Depression among individuals who have been racially and ethnically minoritized in the U.S. can be vastly different from that of White Americans (1). For example, African American adults with depression rate their symptoms as more severe, have a longer illness course, and are more disabled (2, 3). In sum, the burden of depression appears to be higher among African Americans compared to White Americans (2).
African American adults are less likely to receive depression treatment than their White counterparts (4, 5). These inequities are increasingly linked to social, economic, and environmental determinants such as low income, under-resourced educational opportunities, inadequate housing, and lack of access to quality mental health treatment (6–9). Other contributors to this treatment gap include under-detection by providers (10), unreliable medical systems (11), and treatment settings perceived as punitive and inaccessible (12–14).
Frequency of suicidal thoughts and behaviors, which are often associated with depression, is increasing among African American youth. A nationally representative sample of U.S. high school students from 1991 to 2017 found that African American adolescents have experienced a 73% increase in suicide attempts, while the suicide attempt rate decreased 9% among White youth during the same period (15). Further, the suicide death rate among Black children ages 5 to 12 is increasing faster than any other racial/ethnic group in the U.S. (16, 17). Like those among adults, factors associated with the increase in depressive sequelae among African American youth are multi-factorial (18–21). While researchers have described how social determinants affect depression across the life course (22), little attention has been paid to how structural racism and its consequences may contribute to the intergenerational transmission of depression.
Thus, the purpose of this Review is to conceptualize how structural racism and cumulative trauma can be fundamental drivers of the intergenerational transmission of depression. We propose that understanding risk factors for depression, particularly its intergenerational reach, requires accounting for structural racism which is routinely experienced by racially and ethnically minoritized individuals (23). In light of the profoundly different experiences that African Americans have when depressed (i.e., more persistent course of illness and greater disability) (2), it is critical to examine whether intergenerational transmission would apply to structural racism as an emerging explanation for some of these differences.
Structural Racism and Depression
For this Review, we adopt Alvidrez & Tabor’s (2021) recent definition of structural racism as: “Macro-level societal conditions that limit opportunities, resources, and well-being of less privileged groups on the basis of race/ethnicity and/or other statuses, including but not limited to, gender identity, sexual orientation, disability status, social class or socioeconomic status (SES), religion, geographic residence, national origin, immigration status, limited English proficiency, physical characteristics, or health conditions” (24).
It is vital to note that structural racism as defined by Alvidrez and Tabor impacts many populations (e.g., LGBTQ populations, American Indians, Latinx, women, people with low income). A focus on structural racism lends itself to an analysis of how policies and systems impact specific groups and suggests topics on which to intervene (9, 25). Structural racism is evidenced by limited access to opportunities through macro-level systems including healthcare, criminal justice, housing, education, employment, and income. These systems give White people an unjust amount of value, resources, rights, and power while simultaneously dehumanizing and devaluing the privileges of communities of color and other marginalized populations (24, 26).
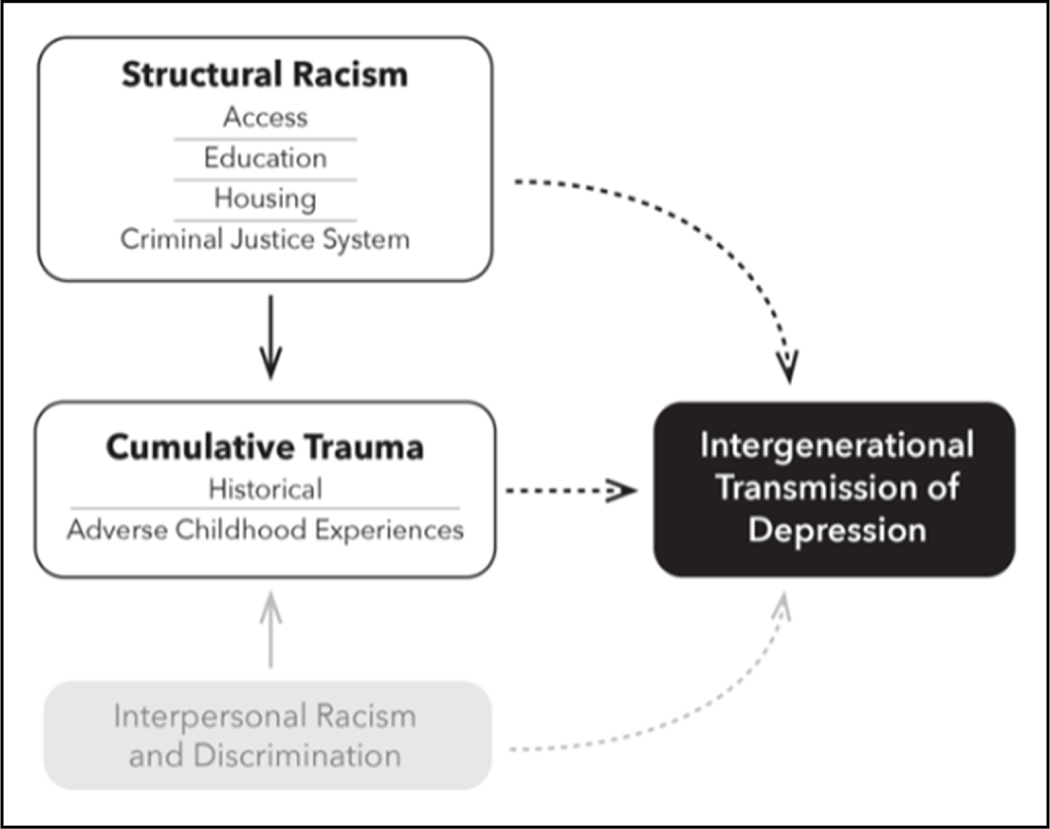
Our focus on structural racism does not minimize the deleterious impact of personally-mediated racial discrimination (e.g., hate crimes, being followed in a shopping store due to suspicion they may steal) or internalized racial inferiority (e.g., self-devaluation, hopelessness, and an embracing of “whiteness”) (27). Indeed, there is a robust evidence base demonstrating the negative mental health and physical impacts of racial discrimination and internalized racial inferiority (28–31). Rather, we aim to emphasize how structural racism cumulative trauma may contribute to the intergenerational transmission of depression. Figure 1 shows our conceptualization of the relationship between structural racism, cumulative trauma, and depression transmission across generations.
