Abstract
A process evaluation was conducted as part of a comparative effectiveness trial of a mailed interactive educational DVD intervention to promote colorectal cancer (CRC) screening among average-risk patients who did not attend a scheduled colonoscopy. Participants (n=371) for the trial were randomized to: 1) mailed DVD; 2) mailed DVD plus patient navigation; or 3) usual care. Participants (n=243) randomized to the two DVD intervention arms were called two weeks after mailing materials to complete a process evaluation interview about the DVD (September 2017-February 2020). Forty-nine (20%) participants were not reached and 194 (80%) participants watched the DVD and completed the interview. The process evaluation assessed whether: 1) the DVD content was helpful; 2) any new information was learned by participants; 3) the appropriate amount of information was included in the DVD; 4) participants were engaged when watching the DVD; 5) the DVD content was relevant; 6) participants were satisfied with the DVD; 7) participants would recommend the DVD to others; and 8) their opinion about CRC screening was changed by watching the DVD. Among participants who watched the DVD, 99% reported the screening information was very or somewhat helpful, 47% learned new information, 75% said the DVD included the right amount of information, they were engaged (mean=3.35 out of 4, SD=0.49), 87% reported all or most information applied to them, they were satisfied (mean=3.42 out of 4, SD=0.39) with DVD content, 99% would recommend the DVD to others, and 45% reported changing their opinion about screening. To understand the effects of interventions being tested in trials and to plan dissemination of evidence-based interventions, process evaluation is critical to assess the dose received and acceptability of behavioral interventions.
Keywords: colorectal cancer, colorectal cancer screening, process evaluation, colonoscopy, fecal immunochemical test, DVD intervention
Background
Colorectal cancer (CRC) is the third most common cancer among both men and women and the second leading cause of cancer deaths in the United States (Siegel et al., 2021). In 2021, there will be an estimated 149,500 new cases of CRC and nearly 53,000 deaths from CRC (Siegel et al., 2021). Screening is cost-effective and can prevent CRC or diagnose it at an early stage, which increases the likelihood of successful treatment (Guy et al., 2014; Meester et al., 2015; Zauber, 2010). Recommended CRC screening tests include direct visualization tests (e.g. colonoscopy) and stool-based tests (e.g. Fecal Immunochemical Test [FIT]) (American Cancer Society, 2020; United States Preventive Services Task Force, 2016). Although CRC screening tests are commonly covered by health insurance, patient-level barriers to CRC screening tests include lack of physician recommendation, forgetting to schedule a test, transportation issues, cost, embarrassment, fear of cancer, and dislike of the bowel prep before undergoing a colonoscopy (Bhise et al., 2016; Klabunde et al., 2005; McLachlan, Clements & Austoker, 2012).
Interventions that include a video/DVD component have been widely adopted and used in cancer prevention and control. In a systematic review of video-based interventions for cancer control, Blake and colleagues (2020) found that most interventions achieved the studies’ primary outcomes (e.g. change in knowledge, attitudes, or behavior). The use of videos/DVDs tend to improve engagement by the use of the narrative especially among individuals who may have limited health literacy skills (Kreuter et al., 2007). Specifically, interventions that included a mailed educational video/DVD have had mixed results about increasing CRC screening behaviors (Cameron et al., 2011; Levy et al., 2012; Zapka et al., 2004).
Another strategy that has provided evidence to increase CRC screening are interventions that include patient navigation (DeGroff et al., 2017; Myers et al., 2014). The goal of patient navigation for CRC screening is to assist patients with navigating the complex health care system by addressing their individual barriers to screening, and to provide encouragement and support during the screening process.
Several CRC screening programs that use mailed educational video/DVD interventions and patient navigation have independently documented an increase uptake of CRC screening (Cameron et al., 2011; DeGroff et al., 2017; Levy et al., 2012; Myers et al., 2014); ). To our knowledge, however, the current comparative effectiveness trial is the first to compare a mailed interactive educational DVD with and without telephone-based patient navigation to increase CRC screening among patients who did not attend their scheduled colonoscopy.
Previous mailed CRC screening educational interventions that include videos/DVDs report the primary outcome of screening completion and have provided limited process evaluation information (e.g. percent of participants who watched the video/DVD) (Zapka et al., 2004; Cameron et al., 2011; Levy et al., 2012). Process evaluation is an essential component of program evaluation and includes not only the assessment of the dose received, but also the acceptability of the intervention content to influence a behavior change that is essential for understanding the primary outcome of trials (Steckler & Linnan, 2002; French et al., 2020).
