In the global movement to enhance transparency in financial relationships between physicians and the healthcare industry, almost all payments from pharmaceutical and medical device companies to physicians in the United States have been publicly disclosed in the Open Payments Database since 2013.1 Allergists and clinical immunologists are experts who received one of the largest per-physician general payments in the country in 2015.2 The coronavirus disease 2019 (COVID-19) pandemic may have limited financial interaction between the healthcare industry and these experts, but few studies have investigated the trend in industry payments related to allergology and immunology during the COVID-19 pandemic.
This cross-sectional study examined the trend in financial relationships between the healthcare industry and allergists and clinical immunologists in the United States during the COVID-19 pandemic, using the relevant data extracted from the Open Payments Database. All general payments made to physicians whose primary specialty was categorized as allergology or clinical immunology between 2014 and 2020 were used. General payments included payments made to physicians for personal purposes such as compensations for lecturing, consulting fees, food and beverages, gifts, honoraria, and travel and lodging.1 Furthermore, we collected demographic information for physicians receiving payments from the US Open Payments physician profile dataset. Trends in payments before and during the COVID-19 pandemic were evaluated by the interrupted time series analysis using population-averaged generalized estimating equation (GEE) models with panel-data of monthly payments at the physician level. Because the payments were highly skewed, the study used a negative binomial regression GEE model for the payments per physician and a linear log-linked regression GEE model with Poisson distribution for the number of physicians with payments.3 , 4 Given that the national emergency concerning the COVID-19 pandemic was declared in the United States on March 13, 2020, we divided the study period into before (January 2014 to February 2020) and during the pandemic (March 2020 to December 2020). To adjust the seasonality of the payments, we included the month variable in the interrupted time series models. Furthermore, a descriptive analysis was conducted for annual and aggregate payments. Regional difference in payments per physician was evaluated by the Mann-Whitney U test, and the US Census regions were used to classify the US regions where physicians practiced. Payment concentration was examined by the Gini index. The Gini index was used to assess the inequality of payment distribution.4 Average relative annual changes in per-physician payments and number of physicians receiving payments were also estimated by the GEE models with panel-data of annual payments per physician.3 The annual trend in total payment amounts was estimated by the robust-adjusted linear regression model. Because this study only included publicly available information, informed consent was waived by the Ethics Committee of the Medical Governance Research Institute.
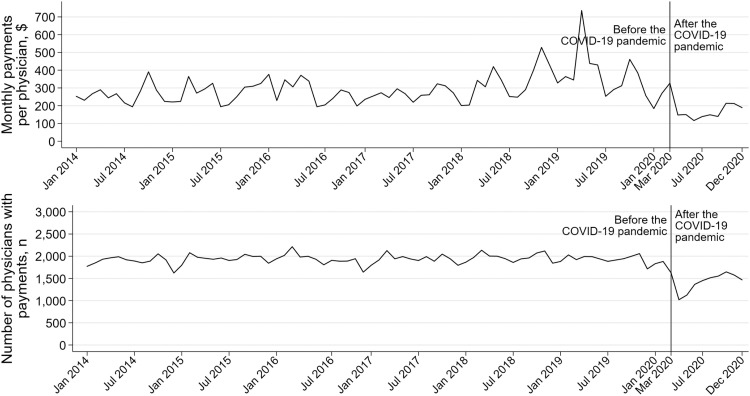
There were 4173 (85.1%) allergists and clinical immunologists receiving 700,054 general payments with a total of $99,444,136 from 632 companies between 2014 and 2020. The monthly payments and number of physicians receiving payments decreased by 52.6% (95% confidence interval [CI], 45.7-58.6; P < .001) and 36.9% (95% CI, 35.3-38.6; P < .001) at the beginning of the pandemic (Fig 1 ). Although the number of physicians receiving payments increased during the pandemic with an average monthly change rate of 3.2% (95% CI, 2.9-3.6; P < .001), there was no clinically meaningful change in the payments per physician within the pandemic.
Figure 1.
Monthly trend in general payments per physician and number of in allergologists and clinical immunologists accepting general payments between 2014 and 2020 in the United States. COVID-19, coronavirus disease 2019.
For annual payments, the number of allergists and clinical immunologists receiving payments significantly decreased from 3230 in 2014 to 3012 in 2020, with an average relative annual change rate of −1.3% (95% CI, −1.7 to −0.9; P < .001). Meanwhile, total payment amounts annually increased from $13,138,393 in 2014 to $19,200,796 in 2019. The payments per physician increased from $395 (interquartile range [IQR], $123-$1233) in 2014 to $597 (IQR, $175-$1531) in 2019, with an average relative annual change rate of 7.2% (95% CI, 4.1-10.4; P < .001). However, the payments per physician decreased by 50.9% (95% CI, 44.7-56.4; P < .001) to $454 (IQR, $115-$1284) in 2020 compared with 2014 to 2019. Similarly, 2582 allergists and clinical immunologists received general payments in 2020, decreasing by 13.9% (95% CI, 12.2-15.6; P < .001) compared with those between 2014 and 2019. Among major payment categories, payments for grants and travel or lodging decreased most markedly by −94.3% ($3000) and −82.5% ($331,669) in 2020 compared with those in 2019 ($52,305 and $1,894,263, respectively). The decrease in total payments was less in 2020 than in 2019 for gifts (−21.5% [$4291 in 2019 to $3368 in 2020]), education (−22.2% [$27,001 in 2019 to $21,010 in 2020]), and consulting services (−23.8% [$3,325,101 in 2019 to $2,533,153 in 2020]). The payments for food or beverages (−46.6% [$2,528,921 in 2019 to $1,350,627 in 2020]) and speaking compensation (−53.1% [$9,042,546 in 2019 to $4,242,391 in 2020]) decreased by approximately half in 2020 compared with 2019.