Figure 1.
Relationship between Structural Racism, Cumulative Trauma, and the Intergenerational Transmission of Depression
Cumulative Trauma and Depression
Cumulative trauma is a term is used to explain syndromes that result from repeated injury or are aggravated by repetitive insults. Examples in medicine are carpal tunnel syndrome, low back pain, or tennis elbow (32). Similarly, there are likely cumulative psychological consequences resulting from traumatic experiences. The frequency, severity, duration, and timing of these traumatic exposures are positively correlated with severity of health outcomes, including depression. The effects are even more devastating when there is betrayal, when a trusted person like a parent or close friend betrays the trust of the victim and inflicts harm (33). Traumatic experiences stemming directly from structural racism represent the failure of a trusted entity (institutions, society, the government) to protect one from harm.
Related to cumulative trauma is the idea of “historical trauma,” which refers to intergenerational trauma experienced by a group of individuals that have been systematically oppressed in prior generations (34). Historical trauma theory postulates that the psychological and emotional consequences of mass traumatic experiences can be transmitted to subsequent generations through physiological, environmental, and social pathways (25, 34). This results in an intergenerational cycle of trauma response, including physical (e.g., compromised immune system, endocrine impairment, adrenal maladaptation), social (e.g., domestic violence, child maltreatment, substance abuse, involvement in crime), and psychological (e.g., depression, panic/anxiety disorders, post-traumatic stress disorder) (25, 35). Other psychological mechanisms include people’s beliefs (i.e., cognitive factors) that are transmitted across generations. For example, children may be socialized within their families and schools to perceive racially minoritized groups as deficient (36).
The concept of intergenerational trauma was introduced in the psychiatric literature through descriptions of behavioral and clinical problems in offspring of Holocaust survivors (37). Subsequently, there have been discussions about the impact of historical events such as colonization, slavery, and displacement trauma in many cultures, including First Nations and native American communities (38), African Americans (39, 40), Australian aboriginal people (41), and Maori people of New Zealand (42). Intergenerational trauma has also been studied in societies exposed to genocide, ethnic cleansing, or war, such as people of Cambodian (43), Armenian (44), Rwandan (45), and Palestinian descent (46). The data is even scarcer among those experiencing both and yet distinct well-documented cumulative and historical traumata – sexual minorities among racial/ethnic minorities (47).
Adverse Childhood Experiences (ACEs) are adverse events experienced by children under 18 years of age (48). Early studies defined ACEs as emotional, physical, or sexual abuse; emotional and physical neglect; witnessing violence against mother; parental separation/divorce; and living with household members who were ever incarcerated, had mental illness or were suicidal, or misused substances (48, 49). Expanded ACEs studies also include experiences of racism, bullying, low neighborhood safety, community violence, and living in foster care as additional forms of childhood trauma (50). Numerous ACEs studies have documented a strong, graded dose-response relationship between the number of ACEs; individuals with 4 or more ACEs have been found to be at the highest risk for or have experienced negative health, social, and behavioral outcomes in adulthood (51). Further, a long-standing body of evidence indicates childhood exposure to intimate partner violence and other forms of abuse is positively correlated with perpetrating various forms of violence across the life course (52).
Numerous studies have shown the long-term negative impact of childhood adversity and maltreatment on increased risk of depression across the lifespan (53–55). The rates of childhood adversity, poor parental bonding, and family instability are clustered among parents with depression (56). The literature is replete with studies documenting the adverse and cumulative effects of interpersonal trauma upon a person’s psychological wellbeing (57–59). Left untreated, the outcome of these traumatic stressors and violent episodes includes enduring cognitive and physiological consequences, including depression (60).