In this comparative effectiveness trial, the program staff did not know if participants watched the mailed DVD so we conducted an in-depth process evaluation. The purpose of the process evaluation of the mailed intervention was to determine if participants viewed the DVD, their perceptions of DVD content (whether information was new, helpful, and personally relevant), and participants’ engagement and satisfaction with the DVD. In addition, the process evaluation included whether participants would recommend the DVD to others and if their opinion changed about completing CRC screening. Detailed information about the patient navigation component of the trial is being described elsewhere and is not included in this report since navigation extended well beyond the time of the DVD process evaluation interview. The comparative effectiveness trial to promote CRC screening, including the process evaluation, was funded by the Patient Centered Outcomes Research Institute (PCORI; IHS-1507-31333).
METHODS
Development of CRC Screening Interactive Educational DVD Intervention
With assistance from community advisory board members associated with the trial, an interactive educational DVD was developed entitled “Time to ACT: Approaches to Colon Testing.” The DVD was a refinement of a tablet-based computerized tailored intervention, which was previously developed to promote CRC screening (Rawl et al., 2021). The intent of the DVD was to encourage participants who did not attend a scheduled colonoscopy to complete the procedure. If they were not willing to complete a colonoscopy, the DVD included information about completing a stool blood test (e.g. FIT) as an alternative way to screen for CRC. The DVD content was guided by the Health Belief Model (HBM); a value-expectancy theory (Rosenstock, 1974). For CRC screening, it is the value an individual places on avoiding colon cancer and expects that by completing screening they will prevent cancer or diagnose it in an early stage when it is easier to treat. Thus, the DVD addressed key HBM theoretical constructs by including information to improve knowledge (severity and susceptibility to CRC), messages that addressed health beliefs (screening benefits and barriers), and screening test instructions to improve self-efficacy (confidence about test preparation).
The CRC screening content embedded in the DVD included generic and tailored messages, graphics, animation, video clips, and testimonials intended to support the theoretical constructs (susceptibility, severity, knowledge, benefits, and barriers) related to CRC screening behavior. A professional actor played the role of a physician and men and women of various races and ethnicities who were screening advocates delivered messages and testimonials. The DVD included in this trial was different than previous mailed passive video/DVD interventions because it was interactive and provided tailored messages based on input by the participant using the remote control, and it also included testimonials (narratives), which are strategies that have been shown to change behaviors (Kreuter et al., 2003; Kreuter et al., 2007).
The interactive educational DVD was divided into three main sections with some sections tailored to the individual based on the participant inputting responses to prompts (e.g. barriers to colonoscopy) using the remote control. The first section addressed the importance of CRC screening and included a description of the relevant anatomy, how colon polyps can grow and become cancer, CRC risk factors, screening benefits, and an overview of colonoscopy and FIT.
The next section described the process for colonoscopy (i.e. sedation, potential polyp removal), how to take medicines and modify diet during the bowel prep process, and testimonials by CRC screening advocates about overcoming barriers to complete a colonoscopy. Tailoring during this section of the DVD included participants choosing the type of bowel prep prescribed by their provider (NuLYTELY or MiraLAX). Depending on the chosen bowel prep, the DVD content reviewed the timing of when to complete the different steps in the process of cleaning the bowel. In addition, tailoring of the DVD content in this section was based on a participant’s reported barriers to completing a colonoscopy. The DVD content listed common colonoscopy barriers (embarrassment, bowel injury, pain, cost, prep, transportation issues) and the participant had to respond yes or no to each barrier. If a participant responded “yes” to any of the barriers, a CRC screening advocate provided information to overcome that barrier. Participants could choose to watch the final section of the DVD focused on FIT or go to the message at the end of the DVD.
The third section of the DVD focused on FIT, including how to collect a stool specimen (preparing the toilet, writing name and date on the collection tube), and testimonials to overcome barriers to completing the test. The DVD content in this section was tailored to the participant by listing common FIT barriers (unpleasant to complete, embarrassment, cost) and participants had to respond yes or no to indicate whether each was relevant to them. If a participant responded “yes” to any of the barriers, a screening advocate provided information to overcome that barrier. This section ended with a summary of the advantages and disadvantages of colonoscopy compared to FIT.
The ending of the DVD included a positive message to maintain good health by completing CRC screening. On average, the CRC screening interactive educational DVD required approximately 20 minutes to complete.
Recruitment, Eligibility, and Randomization of Participants for the Comparative Effectiveness Trial
Staff in the endoscopy department generated a weekly list of age-eligible patients who were at average-risk and did not attend their scheduled colonoscopy appointment. Trained research staff sent potential participants an introductory letter, a recruitment brochure, and an information sheet that explained the trial, including the planned evaluation. The Institutional Review Board at Indiana Purdue University Indianapolis approved the trial, including process and outcome evaluation.
