Abstract
BACKGROUND AND AIMS:
Uniportal thoracoscopic surgery has been reported to result in alleviating the postoperative pain when compared with traditional video-assisted thoracoscopic surgery (VATS). However, postoperative pain is still the main concerns associated with thoracic surgeries. The objective of this study is to evaluate the postoperative pain of patients undergoing uniportal VATS, especially wedge resection, with the use of intraoperative intercostal nerve block.
METHODS:
All consecutive patients undergoing the uniportal VATS wedge resection between January 2019 and March 2020 were reviewed retrospectively. Twenty consecutive patients in Group A underwent the uniportal VATS wedge resection without intraoperative intercostal nerve block. The other 20 consecutive patients in Group B underwent the uniportal VATS wedge resection with intraoperative intercostal nerve block. The numeric pain rating scale (NRS) scores were recorded at 1, 12, and 24 h, postoperatively. The number of opioid consumption was also recorded until the time to chest tube removal.
RESULTS:
There was no difference between groups with regard to sex, age, chest tube duration, length of stay, operative time, laterality time, and diagnosis. There was a significant difference in postoperative NRS scores at 1 h (P = 0.001) and 12 h (P = 0.022) between the groups. The opioid consumption was significantly in Group B lower than those in Group A (P = 0.025).
CONCLUSION:
The intraoperative intercostal nerve block with bupivacaine provided immediate postoperative pain relief with reducing the postoperative opioid consumption compared in patients who underwent uniportal VATS, especially wedge resection of the lung.
Keywords: Intercostal nerve block, pain, postoperation, uniport, uniportal video-assisted thoracoscopic surgery, wedge resection
In the field of thoracic surgery, video-assisted thoracoscopic surgery (VATS) has become the favored approach since VATS has an advantage in alleviating the postoperative pain when compared with thoracotomy.[1] Recently, a number of surgeons have demonstrated the feasibility of performing a VATS though a single incision. In comparison with multiport VATS, uniportal VATS has demonstrated favorable outcomes to date.[2,3,4,5] Despite this refined technique, patients are still suffering from postoperative pain associated with thoracic surgeries. Several methods such as local analgesia, thoracic epidural block, paravertebral block, and intercostal nerve block were suggested for the treatment of VATS postoperative pain. Bolotin et al. have demonstrated the utility of the advantage of the thoracoscopic internal intercostal block.[6] The objective of this retrospective observational study is to evaluate the postoperative pain of patients undergoing uniportal VATS, especially wedge resection, with the use of intraoperative intercostal nerve block.
Methods
Patients
The patients were divided into two groups. In Group A, 20 consecutive patients underwent the elective uniportal VATS wedge resection without intraoperative intercostal nerve block between January 2019 and October 2019. In Group B, 20 consecutive patients underwent the elective uniportal VATS wedge resection with intraoperative intercostal nerve block between November 2019 and March 2020. Until October 2019, except for intraoperative intercostal nerve block, 20 patients who underwent uniportal VATS wedge resection by the same surgeon with the same other conditions belonged to Group A. The reason that patients who underwent wedge resection from November 2019 belonged to group B is because intercostal nerve block was performed intraoperatively from November 2019 at our hospital. If the patient had additional analgesic requirement postoperatively, tramadol 50 mg was injected when numeric pain rating scale (NRS) score was more than 6. The NRS is a numeric version of the visual analog scale. Patients can select a number from 0 to 10 integers that can reflect the intensity of their pain appropriately (0 being no pain and 10 being worst pain imaginable). The NRS needs minimal language translation and is widely used in South Korea. During the postoperative period, patient's pain level was assessed by NRS scores, which was the primary outcome. The NRS scores were recorded at 1, 12, and 24 h, postoperatively. The secondary outcomes were the number of opioid consumption until the time to chest tube removal. This retrospective study was approved by the Institutional Review Board of Haeundae Paik Hospital at the Inje University of Korea.
Surgical technique: Uniportal video-assisted thoracoscopic surgery
In both groups, a single port was made in the fifth intercostal space on the anterior axillary line. Soft tissue and intercostal muscles were retracted with a small X-shaped wound retractor to secure the intercostal space and protect the intercostal neurovascular bundle. All procedures were performed with a 5-mm, 30 video thoracoscope, placenta forceps, and an endoscopic linear stapler. At the end of the procedure, a chest tube (20 Fr.) was placed in the thoracic cavity. The chest tube was inserted through a single incision [Figure 1].
Figure 1.