Intergenerational Transmission of Depression
Numerous studies from the U.S. and internationally show that the offspring of depressed parents are at increased risk of developing depression and other adverse clinical outcomes (61–67). Transmission of depression from parent to child may begin early, even in utero. New studies of the offspring of depressed mothers are increasingly focused on the pregnancy itself and the effects of maternal depression on the offspring during pregnancy, delivery, and post-partum (68, 69). These studies show that depressive episodes in the mother are associated with premature delivery, low birth weight, and atypical adjustment, which can lead to greater risk for childhood adjustment problems as they mature (70, 71).
Of great relevance to African Americans and other marginalized groups is the notion that depression risk among those directly impacted by structural racism and cumulative trauma may extend to their descendants. The following vignette is based on a real patient named “Barbara.” Some details have been modified with patient consent to protect patient confidentiality. The case describes how structural racism and cumulative trauma impacted the intergenerational transmission and illness course of depression in an African American family.
CLINCAL CASE HISTORY
Barbara is a 64 year-old African American woman who is an adjunct professor and lives in a large urban city in the northeast U.S. She has a past psychiatric history of depression and post-traumatic stress disorder (PTSD). Her family history is significant for depression and trauma. Barbara’s mother was diagnosed with depression and had multiple depressive episodes during Barbara’s childhood. She remembers her mother developing certain patterns and behaviors when she was depressed, most prominent of which were social isolation (e.g., not wanting to go out or see friends), sleep problems, missing many days from work, and filing for disability at an early age. Despite acknowledging that she was depressed, Barbara’s mother never sought treatment for her illness stating, “The only thing psychiatrists do for us (African Americans) is lock us up in the hospital. I’ll handle this by myself.”
Barbara’s father was born in a town in the deep South. On two separate occasions he woke up to see a Cross burning on his front yard. His family migrated to a large northern, urban city shortly after Emmett Till was murdered, because his mother was terrified that her son’s life would be in danger as he got older. Several years after graduating high school, Barbara’s father and mother got married. He sought full-time jobs but was denied multiple vocational opportunities due to “lack of experience.” After finding work and saving enough money to move to his desired neighborhood, the family was denied an apartment because the neighborhood did not rent to African Americans. Barbara’s father mentioned on multiple occasions that the family tried to rent an apartment but was never given a reason why their application was denied. In 1974, he was arrested when Barbara was an adolescent and sentenced to 15 years in prison for possession of marijuana. Although this was his first criminal offense, he was incarcerated for eight of his 15 year sentence.
Barbara experienced a range of ACEs before having her first depressive episode as a young adult: her mother had depression, her father was incarcerated when she was 17 years old, and she was a survivor of physical and sexual abuse from a close male relative. Barbara was also bullied by White students at school when they discovered her father had been incarcerated.
To this day, Barbara experiences recurrent depressive episodes and symptoms of PTSD, most notably hypervigilance. Her symptoms are exacerbated by present-day events, such as the murder of George Floyd in 2020, that remind her of the historical traumatic events to which her family was exposed. Furthermore, she has attributed persistence of her depressive symptoms to challenges navigating the healthcare system, mistreatment by mental health care providers, and lack of access to affordable, high quality treatment. Protective factors that she cites include spirituality, a strong social network of friends, and engagement with a trauma-informed psychiatrist and therapist. Breaking the familial cycle of depression illustrated in Barbara’s case must involve directly addressing the structural barriers she, her father, and mother experienced.
RECOMMENDATIONS TO DISRUPT STRUCTURAL RACISM
Advocate for Anti-Racist Policies
Morsy & Rothstein (2019) note that social class, income, and race can contribute to toxic stress, which can lead to behavioral problems and depression. They recommend improved support (i.e., home visits and/or therapy services by community health workers or other specialists) to promote protective parenting, improved training of school staff to support children (72), addressing racially disparate policies and practices in schools (i.e., inequitable discipline policies which can induce stress), and training health care professionals in screening and treatment for stressful experiences such as trauma (73). Public policies that address inequities in social determinants of health (e.g., education, housing, employment, and food insecurity) that are rooted in structural racism are also needed.
Similarly, the mass incarceration of African American men has been well documented (74). Barbara’s father was victim to excessively harsh drug laws in the 1970s that gave a minimum of 15 years to life in prison to people charged with possession of illicit substances (75, 76). Policies that promote criminal justice reform hold great promise for disrupting the cycle of intergenerational trauma (77). Any one of these policies may have improved Barbara’s quality of life and the trajectory of her depression.
Address Societal Attitudes and Biases
It is critical that we adequately address conscious and unconscious biases throughout society. Providing inclusive and complete histories about minoritized groups within our educational system – beginning in children’s formative years – is a meaningful first step to disrupting the cross generational transmission of deficit-based beliefs about minoritized groups. Meaningful change must be comprehensive, coordinated, and multi-tiered. Rigorously testing the impact of these strategies will be crucial to assess the utility of widespread dissemination.
Conduct Longitudinal Studies with Racially Diverse Samples
Intergenerational questions require intergenerational study designs. Until intergenerational cohorts of groups exposed to structural racism become more readily accessible, questions about the intergenerational ramifications of racism and trauma will remain unanswered. To date, the vast majority of longitudinal studies have been conducted with mostly White subjects.