One week after mailing the introductory letters and information about the trial, trained recruiters called potentially eligible participants who did not opt-out and explained the requirements of participation, potential risks, compensation, and answered any questions. After determining eligibility, recruiters obtained both verbal informed consent and verbal HIPAA authorization and scheduled a convenient time to conduct the baseline interview. Each potential participant was called up to ten times in an attempt to reach them and reason for refusal was recorded for individuals who declined to participate in the trial.
Eligibility criteria for the comparative effectiveness trial included: 1) being referred and scheduled for a screening colonoscopy but did not attend their scheduled appointment; 2) age of 45 to 75 years old if Black or 50 to 75 years old if not Black (recommended ages for screening colonoscopy); 3) able to speak and read English; and 4) providing consent. Individuals who had completed a FIT with positive results in the past 12 months were eligible since a subsequent colonoscopy is required to complete the CRC screening process. Individuals were excluded for any of the following: 1) a personal history of CRC, adenomatous polyps or conditions that increased CRC risk (ulcerative colitis, Crohn’s disease, or known hereditary syndromes); 2) a family history that increased CRC risk; 3) being up-to-date with CRC screening based upon having a negative FIT in the past 12 months; 4) being unable to speak, read, and write English; and 5) any speech, hearing, cognitive, or vision impairments.
Participants (n=371) were randomized to one of three arms of the trial: 1) mailed CRC screening interactive educational DVD; 2) mailed CRC screening interactive educational DVD plus telephone-based patient navigation by a trained nurse to address individual barriers to completing CRC screening, if needed; or 3) usual care. The primary outcome of this comparative effectiveness trial is completion of CRC screening documented nine months after randomization. This report focuses on the process evaluation conducted among participants randomized to the two intervention arms that included the mailed CRC screening interactive educational DVD to determine the dose received, the acceptability of the intervention content, and if the intervention influenced the participants’ opinion about completing CRC screening, which are important in the assessment of the trial’s primary outcome.
Process Evaluation Recruitment
To assess the CRC screening interactive educational DVD, an attempt was made to contact all participants (n=243) randomized to the two intervention arms from September 2017 to February 2020. Trained interviewers called participants about two weeks after the DVD was mailed to conduct a brief process evaluation interview. At least ten call attempts were made to reach each participant to conduct the process evaluation. If a participant reported not watching the DVD, the main reason for not watching it was documented, a reminder to watch the DVD was provided, and a future time to call to complete the interview was arranged. If needed, we mailed a second DVD or loaned a portable DVD player to participants. Participants were mailed a $50 gift card in appreciation of their time for completing the process evaluation interview.
Process Evaluation Data
Participants’ demographic characteristics (age, gender, race, ethnicity, marital status, education, employment status, annual household income, health insurance, and health literacy (Chew, Bradley & Boyko, 2004)) were obtained from the baseline interview conducted for the trial. The dose received (e.g. the extent that participants used and were engaged with the intervention materials) was evaluated through the telephone interview made by trained interviewers to assess if the participants watched the DVD and to obtain their opinions about the DVD content. Most items were closed-ended and responses included “Don’t know/remember” and “Refused.” Don’t know/remember or refused responses were considered as missing and answers to open-ended questions were entered verbatim.
Each telephone call attempt to conduct the process evaluation interview was documented. When reached, the interviewers asked participants if they recalled receiving the DVD and if they had watched it. Responses were recorded as “Yes, No, Don’t remember, or Refused.” Interviewers documented the main reasons participants gave for not watching the DVD.
Participants were asked whether: 1) the DVD content was helpful (Very helpful, Somewhat helpful, Not very helpful, Don’t remember, Don’t know, Refused); 2) any new CRC or CRC screening information was learned (Yes, No, Don’t know, Refused); and if yes, we asked what information was new to them (open-ended question). To determine if the amount and detail of the CRC screening information was appropriate, participants were asked if the DVD gave them “More information than you would have liked,” “Just the right amount of information,” or “Less information than you would have liked.”
Engagement and satisfaction with the DVD was assessed using modified items from previous research (Skinner et al., 2011). Engagement was assessed using a 4-item scale with responses on a 4-point Likert Scale (Strongly Disagree to Strongly Agree). Engagement items included contemplation of future CRC screening (colonoscopy and FIT), perception of time passing quickly when watching the DVD, and attention to the DVD. Scores were averaged to provide a composite engagement score for each participant.
Satisfaction with the DVD was assessed through a 10-item scale using a 4-point Likert Scale for responses (Strongly Disagree to Strongly Agree). Satisfaction items included: clarity of information, importance, relatability, comfort, personalization, enjoyment when learning about various topics (CRC, colonoscopy, and stool blood test), and quality. Scores were averaged to provide a composite satisfaction score for each participant.
Content relevance was assessed by asking the viewer how much of the DVD applied to them. Responses included “All of the information,” “Most of it,” “Some of it,” or “None of the information applied to you.”
