Abstract
Objectives: This study aimed to investigate dental undergraduate students’ tobacco usage and social nicotine dependence in Australia. A special interest was to identify the role of factors such as age, gender, year of dental education and cohabitants’ smoking status for social nicotine dependence. Materials and methods: A sample of 252, first-to-fifth year undergraduate students in an Australian dental school was used. Each completed a self-administered questionnaire. Results: The smoking rate was 4.8%. Current smokers displayed higher social nicotine dependence than those that had never smoked (t = 3.1, df = 244, P = 0.002). Dental undergraduate students that showed higher social nicotine dependence (P = 0.001, OR = 1.3, 95% CI: 1.1–1.6), or that had smoking cohabitants (P = 0.016, OR = 4.8, 95% CI: 1.3–17.0), were more likely to smoke. Students’ social nicotine dependence increased with year of dental study (P = 0.043, β = 0.4, t = 2.0). Social nicotine dependence enhanced tobacco usage among Year-1-to-4 students (P = 0.005, OR = 1.4, 95% CI: 1.1–1.7) but not Year-5 undergraduates (P = 0.432). Conclusions: Social nicotine dependence has become a developing issue in dental education. Tobacco control should be highlighted in the dental curriculum. Future investigations into the effects of dental education on social nocotine dependence and tobacco usage are indicated.
Key words: Undergraduate dental education, social nicotine dependence, smoking
INTRODUCTION
Dentists can play an ideal role in tobacco cessation because they ‘have regular contact with patients, are the first to see the effects of tobacco in the mouth and are the only health professionals who frequently see ‘healthy’ patients’1. A majority of dental practitioners agreed that offering brief smoking cessation advice to patients is a part of their professional responsibility2. Intervention of tobacco cessation in dental settings has shown varying degrees of effectiveness3., 4.. Worldwide dental education organisations have policies encouraging members to provide tobacco cessation service to patients5.
During the current decade, the literature has reported that less than 10% of dentists were smokers6., 7.. Smoking rates among dental undergraduate students remained higher in some recent studies8., 9., 10., 11., 12., 13.. Those dental professionals who smoked provided the intervention of tobacco cessation to their patients less often than those dentists who did not smoke7. A positive attitude towards dentists’ smoking behaviour and a passive attitude towards smoking cessation programmes conducted by dentists were also found in the smoking group of dental students8., 13.. Tobacco usage among dental undergraduate students may consequently, after they become dentists, reduce the frequency and/or effectiveness of tobacco cessation schemes provided to their patients.
Nicotine dependence has been identified as a determinant for effectiveness and/or motivation of smoking abstinence14., 15., 16.. Connections between educational activities and nicotine dependence have been reported10., 14.. Croucher et al.14 demonstrated that those with low physical nicotine dependency succeeded in tobacco cessation with brief encouragement and advice alone, without application of nicotine replacement therapy. A new concept of social nicotine dependence has been defined as ‘a misperception of smoking caused by smokers’ attempts, for example, to deny the ill effects of tobacco and/or to justify themselves by regarding smoking as acceptable cultural and social behavior’16. In a previous publication, a decrease in smoking students’ social nicotine dependence after their attedance at a tobacco-control educational programme at two dental schools was reported10. A correlation between social and physical nicotine dependence has been suggested16.
Since there is a connection between social as well as physical nicotine dependence and a potential to reduce the dependence by education, a survey of social nicotine dependence may explore the relevance of tobacco-control courses in dental education. This paper aimed to investigate dental undergraduate students’ tobacco usage and social nicotine dependence in Australia. A special interest was to identify the role of factors such as age, gender, year of dental education and cohabitants’ smoking status for social nicotine dependence.
MATERIALS AND METHODS
A cross-sectional survey was conducted in an Australian university. Undergraduate students from all 5 years of the dental school were invited to participate. The appropriate research ethics approval was obtained from the university. Occasions were identified when students would attend a lecture together. The lecturers were approached, and permission was sought to survey the students at the end of the lectures. A researcher explained the purpose of the study to the students, sought their consent to participate and assured them of confidentiality.