A notable exception is the Boricua Youth Study (BYS) – a longitudinal, population-based sample of Puerto Rican children and adolescents in two separate locations: the South Bronx, New York and the San Juan and Caguas Metropolitan Area, Puerto Rico. Importantly, the BYS is the only study to date to examine developmental psychopathology in children of the same ethnic group living in two highly disadvantaged contexts in the US. Although in both contexts children are disproportionately exposed to structural racism, Puerto Rican children residing in the South Bronx (SBx) have the additional experience of being an ethnically minoritized group. It has thus been possible, for the past 20 years to examine how the experience of being part of an ethnically minoritized group – which putatively implicates increased exposure to racism, discrimination, acculturation, and cultural stress (78, 79) – shapes risk for psychopathology differently for Puerto Rican children residing outside of the archipelago.
The BYS has consistently documented higher prevalence of a number of psychiatric disorders in children residing in the SBx. Notably, although the risk and resiliency factors to developing psychopathology have been similar across both contexts, risk factors (including cultural stress and discrimination) were more frequently present in the SBx. In fact, our studies have shown that even when controlling for sociodemographic factors and stressful life events, cultural stress (79, 80) remains a strong predictor of psychopathology in children. Further, findings from the most recent wave of data collection (78) suggest that the intersecting contexts of minoritized participants might be particularly important for understanding risk for depression.
“Co-produce” clinical interventions and research
There is a growing body of evidence showing that policy makers, clinicians, and researchers need to co-produce research and interventions (e.g., programs, services, policies) in collaboration with people of color instead of coming up with “top down” solutions (81). Community-Partnered Participatory Research (CPPR) is one of many community engagement strategies that fosters collaborations between community members, researchers, and clinicians (82). CPPR emphasizes two-way sharing of knowledge, respect for diversity, and equity (83). Community-partnered approaches enable shared power among stakeholders, increase trust within marginalized communities, (e.g., Tuskegee Syphilis Study), and reduce mental health disparities (84, 85).
Culturally Tailor Depression Interventions for Males of Color
The aforementioned Boricua Youth Study (BYS) documented unusually high rates of depression among males in both study sites, so much so that the expected sex differences in depression rates were not observed. It may be that the lack of opportunities, high poverty, and lack of social mobility present across both contexts may interact with cultural gender norms and generate frustration among young men who may feel like inadequate providers for their families. Because racial and ethnic minorities are more likely to reside in underserved communities, our findings highlight how multiple intersecting factors, including structural racism manifestations and poverty, shape depression risk across the life course.
Intersectionality theory, rooted in feminist approaches and Critical Race Theory, posits that social identities involve complex intersections of individuals’ lived experiences nested within systems of oppression (86, 87). We propose the use of intersectionality to adapt depression interventions for men of color, whose socially constructed identity categorizations (i.e., race), experiences (e.g., depression, criminal justice involvement), and gender impact perceived racial discrimination and utilization of mental health services (88). Given the rising rates of suicidality among Black boys, culturally tailoring depression interventions is a pressing clinical and public health need. Conversely, we should be wary about overdeveloping culturally based solutions. This may suggest inherent defects within marginalized or stigmatized populations that inadvertently support the notion that whiteness equates to perfection. Intersectionality may also guide the development of a more diverse workforce to deliver mental health interventions to and in marginalized communities.
CONCLUSION
We assert that structural racism and cumulative trauma are fundamental drivers of the intergenerational transmission of depression. The clinical vignette highlights the ways in which structural racism (e.g., familial housing discrimination, lack of access to mental health treatment) and cumulative trauma (e.g., exposure to hate crimes via Cross burnings, parental incarceration, ACEs) interact to influence the intergenerational transmission of depression. Action should be directed towards policies that dismantle structurally racist institutions and practices; improve protective systems, including a mental health treatment system that is equitable, high quality, and accessible; and generate knowledge to understand the intergenerational course of depression among historically racially and ethnically minoritized families.
Acknowledgements
Funding for this manuscript was provided by the National Institute of Mental Health (Dr. Hankerson) Award Number 1R01 MH121590 and Award Number T32MH096724 (Dr. Waller). We acknowledge the work of Drs. Chester Pierce, Camara Jones, and David Williams, among others, whose conceptualization of racism led to groundbreaking empirical studies which highlighted the deleterious impact of racism on mental health.
Previous presentation
Some of this material was presented at the National Institute of Mental Health Workshop “Identifying New Directions in Mental Health Disparities Research: Innovations with a Multidimensional Lens” November 9-10, 2020
Footnotes
Location of work and address for reprints
This manuscript was produced in the Departments of Psychiatry and Medicine, Columbia University Irving Medical Center, New York, New York. Dr. Sidney Hankerson is corresponding author. His address is 1425 Madison Avenue, 2nd Floor, New York, NY 10029. Reprint requests can be sent to Dr. Hankerson at sidney.hankerson@mountsinai.org
Conflicts of Interest:
All authors have no conflicts of interest to disclose
Contributor Information
Sidney H. Hankerson, Icahn School of Medicine at Mount Sinai, Department of Psychiatry, Department of Population Health Sciences & Policy, 1425 Madison Avenue, New York, NY 10029.