Participants were asked if they would recommend the DVD to others (Yes, No, Not sure, Don’t know, Refused) and the interview ended with the following final question: “As a result of the DVD we sent you, did you change your opinion about having a colon test?” (Yes, No).
Process Evaluation Data Analysis
Descriptive statistics were used to summarize demographic characteristics of participants, viewership, engagement, satisfaction, and the content relevance of the DVD. Demographic characteristics were examined to determine if they differed between participants who viewed the DVD and completed the interview compared to those who did not complete the interview by using a Chi-square test for categorical variables, Fisher’s exact test when there were small cells for categorical variables, and t-test for continuous variables.
Results
Participant Characteristics
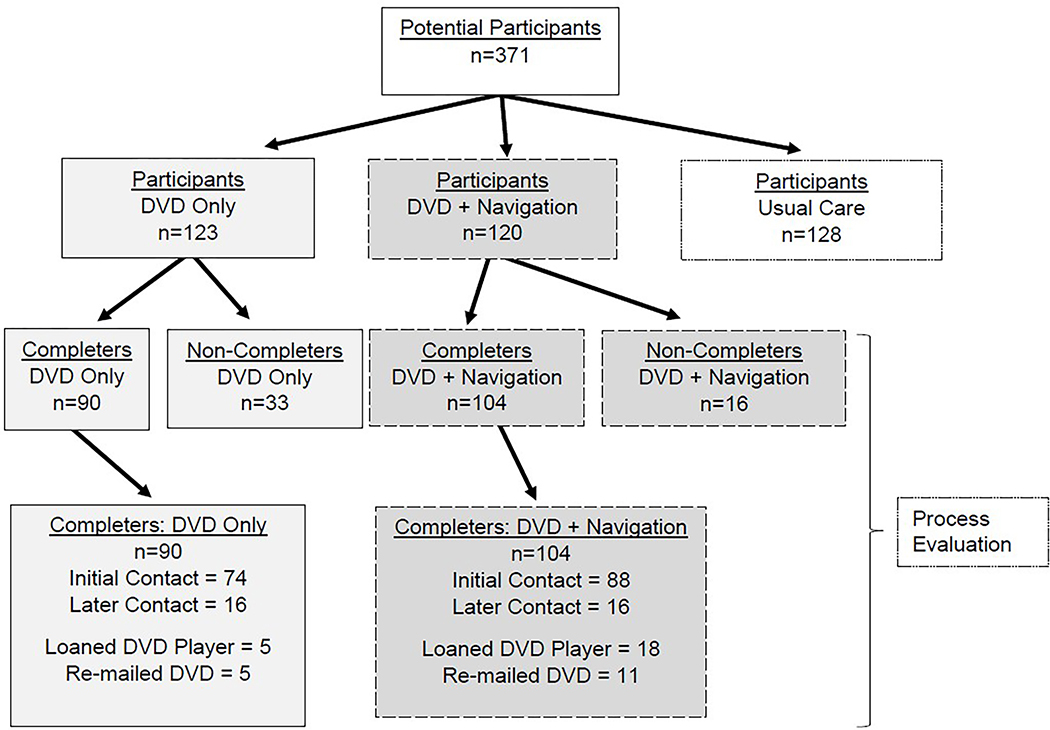
Among 243 participants randomized to the intervention arms of the trial, 194 (80%) viewed the DVD and completed the telephone process evaluation interview and 49 (20%) did not complete the interview (Table 1, Figure 1). Among the 49 participants who did not complete the interview, the majority of participants (n=47) were never reached, one refused, and one was not able to complete the interview.
Table 1.