Data of social nicotine dependence were collected using the Kano Test for Social Nicotine Dependence (KTSND)17. The KTSND is composed of ten items, one of which is reverse-scored, measured on a four-point Likert scale from ‘strongly agree’, ‘somewhat agree’, ‘somewhat disagree’ to ‘strongly disagree’. The possible range of KTSND scores is 0, indicating low social nicotine dependence, to 30, indicating high dependence. The KTSND questionnaire was originally developed in the Japanese language. Firstly it was translated from Japanese into English. The English version was re-translated into Japanese by a different interpreter to check validation. A pilot study was carried out to test the administration of questionnaires. The results confirmed the protocol was feasible and the translation was adequate.
Each student completed a self-administered questionnaire. Questions regarding age, gender, year of dental education, personal smoking experience and cohabitants’ smoking status were also included. Completion of the questionnaire took 5–10 minutes. Upon completion, participants were given identical envelopes in which to seal their questionnaires. This was to ensure students’ anonymity when they returned the questionnaires to the researcher.
Data entry and statistical analysis were carried out with the IBM SPSS Statistics (version 19.0, IBM Corporation, Somers, NY, USA). Data analysis included frequency distribution and cross tabulation. Tobacco usage status was separated as current smokers and non-smokers (comprising former smokers and those who had never smoked). A binary logistic regression method was used to establish a relationship between current tobacco usage and potential factors. Stepwise linear regression analysis was conducted to identify covariates of KTSND scores. The level of significance was set at 5%.
RESULTS
Two hundred and sixty students were invited to participate, based on the registration records of the dental school in the first academic semester of 2008. Five of the 260 students were absent from school on the days of questionnaire administration. Of the 255 questionnaires that were returned, 252 were completed fully for a response rate of 96.9%; 147 participants were female (58.3%), and 105 (41.7%) were male. Students’ age ranged from 17 to 36, with a mean of 20.9 (SD = 3.1). Sixty-four undergraduate students were living with tobacco users (25.4%), whilst 188 did not have smoking cohabitants (74.6%).
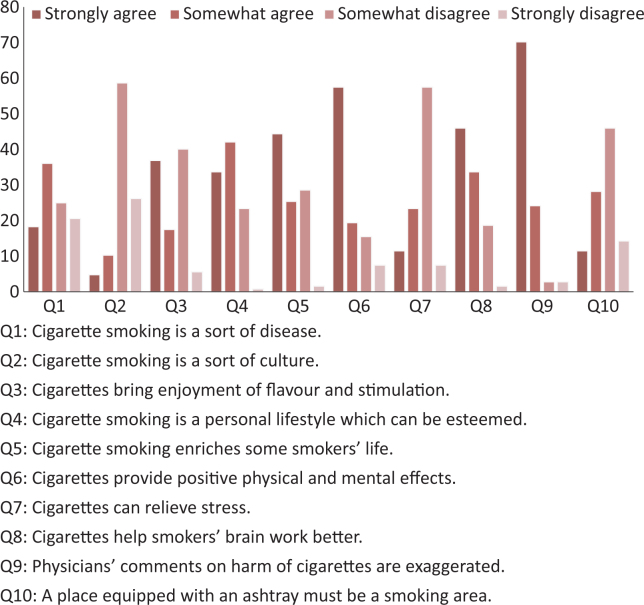
The current smoking rate in the sample was 4.8% (95% CI: 2.6–8.4). When including former smokers, the prevalence of tobacco usage was 7.1% (95% CI: 4.4–11.2). Cronbach’s alpha which measured the internal consistency of the 10 KTSND items was 0.7. This indicated an acceptable reliability. Figure 1 illustrates the outcomes of individual KTSND items.
Figure 1.
Percentage distribution of outcomes of individual KTSND items in the sample of the study (n = 252).