Nathalie Moise, Columbia University Irving Medical Center, Department of Medicine, 622 West 168 Street, PH 9, New York, NY 10032.
Diane Wilson, Icahn School of Medicine at Mount Sinai, New York; Department of Medicine Columbia University Irving Medical Center, New York; City University of New York.
Bernadine Y. Waller, Columbia University Irving Medical Center, Department of Psychiatry, New York State Psychiatric Institute, 1051 Riverside Drive, New York, NY 10032.
Kimberly T. Arnold, University of Pennsylvania Perelman School of Medicine, Department of Family Medicine and Community Health, University of Pennsylvania Center for Public Health Initiatives, University of Pennsylvania Leonard Davis Institute of Health Economics, Penn Presbyterian Medical Center, Andrew Mutch Building, Floor 6, 51 N. 39th Street, Philadelphia, PA 19104.
Cristiane Duarte, Columbia University Irving Medical Center, New York State Psychiatric Institute, Department of Psychiatry, 1051 Riverside Drive, New York, NY 10032.
Claudia Lugo-Candelas, Columbia University Irving Medical Center, Department of Psychiatry, New York State Psychiatric Institute, 1051 Riverside Drive, New York, NY 10032.
Myrna M Weissman, Columbia University, Mailman School of Public Health, Columbia University Irving Medical Center, New York State Psychiatric Institute, 1051 Riverside Drive Unit 24, New York, New York 10032.
Milton Wainberg, Columbia University Irving Medical Center, New York State Psychiatric Institute, Department of Psychiatry, 1051 Riverside Drive, New York, NY 10032.
Rachel Yehuda, Icahn School of Medicine at Mount Sinai, Department of Psychiatry, The Bronx James J. Peters VA Medical Center, 1 Gustave L. Levy Pl, New York, NY 10029.
Ruth Shim, University of California at Davis, Department of Psychiatry.
REFERENCES
- 1.Gonzalez HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: too little for too few. Arch Gen Psychiatry. 2010;67(1):37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–15. [DOI] [PubMed] [Google Scholar]
- 3.Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35(3):317–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hankerson SH, Fenton MC, Geier TJ, Keyes KM, Weissman MM, Hasin DS. Racial differences in symptoms, comorbidity, and treatment for major depressive disorder among black and white adults. J Natl Med Assoc. 2011;103(7):576–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGregor B, Li C, Baltrus P, Douglas M, Hopkins J, Wrenn G, et al. Racial and Ethnic Disparities in Treatment and Treatment Type for Depression in a National Sample of Medicaid Recipients. Psychiatr Serv. 2020;71(7):663–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Compton MT, Shim RS. Why Employers Must Focus on the Social Determinants of Mental Health. Am J Health Promot. 2020;34(2):215–9. [DOI] [PubMed] [Google Scholar]
- 7.Metzl JM, Hansen H. Structural Competency and Psychiatry. JAMA Psychiatry. 2018;75(2):115–6. [DOI] [PubMed] [Google Scholar]
- 8.Moise N, Hankerson S. Addressing Structural Racism and Inequities in Depression Care. JAMA Psychiatry. 2021. [DOI] [PubMed] [Google Scholar]
- 9.Shim RS. Dismantling Structural Racism in Psychiatry: A Path to Mental Health Equity. Am J Psychiatry. 2021;178(7):592–8. [DOI] [PubMed] [Google Scholar]
- 10.Akincigil A, Olfson M, Siegel M, Zurlo KA, Walkup JT, Crystal S. Racial and ethnic disparities in depression care in community-dwelling elderly in the United States. Am J Public Health. 2012;102(2):319–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beach MC, Saha S, Park J, Taylor J, Drew P, Plank E, et al. Testimonial Injustice: Linguistic Bias in the Medical Records of Black Patients and Women. J Gen Intern Med. 2021;36(6):1708–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hankerson SH, Watson KT, Lukachko A, Fullilove MT, Weissman M. Ministers’ perceptions of church-based programs to provide depression care for African Americans. J Urban Health. 2013;90(4):685–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Upadhyay N, Aparasu R, Rowan PJ, Fleming ML, Balkrishnan R, Chen H. The association between geographic access to providers and the treatment quality of pediatric depression. J Affect Disord. 2019;253:162–70. [DOI] [PubMed] [Google Scholar]
- 14.Goff SL, Mazor KM, Guhn-Knight H, Budway YY, Murphy L, White KO, et al. Factors That Matter to Low-Income and Racial/Ethnic Minority Mothers When Choosing a Pediatric Practice: a Mixed Methods Analysis. J Racial Ethn Health Disparities. 2017;4(6):1051–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindsey MA, Sheftall AH, Xiao Y, Joe S. Trends of Suicidal Behaviors Among High School Students in the United States: 1991–2017. Pediatrics. 2019;144(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bridge JA, Asti L, Horowitz LM, Greenhouse JB, Fontanella CA, Sheftall AH, et al. Suicide Trends Among Elementary School-Aged Children in the United States From 1993 to 2012. JAMA Pediatr. 2015;169(7):673–7. [DOI] [PubMed] [Google Scholar]
