoperative pulmonary complications
We followed up the patients in the postoperative 3 days and found that 2 patients in Group A developed pulmonary infection, 3 patients developed atelectasis and 1 patient developed hypoxemia. While in Group B, 3 patients developed pulmonary infection, 6 patients developed atelectasis and 2 patients developed hypoxemia. The length of stay after surgery was 7.4 ± 1.9 days and 8.1 ± 3.1 days respectively. Although the number of cases in Group B was higher, the incidence of postoperative pulmonary complications did not differ between the two groups (p > 0.05). Nor did the postoperative length of stay (p > 0.05).
Discussion
In this study, the optimal PEEP obtained by PEEP decremental titration based on lung compliance after ARM was 8.8 ± 2.4 cmH2O, which was significantly different from the conventional setting of 5 cmH2O, indicating that the values we set in daily use are relatively conservative. This may be due to the adequate pulmonary recruitment with the use of volume controlled ventilation to gradually increase tidal volume and lengthen the I/E, followed by PEEP to maintain the end-expiratory lung volume, which improved ventilation efficiency and reduced physiological dead volume.5, 6 During one-lung ventilation, we slightly reduced the tidal volume to 5–7 mL.kg-1 of predicted body weight, to ensure that patients could obtain enough ventilation similar to two-lung ventilation. In addition, we carried out a further exploration about which patient’s characteristics are relevant to the optimal PEEP. Finally, we found that the optimal PEEP had a significantly positive correlation with BMI, and also had a certain positive correlation with FVC, which may have a guiding significance for clinical practice. As it is difficult to demonstrate the interdependence between them, we are unable to provide a fixed quantitative formula.
As for the comparison of respiratory mechanics, it can be seen that there was no significant difference in airway pressure between the two groups after the application of PEEP. It shows that the application of individualized PEEP, although higher than the commonly used level, does not result in a significant increase in airway pressure. The application of PEEP can effectively improve pulmonary compliance. In our study, the effect of individualized PEEP was more obvious and lasted until the end of surgery, although at the end of one-lung ventilation we had stopped the use of PEEP. Further studies are needed to ascertain how long the effect can last, and whether it could benefit patients in the postoperative period.7 Driving pressure is the pressure gradient required to generate a given tidal volume, equal to the ratio of tidal volume to lung compliance, simplified by PPLAT minus PEEP.8 The use of PEEP reduced driving pressure needed to achieve the same level of tidal volume, and the individualized PEEP was more effective, but this effect was only maintained during one-lung ventilation.
Hypoxemia is a common phenomenon that occurs at the beginning of one-lung ventilation due to the imbalance between ventilation and blood flow, the increase of intra-pulmonary shunting, and the effect of gravity in the lateral position.9, 10 In clinical practice, hypoxemia can be partially alleviated by increasing the concentration of inspired oxygen, manual pulmonary recruitment, using of PEEP and sputum suction.11 In this study, the oxygenation during one-lung ventilation also reached a satisfactory level, and the PaO2 in Group A was significantly higher than that in Group B at T4, indicating that individualized PEEP was helpful for improving oxygenation, although it needed some time to fully exert its effect. Another study compared ventilation under the guidance of minimal driving pressure with traditional lung protective ventilation and found there was no significant difference in oxygenation between groups during one-lung ventilation.12 Furthermore, studies have investigated whether ARM or the use of PEEP can improve oxygenation, and finally concluded that the use of PEEP alone could significantly improve oxygenation in patients undergoing nonabdominal surgery.13 Other studies have suggested that individualized ARM should be followed by individualized PEEP to make ventilation parameter settings more accurate.14 Although these studies have been performed in different types of surgery and have produced slightly different results, the application of individualized PEEP is harmless in general for improving patients’ oxygenation and tend to be continuous after ARM.
Through continuous monitoring of hemodynamics, the application of individualized PEEP did not result in the decrease of cardiac output or dramatic fluctuation in hemodynamics under the premise of optimizing the volume state. It was observed that SVV in Group A was higher than that in Group B at T3, reflecting that a potential liquid demand might exist in the early stage for the use of a higher level of PEEP within a reasonable range. However, it did not affect the cardiac output. It had been reported in the literature that the application level of PEEP above 12 cmH2O during open abdominal surgery could increase the fluid requirements.15 At present, the accuracy of using SVV to guide infusion when using PEEP in thoracic surgery is still in dispute.16, 17, 18 Although, it is important to have a reference that helps understanding the capacity demand of patients according to the dynamic changes of SVV, which needs to be analyzed according to the specific clinical conditions.19
Postoperative pulmonary complications refer to fatal or non-fatal respiratory events newly happened in the postoperative period, including respiratory failure, lung injury, pulmonary infection, atelectasis, hypoxemia, unplanned endotracheal intubation, and mechanical ventilation. They are associated with increased morbidity, length of stay in hospital and mortality after major surgery.20 In this study, we followed up the incidence of pulmonary infection, hypoxemia, and atelectasis within 3 days after surgery and the length of postoperative hospital stay. The diagnosis of pulmonary infection could be made if the white blood cell count exceeded 12*109/L in two consecutive routine blood tests after surgery. The diagnosis of hypoxemia could be made if PaO2 was lower than 60 mmHg in two consecutive blood gas analyses after surgery. Atelectasis was diagnosed by the radiologist according to the result of the pulmonary CT scan on the third day after surgery.