The mean of the KTSND scores was 11.6 (95% CI: 11.1–12.1). Current smokers and non-smokers (comprising former smokers and those who had never smoked) showed a mean KTSND score at 15.3 (95% CI: 12.5–18.2) and 11.4 (95% CI: 10.9–11.9), respectively (Table 1). Dental undergraduate students that reported a higher KTSND score (P = 0.001, OR = 1.3, 95% CI: 1.1–1.6), or that had smoking cohabitants (P = 0.016, OR = 4.8, 95% CI: 1.3–17.0), were more likely to be current smokers (Tables 1 and 2). Thus, scoring 30 points in KTSND was 5,557.8 times the smoking probablity of scoring 0 point (95% CI: 30.0–1,060,510.4). Age, gender and year of dental education were not associated with current tobacco usage (P ≥ 0.359).
Table 1.
Relationship of current tobacco usage and KTSND scores in the sample of the study (n = 252)
| Smoker | Non-smoker† | All | OR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Mean KTSND score (95% CI) | 15.3 (12.5–18.2) | 11.4 (10.9–11.9) | 11.6 (11.1–12.1) | 1.3 (1.1–1.6) | 0.001* |
P < 0.05.
Comprising former smokers and those who had never smoked.
Table 2.
Frequency distribution of current tobacco usage by gender, year of dental education and cohabitants’ smoking status in the sample of the study (n = 252)
| Smoker | Non-smoker† | All | OR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 7 (4.8%) | 140 (95.2%) | 147 (58.3%) | 1 | |
| Male | 5 (4.8%) | 100 (95.2%) | 105 (41.7%) | 1.0 (0.3–3.2) | 1.000 |
| Year of dental education | |||||
| First | 2 (3.6%) | 53 (96.4%) | 55 (21.8%) | 1 | |
| Second | 2 (3.1%) | 63 (96.9%) | 65 (25.8%) | 0.8 (0.1–6.2) | 0.865 |
| Third | 4 (8.3%) | 44 (91.7%) | 48 (19.0%) | 2.4 (0.4–13.8) | 0.323 |
| Fourth | 2 (5.1%) | 37 (94.9%) | 39 (15.5%) | 1.4 (0.2–10.6) | 0.725 |
| Fifth | 2 (4.4%) | 43 (95.6%) | 45 (17.9%) | 1.2 (0.2–9.1) | 0.838 |
| Cohabitants’ smoking status | |||||
| Without smoking cohabitants | 6 (3.2%) | 180 (96.8%) | 186 (74.4%) | 1 | |
| With smoking cohabitants | 6 (9.4%) | 58 (90.6%) | 64 (25.6%) | 4.8 (1.3–17.0) | 0.016* |
P < 0.05.
Comprising former smokers and those who had never smoked.
The population was further divided into two groups, Year-1-to-4 and Year-5 students, according to the degree of exposure to clinical practice. Those junior-year students who had a higher KTSND score were more likely to smoke (P = 0.005, OR = 1.4, 95% CI: 1.1–1.7). Living with smokers was marginally related to current tobacco usage (P = 0.079, OR = 4.7, 95% CI: 0.8–26.7). Age, gender and year of dental study were not associated with junior-year students’ smoking status (P ≥ 0.306). Year-5 students’ current tobacco usage was somewhat associated with age (P = 0.098, OR = 1.4, 95% CI: 0.9–2.0). KTSND scores, gender and smoking cohabitants did not have an influence on senior-year students’ smoking status (P ≥ 0.432).
Students that were undertaking a higher year of dental study displayed a higher KTSND score (P = 0.043, β = 0.4, t = 2.0). Age, gender and cohabitants’ smoking status were not related to KTSND scores (P ≥ 0.149). Table 3 compares the mean KTSND scores by gender, year of dental education and cohabitants’ smoking status.
Table 3.
Comparison of mean KTSND scores by gender, year of dental education and cohabitants’ smoking status in the sample of the study (n = 252)
| Mean KTSND Score (95% CI) | P-value | |
|---|---|---|
| Year of dental education | ||
| First | 10.9 (9.6–12.2) | 0.043* |
| Second | 10.3 (9.2–11.4) | |
| Third | 13.7 (12.6–14.8) | |
| Fourth | 11.9 (10.7–13.2) | |
| Fifth | 11.8 (10.7–12.9) | |
| Gender | ||
| Male | 12.1 (11.2–12.9) | 0.149 |
| Female | 11.3 (10.6–11.9) | |
| Cohabitants’ smoking status | ||
| With smoking cohabitants | 10.9 (9.9–11.9) | 0.173 |
| Without smoking cohabitants | 11.8 (11.1–12.4) | |
P < 0.05.
