Abstract
Measurement of the lateral parapharyngeal wall has been shown to correlate with severity of obstructive sleep apnea, which is believed to increase risk of difficulty in mask ventilation (MV). This study aimed to assess the efficacy of using ultrasound to measure the lateral parapharyngeal wall thickness (LPWT) to predict the difficulty of MV. The LPWT was measured as the distance between the inferior border of the carotid artery and the lateral wall of the pharynx. Difficulty of MV was assessed according to an MV scale. A total of 92 patients were enrolled. Measurements of the LPWT ranged from 1.52 to 4.43 cm. There was a significant correlation between LPWT and difficulty of MV (P = 0.004). Every increase in 1 cm of LPWT was associated with an odds of increase in MV score of 3.17 (P < 0.05). With a cutoff of 3.5 cm, the area under the curve for LPWT was 0.67. The negative predictive value was 0.89, and the positive predictive value was 0.57. Use of point-of-care ultrasound to measure the LPWT shows promise in its ability to aid in airway management planning. Ultrasonic measurements of the LPWT have reasonable accuracy for predicting difficulty of MV.
Keywords: Difficult airway, lateral parapharyngeal wall, mask ventilation, obstructive sleep apnea, ultrasonography
Mask ventilation (MV) reduces the incidence of hypoxia and hypercarbia prior to intubation and provides a means of ventilation if a patient cannot be intubated. Most of the existing literature focuses on identifying factors that predispose the patient to a difficult intubation. As ease of MV does not necessarily imply ease of intubation and vice versa, there is a need to identify factors that contribute specifically to difficulty in MV.1 The basis of the difficult airway algorithm relies on the presumption that a patient can be mask ventilated.2 Patient characteristics such as age >55 years, body mass index (BMI) >26 kg/m2, and history of a sleep breathing disorder have been found to be risk factors for difficult MV.3,4 In several large studies, patients with obstructive sleep apnea (OSA) were four times more likely to have difficult MV when compared to non-OSA patients.5,6 More recently, studies have found a correlation between OSA and increased lateral parapharyngeal wall thickness (LPWT).7,8 Therefore, we hypothesized that measuring LPWT can help predict the difficulty of MV. The primary aim of this study was to assess the efficacy of using point-of-care ultrasound to measure the LPWT in the preoperative period to predict the difficulty of MV.
METHODS
This single-center, prospective study involved patients who underwent elective surgery requiring endotracheal intubation or supraglottic airway placement from May to July 2021 at George Washington University Hospital. The study was approved by the institutional review board at this institution (IRB #NCR203147). All data were securely stored in REDCap (Vanderbilt University, Nashville, TN). Adult patients were eligible for the study. Exclusion criteria included limited range of neck motion and/or a fracture or deformity that restricted ultrasound probe access to the lateral neck. All patients received information about the study in the preoperative period and consent was obtained to participate in the study. Additional demographic data including Mallampati score, BMI, and neck circumference was obtained.
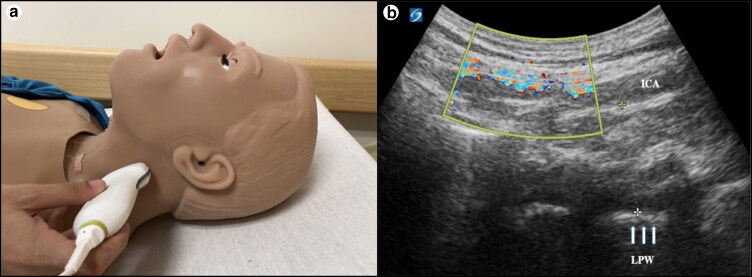
Airway sonography was performed using a SonoSite X-porte ultrasound system (FujiFilm, Philips Healthcare, Bothell, WA) equipped with a 3 to 8 MHz curvilinear transducer. Measurements were taken by three trained researchers before surgery, while the patient was in a supine position with the neck in a neutral position. The ultrasound probe was placed in the coronal plane on the lateral neck below the mastoid process (Figure 1). The internal carotid artery (ICA) and internal jugular vein were visualized utilizing Doppler imaging. The lateral pharyngeal wall was identifiable as a hypoechoic interface inferior to the ICA. The LPWT was measured as the distance between the inferior border of the ICA and the lateral wall of the pharynx, as described by Chen et al.7 All measurements were performed prior to MV or intubation.
Figure 1.
Ultrasonographic measurement of lateral pharyngeal wall thickness. (a) Scanning position to obtain measurement. (b) Identification of the internal carotid artery using color Doppler imaging; the lateral wall of the pharynx was visible as a hyperechoic interface (arrows).
