Abstract
Atrial fibrillation/flutter (AF) and COVID-19 are associated with an elevated risk of arterial and venous thrombosis. Whether preadmission oral anticoagulation (OAC) for AF reduces the incidence of in-hospital death or thrombotic events among patients with COVID-19 is unknown. We identified 630 patients with pre-existing AF and a hospitalization diagnosis of COVID-19 and stratified them according to preadmission OAC use. Multivariable logistic regression was employed to relate preadmission OAC to composite in-hospital mortality or thrombotic events. Unadjusted composite in-hospital mortality or thrombotic complications occurred less often in those on than not on preadmission OAC (27.1% vs 46.8%, p <0.001). After adjustment, the incidence of composite in-hospital all-cause mortality or thrombotic complications remained lower with preadmission OAC (odds ratio 0.37, confidence interval 0.25 to 0.53, p <0.0001). Secondary outcomes including all-cause mortality (16.3% vs 24.9%, p = 0.007), intensive care unit admission (14.7% vs 29.0%, p <0.001), intubation (6.4% vs 18.6%, p <0.001), and noninvasive ventilation (18.6% vs 27.5%, p = 0.007) occurred less frequently, and length of stay was shorter (6 vs 7 days, p <0.001) in patients on than those not on preadmission OAC. A higher CHA2DS2-VASc score was associated with an increased risk of thrombotic events. In conclusion, among patients with baseline AF who were hospitalized with COVID-19, those on preadmission OAC had lower rates of death, arterial and venous thrombotic events, and less severe COVID-19.
Atrial fibrillation/flutter (AF) are the most commonly encountered cardiac dysrhythmias in the United States.1 AF is associated with an increased risk of arterial and venous thromboembolism. Risk scores, such as CHA2DS2- -VASc, have been developed and validated to predict arterial thromboembolic events in patients with AF,2 and oral anticoagulation (OAC) with either a direct oral anticoagulant (DOAC) or vitamin K antagonist (VKA) reduces the incidence of these events among those at elevated risk.3, 4, 5 COVID-19 is associated with micro- and macrovascular arterial and venous thrombosis, with meta-analytic data suggesting that thrombotic complications occur in 22% of hospitalized patients and 43% of those admitted to an intensive care unit (ICU) with COVID-19.6 The risk of mortality7 , 8 and thromboembolic complications9 is higher among patients with COVID-19 who also have AF. Whether preadmission OAC reduces in-hospital arterial and venous thrombosis in patients with COVID-19 and pre-existing AF remains to be established.10 We related preadmission OAC used to incident death or thrombotic events among consecutive patients with AF admitted with COVID-19 to a large New England health system.
Methods
Data on demographics, co-morbidities, CHA2DS2−VASc score, vital signs, test results, treatments, and outcomes were extracted from the Epic electronic health record using automated queries. The Charlson co-morbidity index was calculated for each patient using International Classification of Diseases, Tenth Revision (ICD-10) codes.11
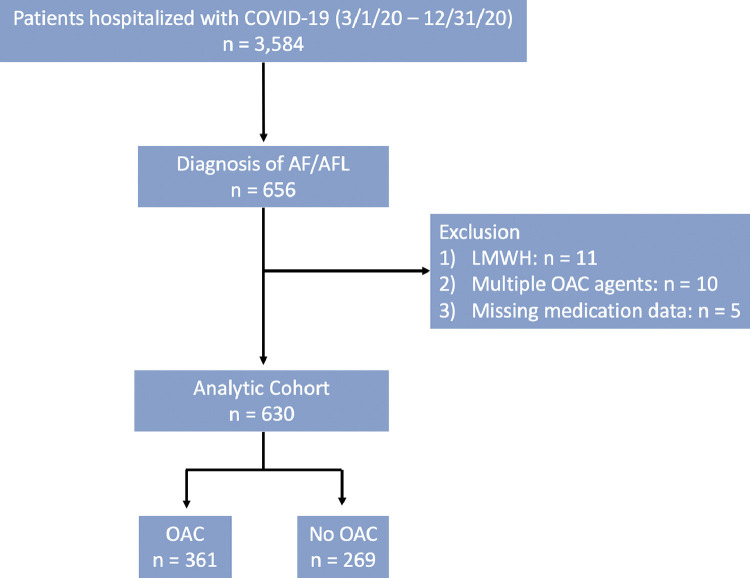
A study flow is shown in Figure 1. All patients ≥18 years of age with a history of AF admitted to Rhode Island, The Miriam, or Newport Hospital with a diagnosis of COVID-19 between March 1 and December 31, 2020, were included. The cohort was restricted to patients with AF to limit the impact of confounding by indication for anticoagulation given their persistently elevated thrombotic risk and a common indication for OAC.12 , 13 Patients on preadmission low molecular weight heparin, multiple anticoagulants, or who were missing information on preadmission OAC use were excluded. Co-morbidities, COVID-19 status, and in-hospital outcomes were ascertained using ICD-10 codes and discharge disposition (Supplementary Table 1). The study was approved by The Lifespan - Miriam Hospital Institutional Review Board and a waiver of informed consent was granted.
Figure 1.
Study Flowchart. 3,584 patients were admitted with COVID-19 between 3/1/20–12/31/20. After applying exclusion criteria, 630 of these had atrial fibrillation or flutter (AF), of which 361 (57%) were single-agent OAC users, and 269 (43%) were non-OAC users.
Patients were classified according to whether they were prescribed a DOAC including apixaban, rivaroxaban, edoxaban, dabigatran, or the VKA, warfarin, before admission for the primary analysis. In secondary analysis, the CHA2DS2-VASc score was related to study outcomes. The calculation of this score is detailed in supplementary data. Supplementary Tables 2 to 4.
