ABSTRACT
As Helicobacter pylori management has become more challenging and less efficient over the last decade, the interest in innovative interventions is growing by the day. Probiotic co-supplementation to antibiotic therapies is reported in several studies, presenting a moderate reduction in drug-related side effects and a promotion in positive treatment outcomes. However, the significance of gut microbiota involvement in the competence of probiotic co-supplementation is emphasized by a few researchers, indicating the alteration in the host gastrointestinal microbiota following probiotic and drug uptake. Due to the lack of long-term follow-up studies to determine the efficiency of probiotic intervention in H. pylori eradication, and the delicate interaction of the gut microbiota with the host wellness, this review aims to discuss the gut microbiota alteration by probiotic co-supplementation in H. pylori management to predict the comprehensive effectiveness of probiotic oral administration.
Abbreviations: acyl-CoA- acyl-coenzyme A; AMP- antimicrobial peptide; AMPK- AMP-activated protein kinase; AP-1- activator protein 1; BA- bile acid; BAR- bile acid receptor; BCAA- branched-chain amino acid; C2- acetate; C3- propionate; C4- butyrate; C5- valeric acid; CagA- Cytotoxin-associated gene A; cAMP- cyclic adenosine monophosphate; CD- Crohn’s disease; CDI- C. difficile infection; COX-2- cyclooxygenase-2; DC- dendritic cell; EMT- epithelial-mesenchymal transition; FMO- flavin monooxygenases; FXR- farnesoid X receptor; GPBAR1- G-protein-coupled bile acid receptor 1; GPR4- G protein-coupled receptor 4; H2O2- hydrogen peroxide; HCC- hepatocellular carcinoma; HSC- hepatic stellate cell; IBD- inflammatory bowel disease; IBS- irritable bowel syndrome; IFN-γ- interferon-gamma; IgA immunoglobulin A; IL- interleukin; iNOS- induced nitric oxide synthase; JAK1- janus kinase 1; JAM-A- junctional adhesion molecule A; LAB- lactic acid bacteria; LPS- lipopolysaccharide; MALT- mucosa-associated lymphoid tissue; MAMP- microbe-associated molecular pattern; MCP-1- monocyte chemoattractant protein-1; MDR- multiple drug resistance; mTOR- mammalian target of rapamycin; MUC- mucin; NAFLD- nonalcoholic fatty liver disease; NF-κB- nuclear factor kappa B; NK- natural killer; NLRP3- NLR family pyrin domain containing 3; NOC- N-nitroso compounds; NOD- nucleotide-binding oligomerization domain; PICRUSt- phylogenetic investigation of communities by reconstruction of unobserved states; PRR- pattern recognition receptor; RA- retinoic acid; RNS- reactive nitrogen species; ROS- reactive oxygen species; rRNA- ribosomal RNA; SCFA- short-chain fatty acids; SDR- single drug resistance; SIgA- secretory immunoglobulin A; STAT3- signal transducer and activator of transcription 3; T1D- type 1 diabetes; T2D- type 2 diabetes; Th17- T helper 17; TLR- toll-like receptor; TMAO- trimethylamine N-oxide; TML- trimethyllysine; TNF-α- tumor necrosis factor-alpha; Tr1- type 1 regulatory T cell; Treg- regulatory T cell; UC- ulcerative colitis; VacA- Vacuolating toxin A.
KEYWORDS: Helicobacter pylori, gastrointestinal microbiota, gut metabolome, probiotic supplementation, intestinal homeostasis, metabolic disorder, gastric cancer
Introduction
Gastric carcinoma, as one of the leading causes of cancer-associated deaths, is mainly developed as a result of Helicobacter pylori (H. pylori) infection. The prevalence of H. pylori infection exceeds half of the world’s population; however, the likelihood of affecting health or disease is not uniform and largely relies on host genetics, bacterial virulence, and environmental conditions.1 By leveraging several virulence factors, H. pylori interferes with various cellular components of the host to induce proliferation, apoptosis, migration, and inflammatory responses.2 H. pylori has a substantial association with chronic gastritis, gastric ulcer, mucosa-associated lymphoid tissue (MALT) lymphoma, and gastric adenocarcinoma.3 The combination of up to four drugs including two or three types of antibiotics as well as a proton-pump inhibitor for two weeks is suggested as the first-line of H. pylori treatment.4–6 However, the ideal approach for H. pylori eradication remains elusive and current prescriptions are mostly empirical, heedless of the bacterial antibiotic susceptibility.7
The increased prevalence of antibiotic resistance and antibiotic-associated adverse effects are the primary reasons explaining the requirement for alternative approaches to manage H. pylori infection.8 The interaction of probiotics with the host and gastrointestinal microbiome through alteration in the gut microbiota composition, competition for accessible nutrients and attachment sites, and prevention of bacterial colonization to mediate health benefits indicates the advantage of probiotic co-supplementation in antibiotic treatments.9 Intervention studies have demonstrated a reduction in gastrointestinal symptoms and drug-related side effects by probiotic oral administration.10 However, long-term follow-up investigations are required to elucidate the efficiency of adjuvant interventions on H. pylori treatment.
Here, we aim to highlight the great significance of the host gut microbiota involvement in the competence of probiotic supplementation. We will further discuss the bidirectional interaction of probiotic strains and indigenous gastrointestinal microbiota to predict the effectiveness of this adjuvant therapy and provide an outlook for future investigations within the nascent and promising research field.
Gut microbiota
In addition to the tremendous community of microorganisms inside and on the human body, the gastrointestinal tract harbors a diverse and dynamic consortia of commensal or mutualistic microorganisms, mainly consisting of Firmicutes, Bacteroidetes, Actinobacteria, Proteobacteria, and Verrucomicrobia phyla.11 Based on the ecological characteristics of the gastrointestinal tract, the microbial load ranges from 1012 CFU/ml in the oral cavity and a narrow diversity of 107 CFU/ml in the stomach and duodenum to a vast diversity of 1014 CFU/ml in the colon (Figure 1).12 Due to the reduction in oxygen concentration along the longitudinal axis, the upper gastrointestinal tract is the residence of Gram-positive cocci, such as Gemella and Streptococcus, whereas the intestines and colon are enriched with anaerobes including the Clostridium and Faecalibacterium genera.16 Furthermore, the luminal to mucosal axis organizes the bacteria based on their ability for mucus degradation. Bacteroides thetaiotaomicron, Akkermansia muciniphila, Ruminoccous gnavus, Bacteroides fragilis, and Bifidobacterium bifidium are predominant bacteria within the mucus layer that utilize glycans as their energy source by glycosidase, sulphatase, and sialidase enzymes.17 Despite the dynamic colonization of indigenous commensals within the intestinal niches created by glycans, the lack of dietary fiber polysaccharides potentially emphasizes the significance of the host intestinal mucin as a reliable energy source for the gut microbiota.18
Figure 1.
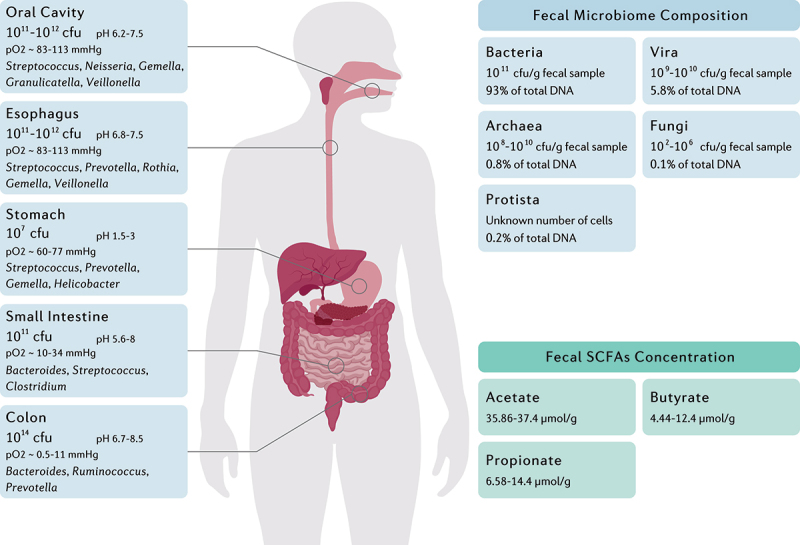
The main genera and total abundance of bacteria vary along the gastrointestinal tract. The colon is characterized by low levels of oxygen as well as the presence of enormous numbers and species of bacteria. On the other hand, the microbial composition and metabolite concentration of stool samples are distinguished from gut biopsies, in which the bacteria and the fungi constitute the majority and minority of total fecal DNA, respectively.12–15 Fecal concentration of SCFAs are also demonstrated as they might be considered key regulators of the intestinal homeostasis.
The role of immune system in shaping gut microbiota
A distinctive characteristic of the intestinal immune system is its capacity to distinguish mutualistic microorganisms from pathogens and further establish active tolerance toward commensal bacteria.19 Identification of microbe-associated molecular patterns (MAMPs) by pattern recognition receptors (PRRs), such as toll-like receptors (TLRs) and nucleotide-binding oligomerization domain receptors (NODs), leads to the activation of various cellular signaling pathways. Consequently, modulation of gene expression by multiple ligands, transcription factors, and kinases can modify the production levels of inflammatory cytokines, chemokines, and immunoreceptors.20 Although pathogens and commensals share common ligands that activate the TLRs, several mechanisms are considered for TLR-mediated discrimination of gut bacteria. Commensals can be simply distinguished from pathogens owing to the lack of virulence factors and differences in invasiveness. Furthermore, the cellular location of TLRs on the intestinal epithelium is inaccessible to commensal bacteria. Different PAMP affinity for TLRs and activation of ligand-specific signaling pathways are other possible mechanisms to identify commensals from pathogens.21 On the other hand, NOD2 recognizes conserved motifs of bacterial peptidoglycan and maintains mucus layer activity; thereby, NOD2 deficiency or mutation might lead to pathogen overgrowth, inflammation, and colon cancer.22 A recent study indicated that NOD2 knockout mice demonstrated an impaired recovery of gut microbiota composition following an antibiotic intervention, suggesting the remarkable contribution of this receptor in shaping the gut microbial community.23 Furthermore, NOD1 activation as a consequence of peptidoglycan recognition can trigger both immune memory and tolerance.24 Irving et al. demonstrated the development of peptidoglycan-specific immunity following H. pylori infection and the subsequent NOD1 activation and autophagy induction.25
The mucus layer of the intestinal epithelium intervenes between the resident microbiome and epithelial layer to form a static shield and narrow the immunogenicity of antigens by provoking dendritic cells (DCs) to an anti-inflammatory response. Moreover, the complex architecture of the intestinal epithelium, as well as their secretions, such as antimicrobial peptides (AMPs) and immunoglobulins, preserve the functionality of the mucosal barrier.26 The most abundant AMPs are defensins that develop small pores in bacterial membranes to disrupt cellular integrity. α- and β-defensins are the two subfamilies of defensins, predominantly released by Paneth cells and colonic epithelial cells, respectively.27 In addition to pore formation, these AMPs can trap bacteria by degenerating the bacterial cytoplasm and developing extracellular net-like structures.28 Furthermore, cathelicidin is the primary AMP expressed during infancy regardless of the bacterial presence and remarkably influences the early development of gut microbiota.29 Perturbation of the gastrointestinal microbiota of preterm and term infants may lead to persistent immune and metabolic disorders.30 Collectively, the intestinal epithelium can establish an efficacious physico-chemical barrier that prevents pathogen colonization on the mucosal surface while creating immune tolerance against commensal bacteria.
In addition to the innate immune system, recent studies exhibited a mutualistic interaction of the adaptive immune system in shaping gut microbial composition. B cells are critical modulators of intestinal homeostasis, mainly through expressing secretory immunoglobulin A (SIgA) in response to commensal recognition.31 The pivotal and often oversimplified role of SIgA depends on the gut microbial community. Chaotic or excessive reaction to alteration in the richness or pro-inflammatory behavior of particular strains by SIgA influences not only the specific bacteria but probably the whole microbiota.32 SIgA predominantly prevents the translocation of microorganisms from lamina propria to the bloodstream, interferes with conjugative plasmid transfer, and facilitates the colonization of commensal bacteria.33 On the other hand, T follicular helper cells are specialized to cooperate with B cells and modify humoral immunity.34 Although several studies began to elucidate the mechanistic interaction of cellular immunity with gut microbiota through inflammatory signaling pathways, we have yet to fully understand the aspects of the adaptive immune system in shaping the gut microbiota.
Gut microbial metabolites in preserving homeostasis
The gut microbiota plays a critical role in preserving the normal bioactivity of the host through gut microbiota-derived metabolites, especially bile acids (BAs), short-chain fatty acids (SCFAs), branched-chain amino acids (BCAAs), trimethylamine N-oxide (TMAO), tryptophan, and indole derivatives.35 Nevertheless, the knowledge concerning the direct effect of the gut microbiota on the host metabolism remains scarce; however, the gastrointestinal microbiota has a particular interaction with mitochondria owing to their common origin.36 It has been recently indicated that delta-valerobetaine production by the gut microbiome reduces cellular carnitine and mitochondrial long-chain acyl-coenzyme A (acyl-CoA); consequently, this obesogenic metabolite prevents mitochondrial fatty acid oxidation and leads to diet-dependent obesity.37
SCFAs are saturated fatty acids acquired from microbiota-accessible carbohydrates and mainly include acetate (C2), propionate (C3), butyrate (C4), and valeric acid (C5) in the human body.38,39 Nevertheless, the abundance of each SCFA depends on substrate availability, gut microbiota composition, and gastrointestinal transit time. SCFAs exhibit several local effects, such as preserving the intestinal barrier integrity and pH reduction as their concentration increase from the distal ileum (6.5–7.5) to the proximal colon (5.5–7.5).40,41 Moreover, SCFAs promote the induction and expansion of intestinal regulatory T cells,42 DCs, and macrophages,43 exert an anti-carcinogenic and anti-oxidative effect in the intestine,44 and suppress pathogen-induced inflammation (Figure 2).45
Figure 2.
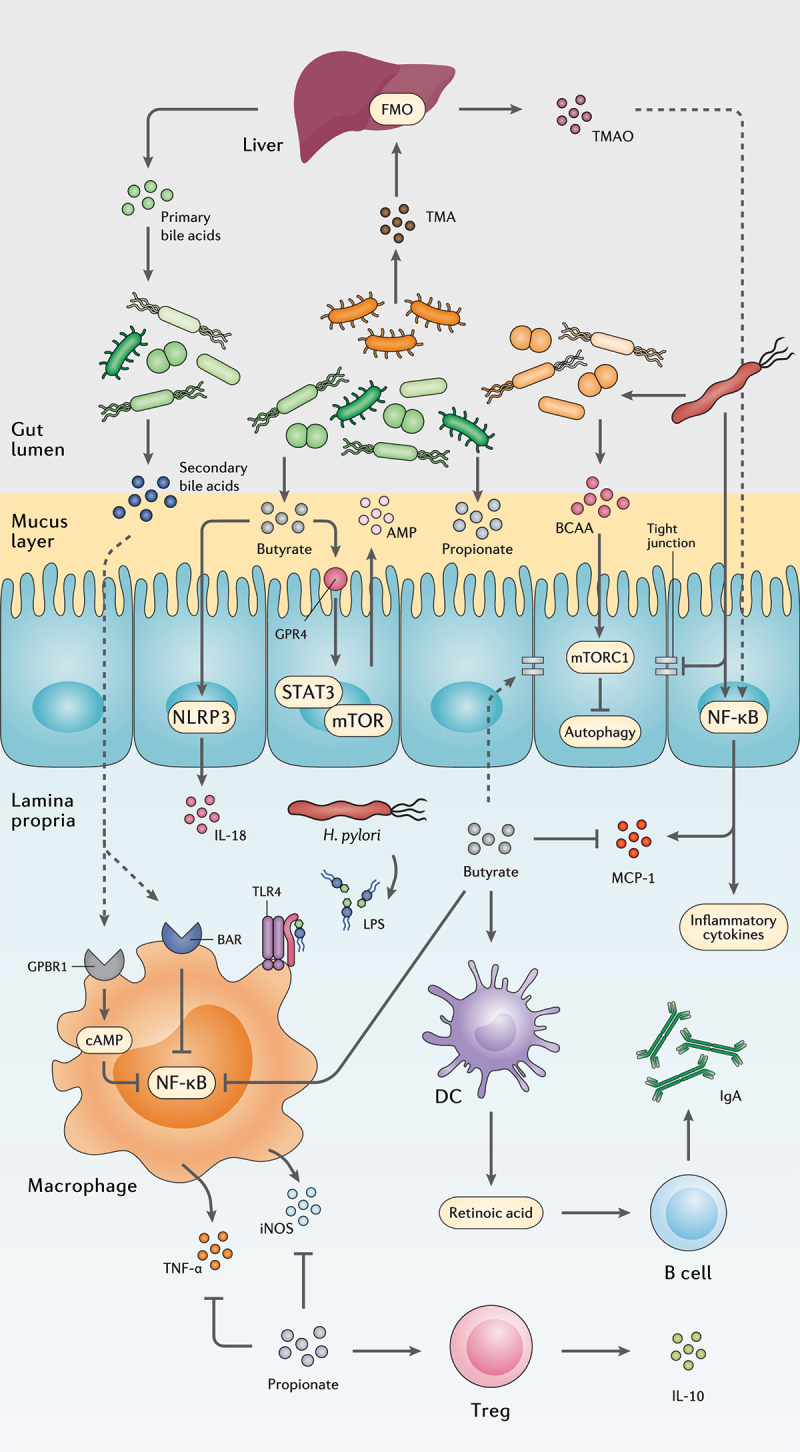
The interplay between the gut metabolome, H. pylori, and the host immune system. H. pylori induces chronic gastric inflammation through the activation of transcriptional factors such as NF-κB. By stimulating the production of BCAA from the gut microbiota, H. pylori activates the mTORC1 complex and ultimately inhibits autophagic response. H. pylori further disrupts the integrity of the gastric epithelial barrier by suppressing the expression of tight junction proteins. On the other hand, microbiota production of SCFAs and secondary bile acids modulate gastric inflammation and immune system activation by reducing NF-κB activation, promoting the secretion of anti-inflammatory cytokines, AMPs, and IgA, and preserving the integrity of the gut barrier.