DISCUSSION
Undergraduate students’ smoking rate observed in this Australian dental school was lower than that reported by some researchers8., 9., 10., 11., 12., 13., although this resembled the findings from dental institutions in Taiwan10, Thailand12 and India12. The rate was also much lower than that among the general population in Australia18. A similar gap between dental undergraduate students and the general population has been displayed in an Irish sample11. This disagreed with a study which suggested a similar smoking rate between the two populations in Italy9.
The mean KTSND score observed in this population is in agreement with previous studies based on samples of dental students10 and the general population16., 17.. Compared with the difference of smoking rates between dental undergraduate students and the general population, a gap for social nicotine dependence was not found. Furthermore, this study showed that KTSND scores were highly associated with smoking behaviour, assenting to former findings10., 16., 17.. This suggested that social nicotine dependence is a developing issue in dental education.
The year of dental study was not associated with the smoking rate at this school. This disagrees with some papers that have reported a higher smoking rate among senior-year students8., 9.. Since approximately 2% of the students were former smokers in this study, consistency of the smoking rate among dental years could be due to a similarly low percentage of senior-year students’ initiation of tobacco usage. This assumption agrees with Haresaku et al.13 who demonstrated an effect of having information about tobacco in the dental curriculum on the protection of smoking initiation other than the induction of cessation, based on an unchanged smoking rate amongst the same dental students in two surveys at a 3-year interval.
This study demonstrated a positive relationship between the year of dental study and social nicotine dependence. Because KTSND scores were not associated with age in this population, this indicated a connection between senior-year students’ high KTSND scores and the dental education that they have received. On the other hand, the current smoking rate did not increase with the year of dental study even though senior-year students had higher social nicotine dependence than junior-year students. Since the smoking rate was related to social nicotine dependence other than age, the reason why senior-year students’ higher social nicotine dependence failed to result in a higher smoking rate can be ascribed to dental education. In this study, signifcant contribution of social nicotine dependence to tobacco usage amongst the Year-1 to -4 students but not the Year-5 students further confirmed the effect of dental education on tobacco control.
As this research used a cross-sectional study method, a cause-result sequence could not be confirmed directly. Further research is required to explore changes in smoking behaviour and social nicotine dependence following each year of dental education.
CONCLUSIONS
This study has manifested a key role of dental education on dental undergraduate students’ tobacco control by disclosing that senior-year students’ higher social nicotine dependence did not predispose to smoking. In addition, evaluation of social nicotine dependence with the English version of the KTSND has been confirmed to be feasible.
Social nicotine dependence has become a relevant issue in dental education. Tobacco control should be highlighted in the dental curriculum to benefit students, dental professionals, patients and the community. Further investigations into the effects of dental education on social nocotine dependence and smoking behaviour are indicated.
Acknowledgements
This study was supported by a Rankine Memorial Fund Grant from the University of Western Australia. The authors would like to show appreciation to the Rankine Bequest and those staff as well as the students who helped and/or participated in this project.