Demographic characteristics of participants by DVD completion (N=243)
| Completion Status (DVD viewed and interview completed) | ||||
|---|---|---|---|---|
| Characteristic | Total N=243a n (%) | Non-Completer N=49 n (%) | Completer N=194 n (%) | p-value |
| Age Mean (SD) | 57.63 (5.84) | 58.96 (6.62) | 57.29 (5.60) | 0.075 |
| Gender | 0.959 | |||
| Male | 95 (39.1%) | 19 (20.0%) | 76 (80.0%) | |
| Female | 148 (60.9%) | 30 (20.3%) | 118 (79.7%) | |
| Race | 0.657 | |||
| Black or African American | 157 (64.6%) | 33 (21.0%) | 124 (79.0%) | |
| White or Caucasian | 68 (28.0%) | 14 (20.6%) | 54 (79.4%) | |
| Other | 14 (5.8%) | 1 (7.1%) | 13 (92.9%) | |
| Hispanic | 0.756 | |||
| No | 235 (96.7%) | 48 (20.4%) | 187 (79.6%) | |
| Yes | 6 (2.5%) | 1 (16.7%) | 5 (83.3%) | |
| Married/Partnered | 0.831 | |||
| No | 168 (69.1%) | 35 (20.8%) | 133 (79.2%) | |
| Yes | 74 (30.5%) | 14 (18.9%) | 60 (81.1%) | |
| Education | 0.829 | |||
| No school-11 grade | 50 (20.6%) | 12 (24.0%) | 38 (76.0%) | |
| 12th grade/High school/GED | 83 (34.2%) | 15 (18.1%) | 68 (81.9%) | |
| Vocational school-3 years of college | 84 (34.6%) | 16 (19.0%) | 68 (81.0%) | |
| 4-year College/Graduate Degree | 26 (10.7%) | 6 (23.1%) | 20 (76.9%) | |
| Employment | 0.941 | |||
| Not employed | 149 (61.3%) | 29 (19.5%) | 120 (80.5%) | |
| Full-time | 57 (23.5%) | 12 (21.1%) | 45 (78.9%) | |
| Part-time | 37 (15.2%) | 8 (21.6%) | 29 (78.4%) | |
| Health Insurance | 0.496 | |||
| No | 15 (6.2%) | 2 (13.3%) | 13 (86.7%) | |
| Yes | 228 (93.8%) | 47 (20.6%) | 181 (79.4%) | |
| Household Income | 0.859 | |||
| <15K | 102 (42.0%) | 21 (20.6%) | 81 (79.4%) | |
| >=15K | 133 (54.7%) | 27 (20.3%) | 106 (79.7%) | |
| Health Literacy Sum (SD) | 12.09 (2.69) | 12.02 (2.60) | 12.10 (2.72) | 0.847 |
Note: Chi-square test and Fisher’s exact test for categorical variables, t-tests for continuous variables
Health literacy: 3-item brief health literacy screening test (sum scores 3–15; higher numbers = adequate health literacy) [16]
DVD: Digital Video Disc
Missing data included: n=4 for Race, n=1 for Married/partnered, n=8 for Household Income, and n=1 for Health Literacy
Figure 1.
Flow diagram of participants included in process evaluation
Participants (n=194) who completed the interview included 90 randomized to the DVD only arm and 104 to the DVD plus patient navigation arm. Demographic characteristics of the participants are listed in Table 1. Participants who completed the process evaluation interview were not significantly different from participants who did not complete the interview (all p-values>0.05). Overall, participants had a mean age of 57.6 ± 5.8 years. In addition, they were mostly female (61%), non-Hispanic Black (65%), not married/partnered (69%) had less than a college education (89%), were currently unemployed (61%), and had some form of health insurance (94%). In addition, 42% of participants reported having annual household incomes less than $15,000 and adequate health literacy (12.1 on a scale from 3 to 15).
Dose Received: DVD Viewed
Among the participants who watched the DVD and completed the interview, 162 (84%) reported having watched the DVD when initially contacted by the interviewer. Among the 32 (16%) participants who did not watch the DVD when the interviewer first contacted them, the main reasons for reporting not watching the DVD were technical issues with DVD players (n=16), and being too busy or not having the time to watch (n=16). In addition, we sent a second DVD to 16 (8%) and we loaned a DVD player to 23 (12%) participants prior to their interview. To reach each participant, it took interviewers an average of 4.5 attempts. The process evaluation interview on average took nine minutes to complete (range 3 to 21 minutes, SD=3.08 minutes).
DVD Engagement, Relevance, and Satisfaction
Participants (n=193; 99%) reported that the DVD was very or somewhat helpful, and almost half (n=91; 47%) reported that they learned new information including details about the colonoscopy procedure and polyp removal (n=60), general CRC information (e.g. incidence, mortality, age to start screening, symptoms, etc.) (n=31), and information about the FIT test (n=16). Participants reported that the DVD included just the right amount of information (n=144; 75%), while some thought there was too much information (n=45; 23%) and fewer thought there was too little information (n=4; 2%).
Participants reported being engaged (mean score=3.35 out of 4, SD=0.49) with the DVD (Table 2). Only 15 (8%) participants reported having trouble paying attention while watching the DVD. Participants reported being satisfied (mean score=3.42 out of 4, SD=0.39) with the CRC screening educational DVD and most participants (n=149; 77%) agreed that the sounds and images in the DVD were attractive (Table 2).
Table 2.