Hepatocytes synthesize primary bile acids from cholesterol, conjugate them to taurine or glycine, and then release them into the gall bladder to form bile in combination with cholesterol, phospholipids, minerals, electrolytes, bilirubin, biliverdin, and protein.46 Intestinal bacteria will deconjugate primary BAs that fail reabsorption in the terminal ileum and thereby convert them to secondary BAs by microbial biotransformation, including dehydroxylation, epimerization, and oxidation of hydroxyl groups.47 Secondary BAs are involved in the modulation of cell signaling, microbial composition, intestinal metabolism, and the host immune response. Reduced BA deconjugation is associated with inflammatory bowel diseases (IBD) including ulcerative colitis (UC) and Crohn’s disease (CD), as well as irritable bowel syndrome (IBS).48 Free BAs, such as cholic acid, deoxycholic acid, and chenodeoxycholic acid, can stimulate apoptosis and reduce interleukin 6 (IL-6) production, while conjugated BAs such as glycolic acid, glycodeoxycholic acid, and glycochenodeoxycholic acid promote cell growth and induce IL-6 production.49 However, excessive production of the secondary BA deoxycholic acid triggers the expression of inflammatory and tumorigenic factors in hepatic stellate cells (HSCs), contributing to hepatocellular carcinoma development.50 Secondary BAs might also activate farnesoid X receptor (FXR) and elevate the risk of developing colorectal cancer and hepatocellular carcinoma.51
As an essential amino acid in the human body, tryptophan must be obtained by diet and further metabolized through host or microbial pathways. The indole pathway for tryptophan metabolism is mediated by the gut microbiome leading to a variety of indole metabolites, some of which are involved in mucosal homeostasis, gastrointestinal motility, and the host immune response.52 However, BCAAs valine, leucine, and isoleucine are possible biomarkers in human carcinogens owing to their requirement in cancer cell growth and tumor progression.53 Although BCAAs are involved in carcinogenesis and metabolic disorders, such as obesity, insulin resistance, and type 2 diabetes (T2D), sports supplements with these amino acids might improve strenuous training.54
Gut bacteria produces TMA, which is transferred to the liver through the bloodstream and further converted to TMAO by hepatic flavin monooxygenases (FMOs). Animal products such as meat, fish, and eggs are rich in TMA precursors.55 TMAO is a major risk factor for cardiovascular disease, renal fibrosis and functional impairment, atherosclerosis, and colorectal cancer.56,57 It is further indicated that a precursor to TMAO, trimethyllysine (TML), alone and combined with TAMO, is involved in cardiovascular events for patients with the acute coronary syndrome.58
Gut microbial dysbiosis
Defining the gut microbiota composition and function of metabolically healthy individuals is a prerequisite for claiming gut dysbiosis and identifying disease-related biomarkers. The efforts in this field are encountered with an intimidating complexity in the host–microbiota interaction, which needs comprehensive, multidisciplinary approaches for further elucidation.59 Although a healthy microbiome composition is yet to be determined, the relative alteration of gastrointestinal microorganisms in disease conditions can be mainly classified as pathobiont enrichment, commensal depletion, or diversity reduction.60 Pathobionts are among the host indigenous microbiome that can trigger or accelerate diseases in particular genetic or environmental conditions.61 An increased proportion of Enterobacteriaceae, including Escherichia coli, Klebsiella spp., and Proteus spp., is a typical example of pathobionts enrichment. This family of Gram-negative symbionts is commonly overgrown in multiple inflammatory situations including intestinal bowel disease, obesity, celiac disease, colon cancer, and antibiotic therapies.62 In contrast to the overgrowth of pathobionts, the gut microbial community frequently suffers a tremendous depletion or total loss of some commensal bacteria following microbial elimination or reduced bacterial proliferation.60 Commensal bacteria are responsible for providing energy resources for the host enterocytes,63 inhibiting pathogen colonization,64 preserving lymphoid tissue architecture, and regulating the immune response.26 Bio-engineered commensal supplementation is an innovative strategy, recently used for delivering tailored substances to target particular metabolic pathways.65 On the other hand, a common and recurrent feature of disease-related dysbiosis is reduced microbial diversity. Although reduced alpha diversity might be the effect rather than the cause of disorders, this characteristic is correlated to gastrointestinal and extra-gastrointestinal diseases, such as CD, IBS, colorectal cancer, and autism.66 Furthermore, the development of a mature microbiome through lifespan highly relies on alpha diversity. Interestingly, specific bacteria can be used as markers for the development and maturation of the microbiota such as R. gnavus, which is inversely correlated to microbial richness at all ages and reduces from childhood toward adulthood.67 Accordingly, there is a delicate interaction between gut homeostasis and the host biological function. Disruption of the intricate equilibrium of metabolic interactions by pathogen colonization or microbiota modifying interventions can damage the integrity of the gut barrier, change the host indigenous bacteria, and further lead to metabolic disorders.
H. pylori and gut microbiota
The clinical implications of H. pylori infection are not limited to gastrointestinal disorders but also include H. pylori association with obesity, diabetes, IBD, allergic disorders, as well as cardiovascular, hepatobiliary, skin, kidney, autoimmune, neurologic, and psychiatric diseases.68 This might indicate the importance of H. pylori and gut microbiota crosstalk, as several mechanisms are reported for this pathogen influencing the host microbiome.69 Modulation of the host immune response, manipulation of the cellular signaling, impairment of the epithelial cell polarity, and alteration of gastric acidity are the primary mechanisms contributing to gut microbiota alteration during H. pylori infection.70 Below, we discuss several aspects of H. pylori infection interacting with gastric and intestinal microbiome, as well as gut microbial metabolites (Figure 3).
Figure 3.
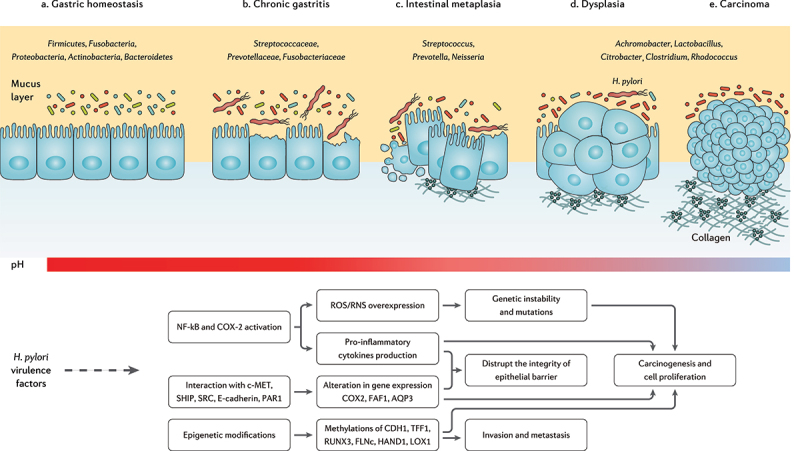
The progression of chronic gastritis toward gastric carcinoma has been characterized by the reduction in the Helicobacter genus, overgrowth of opportunistic bacteria, increased apoptosis, necrosis, and collagen production, changes in the cytoskeleton and polarity of the gastric epithelium, and gradual suppression of gastric acidity. The main mechanisms of action through which H. pylori virulence factors promote the risk of developing gastric cancer are further depicted.71–73
Gastric microbiota
In the last decade, several studies have compared the gut microbiota composition of H. pylori-infected and non-infected individuals, reporting controversial data even regarding the diversity and richness of the microbial community.74 It is possibly due to the remarkable dependence of microbiota composition on individual and environmental factors, such as host genetics, ethnicity, geography, socioeconomic status, and diet.75,76 Furthermore, the microbial community is highly variable along the longitudinal axis of gastrointestinal tract. Hence, in a recent study, corpus and antrum bacteria were reported to significantly differ between individuals positive or negative for H. pylori, while the bacterial community from the lower gastrointestinal tract and stool samples were comparable.77
Although H. pylori antigen load exhibited a reverse relationship with Fusicatenibacter, Alistipes, Bacteroides, and Barnesiella genera, gut microbiota composition is mainly dominated by the same phyla yet different richness in H. pylori-infected and non-infected individuals.72 Streptococcus, Neisseriae, Prevotella, Rothia, Fusobacterium, Veillonella, and Haemophilus are considered the main gastric bacterial genera enriched in H. pylori-positive individuals, compared to H. pylori-negative subjects.78,79 Likewise, the overgrowth of Candida species in the stomach has been reported during H. pylori infection, which might result in synergistic effects on the H. pylori pathogenesis.80 However, H. pylori-induced gastric microbiota alteration is strain-specific and independent of the host-microbial colonization burden. A recent in vivo study demonstrated the substantial reduction of Akkermansia, Bacteroides, and Lachnospiraceae genera in gerbils infected with a cytotoxin-associated gene A (CagA)-positive H. pylori strain compared to a CagA-negative strain. Yet, comparable alpha diversity for the gastric microbiota has been reported for the investigated groups.81 Furthermore, allelic variation in the H. pylori vacuolating toxin A (VacA) is associated with distinct modification of the gastric microbiota.82
The microbiome alteration further relies on the stages of gastric tumorigenesis along with substantial enrichment of oral microbial species including Peptostreptococcus stomatis, Streptococcus anginosus, Parvimonas micra, Slackia exigua, and Dialister pneumosintes toward carcinogenesis.83 Some studies reported an increased colonization burden and microbial diversity, as well as the overgrowth of cancer promoting bacteria in the gastric mucosa of patients with gastric cancer compared to gastritis.84,85 However, a metagenomics study indicated that the microbiota tends to be gradually depleted in the gastric mucosa from non-atrophic gastritis toward intestinal metaplasia and gastric cancer. In this regard, a significant reduction in TM7, Porphyromonas sp, Neisseria sp, and Streptococcus sinensis, as well as a substantial enrichment in Lactobacillus coleohominis and Lachnospiraceae have been further reported.86
Even though Helicobacter is the most abundant genus in chronic gastritis, gastric carcinoma is reported with a significant reduction in the proportion of this genus. Meanwhile, certain commensals but potentially opportunistic pathogenic taxa such as Citrobacter, Clostridium, Lactobacillus, Achromobacter, and Rhodococcus were found to be enriched among gastric microbiota in gastric cancer.87 Another study further reported Streptococcus, Lactobacillus, Veillonella, Prevotella, Neisseria, and Haemophilus as the highly prevalent gastric microbial genera in patients with gastric carcinoma.88 Consistent with the foregoing data, an enriched proportion of Fusobacterium, Neisseria, Prevotella, Veillonella, and Rothia genera have been characterized in patients with advanced gastric lesion compared to the healthy/superficial gastritis group.89
Lactic acid bacteria are mainly reported as protective bacteria in gastric carcinoma, while their increased abundance during cancer progression might indicate otherwise. Reactive oxygen species (ROS), N-nitroso compounds (NOC), and lactate production, as well as induction of epithelial–mesenchymal transition (EMT) and immune tolerance, are among carcinogenic factors promoted by lactic acid bacteria.90 On the other hand, the destruction of stomach hydrochloric acid-producing glands by H. pylori infection increases the stomach pH and eventually promotes the colonization of NOC-producing bacteria.91,92 Veillonella, Clostridium, Haemophilus, Staphylococcus, Neisseria, Lactobacillus, and Nitrospirae are involved in gastric carcinogenesis by NOC production and further induction of mutagenesis, angiogenesis, and proto-oncogenes expression as well as apoptosis prevention.90
Intestinal microbiota
Compared to studies exploring the influence of H. pylori on the gastric microbiota, a limited number of studies investigated the effect of H. pylori on the intestinal microbiota. Considering the intestinal microbiota at the phylum level, Firmicutes, Proteobacteria, Actinobacteria, and Acidobacteria have been elevated, while Bacteroidetes has been reduced following H. pylori infection.93,94 At the genus level, Bacteroides, Barnesiella, Alistipes, and Fusicatenibacter have been negatively associated with H. pylori stool antigen load.95 Lapidot et al. also demonstrated a strong association between H. pylori infection and Prevotella copri and Eubacterium biforme in school-age children.96 Additionally, long-term H. pylori infection of Mongolian gerbils has been characterized by Akkermansia enrichment in the colon.97 Moreover, Candida glabrata and other unclassified fungi have been reported to be increased in stool samples following H. pylori infection in adults.98 However, regarding the alpha diversity of the intestinal microbiota, contradictory reports indicated microbial enrichment,98–100 microbial depletion101 or no significant alteration102–104 in H. pylori-infected patients. Except for one study, no significant alteration has been indicated for microbial alpha diversity following H. pylori infection. This might suggest that H. pylori promotes the host’s resilience against microbial depletion, reflecting the co-evolution of H. pylori and humans over tens of thousands of years.95,105 Furthermore, the geological and cultural differences among the investigated population might be responsible for the inconsistency in the aforementioned studies.106 Several aspects of H. pylori-induced alteration of intestinal microbiota remain to be further investigated. However, H. pylori-induced gastric immunopathogenesis including hypochlorhydria and hypergastrinemia is held responsible for H. pylori-associated intestinal dysbiosis.107,108
Gut metabolome
H. pylori interactions with epithelial cells results in disruption of tight junctions and activation of the host inflammatory responses (Figure 2).109 This recalcitrant pathogen provokes the activity of the nuclear factor kappa B (NF-κB) transcription factor, stimulates the expression of monocyte chemoattractant protein-1 (MCP-1) from epithelial cells to induce monocyte infiltration, and activates monocytes through LPS interaction with TLR4. Consequently, H. pylori infection leads to the overexpression of pro-inflammatory cytokines including induced nitric oxide synthase (iNOS), tumor necrosis factor-α (TNF-α), interferon-gamma (IFN-γ), IL-8, IL-6, IL-4, and IL-1β.110
The interaction between H. pylori infection and SCFA is far from being fully elucidated, yet the reduction of SCFA has been reported in the feces of H. pylori-infected mice.111 Specifically, butyrate promotes intestinal barrier function via activating AMP-activated protein kinase (AMPK) or inhibiting claudin-2 production to stimulate the expression of tight junction proteins.40 Through the G protein-coupled receptor 4 (GPR4) and mammalian target of rapamycin (mTOR)/signal transducer and activator of transcription 3 (STAT3) signaling pathway, butyrate promotes AMPs expression in epithelial cells. SCFAs might lead to NLR family pyrin domain containing 3 (NLRP3) inflammasome activation by GPR4 receptor inducing IL-18 secretion from the epithelium. GPR109A is a surface receptor on DCs and macrophages that detects butyrate and further induces the development of regulatory T cells (Treg) and prevents the proliferation of T helper 17 (Th17) cells.112 Moreover, butyrate can suppress the production of iNOS, TNF-α, IL-6, MCP-1, and IFN-γ by inhibiting NF-κB activation.113 On the other hand, propionate downregulates the production of pro-inflammatory cytokines including IL-4, IL-5, and IL-17A, and stimulates Treg cells to release the anti-inflammatory cytokine IL-10. In LPS-activated monocytes, propionate is reported to inhibit TNF-α and iNOS expression.45 It is also suggested that the interaction of SCFAs with DCs elevates retinoic acid (RA) production and consequently increases IgA secretion by B cells in lamina propria.114
BAs interaction with bile acid receptor (BAR) in LPS-activated macrophages inhibits NF-κB transcription; therefore, downregulates the overexpression of pro-inflammatory cytokines. Furthermore, G-protein-coupled bile acid receptor 1 (GPBAR1) activation by BAs stimulates cyclic adenosine monophosphate (cAMP) production; therefore, BAs interfere with the NF-κB signaling pathway either directly or through competition of cAMP for the transcription region.115
VacA, as a major virulence factor in H. pylori bacteria, induces cellular autophagy to promote the growth and colonization of this pathogen in the mucosal layer.116 Thereafter, H. pylori may provoke the gut microbiome to produce BCAAs isoleucine, leucine, and valine, and thereby activates the mTORC1 complex to inhibit autophagy within the gut epithelium and further induces chronic inflammation.117 Another inflammatory metabolite in the intestine is TAMO, which induces NF-κB activation and promotes the expression of pro-inflammatory cytokines; consequently, a positive correlation has been reported between TAMO circular concentration and serum levels of IL-8 and TNF-α.118,119
Microbiome modifying interventions
Antibiotic therapy
Clinical studies have used innovative approaches including targeted sequencing of 16S ribosomal RNA (rRNA), PICRUSt (phylogenetic investigation of communities by reconstruction of unobserved states), and high-throughput DNA sequencing to facilitate the identification of microbial gene or taxon as disease biomarkers. Nonetheless, intra-individual variability of the gut microbiota, as well as microbiologically heterogeneous subjects has forced the host–microbiota interaction to remain fraught and challenging.120 Notwithstanding the individual distinctions in microbial composition and the enormous differences in pathologies of metabolic diseases, intervention in the fragile host-microbiota crosstalk can lead to joint and disease-specific alteration in the community and activity of gut microbiota. Obesity, T2D, cardio-metabolic disease, metabolic liver disease, and malnutrition are primary metabolic disorders resulting from microbiome dysbiosis.121
Antibiotic treatment as a major disrupter of the gastrointestinal microbial community may lead to alpha diversity reduction, metabolome alteration, and antibiotic resistance.122 Antibiotic administration not only influences the resistome of the subject to whom it is given, but also the whole population owing to selection for resistance to its function.123 The propagation and spread of antibiotic resistance genes in the mucus layer is a defensive function for gut microbiota to minimize the effect of antibiotics, yet short-term antibiotic therapy can cause a long-term reduction in certain commensal bacteria.124 In addition to the antibiotic-directed modification of the gut microbiota, researchers have reported that intervention therapies can remodel the gene expression and overall metabolic activity of the gastrointestinal microbiota.125 Moreover, PPIs as essential drugs in H. pylori eradication can directly disrupt microbial composition, in addition to increasing the stomach pH and thereby influencing which bacteria reach the intestine.126 It is also suggested that the gut microbiota response to antibiotic treatment is determined by particular bacteria in the pre-treatment microbiome; thereby, targeting these bacteria may reduce the risk of dysbiosis and antibiotic-related metabolic disorders.127
Probiotic supplementation
Multiple microorganisms comply with the definition of probiotics as live microorganisms providing a health benefit when supplemented in sufficient amounts.128 The empirical top-down strategy to study indigenous bacteria enriched in healthy subjects is still a major approach to identify probiotic strains with sufficient beneficial effects on human health.129 Common probiotics classify as probiotic lactic acid bacteria (LAB) such as Lactobacillus spp., Bifidobacterium spp., and Streptococcus spp., non-LAB probiotics, such as Clostridium butyricum, Bacillus spp., and E. coli Nissle 1917, and next-generation probiotics, such as Akkermansia muciniohila, Faecalibacterium prausnitzii, and Bacteroides species.130
The impact of probiotic supplementation on human health has been largely investigated and reported to interfere with acute diarrhea, improve IBD, reduce the risk for late-onset neonatal sepsis, cardiometabolic syndrome, and necrotizing enterocolitis, increase H. pylori eradication rate, decrease the prevalence and intensity of respiratory infection, ease depression and manage atopic dermatitis.131 Although several studies have failed to investigate mucosal or fecal microbiota composition of individuals during therapeutic interventions, strong evidence points out that the effectiveness of probiotic strains might not rely on colonizing the gastrointestinal tract but rather reside in their capacity of sharing genes and metabolites, reinforcing disturbed bacteria, and directly affecting the gut barrier and immune cells.132 The differences in responding to the same probiotic supplementation in healthy adults further suggest that an individual’s basal gut microbiota influences the body’s response to probiotic strains.133 Considering the variabilities in the host genetics, diet, disease-associated dysbiosis, and indigenous gut microbiota composition, the responses to the same intervention therapy might differ within the study population.