REFERENCES
- 1.Beaglehole RH. Tobacco control and the dental profession: time for action. Dev Dent. 2004;5:13–15. [Google Scholar]
- 2.Stacey F, Heasman PA, Heasman L, et al. Smoking cessation as a dental intervention – views of the profession. Br Dent J. 2006;201:109–113. doi: 10.1038/sj.bdj.4813829. [DOI] [PubMed] [Google Scholar]
- 3.Gordon JS, Severson HH. Tobacco cessation through dental office settings. J Dent Educ. 2001;65:354–363. [PubMed] [Google Scholar]
- 4.Hanioka T, Ojima M, Tanaka H, et al. Intensive smoking-cessation intervention in the dental setting. J Dent Res. 2010;89:66–70. doi: 10.1177/0022034509350867. [DOI] [PubMed] [Google Scholar]
- 5.Gordon JS, Albert DA, Crews KM, et al. Tobacco education in dentistry and dental hygiene. Drug Alcohol Rev. 2009;28:517–532. doi: 10.1111/j.1465-3362.2009.00108.x. [DOI] [PubMed] [Google Scholar]
- 6.Smith DR, Leggat PA. Tobacco smoking prevalence among a cross-section of dentists in Queensland, Australia. Kurume Med J. 2005;52:147–151. doi: 10.2739/kurumemedj.52.147. [DOI] [PubMed] [Google Scholar]
- 7.Crews KM, Sheffer CE, Payne TJ, et al. A survey of oral and maxillofacial surgeons’ tobacco-use-related knowledge, attitudes and intervention behaviors. J Am Dent Assoc. 2008;139:1643–1651. doi: 10.14219/jada.archive.2008.0106. [DOI] [PubMed] [Google Scholar]
- 8.Furukawa S, Tokunaga R, Abe S, et al. Dental students’ smoking behavior and their attitude towards smoking. Kokubyo Gakkai Zasshi. 2005;72:201–208. doi: 10.5357/koubyou.72.201. [DOI] [PubMed] [Google Scholar]
- 9.Pizzo G, Licata ME, Piscopo MR, et al. Attitudes of Italian dental and dental hygiene students toward tobacco-use cessation. Eur J Dent Educ. 2010;14:17–25. doi: 10.1111/j.1600-0579.2009.00587.x. [DOI] [PubMed] [Google Scholar]
- 10.Inagaki K, Hayashi J, Ting CC, et al. Dental undergraduates’ smoking status and social nicotine dependence in Japan and Taiwan – comparison between two dental schools. Jpn J Tob Control. 2008;3:81–85. [Google Scholar]
- 11.McCartan B, McCrear C, Healy C. Attitudes of Irish dental, dental hygiene and dental nursing students and newly qualified practitioners to tobacco use cessation: a national survey. Eur J Dent Educ. 2008;12:17–22. doi: 10.1111/j.1600-0579.2007.00466.x. [DOI] [PubMed] [Google Scholar]
- 12.Warren CW, Jones NR, Chauvin J, et al. GTSS Collaborative Group. Tobacco use and cessation counselling: cross-country. Data from the Global Health Professions Student Survey (GHPSS), 2005-7. Tob Control. 2008;17:238–247. doi: 10.1136/tc.2007.023895. [DOI] [PubMed] [Google Scholar]
- 13.Haresaku S, Hanioka T, Yamamoto M, et al. Impact of a tobacco curriculum on smoking behaviour and attitudes toward smoking in dental students in Japan: a three-year follow-up study. Int Dent J. 2010;60:99–105. [PubMed] [Google Scholar]
- 14.Croucher R, Islam S, Jarvis MJ, et al. Oral tobacco cessation with UK resident Bangladeshi women: a community pilot investigation. Health Educ Res. 2003;18:216–223. doi: 10.1093/her/18.2.216. [DOI] [PubMed] [Google Scholar]
- 15.Dale LC, Glover ED, Sachs DP, et al. Bupropion for smoking cessation: predictors of successful outcome. Chest. 2001;119:1357–1364. doi: 10.1378/chest.119.5.1357. [DOI] [PubMed] [Google Scholar]
- 16.Otani T, Yoshii C, Kano M, et al. Validity and reliability of Kano Test for Social Nicotine Dependence. Ann Epidemiol. 2009;19:815–822. doi: 10.1016/j.annepidem.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Yoshii C, Kano M, Isomura T, et al. Innovative questionnaire examining psychological nicotine dependence, “The Kano Test for Social Nicotine Dependence (KTSND)”. J UOEH. 2006;28:45–55. doi: 10.7888/juoeh.28.45. [DOI] [PubMed] [Google Scholar]
- 18.Winstanley M, White V. In: Tobacco in Australia: Facts and Issues. 3rd ed. Scollo MM, Winstanley MH, editors. Cancer Council Victoria; Melbourne: 2008. Chapter 1. Trends in the prevalence of smoking. Available from: http://www.tobaccoinaustralia.org.au/chapter-1-prevalence. Accessed 28 September 2010. [Google Scholar]