- 17.Bridge JA, Horowitz LM, Fontanella CA, Sheftall AH, Greenhouse J, Kelleher KJ, et al. Age-Related Racial Disparity in Suicide Rates Among US Youths From 2001 Through 2015. JAMA Pediatr. 2018;172(7):697–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindsey MA, Banks A, Cota CF, Scott ML, Joe S. A Review of Treatments for Young Black Males Experiencing Depression. Res Soc Work Pract. 2018;28(3):320–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xiao Y, Romanelli M, Velez-Grau C, Lindsey MA. Unpacking Racial/Ethnic Differences in the Associations between Neighborhood Disadvantage and Academic Achievement: Mediation of Future Orientation and Moderation of Parental Support. J Youth Adolesc. 2020. [DOI] [PubMed] [Google Scholar]
- 20.Xiao Y, Romanelli M, Lindsey MA. A latent class analysis of health lifestyles and suicidal behaviors among US adolescents. J Affect Disord. 2019;255:116–26. [DOI] [PubMed] [Google Scholar]
- 21.Assari S, Gibbons FX, Simons R. Depression among Black Youth; Interaction of Class and Place. Brain Sci. 2018;8(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watkins DC. Depression over the adult life course for African American men: toward a framework for research and practice. Am J Mens Health. 2012;6(3):194–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Priest N, Williams DR. Structural Racism: A Call to Action for Health and Health Disparities Research. Ethn Dis. 2021;31(Suppl 1):285–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alvidrez J, Tabor DC. Now Is the Time to Incorporate the Construct of Structural Racism and Discrimination into Health Research. Ethn Dis. 2021;31(Suppl 1):283–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sotero MJ. A conceptual model of historical trauma: Implications for public health practice and research. Journal of Health Disparities Research and Practice 2006;1(1):93–108. [Google Scholar]
- 26.Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet (London, England). 2017;389(10077):1453–63. [DOI] [PubMed] [Google Scholar]
- 27.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williams DR, Williams-Morris R. Racism and Mental Health: the African American experience. Ethnicity & Health. 2000;5(3/4):243–68. [DOI] [PubMed] [Google Scholar]
- 29.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molina KM, James D. Discrimination, internalized racism, and depression: A comparative study of African American and Afro-Caribbean adults in the US. Group Process Intergroup Relat. 2016;19(4):439–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hudson DL, Neighbors HW, Geronimus AT, Jackson JS. Racial Discrimination, John Henryism, and Depression Among African Americans. J Black Psychol. 2016;42(3):221–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Silverstein BA, Fine LJ, Armstrong TJJO, Medicine E. Hand wrist cumulative trauma disorders in industry. 1986;43(11):779–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martin CG, Cromer LD, Deprince AP, Freyd JJ. The Role of Cumulative Trauma, Betrayal, and Appraisals in Understanding Trauma Symptomatology. Psychol Trauma. 2013;52(2):110–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ehlers CL, Gizer IR, Gilder DA, Ellingson JM, Yehuda R. Measuring historical trauma in an American Indian community sample: contributions of substance dependence, affective disorder, conduct disorder and PTSD. Drug Alcohol Depend. 2013;133(1):180–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yehuda R, Lehrner A. Intergenerational transmission of trauma effects: putative role of epigenetic mechanisms. World Psychiatry. 2018;17(3):243–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goff PA, Jackson MC, Di Leone BA, Culotta CM, DiTomasso NA. The essence of innocence: consequences of dehumanizing Black children. Journal of personality and social psychology. 2014;106(4):526–45. [DOI] [PubMed] [Google Scholar]
- 37.Yehuda R, Bell A, Bierer LM, Schmeidler J. Maternal, not paternal, PTSD is related to increased risk for PTSD in offspring of Holocaust survivors. J Psychiatr Res. 2008;42(13):110411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Evans-Campbell T.Historical trauma in American Indian/Native Alaska communities: a multilevel framework for exploring impacts on individuals, families, and communities. J Interpers Violence. 2008;23(3):316–38. [DOI] [PubMed] [Google Scholar]
- 39.Degruy-Leary J.Post-traumatic Slave Syndrome: America’s legacy of enduring injury. Portland, OR: Joy DeGruy Publications Inc; 2017. [Google Scholar]
- 40.Eyerman R.Cultural trauma: Slavery and the formation of African American identity: Cambridge University Press; 2001. [Google Scholar]
- 41.Krieg A.The experience of collective trauma in Australian Indigenous communities. Australas Psychiatry. 2009;17 Suppl 1:S28–32. [DOI] [PubMed] [Google Scholar]
- 42.Pihama L, Reynolds P, Smith C, Reid J, Smith LT, Nana RTJAAIJoIP. Positioning historical trauma theory within Aotearoa New Zealand. 2014;10(3):248–62. [Google Scholar]
- 43.Münyas BJ. Genocide in the minds of Cambodian youth: transmitting (hi) stories of genocide to second and third generations in Cambodia. Journal of Genocide Research. 2008;10(3):413–39. [Google Scholar]