Next-generation probiotic supplementation
Next-generation probiotics, also termed as live biotherapeutics, emphasize emerging microorganisms not being used as health-promoting factors to date, which will probably be taken under a drug regulatory framework. Regarding the importance of the gut microbiota, these probiotic strains mainly originate from the human microbiome symbionts including A. muciniphila, F. prausnitzii, and several Bacteroides species.134 A. muciniphila as an abundant bacterium within the host intestine is involved in regulating metabolic pathways, modulating the immune response, and preserving the intestinal barrier.135 The prevalence of this bacterium is negatively associated with obesity, T2D, IBD, and appendicitis.136 Daily administration of 1010 A. muciniphila bacteria to obese volunteers for 90 days is reported to reduce insulin resistance, plasma cholesterol, and the risk for developing liver dysfunction and inflammation, whereas no significant alteration is demonstrated in the gut microbiota.137 On the other hand, F. prausnitzii is reported to be reduced in patients with IBD,138 IBS,139 colorectal cancer,140 obesity, and diabetes.141 Owing to the oxygen sensitivity of this bacterium and several other candidate strains, little is known about their efficiency and safety as probiotic supplements.142 It is suggested that prebiotic co-supplementation with next-generation probiotics may promote the survivability and activity of probiotic strains in the human gut.143 Nevertheless, the development of gastrointestinal modeling through organoid technology can deepen our knowledge of the complexity of probiotic-host interaction and provide the opportunity of designing personalized therapeutics and develop next-generation probiotics.144
H. pylori eradication
International guidelines highly recommend H. pylori eradication for individuals who test positive.145,146 According to the test-and-treat strategy, randomized clinical trials were conducted to demonstrate the long-term safety of H. pylori treatment and further report that despite the transient alteration in gastrointestinal microbiota and elevation in specific antibiotic resistance, this perturbation diminished 8 weeks or one year after treatment. Meanwhile, the reduction in insulin resistance and triglyceride serum concentrations were demonstrated as the advantages of H. pylori management.147 Moreover, the incidence of developing gastric carcinogenesis can be decreased by 50% following therapeutic management of H. pylori infection.148 However, H. pylori eradication not only stimulates gut dysbiosis but may also selects out drug-resistant species from the gut microbiota and further expands single-drug resistance (SDR) and multiple-drug resistance (MDR) mechanisms in other microbial species.149 Furthermore, H. pylori eradication can lead to major drug-related side effects including T2D and gastric adenocarcinoma.150,151 The tight interaction of the gastrointestinal microbiota and host wellness, as well as microbiome alteration and alpha diversity reduction during intervention therapies suggest a substantial involvement of the host microbiota in the adverse effects of H. pylori treatment.152
As the gut microbiota can potentially spread the resistance genes from commensals to pathogens and regulate the host bioactivity,54 reducing antibiotic resistance genes and preserving the intrinsic gut microbiota composition might increase H. pylori eradication rate and reduce collateral damages. Probiotic supplementation during treatment can preserve the host indigenous microbiota, facilitate rebiosis, and restore the intrinsic balance of bacteria in the gastrointestinal tract.153,154 It has been recently indicated that probiotic administration reduces the resistome configuration in colonization-permissive individuals. However, post-treatment probiotic supplementation has been reported to inhibit the reduction of antibiotic resistance genes number and further spread the resistance mechanisms in the intestinal mucosa.155 Cifuentes et al. reported a substantial reduction in resistant genes for lincosamides, tetracyclines, MLS-B (macrolide, lincosamide, and streptogramin B), and beta-lactam class following Saccharomyces boulardii CNCM I-745 supplementation during H. pylori eradication.156 Moreover, a recent meta-analysis of 5792 cases indicated that probiotic supplementation significantly increases the H. pylori eradication rate. Zhang et al. further reported that long-term (>10 days) probiotic administration leads to a statistically higher eradication rate compared with short-term administration.157 However, limited effectiveness has been obtained in H. pylori eradication through probiotic supplementation as the main treatment strategy without being co-supplemented with conventional antibiotic regiments.158
Owing to the high prevalence of H. pylori infection in childhood, mostly adolescence, or young adulthood should be considered for screening studies.148 Clinical symptoms, epidemiology, diagnostic approaches, antibiotic susceptibility, and treatment strategies for H. pylori infection significantly differ from the ones in adults and children.159 Yet, significant improvement has been obtained in H. pylori management, decreasing clinical manifestations, and the incidence of antibiotic-related side effects through probiotic supplementation in children. Lactobacillus casei strains and multi-strain consortia of Lactobacillus acidophilus and Lactobacillus rhamnosus are reported as the foremost adjuvant supplement in promoting H. pylori eradication rate and reducing drug-associated adverse effects in children, respectively.160 However, major limitations to meta-analysis studies include the different study designs, the wide spectrum of the co-supplemented antibiotic regimen, and the few studies conducted on the same probiotic strain.160
Probiotics mechanism of action in modulating H. pylori infection
Studies have indicated that advantageous impacts of probiotics against H. pylori infection occur through a variety of mechanisms, such as reinforcement of gut mucosal barrier, elimination of pathogens, enhancement of the host immune system, and microbiome modification (Figure 4).161 Several probiotic species are antagonistic toward invasive pathogens, yet in H. pylori eradication, solid proof indicates that probiotics mainly reduce antibiotic-induced side effects.162 However, there are considerable limitations in these mechanistic studies including high reliability on cell-culture systems not attributed to complex intestinal environment and low colonization capacity of human probiotic strains in the gastrointestinal tract of mice models.131 Nonetheless, multiple key mechanisms are demonstrated for probiotic administration in clinical, in vitro, and in vivo studies, as detailed further below.
Figure 4.
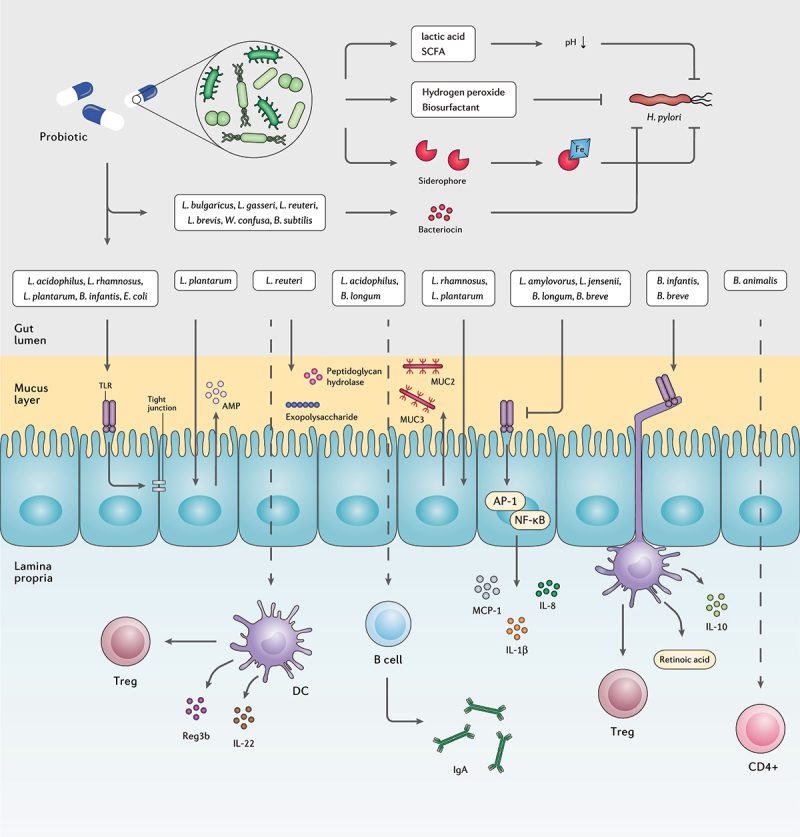
The interplay between probiotic strains, H. pylori, and the host immune system. Several probiotic strains can directly eliminate H. pylori cells by producing bacteriocins, siderophore, hydrogen peroxide, biosurfactant, lactic acid, and SCFAs. Probiotic bacteria can retain the activity of the gut barrier by stimulating the production of mucin and tight junction proteins. Certain probiotic species preserve the inherent structure of the gut microbiota by increasing the concentration of AMPs, peptidoglycan hydrolase, and exopolysaccharides. Furthermore, several probiotic bacteria regulate the host inflammatory response and prevent the development of chronic inflammation.
Promotion of mucosal barrier
The gastrointestinal epithelium as the front line of the host innate defense against pathogenic invaders is required to preserve the integrity of the gastrointestinal barrier. Despite the uncovered mechanisms concerning the exact relationship between the intestinal barrier and inflammatory disorders, a defective epithelial barrier rather than immune dysfunction may result in chronic inflammation.163 Accordingly, H. pylori-associated carcinogenesis is either indirectly accelerated by chronic inflammation and tumorigenesis or directly through induction of epigenetic alteration in the gastric epithelial cells by bacterial factors.164
The protective properties of the mucosal barrier largely rely on the gut microbiota community and their components and metabolites. Due to the presence of mucin glycan, the so-called mucus-associated microorganisms can colonize and attach to the intestinal mucus layer.165 Recent advances in characterizing the beneficial mechanisms of commensal bacteria have led to novel strategies to maintain and promote intestinal barrier function. Lactobacillus plantarum ZS2058 as a probiotic can preserve the gut barrier function and permeability by modulating the expression of tight junctions and improving the intestinal epithelium.166 L. plantarum 299 v and L. rhamnosus GG promote the expression of key mucin genes mucin 2 (MUC2) and MUC3 to maintain the integrity of the intestinal barrier.167 Moreover, L. plantarum ZS2058 is reported enhancing the host defense peptides such as pBD2 and PG1-5; therefore, elevating the intestinal barrier function.166 As a key bacterium in healthcare-related gastrointestinal infection, Clostridioides difficile colonization in the intestine contributes to nosocomial diarrhea with significant morbidity and mortality.168 For which, Lactobacillus reuteri LMG P-27481 is demonstrated to provoke IL-10 production in immature DCs, repair the mucosal barrier function, and obtain a distinguish outcome in preventing C. difficile colonization and toxin load possibly by expressing bioactive molecules including exopolysaccharide and peptidoglycan hydrolases.169
H. pylori can overcome the epithelial barrier by mislocalizing or reducing the expression of tight junction transmembrane protein components including junctional adhesion molecule A (JAM-A) and further disrupt the tight junctional defense barrier.170 The aforementioned mechanism highlights the activity of probiotics, such as L. rhamnosus GG, L. acidophilus, L. plantarum MB452, Bifidobacterium infantis BB-02, and E. coli Nissle 1917 that stimulate TLR activation and further promote epithelial barrier by regulation of tight junction proteins production.171 Nevertheless, some strains such as Lactobacillus amylovorus DSM 16698 T and Lactobacillus jensenii TL2937 negatively regulate TLR activation to inhibit the expression of pro-inflammatory cytokines IL-8 and IL-1β. Moreover, Bifidobacterium longum BB536 and Bifidobacterium breve M-16 V can significantly suppress IL-8, IL-6, and MCP-1 secretion by inhibiting activator protein 1 (AP-1) and NF-κB activation through interaction with TLR and increasing the expression of ubiquitin editing protein A20.172
Secretion of antimicrobial substances
Lactic acid, SCFAs, hydrogen peroxide, and bacteriocin are the major antibacterial substances secreted from probiotics. The incomplete ionization of lactic acid and SCFAs act as proton carriers, lowering the cytoplasmic pH and accumulating toxic anions to prevent H. pylori colonization. Probiotics can further eliminate H. pylori by generating hydrogen peroxide (H2O2) and damaging pathogenic proteins, membrane lipids, and DNA of the bacterial cell.173 However, due to their oxygen tolerance, lactic acid bacteria have anti-oxidative properties suppressing oxidative stress through radical scavenging, metal ion chelation, antioxidant enzyme expression, and host antioxidant and ROS-producing enzyme regulation.174
Bacteriocin expression has been considered as a pivotal property of probiotics to inhibit pathogen colonization and obtain a competitive advantage. The antimicrobial mechanisms of action differ among bacteriocins, yet common mechanisms are the elevation of membrane permeability and prevention of nucleic acid and/or cell wall protein synthesis.175 Bacillus subtilis 3, Weissella confuse PL9001, Lactobacillus gasseri Kx110A1, Lactobacillus brevis ATCC 14869, Lactobacillus bulgaricus, and L. reuteri ATCC 55730 demonstrated inhibitory activity against H. pylori through bacteriocin production.167,173 Less-studied antimicrobial compounds in probiotics are siderophores that prevent pathogen access to iron, biosurfactants that interrupt or lyse pathogen cell membrane, and adhesion inhibitors, which interfere with the pathogen adhesion to epithelial cells and consequently prevent its virulence function.175
Immune promotion
Probiotic strains may indirectly suppress H. pylori infection through the host immune response promotion by stimulating the activity of phagocytoses and natural killer (NK) cells, modifying phenotype and cytokine pattern of DCs, as well as increasing antibody and anti-inflammatory cytokines secretion.176 Interestingly, researchers reported that viable and non-viable bacteria had a different impact on the host cellular gene expression, suggesting the importance of both microbial cell surface and actively released substances on the gut transcriptome.177
B. infantis 35624 and B. breve YIT10347 activate the intestinal DCs by interacting with TLRs and stimulating RA metabolism. As a result, DCs activation elevates the expression of IL-10 and the number of Foxp3+ Treg and type 1 regulatory T (Tr1) cells. Moreover, L. rhamnosus GG and L. acidophilus can reduce the number of Th17 cells and the expression of IL-23 and IL-17 cytokines through prevention of STAT3 and NF-κB signaling and further shift the balance between pro-inflammatory M1 and immunosuppressive M2 macrophage toward M2 phenotype.178 In contrast, Bifidobacterium animalis spp. lactis Bl 5764 is able to promote IL-17A expression by CD4+ T lymphocytes in vitro. L. reuteri Lr 5454 co-culture with DCs can promote Tregs, and regenerating islet-derived protein 3-beta (Reg3b) expression in a NOD2-dependent manner and further induce IL-22 production.179 IL-22 plays an imperative role in preserving gut homeostasis and tissue regeneration. Furthermore, this cytokine accelerates the colonization of Phascolarctobacterium bacterium and thereby prevents C. difficile infection (CDI).180
Immunoglobulin A (IgA) as the main immunoglobulin isotype in the gut mucosa, regulates bacterial translocation and interferes with bacterial toxicity.181 L. acidophilus and B. longum are the major probiotic species demonstrated to increase IgA production from B cells in the intestinal lamina propia.182 Intestinal secretory IgA antibodies coat bacteria to prevent them from adhering the epithelium and barricading inflammation development. However, in vitro studies indicated that commensal microorganisms coated with IgA can grow without remarkable alteration. Moreover, high-affinity IgA coating elevates the risk of bacterial invasion and activation of inflammatory pathways. As H. pylori expresses receptors detecting IgA glycoprotein motifs, IgA attachment to these surface receptors improves H. pylori adhesion to the epithelial layer and facilitates its colonization.183
Probiotic supplementation and gut microbiota alteration
Regarding H. pylori eradication, multiple studies investigated the impact of probiotic administration on the gut microbiota composition (Table 1). In the following sections, we aim to discuss the bioactivity of microbiota that noted significantly altered within the gastrointestinal tract of individuals who underwent H. pylori eradication by probiotic supplementation.
Table 1.
Summary of studies examining the effects of probiotic co-supplementation to H. pylori eradication on the human gut microbiota.
| Studies | Design | Eradication therapy | Probiotic strain/placebo | Methodology | Post-therapy evaluation (week after baseline) | Group specific alteration in the gut microbiota |
|
|---|---|---|---|---|---|---|---|
| Antibiotic/placebo group | Probiotic group | ||||||
| Oh et al., 2016184 | 10 subjects in each group | Amoxicillin 1 g bid, clarithromycin 500 mg bid, lansoprazole 30 mg bid, 14 days | Streptococcus faecium 9 × 108, Bacillus subtilis 1 × 108, twice daily, 14 days | 16S rRNA gene-pyrosequencing (V1-V3) | 2 weeks | Citrobacter, Klebsiella, Pseudomonas, and Escherichia | NS |
| Oh et al., 2016185 | Age: 44–55 3 subjects in each group |
Amoxicillin 1 g bid, clarithromycin 500 mg bid, lansoprazole 30 mg bid, 14 days | Streptococcus faecium 9 × 108, Bacillus subtilis 1 × 108, twice daily, 14 days | Whole metagenome sequencing. Miseq platform (Illumina) | 2 weeks | Klebsiella pneumoniae, Prevotella stercorea ↑ | Lactobacillus ruminis, Escherichia coli, Bacteroides coprocola ↑ |
| Chen et al., 201899 | Age: 18–70 Antibiotic group: 32 subjects Probiotic group: 31 subjects |
Amoxicillin 1 g bid, colloidal bismuth pectin 400 mg bid, furazolidone 100 mg bid, pantoprazole 40 mg bid, 14 days | Clostridium butyricum CBM 588 40 mg tid, 14 days | 16S rRNA gene (V3-V4). Miseq platform (Illumina) | 2 weeks | Lentisphaerae ↓ Proteobacteria, Cyanobacteria ↑ Lactococcus raffinolactis, Lactobacillus sakei, Acinetobacter baumannii NIPH60 ↑ |
Fusobacteria, Tenericutes ↓ Actinobacteria, Cyanobacteria ↑ |
| 8 weeks | NS | NS | |||||
| Wu et al., 2019186 | Age: 18–65 20 subjects with dudenal ulcer in each group |
Amoxicillin 1 g bid, clarithromycin 500 mg bid, esomeprazole 20 mg bid, 14 days | Bacillus subtilis and Enterococcus faecium coated capsules 500 mg tid, 6 weeks following eradication | 16S rDNA (V4) | 2 weeks | Dialister | Actinomadura, Atopobium, Brevundimonas, Butyrivibrio, Coprococcus, Coraliomargarita, Corynebacterium, Desulfobacca, Desulfobulbus, Eggerthella, Faecalibacterium, GOUTA19, Helicobacter, Lewinella, Oscillospira, Rhodobacter, Rhodoplanes, Roseburia, Roseomonas, Rubrivivax, Thauera, Thiobacillus |
| 6 weeks | Dialister, Plesiomonas | Actinomadura, Anaerofilum, Candidatus Nitrososphaera, Candidatus Solibacter, Coprococcus, Coraliomargarita, Dechloromonas, Desulfomonile, Desulfobulbus, Dok59, Dorea, Leuconostoc, Luteimonas, Lewinella, Luteolibacter, Neisseria, Nitrosopumilus, Oscillospira, Parapedobacter, Planctomyces, Thauera, Syntrophobacter, Syntrophomonas, T78, Thermomonas, Thiobacillus | |||||
| 10 weeks | Dialister | Achromobacter, Actinomyces, Cupriavidus, Bradyrhizobium, Candidatus Solibacter, Coprococcus, Chelativorans, Cetobacterium, Thiobacillus, Leuconostoc | |||||
| Cárdenas et al., 2020187 | Age: 18–55 Antibiotic group: 22 Probiotic group:16 |
Amoxicillin 1 g tid, tinidazole 1 g qd, omeprazole 40 mg bid, 14 days | Saccharomyces boulardii CNCM I-745 750 mg qd, 14 days | 16S rRNA. Miseq platform (Illumina) | 2 weeks | NS |
Prevotella, Lachnospira, Ruminococcus ↓ Gammaproteobacteria ↑ |
| 6 weeks | NS |
Prevotella, Lachnospira, Ruminococcus ↓ Gammaproteobacteria ↑ |
|||||
| Kakiuchi et al., 2020188 | Antibiotic group: 26 Probiotic group: 23 |
Amoxicillin 750 mg bid, clarithromycin 400 mg bid, vonoprazan 20 mg bid, 7 days | BFR tid, 7 days | 16S rDNA (V3-V4). Miseq platform (Illumina) | 1 week | Collinsella, Bifidobacterium ↓ | Blautia ↑ |
| Tang et al., 2020189 | Age: 18–65 Placebo group: 74 Probiotic group: 77 |
Amoxicillin 1 g bid, bismuth potassium citrate 220 mg bid, furazolidone 100 mg bid, esomeprazole 20 mg bid, 14 days | Enterococcus faecium 4.5 × 108 and Bacillus subtilis 5.0 × 107, or maltodextrin tid, 4 weeks | 16S rRNA (V3-V4). Miseq platform (Illumina) | 2 weeks | Dialister, Anaerotruncus, Megasphaera | Oscillospira, Citrobacter, Enterococcus |
| 4 weeks | Collinsella, Sutterella, Ruminococcus | Thermomonas, Bacillus, Lactobacillales, Enterococcus | |||||
| 6 weeks | Coprococcus | Bulleidia, Anaerofustis | |||||
| 8 weeks | Faecalibacterium | Phascolarctobacterium | |||||
| Guillemard et al., 2021190 | Age: 18–65 68 subjects in each group |
Amoxicillin 1 g bid, clarithromycin 500 mg bid, pantoprazole 40 mg bid, 14 days | Lacticaseibacillus paracasei CNCM I-1518, Lacticaseibacillus paracasei CNCM I-3689, Lacticaseibacillus rhamnosus CNCM I-3690, Streptococcus thermophilus (CNCM I-2773, CNCM I-2835, CNCM I-2778), Lactobacillus delbrueckii subsp bulgaricus CNCM I-2787, 28 days | 16S rRNA (V3-V4) | 2 weeks | Enterorhabdus, Escherichia-Shigella, Roseburia, Leuconostoc, Akkermansia | Parasutterella, Howardella, Slackia, Desulfovibrio, Streptococcus, Lactobacillus, Alloprevotella, Succiniclasticum |
| 4 weeks | Enterorhabdus, Escherichia-Shigella, Roseburia, Megaphaera | Lactobacillus, Streptococcus, Butyricimonas, Methanobrevibacter, Pediococcus, Parasutterella, Howardella, Slackia, Desulfovibrio | |||||
| 6 weeks | Enterorhabdus, Escherichia-Shigella, Roseburia, Megaphaera, Klebsiella, Succiniclasticum | Pediococcus, Parasutterella, Howardella, Slackia, Desulfovibrio, Megamonas, Lachnospira, Catenibacterium, Butyricimonas | |||||
| Yang et al., 2021191 | Age: 18–70 94 subjects in each group |
Amoxicillin 1 g bid, clarithromycin 500 mg bid, esomeprazole 20 mg bid, 14 days | Non-viable Lactobacillus reuteri DSM17648 2 × 1010 bid, 2 weeks pre-treatment | 16S rRNA (V3-V4) | 2 weeks | Proteobacteria Escherichia-Shigella |
Bacteroidota Bacteroides, Fusicatenibacter |
| 8 weeks | NS | Faecalibacterium, Subdoligranulum | |||||
| Yuan et al., 2021192 | Age: 18–30 Antibiotic group: 34 Probiotic group: 31 |
Amoxicillin 1 g bid, clarithromycin 500 mg bid, potassium bismuth citrate 200 mg bid, esomeprazole 20 mg bid, 14 days | Bifidobacterium tetravaccine tablets included B. infantis >0.5 × 106 CFU/tablet, L. acidophilus >0.5 × 106 CFU/tablet, E. faecalis >0.5 × 106 CFU/tablet, B. cereus >0.5 × 105 CFU/tablet, three tablets each time, three times a day, 14 days | 16S rRNA (V3-V4). Miseq platform (Illumina) | 10 weeks | Gastric mucosa: Erysipelatoclostridium, Ralstonia |
Gastric mucosa: Lachnospiraceae UCG 006 |
| Gastric juice: Proteobacteria was more abundnt than Firmicutes Fusobacterium, Mycoplasma (Tenericutes), Leptotrichia, Campylobacter |
Gastric juice: Firmicutes was more abundnt than Proteobacteria Ruminococcaceae UCG014, Eubacterium ventriosum |
||||||
qd, once a day; bid, twice a day; tid, three times a day; NS, not significant
Single-strain probiotic supplementation
C. butyricum is an anaerobic bacterium that consumes undigested dietary fibers and mainly produces butyrate and acetate. Although some C. butyricum strains are equipped with toxins, others are antibiotic-sensitive and free of pathogenic markers and clostridial toxin genes.193 In particular, C. butyricum CBM 588 can inhibit gastrointestinal inflammation and side effects of antibiotic treatments, such as diarrhea. Consequently, oral administration of this probiotic might prevent inflammation-associated diseases such as UC.194 Chen et al. reported that C. butyricum CBM 588 co-supplementation with H. pylori quadruple therapy exhibited a significant reduction in Fusobacteria and Tenericutes phyla as well as an increase in Actinobacteria phylum following H. pylori eradication. However, Lactococcus raffinolactis, Lactobacillus sakei, and Acinetobacter baumannii NIPH60 were significantly increased only in the antibiotic group.99
Disregarding health conditions, over 100 uncultured Tenericutes have been recently discovered in the human gastrointestinal metagenome. Although the complex behavior of this phylum is not fully understood, Tenericutes bacteria in the host gastrointestinal tract demonstrated a substantial reduction in their genomes and metabolic capacities compared to environmental Tenericutes.195 Furthermore, Tenericutes is suggested to play a key role in the host metabolic pathways, such as bile acid metabolism.196 However, pathogenic species of this phylum are presented with virulence factors including hydrogen peroxide, toxins, surface polysaccharides, and sialic acid catabolism.195 Therefore, the reduction in the population of this taxon may cause various metabolic changes in the host, which needs further in-depth investigations at the strain level. Moreover, Fusobacteria is not prevalent nor relatively enriched in non-colorectal cancer individuals.197 This genus can stimulate cancer cell survival through modulation of STAT3, janus kinase 1 (JAK1), and MYC oncogenes and further induce tumor cell invasion by promoting IL-8 expression.198 Consequently, Fusobacteria depletion in the probiotic supplemented group may indicate a potentially beneficial effect for C. butyricum CBM 588 consumption during H. pylori eradication. On the other hand, A. baumannii bacteria are opportunistic pathogens and mainly contribute to ventilator-associated pneumonia and bloodstream infections.199 This pathogen has become a global health-care problem owing to the several mechanisms underlying its antibiotic resistance.200 As a result, the enrichment of this pathogenic species in the antibiotic group is consistent with the foregoing favorable effectiveness of probiotic administration. However, L. sakei that enriched in the antibiotic group is beneficially involved in obesity, cardiovascular disease, and gastrointestinal inflammation.201
Enterococcus faecium strains are particularly adaptive to their respective environment owing to their salt and acid tolerance. Although E. faecium are antibiotic-resistant infectious agents, they are hardly reported to induce infection in the human body. Moreover, certain E. faecium and E. faecalis strains are the only enterococci bacteria supplemented as probiotics.202 Biofermin-R (multidrug-resistant preparation of E. faecium 129 BIO 3B-R) administration with H. pylori triple therapy demonstrated beneficial advantages.188 This probiotic strain was reported to promote Blautia genus colonization, which is most commonly accompanied by probiotic activities.203 The reduced proportion of Bifidobacterium genus in the antibiotic treated group further highlights the delicate impact of Biofermin-R supplementation on preserving the abundance of probiotic genera among gut bacteria.