The primary outcome of interest was a composite of in-hospital all-cause mortality or arterial or venous thrombotic events. Arterial events included acute coronary syndrome (unstable angina, non–ST-elevation myocardial infarction, and ST-elevation myocardial infarction), transient ischemic attack (TIA), acute ischemic stroke, acute limb ischemia, and acute mesenteric ischemia. Venous thromboembolism included acute deep vein thrombosis (DVT) and acute pulmonary embolism (PE). Secondary end points included the individual components of the primary outcome, admission to an ICU, invasive or noninvasive ventilation, the requirement for supplemental oxygen, cardiac arrest, red blood cell transfusion, major bleeding, length of stay, and discharge disposition.
Continuous variables appear as mean ± SD or medians with interquartile ranges, depending on their distribution. Categorical variables were reported as counts with percentages and compared with Mantel-Haenszel chi-square or Fisher's exact test, as appropriate. Student's t test or Mann-Whitney U test were employed for unadjusted comparisons of these data, respectively. Plausible demographic and clinical characteristics that were related to the primary outcome (p ≤0.15) were entered into a multivariable logistic regression model, along with an indicator variable for preadmission OAC (Supplementary Table 5). A sensitivity analysis was applied to the AF subtype (permanent > persistent > paroxysmal) to examine the association of AF with the primary outcome. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, North Carolina) and R statistical software version 4.0.3 (The R Project for Statistical Computing, Vienna, Austria). A p <0.05 was considered significant.
Results
During the study interval, 3,584 patients were admitted with COVID-19. Of these, 656 patients had a history of AF. After excluding patients who were on outpatient low molecular weight heparin (n = 11), multiple OAC agents (n = 10), or who were missing data regarding OAC therapy (n = 5), the final study cohort comprised 630 patients, of which 361 (57.3%) were prescribed outpatient OAC. Baseline demographic and clinical characteristics, stratified by preadmission OAC use, are shown in Table 1 . Patients on preadmission OAC had a higher prevalence of demographic and co-morbid characteristics associated with adverse outcomes during hospitalization for COVID-19.14 , 15 Patients on preadmission OAC were older, more frequent tobacco users, more often Hispanic, and more likely to have a history of heart failure, myocardial infarction, TIA, stroke, DVT, PE, chronic kidney disease, and cancer, and were less likely to have a history of alcohol use disorder. These patients were also less likely to be taking aspirin or a P2Y12 inhibitor, and more likely to be on a statin before admission when compared with those who were not taking OAC. The median CHA2DS2−VASc score was significantly higher among those on vs not on preadmission OAC (3 vs 2, p <0.001).
Table 1.
Baseline demographic and clinical characteristics
| Variable | Total(N = 630) | Anticoagulation |
p Value | |
|---|---|---|---|---|
| Yes (N = 361) | No (N = 269) | |||
| Age (years) | 77.4 ± 11.8 | 78.5 ± 10.6 | 75.9 ± 13.2 | 0.005 |
| Men | 354 (56.2%) | 206 (57.1%) | 148 (55.0%) | 0.61 |
| Body mass index (kg/m2) | 29.1 ± 7.8 | 29.2 ± 7.8 | 28.8 ± 7.9 | 0.59 |
| Race | ||||
| Black | 47 (7.5%) | 19 (5.3%) | 28 (10.4%) | 0.10 |
| White | 495 (78.6%) | 295 (81.7%) | 200 (74.3%) | |
| Asian | 6 (1.0%) | 4 (1.1%) | 2 (0.7%) | |
| Other | 77 (12.2%) | 41 (11.4%) | 36 (13.4%) | |
| Unknown | 5 (0.8%) | 2 (0.6%) | 3 (1.1%) | |
| Hispanic or Latino ethnicity | 75 (11.9%) | 35 (9.7%) | 40 (14.9%) | 0.029 |
| Smoking status | ||||
| Current | 33 (5.2%) | 18 (5.0%) | 15 (5.6%) | < 0.001 |
| Former | 296 (47.0%) | 190 (52.6%) | 106 (39.4%) | |
| Never | 240 (38.1%) | 135 (37.4%) | 105 (39.0%) | |
| Unknown | 61 (9.7%) | 18 (5.0%) | 43 (16.0%) | |
| Hypertension | 542 (86.0%) | 311 (86.1%) | 231 (85.9%) | 0.92 |
| Hyperlipidemia | 398 (63.2%) | 229 (63.4%) | 169 (62.8%) | 0.88 |