As for the analysis of payment concentration and difference, 21.3% (890), 8.3% (345), and 5.3% (221) of allergists and clinical immunologists received more than $10,000, $50,000, and $100,000 during the 7 years, respectively. The Gini index for the 7-year combined payments was 0.876, indicating that large amounts of personal payments were substantially concentrated on a small number of physicians. Physicians practicing in the Midwest received the lowest median payments per physician of $1640 (IQR, $336-$6526), whereas physicians practicing in the South region received the highest median payments of $3399 (IQR, $817-$9905). There was no significant difference in median payments per physician between the Midwest and the West ($1640 vs $1834; P = .06) and between the Midwest and the Northeast ($1640 vs $1859; P = .27) in the U test. Moreover, 74.6% of payments ($74,169,933) were associated with specific products. The highest paid product was Dupixent, representing 9.6% of total payments ($9,508,972), followed by Xolair (8.3%, $8,235,740), Fasenra (6.4%, $6,345,192), Cinryze (6.1%, $6,085,639), and Nucala (3.0%, $3,029,453).
Despite several limitations, including no inclusion of physicians without payments and unmeasured confounding factors as in other studies,5 , 6 this study is, to the best of our knowledge, the first to demonstrate that the COVID-19 pandemic potentially led to the decrease in financial relationships between allergists and clinical immunologists and the healthcare industry in the United States. An increase in the number of allergists and clinical immunologists receiving payment since the inception of the pandemic may have suggested a gradual resumption of promotional activities by the healthcare industry in this field. Furthermore, the analysis of annual payments elucidated that allergists and clinical immunologists have increasingly accepted personal payments from the industry, mainly in the form of food and beverages, since the inception of the Open Payments program. This increasing trend is because of the introduction of novel biological drugs for asthma, atopic dermatitis, and angioedema. Future studies should investigate the long-term trend of industry payments to clarify how promotional activities would bias the care of patients, in addition to the difference in payments owing to the demographic characteristics of physicians, such as sex and whether they are in leading positions in this field.
Footnotes
Disclosures: Dr Saito received personal fees from Taiho Pharmaceutical Co Ltd outside the scope of the submitted work. Dr Ozaki and Dr Tanimoto received personal fees from Medical Network Systems, a dispensing pharmacy, outside the scope of the submitted work. Dr Tanimoto also received personal fees from Bionics Co Ltd, a medical device company, outside the scope of the submitted work. The remaining authors have no conflicts of interest to report. Regarding nonfinancial conflicts of interest, all are engaged in ongoing research examining financial and nonfinancial conflicts of interest among healthcare professionals and pharmaceutical companies in Japan and the United States.
Funding: The authors have no funding sources to report.
References
- 1.Marshall DC, Jackson ME, Hattangadi-Gluth JA. Disclosure of industry payments to physicians: an epidemiologic analysis of early data from the open payments program. Mayo Clin Proc. 2016;91(1):84–96. doi: 10.1016/j.mayocp.2015.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tringale KR, Marshall D, Mackey TK, Connor M, Murphy JD, Hattangadi-Gluth JA. Types and distribution of payments from industry to physicians in 2015. JAMA. 2017;317(17):1774–1784. doi: 10.1001/jama.2017.3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kusumi E, Murayama A, Kamamoto S, Kawashima M, Yoshida M, Saito H, et al. Pharmaceutical payments to Japanese certified hematologists: a retrospective analysis of personal payments from pharmaceutical companies between 2016 and 2019. Blood Cancer J. 2022;12(4):54. doi: 10.1038/s41408-022-00656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murayama A, Kamamoto S, Saito H, Yamada K, Bhandari D, Shoji I, et al. Pharmaceutical payments to Japanese board-certified infectious disease specialists: a four-year retrospective analysis of payments from 92 pharmaceutical companies between 2016 and 2019. Int J Environ Res Public Health. 2022;19(12):7417. doi: 10.3390/ijerph19127417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Putman MS, Goldsher JE, Crowson CS, Duarte-García A. Industry payments to practicing US rheumatologists, 2014-2019. Arthritis Rheumatol. 2021;73(11):2138–2144. doi: 10.1002/art.41896. [DOI] [PubMed] [Google Scholar]
- 6.Annapureddy A, Murugiah K, Minges KE, Chui PW, Desai N, Curtis JP. Industry payments to cardiologists. Circ Cardiovasc Qual Outcomes. 2018;11(12) doi: 10.1161/CIRCOUTCOMES.118.005016. [DOI] [PubMed] [Google Scholar]