Multi-strain probiotic supplementation
A randomized, controlled trial conducted in Germany demonstrated the advantage of probiotic co-supplementation in H. pylori eradication.190 In this study, the intestine of probiotic supplemented individuals was the residence of a higher proportion of Slackia bacteria that are suggested beneficially involved in the host isoflavone, fat, and energy metabolism.204,205 On the other hand, Fusobacterium that was enriched in the antibiotic group was correlated to digestive disorders, gastrointestinal inflammation, and colorectal carcinoma.206,207 However, Desulfovibrio, as Gram-negative sulfate-reducing bacteria, produce hydrogen sulfide and lipopolysaccharide and might contribute to the pathogenesis of Parkinson’s disease;208 consequently, the increased proportion of these bacteria in the gut bacterial community may cause post-therapy adverse effects following probiotic consumption. Moreover, Methanobrevibacter that enriched in the probiotic group are reported more abundant in Parkinson’s disease and gut dysbiosis.209 On the other hand, Roseburia, as major butyrate-producing bacteria in the intestine, can reduce oxidative stress, repair intestinal mucosa, and suppress intestinal inflammation.210 Therefore, the increased abundance of Roseburia bacteria in the antibiotic group may accelerate gut rebiosis after H. pylori treatment.
B. subtilis bacteria are consists of mesophilic, neutrophilic, and some pH tolerant strains with the capacity to produce a vast diversity of antimicrobial compounds.211 Several studies used B. subtilis and E. faecium combination as oral supplemented probiotic and further evaluated their synergic effect on H. pylori eradication, such as the research conducted by Oh et al. exhibiting that resistant bacteria to clarithromycin and amoxicillin, including Citrobacter, Klebsiella, Pseudomonas, and Escherichia, were significantly enriched in the antibiotic group than probiotic-supplemented group.184 Klebsiella pneumoniae, known as Gram-negative opportunistic pathogens, are responsible for the respiratory tract, urinary tract, and bloodstream infections. Due to the antibiotic resistance and hypervirulent characteristic of Klebsiella pneumoniae strains, clinical management of this pathogen has become progressively challenging.212 Oh et al. further reported the increased abundance of Prevotella stercorea in the antibiotic group, whereas Lactobacillus ruminis were enriched in the probiotic group.185 P. stercorea has been suggested to be positively correlated with the expression of mucosal pro-inflammatory cytokines especially TNF-α.213 Despite the poorly understood interaction of L. ruminis with the host biofunction, these bacteria may stimulate immune response through TLR2-mediated NF-κB activation and inhibit the growth of pathogens by acid secretion and competition for binding sites.214
As a result of probiotic administration for H. pylori treatment, Tang et al. reported the enrichment of beneficial bacteria including Oscillospira, Lactobacillales, and Phascolarctobacterium in the feces of probiotic-supplemented individuals.189 Although some studies indicated a positive correlation between Oscillospira and intestinal inflammation, it has been demonstrated that the relative abundance of Oscillospira is negatively associated with the expression of pro-inflammatory MCP-1, as well as the development of UC, IBD, and pediatric nonalcoholic fatty liver disease (NAFLD); therefore, Oscillospira is a candidate for the next-generation probiotics.215 Moreover, Lactobacillales of the Bacilli family can stimulate the innate and adaptive immune system and suppress inflammation by regulating IL-17 production.216 Phascolarctobacterium are reduced in hepatitis B virus-infected patients217 as well as individuals with postpartum depression disorder.218 As succinate consumers, Phascolarctobacterium bacteria can interfere with the colonization of succinate-consuming bacteria; therefore, preventing CDI.219 On the other hand, pathogenic bacteria have been reported to be enriched in the antibiotic group as Dialister, Sutterella, and Collinsella are mainly responsible for gut inflammation, liver diseases, and digestive disorder.220–222 Furthermore, Anaerotruncus that enriched in the antibiotic group are butyrate-producing bacteria with a positive correlation to saturated fatty acid and cholesterol intake; therefore, they are involved in obesity and NAFLD-associated hepatocellular carcinoma (HCC).223,224 Citrobacter genus presented a low virulence activity following their colonization in the gastrointestinal tract. However, increased abundance of Citrobacter species might lead to severe diseases in respiratory and urinary tract, central nervous system, bloodstream, and intestines in the probiotic supplemented patients.225 Anaerofustis genus is associated with movement and psychiatric disorders as well as pro-inflammatory activities.226 Furthermore, decreased starch degradation, possibly as a result of Collinsella reduction, leads to low levels of SCFAs production and weakens the gut epithelial barrier and host immune response in the probiotic group.227 Moreover, certain commensal bacteria including Megasphaera, Ruminococcus, and Coprococcus were significantly increased in the antibiotic group. Although some studies indicated that Ruminococcus species, particularly Ruminococcus gnavus, are correlated with T2D, CD, and UC,228,229 certain species such as Ruminococcus bromii, are abundant in healthy individuals and may lower cardiovascular risk and provide anti-inflammatory compounds through carbohydrate degradation.230,231 Furthermore, the proportion of gut Ruminococcus species is possibly associated with the number of CD8+ Treg cells in the human body, and thereby Ruminococcus bacteria may lower the risk for developing type 1 diabetes (T1D).232 Megasphaera are capable of SCFAs synthesis, osmotic diarrhea regulation, and host immune response promotion.233 Moreover, Coprococcus are inversely correlated to depression, lung cancer, and Parkinson’s disease.234–236
In consistent with the aforementioned studies, Wu et al. reported Dialister and Plesiomonas as the main genera in the patients undergoing H. pylori triple therapy regimen,186,187in which Plesiomonas shigelloides, as a single species in the Plesiomonas genus, is involved in gastrointestinal disorders including gastroenteritis and diarrhea.237 Nevertheless, some pathogenic bacteria, such as Achromobacter, Actinomyces, and Cupriavidus, were enriched during the study follow-up of the probiotic-supplemented group.
Non-viable probiotic supplementation
The capacity of supplemented probiotics to temporarily or persistently colonize the gut mucosa and whether it is essential for their effects on the host biofunction are yet to be fully elucidated. A vast majority of researchers examined the successful probiotic colonization in the host mucosal layer by the proportion of probiotic bacteria in stool without direct assessment of mucosal samples.238 In a recent study, the comparison of fecal and mucosal expansion of supplemented probiotic species demonstrated that fecal presence of probiotic strains cannot identify permissive and resistant individuals, suggesting the passage of probiotic bacteria through the gastrointestinal tract without substantial adhesion nor colonization.239 Consequently, some studies investigated the effects of probiotic strains without the colonization capacity through the administration of dead and inactivated microorganisms, also termed as paraprobiotics.
Through leveraging a non-viable probiotic to reduce the cost and biological risk of treatment, Yang et al. demonstrated Fusicatenibacter, Bacteroides, Faecalibacterium, and Subdoligranulum as the main genera in the stool sample of individuals undergoing H. pylori triple therapy plus probiotic regimen.191 Several Bacteroides species are commensal bacteria providing nutrition and vitamins and playing a key role in cancer immunotherapy and prevention.240 Faecalibacterium genus mainly promote the host immune system by producing anti-inflammatory substances such as butyric acid and bioactive peptides; thereby, the reduced proportion of Faecalibacterium bacteria is correlated with the progression of IBD.241 Although the exact bioactivity of Subdoligranulum are not fully understood, this genus is suggested to have probiotic properties, particularly in the host metabolic health.242 Moreover, Fusicatenibacter are involved in butyric acid production and inversely correlated with IL-8 expression.243 On the other hand, Escherichia-Shigella, as the abundant bacteria in the antibiotic group, are associated with macrophage cell death, gut inflammation, and diarrhea.244,245
A recent study conducted in China reported the advantage of multi-strain probiotic administration in which detrimental bacteria were enriched in the antibiotic group while commensal bacteria were more abundant in the probiotic group.192 Lachnospiraceae UCG 006 and Eubacterium ventriosum, as commensal bacteria, can protect the human intestinal against colorectal cancer by producing SCFAs.246,247 Furthermore, Ruminococcaceae bacteria are one of the main butyrate producers in the human digestive tract; therefore, promoting the integrity of the gut barrier.248 On the other hand, the increased proportion of Leptotrichia is a risk factor for colorectal cancer;249 however, certain Leptotrichia species might be inversely correlated to pancreatic cancer.250 Moreover, Leptotrichia is reported as an oral health-related genus, substantially enriched in healthy individuals without dental caries experience.251
As one of the major causes of gastroenteritis, Campylobacter genus prevalence increased during the last decade globally. Well-studied species within the Campylobacter genus are C. jejuni and C. fetus, mainly responsible for the vast majority of reported Campylobacter infections and bloodstream infections, respectively.252 Therefore, the enhanced colonization of Campylobacter bacteria in the antibiotic group may further emphasize the beneficial effect of paraprobiotic consumption. Although Erysipelatoclostridium are SCFAs producers, the relative abundance of this genus is demonstrated to be enriched in the intestine of patients with gout, metabolic syndrome, and IBS.253,254 Furthermore, Ralstonia is a genus of Gram-negative opportunistic bacteria causing infection in immunocompromised hosts.255 However, these bacteria are more abundant in H. pylori-negative individuals than infected patients.256 Consequently, Erysipelatoclostridium and Ralstonia enrichment may increase the risk of developing gastrointestinal inflammation and immune disorders in the antibiotic group.
The pros and cons of probiotic supplementation
While the safety of probiotic strains constitutes decades of ongoing conflict, researchers have generally reported beneficial advantages of probiotic supplementation in maintaining the host indigenous microbiome and reducing drug-related adverse effects.257 Notwithstanding, probiotic-induced adverse effects are poorly investigated and less noted in clinical trials.258 It has been recently indicated that the exposure of neonates to probiotic species is associated with a higher risk of oral, respiratory, and gastrointestinal infection throughout the lifespan.259 Furthermore, probiotic co-supplemented therapies, especially with Lactobacillus species, might be correlated with a delayed and incomplete post-antibiotic recovery of normal host–microbiome balance resulting in a long-term gut dysbiosis.260
Although fecal microbial composition may not exactly indicate the intestinal mucosa-adherent microbiome,261 only a limited number of clinical trials have investigated the influence of probiotic consumption on the gastrointestinal microbiota in situ. Thus, till the performance of more accurate studies, comparing the microbiota profile of patient’s stool sample following probiotic interventions and various other conditions may roughly represent the long-term safety and efficacy of probiotic supplementation. In this regard, C. butyricum CBM 588 co-supplementation99 may inhibit the replication of commensal bacteria and cause metabolic disorder, meanwhile reducing the risk of colorectal cancer and preventing the overgrowth of certain opportunistic pathogens. Furthermore, consumption of single-strain probiotic Biofermin-R188 may potentially promote the colonization of commensal bacteria.
Concerning multi-strain probiotic supplementation, results from the study by Guillemard et al.190 indicate the possibility of developing Parkinson’s disease and depletion of key butyrate-producing bacteria. However, this study may further point out the beneficial effect of probiotic supplementation through regulating the host isoflavone, fat, and energy metabolism, and reducing the risk of developing digestive disorders, gastrointestinal inflammation, and colorectal carcinoma. On the other hand, B. subtilis and E. faecium administration184,185 can inhibit the colonization of some opportunistic pathogens and potentially prevent respiratory tract, urinary tract, and bloodstream infections, as well as gastrointestinal inflammation. Gastrointestinal microbiota alteration following probiotic supplementation in the Tang et al.189 study further indicates the capacity of probiotic strains to prevent intestinal inflammation, as well as the development of UC, IBD, NAFLD, and CDI. However, the persistence of pathogenic genera in the probiotic supplemented group may provoke the emergence of severe gastrointestinal and extra-gastrointestinal diseases. Moreover, Wu et al.186 reported the enrichment of pathogenic bacteria in both the probiotic and the antibiotic groups. This might indicate limited effectiveness for the consumed probiotic strains in modulating drug-related adverse events.
Data from the study by Yang et al.191 may demonstrate the potential capacity of paraprobiotic consumption in promoting the host immune response, preventing intestinal inflammation and IBD development, and improving nutritional availability. Likewise, paraprobiotic administration192 may also promote the replication of SCFA-producing bacteria and prevent colorectal cancer, and preserve the integrity of the gut barrier. This might further inhibit pathogen colonization and lower the risk of developing bloodstream infection, metabolic syndrome, and IBS.
Limitations and outstanding questions
Extensive complexity might describe the foremost characteristic of the host-microbiota multifaceted interplay. The individual gut microbiota composition at deep resolution levels and enormous structural diversity affecting bacterial functionality remain the challenge of grasping a profound knowledge in the field of host health and probiotic supplementation. This complexity leads to major limitations in determining the source of metabolites as host, probiotic, or indigenous microbiota;54 understanding the whole spectrum of condition-dependent and dose-dependent influence of probiotics; and exploring probiotic-host interaction in cell-culture systems or animal models.131 These limitations are frequently intermingled in ways that force conceptual and statistical interpretation toward substantial challenges. Nonetheless, several cohort studies with probiotic-oriented approaches guided experimental reductionism to elucidate mechanistic comprehension regarding probiotic involvement in human health and disease. Furthermore, the introduction of specific microbiome including probiotic strains into organoids by microinjection is a novel strategy to investigate the accurate cause and effect interaction between the host and microbiome.262
Recent advances in the knowledge about microbiota and the presentation of innovative experimental techniques would enable the integration of strain-specific features of probiotics and consideration of biologically related notions to accelerate the development of tailored therapeutics. The clinically controlled trials are the most practical way toward probiotic strain selection, in which a mechanism-oriented strategy should be pursued and certain questions should be contemplated. Is the probiotic interaction with the host mediated through the secretion of metabolites and alteration of the gut microbiota or colonization of the intestinal surface or other possible contact-dependent interactions? Should a next-generation probiotic strain be considered safe to provide a medical advantage in therapeutic interventions? What are the long-term consequences of probiotic-mediated alteration of the host microbiome? These critically important questions might be resolved by the novel paradigms of microbiome-on-a-chip technology, which can provide the real-time assessment of the host-microbiome interaction and explore the emergence of microbiome-related therapeutics.263
Conclusions and outlook
The oral supplementation of a narrow diversity of Gram-positive bacteria demonstrated distinct amelioration in H. pylori-related clinical symptoms; however, the identified alteration in the gut microbiota demonstrates the possibility of intestinal or extra-gastrointestinal disease development later in life. Considering the enriched and depleted genera in the stool samples of probiotic-supplemented individuals, oral administration of multi-strain probiotics and paraprobiotics than single-strain probiotics might reduce the incidence of developing metabolic disorders. Yet, various characteristics of different strains in a common genus require innovative clinical approaches with high-throughput sequencing technology to determine gut microbiota alteration at the strain level.