| Diabetes mellitus | 280 (44.4%) | 158 (43.8%) | 122 (45.4%) | 0.69 |
| Ischemic heart disease | 346 (54.9%) | 203 (56.2%) | 143 (53.2%) | 0.44 |
| History of myocardial infarction | 95 (15.1%) | 64 (17.7%) | 31 (11.5%) | 0.031 |
| History of peripheral artery disease | 7 (1.1%) | 4 (1.1%) | 3 (1.1%) | 0.99 |
| Heart failure | 310 (49.2%) | 200 (55.4%) | 110 (40.9%) | < 0.001 |
| Valvular heart disease | 91 (14.4%) | 59 (16.3%) | 32 (11.9%) | 0.12 |
| History of TIA or stroke | 92 (14.6%) | 62 (17.2%) | 30 (11.2%) | 0.034 |
| Chronic obstructive pulmonary disease | 83 (13.2%) | 55 (15.2%) | 28 (10.4%) | 0.08 |
| Chronic kidney disease | 178 (28.3%) | 113 (31.3%) | 65 (24.2%) | 0.049 |
| End stage kidney disease | 51 (8.1%) | 23 (6.4%) | 28 (10.4%) | 0.07 |
| Chronic anemia | 90 (14.3%) | 47 (13.0%) | 43 (16.0%) | 0.29 |
| Liver disease | 57 (9.0%) | 26 (7.2%) | 31 (11.5%) | 0.06 |
| Alcohol use disorder | 23 (3.7%) | 7 (1.9%) | 16 (5.9%) | 0.007 |
| Obstructive sleep apnea | 81 (12.9%) | 48 (13.3%) | 33 (12.3%) | 0.70 |
| Cancer | 84 (13.3%) | 57 (15.8%) | 27 (10.0%) | 0.035 |
| Inflammatory rheumatic disease | 118 (18.7%) | 77 (21.3%) | 41 (15.2%) | 0.05 |
| History of deep vein thrombosis | 31 (4.9%) | 23 (6.4%) | 8 (3.0%) | 0.05 |
| History of pulmonary embolism | 24 (3.8%) | 23 (6.4%) | 1 (0.4%) | < 0.001 |
| Charlson comorbidity score | 2.8 ± 1.8 | 2.9 ± 1.7 | 2.7 ± 1.8 | 0.13 |
| CHA2DS2-VASc score | 3.0 (2.0, 4.0) | 3.0 (2.0, 4.0) | 2.0 (2.0, 3.0) | < 0.001 |
| Ordinal CHA2DS2-VASc scores | 0.07 | |||
| 0 | 19 (3.0%) | 8 (2.2%) | 11 (4.1%) | |
| 1 | 93 (14.8%) | 46 (12.7%) | 47 (17.5%) | |
| 2 | 189 (30.0%) | 99 (27.4%) | 90 (33.5%) | |
| 3 | 171 (27.1%) | 103 (28.5%) | 68 (25.3%) | |
| 4 | 81 (12.9%) | 53 (14.7%) | 28 (10.4%) | |
| 5 | 43 (6.8%) | 27 (7.5%) | 16 (5.9%) | |
| 6 | 31 (4.9%) | 23 (6.4%) | 8 (3.0%) | |
| 7 | 3 (0.5%) | 2 (0.6%) | 1 (0.4%) | |
| Outpatient medications | ||||
| Vitamin K antagonist | 97 (15.4%) | 97 (26.9%) | 0 (0.0%) | < 0.001 |
| DOAC* | 264 (41.9%) | 264 (73.1%) | 0 (0.0%) | < 0.001 |
| Apixaban | 191 (30%) | 191 (72%) | - | |
| Rivaroxaban | 66 (10%) | 66 (25%) | - | |
| Dabigatran | 7 (1.1%) | 7 (3%) | - | |
| Aspirin | 284 (45.1%) | 150 (41.6%) | 134 (49.8%) | 0.039 |
| Dual antiplatelet therapy | 35 (5.6%) | 10 (2.8%) | 25 (9.3%) | < 0.001 |
| P2Y12 inhibitor† | 61 (9.7%) | 27 (7.5%) | 34 (12.6%) | 0.030 |
| Clopidogrel | 54 (8.6%) | 22 (6.1%) | 32 (11.9%) | |
| Ticagrelor | 3 (0.5%) | 1 (0.3%) | 2 (0.7%) | |
| Aspirin or oral P2Y12 inhibitor | 307 (48.7%) | 164 (45.4%) | 143 (53.2%) | 0.054 |
| Statin | 419 (66.5%) | 254 (70.4%) | 165 (61.3%) | 0.017 |
| Non-statin lipid lowering agent | 38 (6.0%) | 28 (7.8%) | 10 (3.7%) | 0.035 |
| Beta blocker | 351 (55.7%) | 210 (58.2%) | 141 (52.4%) | 0.15 |
| Calcium channel blocker | 208 (33.0%) | 122 (33.8%) | 86 (32.0%) | 0.63 |
| ACE inhibitor | 187 (29.7%) | 103 (28.5%) | 84 (31.2%) | 0.46 |
| ARB | 105 (16.7%) | 71 (19.7%) | 34 (12.6%) | 0.019 |
| Digoxin | 35 (5.6%) | 27 (7.5%) | 8 (3.0%) | 0.014 |
| Inpatient medications | ||||
| Remdesivir | 240 (38.2%) | 134 (37.2%) | 106 (39.4%) | 0.58 |
| Interleukin-6 antagonist‡ | 2 (0.3%) | 2 (0.6%) | 0 (0.0%) | 0.22 |
| Systemic steroid§ | 350 (55.6%) | 190 (52.6%) | 160 (59.5%) | 0.09 |
ACE = angiotensin converting enzyme; ARB = angiotensin receptor blockers; DOAC = direct oral anticoagulant; TIA = transient ischemic attack.
Values n (%), mean ± SD, or median (IQR).
There were no patients on pre-admission edoxaban.
There were no patients on pre-admission prasugrel.
IL-6 antagonists include the medications idarucizumab and rituximab
Systemic steroids include the medications dexamethasone, prednisone, methylprednisolone, and hydrocortisone.
Patients on preadmission OAC had lower initial body temperatures than those not on OAC therapy. Baseline estimated glomerular filtration rate, anion gap, d-dimer, C-reactive protein, and baseline and peak troponin were all lower in those on vs not on preadmission OAC (Table 2 ). Vital sign and laboratory value missingness, stratified by preadmission OAC use, is characterized in Supplementary Figure 1.
Table 2.