- 44.Azarian-Ceccato N.Reverberations of the Armenian genocide: Narrative’s intergenerational transmission and the task of not forgetting. J Narrative Inquiry. 2010;20(1):106–23. [Google Scholar]
- 45.Roth M, Neuner F, Elbert T. Transgenerational consequences of PTSD: risk factors for the mental health of children whose mothers have been exposed to the Rwandan genocide. J International journal of mental health systems. 2014;8(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barron IG, Abdallah G. Intergenerational trauma in the occupied Palestinian territories: Effect on children and promotion of healing. Journal of Child Adolescent Trauma. 2015;8(2):103–10. [Google Scholar]
- 47.Katz-Wise SL, Hyde JS. Victimization experiences of lesbian, gay, and bisexual individuals: a meta-analysis. J Sex Res. 2012;49(2–3):142–67. [DOI] [PubMed] [Google Scholar]
- 48.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–58. [DOI] [PubMed] [Google Scholar]
- 49.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. Jama. 2001;286(24):3089–96. [DOI] [PubMed] [Google Scholar]
- 50.Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, et al. Adverse Childhood Experiences: Expanding the Concept of Adversity. Am J Prev Med. 2015;49(3):354–61. [DOI] [PubMed] [Google Scholar]
- 51.Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC. Adverse childhood experiences and life opportunities: Shifting the narrative. Children Youth Services Review. 2017;72:141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kimber M, Adham S, Gill S, McTavish J, MacMillan HL. The association between child exposure to intimate partner violence (IPV) and perpetration of IPV in adulthood-A systematic review. Child Abuse Negl. 2018;76:273–86. [DOI] [PubMed] [Google Scholar]
- 53.Choi KW, Houts R, Arseneault L, Pariante C, Sikkema KJ, Moffitt TE. Maternal depression in the intergenerational transmission of childhood maltreatment and its sequelae: Testing postpartum effects in a longitudinal birth cohort. Dev Psychopathol. 2019;31(1):143–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Ann Epidemiol. 2010;20(5):385–94. [DOI] [PubMed] [Google Scholar]
- 55.McNeil S, Harris-McKoy D, Brantley C, Fincham F, Beach SRJJoC, Studies F. Middle class African American mothers’ depressive symptoms mediate perceived discrimination and reported child externalizing behaviors. 2014;23(2):381–8. [Google Scholar]
- 56.Scorza P, Duarte CS, Hipwell AE, Posner J, Ortin A, Canino G, et al. Research Review: Intergenerational transmission of disadvantage: epigenetics and parents’ childhoods as the first exposure. J Child Psychol Psychiatry. 2019;60(2):119–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abraham EH, Antl SM, McAuley T. Trauma exposure and mental health in a community sample of children and youth. Psychol Trauma. 2021. [DOI] [PubMed] [Google Scholar]
- 58.De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23(2):185–222, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Waller B, Quinn CR, Boyd D, DiClemente R, Voisin DR. Correlates of depression among Black girls exposed to violence. J Racial Ethn Health Disparities. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gloger S, Vohringer PA, Martinez P, Chacon MV, Caceres C, Diez de Medina D, et al. The contribution of early adverse stress to complex and severe depression in depressed outpatients. Depress Anxiety. 2021;38(4):431–8. [DOI] [PubMed] [Google Scholar]
- 61.Gotlib IH, Joormann J, Foland-Ross LC. Understanding Familial Risk for Depression: A 25-Year Perspective. Perspect Psychol Sci. 2014;9(1):94–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gotlib IH, Goodman SH, Humphreys KL. Studying the Intergenerational Transmission of Risk for Depression: Current Status and Future Directions. Curr Dir Psychol Sci. 2020;29(2):174–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pierce M, Hope HF, Kolade A, Gellatly J, Osam CS, Perchard R, et al. Effects of parental mental illness on children’s physical health: systematic review and meta-analysis. Br J Psychiatry. 2020;217(1):354–63. [DOI] [PubMed] [Google Scholar]
- 64.Ranning A, Benros ME, Thorup AAE, Davidsen KA, Hjorthoj C, Nordentoft M, et al. Morbidity and Mortality in the Children and Young Adult Offspring of Parents With Schizophrenia or Affective Disorders-A Nationwide Register-Based Cohort Study in 2 Million Individuals. Schizophr Bull. 2020;46(1):130–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta-analysis of family highrisk studies. Schizophr Bull. 2014;40(1):28–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Weissman MM, Berry OO, Warner V, Gameroff MJ, Skipper J, Talati A, et al. A 30-Year Study of 3 Generations at High Risk and Low Risk for Depression. JAMA Psychiatry. 2016;73(9):970–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weissman MM, Talati A, Gameroff MJ, Pan L, Skipper J, Posner JE, et al. Enduring problems in the offspring of depressed parents followed up to 38 years. EClinicalMedicine. 