Recent studies have expressed the intention of seeking next-generation probiotics and genetically modified microorganisms to promote the beneficial effect of probiotic supplementation in clinical outcomes. Concerning current probiotic strains, two main strategies are suggested for developing next-generation probiotics. One way is to identify the presence or absence of particular strains within the disease condition and investigate the efficiency of supplementing those strains to recover the health state. Another strategy is to harness a well-characterized probiotic strain to express a particular metabolites such as AMPs.264 Recent discoveries in biotechnology will accelerate the emergence of novel candidate probiotic strains and facilitate the transition from empiric into target-oriented interventions. Furthermore, the integration of nanotechnology with microencapsulation strategies may efficiently enhance the probiotic delivery system and thereby provide a regulatory framework to reduce the metabolic consequences of probiotic supplementation. Large-scale population studies with broad-spectrum antibiotic regimens and probiotic strains, as well as germ-free mice modeled by the human microbiome, will shed light on the long-term outcome of probiotic supplementation and elucidate unconventional ways to leverage diet and clinical interventions and personalize them to the subjects’ biology and microbiota.
Acknowledgments
We sincerely thank all the members of the Foodborne and Waterborne Diseases Research Center at the Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Funding Statement
This study was financially supported by a research grant (no. RIGLD 1128, IR.SBMU.RIGLD.REC.1399.046) from the Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Author contributions
ANR and AY contributed significantly to the literature review and wrote the draft of the manuscript. ANR and AY designed and illustrated the figures. AY worked on the concept and design of the study and interpreted the collected information. AS, HAA, and MRZ provided clinical advice and guidance for the improvement of the manuscript. AY and SMS critically revised the final version of the manuscript. All authors have seen and approved the final version of the manuscript and the author list.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this work.
References
- 1.Miller AK, Williams SM.. Helicobacter pylori infection causes both protective and deleterious effects in human health and disease. Genes Immun. 2021;22(4):218–34. doi: 10.1038/s41435-021-00146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nabavi-Rad A, Azizi M, Jamshidizadeh S, Sadeghi A, Aghdaei HA, Yadegar A, Zali MR. The effects of vitamins and micronutrients on helicobacter pylori pathogenicity, survival, and eradication: a crosstalk between micronutrients and immune system. J Immunol Res. 2022;2022:4713684. doi: 10.1155/2022/4713684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Senchukova MA, Tomchuk O, Shurygina EI. Helicobacter pylori in gastric cancer: features of infection and their correlations with long-term results of treatment. World J Gastroenterol. 2021;27(37):6290–6305. doi: 10.3748/wjg.v27.i37.6290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suzuki S, Gotoda T, Kusano C, Ikehara H, Ichijima R, Ohyauchi M, Ito H, Kawamura M, Ogata Y, Ohtaka M, et al. Seven-day vonoprazan and low-dose amoxicillin dual therapy as first-line Helicobacter pylori treatment: a multicentre randomised trial in Japan. Gut. 2020;69(6):1019. doi: 10.1136/gutjnl-2019-319954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malfertheiner P, Megraud F, O’Morain CA, Gisbert JP, Kuipers EJ, Axon AT, Bazzoli F, Gasbarrini A, Atherton J, Graham DY, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66(1):6–30. doi: 10.1136/gutjnl-2016-312288. [DOI] [PubMed] [Google Scholar]
- 6.Liu WZ, Xie Y, Lu H, Cheng H, Zeng ZR, Zhou LY, Chen Y, Wang JB, Du YQ, Lu NH, et al. Fifth Chinese national consensus report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2):e12475. doi: 10.1111/hel.12475. [DOI] [PubMed] [Google Scholar]
- 7.Nyssen OP, Bordin D, Tepes B, Pérez-Aisa Á, Vaira D, Caldas M, Bujanda L, Castro-Fernandez M, Lerang F, Leja M, et al. European registry on Helicobacter pylori management (Hp-EuReg): patterns and trends in first-line empirical eradication prescription and outcomes of 5 years and 21 533 patients. Gut. 2021;70(1):40. doi: 10.1136/gutjnl-2020-321372. [DOI] [PubMed] [Google Scholar]
- 8.McNicholl AG, Molina-Infante J, Lucendo AJ, Calleja JL, Pérez‐Aisa Á, Modolell I, Aldeguer X, Calafat M, Comino L, Ramas M, et al. Probiotic supplementation with lactobacillus plantarum and pediococcus acidilactici for Helicobacter pylori therapy: a randomized, double-blind, placebo-controlled trial. Helicobacter. 2018;23(5):e12529. doi: 10.1111/hel.12529. [DOI] [PubMed] [Google Scholar]
- 9.Cunningham M, Azcarate-Peril MA, Barnard A. Shaping the Future of Probiotics and Prebiotics. Trends Microbiol. 2021;29(8):667–685. [DOI] [PubMed] [Google Scholar]
- 10.Goderska K, Agudo Pena S, Alarcon T. Helicobacter pylori treatment: antibiotics or probiotics. Appl Microbiol Biotechnol. 2018;102(1):1–7. doi: 10.1007/s00253-017-8535-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferraris C, Elli M, Tagliabue A. Gut microbiota for health: how can diet maintain a healthy gut microbiota? Nutrients. 2020;12(11):3596. doi: 10.3390/nu12113596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Vos WM, Tilg H, Van Hul M, Cani PD. Gut microbiome and health: mechanistic insights. Gut. 2022;71(5):1020–1032. doi: 10.1136/gutjnl-2021-326789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hillman ET, Lu H, Yao T, Nakatsu CH. Microbial ecology along the gastrointestinal tract. Microbes Environ. 2017;32(4):300–313. doi: 10.1264/jsme2.ME17017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shkoporov AN, Hill C. Bacteriophages of the human gut: the “known unknown” of the microbiome. Cell Host Microbe. 2019;25(2):195–209. doi: 10.1016/j.chom.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 15.O’Riordan KJ, Collins MK, Moloney GM, Knox EG, Aburto MR, Fülling C, Morley SJ, Clarke G, Schellekens H, Cryan JF, et al. Short chain fatty acids: microbial metabolites for gut-brain axis signalling. Mol Cell Endocrinol. 2022;546:111572. doi: 10.1016/j.mce.2022.111572. [DOI] [PubMed] [Google Scholar]
- 16.Engevik M, Versalovic J. Taking a closer look at the biogeography of the human gastrointestinal microbiome. Gastroenterology. 2019;157(4):927–929. doi: 10.1053/j.gastro.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Herath M, Hosie S, Bornstein JC, Franks AE, Hill-Yardin EL. The role of the gastrointestinal mucus system in intestinal homeostasis: implications for neurological disorders. Front Cell Infect Microbiol. 2020;10:248. doi: 10.3389/fcimb.2020.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martens EC, Neumann M, Desai MS. Interactions of commensal and pathogenic microorganisms with the intestinal mucosal barrier. Nat Rev Microbiol. 2018;16(8):457–470. doi: 10.1038/s41579-018-0036-x. [DOI] [PubMed] [Google Scholar]
- 19.Mowat AM. To respond or not to respond - a personal perspective of intestinal tolerance. Nat Rev Immunol. 2018;18(6):405–415. doi: 10.1038/s41577-018-0002-x. [DOI] [PubMed] [Google Scholar]
- 20.Yoo JY, Groer M, Dutra SVO, Sarkar A, McSkimming DI. Gut microbiota and immune system interactions. Microorganisms. 2020;8(10):1587. doi: 10.3390/microorganisms8101587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le Noci V, Bernardo G, Bianchi F, Tagliabue E, Sommariva M, Sfondrini L. Toll like receptors as sensors of the tumor microbial dysbiosis: implications in cancer progression. Front Cell Dev Biol. 2021;9:732192. doi: 10.3389/fcell.2021.732192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrand A, Al Nabhani Z, Tapias NS, Mas E, Hugot JP, Barreau F. NOD2 expression in intestinal epithelial cells protects toward the development of inflammation and associated carcinogenesis. Cell Mol Gastroenterol Hepatol. 2019;7(2):357–369. doi: 10.1016/j.jcmgh.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moltzau Anderson J, Lipinski S, Sommer F, Pan W-H, Boulard O, Rehman A, Falk-Paulsen M, Stengel ST, Aden K, Häsler R, et al. NOD2 influences trajectories of intestinal microbiota recovery after antibiotic perturbation. Cell Mol Gastroenterol Hepatol. 2020;10(2):365–389. doi: 10.1016/j.jcmgh.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernández-García V, González-Ramos S, Martín-Sanz P, Portillo FG-D, Laparra JM, Boscá L. NOD1 in the interplay between microbiota and gastrointestinal immune adaptations. Pharmacological Research. 2021;171:105775. doi: 10.1016/j.phrs.2021.105775. [DOI] [PubMed] [Google Scholar]
- 25.Irving AT, Mimuro H, Kufer TA, Lo C, Wheeler R, Turner L, Thomas B, Malosse C, Gantier M, Casillas L, et al. The immune receptor NOD1 and kinase RIP2 interact with bacterial peptidoglycan on early endosomes to promote autophagy and inflammatory signaling. Cell Host Microbe. 2014;15(5):623–635. doi: 10.1016/j.chom.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 26.Zheng D, Liwinski T, Elinav E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020;30(6):492–506. doi: 10.1038/s41422-020-0332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zong X, Fu J, Xu B, Wang Y, Jin M. Interplay between gut microbiota and antimicrobial peptides. Animal Nutrition. 2020;6(4):389–396. doi: 10.1016/j.aninu.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lueschow SR, McElroy SJ. The paneth cell: the curator and defender of the immature small intestine. Front Immunol. 2020;11:587. doi: 10.3389/fimmu.2020.00587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liang W, Enee E, Andre-Vallee C, Falcone M, Sun J, Diana J. Intestinal cathelicidin antimicrobial peptide shapes a protective neonatal gut microbiota against pancreatic autoimmunity. Gastroenterology. 2021;162(4):1288–1302.e16. doi: 10.1053/j.gastro.2021.12.272. [DOI] [PubMed] [Google Scholar]
- 30.Healy DB, Ryan CA, Ross RP, Stanton C, Dempsey EM. Clinical implications of preterm infant gut microbiome development. Nat Microbiol. 2022;7(1):22–33. doi: 10.1038/s41564-021-01025-4. [DOI] [PubMed] [Google Scholar]
- 31.Lycke NY, Bemark M. The regulation of gut mucosal IgA B-cell responses: recent developments. Mucosal Immunol. 2017;10(6):1361–1374. doi: 10.1038/mi.2017.62. [DOI] [PubMed] [Google Scholar]
- 32.Pabst O, Slack E. IgA and the intestinal microbiota: the importance of being specific. Mucosal Immunol. 2020;13(1):12–21. doi: 10.1038/s41385-019-0227-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abokor AA, McDaniel GH, Golonka RM, Campbell C, Brahmandam S, Yeoh BS, Joe B, Vijay-Kumar M, Saha P. Immunoglobulin A, an active liaison for host-microbiota homeostasis. Microorganisms. 2021;9(10):2117. doi: 10.3390/microorganisms9102117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krishnaswamy JK, Alsen S, Yrlid U, Eisenbarth SC, Williams A. Determination of t follicular helper cell fate by dendritic cells. Front Immunol. 2018;9:2169. doi: 10.3389/fimmu.2018.02169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agus A, Clément K, Sokol H. Gut microbiota-derived metabolites as central regulators in metabolic disorders. Gut. 2021;70(6):1174–1182. doi: 10.1136/gutjnl-2020-323071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Michaudel C, Sokol H. The gut microbiota at the service of immunometabolism. Cell Metab. 2020;32(4):514–523. doi: 10.1016/j.cmet.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 37.Liu KH, Owens JA, Saeedi B, Cohen CE, Bellissimo MP, Naudin C, Darby T, Druzak S, Maner-Smith K, Orr M, et al. Microbial metabolite delta-valerobetaine is a diet-dependent obesogen. Nature Metabolism. 2021;3(12):1694–1705. doi: 10.1038/s42255-021-00502-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lavelle A, Sokol H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2020;17(4):223–237. doi: 10.1038/s41575-019-0258-z. [DOI] [PubMed] [Google Scholar]
- 39.Portincasa P, Bonfrate L, Vacca M, De Angelis M, Farella I, Lanza E, Khalil M, Wang DQH, Sperandio M, Di Ciaula A, et al. Gut microbiota and short chain fatty acids: implications in glucose homeostasis. Int J Mol Sci. 2022;23(3):1105. doi: 10.3390/ijms23031105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dalile B, Van Oudenhove L, Vervliet B, Verbeke K. The role of short-chain fatty acids in microbiota-gut-brain communication. Nat Rev Gastroenterol Hepatol. 2019;16(8):461–478. doi: 10.1038/s41575-019-0157-3. [DOI] [PubMed] [Google Scholar]
- 41.Nugent SG, Kumar D, Rampton DS, Evans DF. Intestinal luminal pH in inflammatory bowel disease: possible determinants and implications for therapy with aminosalicylates and other drugs. Gut. 2001;48(4):571–577. doi: 10.1136/gut.48.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Traxinger BR, Richert-Spuhler LE, Lund JM. Mucosal tissue regulatory T cells are integral in balancing immunity and tolerance at portals of antigen entry. Mucosal Immunol. 2021;15(3):398–407]. doi: 10.1038/s41385-021-00471-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim CH. Control of lymphocyte functions by gut microbiota-derived short-chain fatty acids. Cell Mol Immunol. 2021;18(5):1161–1171. doi: 10.1038/s41423-020-00625-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu P, Wang Y, Yang G, Zhang Q, Meng L, Xin Y, Jiang X. The role of short-chain fatty acids in intestinal barrier function, inflammation, oxidative stress, and colonic carcinogenesis. Pharmacol Res. 2021;165:105420. doi: 10.1016/j.phrs.2021.105420. [DOI] [PubMed] [Google Scholar]
- 45.He J, Zhang P, Shen L, Niu L, Tan Y, Chen L, Zhao Y, Bai L, Hao X, Li X, et al. Short-chain fatty acids and their association with signalling pathways in inflammation, glucose and lipid metabolism. Int J Mol Sci. 2020;21(17):6356. doi: 10.3390/ijms21176356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Aguiar Vallim TQ, Tarling EJ, Edwards PA. Pleiotropic roles of bile acids in metabolism. Cell Metab. 2013;17(5):657–669. doi: 10.1016/j.cmet.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Funabashi M, Grove TL, Wang M, Varma Y, McFadden ME, Brown LC, Guo C, Higginbottom S, Almo SC, Fischbach MA, et al. A metabolic pathway for bile acid dehydroxylation by the gut microbiome. Nature. 2020;582(7813):566–570. doi: 10.1038/s41586-020-2396-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guzior DV, Quinn RA. Review: microbial transformations of human bile acids. Microbiome. 2021;9(1):140. doi: 10.1186/s40168-021-01101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jia X, Lu S, Zeng Z, Liu Q, Dong Z, Chen Y, Zhu Z, Hong Z, Zhang T, Du G, et al. Characterization of gut microbiota, bile acid metabolism, and cytokines in intrahepatic cholangiocarcinoma. Hepatology. 2020;71(3):893–906. doi: 10.1002/hep.30852. [DOI] [PubMed] [Google Scholar]
- 50.Zhang M, Serna-Salas S, Damba T, Borghesan M, Demaria M, Moshage H. Hepatic stellate cell senescence in liver fibrosis: characteristics, mechanisms and perspectives. Mech Ageing Dev. 2021;199:111572. doi: 10.1016/j.mad.2021.111572. [DOI] [PubMed] [Google Scholar]
- 51.Jia W, Xie G, Jia W. Bile acid-microbiota crosstalk in gastrointestinal inflammation and carcinogenesis. Nat Rev Gastroenterol Hepatol. 2018;15(2):111–128. doi: 10.1038/nrgastro.2017.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roager HM, Licht TR. Microbial tryptophan catabolites in health and disease. Nat Commun. 2018;9(1):3294. doi: 10.1038/s41467-018-05470-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peng H, Wang Y, Luo W. Multifaceted role of branched-chain amino acid metabolism in cancer. Oncogene. 2020;39(44):6747–6756. doi: 10.1038/s41388-020-01480-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krautkramer KA, Fan J, Bäckhed F. Gut microbial metabolites as multi-kingdom intermediates. Nat Rev Microbiol. 2021;19(2):77–94. doi: 10.1038/s41579-020-0438-4. [DOI] [PubMed] [Google Scholar]
- 55.Li X, Hong J, Wang Y, Pei M, Wang L, Gong Z. Trimethylamine-N-Oxide Pathway: a Potential Target for the Treatment of MAFLD. Front Mol Biosci. 2021;8:733507. doi: 10.3389/fmolb.2021.733507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brown JM, Hazen SL. Microbial modulation of cardiovascular disease. Nat Rev Microbiol. 2018;16(3):171–181. doi: 10.1038/nrmicro.2017.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dalal N, Jalandra R, Bayal N. Gut microbiota-derived metabolites in CRC progression and causation. J Cancer Res Clin Oncol. 2021;147(11):3141–3155. doi: 10.1007/s00432-021-03729-w. [DOI] [PubMed] [Google Scholar]
- 58.Li XS, Obeid S, Wang Z, Hazen BJ, Li L, Wu Y, Hurd AG, Gu X, Pratt A, Levison BS, et al. Trimethyllysine, a trimethylamine N-oxide precursor, provides near- and long-term prognostic value in patients presenting with acute coronary syndromes. Eur Heart J. 2019;40(32):2700–2709. doi: 10.1093/eurheartj/ehz259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McBurney MI, Davis C, Fraser CM, Schneeman BO, Huttenhower C, Verbeke K, Walter J, Latulippe ME. Establishing what constitutes a healthy human gut microbiome: state of the science, regulatory considerations, and future directions. J Nutr. 2019;149(11):1882–1895. doi: 10.1093/jn/nxz154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Levy M, Kolodziejczyk AA, Thaiss CA, Elinav E. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17(4):219–232. doi: 10.1038/nri.2017.7. [DOI] [PubMed] [Google Scholar]
- 61.Jochum L, Stecher B. Label or concept - what is a pathobiont? Trends Microbiol. 2020;28(10):789–792. doi: 10.1016/j.tim.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 62.Zeng MY, Inohara N, Nunez G. Mechanisms of inflammation-driven bacterial dysbiosis in the gut. Mucosal Immunol. 2017;10(1):18–26. doi: 10.1038/mi.2016.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hiippala K, Jouhten H, Ronkainen A, Hartikainen A, Kainulainen V, Jalanka J, Satokari R. The potential of gut commensals in reinforcing intestinal barrier function and alleviating inflammation. Nutrients. 2018;10(8):988. doi: 10.3390/nu10080988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Khan R, Petersen FC, Shekhar S. Commensal bacteria: an emerging player in defense against respiratory pathogens. Front Immunol. 2019;10:1203. doi: 10.3389/fimmu.2019.01203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carvalho AL, Fonseca S, Miquel-Clopes A, Cross K, Kok K-S, Wegmann U, Gil-Cardoso K, Bentley EG, Al Katy SHM, Coombes JL, et al. Bioengineering commensal bacteria-derived outer membrane vesicles for delivery of biologics to the gastrointestinal and respiratory tract. J Extracell Vesicles. 2019;8(1):1632100. doi: 10.1080/20013078.2019.1632100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mosca A, Leclerc M, Hugot JP. Gut microbiota diversity and human diseases: should we reintroduce key predators in our ecosystem? Front Microbiol. 2016;7:455. doi: 10.3389/fmicb.2016.00455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roswall J, Olsson LM, Kovatcheva-Datchary P, Nilsson S, Tremaroli V, Simon M-C, Kiilerich P, Akrami R, Krämer M, Uhlén M, et al. Developmental trajectory of the healthy human gut microbiota during the first 5 years of life. Cell Host Microbe. 2021;29(5):765–776 e763. doi: 10.1016/j.chom.2021.02.021. [DOI] [PubMed] [Google Scholar]