Following induction of general anesthesia, difficulty in MV was assessed according to the grading scale developed by Han et al in which a score of 1 corresponds to an easy MV and a score of 4 is assigned when the provider is unable to initiate MV.9 The specific technique for MV was left to the discretion of the attending anesthesiologist, who was blinded to preoperative LPWT measurements. Difficulty of MV was then assessed by the anesthesiologist who performed the airway management of the patient.
RESULTS
A total of 92 patients were enrolled in the study from May through July 2021. Measurements of the LPWT ranged from 1.52 to 4.43 cm; 62% were easy, 23% required oral airway, 14% required two providers to ventilate, and one patient was unable to undergo MV (Table 1). There was a statistically significant correlation between LPWT and difficulty of MV (P = 0.004); however, there was no correlation between LPWT and BMI (P = 0.459) or between LPWT and Mallampati score (P = 0.381) (Table 2). Ordinal logistic regression analysis revealed that the likelihood of an increase in MV score was 3.17 higher (95% confidence interval 1.6–6.3; P < 0.05) for every 1 cm increase of LPWT (Table 3).
Table 1.
Mask ventilation grading with lateral pharyngeal wall measurements*
| Grade | LPWT (cm) | |
|---|---|---|
| 1 | Easy MV | 2.26 ± 0.44 |
| 2 | Difficult MV requiring an oral airway or other adjunct | 2.73 ± 0.69** |
| 3 | Very difficult MV requiring two providers | 3.32 ± 0.62** |
| 4 | Unable to MV | 4.4 |
Mask ventilation (MV) scoring system as defined by Han et al9 with the corresponding mean and standard deviation measurements of the lateral pharyngeal wall thickness (LPWT).
**Statistically significant (P < 0.05).
Table 2.
P values for correlation of patient characteristics and airway management parameters
| BMI | LPW | MV score | Subjective difficulty of intubation | |
|---|---|---|---|---|
| Body mass index | 0.459 | 0.003* | 0.183 | |
| LPW | 0.459 | 0.004* | 0.635 | |
| MV score | 0.003* | 0.004* | 0.008* |
Statistically significant (P < 0.05).
BMI indicates body mass index; LPW, lateral pharyngeal wall; MV, mask ventilation.
Table 3.
Ordinal logistic regression for mask ventilation score
| Parameter | B | Std. error | Sig. | Exp(B) | 95% Wald confidence interval for Exp(B) |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Lateral pharyngeal wall | 1.153 | 0.3482 | *<0.001 | 3.167 | 1.6 | 6.266 |
| Body mass index | 0.053 | 0.0272 | 0.052 | 1.054 | 1 | 1.112 |
Statistically significant (P < 0.05).
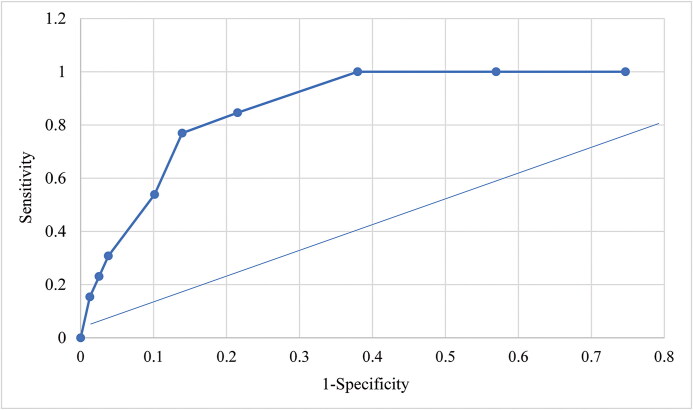
Receiver operating characteristic curve analysis and the area under the curve (AUC) were used to assess the performance of LPWT as a predictor of difficult MV. With a cutoff value of 3.5 cm, the AUC for LPWT was 0.67 (Figure 2). The negative predictive value was 0.89 and the positive predictive value was 0.57. The AUC of 0.67 demonstrates that this test is fairly accurate and has a high sensitivity for predicting difficulty with MV.
Figure 2.
Receiver operating characteristic curve analysis of lateral pharyngeal wall thickness in predicting difficult mask ventilation. The area under the curve is 0.67.
DISCUSSION
Perioperative point-of-care ultrasound is rapidly becoming a tool to assess the airway of patients and has been shown to add significant benefit to predicting airway management. Previous studies have shown that ultrasound measurements of the LPWT correlate with severity of OSA, which has been shown to be associated with difficult MV.5–8,10 The aim of this study was to determine if preoperative ultrasonographic measurements of the LPWT could predict difficult MV. The results confirmed that there is a statistically significant correlation between LPWT and difficult MV.