DVD Engagement and Satisfaction among participants (n=194)
| Percent Agreement* (%) | |
|---|---|
| DVD Engagement | |
| 1. The DVD made me think about having a colonoscopy. | 92 |
| 2. The DVD made me think about doing a stool blood test. | 69 |
| 3. Time passed quickly when I watched the DVD. | 86 |
| 4. I had trouble paying attention to the DVD.** | 8 |
| Mean (SD) of Engagement Score | 3.35 (0.49) |
| DVD Satisfaction | |
| 1. I could understand the information in the DVD. | 99 |
| 2. I enjoyed watching the DVD. | 93 |
| 3. The information I received from the DVD was important to me. | 99 |
| 4. The information in the DVD doesn’t relate to me.** | 16 |
| 5. I was comfortable using the DVD. | 98 |
| 6. The DVD seemed like it was meant just for me. | 61 |
| 7. The DVD was an enjoyable way to learn about colon cancer. | 94 |
| 8. The DVD was an enjoyable way to learn about colonoscopy. | 99 |
| 9. The DVD was an enjoyable way to learn about a stool blood test. | 93 |
| 10. The sounds and images in the DVD were attractive. | 77 |
| Mean (SD) of Satisfaction Score | 3.42 (0.39) |
Percent Agreement includes Agree and Strongly agree on a 4 point scale: Strongly Disagree, Disagree, Agree, Strongly Agree;
Reverse coding
DVD: Digital Video Disc
The majority of participants (n=169; 87%) reported that most or all of the information included in the DVD applied to them, while 30 (16%) participants reported that the information in the DVD did not relate to them. Almost all participants (n=192; 99%) reported that they would recommend the educational DVD to other people. In addition, 87 (45%) participants reported that they changed their opinion about completing a CRC screening test based on the information included in the DVD.
Discussion
The mailed interactive CRC screening educational DVD, “Time to ACT: Approaches to Colon Testing” intervention included information to improve knowledge, address beliefs and barriers to CRC screening, and improve self-efficacy to complete a screening test. Addressing the main theoretical constructs from a well-established health behavior theory and by tailoring messages to an individual’s screening barriers in the intervention was especially important since the participants included in the comparative effectiveness trial had not attended a scheduled colonoscopy appointment.
Overall, participants reported engagement and satisfaction with the DVD, thought the content was important and relevant to them, and believed an appropriate amount of information about CRC screening was included in the intervention. Nearly half of the participants reported that the DVD content had changed their opinion about completing a CRC screening test.
Several participants (n=32, 16%) who completed the process interview reported not watching the DVD when initially contacted. Thus, the planned process evaluation was important since it acted as a check on the dose of the intervention received and provided an opportunity to re-mail the DVD and/or loan the participant a DVD player, if needed. This is an important finding considering the significant resources used to develop and distribute the intervention. In addition, this finding is important because it provides evidence to explain why a mailed intervention may fail to change an individual’s behavior.
In general, process evaluation addresses the participant’s exposure to the intervention and may assist in explaining the factors contributing to the success or failure of the primary outcome of the intervention (Steckler & Linnan, 2002; French et al., 2020). Reports of previous process evaluation for mailed DVD interventions to increase CRC screening provide limited information (Zapka et al., 2004; Cameron et al., 2011; Levy et al., 2012). Participants who were reached or responded to a post-education interview or survey ranged from 34.7% to 95.5%; and among those contacted and reported receiving the intervention materials, the participants who watched the video/DVD ranged from 30% to 67% (Zapka et al., 2004; Cameron et al., 2011; Levy et al., 2012). Additional information documented during the process evaluation varied by these previously mailed CRC video/DVD interventions. Participants who watched the video/DVD reported more discussion with providers about screening and completed a sigmoidoscopy (Zapka et al., 2004). Reasons for not watching the DVD included no time/too busy, not interested, and lack of a DVD player or not able to use one by Cameron and colleagues (2011). Levy and colleagues (20212) documented that most participants reported the amount of information in the DVD was just right and 61% of participants reported that the information helped them make the decision about which CRC screening test to complete (Levy et al., 2012).
The key components of the process evaluation addressed in the current trial included the dose received, the participants’ engagement and satisfaction with the intervention, its acceptability and relevance, and if the content changed their opinion about CRC screening. Conducting the process evaluation interview shortly after mailing the intervention provided an opportunity for the staff to address technical issues (e.g. send a loaner DVD player if needed), and thus increased the number of participants who reported that they watched the DVD. This action may have an effect on the trial’s primary outcome of completing CRC screening because more participants watched the DVD, which may have improved their knowledge and the tailored messages based on input from each individual addressed their barriers to screening. This information will be critical to consider when conducting the analysis of the final primary outcome data from the trial. In addition, this information is important for clinical practice as more mailed CRC screening programs are being used to increase screening among vulnerable populations (Gupta et al., 2020).
The strengths of this detailed process evaluation include being a planned component of the comparative effectiveness trial. This is critical since it is important to consider both the participant burden and resources needed to conduct the process evaluation and analyze the data. In addition, the process evaluation was conducted a short time after the mailed DVD allowing a second DVD to be mailed or a DVD player to be loaned to participants to watch the DVD, if needed. The current process evaluation determined the intervention dose received for the mailed intervention, and furthermore included assessment of the participants’ engagement, content relevance, and satisfaction with the educational material. This information is important to consider when focusing on the primary outcome of the trial and prior to dissemination of the intervention.