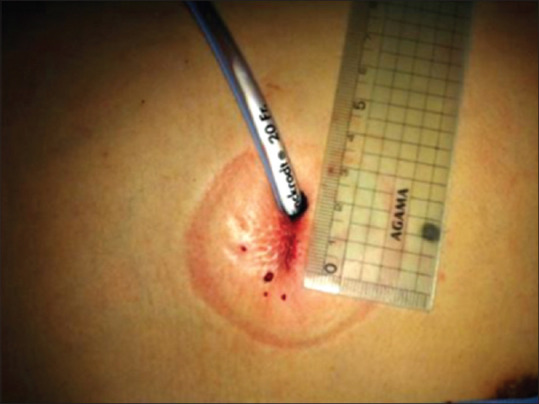
Surgical wound after uniportal video-assisted thoracoscopic surgery
Intraoperative internal intercostal nerve block
At the end of VATS wedge resection, a 23-gauge scalp needle was introduced through the uniport. According to the need, the scalp needle was bent about 30°. The injection of 5 cc of 0.5% bupivacaine HCl 0.5% was done under the parietal pleura in the region of the intercostal bundle after careful aspiration. The location of the injection was from the third to seventh intercostal space lateral to the sympathetic chain. We injected 25cc bupivacaine in total. A bulge of the parietal pleura and bleeding was monitored through the thoracoscope.
Statistical analysis
Continuous variables were presented with a median and interquartile range for nonnormally distributed data and mean ± standard deviation for normally distributed data. To compare continuous variables, the Mann–Whitney's U-test was used. Categorical variables were presented with number and percentage. To compare categorical variables, the Chi-square test or Fisher's exact test was used. The statistical analysis was conducted using SPSS (Version window 26.0; SPSS Inc., Chicago, USA). For all analyses, statistical significance was set at P < 0.05.
Results
A total of 40 patients undergoing wedge resection using uniportal VATS were included in this analysis. The Group B 20 patients received intraoperative intercostal nerve block using 0.5% bupivacaine HCl 0.5% at the end of the surgery, whereas the remaining Group A 20 patients did not receive intraoperative intercostal nerve block. The patients’ demographics included sex, age, chest tube duration, length of stay, operative time, laterality time, and diagnosis. There were no significant differences between both groups [Table 1].
Table 1.
Patient characteristics
| Characteristics | Group A (n=20) | Group B (n=20) | P |
|---|---|---|---|
| Sex | |||
| Male, n(%) | 19 (95.0) | 17 (85.0) | 0.605 |
| Age (years) | 29.70 (20-34) | 31.60 (19-42) | 0.748 |
| Chest tube duration (h) | 72.50 (53.38-91.38) | 86.15 (47.0-93.63) | 0.406 |
| Length of stay (days) | 4.00 (3.00-4.75) | 4.35 (3.00-5.75) | 0.624 |
| Operative time (min), mean±SD | 43.50±21.03 | 48.50±25.08 | 0.499 |
| Laterality, n (%) | |||
| Left | 10 (50.0) | 9 (45.0) | 0.752 |
| Diagnosis, n (%) | |||
| Pneumothorax | 19 (95.0) | 18 (90.0) | - |
| Metastasis | - | 1 (5.00) | - |
| Benign disease | 1 (5.00) | 1 (5.00) | - |
*Values in parentheses are interquartile range or %. SD=Standard deviation
Postoperative NRS scores are shown in Table 2. There was a significant difference in postoperative NRS scores at 1 h and 12 h later between the two groups. The number of postoperative analgesics injection until the time to chest tube removal is shown in Table 3. The opioid consumption until the time to chest tube removal was significantly lower in Group B than those in Group A.
Table 2.
Postoperative numeric pain rating scale scores
| Time after surgery | Group A (n=20) | Group B (n=20) | P |
|---|---|---|---|
| 1 h | 5.60±1.31 | 4.10±1.45 | 0.001 |
| 12 h | 5.00±1.41 | 3.80±1.74 | 0.022 |
| 24 h | 3.80±0.89 | 3.35±1.23 | 0.193 |
*Values are presented as mean±SD of numeric pain score. SD=Standard deviation
Table 3.