Admission vital signs and laboratory data
| Reference range | Total(N = 630) | Anticoagulation |
p Value | ||
|---|---|---|---|---|---|
| Yes (N = 361) | No (N = 269) | ||||
| Vital Signs | |||||
| Temperature (F) | 98.3 ± 1.4 | 98.2 ± 1.3 | 98.6 ± 1.5 | < 0.001 | |
| Systolic blood pressure (mm Hg) | 130.8 ± 26.6 | 128.8 ± 26.0 | 133.4 ± 27.3 | 0.031 | |
| Diastolic blood pressure (mm Hg) | 72.9 ± 16.6 | 72.2 ± 16.7 | 73.7 ± 16.4 | 0.26 | |
| Heart rate (beats/min) | 93.4 ± 27.4 | 91.8 ± 26.7 | 95.6 ± 28.3 | 0.08 | |
| Respiratory rate (breaths/min) | 21.2 ± 6.4 | 21.2 ± 6.4 | 21.2 ± 6.3 | 1.0 | |
| Oxygen saturation | 95.1± 5.6 | 95.2 ± 6.4 | 94.9 ± 4.5 | 0.64 | |
| Laboratory tests | |||||
| WBC (109/L) | 3.5 - 11 | 8.6 ± 5.4 | 8.2 ± 5.3 | 9.1 ± 5.5 | 0.06 |
| Hgb (g/dL) | 11.0 – 15.0 | 11.9 ± 2.4 | 11.8 ± 2.4 | 12.0 ± 2.4 | 0.41 |
| Platelets (x109/L) | 150-400 | 213.7 ± 99.5 | 218.2 ± 104.8 | 207.6 ± 91.7 | 0.20 |
| eGFR (mL/min/1.73M) | > 60 | 68.0 ± 43.7 | 64.8 ± 38.0 | 72.3 ± 50.1 | 0.035 |
| Serum creatinine (mg/dL) | 0.44 – 1.03 | 1.7 ± 1.6 | 1.6 ± 1.3 | 1.8 ± 2.0 | 0.12 |
| Anion gap | 3 - 13 | 11.3 ± 3.4 | 10.8 ± 2.9 | 11.8 ± 4.0 | < 0.001 |
| INR | 0.8 – 1.2 | 1.8 ± 1.3 | 2.2 ± 1.5 | 1.3 ± 0.5 | < 0.001 |
| D-dimer (mg/L) | < 232 | 1472.7 ± 5461.7 | 829.3 ± 3774.3 | 2294.2 ± 6977.4 | 0.003 |
| C-reactive protein (mg/L) | < 5.0 | 91.9 ± 83.9 | 81.8 ± 69.5 | 105.9 ± 99.0 | 0.001 |
| Baseline troponin-I (ng/mL) | 0.006 – 0.06 | 0.6 ± 3.8 | 0.3 ± 1.2 | 1.1 ± 5.6 | 0.006 |
| Peak troponin-I (ng/mL) | 0.006 – 0.060 | 1.2 ± 7.0 | 0.6 ± 3.3 | 2.0 ± 9.9 | 0.016 |
| Whole blood lactate (mEq/L) | 0.2 – 1.9 | 2.1 + 2.0 | 2.1 + 1.9 | 2.1 + 2.1 | 0.79 |
eGFR = estimated glomerular filtration rate; Hgb = Hemoglobin; INR = international normalized ratio; WBC = white blood cell count.
Of patients prescribed preadmission OAC, 264 (73%) were on a DOAC, and 97 (27%) had a VKA. Of those on a DOAC, 191 (72%) were on apixaban, 66 (25%) on rivaroxaban, and 7 (3%) on dabigatran. No patients were taking edoxaban.
Among those who were not on preadmission OAC, therapeutic and non-therapeutic anticoagulation was initiated in 38.3% and 49.8%, respectively. The use of thrombolytic therapy and vasopressors was more common in those not on preadmission OAC. There was no difference in the rate of in-hospital systemic steroid, remdesivir, or interleukin-6 antagonist use between those who were and were not taking preadmission OAC (Table 2).
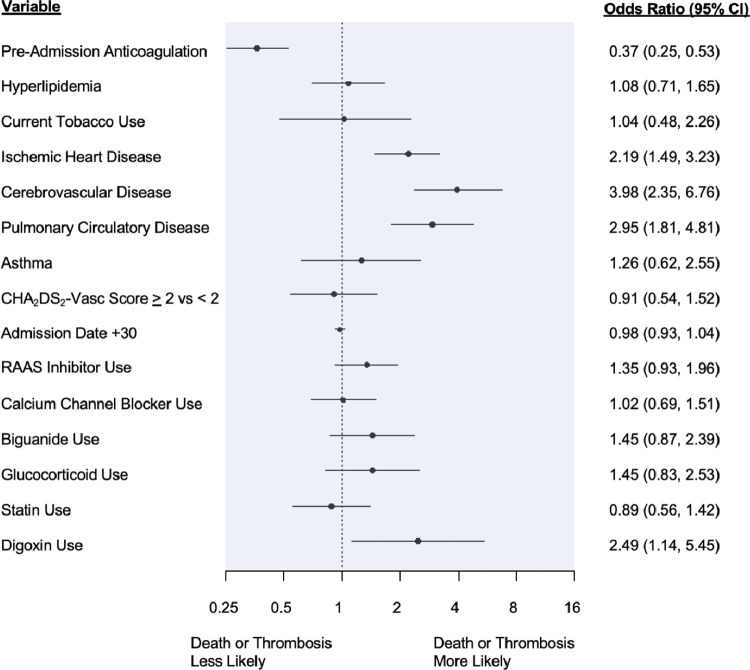
Unadjusted outcomes are shown in Table 3 . A primary composite outcome event occurred in 224 (35.6%) patients, 98 (27.1%) of those on and 126 (46.8%) of those not on preadmission OAC (p <0.001). After adjustment for multiple covariates, the use of preadmission OAC was associated with 63% lower odds of all-cause mortality or thrombotic complications (odds ratio 0.37, confidence interval 0.25 to 0.53, p <0.0001) (Figure 2 ). Primary outcomes were similar when comparing those on preadmission DOAC versus VKA (Supplementary Table 6).
Table 3.