Limitations of this process evaluation include the lack of being able to contact all participants to collect information about dose received. Those who did not watch the DVD or who did not like the DVD may have been less likely to complete the interview. In addition, since it was not possible to directly observe the participants’ exposure to the DVD, the process data obtained is based on the self-report of viewing the DVD. As a final point, the evaluation of the patient navigation component of the trial is not included in this report because it was conducted six months after mailing the DVD intervention.
Implications for Research and Practice
Significant resources were devoted to develop and disseminate the interactive educational DVD used in this trial. Consequently, this report highlights the importance of conducting process evaluation for mailed interventions and has implications for interventions not conducted in-person. The process evaluation interview was able to be delayed after reminding 16% of participants to watch the DVD or assist them with their technology issues after initially contacting them. This information will be important to consider in the evaluation of the trial’s primary outcome of completing CRC screening.
Implications for research and practice suggest that it is important to develop strategies to address logistical problems when planning and implementing mailed interventions. In the real world setting, it is important to have a plan for technological issues (e.g. loaner DVD player) when implementing mailed interventions that include a DVD or to have plans for digital limitations for online educational interventions. A recent summary of mailed FIT interventions makes suggestions for several components (e.g. notification primer, simple instructions for individuals with limited literacy, reminders to patients who do not complete screening) to include in an outreach program to increase CRC screening (Gupta et al., 2020). We think it is especially important to include process evaluation when planning multi-component mailed interventions to promote CRC screening, not only to check the dose of the intervention received but also to evaluate whether the content is relevant to the population. When conducting research or in practice, using community-engaged strategies when developing interventions usually addresses the content relevance and determines the best channel for intervention delivery. However, it is critical to check on these issues by using process evaluation so that any needed modifications may be addressed prior to dissemination of an evidence-based intervention.
Funding:
Patient Centered Outcomes Research Institute (PCORI; IHS-1507-31333, Rawl, PI). Caeli Malloy was supported by training grant number 1T32NR018407 from the National Institute of Nursing Research.
Footnotes
Conflict of Interest: None
Contributor Information
Mira L. Katz, College of Public Health, The Ohio State University, Columbus, Ohio.
Brent Emerson, College of Public Health, The Ohio State University, Columbus, Ohio.
Victoria L. Champion, School of Nursing, Indiana University, Indianapolis, Indiana.
Peter H. Schwartz, School of Medicine, Indiana University, Indianapolis, Indiana.
Thomas F. Impleriale, School of Medicine, Indiana University, Indianapolis, Indiana.
Hala Fatima, School of Medicine, Indiana University, Indianapolis, Indiana.
Electra D. Paskett, College of Medicine, The Ohio State University, Columbus, Ohio.
Susan M. Perkins, School of Medicine, Indiana University, Indianapolis, Indiana.
Yan Tong, School of Medicine, Indiana University, Indianapolis, Indiana.
Netsanet Gebregziabher, School of Medicine, Indiana University, Indianapolis, Indiana.
Connie Krier, School of Nursing, Indiana University, Indianapolis, Indiana.
Kevin Tharp, Research Technologies for the Center for Survey Research, Indiana University, Bloomington, Indiana.
Caeli Malloy, School of Nursing, Indiana University, Indianapolis, Indiana.
Sylvia Strom, Community Advisory Board Member, Indianapolis, Indiana.
Susan M. Rawl, School of Nursing, Indiana University, Indianapolis, Indiana and member of the Indiana University Melvin and Bren Simon Comprehensive Cancer Center.