- 68.Pellicano R, Ianiro G, Fagoonee S, Settanni CR, Gasbarrini A. Review: extragastric diseases and Helicobacter pylori. Helicobacter. 2020;25(Suppl 1):e12741. doi: 10.1111/hel.12741. [DOI] [PubMed] [Google Scholar]
- 69.Ohno H, Satoh-Takayama N. Stomach microbiota, Helicobacter pylori, and group 2 innate lymphoid cells. Exp Mol Med. 2020;52(9):1377–1382. doi: 10.1038/s12276-020-00485-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Iino C, Shimoyama T. Impact of Helicobacter pylori infection on gut microbiota. World J Gastroenterol. 2021;27(37):6224–6230. doi: 10.3748/wjg.v27.i37.6224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Engstrand L, Graham DY. Microbiome and Gastric Cancer. Dig Dis Sci. 2020;65(3):865–873. doi: 10.1007/s10620-020-06101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen CC, Liou JM, Lee YC, Hong TC, El-Omar EM, Wu MS. The interplay between Helicobacter pylori and gastrointestinal microbiota. Gut Microbes. 2021;13(1):1–22. doi: 10.1080/19490976.2021.1909459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wadhwa R, Song S, Lee JS, Yao Y, Wei Q, Ajani JA. Gastric cancer-molecular and clinical dimensions. Nat Rev Clin Oncol. 2013;10(11):643–655. doi: 10.1038/nrclinonc.2013.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Martin-Nuñez GM, Cornejo-Pareja I, Clemente-Postigo M, Tinahones FJ. Gut microbiota: the missing link between helicobacter pylori infection and metabolic disorders? Front Endocrinol (Lausanne). 2021;12(657). doi: 10.3389/fendo.2021.639856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Martinez JE, Kahana DD, Ghuman S, Wilson HP, Wilson J, Kim SCJ, Lagishetty V, Jacobs JP, Sinha-Hikim AP, Friedman TC, et al. unhealthy lifestyle and gut dysbiosis: a better understanding of the effects of poor diet and nicotine on the intestinal microbiome. Front Endocrinol (Lausanne). 2021;12:667066. doi: 10.3389/fendo.2021.667066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gaulke CA, Sharpton TJ. The influence of ethnicity and geography on human gut microbiome composition. Nat Med. 2018;24(10):1495–1496. doi: 10.1038/s41591-018-0210-8. [DOI] [PubMed] [Google Scholar]
- 77.Vasapolli R, Schutte K, Schulz C, Vital M, Schomburg D, Pieper DH, Vilchez-Vargas R, Malfertheiner P. Analysis of transcriptionally active bacteria throughout the gastrointestinal tract of healthy individuals. Gastroenterology. 2019;157(4):1081–1092 e1083. doi: 10.1053/j.gastro.2019.05.068. [DOI] [PubMed] [Google Scholar]
- 78.Bik EM, Eckburg PB, Gill SR. Molecular analysis of the bacterial microbiota in the human stomach. Proc Natl Acad Sci U S A. 2006;103(3):732–737. doi: 10.1073/pnas.0506655103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li XX, Wong GL, To KF, Wong VWS, Lai LH, Chow DKL, Lau JYW, Sung JJY, Ding C. Bacterial microbiota profiling in gastritis without Helicobacter pylori infection or non-steroidal anti-inflammatory drug use. PLoS One. 2009;4(11):e7985. doi: 10.1371/journal.pone.0007985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen X, Zhou X, Liao B, Zhou Y, Cheng L, Ren B. The cross-kingdom interaction between Helicobacter pylori and Candida albicans. PLoS Pathog. 2021;17(5):e1009515–e1009515. doi: 10.1371/journal.ppat.1009515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Noto JM, Zackular JP, Varga MG, Delgado A, Romero-Gallo J, Scholz MB, Piazuelo MB, Skaar EP, Peek RM. Modification of the gastric mucosal microbiota by a strain-specific helicobacter pylori oncoprotein and carcinogenic histologic phenotype. mBio. 2019;10(3). doi: 10.1128/mBio.00955-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang L, Xin Y, Zhou J. Gastric mucosa-associated microbial signatures of early gastric cancer. Front Microbiol. 2020;11:1548. doi: 10.3389/fmicb.2020.01548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Coker OO, Dai Z, Nie Y, Zhao G, Cao L, Nakatsu G, Wu WK, Wong SH, Chen Z, Sung JJY, et al. Mucosal microbiome dysbiosis in gastric carcinogenesis. Gut. 2018;67(6):1024–1032. doi: 10.1136/gutjnl-2017-314281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang L, Zhou J, Xin Y. Bacterial overgrowth and diversification of microbiota in gastric cancer. Eur J Gastroenterol Hepatol. 2016;28(3):261–266. doi: 10.1097/MEG.0000000000000542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Eun CS, Kim BK, Han DS, Kim SY, Kim KM, Choi BY, Song KS, Kim YS, Kim JF. Differences in gastric mucosal microbiota profiling in patients with chronic gastritis, intestinal metaplasia, and gastric cancer using pyrosequencing methods. Helicobacter. 2014;19(6):407–416. doi: 10.1111/hel.12145. [DOI] [PubMed] [Google Scholar]
- 86.Aviles-Jimenez F, Vazquez-Jimenez F, Medrano-Guzman R, Mantilla A, Torres J. Stomach microbiota composition varies between patients with non-atrophic gastritis and patients with intestinal type of gastric cancer. Sci Rep. 2014;4(1):4202. doi: 10.1038/srep04202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ferreira RM, Pereira-Marques J, Pinto-Ribeiro I, Costa JL, Carneiro F, Machado JC, Figueiredo C. Gastric microbial community profiling reveals a dysbiotic cancer-associated microbiota. Gut. 2018;67(2):226–236. doi: 10.1136/gutjnl-2017-314205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dicksved J, Lindberg M, Rosenquist M, Enroth H, Jansson JK, Engstrand L. Molecular characterization of the stomach microbiota in patients with gastric cancer and in controls. J Med Microbiol. 2009;58(Pt 4):509–516. doi: 10.1099/jmm.0.007302-0. [DOI] [PubMed] [Google Scholar]
- 89.Guo Y, Zhang Y, Gerhard M, Gao -J-J, Mejias-Luque R, Zhang L, Vieth M, Ma J-L, Bajbouj M, Suchanek S, et al. Effect of Helicobacter pylori on gastrointestinal microbiota: a population-based study in Linqu, a high-risk area of gastric cancer. Gut. 2020;69(9):1598–1607. doi: 10.1136/gutjnl-2019-319696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yang J, Zhou X, Liu X, Ling Z, Ji F. Role of the gastric microbiome in gastric cancer: from carcinogenesis to treatment. Front Microbiol. 2021;12:641322. doi: 10.3389/fmicb.2021.641322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Navashenaq JG, Shabgah AG, Banach M, Jamialahmadi T, Penson PE, Johnston TP, Sahebkar A. The interaction of Helicobacter pylori with cancer immunomodulatory stromal cells: new insight into gastric cancer pathogenesis. Semin Cancer Biol. 2021. doi: 10.1016/j.semcancer.2021.09.014. [DOI] [PubMed] [Google Scholar]
- 92.Bakhti SZ, Latifi-Navid S. Interplay and cooperation of Helicobacter pylori and gut microbiota in gastric carcinogenesis. BMC Microbiol. 2021;21(1):258. doi: 10.1186/s12866-021-02315-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gao JJ, Zhang Y, Gerhard M, Mejias-Luque R, Zhang L, Vieth M, Ma J-L, Bajbouj M, Suchanek S, Liu W-D, et al. Association between gut microbiota and helicobacter pylori-related gastric lesions in a high-risk population of gastric cancer. Front Cell Infect Microbiol. 2018;8:202. doi: 10.3389/fcimb.2018.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.He C, Peng C, Wang H, Ouyang Y, Zhu Z, Shu X, Zhu Y, Lu N. The eradication of Helicobacter pylori restores rather than disturbs the gastrointestinal microbiota in asymptomatic young adults. Helicobacter. 2019;24(4):e12590. doi: 10.1111/hel.12590. [DOI] [PubMed] [Google Scholar]
- 95.Frost F, Kacprowski T, Ruhlemann M, Bang C, Franke A, Zimmermann K, Nauck M, Völker U, Völzke H, Biffar R, et al. Helicobacter pylori infection associates with fecal microbiota composition and diversity. Sci Rep. 2019;9(1):20100. doi: 10.1038/s41598-019-56631-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lapidot Y, Reshef L, Cohen D, Muhsen K. Helicobacter pylori and the intestinal microbiome among healthy school-age children. Helicobacter. 2021;26(6):e12854. doi: 10.1111/hel.12854. [DOI] [PubMed] [Google Scholar]
- 97.Heimesaat MM, Fischer A, Plickert R, Wiedemann T, Loddenkemper C, Göbel UB, Bereswill S, Rieder G. Helicobacter pylori induced gastric immunopathology is associated with distinct microbiota changes in the large intestines of long-term infected mongolian gerbils. PLOS ONE. 2014;9(6):e100362. doi: 10.1371/journal.pone.0100362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dash NR, Khoder G, Nada AM, Al Bataineh MT. Exploring the impact of Helicobacter pylori on gut microbiome composition. PLoS One. 2019;14(6):e0218274. doi: 10.1371/journal.pone.0218274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen L, Xu W, Lee A, He J, Huang B, Zheng W, Su T, Lai S, Long Y, Chu H, et al. The impact of Helicobacter pylori infection, eradication therapy and probiotic supplementation on gut microenvironment homeostasis: an open-label, randomized clinical trial. EBioMedicine. 2018;35:87–96. doi: 10.1016/j.ebiom.2018.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Iino C, Shimoyama T, Chinda D, Sakuraba H, Fukuda S, Nakaji S. Influence of helicobacter pylori infection and atrophic gastritis on the gut microbiota in a Japanese population. Digestion. 2020;101:422–432. [DOI] [PubMed] [Google Scholar]
- 101.Cornejo-Pareja I, Martin-Nunez GM, Roca-Rodriguez MM. H. pylori eradication treatment alters gut microbiota and GLP-1 secretion in humans. J Clin Med. 2019;8(4). doi: 10.3390/jcm8040451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang D, Li Y, Zhong H, Ding Q, Lin Y, Tang S, Zong Y, Wang Q, Zhang X, Yang H, et al. Alterations in the human gut microbiome associated with helicobacter pylori infection. FEBS Open Bio. 2019;9(9):1552–1560. doi: 10.1002/2211-5463.12694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yang L, Zhang J, Xu J, Wei X, Yang J, Liu Y, Li H, Zhao C, Wang Y, Zhang L, et al. Helicobacter pylori infection aggravates dysbiosis of gut microbiome in children with gastritis. Front Cell Infect Microbiol. 2019;9:375. doi: 10.3389/fcimb.2019.00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhou Y, Ye Z, Lu J, Miao S, Lu X, Sun H, Wu J, Wang Y, Huang Y. Long-term changes in the gut microbiota after 14-day bismuth quadruple therapy in penicillin-allergic children. Helicobacter. 2020;25(5):e12721. doi: 10.1111/hel.12721. [DOI] [PubMed] [Google Scholar]
- 105.Munoz-Ramirez ZY, Pascoe B, Mendez-Tenorio A, Mourkas E, Sandoval-Motta S, Perez-Perez G, Morgan DR, Dominguez RL, Ortiz-Princz D, Cavazza ME, et al. A 500-year tale of co-evolution, adaptation, and virulence: helicobacter pylori in the Americas. ISME J. 2021;15(1):78–92. doi: 10.1038/s41396-020-00758-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, Magris M, Hidalgo G, Baldassano RN, Anokhin AP, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486(7402):222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lopetuso LR, Scaldaferri F, Franceschi F, Gasbarrini A. The gastrointestinal microbiome – functional interference between stomach and intestine. Best Pract Res Clin Gastroenterol. 2014;28(6):995–1002. doi: 10.1016/j.bpg.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 108.Kienesberger S, Cox LM, Livanos A, Zhang X-S, Chung J, Perez-Perez G, Gorkiewicz G, Zechner E, Blaser M. Gastric Helicobacter pylori infection affects local and distant microbial populations and host responses. Cell Rep. 2016;14(6):1395–1407. doi: 10.1016/j.celrep.2016.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Takahashi-Kanemitsu A, Knight CT, Hatakeyama M. Molecular anatomy and pathogenic actions of Helicobacter pylori CagA that underpin gastric carcinogenesis. Cell Mol Immunol. 2020;17(1):50–63. doi: 10.1038/s41423-019-0339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Baj J, Forma A, Sitarz M, Portincasa P, Garruti G, Krasowska D, Maciejewski R. Helicobacter pylori virulence factors-mechanisms of bacterial pathogenicity in the gastric microenvironment. Cells. 2020;10(1):27. doi: 10.3390/cells10010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Huang Y, Ding Y, Xu H, Shen C, Chen X, Li C. Effects of sodium butyrate supplementation on inflammation, gut microbiota, and short-chain fatty acids in Helicobacter pylori-infected mice. Helicobacter. 2021;26(2):e12785. doi: 10.1111/hel.12785. [DOI] [PubMed] [Google Scholar]
- 112.Zhang Z, Tang H, Chen P, Xie H, Tao Y. Demystifying the manipulation of host immunity, metabolism, and extraintestinal tumors by the gut microbiome. Signal Transduct Target Ther. 2019;4:41. doi: 10.1038/s41392-019-0074-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wibowo H, Harbuwono DS, Tahapary DL, Kartika R, Pradipta S, Larasati RA. Impact of sodium butyrate treatment in LPS-stimulated peripheral blood mononuclear cells of poorly controlled type 2 DM. Front Endocrinol (Lausanne). 2021;12:652942. doi: 10.3389/fendo.2021.652942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Campos-Perez W, Martinez-Lopez E. Effects of short chain fatty acids on metabolic and inflammatory processes in human health. Biochimica Et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2021;1866(5):158900. doi: 10.1016/j.bbalip.2021.158900. [DOI] [PubMed] [Google Scholar]
- 115.Postler TS, Ghosh S. Understanding the Holobiont: how Microbial Metabolites Affect Human Health and Shape the Immune System. Cell Metab. 2017;26(1):110–130. doi: 10.1016/j.cmet.2017.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sit WY, Chen YA, Chen YL, Lai CH, Wang WC. Cellular evasion strategies of Helicobacter pylori in regulating its intracellular fate. Semin Cell Dev Biol. 2020;101:59–67. doi: 10.1016/j.semcdb.2020.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cuomo P, Papaianni M, Sansone C, Iannelli A, Iannelli D, Medaglia C, Paris D, Motta A, Capparelli R. an in vitro model to investigate the role of helicobacter pylori in type 2 diabetes, obesity, alzheimer’s disease and cardiometabolic disease. Int J Mol Sci. 2020;21(21):8369. doi: 10.3390/ijms21218369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Farhangi MA, Vajdi M. Novel findings of the association between gut microbiota-derived metabolite trimethylamine N-oxide and inflammation: results from a systematic review and dose-response meta-analysis. Crit Rev Food Sci Nutr. 2020;60(16):2801–2823. doi: 10.1080/10408398.2020.1770199. [DOI] [PubMed] [Google Scholar]
- 119.Wu D, Cao M, Peng J, Li N, Yi S, Song L, Wang X, Zhang M, Zhao J. The effect of trimethylamine N-oxide on Helicobacter pylori-induced changes of immunoinflammatory genes expression in gastric epithelial cells. Int Immunopharmacol. 2017;43:172–178. doi: 10.1016/j.intimp.2016.11.032. [DOI] [PubMed] [Google Scholar]
- 120.Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375(24):2369–2379. doi: 10.1056/NEJMra1600266. [DOI] [PubMed] [Google Scholar]
- 121.Fan Y, Pedersen O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. 2021;19(1):55–71. doi: 10.1038/s41579-020-0433-9. [DOI] [PubMed] [Google Scholar]
- 122.Ramirez J, Guarner F, Bustos Fernandez L, Maruy A, Sdepanian VL, Cohen H. Antibiotics as major disruptors of gut microbiota. Front Cell Infect Microbiol. 2020;10(731). doi: 10.3389/fcimb.2020.572912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Blaser MJ. Antibiotic use and its consequences for the normal microbiome. Science. 2016;352(6285):544–545. doi: 10.1126/science.aad9358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Palleja A, Mikkelsen KH, Forslund SK, Kashani A, Allin KH, Nielsen T, Hansen TH, Liang S, Feng Q, Zhang C, et al. Recovery of gut microbiota of healthy adults following antibiotic exposure. Nat Microbiol. 2018;3(11):1255–1265. doi: 10.1038/s41564-018-0257-9. [DOI] [PubMed] [Google Scholar]
- 125.Zarrinpar A, Chaix A, Xu ZZ, Chang MW, Marotz CA, Saghatelian A, Knight R, Panda S. Antibiotic-induced microbiome depletion alters metabolic homeostasis by affecting gut signaling and colonic metabolism. Nat Commun. 2018;9(1):2872. doi: 10.1038/s41467-018-05336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Maier L, Pruteanu M, Kuhn M, Zeller G, Telzerow A, Anderson EE, Brochado AR, Fernandez KC, Dose H, Mori H, et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature. 2018;555(7698):623–628. doi: 10.1038/nature25979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rashidi A, Ebadi M, Rehman TU, Elhusseini H, Nalluri H, Kaiser T, Holtan SG, Khoruts A, Weisdorf DJ, Staley C, et al. Gut microbiota response to antibiotics is personalized and depends on baseline microbiota. Microbiome. 2021;9(1):211. doi: 10.1186/s40168-021-01170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Salminen S, Collado MC, Endo A, Hill C, Lebeer S, Quigley EMM, Sanders ME, Shamir R, Swann JR, Szajewska H, et al. The international scientific association of probiotics and prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat Rev Gastroenterol Hepatol. 2021;18(9):649–667. doi: 10.1038/s41575-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Veiga P, Suez J, Derrien M, Elinav E. Moving from probiotics to precision probiotics. Nat Microbiol. 2020;5(7):878–880. doi: 10.1038/s41564-020-0721-1. [DOI] [PubMed] [Google Scholar]
- 130.Gao J, Li X, Zhang G, Sadiq FA, Simal‐Gandara J, Xiao J, Sang Y. Probiotics in the dairy industry-advances and opportunities. Compr Rev Food Sci Food Saf. 2021;20(4):3937–3982. doi: 10.1111/1541-4337.12755. [DOI] [PubMed] [Google Scholar]
- 131.Suez J, Zmora N, Segal E, Elinav E. The pros, cons, and many unknowns of probiotics. Nat Med. 2019;25(5):716–729. doi: 10.1038/s41591-019-0439-x. [DOI] [PubMed] [Google Scholar]