Unadjusted primary and secondary outcomes according to pre-admission anticoagulant use
| Total (N = 630) | Anticoagulation |
p Value | ||
|---|---|---|---|---|
| Yes (N = 361) | No (N = 269) | |||
| Composite of all-cause mortality and arterial or venous thrombosis | 224 (35.6%) | 98 (27.1%) | 126 (46.8%) | < 0.001 |
| All-cause mortality | 126 (20.0%) | 59 (16.3%) | 67 (24.9%) | 0.007 |
| Composite arterial or venous thrombosis | 135 (21.4%) | 53 (14.7%) | 82 (30.5%) | < 0.001 |
| Venous thromboembolism | 55 (8.7%) | 14 (3.9%) | 41 (15.2%) | <0.001 |
| Acute DVT | 28 (4.4%) | 7 (1.9%) | 21 (7.8%) | < 0.001 |
| Acute pulmonary embolism | 31 (4.9%) | 8 (2.2%) | 23 (8.6%) | < 0.001 |
| Arterial thrombosis | 91 (14.4%) | 42 (11.6%) | 49 (18.2%) | 0.020 |
| Acute coronary syndrome | 52 (8.3%) | 25 (6.9%) | 27 (10.0%) | 0.16 |
| TIA | 5 (0.8%) | 4 (1.1%) | 1 (0.4%) | 0.30 |
| Stroke | 36 (5.7%) | 16 (4.4%) | 20 (7.4%) | 0.11 |
| Acute limb ischemia | 6 (1.0%) | 3 (0.8%) | 3 (1.1%) | 0.72 |
| Acute mesenteric ischemia | 3 (0.5%) | 0 (0.0%) | 3 (1.1%) | 0.044 |
| ICU admission | 131 (20.8%) | 53 (14.7%) | 78 (29.0%) | < 0.001 |
| Intubation | 73 (11.6%) | 23 (6.4%) | 50 (18.6%) | < 0.001 |
| Non-invasive ventilation | 141 (22.4%) | 67 (18.6%) | 74 (27.5%) | 0.007 |
| Supplemental oxygen requirement | 486 (77.1%) | 271 (75.1%) | 215 (79.9%) | 0.15 |
| Cardiac arrest | 23 (3.7%) | 9 (2.5%) | 14 (5.2%) | 0.07 |
| Red blood cell transfusion | 65 (10.3%) | 30 (8.3%) | 35 (13.0%) | 0.055 |
| Major bleed | 94 (14.9%) | 47 (13.0%) | 47 (17.5%) | 0.12 |
| Length of stay – days | 7.0 (4.0, 12.0) | 6.0 (3.0, 11.0) | 7.0 (4.0, 14.0) | < 0.001 |
ICU = Intensive care unit; DVT = deep vein thrombosis; TIA = transient ischemic attack.
Values are n (%) or median (IQR).
Figure 2.
Multivariable Model of All-Cause Mortality and Thrombotic Outcomes in the Overall Cohort. Shown is a multivariable model relating pre-admission use of oral anticoagulation to composite in-hospital all-cause mortality and thrombotic complications.Abbreviations: RAAS = renin angiotensin aldosterone system. “Admission date +30” was defined as the index date of admission plus 30 days to evaluate the temporal effect of admission on outcomes.
All-cause mortality was less frequent among those who were on preadmission OAC compared with those who were not. Composite thrombotic events were less frequent in patients on vs not on preadmission OAC. Patients on OAC were less likely to suffer acute venous or arterial thrombotic events, including acute DVT, acute PE, and acute mesenteric ischemia. There was no difference in the rate of acute coronary syndromes, TIA, acute ischemic stroke, or acute limb ischemia. There were also no between-group differences in the frequency of cardiac arrest, need for supplemental oxygen, noninvasive ventilation, intubation, red blood cell transfusion, or major bleeding. Length of stay was shorter in patients who were on vs not on preadmission OAC (Table 3). Among survivors, discharge disposition was no different according to preadmission OAC use (Supplementary Table 7). Secondary outcomes were similar to those on preadmission DOAC and VKA (Supplementary Table 8). Results were essentially unchanged when the CHA2DS2-VASc score was included in the multivariable model as an ordinal rather than a dichotomous categorical variable (Supplementary Figure 2). In a sensitivity analysis excluding patients with a CHA2DS2-VASc score of 0, where all remaining patients had a thrombotic risk high enough to warrant OAC, results remained unchanged (Supplementary Table 9). A higher CHA2DS2-VASc score (3.0 ± 1.4 vs 2.7 ± 1.4, p = 0.032) was associated with increased risk of thrombotic events (Supplementary Table 4) but did not predict in-hospital mortality or the composite, all-cause mortality or thrombotic events (Supplementary Tables 2 and 3). Lastly, when examining the effect of OAC according to AF subtype, the results did not change (interaction p = 0.5).
Discussion
In a study of patients with pre-existing AF who were hospitalized with COVID-19, we observed that those on preadmission OAC had lower composite rates of death or thrombotic events, and less severe COVID-19, as reflected by more favorable admission data, a lower incidence of ICU admission, intubation, noninvasive ventilation, and shorter length of stay. These observations were apparent despite the more adverse demographic and co-morbid profile of those on preadmission OAC. Furthermore, a higher CHA2DS2-VASc score was associated with a greater incidence of composite arterial and venous thrombotic complications.
Although data suggest that thrombosis begins early during the disease course,16 , 17 it is unclear whether “upstream” (i.e., preadmission) therapeutic-dose OAC confers a benefit. Multiple randomized trials have demonstrated that when compared with standard thromboprophylaxis, therapeutic anticoagulation reduces the risk of death and composite death or thrombotic events in non-critically ill patients admitted with COVID-19.18 , 19 In contrast, randomized trials in low-risk outpatients20 with COVID-19 have found no benefit with therapeutic anticoagulation. It is unknown whether outpatients who are at elevated baseline risk for thrombotic events, such as those with AF, might benefit from preadmission therapeutic anticoagulation.21 , 22
Patients with AF are at persistently elevated risk for thromboembolism secondary to endothelial dysfunction, blood stasis, coagulation activation, and systemic inflammation, pathologic mechanisms similar to those observed in COVID-19.23 , 24 Meta-analyses have found that pre-existing AF is associated with increased mortality in patients hospitalized with COVID-19, however, the reasons for this observation have not been elucidated; neither anticoagulation status nor thrombotic outcomes have been characterized in these studies.25 , 26 Preadmission anticoagulation with either a DOAC or VKA may counteract the pro-thrombotic effects of the virus, ultimately preventing subclinical and clinical thrombosis. Notably, apixaban and rivaroxaban reduce d-dimer levels,27 , 28 which have been associated with worse clinical outcomes in patients with COVID-19;29 it is plausible that the impact such agents have on the coagulation cascade results in more favorable outcomes.