Our study also had some limitations. Firstly, there was no measurement of auto PEEP. Apart from the different effects of the location and the size of lung masses on pulmonary function in patients undergoing thoracic surgery, other pulmonary diseases may have different effects on lung compliance. Patients with obstructive pulmonary disease may have a higher auto PEEP.21 Secondly, we did not measure the pressure in the cuff. There might be cases where the pressure in the cuff was lower than the peak pressure, so that air leakage occurred during the ARM process. Thirdly, the inhalation of pure oxygen in order to exclude the influence of other confounding factors might result in absorptive atelectasis and oxidative stress lung injury.22, 23 Lastly, the postoperative recovery was diagnosed based on the routine examination of patients after surgery due to the limited condition. It seems to be underpowered to evaluate postoperative outcomes. Here we also want to emphasize that some physiological parameters were improved by ARM and PEEP titration, clinical outcomes and even PaO2 benefits seemed somewhat clinically irrelevant, although statistically significant.
Conclusion
In summary, the optimal PEEP obtained by PEEP decremental titration based on individual lung compliance after ARM was 8.8 ± 2.4 cmH2O. On the premise of optimized volume status and stable hemodynamics, the application of individualized PEEP during one-lung ventilation can significantly increase lung compliance, reduce driving pressure, and improve pulmonary oxygenation status, with little effect on hemodynamics.
Conflicts of interest
The authors declare no conflicts of interest.
Glossary
- ΔP
Driving Pressure
- ARM
Alveolar Recruitment Maneuver
- ASA
American Society of Anesthesiologists
- BIS
Bispectral Index
- BMI
Body Mass Index
- CO
Cardiac Output
- CPAT
Pulmonary Compliance
- EtCO2
End-Tidal Carbon Dioxide
- FEV1
Forced Expiratory Volume in the first second
- FiO2
Fractional Inspired Oxygen Concentration
- FVC
Forced Vital Capacity
- HR
Heart Rate
- I/E
Inspiration and Expiration Ratio
- MAP
Mean Arterial Pressure
- NYHA
New York Heart Association
- OLV
One-Lung Ventilation
- PaCO2
Arterial Partial Carbon Dioxide Pressure
- PaO2
Arterial Partial Oxygen Pressure
- PEEP
Positive End-Expiratory Pressure
- PPEAK
Peak Pressure
- PPLAT
Plateau Pressure
- SpO2
Peripheral Oxygen Saturation
- SVV
Stroke Volume Variation
References
- 1.Ball L., Costantino F., Orefice G., et al. Intraoperative mechanical ventilation: state of the art. Minerva Anestesiol. 2017;83:1075–1088. doi: 10.23736/S0375-9393.17.11970-X. [DOI] [PubMed] [Google Scholar]
- 2.Young C.C., Harris E.M., Vacchiano C., et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth. 2019;123:898–913. doi: 10.1016/j.bja.2019.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Severgnini P., Selmo G., Lanza C., et al. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;118:1307–1321. doi: 10.1097/ALN.0b013e31829102de. [DOI] [PubMed] [Google Scholar]
- 4.Maisch S., Reissmann H., Fuellekrug B., et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106:175–181. doi: 10.1213/01.ane.0000287684.74505.49. [DOI] [PubMed] [Google Scholar]
- 5.Choi Y.S., Bae M.K., Kim S.H., et al. Effects of alveolar recruitment and positive end-expiratory pressure on oxygenation during one-lung ventilation in the supine position. Yonsei Med J. 2015;56:1421–1427. doi: 10.3349/ymj.2015.56.5.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wirth S., Kreysing M., Spaeth J., et al. Intraoperative compliance profiles and regional lung ventilation improve with increasing positive end-expiratory pressure. Acta Anaesthesiol Scand. 2016;60:1241–1250. doi: 10.1111/aas.12767. [DOI] [PubMed] [Google Scholar]
- 7.Östberg E., Thorisson A., Enlund M., et al. Positive end-expiratory pressure and postoperative atelectasis: a randomized controlled trial. Anesthesiology. 2019;131:809–817. doi: 10.1097/ALN.0000000000002764. [DOI] [PubMed] [Google Scholar]