Patient characteristics such as age, BMI, and history of a sleep breathing disorder may provide some indication that MV will be difficult in the patient; however, these are not always reliable predictors.3 Similarly, clinical assessments of difficult airway, including the classic Mallampati score and thyromental distance, are diagnostically poor predictors of difficult airways, with sensitivities ranging from 42% to 81% and specificities ranging from 66% to 84%.11,12 Data from multiple studies show that ultrasonographic measurements of airway structures improve the ability to predict difficult airways.13–15 When these ultrasonographic measurements are combined with clinical examination findings, the diagnostic accuracy improves significantly, with sensitivities of 100%.16 These results suggest that the success of both MV and laryngoscopy relies on a complex interplay between different anatomical structures and that no single test can predict a difficult clinical scenario.
Previous studies have found a positive correlation between ultrasonographic measurements of various anatomical airway structures and severity of OSA. However, a recent meta-analysis of eight studies looking at various ultrasound measurements—including tongue base thickness, distance between lingual arteries, and retropalatal shortening—found a high sensitivity for diagnosing OSA, but only moderate specificity.17 Although this evidence suggests that ultrasound measurements can be used to predict severity of OSA, none of these studies took place in the perioperative setting.
The correlation between OSA and difficulty in MV has generally been attributed to increased collapsibility of the pharynx; however, recent evidence suggests that OSA is more complex and that anatomical factors alone do not equate to severity of OSA.18 Overnight ultrasonographic measurements have confirmed a posterior displacement of the tongue in OSA patients.19 Posterior displacement of the tongue likely obstructs airflow; however, there may be further restriction of airflow by lateral collapse which contributes to apnea. This is also supported by the point that a simple oral airway, whose function is to prevent the tongue from collapsing, is not fully effective in improving MV. Although the physiology of OSA may not be completely understood at this time, its association with difficulty in MV cannot be disregarded.
The complexity of the interactions between the airway structures is further complicated by the anatomic changes that occur during sleep and during drug-induced sedation. Propofol-induced sleep endoscopy is routinely used to understand the anatomic variations that lead to sleep-disordered breathing in patients with OSA; however, the mechanism for these changes has not been completely elucidated.20 Bianchini et al recently proposed a mechanism to explain the obstruction of airflow through the oro- and nasopharynx in patients following induction of anesthesia.13 They stated that collapse in the anterior-posterior plane of the airway, posterior tongue displacement, and hyomental distance shortening are all factors that are critical to airway collapse. Adding measurements of LPWT in the coronal plane to make this a three-dimensional model would further increase the reliability of these measures and allow clinicians to measure the narrowing of the airway in a novel plane. From a clinical perspective, if a practitioner has solid evidence of ease of MV, he or she may choose to do asleep fiber-optic as opposed to awake, potentially saving the patient from undue stress and anxiety.
There are some limitations to our study. First, it is a single-center study and patients with a known or presumed difficult airway were excluded due to patient safety. Therefore, these findings may not be generalizable to different populations. Another important limitation is that while ultrasound airway assessment techniques are becoming more common, ultrasound imaging and interpretation of the results remain user dependent. Furthermore, although this study was based on the correlation between MV and OSA, a history of a sleep breathing disorder was not recorded and may be helpful in future studies to determine if LPWT measurements are applicable in both OSA and non-OSA patients. Finally, the main limitation of this study is that even though the grading of MV was done according to preset parameters, it is still a subjective representation of the difficulty of MV.
In conclusion, given the high risk of morbidity and mortality if a patient cannot undergo MV in the time that it takes to secure an airway, more precise tools are needed in the perioperative period to better prepare for these situations. Ultrasonography has emerged as an attractive modality for predicting MV difficulty as it is readily available, minimally invasive, and allows for visualization of deeper airway structures. The results of this study suggest that the use of point-of-care ultrasound to measure the LPWT is an efficient and effective strategy for predicting MV difficulty and may transform preoperative airway evaluation and planning. Further studies with a larger sample size and multivariate analysis of complex measures will add to the findings of this study.