Observational studies relating preadmission OAC to outcomes in patients hospitalized with COVID-19 have yielded mixed results. Multiple studies have reported increased disease severity and higher mortality rates in patients who were on OAC at the time of hospital admission.30, 31, 32 Others have found no association,33 , 34 whereas some have suggested that DOAC use is associated with a lower risk of adverse outcomes.35, 36, 37, 38 Most of these studies did not preferentially include patients at persistently elevated baseline risk for thrombosis, and few accounted for differential thrombotic risk between treatment and control groups. Our study overcame many of the limitations of previous studies by including a cohort exclusively comprised patients with AF who were consequently at elevated baseline thrombotic risk,13 compared treatment and control groups with similar thrombotic risk and similar indications for OAC, and yielded a large number of both venous and arterial thrombotic events for comparison.
The decision to initiate OAC in patients with AF is ideally made through shared decision-making that takes into consideration the risks of thromboembolic events and bleeding while incorporating patient preference. In our study cohort, after adjusting for baseline CHA2DS2-VASc score and restricting our analysis to those with a CHA2DS2-VASc score of 1 or higher, we observed that preadmission OAC use was associated with a more favorable in-hospital outcome. Although our study design does not allow us to infer causality, our results do call into question whether the risk-benefit balance should be reconsidered in ambulatory patients with AF who develop COVID-19. A higher short-term risk of death or thromboembolic events might favor the decision to initiate OAC in patients at high thrombotic risk who were otherwise not taking OAC.
There are important limitations to our study. First, we cannot rule out the possibility of residual confounding or bias despite the use of multivariable adjustment. Second, the use of ICD-10 codes to define clinical outcomes may have resulted in under- or miscoding; however, had this occurred, it would have biased our results toward the null. Third, we cannot confirm patient adherence to outpatient OAC therapy before admission; had adherence been suboptimal, this also would have biased our results toward the null. Similarly, it is possible that those on OAC had better access to medical care which may have biased our results. Fourth, routine screening for thrombotic complications (e.g., vascular ultrasound testing and CT angiography) was not performed in our cohort, therefore, the true incidence of composite thrombotic events in our study cohort is unknown and our findings reflect only clinically manifest thrombotic complications as captured by ICD-10 coding. In addition, because this was a retrospective study of in-hospital outcomes, post-discharge thromboembolic complications and vital status were not known, and the reasons for OAC non-use preadmission were not available.
In conclusion, among patients at elevated baseline thrombotic risk because of AF who were hospitalized with COVID-19, those on preadmission OAC had lower rates of death, arterial and venous thrombotic events, and less severe COVID-19. Further investigation is needed to establish the safety and efficacy of OAC in ambulatory patients with symptomatic COVID-19 who are at elevated thrombotic risk.
Disclosures
The authors have no conflicts of interest to declare.
Footnotes
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.amjcard.2022.07.006.
Appendix. Supplementary materials
References
- 1.DeLago AJ, Essa M, Ghajar A, Hammond-Haley M, Parvez A, Nawaz I, Shalhoub J, Marshall DC, Nazarian S, Calkins H, Salciccioli JD, Philips B. Incidence and mortality trends of atrial fibrillation/atrial flutter in the United States 1990 to 2017. Am J Cardiol. 2021;148:78–83. doi: 10.1016/j.amjcard.2021.02.014. [DOI] [PubMed] [Google Scholar]
- 2.Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen AM, Gislason GH. Torp-Pedersen C. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124. doi: 10.1136/bmj.d124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, ROCKET AF Investigators Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 4.Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L, ARISTOTLE Committees and Investigators Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 5.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L. RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 6.Xiong X, Chi J, Gao Q. Prevalence and risk factors of thrombotic events on patients with COVID-19: a systematic review and meta-analysis. Thromb J. 2021;19:32. doi: 10.1186/s12959-021-00284-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen MY, Xiao FP, Kuai L, Zhou HB, Jia ZQ, Liu M, He H, Hong M. Outcomes of atrial fibrillation in patients with COVID-19 pneumonia: a systematic review and meta-analysis. Am J Emerg Med. 2021;50:661–669. doi: 10.1016/j.ajem.2021.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harrison SL, Fazio-Eynullayeva E, Lane DA, Underhill P, Lip GYH. Atrial fibrillation and the risk of 30-day incident thromboembolic events, and mortality in adults >50 years with COVID-19. J Arrhythm. 2021;37:231–237. doi: 10.1002/joa3.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pardo Sanz A, Salido Tahoces L, Ortega Pérez R, González Ferrer E, Sánchez Recalde Á, Zamorano Gómez JL. New-onset atrial fibrillation during COVID-19 infection predicts poor prognosis. Cardiol J. 2021;28:34–40. doi: 10.5603/CJ.a2020.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harenberg J, Bauersachs R, Ageno W. Does chronic treatment with oral anticoagulants ameliorate the clinical course of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in coronavirus disease 2019 (COVID-19)? Semin Thromb Hemost. 2021;47:338–340. doi: 10.1055/s-0040-1715091. [DOI] [PubMed] [Google Scholar]