References
- American Cancer Society Colorectal Cancer Facts & Figures 2020–2022. (2020). Atlanta, GA, American Cancer Society. [Google Scholar]
- Bhise V, Modi V, Kalavar A, Espadas D, Hanser L, Gould M, et al. (2016). Patient-reported attributions for missed colonoscopy appointments in two large healthcare systems. Dig Dis Sci, 61, 1853–1861. 10.1007/s10620-016-4096-3. [DOI] [PubMed] [Google Scholar]
- Blake KD, Thai C, Falisi A, Chou W-YS, Oh A, Jackson D, et al. (2020). Video-based interventions for cancer control: A systematic review. Health Educ Behav, 47, 249–257. [DOI] [PubMed] [Google Scholar]
- Cameron KA, Persell SD, Brown T, Thompson J, & Baker DW (2011). Patient outreach to promote colorectal cancer screening among patients with an expired order for colonoscopy. A randomized controlled trial. Arch Intern Med, 171, 642–646. [DOI] [PubMed] [Google Scholar]
- Chew LD, Bradley KA, & Boyko EJ (2004). Brief questions to identify patients with inadequate health literacy. Fam Med, 36, 588–594. [PubMed] [Google Scholar]
- DeGroff A, Schroy PC, Morrissey KG, Slotman B, Rohan EA, Bethel J, Murillo, et al. (2017). Patient navigation for colonoscopy completion: Results of an RCT. Am J Prev Med, 53, 363–372. 10.1016/j.amepre.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French C, Pinnock H, Forbes G, Skene I, & Taylor SJC. (2020). Process evaluation within pragmatic randomised controlled trials: what is it, why is it done, and can we find it? -a systematic review. BMC, 21, 916. 10.1186/s13063-020-04762-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Coronado GD, Argenbright K, Benner AT, Castaneda SF, Dominitz JA et al. (2020). Mailed fecal immunochemical test outreach for colorectal cancer screening: Summary of a Centers for Disease Control and Prevention-sponsored Summit. CA Cancer J Clin, 70, 283–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy GP Jr., Richardson LC, Pignone MP, & Plescia M (2014). Costs and benefits of an organized fecal immunochemical test-based colorectal cancer screening program in the United States. Cancer, 120(15), 2308–2315. 10.1002/cncr.28724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klabunde CN, Vernon SW, Nadel MR, Breen N, Seef LC, & Brown ML (2005). Barriers to colorectal cancer screening: a comparison of reports from primary care physicians and average-risk adults. Med Care, 43, 939–944. 10.1097/01.mlr.0000173599.67470.ba. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Green MC, Capella JN, Slater MD, Wise ME, Storey D, et al. (2007). Narrative communication in cancer prevention and control: A framework to guide research and application. Ann Behav Med, 33, 221–235. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, & Wray RJ (2003). Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav, 27 Suppl3:S227–S232. [DOI] [PubMed] [Google Scholar]
- Levy BT, Daly JM, Xu Y, & Ely JW (2012). Mailed fecal immunochemical tests plus educational materials to improve colon cancer screening rates in Iowa Research Network (IRENE) practices. J Am Board Fam Med, 25, 73–82. [DOI] [PubMed] [Google Scholar]
- McLachlan SA, Clements A, & Austoker J (2012). Patients’ experiences and reported barriers to colonoscopy in the screening context—a systematic review of the literature. Patient Educ Counsel, 86,137–146. 10.1016/j.pec.2011.04.010. [DOI] [PubMed] [Google Scholar]
- Meester RG, Doubeni CA, Zauber AG, Goede SL, Levin TR, Corley DA, et al. (2015). Public health impact of achieving 80% colorectal cancer screening rates in the United States by 2018. Cancer, 121, 2281–2285. 10.1002/cncr.29336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers RE, Sifri R, Daskalaskis C, DiCarlo M, Geethakumari PR, Cocroft J et al. (2014). Increasing colon cancer screening in primary care among African Americans. JNCI, 106, dju344. 10.1093/jnci/dju344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawl SM, Christy SM, Perkins SM, Tong Y, Krier C, Wang HL, et al. (2021). Computer-tailored intervention increases colorectal cancer screening among low-income African Americans in primary care. Prev Med, 145, E-pub ahead of print. 10.1016/j.ypmed.2021.106449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM (1974), The Health Belief Model and preventive health behavior. Health Education Monographs 2, 354–386. [DOI] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, Fuchs HE, & Jemal A (2021), Cancer Statistics, 2021. CA Cancer J Clin, 7, 7–33. 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- Skinner CS, Buchanan A, Champion V, Monahan P, Rawl S, Springston J, Qianqian Z, & Bourff S (2011). Process outcomes from a randomized controlled trial comparing tailored mammography interventions delivered via telephone vs. DVD. Patient Education and Counseling, 85(2), 308–312. 10.1016/j.pec.2010.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steckler A & Linnan L (Eds.) (2002). Process evaluation for public health interventions and research. San Francisco, CA: John Wiley & Sons, Inc. [Google Scholar]
- United States Preventive Services Task Force. (2016). Screening for colorectal cancer. US Preventive Services Task Force Recommendation Statement. JAMA, 315, 2564–2575. [DOI] [PubMed] [Google Scholar]
- Zapka JG, Lemon SC, Puleo E, Estabrook B, Luckmann R, Erban S (2004). Patient education for colon cancer screening: A randomized trial of a video mailed before a physical examination. Ann Intern Med, 141, 683–692. [DOI] [PubMed] [Google Scholar]
- Zauber AG (2010). Cost-effectiveness of colonoscopy. Gastrointest Endosc Clin N Am, 20(4), 751–770. 10.1016/j.giec.2010.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]