Postoperative analgesics usage
| Number of injections (mean±SD) | Group A (n=20) | Group B (n=20) | P |
|---|---|---|---|
| Opioid | 1.15±1.31 | 0.40±0.60 | 0.025 |
*Values are presented as mean±SD of injection number. SD=Standard deviation
Discussion
Despite the advantages over the thoracotomy, VATS could still induce significant postoperative pain and temporary impairment of lung function. There have been various efforts to alleviate VATS postoperative pain: local analgesia, general intravenous analgesia, epidural block, and intercostal nerve block.[7] Bolotin et al. reported a significant advantage of intercostal nerve block for pain management after thoracoscopic surgery.[6] The advantage of the intraoperative intercostal nerve block is the accuracy of the block. The injection of local anesthetics is performed under direct vision, and a bulge of the parietal pleura could be seen over the intercostal space. Temes et al. reported a thoracoscopic nerve block supplying the intercostal spaces entered.[8] However, it could not be done under direct vision, and immediate leak of the local anesthetics through the damaged parietal pleura would occur. In our study, the injection was done at multiple levels: from the third to seventh intercostal space to alleviate the pain caused by the uniport performed through the fifth intercostal space.
Because there have been several reports demonstrating the feasibility of the uniportal VATS, this technique has been adopted by several centers in Europe and Asia. Beginning in 2011, our hospital adopted uniportal VATS, and it is currently used as a standard means of minimal invasive thoracic surgery. To improve on the results of the uniportal VATS, we thought that appropriate postoperative pain would be very important. In our study, a decrease of immediate postoperative pain, which was assessed at 1 and 12 h postoperatively was achieved using an intraoperative intercostal nerve block. Furthermore, postoperative opioid consumption until the time to chest tube removal was also decreased in the intraoperative intercostal nerve block using group.
This study has several limitations. First, this study is a retrospective study based on relatively small cohort from a single institution. To evaluate the efficacy of intraoperative intercostal nerve block in the uniportal VATS, a larger multi-institutional prospective study may be necessary. Second, our study only investigated the immediate postoperative period, so we could not recognize the development of chronic pain. Third, for methodological reasons, we performed intraoperative intercostal nerve block on wedge resection cases. Therefore, this technique needs to be applied for a variety of procedures including anatomic resections and other major thoracic procedures. To minimize potential bias in a retrospective study, all procedures were performed by a single surgeon.
In conclusion, intraoperative intercostal nerve block with bupivacaine during the uniportal VATS, especially wedge resection of the lung, could alleviate the immediate postoperative pain.
Conclusion
The results of our retrospective study showed that the intraoperative intercostal nerve block with bupivacaine provided immediate postoperative pain relief with reducing the postoperative opioid consumption in patients who underwent uniportal VATS, especially wedge resection of the lung.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nagahiro I, Andou A, Aoe M, Sano Y, Date H, Shimizu N. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: A comparison of VATS and conventional procedure. Ann Thorac Surg. 2001;72:362–5. doi: 10.1016/s0003-4975(01)02804-1. [DOI] [PubMed] [Google Scholar]
- 2.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg. 2004;77:726–8. doi: 10.1016/S0003-4975(03)01219-0. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Rivas D, Paradela M, Fernandez R, Delgado M, Fieira E, Mendez L, et al. Uniportal video-assisted thoracoscopic lobectomy: Two years of experience. Ann Thorac Surg. 2013;95:426–32. doi: 10.1016/j.athoracsur.2012.10.070. [DOI] [PubMed] [Google Scholar]
- 4.Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: A retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg. 2016;49(Suppl 1):i37–41. doi: 10.1093/ejcts/ezv320. [DOI] [PubMed] [Google Scholar]
- 5.Yang Z, Shen Z, Zhou Q, Huang Y. Single-incision versus multiport video-assisted thoracoscopic surgery in the treatment of lung cancer: A systematic review and meta-analysis. Acta Chir Belg. 2018;118:85–93. doi: 10.1080/00015458.2017.1379800. [DOI] [PubMed] [Google Scholar]
- 6.Bolotin G, Lazarovici H, Uretzky G, Zlotnick AY, Tamir A, Saute M. The efficacy of intraoperative internal intercostal nerve block during video-assisted thoracic surger on postoperative pain. Ann Thorac Surg. 2000;70:1872–5. doi: 10.1016/s0003-4975(00)01757-4. [DOI] [PubMed] [Google Scholar]
- 7.Mulder DS. Pain management principles and anesthesia techniques for thoracoscopy. Ann Thorac Surg. 1993;56:630–2. doi: 10.1016/0003-4975(93)90933-9. [DOI] [PubMed] [Google Scholar]
- 8.Temes RT, Won RS, Kessler RM, Wernly JA. Thoracoscopic intercostal nerve block. Ann Thorac Surg. 1995;59:787–8.8. doi: 10.1016/s0003-4975(99)80014-9. [DOI] [PubMed] [Google Scholar]