- 11.Beyrer J, Manjelievskaia J, Bonafede M, Lenhart G, Nolot S, Haldane D, Johnston J. Validation of an International Classification of Disease, 10th revision coding adaptation for the Charlson Co-morbidity Index in United States healthcare claims data. Pharmacoepidemiol Drug Saf. 2021;30:582–593. doi: 10.1002/pds.5204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC, Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients With atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74:104–132. doi: 10.1016/j.jacc.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Lutsey PL, Norby FL, Alonso A, Cushman M, Chen LY, Michos ED, Folsom AR. Atrial fibrillation and venous thromboembolism: evidence of bidirectionality in the Atherosclerosis Risk in Communities Study. J Thromb Haemost. 2018;16:670–679. doi: 10.1111/jth.13974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aciksari G, Cetinkal G, Kocak M, Cag Y, Atici A, Altunal LN, Barman HA, Aydin M, Kocas BB, Cam G, Guclu KG, Caliskan M. Evaluation of modified ATRIA risk score in predicting mortality in hospitalized patients with COVID-19. Am J Med Sci. 2021;362:553–561. doi: 10.1016/j.amjms.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raad M, Gorgis S, Abshire C, Yost M, Dabbagh MF, Chehab O, Aurora L, Patel S, Nona P, Yan J, Singh G, Syrjamaki J, Kaatz S, Parikh S. COVID-19 risk index (CRI): a simple and validated emergency department risk score that predicts mortality and the need for mechanical ventilation. J Thromb Thrombolysis. 2022;53:567–575. doi: 10.1007/s11239-021-02565-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, Kucher N, Studt JD, Sacco C, Bertuzzi A, Sandri MT, Barco S. Humanitas COVID-19 Task Force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whyte MB, Kelly PA, Gonzalez E, Arya R, Roberts LN. Pulmonary embolism in hospitalized patients with COVID-19. Thromb Res. 2020;195:95–99. doi: 10.1016/j.thromres.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.ATTACC Investigators. ACTIV-4a Investigators. REMAP-CAP Investigators. Lawler PR, Goligher EC, Berger JS, Neal MD, McVerry BJ, Nicolau JC, Gong MN, Carrier M, Rosenson RS, Reynolds HR, Turgeon AF, Escobedo J, Huang DT, Bradbury CA, Houston BL, Kornblith LZ, Kumar A, Kahn SR, Cushman M, McQuilten Z, Slutsky AS, Kim KS, Gordon AC, Kirwan BA, Brooks MM, Higgins AM, Lewis RJ, Lorenzi E, Berry SM, Berry LR, Aday AW, Al-Beidh F, Annane D, Arabi YM, Aryal D, Baumann Kreuziger L, Beane A, Bhimani Z, Bihari S, Billett HH, Bond L, Bonten M, Brunkhorst F, Buxton M, Buzgau A, Castellucci LA, Chekuri S, Chen JT, Cheng AC, Chkhikvadze T, Coiffard B, Costantini TW, de Brouwer S, Derde LPG, Detry MA, Duggal A, Džavík V, Effron MB, Estcourt LJ, Everett BM, Fergusson DA, Fitzgerald M, Fowler RA, Galanaud JP, Galen BT, Gandotra S, García-Madrona S, Girard TD, Godoy LC, Goodman AL, Goossens H, Green C, Greenstein YY, Gross PL, Hamburg NM, Haniffa R, Hanna G, Hanna N, Hegde SM, Hendrickson CM, Hite RD, Hindenburg AA, Hope AA, Horowitz JM, Horvat CM, Hudock K, Hunt BJ, Husain M, Hyzy RC, Iyer VN, Jacobson JR, Jayakumar D, Keller NM, Khan A, Kim Y, Kindzelski AL, King AJ, Knudson MM, Kornblith AE, Krishnan V, Kutcher ME, Laffan MA, Lamontagne F, Le Gal G, Leeper CM, Leifer ES, Lim G, Lima FG, Linstrum K, Litton E, Lopez-Sendon J, Lopez-Sendon Moreno JL, Lother SA, Malhotra S, Marcos M, Saud Marinez A, Marshall JC, Marten N, Matthay MA, McAuley DF, McDonald EG, McGlothlin A, McGuinness SP, Middeldorp S, Montgomery SK, Moore SC, Morillo Guerrero R, Mouncey PR, Murthy S, Nair GB, Nair R, Nichol AD, Nunez-Garcia B, Pandey A, Park PK, Parke RL, Parker JC, Parnia S, Paul JD, Pérez González YS, Pompilio M, Prekker ME, Quigley JG, Rost NS, Rowan K, Santos FO, Santos M, Olombrada Santos M, Satterwhite L, Saunders CT, Schutgens REG, Seymour CW, Siegal DM, Silva DG, Shankar-Hari M, Sheehan JP, Singhal AB, Solvason D, Stanworth SJ, Tritschler T, Turner AM, van Bentum-Puijk W, van de Veerdonk FL, van Diepen S, Vazquez-Grande G, Wahid L, Wareham V, Wells BJ, Widmer RJ, Wilson JG, Yuriditsky E, Zampieri FG, Angus DC, McArthur CJ, Webb SA, Farkouh ME, Hochman JS, Zarychanski R. Therapeutic anticoagulation with heparin in noncritically ill patients with COVID-19. N Engl J Med. 2021;385:790–802. doi: 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spyropoulos AC, Goldin M, Giannis D, Diab W, Wang J, Khanijo S, Mignatti A, Gianos E, Cohen M, Sharifova G, Lund JM, Tafur A, Lewis PA, Cohoon KP, Rahman H, Sison CP, Lesser ML, Ochani K, Agrawal N, Hsia J, Anderson VE, Bonaca M, Halperin JL, Weitz JI. HEP-COVID Investigators. Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with COVID-19: the HEP-COVID randomized clinical trial. JAMA Intern Med. 2021;181:1612–1620. doi: 10.1001/jamainternmed.2021.6203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Connors JM, Brooks MM, Sciurba FC, Krishnan JA, Bledsoe JR, Kindzelski A, Baucom AL, Kirwan BA, Eng H, Martin D, Zaharris E, Everett B, Castro L, Shapiro NL, Lin JY, Hou PC, Pepine CJ, Handberg E, Haight DO, Wilson JW, Majercik S, Fu Z, Zhong Y, Venugopal V, Beach S, Wisniewski S, Ridker PM, ACTIV-4B Investigators Effect of antithrombotic therapy on clinical outcomes in outpatients With clinically stable symptomatic COVID-19: the ACTIV-4B randomized clinical trial. JAMA. 2021;326:1703–1712. doi: 10.1001/jama.2021.17272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Capell WH, Barnathan ES, Piazza G, Spyropoulos AC, Hsia J, Bull S, Lipardi C, Sugarmann C, Suh E, Rao JP, Hiatt WR, Bonaca MP. Rationale and design for the study of Rivaroxaban to reduce thrombotic events, hospitalization and death in outpatients with COVID-19: the PREVENT-HD study. Am Heart J. 2021;235:12–23. doi: 10.1016/j.ahj.