- 132.Wieërs G, Belkhir L, Enaud R, Leclercq S, Philippart de Foy J-M, Dequenne I, de Timary P, Cani PD. How probiotics affect the microbiota. Front Cell Infect Microbiol. 2020;9(454). doi: 10.3389/fcimb.2019.00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hou Q, Zhao F, Liu W, Lv R, Khine WWT, Han J, Sun Z, Lee Y-K, Zhang H. Probiotic-directed modulation of gut microbiota is basal microbiome dependent. Gut Microbes. 2020;12(1):1736974. doi: 10.1080/19490976.2020.1736974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Singh TP, Natraj BH. Next-generation probiotics: a promising approach towards designing personalized medicine. Crit Rev Microbiol. 2021;47(4):479–498. doi: 10.1080/1040841X.2021.1902940. [DOI] [PubMed] [Google Scholar]
- 135.Zhai Q, Feng S, Arjan N, Chen W. A next generation probiotic, Akkermansia muciniphila. Crit Rev Food Sci Nutr. 2019;59(19):3227–3236. doi: 10.1080/10408398.2018.1517725. [DOI] [PubMed] [Google Scholar]
- 136.Keshavarz Azizi Raftar S, Abdollahiyan S, Azimirad M, Yadegar A, Vaziri F, Moshiri A, Siadat SD, Zali MR. The anti-fibrotic effects of heat-killed akkermansia muciniphila muct on liver fibrosis markers and activation of hepatic stellate cells. Probiotics Antimicrob Proteins. 2021;13(3):776–787. doi: 10.1007/s12602-020-09733-9. [DOI] [PubMed] [Google Scholar]
- 137.Depommier C, Everard A, Druart C, Plovier H, Van Hul M, Vieira-Silva S, Falony G, Raes J, Maiter D, Delzenne NM, et al. Supplementation with akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nat Med. 2019;25(7):1096–1103. doi: 10.1038/s41591-019-0495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.De Palma G, Nadal I, Medina M, Donat E, Ribes-Koninckx C, Calabuig M, Sanz Y. Intestinal dysbiosis and reduced immunoglobulin-coated bacteria associated with coeliac disease in children. BMC Microbiol. 2010;10(1):63. doi: 10.1186/1471-2180-10-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Rajilic-Stojanovic M, Biagi E, Heilig HG, Kajander K, Kekkonen RA, Tims S, de Vos WM. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology. 2011;141(5):1792–1801. doi: 10.1053/j.gastro.2011.07.043. [DOI] [PubMed] [Google Scholar]
- 140.Balamurugan R, Rajendiran E, George S, Samuel GV, Ramakrishna BS. Real-time polymerase chain reaction quantification of specific butyrate-producing bacteria, desulfovibrio and Enterococcus faecalis in the feces of patients with colorectal cancer. J Gastroenterol Hepatol. 2008;23(8 Pt 1):1298–1303. doi: 10.1111/j.1440-1746.2008.05490.x. [DOI] [PubMed] [Google Scholar]
- 141.Furet J-P, Kong L-C, Tap J, Poitou C, Basdevant A, Bouillot J-L, Mariat D, Corthier G, Doré J, Henegar C, et al. Differential adaptation of human gut microbiota to bariatric surgery–induced weight loss. Diabetes. 2010;59(12):3049–3057. doi: 10.2337/db10-0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Martin R, Miquel S, Benevides L, Bridonneau C, Robert V, Hudault S, Chain F, Berteau O, Azevedo V, Chatel JM, et al. Functional characterization of novel faecalibacterium prausnitzii strains isolated from healthy volunteers: a step forward in the use of F. prausnitzii as a next-generation probiotic. Front Microbiol. 2017;8:1226. doi: 10.3389/fmicb.2017.01226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fei Y, Chen Z, Han S, Zhang S, Zhang T, Lu Y, Berglund B, Xiao H, Li L, Yao M, et al. Role of prebiotics in enhancing the function of next-generation probiotics in gut microbiota. Crit Rev Food Sci Nutr. pp.1–18. 2021. doi: 10.1080/10408398.2021.1958744 [DOI] [PubMed] [Google Scholar]
- 144.Min S, Kim S, Cho SW. Gastrointestinal tract modeling using organoids engineered with cellular and microbiota niches. Exp Mol Med. 2020;52(2):227–237. doi: 10.1038/s12276-020-0386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shah SC, Iyer PG, Moss SF. AGA clinical practice update on the management of refractory Helicobacter pylori infection: expert review. Gastroenterology. 2021;160(5):1831–1841. doi: 10.1053/j.gastro.2020.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Fallone CA, Chiba N, van Zanten SV, Fischbach L, Gisbert JP, Hunt RH, Jones NL, Render C, Leontiadis GI, Moayyedi P, et al. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology. 2016;151(1):51–69.e14. doi: 10.1053/j.gastro.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 147.Liou JM, Chen CC, Chang CM, Fang Y-J, Bair M-J, Chen P-Y, Chang C-Y, Hsu Y-C, Chen M-J, Chen -C-C, et al. Long-term changes of gut microbiota, antibiotic resistance, and metabolic parameters after Helicobacter pylori eradication: a multicentre, open-label, randomised trial. Lancet Infect Dis. 2019;19(10):1109–1120. doi: 10.1016/S1473-3099(19)30272-5. [DOI] [PubMed] [Google Scholar]
- 148.Ford AC, Yuan Y, Moayyedi P. Helicobacter pylori eradication therapy to prevent gastric cancer: systematic review and meta-analysis. Gut. 2020;69(12):2113–2121. doi: 10.1136/gutjnl-2020-320839. [DOI] [PubMed] [Google Scholar]
- 149.Tshibangu-Kabamba E, Yamaoka Y. Helicobacter pylori infection and antibiotic resistance - from biology to clinical implications. Nat Rev Gastroenterol Hepatol. 2021;18(9):613–629. doi: 10.1038/s41575-021-00449-x. [DOI] [PubMed] [Google Scholar]
- 150.Cheung KS, Chan EW, Wong AYS, Chen L, Wong ICK, Leung WK. Long-term proton pump inhibitors and risk of gastric cancer development after treatment for Helicobacter pylori: a population-based study. Gut. 2018;67(1):28–35. doi: 10.1136/gutjnl-2017-314605. [DOI] [PubMed] [Google Scholar]
- 151.Yuan J, He Q, Nguyen LH, Wong MCS, Huang J, Yu Y, Xia B, Tang Y, He Y, Zhang C, et al. Regular use of proton pump inhibitors and risk of type 2 diabetes: results from three prospective cohort studies. Gut. 2021;70(6):1070–1077. doi: 10.1136/gutjnl-2020-322557. [DOI] [PubMed] [Google Scholar]
- 152.Ye Q, Shao X, Shen R, Chen D, Shen J. Changes in the human gut microbiota composition caused by Helicobacter pylori eradication therapy: a systematic review and meta-analysis. Helicobacter. 2020;25(4):e12713. doi: 10.1111/hel.12713. [DOI] [PubMed] [Google Scholar]
- 153.Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. BMJ. 2018;361:k2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Handa O, Naito Y, Osawa M. Nutrients and probiotics: current trends in their use to eradicate Helicobacter pylori. J Clin Biochem Nutr. 2020;67(1):26–28. doi: 10.3164/jcbn.20-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Montassier E, Valdes-Mas R, Batard E. Probiotics impact the antibiotic resistance gene reservoir along the human GI tract in a person-specific and antibiotic-dependent manner. Nat Microbiol. 2021;6(8):1043–1054. doi: 10.1038/s41564-021-00920-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cifuentes SG, Prado MB, Fornasini M, Cohen H, Baldeon ME, Cardenas PA. Saccharomyces boulardii CNCM I-745 supplementation modifies the fecal resistome during Helicobacter pylori eradication therapy. Helicobacter. 2022;27(2):e12870. doi: 10.1111/hel.12870. [DOI] [PubMed] [Google Scholar]
- 157.Zhang M, Zhang C, Zhao J, Zhang H, Zhai Q, Chen W. Meta-analysis of the efficacy of probiotic-supplemented therapy on the eradication of H. pylori and incidence of therapy-associated side effects. Microb Pathog. 2020;147:104403. doi: 10.1016/j.micpath.2020.104403. [DOI] [PubMed] [Google Scholar]
- 158.Losurdo G, Cubisino R, Barone M, Principi M, Leandro G, Ierardi E, Leo AD. Probiotic monotherapy and Helicobacter pylori eradication: a systematic review with pooled-data analysis. World J Gastroenterol. 2018;24(1):139–149. doi: 10.3748/wjg.v24.i1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kori M, Daugule I, Urbonas V. Helicobacter pylori and some aspects of gut microbiota in children. Helicobacter. 2018;23(Suppl 1):e12524. doi: 10.1111/hel.12524. [DOI] [PubMed] [Google Scholar]
- 160.Feng JR, Wang F, Qiu X, McFarland LV, Chen P-F, Zhou R, Liu J, Zhao Q, Li J. Efficacy and safety of probiotic-supplemented triple therapy for eradication of Helicobacter pylori in children: a systematic review and network meta-analysis. Eur J Clin Pharmacol. 2017;73(10):1199–1208. doi: 10.1007/s00228-017-2291-6. [DOI] [PubMed] [Google Scholar]
- 161.Kamiya S, Yonezawa H, Osaki T. Role of probiotics in eradication therapy for Helicobacter pylori infection. Adv Exp Med Biol. 2019;1149:243–255. [DOI] [PubMed] [Google Scholar]
- 162.Fang HR, Zhang GQ, Cheng JY, Li ZY. Efficacy of lactobacillus-supplemented triple therapy for Helicobacter pylori infection in children: a meta-analysis of randomized controlled trials. Eur J Pediatr. 2019;178(1):7–16. doi: 10.1007/s00431-018-3282-z. [DOI] [PubMed] [Google Scholar]
- 163.McElrath C, Espinosa V, Lin JD. Critical role of interferons in gastrointestinal injury repair. Nat Commun. 2021;12(1):2624. doi: 10.1038/s41467-021-22928-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.George S, Lucero Y, Torres JP, Lagomarcino AJ, O’Ryan M. Gastric damage and cancer-associated biomarkers in Helicobacter pylori-infected children. Front Microbiol. 2020;11(90). doi: 10.3389/fmicb.2020.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Paone P, Cani PD. Mucus barrier, mucins and gut microbiota: the expected slimy partners? Gut. 2020;69(12):2232–2243. doi: 10.1136/gutjnl-2020-322260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Ghosh S, Whitley CS, Haribabu B, Jala VR. Regulation of intestinal barrier function by microbial metabolites. Cell Mol Gastroenterol Hepatol. 2021;11(5):1463–1482. doi: 10.1016/j.jcmgh.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Qureshi N, Li P, Gu Q. Probiotic therapy in Helicobacter pylori infection: a potential strategy against a serious pathogen? Appl Microbiol Biotechnol. 2019;103(4):1573–1588. doi: 10.1007/s00253-018-09580-3. [DOI] [PubMed] [Google Scholar]
- 168.Azimirad M, Krutova M, Yadegar A, Shahrokh S, Olfatifar M, Aghdaei HA, Fawley WN, Wilcox MH, Zali MR. Clostridioides difficile ribotypes 001 and 126 were predominant in Tehran healthcare settings from 2004 to 2018: a 14-year-long cross-sectional study. Emerg Microbes Infect. 2020;9(1):1432–1443. doi: 10.1080/22221751.2020.1780949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Cristofori F, Dargenio VN, Dargenio C, Miniello VL, Barone M, Francavilla R. Anti-inflammatory and immunomodulatory effects of probiotics in gut inflammation: a door to the body. Front Immunol. 2021;12:578386. doi: 10.3389/fimmu.2021.578386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Marques MS, Costa AC, Osório H, Pinto ML, Relvas S, Dinis-Ribeiro M, Carneiro F, Leite M, Figueiredo C. Helicobacter pylori PqqE is a new virulence factor that cleaves junctional adhesion molecule A and disrupts gastric epithelial integrity. Gut Microbes. 2021;13(1):1921928. doi: 10.1080/19490976.2021.1921928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Rose EC, Odle J, Blikslager AT, Ziegler AL. Probiotics, prebiotics and epithelial tight junctions: a promising approach to modulate intestinal barrier function. Int J Mol Sci. 2021;22(13):6729. doi: 10.3390/ijms22136729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Llewellyn A, Foey A. Probiotic Modulation of Innate Cell Pathogen Sensing and Signaling Events. Nutrients. 2017;9(10):1156. doi: 10.3390/nu9101156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ji J, Yang H. Using probiotics as supplementation for helicobacter pylori antibiotic therapy. Int J Mol Sci. 2020;21(3):1136. doi: 10.3390/ijms21031136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Feng T, Wang J. Oxidative stress tolerance and antioxidant capacity of lactic acid bacteria as probiotic: a systematic review. Gut Microbes. 2020;12(1):1801944. doi: 10.1080/19490976.2020.1801944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.van Zyl WF, Deane SM, Dicks LMT. Molecular insights into probiotic mechanisms of action employed against intestinal pathogenic bacteria. Gut Microbes. 2020;12(1):1831339. doi: 10.1080/19490976.2020.1831339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sanders ME, Merenstein DJ, Reid G, Gibson GR, Rastall RA. Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nat Rev Gastroenterol Hepatol. 2019;16(10):605–616. doi: 10.1038/s41575-019-0173-3. [DOI] [PubMed] [Google Scholar]
- 177.van Baarlen P, Troost FJ, van Hemert S, van der Meer C, de Vos WM, de Groot PJ, Hooiveld GJEJ, Brummer RJM, Kleerebezem M. Differential NF-κB pathways induction by Lactobacillus plantarum in the duodenum of healthy humans correlating with immune tolerance. Proc Natl Acad Sci U S A. 2009;106(7):2371–2376. doi: 10.1073/pnas.0809919106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Fong W, Li Q, Yu J. Gut microbiota modulation: a novel strategy for prevention and treatment of colorectal cancer. Oncogene. 2020;39(26):4925–4943. doi: 10.1038/s41388-020-1341-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Hrdý J, Alard J, Couturier-Maillard A, Boulard O, Boutillier D, Delacre M, Lapadatescu C, Cesaro A, Blanc P, Pot B, et al. Lactobacillus reuteri 5454 and Bifidobacterium animalis ssp. lactis 5764 improve colitis while differentially impacting dendritic cells maturation and antimicrobial responses. Sci Rep. 2020;10(1):5345. doi: 10.1038/s41598-020-62161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Lu K, Dong S, Wu X, Jin R, Chen H. Probiotics in Cancer. Front Oncol. 2021;11:638148. doi: 10.3389/fonc.2021.638148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Tezuka H, Ohteki T. Regulation of IgA Production by Intestinal Dendritic Cells and Related Cells. Front Immunol. 2019;10:1891. doi: 10.3389/fimmu.2019.01891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Eslami M, Yousefi B, Kokhaei P, Jazayeri Moghadas A, Sadighi Moghadam B, Arabkari V, Niazi Z. Are probiotics useful for therapy of Helicobacter pylori diseases? Comp Immunol Microbiol Infect Dis. 2019;64:99–108. doi: 10.1016/j.cimid.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 183.Motta JP, Wallace JL, Buret AG, Deraison C, Vergnolle N. Gastrointestinal biofilms in health and disease. Nat Rev Gastroenterol Hepatol. 2021;18(5):314–334. doi: 10.1038/s41575-020-00397-y. [DOI] [PubMed] [Google Scholar]
- 184.Oh B, Kim BS, Kim JW, Kim JS, Koh S-J, Kim BG, Lee KL, Chun J. The effect of probiotics on gut microbiota during the Helicobacter pylori eradication: randomized controlled trial. Helicobacter. 2016;21(3):165–174. doi: 10.1111/hel.12270. [DOI] [PubMed] [Google Scholar]
- 185.Oh B, Kim JW, Kim BS. Changes in the functional potential of the gut microbiome following probiotic supplementation during Helicobacter Pylori treatment. Helicobacter. 2016;21:493–503. [DOI] [PubMed] [Google Scholar]
- 186.Wu L, Wang Z, Sun G. Effects of anti-H. pylori triple therapy and a probiotic complex on intestinal microbiota in duodenal ulcer. Sci Rep. 2019;9(1):12874. doi: 10.1038/s41598-019-49415-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Cárdenas PA, Garcés D, Prado-Vivar B, Flores N, Fornasini M, Cohen H, Salvador I, Cargua O, Baldeón ME. Effect of Saccharomyces boulardii CNCM I-745 as complementary treatment of Helicobacter pylori infection on gut microbiome. Eur J Clin Microbiol Infect Dis. 2020;39(7):1365–1372. doi: 10.1007/s10096-020-03854-3. [DOI] [PubMed] [Google Scholar]
- 188.Kakiuchi T, Mizoe A, Yamamoto K, Imamura I, Hashiguchi K, Kawakubo H, Yamaguchi D, Fujioka Y, Nakayama A, Okuda M, et al. Effect of probiotics during vonoprazan-containing triple therapy on gut microbiota in Helicobacter pylori infection: a randomized controlled trial. Helicobacter. 2020;25(3):e12690. doi: 10.1111/hel.12690. [DOI] [PubMed] [Google Scholar]
- 189.Tang B, Tang L, Huang C, Tian C, Chen L, He Z, Yang G, Zuo L, Zhao G, Liu E, et al. The effect of probiotics supplementation on gut microbiota after Helicobacter pylori eradication: a multicenter randomized controlled trial. Infect Dis Ther. 2021;10(1):317–333. doi: 10.1007/s40121-020-00372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Guillemard E, Poirel M, Schäfer F, Quinquis L, Rossoni C, Keicher C, Wagner F, Szajewska H, Barbut F, Derrien M, et al. A randomised, controlled trial: effect of a multi-strain fermented milk on the gut microbiota recovery after helicobacter pylori therapy. Nutrients. 2021;13(9):3171. doi: 10.3390/nu13093171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Yang C, Liang L, Lv P, Liu L, Wang S, Wang Z, Chen Y. Effects of non-viable Lactobacillus reuteri combining with 14-day standard triple therapy on Helicobacter pylori eradication: a randomized double-blind placebo-controlled trial. Helicobacter. 2021;26(6):e12856. doi: 10.1111/hel.12856. [DOI] [PubMed] [Google Scholar]
- 192.Yuan Z, Xiao S, Li S, Suo B, Wang Y, Meng L, Liu Z, Yin Z, Xue Y, Zhou L, et al. The impact of Helicobacter pylori infection, eradication therapy, and probiotics intervention on gastric microbiota in young adults. Helicobacter. 2021;26(6):e12848. doi: 10.1111/hel.12848. [DOI] [PubMed] [Google Scholar]
- 193.Stoeva MK, Garcia-So J, Justice N, Myers J, Tyagi S, Nemchek M, McMurdie PJ, Kolterman O, Eid J. Butyrate-producing human gut symbiont, Clostridium butyricum, and its role in health and disease. Gut Microbes. 2021;13(1):1–28. doi: 10.1080/19490976.2021.1907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ariyoshi T, Hagihara M, Tomono S, Eguchi S, Minemura A, Miura D, Oka K, Takahashi M, Yamagishi Y, Mikamo H, et al. Clostridium butyricum MIYAIRI 588 modifies bacterial composition under antibiotic-induced dysbiosis for the activation of interactions via lipid metabolism between the gut microbiome and the host. Biomedicines. 2021;9(8):1065. doi: 10.3390/biomedicines9081065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Wang Y, Huang JM, Zhou YL, Almeida A, Finn RD, Danchin A, He L-S. Phylogenomics of expanding uncultured environmental Tenericutes provides insights into their pathogenicity and evolutionary relationship with Bacilli. BMC Genomics. 2020;21(1):408. doi: 10.1186/s12864-020-06807-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Yuan X, Chen R, McCormick KL, Zhang Y, Lin X, Yang X. The role of the gut microbiota on the metabolic status of obese children. Microb Cell Fact. 2021;20(1):53. doi: 10.1186/s12934-021-01548-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Yeoh YK, Chen Z, Wong MCS, Hui M, Yu J, Ng SC, Sung JJY, Chan FKL, Chan PKS. Southern Chinese populations harbour non-nucleatum Fusobacteria possessing homologues of the colorectal cancer-associated FadA virulence factor. Gut. 2020;69(11):1998–2007. doi: 10.1136/gutjnl-2019-319635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Harrandah AM, Chukkapalli SS, Bhattacharyya I, Progulske-Fox A, Chan EKL. Fusobacteria modulate oral carcinogenesis and promote cancer progression. J Oral Microbiol. 2020;13:1849493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Harding CM, Hennon SW, Feldman MF. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat Rev Microbiol. 2018;16(2):91–102. doi: 10.1038/nrmicro.2017.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Song WY, Kim HJ. Current biochemical understanding regarding the metabolism of acinetobactin, the major siderophore of the human pathogen Acinetobacter baumannii, and outlook for discovery of novel anti-infectious agents based thereon. Nat Prod Rep. 2020;37(4):477–487. doi: 10.1039/C9NP00046A. [DOI] [PubMed] [Google Scholar]