2021;38:101000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gingrich JA, Malm H, Ansorge MS, Brown A, Sourander A, Suri D, et al. New Insights into How Serotonin Selective Reuptake Inhibitors Shape the Developing Brain. Birth Defects Res. 2017;109(12):924–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Malm H, Brown AS, Gissler M, Gyllenberg D, Hinkka-Yli-Salomaki S, McKeague IW, et al. Gestational Exposure to Selective Serotonin Reuptake Inhibitors and Offspring Psychiatric Disorders: A National Register-Based Study. J Am Acad Child Adolesc Psychiatry. 2016;55(5):359–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Roffman JL, Dunn EC. Neuropsychopharmacology reviews 2022 hot topics: the prenatal environment and risk for mental illness in young people. Neuropsychopharmacology. 2021;18:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wong G, Weir JM, Mishra P, Huynh K, Nijagal B, Gupta V, et al. The placental lipidome of maternal antenatal depression predicts socio-emotional problems in the offspring. Transl Psychiatry. 2021;11(1):107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kennedy-Hendricks A, Huskamp HA, Rutkow L, Barry CL. Improving Access To Care And Reducing Involvement In The Criminal Justice System For People With Mental Illness. Health Aff (Millwood). 2016;35(6):1076–83. [DOI] [PubMed] [Google Scholar]
- 73.Morsy L, Rothstein R. Toxic Stress and Children’s Outcomes: African American Children Growing up Poor Are at Greater Risk of Disrupted Physiological Functioning and Depressed Academic Achievement. Economic Policy Institute. 2019. [Google Scholar]
- 74.Alexander M.The new Jim Crow: Mass incarceration in the age of colorblindness: The New Press; 2020. [Google Scholar]
- 75.James K, Jordan A. The Opioid Crisis in Black Communities. The Journal of Law, Medicine & Ethics. 2018;46(2):404–21. [DOI] [PubMed] [Google Scholar]
- 76.Drucker E.Population impact of mass incarceration under New York’s Rockefeller drug laws: an analysis of years of life lost. J Urban Health. 2002;79(3):434–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cole DM, Thomas DM, Field K, Wool A, Lipiner T, Massenberg N, et al. The 21st Century Cures Act Implications for the Reduction of Racial Health Disparities in the US Criminal Justice System: a Public Health Approach. J Racial Ethn Health Disparities. 2018;5(4):885–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Alegria M, Shrout PE, Canino G, Alvarez K, Wang Y, Bird H, et al. The effect of minority status and social context on the development of depression and anxiety: a longitudinal study of Puerto Rican descent youth. World Psychiatry. 2019;18(3):298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Duarte CS, Bird HR, Shrout PE, Wu P, Lewis-Fernandez R, Shen S, et al. Culture and psychiatric symptoms in Puerto Rican children: longitudinal results from one ethnic group in two contexts. J Child Psychol Psychiatry. 2008;49(5):563–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Duarte CS, Canino GJ, Wall M, Ramos-Olazagasti M, Elkington KS, Bird H, et al. Development, Psychopathology, and Ethnicity II: Psychiatric Disorders Among Young Adults. Journal of the American Academy of Child Adolescent Psychiatry. 2021;60(5):579–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Figueroa C, Castillo EG, Norquist G, Wells KB, Griffith K, Kadkhoda F, et al. A Window of Opportunity: Visions and Strategies for Behavioral Health Policy Innovation. Ethn Dis. 2018;28(Suppl 2):407–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wells KB, Jones L, Chung B, Dixon EL, Tang L, Gilmore J, et al. Community-Partnered Cluster-Randomized Comparative Effectiveness Trial of Community Engagement and Planning or Resources for Services to Address Depression Disparities. Journal of General Internal Medicine. 2013;28(10):1268–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hankerson SH, Wells K, Sullivan MA, Johnson J, Smith L, Crayton L, et al. Partnering with African American Churches to Create a Community Coalition for Mental Health. Ethn Dis. 2018;28(Suppl 2):467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wells KB, Jones L, Chung B, Dixon EL, Tang L, Gilmore J, et al. Community-partnered cluster-randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. J Gen Intern Med. 2013;28(10):1268–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McCallum JM, Arekere DM, Green BL, Katz RV, Rivers BM. Awareness and knowledge of the U.S. Public Health Service syphilis study at Tuskegee: implications for biomedical research. J Health Care Poor Underserved. 2006;17(4):716–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carbado DW, Crenshaw KW, Mays VM, Tomlinson B. INTERSECTIONALITY: Mapping the Movements of a Theory. Du Bois Rev. 2013;10(2):303–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Parra LA, Hastings PD. Integrating the Neurobiology of Minority Stress with an Intersectionality Framework for LGBTQ-Latinx Populations. New Dir Child Adolesc Dev. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hankerson SH, Suite D, Bailey RK. Treatment disparities among African American men with depression: implications for clinical practice. J Health Care Poor Underserved. 2015;26(1):21–34. [DOI] [PMC free article] [PubMed] [Google Scholar]