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barco S, Bingisser R, Colucci G, Frenk A, Gerber B, Held U, Mach F, Mazzolai L, Righini M, Rosemann T, Sebastian T, Spescha R, Stortecky S, Windecker S, Kucher N. Enoxaparin for primary thromboprophylaxis in ambulatory patients with coronavirus disease-2019 (the Ovid study): a structured summary of a study protocol for a randomized controlled trial. Trials. 2020;21:770. doi: 10.1186/s13063-020-04678-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hanff TC, Mohareb AM, Giri J, Cohen JB, Chirinos JA. Thrombosis in COVID-19. Am J Hematol. 2020;95:1578–1589. doi: 10.1002/ajh.25982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo Y, Lip GY, Apostolakis S. Inflammation in atrial fibrillation. J Am Coll Cardiol. 2012;60:2263–2270. doi: 10.1016/j.jacc.2012.04.063. [DOI] [PubMed] [Google Scholar]
- 25.Yang H, Liang X, Xu J, Hou H, Wang Y. Meta-analysis of atrial fibrillation in patients with COVID-19. Am J Cardiol. 2021;144:152–156. doi: 10.1016/j.amjcard.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zuin M, Rigatelli G, Bilato C, Zanon F, Zuliani G, Roncon L. Pre-existing atrial fibrillation is associated with increased mortality in COVID-19 Patients. J Interv Card Electrophysiol. 2021;62:231–238. doi: 10.1007/s10840-021-00992-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kirchhof P, Ezekowitz MD, Purmah Y, Schiffer S, Meng IL, Camm AJ, Hohnloser SH, Schulz A, Wosnitza M, Cappato R. Effects of Rivaroxaban on biomarkers of coagulation and inflammation: A post hoc analysis of the X-VeRT trial. TH Open. 2020;4:e20–e32. doi: 10.1055/s-0040-1701206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeitouni M, Giczewska A, Lopes RD, Wojdyla DM, Christersson C, Siegbahn A, De Caterina R, Steg PG, Granger CB, Wallentin L, Alexander JH, Investigators ARISTOTLE. Clinical and pharmacological effects of apixaban dose adjustment in the Aristotle trial. J Am Coll Cardiol. 2020;75:1145–1155. doi: 10.1016/j.jacc.2019.12.060. [DOI] [PubMed] [Google Scholar]
- 29.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rivera-Caravaca JM, Núñez-Gil IJ, Vivas D, Viana-Llamas MC, Uribarri A, Becerra-Muñoz VM, Trabattoni D, Fernández Rozas I, Feltes G, López-Pais J, El-Battrawy I, Macaya C, Fernandez-Ortiz A, Estrada V, Marín F. HOPE COVID-19 Investigators. Clinical profile and prognosis in patients on oral anticoagulation before admission for COVID-19. Eur J Clin Invest. 2021;51:e13436. doi: 10.1111/eci.13436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schiavone M, Gasperetti A, Mancone M, Curnis A, Mascioli G, Mitacchione G, Busana M, Sabato F, Gobbi C, Antinori S, Galli M, Forleo GB. Oral anticoagulation and clinical outcomes in COVID-19: an Italian multicenter experience. Int J Cardiol. 2021;323:276–280. doi: 10.1016/j.ijcard.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dashti HT, Bates D, Fiskio JM, Roche EC, Mora S, Demler O. Clinical characteristics and severity of COVID-19 disease in patients from Boston area hospitals [published online August 4, 2020]. Preprint. medRxiv. doi:10.1101/2020.07.27.20163071.
- 33.Flam B, Wintzell V, Ludvigsson JF, Mårtensson J, Pasternak B. Direct oral anticoagulant use and risk of severe COVID-19. J Intern Med. 2021;289:411–419. doi: 10.1111/joim.13205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tremblay D, van Gerwen M, Alsen M, Thibaud S, Kessler A, Venugopal S, Makki I, Qin Q, Dharmapuri S, Jun T, Bhalla S, Berwick S, Feld J, Mascarenhas J, Troy K, Cromwell C, Dunn A, Oh WK, Naymagon L. Impact of anticoagulation prior to COVID-19 infection: a propensity score-matched cohort study. Blood. 2020;136:144–147. doi: 10.1182/blood.2020006941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahlström B, Frithiof R, Hultström M, Larsson IM, Strandberg G, Lipcsey M. The Swedish covid-19 intensive care cohort: risk factors of ICU admission and ICU mortality. Acta Anaesthesiol Scand. 2021;65:525–533. doi: 10.1111/aas.13781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fröhlich GM, Jeschke E, Eichler U, Thiele H, Alhariri L, Reinthaler M, Kastrati A, Leistner DM, Skurk C, Landmesser U, Günster C. Impact of oral anticoagulation on clinical outcomes of COVID-19: a nationwide cohort study of hospitalized patients in Germany. Clin Res Cardiol. 2021;110:1041–1050. doi: 10.1007/s00392-020-01783-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harrison RF, Forte K, Buscher MG, Jr Chess A, Patel A, Moylan T, Mize CH, Werdmann M, Ferrigno R. The association of preinfection daily oral anticoagulation use and all-cause in-hospital mortality from novel coronavirus 2019 at 21 days: A retrospective cohort study. Crit Care Explor. 2021;3:e0324. doi: 10.1097/CCE.0000000000000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rossi R, Coppi F, Talarico M, Boriani G. Protective role of chronic treatment with direct oral anticoagulants in elderly patients affected by interstitial pneumonia in COVID-19 era. Eur J Intern Med. 2020;77:158–160. doi: 10.1016/j.ejim.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.