- 8.iPROVE Network investigators, Belda J., Ferrando C., et al. The effects of an open-lung approach during one-lung ventilation on postoperative pulmonary complications and driving pressure: a descriptive, multicenter national study. J Cardiothorac Vasc Anesth. 2018;32:2665–2672. doi: 10.1053/j.jvca.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 9.Karzai W., Schwarzkopf K. Hypoxemia during one-lung ventilation: prediction, prevention, and treatment. Anesthesiology. 2009;110:1402–1411. doi: 10.1097/ALN.0b013e31819fb15d. [DOI] [PubMed] [Google Scholar]
- 10.Chobola M., Homolka P., Benej M., et al. Ventilatory efficiency identifies patients prone to hypoxemia during one-lung ventilation. J Cardiothorac Vasc Anesth. 2019;33:1956–1962. doi: 10.1053/j.jvca.2019.01.057. [DOI] [PubMed] [Google Scholar]
- 11.Spadaro S., Grasso S., Karbing D.S., et al. Physiologic evaluation of ventilation perfusion mismatch and respiratory mechanics at different positive end-expiratory pressure in patients undergoing protective one-lung ventilation. Anesthesiology. 2018;128:531–538. doi: 10.1097/ALN.0000000000002011. [DOI] [PubMed] [Google Scholar]
- 12.Park M., Ahn H.J., Kim J.A., et al. Driving pressure during thoracic surgery: a randomized clinical trial. Anesthesiology. 2019;130:385–393. doi: 10.1097/ALN.0000000000002600. [DOI] [PubMed] [Google Scholar]
- 13.Östberg E., Thorisson A., Enlund M., et al. Positive end-expiratory pressure alone minimizes atelectasis formation in nonabdominal surgery: a randomized controlled trial. Anesthesiology. 2018;128:1117–1124. doi: 10.1097/ALN.0000000000002134. [DOI] [PubMed] [Google Scholar]
- 14.Ferrando C., Tusman G., Suarez-Sipmann F., et al. Individualized lung recruitment maneuver guided by pulse-oximetry in anesthetized patients undergoing laparoscopy: a feasibility study. Acta Anaesthesiol Scand. 2018;62:608–619. doi: 10.1111/aas.13082. [DOI] [PubMed] [Google Scholar]
- 15.The PROVE Network Investigators for the Clinical Trail Network of the European Society of Anaesthesiology High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014;384:495–503. doi: 10.1016/S0140-6736(14)60416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suehiro K., Okutani R. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing one-lung ventilation. J Cardiothorac Vasc Anesth. 2010;24:772–775. doi: 10.1053/j.jvca.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 17.Xu H., Shu S.H., Wang D., et al. Goal-directed fluid restriction using stroke volume variation and cardiac index during one-lung ventilation: a randomized controlled trial. J Thorac Dis. 2017;9:2992–3004. doi: 10.21037/jtd.2017.08.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeong D.M., Ahn H.J., Park H.W., et al. Stroke volume variation and pulse pressure variation are not useful for predicting fluid responsiveness in thoracic surgery. Anesth Analg. 2017;125:1158–1165. doi: 10.1213/ANE.0000000000002056. [DOI] [PubMed] [Google Scholar]
- 19.Lema Tome M., De la Gala F.A., Piñeiro P., et al. Behavior of stroke volume variation in hemodynamic stable patients during thoracic surgery with one-lung ventilation periods. Rev Bras Anestesiol. 2018;68:225–230. doi: 10.1016/j.bjane.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Güldner A., Kiss T., Serpa Neto A., et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123:692–713. doi: 10.1097/ALN.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 21.Parrilla F.J., Morán I., Roche-Campo F., et al. Ventilatory strategies in obstructive lung disease. Semin Respir Crit Care Med. 2014;35:431–440. doi: 10.1055/s-0034-1382155. [DOI] [PubMed] [Google Scholar]
- 22.Staehr-Rye A.K., Meyhoff C.S., Scheffenbichler F.T., et al. High intraoperative inspiratory oxygen fraction and risk of major respiratory complications. Br J Anaesth. 2017;119:140–149. doi: 10.1093/bja/aex128. [DOI] [PubMed] [Google Scholar]
- 23.Okahara S., Shimizu K., Suzuki S., et al. Associations between intraoperative ventilator settings during one-lung ventilation and postoperative pulmonary complications: a prospective observational study. BMC Anesthesiol. 2018;18:13. doi: 10.1186/s12871-018-0476-x. [DOI] [PMC free article] [PubMed] [Google Scholar]