- 201.Zhao X, Zhong X, Liu X, Wang X, Gao X. Therapeutic and improving function of lactobacilli in the prevention and treatment of cardiovascular-related diseases: a novel perspective from gut microbiota. Frontiers in Nutrition. 2021;8(299). doi: 10.3389/fnut.2021.693412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Hanchi H, Mottawea W, Sebei K, Hammami R. The genus enterococcus: between probiotic potential and safety concerns—an update. Front Microbiol. 2018;9(1791). doi: 10.3389/fmicb.2018.01791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Liu X, Mao B, Gu J, Wu J, Cui S, Wang G, Zhao J, Zhang H, Chen W. Blautia —a new functional genus with potential probiotic properties? Gut Microbes. 2021;13(1):1–21. doi: 10.1080/19490976.2021.1875796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Xiang H, Gan J, Zeng D, Li J, Yu H, Zhao H, Yang Y, Tan S, Li G, Luo C, et al. Specific microbial taxa and functional capacity contribute to chicken abdominal fat deposition. Front Microbiol. 2021;12:643025. doi: 10.3389/fmicb.2021.643025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Goris T, Cuadrat RRC, Braune A. Flavonoid-modifying capabilities of the human gut microbiome-an in silico study. Nutrients. 2021;13(8):2688. doi: 10.3390/nu13082688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Engevik MA, Danhof HA, Ruan W, Engevik AC, Chang-Graham AL, Engevik KA, Shi Z, Zhao Y, Brand CK, Krystofiak ES, et al. Fusobacterium nucleatum Secretes outer membrane vesicles and promotes intestinal inflammation. mBio. 2021;12(2). doi: 10.1128/mBio.02706-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ranjbar M, Salehi R, Haghjooy Javanmard S, Rafiee L, Faraji H, Jafarpor S, Ferns GA, Ghayour-Mobarhan M, Manian M, Nedaeinia R, et al. The dysbiosis signature of fusobacterium nucleatum in colorectal cancer-cause or consequences? A systematic review. Cancer Cell Int. 2021;21(1):194. doi: 10.1186/s12935-021-01886-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Murros KE, Huynh VA, Takala TM, Saris PEJ. Desulfovibrio bacteria are associated with parkinson’s disease. Front Cell Infect Microbiol. 2021;11:652617. doi: 10.3389/fcimb.2021.652617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Rosario D, Bidkhori G, Lee S, Bedarf J, Hildebrand F, Le Chatelier E, Uhlen M, Ehrlich SD, Proctor G, Wüllner U, et al. Systematic analysis of gut microbiome reveals the role of bacterial folate and homocysteine metabolism in Parkinson’s disease. Cell Rep. 2021;34(9):108807. doi: 10.1016/j.celrep.2021.108807. [DOI] [PubMed] [Google Scholar]
- 210.Shao J, Li Z, Gao Y, Zhao K, Lin M, Li Y, Wang S, Liu Y, Chen L. Construction of a “Bacteria-Metabolites” co-expression network to clarify the anti-ulcerative colitis effect of flavonoids of sophora flavescens aiton by regulating the “Host-Microbe” interaction. Front Pharmacol. 2021;12:710052. doi: 10.3389/fphar.2021.710052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Caulier S, Nannan C, Gillis A, Licciardi F, Bragard C, Mahillon J. Overview of the antimicrobial compounds produced by members of the Bacillus subtilis group. Front Microbiol. 2019;10:302. doi: 10.3389/fmicb.2019.00302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Martin RM, Bachman MA. Colonization, infection, and the accessory genome of Klebsiella pneumoniae. Front Cell Infect Microbiol. 2018;8:4. doi: 10.3389/fcimb.2018.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Dong S, Jiao J, Jia S, Li G, Zhang W, Yang K, Wang Z, Liu C, Li D, Wang X, et al. 16S rDNA full-length assembly sequencing technology analysis of intestinal microbiome in polycystic ovary syndrome. Front Cell Infect Microbiol. 2021;11:634981. doi: 10.3389/fcimb.2021.634981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Yu X, Åvall-Jääskeläinen S, Koort J, Lindholm A, Rintahaka J, von Ossowski I, Palva A, Hynönen U. A comparative characterization of different host-sourced lactobacillus ruminis strains and their adhesive, inhibitory, and immunomodulating functions. Front Microbiol. 2017;8(657). doi: 10.3389/fmicb.2017.00657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Yang J, Li Y, Wen Z, Liu W, Meng L, Huang H. Oscillospira - a candidate for the next-generation probiotics. Gut Microbes. 2021;13(1):1987783. doi: 10.1080/19490976.2021.1987783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Bartley A, Yang T, Arocha R, Malphurs WL, Larkin R, Magee KL, Vickroy TW, Zubcevic J. Increased abundance of lactobacillales in the colon of beta-adrenergic receptor knock out mouse is associated with increased gut bacterial production of short chain fatty acids and reduced IL17 expression in circulating CD4+ immune cells. Front Physiol. 2018;9(1593). doi: 10.3389/fphys.2018.01593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Chen Z, Xie Y, Zhou F, Zhang B, Wu J, Yang L, Xu S, Stedtfeld R, Chen Q, Liu J, et al. Featured Gut Microbiomes Associated With the Progression of Chronic Hepatitis B Disease. Front Microbiol. 2020;11:383. doi: 10.3389/fmicb.2020.00383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Zhou Y, Chen C, Yu H, Yang Z. Fecal microbiota changes in patients with postpartum depressive disorder. Front Cell Infect Microbiol. 2020;10:567268. doi: 10.3389/fcimb.2020.567268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Nagao-Kitamoto H, Leslie JL, Kitamoto S, Jin C, Thomsson KA, Gillilland MG, Kuffa P, Goto Y, Jenq RR, Ishii C, et al. Interleukin-22-mediated host glycosylation prevents clostridioides difficile infection by modulating the metabolic activity of the gut microbiota. Nat Med. 2020;26(4):608–617. doi: 10.1038/s41591-020-0764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Tito RY, Cypers H, Joossens M, Varkas G, Van Praet L, Glorieus E, Van den Bosch F, De Vos M, Raes J, Elewaut D, et al. Brief report: dialister as a microbial marker of disease activity in spondyloarthritis. Arthritis & Rheumatology. 2017;69(1):114–121. doi: 10.1002/art.39802. [DOI] [PubMed] [Google Scholar]
- 221.Kaakoush NO. Sutterella species, iga-degrading bacteria in ulcerative colitis. Trends Microbiol. 2020;28(7):519–522. doi: 10.1016/j.tim.2020.02.018. [DOI] [PubMed] [Google Scholar]
- 222.Astbury S, Atallah E, Vijay A, Aithal GP, Grove JI, Valdes AM. Lower gut microbiome diversity and higher abundance of proinflammatory genus Collinsella are associated with biopsy-proven nonalcoholic steatohepatitis. Gut Microbes. 2020;11(3):569–580. doi: 10.1080/19490976.2019.1681861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Bailen M, Bressa C, Martinez-Lopez S, González-Soltero R, Montalvo Lominchar MG, San Juan C, Larrosa M. Microbiota features associated with a high-fat/low-fiber diet in healthy adults. Front Nutr. 2020;7:583608. doi: 10.3389/fnut.2020.583608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Zhang X, Coker OO, Chu ES, Fu K, Lau HCH, Wang Y-X, Chan AWH, Wei H, Yang X, Sung JJY, et al. Dietary cholesterol drives fatty liver-associated liver cancer by modulating gut microbiota and metabolites. Gut. 2021;70(4):761–774. doi: 10.1136/gutjnl-2019-319664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Yuan C, Yin Z, Wang J, Qian C, Wei Y, Zhang S, Jiang L, Liu B. Comparative genomic analysis of citrobacter and key genes essential for the pathogenicity of Citrobacter koseri. Front Microbiol. 2019;10:2774. doi: 10.3389/fmicb.2019.02774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ma X, Ma L, Wang Z, Liu Y, Long L, Ma X, Chen H, Chen Z, Lin X, Si L, et al. Clinical features and gut microbial alterations in anti-leucine-rich glioma-inactivated 1 encephalitis-a pilot study. Front Neurol. 2020;11:585977. doi: 10.3389/fneur.2020.585977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Cerqueira FM, Photenhauer AL, Pollet RM, Brown HA, Koropatkin NM. Starch Digestion by Gut Bacteria: crowdsourcing for Carbs. Trends Microbiol. 2020;28(2):95–108. doi: 10.1016/j.tim.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 228.Gurung M, Li Z, You H, Rodrigues R, Jump DB, Morgun A, Shulzhenko N. Role of gut microbiota in type 2 diabetes pathophysiology. EBioMedicine. 2020;51:102590. doi: 10.1016/j.ebiom.2019.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Schirmer M, Garner A, Vlamakis H, Xavier RJ. Microbial genes and pathways in inflammatory bowel disease. Nat Rev Microbiol. 2019;17(8):497–511. doi: 10.1038/s41579-019-0213-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Lordan C, Thapa D, Ross RP, Cotter PD. Potential for enriching next-generation health-promoting gut bacteria through prebiotics and other dietary components. Gut Microbes. 2020;11(1):1–20. doi: 10.1080/19490976.2019.1613124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Tomova A, Bukovsky I, Rembert E, Yonas W, Alwarith J, Barnard ND, Kahleova H. The effects of vegetarian and vegan diets on gut microbiota. Front Nutr. 2019;6:47. doi: 10.3389/fnut.2019.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Shimokawa C, Kato T, Takeuchi T, Ohshima N, Furuki T, Ohtsu Y, Suzue K, Imai T, Obi S, Olia A, et al. CD8(+) regulatory T cells are critical in prevention of autoimmune-mediated diabetes. Nat Commun. 2020;11(1):1922. doi: 10.1038/s41467-020-15857-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Carey MA, Medlock GL, Alam M, Kabir M, Uddin MJ, Nayak U, Papin J, Faruque ASG, Haque R, Petri WA, et al. Megasphaera in the stool microbiota is negatively associated with diarrheal cryptosporidiosis. Clin Infect Dis. 2021;73(6):e1242–e1251. doi: 10.1093/cid/ciab207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Liu F, Li J, Guan Y, Lou Y, Chen H, Xu M, Deng D, Chen J, Ni B, Zhao L, et al. Dysbiosis of the gut microbiome is associated with tumor biomarkers in lung cancer. Int J Biol Sci. 2019;15(11):2381–2392. doi: 10.7150/ijbs.35980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Vascellari S, Palmas V, Melis M, Pisanu S, Cusano R, Uva P, Perra D, Madau V, Sarchioto M, Oppo V, et al. Gut microbiota and metabolome alterations associated with parkinson’s disease. mSystems. 2020;5(5). doi: 10.1128/mSystems.00561-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Valles-Colomer M, Falony G, Darzi Y, Tigchelaar EF, Wang J, Tito RY, Schiweck C, Kurilshikov A, Joossens M, Wijmenga C, et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat Microbiol. 2019;4(4):623–632. doi: 10.1038/s41564-018-0337-x. [DOI] [PubMed] [Google Scholar]
- 237.Yin Z, Zhang S, Wei Y, Wang M, Ma S, Yang S, Wang J, Yuan C, Jiang L, Du Y, et al. Horizontal gene transfer clarifies taxonomic confusion and promotes the genetic diversity and pathogenicity of plesiomonas shigelloides. mSystems. 2020;5(5). doi: 10.1128/mSystems.00448-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Suez J, Zmora N, Elinav E. Probiotics in the next-generation sequencing era. Gut Microbes. 2020;11(1):77–93. doi: 10.1080/19490976.2019.1586039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Zmora N, Zilberman-Schapira G, Suez J, Mor U, Dori-Bachash M, Bashiardes S, Kotler E, Zur M, Regev-Lehavi D, Brik RBZ, et al. Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell. 2018;174(6):1388–1405.e1321. doi: 10.1016/j.cell.2018.08.041. [DOI] [PubMed] [Google Scholar]
- 240.Zafar H, Saier MH Jr. Gut bacteroides species in health and disease. Gut Microbes. 2021;13(1):1–20. doi: 10.1080/19490976.2020.1848158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Zou Y, Lin X, Xue W. Characterization and description of Faecalibacterium butyricigenerans sp. nov. and F. longum sp. nov., isolated from human faeces. Sci Rep. 2021;11(1):11340. doi: 10.1038/s41598-021-90786-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Van Hul M, Le Roy T, Prifti E, Dao MC, Paquot A, Zucker J-D, Delzenne NM, Muccioli GG, Clément K, Cani PD, et al. From correlation to causality: the case of subdoligranulum. Gut Microbes. 2020;12(1):1–13. doi: 10.1080/19490976.2020.1849998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Zhang X, Li N, Chen Q, Qin H. Fecal microbiota transplantation modulates the gut flora favoring patients with functional constipation. Front Microbiol. 2021;12:700718. doi: 10.3389/fmicb.2021.700718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Ashida H, Suzuki T, Sasakawa C. Shigella infection and host cell death: a double-edged sword for the host and pathogen survival. Curr Opin Microbiol. 2021;59:1–7. doi: 10.1016/j.mib.2020.07.007. [DOI] [PubMed] [Google Scholar]
- 245.Guerrant RL, Bolick DT, Swann JR. Modeling enteropathy or diarrhea with the top bacterial and protozoal pathogens: differential determinants of outcomes. ACS Infect Dis. 2021;7(5):1020–1031. doi: 10.1021/acsinfecdis.0c00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Diling C, Longkai Q, Yinrui G, Yadi L, Xiaocui T, Xiangxiang Z, Miao Z, Ran L, Ou S, Dongdong W, et al. CircNF1-419 improves the gut microbiome structure and function in AD-like mice. Aging (Albany NY). 2020;12(1):260–287. doi: 10.18632/aging.102614. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 247.Mukherjee A, Lordan C, Ross RP, Cotter PD. Gut microbes from the phylogenetically diverse genus Eubacterium and their various contributions to gut health. Gut Microbes. 2020;12(1):1802866. doi: 10.1080/19490976.2020.1802866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.van Trijp MPH, Schutte S, Esser D. Minor changes in the composition and function of the gut microbiota during a 12-week whole grain wheat or refined wheat intervention correlate with liver fat in overweight and obese adults. J Nutr. 2021;151(3):491–502. doi: 10.1093/jn/nxaa312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Wang Y, Zhang C, Hou S, Wu X, Liu J, Wan X. Analyses of potential driver and passenger bacteria in human colorectal cancer. Cancer Manag Res. 2020;12:11553–11561. doi: 10.2147/CMAR.S275316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Fan X, Alekseyenko AV, Wu J, Peters BA, Jacobs EJ, Gapstur SM, Purdue MP, Abnet CC, Stolzenberg-Solomon R, Miller G, et al. Human oral microbiome and prospective risk for pancreatic cancer: a population-based nested case-control study. Gut. 2018;67(1):120–127. doi: 10.1136/gutjnl-2016-312580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Schoilew K, Ueffing H, Dalpke A, Wolff B, Frese C, Wolff D, Boutin S. Bacterial biofilm composition in healthy subjects with and without caries experience. J Oral Microbiol. 2019;11(1):1633194. doi: 10.1080/20002297.2019.1633194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Costa D, Iraola G. Pathogenomics of Emerging Campylobacter Species. Clin Microbiol Rev. 2019;32(4). doi: 10.1128/CMR.00072-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Gurwara S, Ajami NJ, Jang A, Hessel F, Chen L, Plew S, Wang Z, Graham D, Hair C, White D, et al. Dietary nutrients involved in one-carbon metabolism and colonic mucosa-associated gut microbiome in individuals with an endoscopically normal colon. Nutrients. 2019;11(3):613. doi: 10.3390/nu11030613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Liu Y, Li W, Yang H. Leveraging 16S rRNA microbiome sequencing data to identify bacterial signatures for irritable bowel syndrome. Front Cell Infect Microbiol. 2021;11:645951. doi: 10.3389/fcimb.2021.645951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Kim JM, Rim JH, Kim DH. Microbiome analysis reveals that ralstonia is responsible for decreased renal function in patients with ulcerative colitis. Clin Transl Med. 2021;11(3):e322. doi: 10.1002/ctm2.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Suárez-Jaramillo A, Baldeón ME, Prado B, Fornasini M, Cohen H, Flores N, Salvador I, Cargua O, Realpe J, Cárdenas PA, et al. Duodenal microbiome in patients with or without Helicobacter pylori infection. Helicobacter. 2020;25(6):e12753. doi: 10.1111/hel.12753. [DOI] [PubMed] [Google Scholar]
- 257.Gareau MG, Sherman PM, Walker WA. Probiotics and the gut microbiota in intestinal health and disease. Nat Rev Gastroenterol Hepatol. 2010;7(9):503–514. doi: 10.1038/nrgastro.2010.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Sniffen JC, McFarland LV, Evans CT, Goldstein EJC. Choosing an appropriate probiotic product for your patient: an evidence-based practical guide. PLoS One. 2018;13(12):e0209205. doi: 10.1371/journal.pone.0209205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Quin C, Estaki M, Vollman DM, Barnett JA, Gill SK, Gibson DL. Probiotic supplementation and associated infant gut microbiome and health: a cautionary retrospective clinical comparison. Sci Rep. 2018;8(1):8283. doi: 10.1038/s41598-018-26423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Suez J, Zmora N, Zilberman-Schapira G, Mor U, Dori-Bachash M, Bashiardes S, Zur M, Regev-Lehavi D, Ben-Zeev Brik R, Federici S, et al. Post-antibiotic gut mucosal microbiome reconstitution is impaired by probiotics and improved by autologous FMT. Cell. 2018;174(6):1406–1423.e1416. doi: 10.1016/j.cell.2018.08.047. [DOI] [PubMed] [Google Scholar]
- 261.Donaldson GP, Lee SM, Mazmanian SK. Gut biogeography of the bacterial microbiota. Nat Rev Microbiol. 2016;14(1):20–32. doi: 10.1038/nrmicro3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Lau HCH, Kranenburg O, Xiao H, Yu J. Organoid models of gastrointestinal cancers in basic and translational research. Nat Rev Gastroenterol Hepatol. 2020;17(4):203–222. doi: 10.1038/s41575-019-0255-2. [DOI] [PubMed] [Google Scholar]
- 263.Jalili-Firoozinezhad S, Gazzaniga FS, Calamari EL, Camacho DM, Fadel CW, Bein A, Swenor B, Nestor B, Cronce MJ, Tovaglieri A, et al. A complex human gut microbiome cultured in an anaerobic intestine-on-a-chip. Nat Biomed Eng. 2019;3(7):520–531. doi: 10.1038/s41551-019-0397-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.O’Toole PW, Marchesi JR, Hill C. Next-generation probiotics: the spectrum from probiotics to live biotherapeutics. Nat Microbiol. 2017;2(5):17057. doi: 10.1038/nmicrobiol.2017.57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this work.