References
- 1.Ramachandran SK, Kheterpal S.. Difficult mask ventilation: does it matter? Anaesthesia. 2011;66:40–44. doi: 10.1111/j.1365-2044.2011.06933.x. [DOI] [PubMed] [Google Scholar]
- 2.American Society of Anesthesiologists . Practice guidelines for management of the difficult airway. In Malhotra SK, ed. Practice Guidelines in Anesthesia. Jaypee Digital; 2016. doi: 10.5005/jp/books/12644_18. [DOI] [Google Scholar]
- 3.Langeron O, Masso E, Huraux C, et al. . Prediction of difficult mask ventilation. Anesthesiology. 2000;92(5):1229–1236. doi: 10.1097/00000542-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Sato S, Hasegawa M, Okuyama M, et al. . Mask ventilation during induction of general anesthesia: influences of obstructive sleep apnea. Anesthesiology. 2017;126(1):28–38. doi: 10.1097/ALN.0000000000001407. [DOI] [PubMed] [Google Scholar]
- 5.Kheterpal S, Han R, Tremper KK, et al. . Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105(5):885–891. doi: 10.1097/00000542-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Nagappa M, Wong DT, Cozowicz C, Ramachandran SK, Memtsoudis SG, Chung F.. Is obstructive sleep apnea associated with difficult airway? Evidence from a systematic review and meta-analysis of prospective and retrospective cohort studies. PloS One. 2018;13(10):e0204904. doi: 10.1371/journal.pone.0204904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen H-C, Wang C-J, Lo Y-L, et al. . Parapharyngeal fat pad area at the subglosso-supraglottic level is associated with corresponding lateral wall collapse and apnea-hypopnea index in patients with obstructive sleep apnea: a pilot study. Sci Rep. 2019;9(1):17722. doi: 10.1038/s41598-019-53515-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, Nishino T.. Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol. 1997;82(4):1319–1326. doi: 10.1152/jappl.1997.82.4.1319. [DOI] [PubMed] [Google Scholar]
- 9.Han R, Tremper KK, Kheterpal S, O’Reilly M.. Grading scale for mask ventilation. Anesthesiology. 2004;101(1):267. doi: 10.1097/00000542-200407000-00059. [DOI] [PubMed] [Google Scholar]
- 10.Bilici S, Engin A, Ozgur Y, Ozlem Onerci C, Ahmet Gorkem Y, Aytul Hande Y.. Submental ultrasonographic parameters among patients with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2017;156(3):559–566. doi: 10.1177/0194599816684109. [DOI] [PubMed] [Google Scholar]
- 11.Lee A, Fan LTY, Gin T, Karmakar MK, Kee WDN.. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006;102(6):1867–1878. doi: 10.1213/01.ane.0000217211.12232.55. [DOI] [PubMed] [Google Scholar]
- 12.Salimi A, Farzanegan B, Rastegarpour A, Kolahi AA.. Comparison of the upper lip bite test with measurement of thyromental distance for prediction of difficult intubations. Acta Anaesthesiol Taiwanica. 2008;46(2):61–65. doi: 10.1016/S1875-4597(08)60027-2. [DOI] [PubMed] [Google Scholar]
- 13.Bianchini A, Nardozi L, Nardi E, Scuppa MF.. Airways ultrasound in predicting difficult face mask ventilation. Minerva Anestesiol. 2021;87(1):26–34. doi: 10.23736/S0375-9393.20.14455-9. [DOI] [PubMed] [Google Scholar]
- 14.You-Ten KE, Siddiqui N, Teoh WH, Kristensen MS.. Point-of-care ultrasound (POCUS) of the upper airway. Can J Anaesth. 2018;65(4):473–484. doi: 10.1007/s12630-018-1064-8. [DOI] [PubMed] [Google Scholar]
- 15.Kundra P, Mishra SK, Ramesh A.. Ultrasound of the airway. Indian J Anaesth. 2011;55(5):456–462. doi: 10.4103/0019-5049.89868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Upadhya RK, Shenoy L, Venkateswaran R.. Effect of intravenous dexmedetomidine administered as bolus or as bolus-plus-infusion on subarachnoid anesthesia with hyperbaric bupivacaine. J Anaesthesiol Clin Pharmacol. 2018;34:46–50. doi: 10.4103/joacp.JOACP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh M, Tuteja A, Wong DT, et al. . Point-of-care ultrasound for obstructive sleep apnea screening: are we there yet? A systematic review and meta-analysis. Anesth Analg. 2019;129(6):1673–1691. doi: 10.1213/ANE.0000000000004350. [DOI] [PubMed] [Google Scholar]
- 18.Magliulo G, Iannella G, Polimeni A, et al. . Laryngopharyngeal reflux in obstructive sleep apnoea patients: literature review and meta-analysis. Am J Otolaryngol. 2018;39(6):776–780. doi: 10.1016/j.amjoto.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Weng CK, Chen JW, Lee PY, Huang CC.. Implementation of a wearable ultrasound device for the overnight monitoring of tongue base deformation during obstructive sleep apnea events. Ultrasound Med Biol. 2017;43(8):1639–1650. doi: 10.1016/j.ultrasmedbio.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Abuan MRA, Lin WN, Hsin LJ, et al. . Tongue imaging during drug-induced sleep ultrasound in obstructive sleep apnea patients. Auris Nasus Larynx. 2020;47(5):828–836. doi: 10.1016/j.anl.2020.02.012. [DOI] [PubMed] [Google Scholar]